
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol., 28 March 2025
Sec. Ethnopharmacology
Volume 16 - 2025 | https://doi.org/10.3389/fphar.2025.1511486
This article is part of the Research TopicEfficacy and Mechanism of Herbal Medicines and Their Functional Compounds in Preventing and Treating Cardiovascular Diseases and Cardiovascular Disease Risk Factors - Volume IIView all 12 articles
Background: Traditional Chinese medicine injections for Tonifying Qi (TCMi-TQs), which exhibits comparable effect of regulating energy metabolism, is commonly used as an adjuvant treatment for acute myocardial infarction (AMI) in China.
Objective: A systematic review and meta-analysis was conducted to contrast the effectiveness and safety of four TCMi-TQs in AMI.
Methods: Eight Databases were thoroughly searched before 31 July 2024, for randomized controlled trials (RCTs) focusing on the application of TCMi-TQs combined with conventional treatments (CT) to treat AMI. The primary outcomes were in-hospital mortality and long-term mortality. Secondary outcomes included malignant arrhythmia, left ventricular ejection fraction (LVEF), and adverse events. Stata17.0 and RevMan 5.4.1 software were employed for meta-analysis. The quality of evidence was evaluated using the GRADE approach.
Results: A total of 113 RCTs involving 10,779 patients were included in the analysis, none of which described in-dependent testing of the purity or potency of the TCMi-TQ product used. 51/113 reported random sequence generation. All RCTs lack adequate description of allocation concealment. 112/113 failed to assess blinding. The meta-analysis results demonstrated that the combined application of TCMi-TQ + CT, compared with CT, significantly reduced in-hospital mortality in AMI patients [RR = 0.58, 95% CI (0.51, 0.67), P < 0.05], decreased the incidence of malignant arrhythmia [RR = 0.51, 95%CI(0.42, 0.63), P < 0.05], increased LVEF [MD = 6.52, 95%CI(5.54, 7.50), P < 0.05], and decreased the incidence of adverse events [RR = 0.70, 95%CI(0.60, 0.81), P < 0.05]. The GRADE evidence quality classification indicated that the evidence for in-hospital mortality, malignant arrhythmia, and adverse events was of moderate quality, while the evidence for LVEF was of low quality.
Conclusion: TCMi-TQ demonstrates additional clinical value in reducing mortality, the risk of malignant arrhythmia, and adverse events in patients with AMI. However, further validation of these findings is warranted through high-quality clinical trials due to methodological weaknesses in randomization, blinding, allocation concealment, and insufficient assessment of the purity/potency of botanical drugs and the quantity of active metabolites.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024573818, identifier PROSPERO (CRD42024573818).
Acute myocardial infarction (AMI) is a significant global health issue characterized by high morbidity and mortality rates, imposing substantial economic and medical burdens (Mensah et al., 2023). AMI is usually caused by coronary artery disease, and research has found that AMI can be associated with cerebrovascular diseases, making clinical diagnosis and treatment more difficult due to comorbidities of the heart and brain (Suzuki et al., 2023). Over the past decade, the management of AMI in China has made some progress. However, the China Cardiovascular Health and Disease Report 2023 Summary revealed an increase in AMI mortality in China from 2002 to 2021 (National Center Cardiovascular Diseases, 2024). With the active promotion of secondary prevention measures for coronary heart disease and early reperfusion therapy for AMI, the mortality rate of AMI patients has decreased (Roger et al., 2010). There are still several unresolved issues after reperfusion, including decreased myocardial contractility, ventricular arrhythmia, and no-reflow phenomenon (Thiele et al., 2017). These complications have a significant impact on the prognosis of patients (Heusch and Gersh, 2017). Therefore, exploring additional effective treatment methods remains essential.
Traditional Chinese medicine (TCM) can play a unique role in improving the clinical prognosis of AMI. Research has found that for STEMI patients, on the basis of standardized biomedicine treatment (including reperfusion therapy and optimal drug therapy), Tongxinluo can significantly improve clinical prognosis, and reduce the risk of major adverse cardiovascular and cerebrovascular events at 30°days and 1°year (Yang et al., 2023). Consequently, there is a growing interest among Chinese medical professionals in exploring therapeutic approaches from TCM to help reduce AMI mortality. This research direction aligns with the principles exemplified by Professor Tu Youyou, the Nobel Prize laureate who successfully extracted artemisinin from Artemisia annua, thereby revolutionizing malaria treatment.
One such intervention gaining attention is the use of traditional Chinese medicine injections for tonifying qi (TCMi-TQs), which possess comparable effects of regulating energy metabolism (Li et al., 2023; Wang et al., 2022; Wang A. et al., 2024; Yang et al., 2022). TCMi-TQs have shown promise in reducing mortality and the incidence of re-infarction among AMI patients (Jia et al., 2023; Lu et al., 2018). To obtain high-quality evidence regarding the safety and efficacy of TCMi-TQs in AMI, this study initiated a search for TCMi-TQs used in the treatment of AMI. The search yielded four TCMi-TQs: Shengmai injection (SGMI), Shenmai injection (SMI), Shenfu injection (SFI), and Astragalus injection (AI). Research has demonstrated that these four TCMi-TQs and their main active metabolites play a significant role in modulating myocardial energy metabolism in patients with myocardial ischemia. SGMI increases the number of myocardial cell mitochondria and scavenges oxygen-free radicals (Lu et al., 2005). SMI enhances myocardial microcirculation parameters (Yang and Wang, 2021), while SFI mitigates mitochondrial oxidative stress (Lu and Xiang, 2023). The primary active compound of AI, astragaloside IV, regulates myocardial cell oxidative stress and enhances mitochondrial function (Guan et al., 2023). Detailed information on these four TCMi-TQs is provided in Supplementary Tables S1–S4. The objective of this study is to systematically collect and analyze the data from these four randomized controlled trials (RCTs) investigating TCMi-TQs in the treatment of AMI, with the aim of evaluating its efficacy and safety for AMI patients presenting with relevant indications based on the current evidence. This study has the potential to bridge the gap between TCMi-TQs and modern medicine for AMI treatment and open up avenues for integrative care models for AMI patients.
The systematic review has been registered in the PROSPERO platform for prospective registration with the registration number CRD42024573818. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (Moher et al., 2015; Page et al., 2021) were employed to conduct our network meta-analysis, as seen in Supplementary Material. To ensure accurate reporting of four TCMIs in this analysis, we adhered to the guidelines established in the consensus statement on the Phytochemical Characterization of Medicinal Plant extract (ConPhyMP) (Supplementary Tables S1–S4) (Heinrich et al., 2022).
The inclusion criteria for this review are as follows:
(1) Study Type: RCTs.
(2) Study Subjects: Patients who meet the diagnostic criteria for AMI.
(3) Type of Intervention: The observation group received any one of the traditional Chinese medicine injections with TCMi-TQ interventions, including SGMI, SMI, SFI, or AI, in addition to conventional treatment. The control group received conventional treatment (CT), which included general treatment (monitoring vital signs, symptom relief, etc.), reperfusion therapy (Percutaneous Coronary Intervention (PCI), thrombolysis, and coronary artery bypass surgery), and pharmacotherapy (antiplatelet agents, anticoagulants, lipid-lowering drugs, etc.), while excluding commercial Chinese polyherbal preparation (CCPP), acupuncture, and other traditional medical treatments. The sole difference between the two groups was the administration of TCMi-TQ.
