
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Phys., 22 July 2022
Sec. Social Physics
Volume 10 - 2022 | https://doi.org/10.3389/fphy.2022.941181
This article is part of the Research TopicNetwork Mining and Propagation Dynamics AnalysisView all 17 articles
 Mingming Zhao1†
Mingming Zhao1† Xing Liu1†
Xing Liu1† Ming Yuan2
Ming Yuan2 Ying Yang3
Ying Yang3 Hao Chen1
Hao Chen1 Mengmeng Li1
Mengmeng Li1 Pan Luo1
Pan Luo1 Yong Duan1
Yong Duan1 Jie Fan1,4
Jie Fan1,4 Leqi Liu5
Leqi Liu5 Li Zhou1*
Li Zhou1*Previous studies have demonstrated that short-term exposure to ambient air pollution was associated with hospital admissions for cardiovascular diseases, but the evidence of its effects on acute myocardial infarction (AMI) in East Asian countries is limited and inconsistent. We aimed to investigate the association between air pollution and AMI hospitalizations in Chongqing, China. This time-stratified case-crossover study included 872 patients with AMI from three hospitals in Chongqing from January 2015 to December 2016. Exposures were compared between days with AMI (case days) and days without AMI (control days). Spearman’s correlation coefficient was applied to explore the correlation between air pollutants and meteorological conditions. Conditional logistic regression was used to assess the associations between air pollution exposure with different lag periods and AMI hospitalizations. Stratification analysis was further implemented by sex, age, and season. Hospitalizations for AMI were signifficantly associated with air pollution. All analyzed air pollutants showed lag-specific at lag 0 day and lag 01 day, whereas a 10 μg/m3 increase of average concentrations in PM2.5, PM10, SO2, NO2, and CO was associated with 1.034% (95% CI: 1.003–1.067%), 1.035% (95% CI:1.015–1.056%), 1.231% (95% CI: 1.053–1.438%), 1.062% (95% CI: 1.018–1.107%), and 1.406% (95% CI: 1.059–1.866%) increase in hospitalizations for AMI, respectively. No effect modifications were detected for sex, age, and season. Our findings suggest that short-term exposure to PM2.5, PM10, SO2, NO2, and CO contributes to increase AMI hospitalizations, which have public health implications for primary prevention and emergency health services.
Acute myocardial infarction (AMI) is a specific manifestation of coronary artery disease which has the characteristics of arrhythmias, heart failure, and angina pectoris with typical distribution [1]. As with the common heart attack event, the global fatality rate of AMI is estimated at more than 2.4 million deaths in the United States, more than four million fatalities in Europe and northern Asia, and is higher in most industrialized countries and low-income countries [2]. In China, AMI has a significant fatality rate and a large economic burden, where it is responsible for over 0.6 million deaths annually [3].
It was previously reported that the underlying influencing factors of AMI may involve genetic background, emotional state, and socioeconomic status, which have been found to be significantly and positively associated with the incidence and pathogenic condition [4], wherea, recent epidemiological studies have reported an association between ambient air pollution and AMI. In Europe, a comprehensive meta-analysis that included 17 time-series studies and 17 case-crossover studies suggested that all the main air pollutants (with the exception of ozone) were significantly associated with an increase in AMI risk [5]. In addition, a time-stratified case-crossover research conducted in England showed significant correlations [6]. It has been shown that ambient air pollution has been connected to deleterious effects on cardiovascular mortality. Furthermore, ambient air pollution has been linked to elevated risks of AMI, including worsening pre-existing symptoms and exacerbating the development of atopic diseases [7–10]. Environmental variables are also thought to be responsible for 24% of global morbidity and 23% of mortality, according to the World Health Organization. Given the ongoing interaction between human beings and the environment, variables such as air pollutants may be potential predictors of cardiovascular diseases [11, 12].
Over the past few decades, the evidence linking air pollution to cardiovascular disease has grown substantially. A time-series study that covered 16 administrative districts of Beijing found an ambient particulate matter of diameter ≤10 µm (PM10), and nitrogen dioxide (NO2) had a significant influence on deaths from cardiovascular diseases [13]. Another cross-sectional study in Shanghai suggested that the particulate matter of diameter ≤2.5 µm (PM2.5) was significantly associated with increased AMI risk on a concurrent day [14]. Meanwhile, Yu’s research about significant adverse effects focused on the city of Guangzhou, which is the central city of South China, and this study found that increased daily levels of PM2.5 increase the daily morbidity of myocardial infarction [15].
