- Navy 971 Hospital of PLA, Qingdao, China
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has become a rapidly spreading worldwide pandemic, seriously threatening global public health security. At present, there is still no vaccine or specific drug available for the virus. Therefore, epidemiological prevention and control is crucial to block further spread of the disease. In this present study, based on the public information of COVID-19 in Qingdao, Shandong Province, China, we analyzed the epidemiological characteristics and treatment effects of 60 confirmed cases. It was revealed that the hospital stay of patients were imported from Wuhan or infected by Wuhan patients was obviously shorter than that of those who were imported from other regions or infected by them. In addition, in Hubei-related patients, the earlier transmission generation, which refers to the imported patients (G0) and the first-generation infections (G1), was associated with reduced cure time. Therefore, we speculated that the treatment sensitivity of SARS-CoV-2 decreased within interpersonal transmission in the early stage of this epidemic.
Introduction
As of October 20, 2020, a total of 40652577 COVID-19 cases and 1119664 deaths have been confirmed globally. To date, the outbreak of COVID-19 in China has been effectively controlled [1]. On the contrary, the worldwide pandemic is still spreading rapidly, with massive increases in the number of cases daily. Therefore, it is necessary to analyze the epidemiological characteristics of COVID-19 for further insights into this disease. By stratified analysis of patients in a city, subgroup analyses can clarify relevant factors that affect therapeutic efficiency, thus providing important evidence for the improvement of the treatment and prevention strategy for COVID-19.
In this study, publicly available data were collected from 60 confirmed COVID-19 patients in Qingdao, Shandong Province (information from the official website of Qingdao Municipal Health Commission). The correlation analysis was performed between treatment effect (hospital stay) and related factors. After multigenerational human-to-human transmission, our study indicated reduced treatment sensitivity of SARS-CoV-2 to the current therapeutic strategy, which could be inferred from the fact that the cure time of Wuhan-imported patients and their associated infections is significantly short than that in other patients. Meanwhile, the earlier transmission generation (G0 and G1) of SARS-CoV-2 was correlated with shorter cure time in patients who can be directly traced to Hubei Province.
Methods
From January 21 to February 23, 2020, information of 60 cases of COVID-19 confirmed in Qingdao was collected from the official website of Qingdao Municipal Health Commission. The public information includes patients’ age, gender, infection type (imported or locally infected), the source of imported cases, contact history of infected cases, and the date of onset of symptoms, admission, diagnosis, and discharge. According to the information, diagnostic time, hospital stay, and cure time of patients could be calculated. Cure time was defined as the period from the diagnosis of COVID-19 to the discharge of the patient. We regarded the cure time as an indicator of the sensitivity of treatment. Pearson’s chi-squared test was carried out to evaluate the relationship of potential influence factors with cure time. Subgroup analyses were applied to evaluate the therapeutic efficiency affected by age, gender, infection type, generation, imported region, and diagnostic time. SPSS (version 16.0) and Review Manager (version 5.3) were adopted for statistical analyses. All statistical tests were 2-tailed, and p-value < 0.05 was regarded significant.