(4) Outcome Measures: The primary outcome measures were in-hospital mortality and long-term mortality. Long-term mortality was defined as mortality occurring at least 1 year after the onset of AMI. Secondary outcomes included the incidence of malignant arrhythmias affecting hemodynamics (such as ventricular fibrillation, polymorphic ventricular tachycardia, and second or third-degree atrioventricular block with hemodynamic disturbance), changes in left ventricular ejection fraction (LVEF) before and after treatment, and adverse safety events (such as dizziness, nausea, and allergic reactions).
The exclusion criteria for this review are as follows:
(1) No mention of diagnostic criteria in the literature or unclear diagnostic criteria.
(2) Control settings of clinical trials that were unreasonable or did not meet the inclusion criteria for this study, such as the inclusion of other CCPP in the experimental group, were excluded.
(3) Duplicate published literature.
(4) Studies that did not include the required effect measures.
We conducted a comprehensive literature search using multiple databases, including PubMed, EMBASE, Scopus, Cochrane Central Register of Controlled Trials, and Web of Science. Additionally, we searched the China Biological Literature Database, China National Knowledge Infrastructure, VIP database, and Wanfang Data Knowledge Service Platform. The search covered the period from the establishment of each database until July 2024. The search strategy is provided in Supplementary Table S5. In addition to electronic database searches, we also examined the reference lists of relevant articles and manually searched printed books and magazines in the field to ensure a comprehensive literature review. To identify relevant clinical trials, we also searched for registered trials on ClinicalTrials.gov to identify any unpublished articles that met our inclusion criteria.
Two reviewers (YX Shi and YZ Li) independently performed each step according to established search rules. The screening process involved reviewing the title and abstract of each retrieved article and applying predefined inclusion and exclusion criteria. Irrelevant articles were excluded, and no discussion took place until the final results were summarized.
After retrieving the articles, the two reviewers (YX Shi and YZ Li) independently processed the data, identified and removed duplicate articles, retained the most recent publications with the most complete data, excluded articles that did not meet the inclusion or exclusion criteria, and documented the reasons for exclusion. The extracted data included the article title, all authors, year of publication, journal, sample size, participant characteristics, treatment interventions, blinding methods, randomization procedures, outcome measures, adverse events, and other relevant information, which were summarized in a table. In case of any disagreements, a third reviewer (HQ Zong) made the final judgment and resolved the discrepancies.
Risk of bias was assessed by two reviewers (YX Shi and YZ Li) independently, using the Cochrane risk of bias tool (RoB 2.0 Tool) (Sterne et al., 2019). Overall quality of evidence was rated using the Grades of Rec ommendations, Assessment, Development and Evaluation (GRADE) approach (Chen et al., 2018).
Any disagreement between the 2 reviewers (YX Shi and YZ Li) will be resolved by a discussion. Further disagreements will be arbitrated by the third author (HQ Zong).
RevMan 5.4.1 software was utilized to analyze the extracted clinical research data. Relative risk (RR) analysis was employed for count data, while mean difference (MD) was used for measurement data when the unit of measurement was the same. Standardized mean difference (SMD) was used for measurement data when the unit of measurement differed. All effect sizes were reported with a 95% confidence interval (CI). For continuous outcomes, the change difference was employed for meta-analysis. The mean and standard deviation of the change difference before and after the intervention were calculated using the formula provided in the Cochrane handbook (Higgins et al., 2023).
In this study, the mortality rate, incidence of malignant arrhythmia, and incidence of adverse events were presented using RR. LVEF was presented using the mean and standard deviation of the difference before and after treatment. Heterogeneity among the included studies was assessed using the Q test. A significance level of P ≤ 0.10 and an I2 value ≥50% were used as criteria for significant heterogeneity. If the P value was greater than 0.1 and the I2 value was less than 50%, a fixed-effect model was used for statistical analysis. If the P value was less than or equal to 0.1 and the I2 value was greater than or equal to 50%, a random-effects model was applied based on sensitivity analysis (Deeks et al., 2023). Statistical significance was defined as P < 0.05.
In cases where heterogeneity (I2 > 50%) was observed among the studies, subgroup analysis and sensitivity analysis were conducted to explore the sources of heterogeneity and verify the stability of the meta-analysis results. Funnel plots were generated using RevMan 5.4.1 software, and Egger’s test was performed using Stata 17.0 software for studies with 10 or more articles to assess potential publication bias. If the P value of Egger’s test was less than 0.05, it indicated the presence of publication bias among the studies (Egger et al., 1997). For studies exhibiting publication bias, the trim-and-fill method was employed to adjust the results, assuming that missing studies likely occupied symmetrical positions relative to the existing ones—these being studies potentially withheld due to publication bias, such as those reporting negative results (Shi and Lin, 2019).
The evidence quality of outcome indicators was evaluated using the GRADEpro GDT online tool. The default assumption was that the evidence quality of RCTs was high (Guyatt et al., 2008). The evidence quality of outcome indicators was assessed based on five downgrade factors: risk of bias, inconsistency, indirectness, imprecision, and publication bias (Chen et al., 2018).
The process of study selection and identification is depicted in Figure 1. Initially, a total of 1709 potentially relevant articles were retrieved from electronic databases. After removing 937 duplicates, 772 articles remained for further screening. Following title and abstract screening, 323 records were excluded, leaving 449 records. Subsequently, 336 articles were excluded for the following reasons: irrelevant study (n = 3), unreasonable experimental and control settings (n = 17), Nonrandomized (n = 14), Non-AMI (n = 19), review (n = 1), full-text unavailable (n = 10), lack of diagnosis criteria (n = 155), and lack of outcome measures (n = 117). Finally, 113 full-text articles were included.
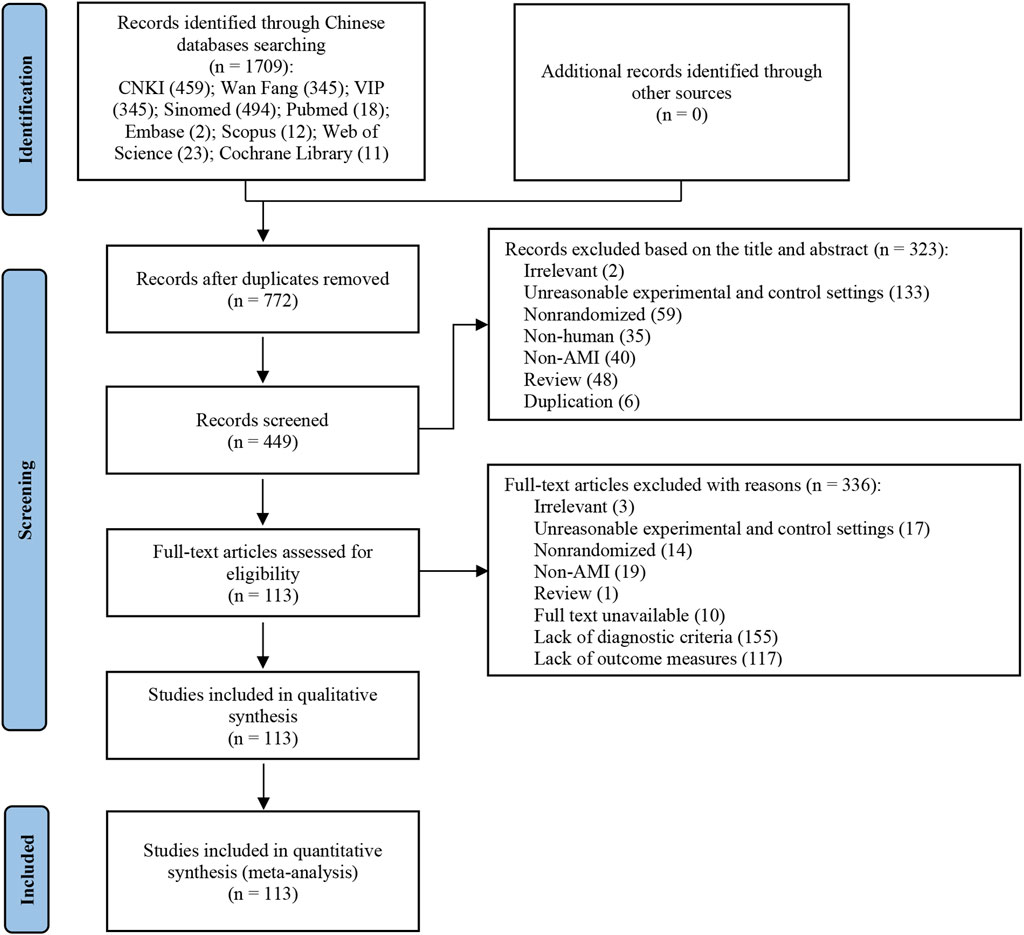
Figure 1. Flow chart of the study selection. The initial review yielded 1709 articles, leaving 772 articles after removing duplicates. After selection based on title or abstract, 449 articles were screened for full text review. Of these, 3 articles were irrelevant, 17 articles had unreasonable experimental and control settings, 14 articles were nonrandomized, 19 articles were non-AMI, an article was review, 10 articles’ full text were unavailable, 155 articles were lack of diagnostic criteria, 117 articles were lack of outcome measures. Finally, 113 full-text articles were included.