All the aforementioned studies indicated that exposure to air pollutants may trigger AMI symptoms or development; however, most of these studies were conducted in the coastal region, and there are currently no studies on heavy industry cities such as Chongqing in inland China. Chongqing is different from the countries or regions mentioned earlier, which are mainly related to the light industry and tertiary industry. The secondary sector in Chongqing accounts for 40% of the total, according to the 2021 Economic Development report, and its value-added has climbed by 4.9 percent. Furthermore, the medical care visits for AMI are clinically meaningful and need to be evaluated for potentially differentiated effects of air pollution in southwest China.
Therefore, this study has selected a major heavy industry city in China as the research site. We conducted a case-crossover analysis to evaluate the associations between short-term exposure to major air pollutants and daily hospital admissions for AMI in Chongqing, a non-coastal region in southwest China.
Data on daily hospitalizations for AMI from 1 January 2015 to 31 December 2016 were extracted from three top-level and general hospitals (the Second Affiliated Hospital of Chongqing Medical University, the University-Town Hospital of Chongqing Medical University, and the Southeast Hospital) with approximately 3,500, 1,500, and 1,200 inpatient beds, respectively. The AMI (the International Classification of Diseases-10 codes: I21) hospitalization was defined as our study outcome. For each AMI death case, we retrieved information on age at hospital admission, sex, diagnosis, dates of admission, and admitted hospital. All the medical information was recorded on the Platform of Medical Data Science Academy of Chongqing Medical University.
We used a time-stratified case-crossover design, which has been widely applied to investigate the acute effects of air pollution on various health outcomes, to examine the relationship between short-term exposure to air pollution and AMI hospitalizations [16, 17]. To control the potential confounding effects of day of the week, long-term trend, and seasonality, the ambient air exposure on the case day (admission day) was matched with the exposure on a series of reference days within the same month on the same day of the week for each AMI case [18].
We obtained daily mean concentrations of PM2.5, PM <10 µm in aerodynamic diameter (PM10), sulfur dioxide (SO2), nitrogen dioxide (NO2), and carbon monoxide (CO) between 1 January 2015 and 31 December 2016 from the National Urban Air Quality Real-Time Publishing Platform in China. In Chongqing, there were 17 air pollution monitoring stations. Due to the high number of missing data at some monitoring stations, 14 monitoring sites were finally retained. To assess air pollutant exposures, we used the inverse distance weighting (IDW) method. Specifically, the Baidu Maps API (http://lbsyun.baidu.com/) was used to geocode the locations of all monitoring and hospital addresses. To analyze the IDW method’s performance in the exposure assessment, we used a 10-fold cross-validation procedure and estimated the coefficient of determination (R2) and root mean square error based on the observed and projected concentrations across the research period. For each AMI case, we calculated the predicted concentration of his/her inpatient hospital as an inverse distance weighted average of concentrations (1/d2) at all monitoring stations on each of the case and control days. In the present study, we estimated single-day lag exposures (lag 1 day to lag 5 days) and moving average day exposures (lag 01 day to lag 05 days).
Weather conditions including daily mean temperature and mean relative humidity were sourced from the National Meteorological Information Centre of China and weather conditions were included in all models to account for their potential confounding effects. We did not take into account the other individual-level covariates, including sex, age, and marital status, because they were held constant in comparing case days to the corresponding control days.
Spearman’s correlation coefficient was applied to investigate the correlation between air pollutants and meteorological conditions. Conditional logistic regression was used to assess the associations between air pollution exposure with different lag periods and AMI hospitalizations. Daily average temperature and relative humidity were included as natural cubic spline functions (with a df of 6 and 3, respectively) in all models to account for potential confounding by meteorologic conditions. The risk estimates were expressed in terms of the odds ratio in AMI hospitalizations per 10 μg/m3 increment of air pollutants (except that CO was per 1 mg/m3) and their respective 95% confidence intervals (CIs). Stratified and sensitivity analyses were performed on the basis of reaching the maximum effect of PM2.5, PM10, SO2, NO2, and CO in the moving average lag structure.