Results
Baseline Characteristics
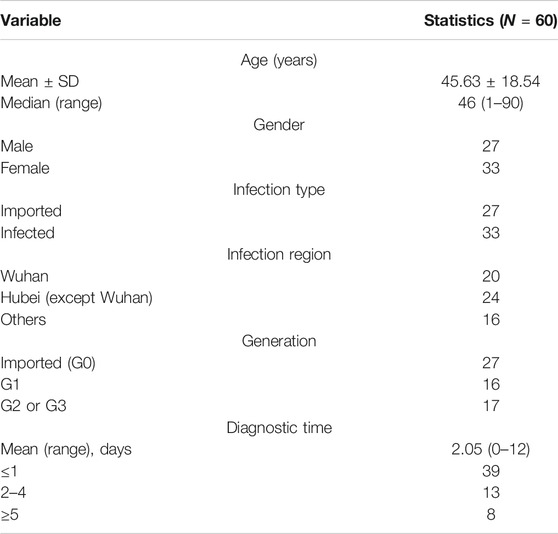
By February 23, 2020, a total of 60 COVID-19 cases were diagnosed in Qingdao with real-time fluorescence polymerase chain reaction detection of SARS-CoV-2 RNA [2] (Table 1). All patients were treated based on Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment (published by the National Health Commission of the People's Republic of China) after the diagnosis. The standard clinical cure was defined as temperature recovery for more than 3 days, with relieved respiratory symptoms and two consecutive negative results for respiratory pathogenic nucleic acid (sampling interval at least 1 day). The patients included 27 males and 33 females. For the 60 patients, the median age was 46 years, ranging from 1 to 90 years. According to the infection type, 27 cases were imported from other regions and 33 cases were locally infected. There were 13 imported patients from Wuhan, 8 from Hubei Province (excluding Wuhan), and 1 from Thailand, thus causing 7, 16, and 2 local infections, respectively. Another 2 cases were imported from Henan Province and 3 cases from Shandong Province, without interpersonal transmission. Another 8 cases were infected by local suspected cases. The average incubation period for the traceable 54 cases was 10.57 days, ranging between 1 and 31 days. Up to March 2nd, 59 cases were cured. The cure rate was 98.33%, and the average hospital stay for the cured cases was 17.69 ± 6.09 days. An 85-year-old female patient died from COVID-19.
Virus Transmission Scenarios
Totally, 27 confirmed imported cases were identified up to March 2. Among them, 10 cases caused local transmission and induced 33 infected patients (Figure 1). Other 22 imported cases displayed no human-to-human transmission. The maximum number of transmissions was 11 from a single imported case. The imported case (Case X2) was identified as a confirmed patient from Tianmen, Hubei Province. There were 16 first-generation infections, 12 second-generation infections, and 5 third-generation infections. Of note, four cases (Cases 50, 52, 56, and 58) were detected as asymptomatic infections, that is, without typical symptoms including fever.
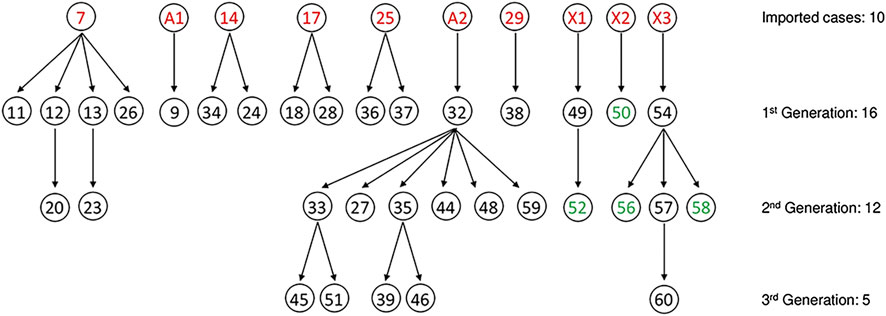
FIGURE 1. SARS-CoV-2 transmission scenarios in Qingdao. Totally, 10 imported COVID cases (red number) cased 33 cases of human-to-human transmission (black or green number), among which 4 cases did not (green number) display typical symptoms of infection, such as fever. A1 was a suspected infected case from Wuhan. A2 was a confirmed infected case from Tianmen, Hubei. X1-3 was a suspected case in Qingdao.