A total of 113 studies (28–140) met the final eligibility criteria and were included in the meta-analysis (Table 1). All studies were single-center trials conducted in China. Two trial was a three-arm study (Wang, 2016; Li, 2006), while the remaining trials were two-arm studies. The sample sizes ranged from 30 (125) to 502 (139), with the mean age ranging from 35 to 75 years. The duration of treatment varied from once (Wang, 2018; Zhang D. L. et al., 2018; Zhang, 2017) to 30 days (Wang, 2016). We identified two ongoing trials that may be relevant to this review. Supplementary Table S6 provides details of the CCPP included in the study.
All studies (n = 113) were considered to be at high risk of bias. The results are presented in Figure 2 and Supplementary Figure S1. Regarding randomization process, 51 studies described specific randomization methods: 45 studies used the random number table method, one used the simple randomization method, one used the dice throwing method, one used the lottery method, one used the stratified randomization principle, one used the parity randomization method, and one used the randomized parallel grouping method. All included studies were deemed to some concerns risk due to inadequate description of allocation sequence concealment. Regarding deviations from the established intervention, one study specifically described the double-blind method and was rated as having a low risk of bias, and the rest of the studies did not describe the specific randomization or blinding methods and were rated as having a high risk of bias. All included studies were deemed to have a low risk of bias due to missing outcome data. 38 studies assessed no effect on outcome measures and were judged to be at low risk of bias. One study was registered on clinicaltrials.gov and presented all results, so it was judged to be at low risk of bias, while the rest of the studies did not mention registration and were assessed as being at some concerns risk.
49 studies (Hao et al., 2021; Zhu et al., 2020; Feng et al., 2019; Zhu et al., 2019; Wang HY. et al., 2018; Zhang DL. et al., 2018; Zhang DM. et al., 2018; Li and Hou, 2017; Wang and Qing, 2017; Chen, 2017; He et al., 2016; Li, 2016; Liu, 2016; Wu et al., 2016; Qi et al., 2015a; Xuan et al., 2015; Li and Cheng, 2014; Zong et al., 2014; Zou, 2014; Liu, 2012; Zhang, 2011; Zhang et al., 2011; Ye, 2010; Mi et al., 2009; Yuan, 2009; Qu, 2007; Cui and Li, 2006; Ding and Xu, 2006; Li, 2006; Liang, 2006; Shen et al., 2006; Zeng, 2005; Zhao et al., 2005; Liu et al., 2004; Han et al., 2003; Bai et al., 2002; Mo and Zhao, 2002; Wei and Liu, 2001; Han et al., 2000; Guo and Zhang, 1999) reported the case fatality rate involving 4,939 patients (Figure 3). The analysis showed no significant heterogeneity (I2 = 0%), and a fixed-effects model was used for statistical analysis. The meta-analysis results demonstrated that the combined application of TCMi-TQ significantly reduced the mortality of AMI patients compared to CT alone [RR = 0.58, 95%CI (0.51, 0.67), P < 0.05]. This effect was observed in both the STEMI subgroup [RR = 0.53, 95%CI (0.50, 0.78), P < 0.05] and the subgroup with ALL AMI cases [RR = 0.56, 95%CI (0.46, 0.67), P < 0.05]. However, in the long-term mortality subgroup (follow-up time >12 months), the combined application of TCMi-TQ did not significantly reduce the mortality of AMI patients compared to CT alone [RR = 0.22, 95%CI (0.01, 4.29), P = 0.32] (Figure 4).
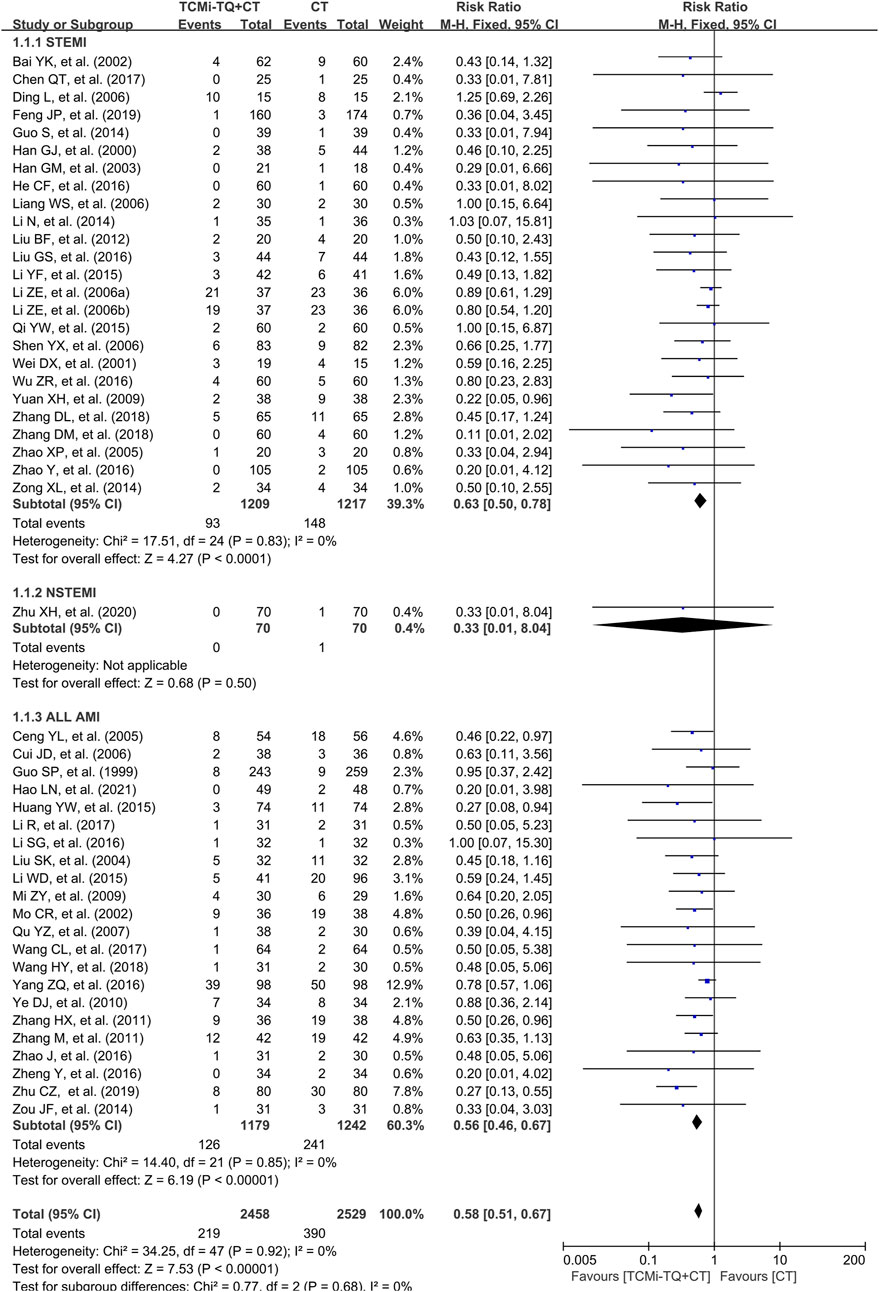
Figure 3. Forest plot of the effect of TCMi-TQ combined with conventional biomedicine treatment on in-hospital mortality in patients with AMI Notes: CI, confidence interval; TCMi-TQ, Traditional Chinese medicine injections for Tonifying Qi; CT, conventional treatment; AMI, acute myocardial infarction; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction.