We explored the potential effect modification of AMI risk by age (≥75 years and <75 years), gender, and season (warm season as 1 April to 30 September and cold season as 1 October to 31 March). The statistical significance of subgroup differences was assessed as
The robustness of our results was evaluated by several sensitivity analyses. First, we fitted a two-pollutant model to exclude the confounding effects of other pollutants. However, correlation coefficients >0.5 were not included to avoid collinearity. Second, the degrees of freedom for temperature and humidity are selected as 4–6 and 7–9, respectively. All analyses were performed using R version 3.6.3. P-value less than 0.05 was considered statistically significant.
There were 872 cases of AMI between 1 January 2015 and 31 December 2016 from the Platform of Medical Data Science Academy of Chongqing Medical University. Table 1 summarized the statistics on AMI patients during the study period. Of the 872 AMI patients, 582 (66.7%) were male and 409 (46.9%) were female, hospitalized in the cold season. The mean age at hospital admission was 75.38 years, and 56.0% of the cases were ≥75 years old.
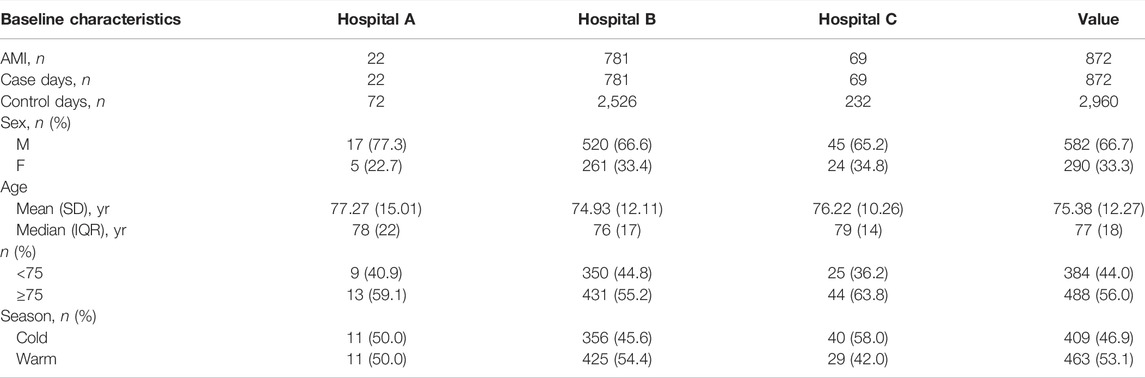
TABLE 1. Distribution of daily AMI admissions and meteorological factors in Chongqing, China (January 2015–December 2016).
Table 2 shows the distributions of air pollutants and meteorological conditions. The mean exposures to PM2.5, PM10, SO2, NO2, and CO were 58.170 μg/m3, 94.046 μg/m3, 113.631 μg/m3, 61.410 μg/m3, and 0.998 mg/m3, respectively. The annual average temperature and relative humidity were 20°C and 75%, respectively, refflecting the typical subtropical climate of Chongqing.
Spearman’s correlation coefficients between air pollutants and meteorological factors are listed in Table 3. PM2.5, PM10, and CO were positively and moderately correlated, while SO2 and NO2 displayed a weak correlation with other air pollutants. Temperature was negatively associated with PM10. Relative humidity was negatively associated with NO2 but not statistically associated with other air pollutants.
Figure 1 (risk of AMI cases for each pollutant at various lags) lists ORs in daily admissions for AMI associated with 10 μg/m3 increase in air pollutant concentrations for different lag structures. All analyzed air pollutants showed consistent significant associations at lag 0 day and lag 01 day. The ORs of PM2.5, PM10, SO2, NO2, and CO peaked at the lag 02 days, lag 0 day, lag 02 days, lag 0 day, lag 01 day, and the corresponding values were 1.034 (95% CI: 1.003–1.067), 1.035 (95% CI: 1.015–1.056), 1.231 (95% CI: 1.053–1.438), 1.062 (95% CI: 1.018–1.107), and 1.406 (95% CI: 1.059–1.866), respectively. The estimated effects in 10 μg/m3 increments are presented in Supplementary Table S1.
The associations between air pollutant exposures and the hospitalizations for AMI were evaluated in the subgroups based on sex, age, and season (Table 4). Although the ORs for PM2.5, PM10, NO2, SO2, and CO varied to some extent, no significant effect modification by sex, age, or season was observed (all p for effect modification >0.05).