Analysis of Clinical Cure
Up to March 2, a total of 59 patients cured after systematic treatment in Qingdao, with an average treatment time of 16.31 (range 6–43) days. Taking the median treatment time (16 days) as the cutoff point, 59 patients were divided into the shorter cure time (≤16 days) and longer cure time (>16 days) groups. Correlation analysis was conducted for relevant factors and cure time (Table 2). The results illustrated no significant difference of age between patients with shorter cure time and those with longer cure time. Moreover, the infection type (imported or infected by interpersonal transmission of virus) also demonstrated no significant correlation with therapeutic effects. It is worth noting that the imported region of SARS-CoV-2 exhibited significant correlation with therapeutic efficiency (p = 0.002). The patients from Wuhan or infected by Wuhan cases displayed shorter cure time than other patients. Given that COVID-19 first broke out from Wuhan and spread to other regions, the results suggested that SARS-CoV-2 became more difficult to remove after multiple generations of human-to-human transmission. Further analysis of the virus transmission generation also supported significantly prolonged cure time in the second and third generation of infected patients in Hubei-associated transmission chain (p = 0.040). However, in terms of 59 cured patients, there was no significant statistical significance between transmission generation of SARS-CoV-2 and cure time of patients. Furthermore, we analyzed the influence of duration time from symptom onset to diagnosis, and no significant difference was observed (p = 0.779). Interestingly, it was clear that gender has a significant impact on the cure time of patients. Compared with female patients, male patients exhibited a trend of reduced hospital stay (p = 0.046).
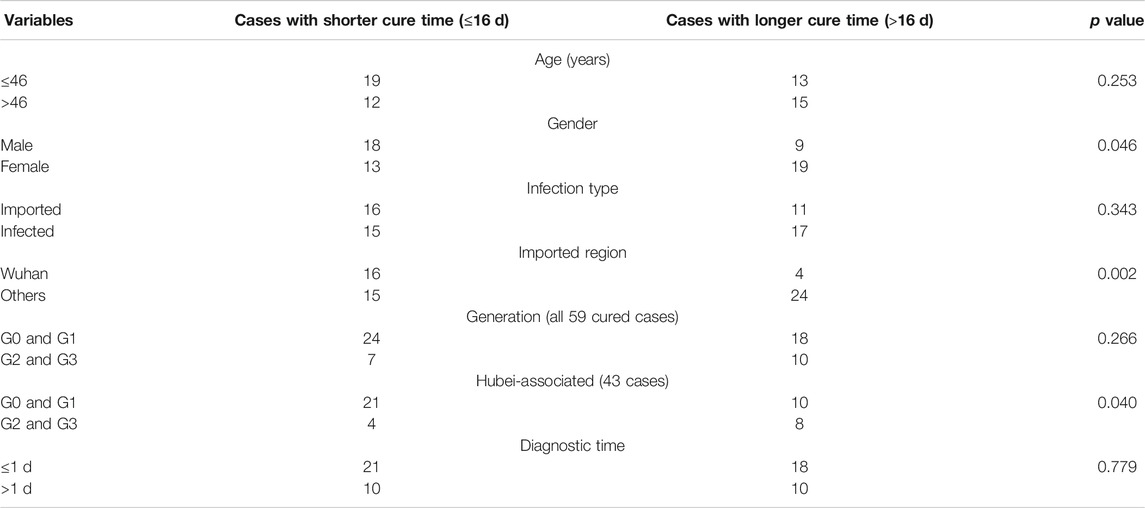
TABLE 2. Correlation analysis of therapeutic efficiency in cured COVID-19 patients in Qingdao (N = 59).
Further pooled analysis (Figure 2) supported that the infection from other regions, rather than Wuhan (HR = 2.08, 95% CI: 1.32–3.27), was a detrimental factor for therapeutic efficiency and was probably related to later generation of interpersonal transmission of SARS-CoV-2. Female gender was also indicated as a promising risk factor for therapeutic efficiency (HR = 1.64, 95% CI: 1.00–2.70). By contrast, increased transmission generation was not identified as a significant risk factor for therapeutic efficiency (HR = 1.39, 95% CI: 0.74–2.59). What is more, no significant favor was observed in age, infection type, or diagnostic time for the cure efficiency.