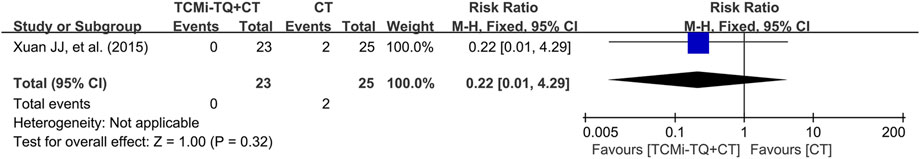
Figure 4. Forest plot of the effect of TCMi-TQ combined with conventional biomedicine treatment on long-term mortality in patients with AMI Notes: CI, confidence interval; TCMi-TQ, Traditional Chinese medicine injections for Tonifying Qi; CT, conventional treatment.
Malignant arrhythmia was reported in 18 studies (1957 patients) (Chen, 2021; Du, 2017; Wang et al., 2017; Zhou, 2017; Li et al., 2016; Liu, 2016; Liu and Tu, 2016; Wu et al., 2016; Zhang et al., 2011; Wang et al., 2010; Ye, 2010; Yuan, 2009; Wang, 2008; Qu, 2007; Liu et al., 2004; Wei and Liu, 2001; Guo and Zhang, 1999; Wang X. et al., 2021). These studies recorded ventricular fibrillation, polymorphic ventricular tachycardia, and second- or third-degree atrioventricular block with hemodynamic disturbances. The meta-analysis, with low heterogeneity between studies (I2 = 36%), indicated that the combination of TCMi-TQ and CT further reduced the incidence of malignant arrhythmia in AMI patients [RR = 0.51.95%CI (0.42, 0.63), P < 0.05]. This effect was observed in both the STEMI subgroup [RR = 0.49.95%CI (0.37, 0.64), P < 0.05] and the subgroup with ALL AMI cases [RR = 0.55.95%CI (0.41, 0.73), P < 0.05]. (Figure 5).
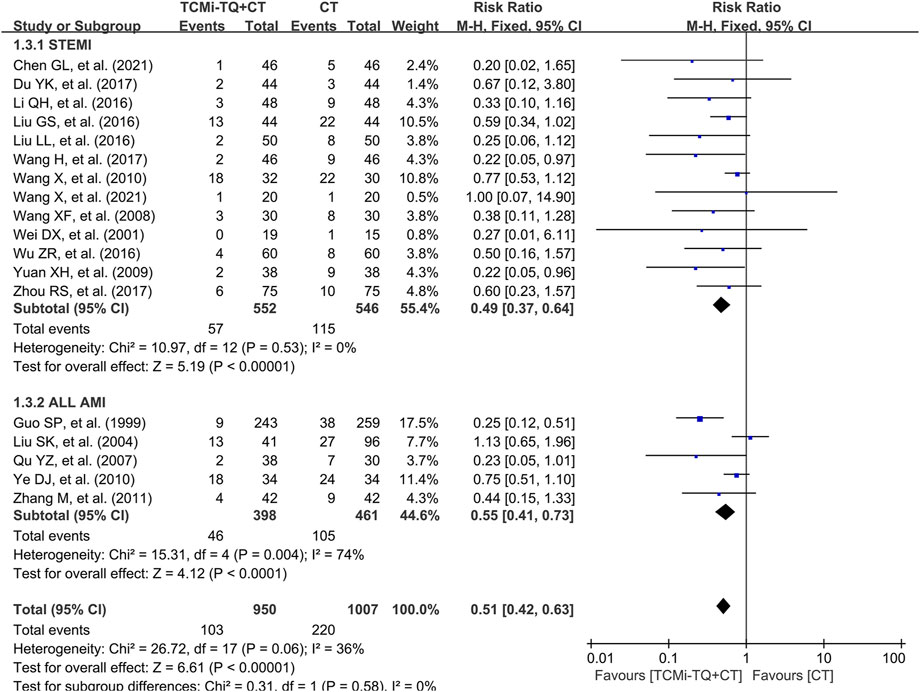
Figure 5. Forest plot of the effect of TCMi-TQ combined with conventional biomedicine treatment on the incidence of malignant arrhythmia in patients with AMI. Notes: CI, confidence interval; TCMi-TQ, Traditional Chinese medicine injections for Tonifying Qi; CT, conventional treatment; AMI, acute myocardial infarction; STEMI, ST-segment elevation myocardial infarction.
LVEF data were reported in 71 studies (Zhou, 2024; Zhan and Cui, 2023; Zhang et al., 2023; Lu and Yao, 2022; Ma et al., 2022; Wu et al., 2022; Xu, 2022; Ji et al., 2021; Wang AJ. et al., 2021; Lan et al., 2021; Zhao and Sun, 2021; Zhao, 2020; Feng et al., 2019; Sun, 2019; Wang, 2019; Wang LM. et al., 2019; Wang XY. et al., 2019; Xian, 2019; Zhang et al., 2019; Chen and Qiao, 2018; Liu, 2018; Shi et al., 2018; Song, 2018; Wang HY. et al., 2018; Wang, 2018; Xie, 2018; Xu, 2018; Yan, 2018; Yan et al., 2018; Zhang DL. et al., 2018; Wang and Huang, 2017; Du, 2017; Kang, 2017; Li et al., 2017; Li and Hou, 2017; Wang et al., 2017; Yan et al., 2017; Yang JW. et al., 2017; Zhang, 2017; Zhou, 2017; Chen, 2017; He et al., 2016; Li et al., 2016; Liu, 2016; Liu and Tu, 2016; Luo, 2016; Wang, 2016; Yang and Cai, 2016; Zhao J. et al., 2016; Zhao Y. et al., 2016; Li WD., 2015; Li YF., 2015; Qi et al., 2015b; Qi et al., 2015c; Xuan et al., 2015; Guo, 2014; Meng, 2014; Wen, 2014; Yang, 2014; Li, 2013; Feng et al., 2011; Shi and Li, 2016; Li et al., 2010; Wang et al., 2010; Mi et al., 2009; Long, 2007; Li, 2006; Shen et al., 2006; Zhu, 2006; Chen et al., 2003). High heterogeneity was observed between these studies (I2 = 98%), and no clear sources of heterogeneity were identified through subgroup analysis (mean age, type of CCPP, treatment duration, sample size) (see Supplementary Figures S2–S5; Table 2 for details). Despite the heterogeneity, which was deemed acceptable in the overall population analysis, a random-effects model was employed. The meta-analysis results revealed that TCMi-TQ combined with CT significantly improved LVEF in both STEMI and NSTEMI patients compared to treatment with biomedicine alone [MD = 6.52, 95%CI (5.54, 7.50), P < 0.05] (Figure 6).