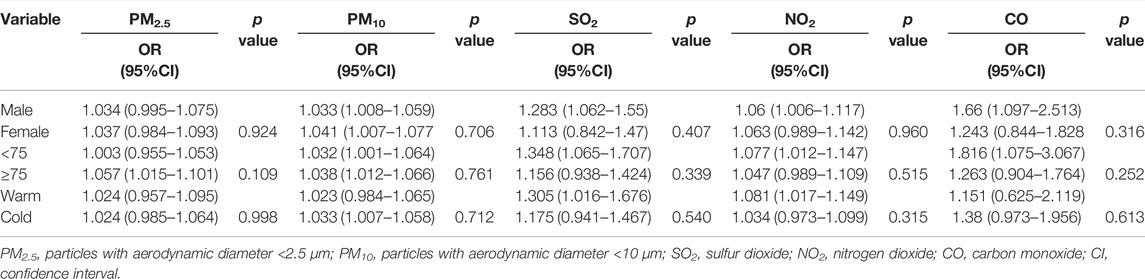
TABLE 4. Risks for AMI hospitalizations with per 10 μg/m3 increase of exposure to PM2.5, PM10, SO2, NO2, and except that CO was per 1 mg/m3 stratified by age, sex, and season.
Table 5 provides the results of the two-pollutant model. When adjusting for co-pollutants, the effect estimates for PM10, NO2, SO2, and CO were slightly reduced but remained statistically significant, and further adjustment for other pollutant exposures did not materially change the associations between PM2.5 exposures and AMI. Sensitivity analysis is presented in Supplementary Table S2. The use of an alternative df value for temperature (4–6) and relative humidity (7–9) had no significant effect on the effect estimates of the associations between air pollution and daily hospital admissions for AMI.
Over the past few decades, a growing body of epidemiological and clinical evidence has raised concerns about the inffluence of air pollution on cardiovascular health in the context of global environmental change, but the data in developing countries are still limited, especially in East Asia. Chongqing is a major heavy industry city with a population of more than 8.6 million in southwest China, and its basin structure has a great impact on ambient air pollution. Therefore, we conducted this time-stratified case-crossover study to evaluate the short-term effects of ambient air pollutants on hospitalizations for AMI in Chongqing.
In the present study, we identified that ambient air pollutants were associated with hospitalizations for AMI. The data indicated that short-term exposure to PM2.5, PM10, SO2, NO2, and CO was significantly associated with increased clinical visits for AMI. In the single-pollutant models, we found that each 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, and CO was associated with a 1.03, 1.03, 1.23, 1.06, and 1.41% increase in AMI hospitalizations, respectively. In the two-pollutant models, the estimated effects of PM10, SO2, and NO2 were all statistically significant when adjusting for co-pollutants. Also all the air pollutants and meteorological factors showed lag effects in the present study. Despite the relatively small effect sizes of unit changes in exposure variables, our results still have considerable public health implications due to ubiquitous exposure. Our results contribute to the limited scientific evidence that ambient air pollution and meteorological factors may influence the incidence of AMI.
It was indicated that air pollutants were positively associated with AMI incidence in previous similar studies [19–21]. For example, a study conducted in Brisbane city has shown that AMI hospitalizations increased by 12.34% (95% CI: 1.44–24.42%) per 10 μg/m3 increase in PM2.5 [19]. Another case-crossover research on fine particulate air pollution and AMI hospitalization rate in 26 Chinese cities also indicated that short-term elevations in PM2.5 concentration may increase the risk of STEMI [20]. Meanwhile, a European multicenter cohort study reported that cardiac readmissions increased by 1.014% (95% CI: 1.001–1.026%) per 200 microg/m3 increase in CO and increased by 1.032% (95% CI: 1.013–1.051) for per 8 microg/m3 NO2 [21].
In China, the evidence of the effects of air pollutant exposure on AMI risk is still controversial in the previous studies. A research study in Hubei province was also a retrospective study with a similar theme but with different observational outcomes [17]. They discovered that short-term elevations of PM and NO2 can increase AMI mortality, and the difference in dependence time lags may be related to different observational outcomes or variation in PM2.5 constituents across. Meanwhile, a study conducted in Hongkong found that PM10 and NO2 were significantly and positively associated with AMI hospitalizations both in the single-pollutant model and multipollutant model [22]. Another research study conducted in Shanghai indicated that PM10, SO2, and NO2 were related to visit for AMI [23], which was consistent with our results. However, a research study from Changzhou observed a negative association between ambient NO2 concentrations and AMI hospitalizations [15]. In addition, several other studies in China found no association between CO, SO2, and AMI risk [24–26].