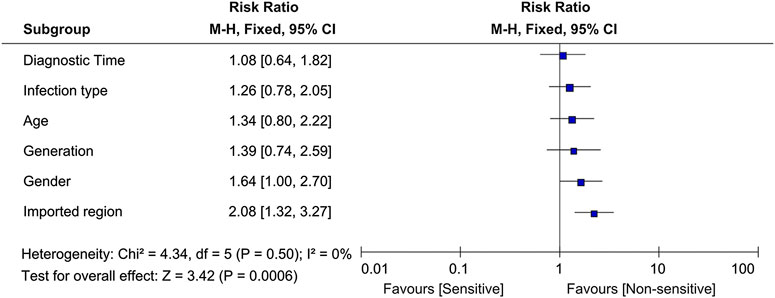
FIGURE 2. Subgroup analyses of therapeutic efficiency through age, gender, infection type, generation, imported region, and diagnostic time in 59 cured COVID-19 patients. Dashed vertical line corresponds to zero heterogeneity of the therapeutic effect. The variables were compared as follows: age, >46 years vs ≤46 years; gender, female vs male; infection type, local transmission vs imported; generation, G2-3 vs G0-1; imported region, other regions vs Wuhan; and diagnosis time, >1 vs. ≤1 day.
Discussion
The limitation of this study was the relatively modest number of identified COVID-19 cases in Qingdao because the results of the regional analysis may be different from those of overall research to some extent. However, because of government’s efforts in epidemic management, up to now, only 65 local cases were confirmed in Qingdao and the last 5 cases confirmed after March 11 were all infected by patients imported from abroad. Considering the possible impact of different sources of virus, these 5 cases were not enrolled in our cohort. With a population of 9.2 million, Qingdao is a large regional city with broad medical and health coverage in the Jiaodong Peninsula. Its detailed and accessible epidemiology information of COVID-19 provided valuable research resources for the treatment and management of this disease. Up to March 2, the mortality rate of COVID-19 in Qingdao was 1.67%, lower than the national level (5.18%, 4,746/91,574, up to October 20, information from the official website of the National Health Commission of the People’s Republic of China). The average time from symptom onset to diagnosis for the infected patients is 2.05 days, which is a reliable guarantee for high cure rate [3].
The systemic treatment of patients was based on Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment that was published by the National Health and Health Commission of China. The adjustment of this guidance may have some impact on the treatment effect because its content was constantly updated, and the treatment strategies were also changed according to clinical treatment effects. However, since all patients in this cohort were admitted to the hospital in a relatively short period (33 days) and the improvement of the clinical guidance was gradual, we believe that the impact of treatment adjustments on the analysis of results is limited and acceptable.
Laboratory diagnosis identified 4 infected patients from close-contact cases (Cases 50, 52, 56, and 58), without typical symptoms including fever [4]. Some infected patients did not display a significant inflammatory response but were positive for the virus detection, which were potential sources for further transmission. Moreover, the cured patients revealed favorable prognosis, and pulmonary fibrosis was rarely observed [5]. In this study, the only died patient was an elderly patient with various underlying diseases, including diabetes, hypertension, coronary heart disease, and heart failure. It was worth noting that the time from symptom onset to the diagnosis of this patient was 12 days. Long diagnosis time may also be a detrimental factor for patients. The correlation of related factors, including old age, underlying disease, and diagnostic time with treatment effect still needs further analysis with larger series of samples [5].