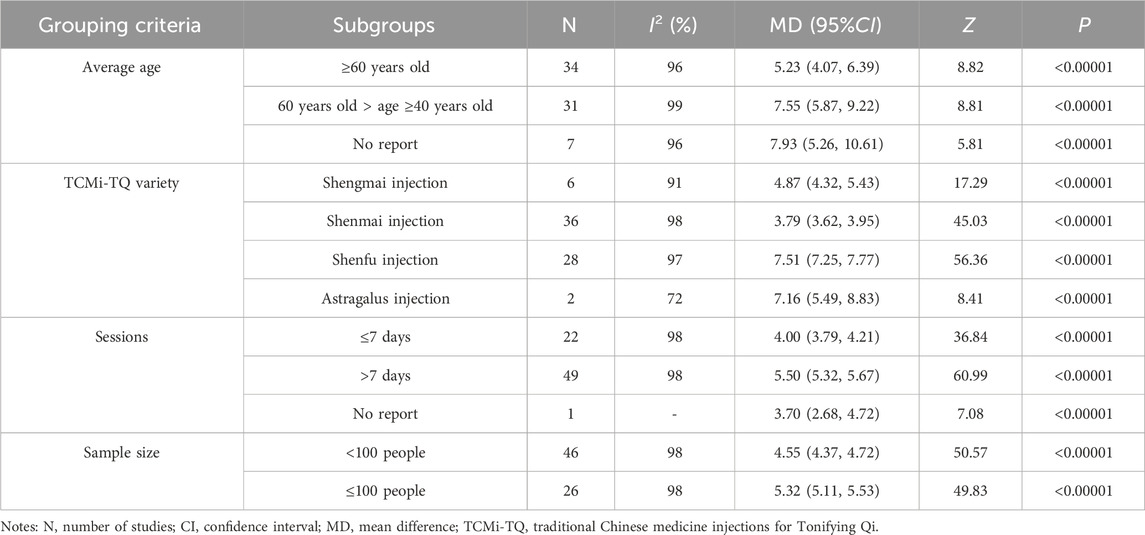
Table 2. Subgroup analysis of LVEF based on mean age, TCMi-TQ category, duration of treatment, and sample size.
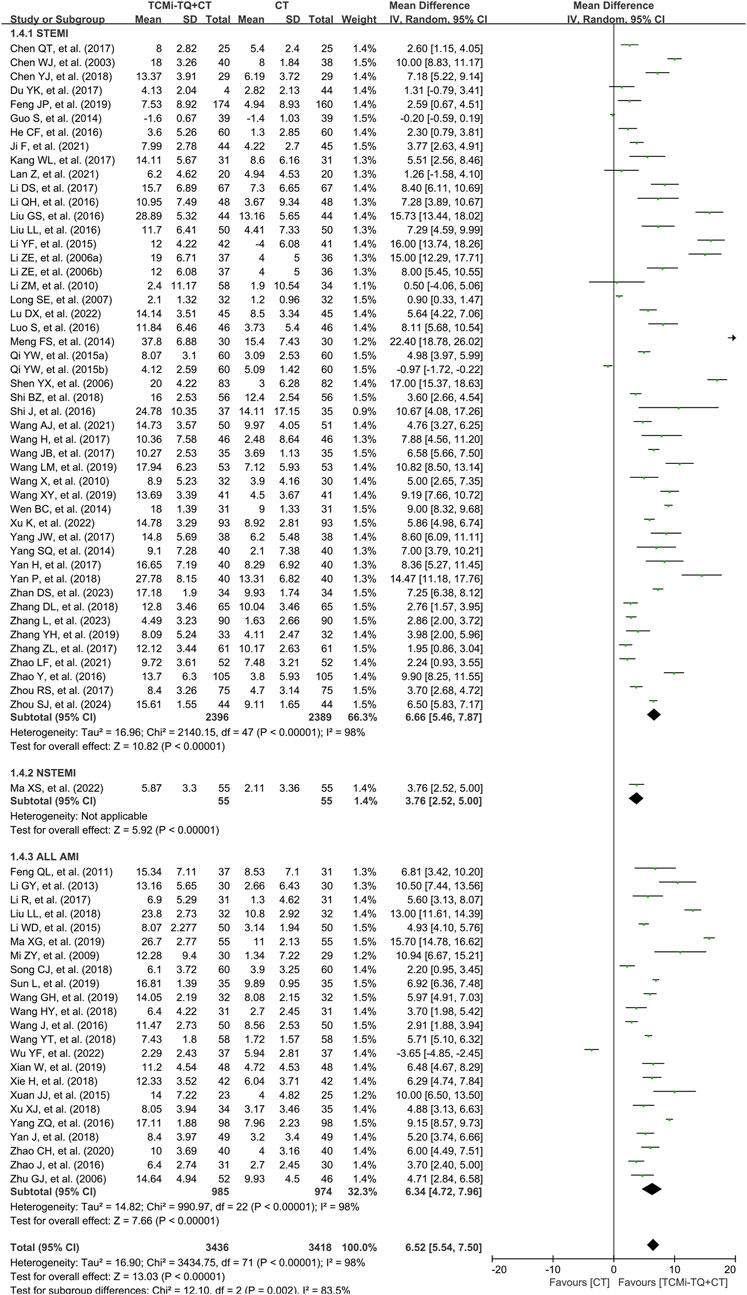
Figure 6. Forest plot of the effect of TCMi-TQ combined with conventional biomedicine treatment on LVEF in patients with AMI Notes: CI, confidence interval; MD, mean difference; TCMi-TQ, Traditional Chinese medicine injections for Tonifying Qi; CT, conventional treatment; AMI, acute myocardial infarction; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; LVEF, left ventricular ejection fraction.
Adverse events were reported in 32 studies (4,896 patients) (Zhan and Cui, 2023; Lu and Yao, 2022; Xu, 2022; Wang AJ. et al., 2021; Yu et al., 2021; Zhu et al., 2020; Pei et al., 2019; Sun, 2019; Tang, 2019; Xian, 2019; Zhang and Jia, 2019; Liu, 2018; Shi et al., 2018; Xie, 2018; Zhang DL. et al., 2018; Zhang DM. et al., 2018; Li et al., 2017; Li and Hou, 2017; Zhou, 2017; Yang and Cai, 2016; Yang et al., 2014; Lu, 2011; Shi and Li, 2016; Yu et al., 2010; Lu, 2009; Long, 2007; Liang, 2006; Han et al., 2003; Wei and Liu, 2001; Han et al., 2000; Guo and Zhang, 1999; Wang X. et al., 2021). These studies recorded bleeding events, abnormal renal function, allergies, headaches, dizziness, abnormal digestive system, respiratory system dysfunction, ecchymosis, and rash. The meta-analysis, with low heterogeneity between studies (I2 = 18%), indicated that the combination of TCMi-TQ and CT further reduced the incidence of adverse events in AMI patients [RR = 0.70.95%CI (0.60, 0.81), P < 0.05] (Figure 7). Specifically, the combination of TCMi-TQ and conventional treatment (CT) reduced the incidence of abnormal digestive system events in AMI patients [RR = 0.31, 95% CI (0.20, 0.47), P < 0.05], with heterogeneity I2 = 33%. Additionally, the combined use of TCMi-TQ and CT did not increase the risk of adverse events such as bleeding events, abnormal renal function, allergies, headaches, dizziness, respiratory system disfunction, ecchymosis, and rash (P > 0.05). These findings suggest that the combined use of TCMi-TQ and CT does not increase the incidence of adverse events (Table 3).