The reason why the change of air quality index concentration in this study affects the change in AMI hospitalization rate can be explained from both medical and environmental aspects. On the one hand, according to the recent mechanistic studies in cells and animal models, the positive association between air pollution and AMI was biologically plausible [27–29]. In addition to inflammatory effects [30], ambient air pollutants have been linked to arterial vasoconstriction and decreased heart rate variability [31]. Air pollutants could aggravate the cardiopulmonary symptoms of AMI or weaken the protection of the respiratory system. Among these hypotheses is the possibility that particles could directly induce the production of reactive oxygen species, resulting in oxidative stress, damage, and inflammation reactions in the immune system [32, 33]. On the other hand, a series of environmental studies have proven that atmospheric aerosol is a composite of various inorganic and organic components, and its physical and chemical properties under the fluctuating environmental conditions determine its impact on air quality and human health [34–37]. Aerosol particles such as PM2.5 and their precursors can have a significant impact on air quality, the ozone layer, and climate on scales ranging from regional to global as anthropogenic activities increase. In terms of PM2.5 particle composition, the creation of PM2.5 particles from atmospheric pollutants (NOx, SO2, etc.) heterogeneously interacted with and condensed on the surfaces of other aerosols in the atmosphere is a process that accelerates toxic gas deposition [38]. Under high relative humidity circumstances, H2O is both a major component of PM2.5 and speeds up the transformation and deposition of accumulated hazardous gases. In this study, we verified the correlation between relative humidity and air pollutants, and the relationships also are rationally followed through other studies [39]. Apart from water-soluble ions, PM2.5 mainly contains sulfate–nitrate–ammonium (SNA) ions, and the sulfate and nitrate are formed by their precursors SO2 and NOx, respectively [40]. High levels of reactive oxygen species (ROS) can be generated from environmentally persistent-free radicals (EPFRs) in PM2.5, and atmospheric pollutants can boost the radical production and EPFR degradation rates through photochemical processes. The capacity of ambient PM to generate ROS can be a reliable predictor of particle-induced unfavorable health effects [41]. It has been shown above that SNA and organic matter can promote the formation of haze and are the main chemical components in the pollution events. That is to say, it proves the relationship between CO, NO2, or SO2 studied in this article, and the relationship between toxic gases accelerates their transformation and deposition. When its emissions increase, it promotes the generation of aerosols and changes the physical and chemical properties of atmospheric aerosols, accelerates the deposition of PM2.5 in the lungs, and then affects the incidence of AMI through pathological reactions [42–44].
The acute inffluences of air pollutants and climate factors on AMI hospital visits were investigated based on a large database in Chongqing, China. Chongqing’s high air pollution levels and distinct seasons provided ample opportunities to investigate the effects of environmental risk factors on AMI conditions. Nevertheless, our study has some potential limitations. First, this is the disadvantage of this research that we do not have, according to the residential address, to perform air pollution exposure assessment, and the exposure misclassification results in an underestimation of the sensitivity of air pollution, which might lead to lower statistical power. Second, this time-stratified study is inherently an ecological analysis, which may limit the ability to adjust for the individual confounders and might understate the effects of air pollution. Last, the data were only collected in Chongqing with a subtropical humid climate, and therefore the results of this study can only be generalized to cities with the same environmental and socioeconomical characteristics.