As it infects patients and causes pandemic, SARS-CoV-2 evolves at the same time. In March 2020, Tang et al. [6] proposed that SARS-CoV-2 developed into two subtypes, namely, L type and S type, among which L type was more aggressive and infectious, accounting for about 70% of infections. Forster’s team [7] put forward three major variants in 160 complete SARS-CoV-2 genomes and named them A, B, and C. Types A and C have a high proportion outside East Asia (i.e., among Europeans and Americans). In contrast, type B is the most common type in East Asia. In early March, Korber et al. [8] identified seven D614G mutations on spike protein from 187 viral sequences, and its frequency increased rapidly when this mutant strain entered the population. In many cases, G614 became the main local form within a few weeks. The team obtained no evidence that the virus carrying the mutation caused more severe clinical symptoms. However, the levels of viral RNA in the nose and mouth of patients infected with G614 appeared to be slightly higher than those in patients with D614. Subsequent studies proved that G614 virus may have enhanced ability to enter cells [9, 10]. Moreover, a medical team from Hubei Province, China, compared the clinical characteristics of patients admitted before and after January 23, and they discovered that the initial symptoms of recently infected patients had become more insidious, and even after being cured and discharged from hospital, virus was rediscovered in three patients [11]. The authors speculate that the new coronavirus may gradually evolve into an influenza-like virus and even hide in asymptomatic patients for a long time [11].
As a reasonable inference, we speculate that in the process of long-term coexistence of the host, with improved adaptation to human cells, the virus may become easier to be transmitted or more difficult to be removed by the host. In cases of this cohort, this adaptation may be manifested in the prolongation of the cure time. This prolongation does not contradict with the decline of COVID-19 mortality worldwide. First, due to the increasing attention paid by countries around the world, the enhancement of admission and treatment capacity, and the standardization of diagnosis and treatment methods, the reduction in death rate of COVID-19 were predictable. Moreover, the evolution of SARS-CoV-2 does not necessarily lead to increased virulence. On the contrary, in the process of adapting to humans, certain functions of highly pathogenic CoV in suppressing host immunity may be weakened or lost [12]. And, this may be conducive to the survival of the virus in the host without increasing the severity of the disease. At present, there exist no specific treatment and vaccine available for the disease [13]. However, the application of treatment, even symptomatic or supportive, is beneficial to the cure of patients. In fact, the treatment sensitivity reflects the virus’ ability to survive in the human body and the difficulty of being cleared in the presence of human intervention. To some extent, it is an indicator of the adaptability of the virus to the host.
This study revealed a reduced cure effect in infectious patients from other regions than those from Wuhan, which was correlated with decreased treatment sensitivity with the interpersonal transmission of SARS-CoV-2. Although neutralizing IgG extracted from the serum of cured COVID-19 patients is equally effective in blocking cell entry of both the D614 and 614G variants of SARS-CoV-2 at this stage [14], we cannot guarantee that new mutations that may threaten the development of antivirus drugs or vaccines will not appear. Before the advent of specific treatments for COVID-19, universal epidemiological control is of great significance to combat the pandemic. Population movement between regions is an important factor influencing the spread of epidemics [15], while virus testing along with case isolation and community quarantine has been proved to be able to prevent rapid local outbreak [16]. Physical distancing of 1 m or more and wearing masks are also believed to significantly reduce the risk of virus transmission [17]. In addition, the government’s promotion of positive preventive measures can contribute to the inhibition of the outbreak [18]. All in all, epidemiology is a powerful weapon against COVID-19, and controlling the source of infection and cutting off the route of transmission should not be ignored at any time.
Data Availability Statement
Publicly available datasets were analyzed in this study. These data can be found here: http://wsjsw.qingdao.gov.cn/n28356065/index.html.
Author Contributions
Guarantor of integrity of the entire study: YW; Study concepts and study design: QW and YW; Literature research, data collection and analysis: QW and TY; All the authors revised and approved the paper.