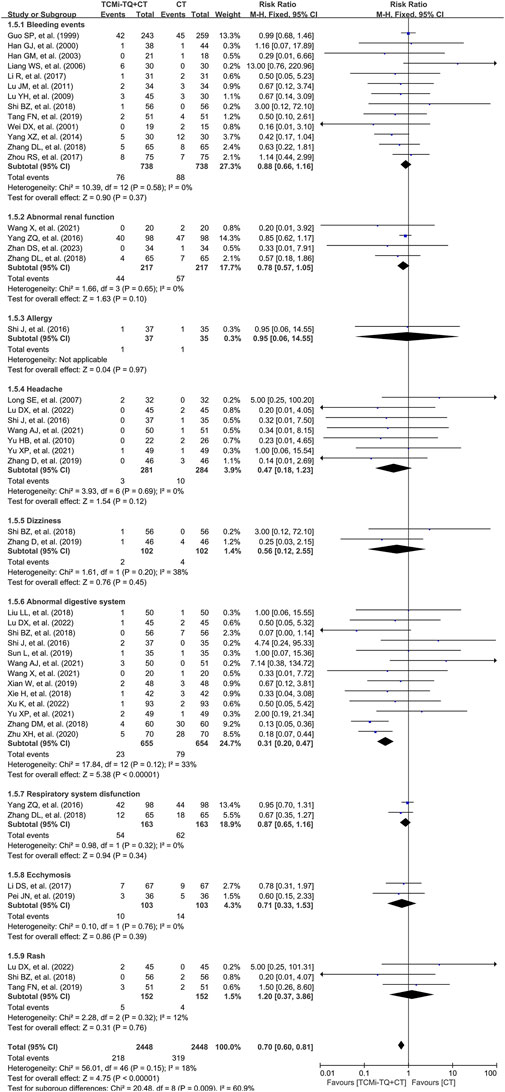
Figure 7. Forest plot of the occurrence of adverse events in patients with AMI treated with TCMi-TQ combined with conventional biomedicine. Notes: CI, confidence interval; RR, risk ratio; TCMi-TQ, Traditional Chinese medicine injections for Tonifying Qi; CT, conventional treatment.
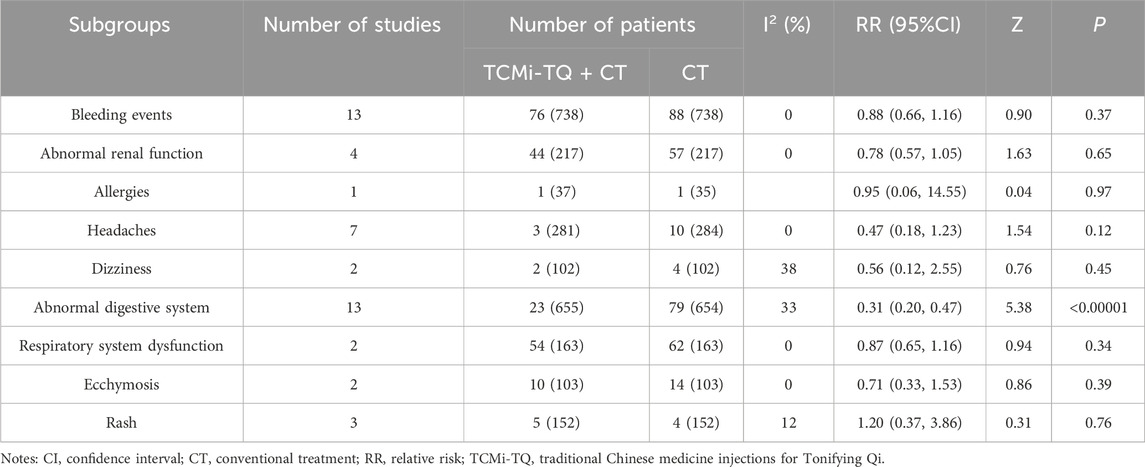
Table 3. Subgroup analysis of adverse events based on bleeding events, abnormal renal function, allergies, headaches, dizziness, abnormal digestive system, respiratory system dysfunction, ecchymosis, and rash.
Funnel plots of mortality, malignant arrhythmia, LVEF, and adverse events are presented in Figures 8–11. The Egger test for two outcome indicators indicated no significant publication bias in LVEF (P = 0.199) and adverse events (P = 0.158). Mortality (P = 0.000) and malignant arrhythmia (P = 0.005) had significant publication bias. The results were corrected using the trim-and-fill method. No additional studies were included after two iterations using the Linear method. The fixed model results showed no change before and after the iterations, indicating that the meta-analysis results were stable.
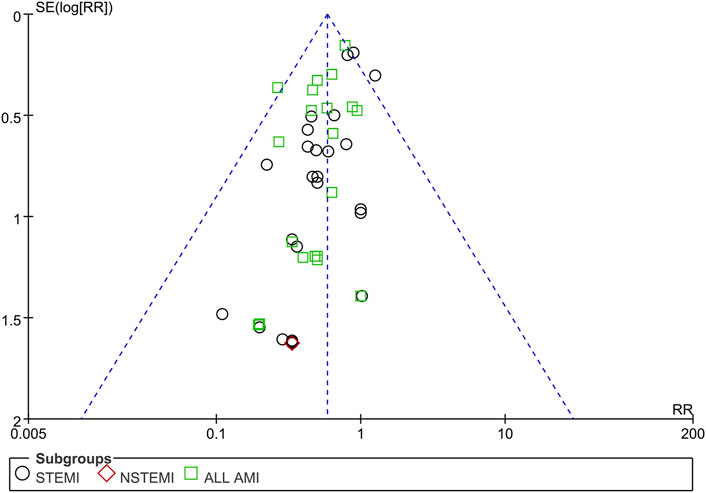
Figure 8. Funnel plot of case fatality rate. Notes: STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; AMI, acute myocardial infarction; RR, risk ratio.
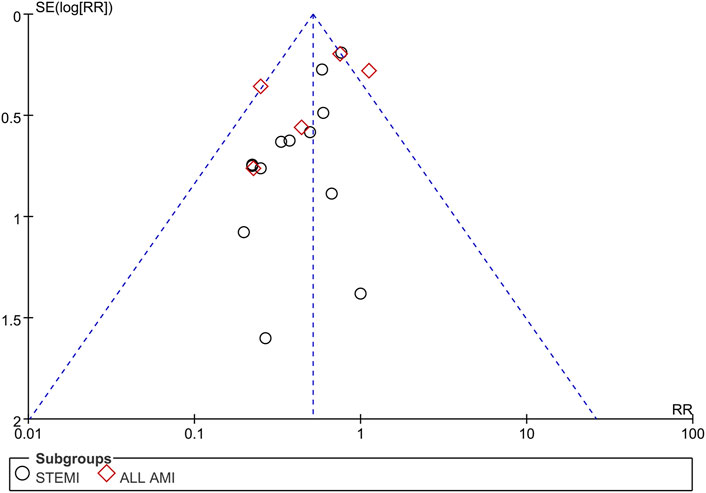
Figure 9. Funnel plot of malignant arrhythmia. Notes: STEMI, ST-segment elevation myocardial infarction; AMI, acute myocardial infarction; RR, risk ratio.