In summary, this study provided clear evidence that ambient air pollution could increase the hospitalization of AMI in Chongqing, China. Further studies from both an epidemiological and a physiological perspective are needed to establish the causal relationship between air pollution, meteorological factors, and AMI.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
MMZ wrote the manuscript and analyzed the data. XL collected and inputted the data. MY, YY, HC, MML, PL, YD, JF, LQL, and LZ reviewed the results and provided guidelines for presentation and interpretation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the Medical Data Science Academy of Chongqing Medical University for providing the population health data.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphy.2022.941181/full#supplementary-material
1. Anderson JL, Morrow DA. Acute Myocardial Infarction. N Engl J Med (2017) 376(21):2053–64. doi:10.1056/nejmra1606915
2. Reed GW, Rossi JE, Cannon CP. Acute Myocardial Infarction. The Lancet (2017) 389(10065):197–210. doi:10.1016/s0140-6736(16)30677-8
3. Xu A, Mu Z, Jiang B, Wang W, Yu H, Zhang L, et al. Acute Effects of Particulate Air Pollution on Ischemic Heart Disease Hospitalizations in Shanghai, China. Int J Environ Res Public Health (2017) 14(2):168. doi:10.3390/ijerph14020168
4. Santurtún A, Sanchez-Lorenzo A, Villar A, Riancho JA, Zarrabeitia MT. The Influence of Nitrogen Dioxide on Arrhythmias in Spain and its Relationship with Atmospheric Circulation. Cardiovasc Toxicol (2017) 17(1):88–96. doi:10.1007/s12012-016-9359-x
5. Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, et al. Main Air Pollutants and Myocardial Infarction: a Systematic Review and Meta-Analysis. JAMA (2012) 307(7):713–21. doi:10.1001/jama.2012.126
6. Butland BK, Atkinson RW, Crichton S, Barratt B, Beevers S, Spiridou A, et al. Air Pollution and the Incidence of Ischaemic and Haemorrhagic Stroke in the South London Stroke Register: a Case-Cross-Over Analysis. J Epidemiol Community Health (2017) 71(7):707–12. doi:10.1136/jech-2016-208025
7. Brunekreef B, Beelen R, Hoek G, Schouten L, Bausch-Goldbohm S, Fischer P, et al. Effects of Long-Term Exposure to Traffic-Related Air Pollution on Respiratory and Cardiovascular Mortality in the Netherlands: the NLCS-AIR Study. Res Rep Health Effects Inst (2009) 139(139):5–71. https://pubmed.ncbi.nlm.nih.gov/19554969/.
8. Kriit HK, Anderson EM, Carlsen HK, Anderson N, Ljungman PLS, Pershagen G, et al. Using Distributed Lag Non-linear Models to Estimate Exposure Lag-Response Associations between Long-Term Air Pollution Exposure and Incidence of Cardiovascular Disease. Int J Environ Res Public Health (2022) 19(5). doi:10.3390/ijerph19052630
9. Stockfelt L, Andersson EM, Molnár P, Gidhagen L, Segersson D, Rosengren A, et al. Long-term Effects of Total and Source-specific Particulate Air Pollution on Incident Cardiovascular Disease in Gothenburg, Sweden. Environ Res (2017) 158:61–71. doi:10.1016/j.envres.2017.05.036
10. Stockfelt L, Andersson EM, Molnár P, Rosengren A, Wilhelmsen L, Sallsten G, et al. Long Term Effects of Residential NOx Exposure on Total and Cause-specific Mortality and Incidence of Myocardial Infarction in a Swedish Cohort. Environ Res (2015) 142:197–206. doi:10.1016/j.envres.2015.06.045
11. Li Q, Yang Y, Chen R, Kan H, Song W, Tan J, et al. Ambient Air Pollution, Meteorological Factors and Outpatient Visits for Eczema in Shanghai, China: A Time-Series Analysis. Int J Environ Res Public Health (2016) 13(11). doi:10.3390/ijerph13111106
12. Royé D, Zarrabeitia MT, Fdez-Arroyabe P, Álvarez Gutiérrez A, Santurtún A. Role of Apparent Temperature and Air Pollutants in Hospital Admissions for Acute Myocardial Infarction in the North of Spain. Revista Española de Cardiología (English Edition) (2019) 72(8):634–40. doi:10.1016/j.rec.2018.07.009
13. Li W, Cao Y, Li R, Ma X, Chen J, Wu Z, et al. The Spatial Variation in the Effects of Air Pollution on Cardiovascular Mortality in Beijing, China. J Expo Sci Environ Epidemiol (2018) 28(3):297–304. doi:10.1038/jes.2016.21
14. Hu J, Tang M, Zhang X, Ma Y, Li Y, Chen R, et al. Size-fractionated Particulate Air Pollution and Myocardial Infarction Emergency Hospitalization in Shanghai, China. Sci Total Environ (2020) 737:140100. doi:10.1016/j.scitotenv.2020.140100
15. Yu Y, Yao S, Dong H, Ji M, Chen Z, Li G, et al. Short-term Effects of Ambient Air Pollutants and Myocardial Infarction in Changzhou, China. Environ Sci Pollut Res (2018) 25(22):22285–93. doi:10.1007/s11356-018-2250-5
16. Carracedo-Martínez E, Taracido M, Tobias A, Saez M, Figueiras A. Case-crossover Analysis of Air Pollution Health Effects: a Systematic Review of Methodology and Application. Environ Health Perspect (2010) 118(8):1173–82. doi:10.1289/ehp.0901485
17. Liu Y, Pan J, Fan C, Xu R, Wang Y, Xu C, et al. Short-Term Exposure to Ambient Air Pollution and Mortality from Myocardial Infarction. J Am Coll Cardiol (2021) 77(3):271–81. doi:10.1016/j.jacc.2020.11.033
18. Bateson TF, Schwartz J. Control for Seasonal Variation and Time Trend in Case-Crossover Studies of Acute Effects of Environmental Exposures. Epidemiology (1999) 10(5):539–44. doi:10.1097/00001648-199909000-00013
19. Cheng J, Tong S, Su H, Xu Z. Hourly Air Pollution Exposure and Emergency Department Visit for Acute Myocardial Infarction: Vulnerable Populations and Susceptible Time Window. Environ Pollut Barking, Essex (1987) 288:2021117806.