Funding
This research was supported by grants from the National Natural Science Foundation of China (81972793, 81502283), Shandong province Medical Health Science and Technology Project (2018WS447), Qingdao Science and Technology Program for Benefiting People Special Project 2019 (19-6-1-25-nsh, 2019-WJZD170), and Qingdao Outstanding Health Professional Development Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Burki T. China’s successful control of COVID-19. Lancet Infect Dis (2020) 48(2):151–3. doi:10.1007/s15010-020-01409-4
2. Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill (2020) 25:45. doi:10.2807/1560-7917.es.2020.25.3.2000045
3. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (2020) 395:497–506. doi:10.1016/s0140-6736(20)30183-5
4. Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet (2020) 395:514–23. doi:10.1016/s0140-6736(20)30154-9
5. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (2020) 395:507–13. doi:10.1016/s0140-6736(20)30211-7
6. Tang X, Wu C, Li X, Song Y, Yao X, Wu X, et al. On the origin and continuing evolution of SARS-CoV-2. Nat Sci Rev (2020) 7:1012–23. doi:10.1093/nsr/nwaa036
7. Forster P, Forster L, Renfrew C, Forster M. Phylogenetic network analysis of SARS-CoV-2 genomes. Proc Natl Acad Sci USA (2020) 117:9241–3. doi:10.1073/pnas.2007433117
8. Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. Spike mutation pipeline reveals the emergence of a more transmissible form of SARS-CoV-2. Nat Sci Rev (2020) 12:122–8. doi:10.1101/2020.04.29.069054
9. Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell (2020) 182:812–27. doi:10.1101/2020.04.29.069054
10. Plante JA, Liu Y, Liu J, Xia H, Johnson BA, Lokugamage KG, et al. Spike mutation D614G alters SARS-CoV-2 fitness and neutralization susceptibility. Preprint repository name [Preprint] (2020). Available from: https://www.biorxiv.org/content/10.1101/2020.09.01.278689v1.
11. Chen Z, Jijia h., Zhang Z, Jiang S, Wang T, Shi Z, et al. Caution: clinical characteristics of COVID-19 patients are changing at admission. SSRN Electron J (2020) 4:32–9. doi:10.1101/2020.03.03.20030833
12. Fung SY, Yuen KS, Ye ZW, Chan CP, Jin DY. A tug-of-war between severe acute respiratory syndrome coronavirus 2 and host antiviral defence: lessons from other pathogenic viruses. Emerg Microb Infect (2020) 9:558–70. doi:10.1080/22221751.2020.1736644
13. Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. J Am Med Assoc (2020) 323:1824–36. doi:10.1001/jama.2020.6019
14. Tan Y, Liu F, Xu X, Ling Y, Huang W, Zhu Z, et al. Durability of neutralizing antibodies and T-cell response post SARS-CoV-2 infection. Front Med (2020) 12:23–7. doi:10.1007/s11684-020-0822-5
15. Yin Q, Wang Z, Xia C, Dehmer M, Emmert-Streib F, Jin Z. A novel epidemic model considering demographics and intercity commuting on complex dynamical networks. Appl Math Comput (2020) 386:125517. doi:10.1016/j.amc.2020.125517
16. Lavezzo E, Franchin E, Ciavarella C, Cuomo-Dannenburg G, Barzon L, Del Vecchio C, et al. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature (2020) 584:425–9. doi:10.1038/s41586-020-2488-1
17. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schunemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet (2020) 395:1973–87. doi:10.1016/j.jvs.2020.07.040
Keywords: COVID-19, human-to-human transmission, treatment sensitivity, generation, region
Citation: Wang Q, Yang T and Wang Y (2020) Reduced Treatment Sensitivity of SARS-CoV-2 After Multigenerational Human-to-Human Transmission. Front. Phys. 8:578024. doi: 10.3389/fphy.2020.578024
Received: 30 June 2020; Accepted: 02 November 2020;
Published: 04 December 2020.
Edited by:
Chengyi Xia, Tianjin University of Technology, ChinaReviewed by:
Xiao Han, University of California, Davis, United StatesZhishuang Wang, Tianjin University of Technology, China
Copyright © 2020 Wang, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Wang, d3k5NzFAeWFuZGV4LmNvbQ==
†These authors have contributed equally to this work
 Qiang Wang
Qiang Wang Tong Yang
Tong Yang Yang Wang
Yang Wang