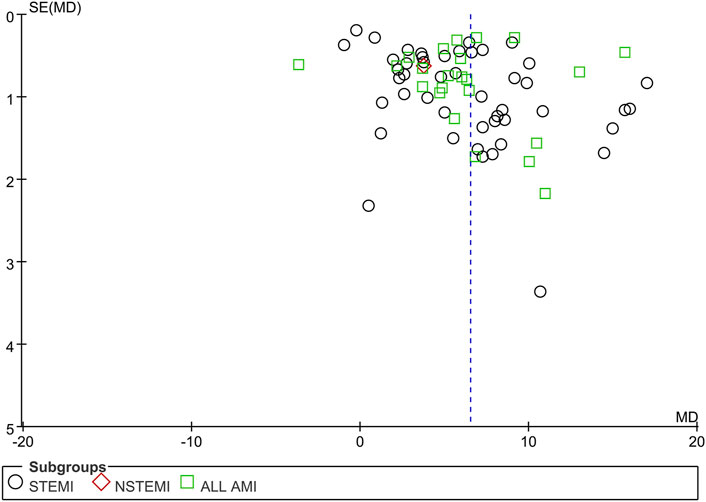
Figure 10. Funnel plot of LVEF Notes: STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; AMI, acute myocardial infarction; LVEF, left ventricular ejection fraction; MD, mean difference.
Regarding other sources of bias, all included RCTs described the comparability of baseline data, indicating a low risk of bias. For LVEF, the results changed significantly after the removal of Feng et al. (2019) in STEMI, suggesting that this RCT may be the source of heterogeneity (Supplementary Figure S6). The results changed significantly after the removal of Wu et al. (2022) and Yang and Cai (2016) in all AMI cases, suggesting that these RCTs may be the sources of heterogeneity (Supplementary Figure S7). After excluding these three studies one by one, the estimated comprehensive effect points of the remaining studies did not exceed the range, and the results were relatively robust (Supplementary Figures S8–S10).
The quality of evidence for the outcomes was assessed using the GRADE method. Due to limitations such as lack of blinding, insufficient allocation concealment, small sample sizes (less than 400 patients), and significant heterogeneity between studies, the quality of evidence for in-hospital mortality, malignant arrhythmias, and adverse events was rated as moderate. The quality of evidence for LVEF was rated as low. A detailed summary of the evidence for each outcome is provided in Table 4.
In China, the integration of TCM and biomedicine is increasingly becoming an anticipated model of medical development, as it contributes to addressing clinical issues more effectively. Taking AMI as an example, despite the rapid development of modern medical techniques, including PCI, in China, a turning point in the reduction of AMI mortality has not yet been observed (Tsao et al., 2022; GBD 2013 Mortality and Causes of Death Collaborators, 2015). Early intervention and diagnosis of diseases can reduce the incidence rate of AMI, but these areas need further research (Wang et al., 2024b; Wang et al., 2024c; Jaiswal et al., 2023). The standardized application of TCM may serve as a valuable approach to addressing this clinical issue. However, the process of integrating traditional and modern medicine requires support from high-quality evidence-based research. Our study contributes precisely to this by conducting relevant work.
Traditional Chinese Medicine injection (TCMi) refers to a sterile preparation extracted and purified from TCM, which can be in the form of a solution, emulsion, lyophilized powder, or concentrated solution (Zhang et al., 2021; Chen et al., 2022). It is known for its high bioavailability and precise therapeutic effects and has been widely used in China particularly in the treatment of AMI.
It is important to mention a concept in TCM known as “tong zheng yi bing” or “different diseases with the same pattern.” Specifically, even if it is not AMI, the same qi deficiency syndrome can be treated with medications that have the function of tonifying qi. Therefore, the use of TCMi may present issues with inappropriate indications. The TCMi selected in this study were those that have the function of tonifying qi. We identified four such TCMi through our search.
In Chinese medicine theory, qi is considered one of the fundamental substances that constitute the human body and maintain vital life activities. Functionally, qi serves roles in promoting, warming, defending, consolidating, and facilitating gasification. Thus, qi can regulate the blood, fluids, and essence; maintain body temperature; defend the body; and sustain the overall connectivity between the interior and exterior of the body. Qi transformation refers to the process of metabolism and the mutual transformation of energy among essence, blood, fluids, and other substances. None of this can be separated from the movement of qi; it can be said that qi, in its forms of ascending, descending, outgoing, and incoming, is the fundamental driving force of all life activities (Wang et al., 2023). It is evident that qi serves as the prime mover of all life activities within the human body. Mitochondria produce ATP, which is the primary source of energy for the body and the main source of power for cardiomyocytes, and the normal structure and function of mitochondria are crucial for myocardial energy metabolism (Lopaschuk and Jaswal, 2010). There is a correlation between qi and mitochondria in terms of their origin, morphology, function, and lesions (Lin et al., 2014; Zhang et al., 2001). Systematic reviews and meta-analyses of RCTs show that Qi-regulating formulations, such as Wenxin Keli and Yangxinshi tablet, may be effective and safe for treating ischemic heart disease (IHD) (Wang et al., 2016; Guo et al., 2023). Research h+as found that they play a certain role in regulating cardiac mitochondrial function (Wu et al., 2020), glucose metabolism, lipid metabolism, and amino acid metabolism (Zhang H. et al., 2018; Jiang et al., 2017). The active metabolite Ginsenoside Rb1 from Panax ginseng, known for its qi-tonifying effects, may promote myocardial recovery in AMI via mechanisms involving mitochondrial autophagy, as demonstrated by both in vivo and in vitro studies (Hu et al., 2022). Therefore, tonifying qi may have certain potential in regulating cardiac energy metabolism.
SGMI is made up of Ginseng Rubra Radix; Ophiopogonis Radix; Schisandrae Chinensis Fructus, and the main pharmacodynamic substances include ginsenoside metabolites and lignans. Clinical studies have demonstrated that SGMI can inhibit the inflammatory response in acute-phase AMI patients (Wang LM. et al., 2019). For patients in the recovery phase of AMI, SGMI can enhance clinical efficacy, boost cardiac function, improve tissue perfusion, and optimize oxygen metabolism (Luan et al., 2022). Additionally, it reduces levels of inflammatory factors (Lu and Yao, 2022), restores endothelial function (Tang, 2019), and improves hemorheological parameters (Wang, 2017). Ginsenosides, schizandrin, and ophiopogonin D are the primary active constituents of SGMI. Jiang et al. (2014) investigated the effects of this combination therapy on energy metabolism in rats with AMI and found that it can stimulate fatty acid oxidation and inhibit glycolysis, there by counteracting the metabolic reprogramming associated with AMI (Jiang et al., 2014). Li et al. (2019) found that SGMI can protect the mitochondrial structure of cardiomyocytes from Ang II-induced damage, stabilize mitochondrial membrane potential, and enhance mitochondrial oxygen utilization. Additionally, it can upregulate the expression of genes related to free fatty acid oxidation, glucose oxidation, and mitochondrial biogenesis by activating the adenosine monophosphate-activated protein kinase (AMPK) signaling pathway, which is crucial for energy metabolism (Li et al., 2019). Zhan et al. (2016) used comparative proteomics techniques to discover that SGMI may exert myocardial protection by modulating multiple energy metabolism pathways: promoting carbohydrate metabolism, inhibiting lipid metabolism, restoring the tricarboxylic acid cycle, and enhancing respiratory chain ATP production (Zhan et al., 2016).