20. Liu H, Tian Y, Cao Y, Song J, Huang C, Xiang X, et al. Fine Particulate Air Pollution and Hospital Admissions and Readmissions for Acute Myocardial Infarction in 26 Chinese Cities. Chemosphere (2018) 192:282–8. doi:10.1016/j.chemosphere.2017.10.123
21. von Klot S, Peters A, Aalto P, Bellander T, Berglind N, D’Ippoliti D, et al. Ambient Air Pollution Is Associated with Increased Risk of Hospital Cardiac Readmissions of Myocardial Infarction Survivors in Five European Cities. Circulation (2005) 112(20):3073–9. doi:10.1161/circulationaha.105.548743
22. Yu IT-s., Qiu H, Wang X, Tian L, Tse LA. Synergy between Particles and Nitrogen Dioxide on Emergency Hospital Admissions for Cardiac Diseases in Hong Kong. Int J Cardiol (2013) 168(3):2831–6. doi:10.1016/j.ijcard.2013.03.082
23. Xie J, He M, Zhu W. Acute Effects of Outdoor Air Pollution on Emergency Department Visits Due to Five Clinical Subtypes of Coronary Heart Diseases in Shanghai, china. J Epidemiol (2014) 24(6):452–9. doi:10.2188/jea.je20140044
24. Chen C, Wang X, Lv C, Li W, Ma D, Zhang Q, et al. The Effect of Air Pollution on Hospitalization of Individuals with Respiratory and Cardiovascular Diseases in Jinan, China. Medicine (2019) 98(22):e15634. doi:10.1097/md.0000000000015634
25. Goggins WB, Chan EYY, Yang C-Y. Weather, Pollution, and Acute Myocardial Infarction in Hong Kong and Taiwan. Int J Cardiol (2013) 168(1):243–9. doi:10.1016/j.ijcard.2012.09.087
26. Li J, Liu C, Cheng Y, Guo S, Sun Q, Kan L, et al. Association between Ambient Particulate Matter Air Pollution and ST-Elevation Myocardial Infarction: A Case-Crossover Study in a Chinese City. Chemosphere (2019) 219:724–9. doi:10.1016/j.chemosphere.2018.12.094
27. Nemmar A, Hoylaerts MF, Hoet PH, Dinsdale D, Smith T, Xu H, et al. Ultrafine Particles Affect Experimental Thrombosis in an In Vivo Hamster Model. Am J Respir Crit Care Med (2002) 166(7):998–1004. doi:10.1164/rccm.200110-026OC
28. Nemmar A, Nemery B, Hoet PHM, Van Rooijen N, Hoylaerts MF. Silica Particles Enhance Peripheral Thrombosis. Am J Respir Crit Care Med (2005) 171(8):872–9. doi:10.1164/rccm.200409-1202oc
29. Peters A, Dockery DW, Muller JE, Mittleman MA. Increased Particulate Air Pollution and the Triggering of Myocardial Infarction. Circulation (2001) 103(23):2810–5. doi:10.1161/01.cir.103.23.2810
30. Ghio AJ, Kim C, Devlin RB. Concentrated Ambient Air Particles Induce Mild Pulmonary Inflammation in Healthy Human Volunteers. Am J Respir Crit Care Med (2000) 162(3 Pt 1):981–8. doi:10.1164/ajrccm.162.3.9911115
31. Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, Silverman F. Inhalation of fine Particulate Air Pollution and Ozone Causes Acute Arterial Vasoconstriction in Healthy Adults. Circulation (2002) 105(13):1534–6. doi:10.1161/01.cir.0000013838.94747.64
32. Boovarahan SR, Kurian GA. Mitochondrial Dysfunction: a Key Player in the Pathogenesis of Cardiovascular Diseases Linked to Air Pollution. Rev Environ Health (2018) 33(2):111–22. doi:10.1515/reveh-2017-0025
33. Huang SK, Zhang Q, Qiu Z, Chung KF. Mechanistic Impact of Outdoor Air Pollution on Asthma and Allergic Diseases. J Thorac Dis (2015) 7(1):23–33. doi:10.3978/j.issn.2072-1439.2014.12.13
34. Farmer DK, Cappa CD, Kreidenweis SM. Atmospheric Processes and Their Controlling Influence on Cloud Condensation Nuclei Activity. Chem Rev (2015) 115(10):4199–217. doi:10.1021/cr5006292
35. Shiraiwa M, Li Y, Tsimpidi AP, Karydis VA, Berkemeier T, Pandis SN, et al. Global Distribution of Particle Phase State in Atmospheric Secondary Organic Aerosols. Nat Commun (2017) 8:15002. doi:10.1038/ncomms15002
36. Kuwata M, Martin ST. Phase of Atmospheric Secondary Organic Material Affects its Reactivity. Proc Natl Acad Sci U.S.A (2012) 109(43):17354–9. doi:10.1073/pnas.1209071109
37. Brunekreef B, Holgate ST. Air Pollution and Health. The Lancet (2002) 360(9341):1233–42. doi:10.1016/s0140-6736(02)11274-8
38. Liang C-S, Duan F-K, He K-B, Ma Y-L. Review on Recent Progress in Observations, Source Identifications and Countermeasures of PM2.5. Environ Int (2016) 86:150–70. doi:10.1016/j.envint.2015.10.016
39. Martin ST. Phase Transitions of Aqueous Atmospheric Particles. Chem Rev (2000) 100(9):3403–54. doi:10.1021/cr990034t
40. Velali E, Papachristou E, Pantazaki A, Choli-Papadopoulou T, Planou S, Kouras A, et al. Redox Activity and In Vitro Bioactivity of the Water-Soluble Fraction of Urban Particulate Matter in Relation to Particle Size and Chemical Composition. Environ Pollut (2016) 208(Pt B):774–86. doi:10.1016/j.envpol.2015.10.058
41. Gehling W, Khachatryan L, Dellinger B. Hydroxyl Radical Generation from Environmentally Persistent Free Radicals (EPFRs) in PM2.5. Environ Sci Technol (2014) 48(8):4266–72. doi:10.1021/es401770y
42. Kampa M, Castanas E. Human Health Effects of Air Pollution. Environ Pollut (2008) 151(2):362–7. doi:10.1016/j.envpol.2007.06.012
43. Franchini M, Mannucci PM. Particulate Air Pollution and Cardiovascular Risk: Short-Term and Long-Term Effects. Semin Thromb Hemost (2009) 35(7):665–70. doi:10.1055/s-0029-1242720
Keywords: acute myocardial infarction, air pollution, environment, hospitalization, risk factor
Citation: Zhao M, Liu X, Yuan M, Yang Y, Chen H, Li M, Luo P, Duan Y, Fan J, Liu L and Zhou L (2022) Ambient Air Pollution and Hospitalization for Acute Myocardial Infarction in Chongqing, China: A Time-Stratified Case Crossover Analysis. Front. Phys. 10:941181. doi: 10.3389/fphy.2022.941181
Received: 11 May 2022; Accepted: 22 June 2022;
Published: 22 July 2022.
Edited by:
Xuzhen Zhu, Beijing University of Posts and Telecommunications (BUPT), ChinaReviewed by:
Yuewei Liu, Sun Yat-sen University, ChinaCopyright © 2022 Zhao, Liu, Yuan, Yang, Chen, Li, Luo, Duan, Fan, Liu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Zhou, emhvdWxpQGNxbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.