SMI is a compound injection made of Ginseng Rubra Radix and ophiopogonis Radix, and the main pharmacodynamic substances include ginsenosides and ophiopogon saponins (Wang et al., 2020). Studies have found that SMI can alleviate oxidative stress in patients during the acute phase of AMI (Cao et al., 2022), improve vascular endothelial injury and apoptosis (Yang FF. et al., 2017), and enhance hemodynamic parameters (Qin, 2021). For patients in the recovery phase of AMI, SMI can effectively suppress inflammatory responses, reduce blood viscosity, and improve cardiac function (Zhou, 2024; Zhan and Cui, 2023). Wang et al. (2018) utilized network analysis to discover that SMI can significantly reverse the downregulation of energy metabolism-related proteins such as ATP synthase and malate dehydrogenase caused by ischemia, thereby modulating signaling pathways associated with oxidative phosphorylation and mitochondrial dysfunction. In a primary cardiomyocyte model of hypoxic injury in rats, they found that SMI can stabilize mitochondrial membrane potential, restore intracellular ATP levels, increase maximal mitochondrial respiration rate, and enhance oxygen reserve capacity, thus reversing energy metabolic imbalance (Wang Y. et al., 2018). Wang et al. (2019) found that SMI can reduce myocardial cell injury following ischemia-reperfusion (I/R). It increases the expression of glucose transporter 4, cluster of differentiation 36, and fructose-6-phosphate kinase, thereby enhancing the utilization of both free fatty acids and glucose (Wang S. et al., 2019).
SFI is made up of Ginseng Rubra Radix and Aconiti Lateralis Radix Praeparata (black shunpian), and the main active metabolites are ginsenosides and panaxynol (Zheng et al., 2022). For patients with acute-phase AMI, SFI can improve hemodynamic parameters (Zhuo et al., 2018) and reduce levels of inflammatory factors (Jin et al., 2017). For patients in the recovery phase of AMI, SFI can mitigate inflammatory responses (Li et al., 2017), improve hemorheological indicators (You and Wang, 2019), enhance fibrinolytic activity (Zhu et al., 2020), improve vascular endothelial function, and reduce oxidative damage (Jia et al., 2016). Studies have found that SFI can protect against myocardial injury by modulating mitochondrial dynamics, improving mitochondrial energy metabolism, reducing mitochondrial oxidative stress, and inhibiting structural damage to mitochondria (Lu and Xiang, 2023). Bai et al. (2018) investigated the effects of SFI on I/R injury in rats and found that it could enhance the clearance of oxygen free radicals, reduce cellular damage, reduce intracellular Ca2+ influx, increase ATP levels, and inhibit inflammation (Bo et al., 2018). Zhan et al. (2024) found that SFI can mediate mitochondrial autophagy in rats with I/R injury by regulating the HIF-1α/BNIP3 pathway, thereby protecting the mitochondrial structure and reducing myocardial cell apoptosis (Zhan et al., 2024). Ji et al. (2011) studied the effects of SFI on myocardial dysfunction following cardiac arrest and resuscitation in pigs and found that it could increase the activity of Na+-K+-ATPase and Ca2+-ATPase, and left ventricular superoxide dismutase, thereby modulating energy metabolism and enhancing antioxidant capacity (Ji et al., 2011). Additionally, Huang et al. (2020) found that Shenfu Formula could synergistically mediate metabolic flexibility of fatty acids and glucose in cardiac energy metabolism in heart failure mice induced by transverse aortic constriction through the AMPK-related pathway, thereby inhibiting cardiac metabolic remodeling (Huang et al., 2020).
AI is an injection made from Astragali Radix, and its main active metabolites include flavonoids, saponins, and amino acids (Yu H. et al., 2019). For patients with acute-phase AMI, AI can improve immune-inflammatory responses and ventricular remodeling (Hou et al., 2012). For patients in the recovery phase of AMI, AI can enhance cellular antioxidant capacity (Zhou et al., 2019), protect vascular endothelium, and increase overall antioxidant ability (Chen et al., 2015). Huang et al. (2018) investigated the effects of major extracts from Astragalus membranaceus on tert-butyl hydroperoxide-induced H9C2 cells and found that they could alleviate oxidative stress and increase cell survival by regulating mitochondrial membrane potential and enhancing mitochondrial bioenergetics parameters, including basal respiration, proton leak, maximal respiration, and non-mitochondrial respiration (Huang et al., 2018). Jin et al. (2014) found that Astragalus can correct impaired free fatty acid and glucose metabolism in AMI model rats, increase myocardial ATP, ADP, and total adenine nucleotide levels, thereby protect ischemic myocardium (Jin et al., 2014). Astragaloside IV, the primary active metabolite of AI, plays a crucial role in regulating cardiac energy metabolism. The underlying mechanisms likely involve multiple pathways: it induces the expression of mitochondria-related proteins (Wang Q. et al., 2021; Zang et al., 2020), protects the structural integrity of cardiac mitochondria (Lu et al., 2015), and modulates mitochondrial function (Dong et al., 2017).
These TCMi-TQs exhibit comparable effects. However, the safety of TCMi has become a growing concern. A retrospective investigation based on China PEACE revealed no benefits of TCMi in patients with acute heart failure (Yu Y. et al., 2019). The annual report on national adverse drug reaction monitoring (2023) revealed 2.627 million cases of suspected adverse drug reactions/events, of which traditional Chinese medicine accounted for 12.6%. Tonifying qi and yin drugs among the top five, and 25.9% of the cases involved injectable drug delivery (National Center For ADR Monitoring C, 2024). Considering the widespread use of TCMi-TQ in the AMI patient population (Spatz et al., 2018), it is necessary to conduct a high-quality systematic evaluation of its efficacy and safety.
This meta-analysis included 113 studies involving 10,779 participants. The results demonstrated that the combined application of TCMi-TQ was more effective in reducing in-hospital mortality, decreasing the occurrence of malignant arrhythmias, reducing the incidence of adverse events, and improving LVEF than biomedicine alone. Safety was also assessed in this meta-analysis, with 32 studies reporting on safety outcomes. No serious adverse events were observed, and the common adverse events included bleeding, ecchymosis, and gastrointestinal discomfort, which could be alleviated through drug withdrawal or symptomatic treatment.
Mortality rate is a crucial indicator reflecting the prognosis of AMI patients (Long et al., 2022). A retrospective study found no significant association between early application of TCMi and in-hospital bleeding or mortality rate in AMI patients (Spatz et al., 2018). However, our study revealed that the combined use of TCMi-TQ significantly reduced AMI mortality, which aligns with the findings of previous systematic reviews examining the effects of SGMI (Lu et al., 2018), SMI (Wang et al., 2015), SFI (Zhu et al., 2018), and AI (Su et al., 2017) in AMI treatment. These findings suggest that TCMi with the specific function of tonifying qi plays a unique role in reducing AMI mortality, possibly due to its comparable effects of regulating energy metabolism. Additionally, this study attempted to investigate the impact of TCMi-TQ combined with CT on the long-term mortality rate of AMI patients. However, due to the limited number of studies evaluating long-term mortality, we were unable to identify potential benefits of TCMi-TQ in long-term mortality, highlighting the need for further research.
Malignant arrhythmia is a significant cause of death in patients with acute myocardial infarction (AMI) (Eryol et al., 2002; Nasution et al., 2020). Studies have consistently demonstrated that malignant arrhythmia accompanies 60%–100% of deaths during the acute phase of AMI (Eldar et al., 1994; Berg et al., 2001). Unfortunately, the benefits of antiarrhythmic drugs for such patients are limited (Piccini et al., 2011). Although a few clinical cases have suggested that TCMi may have adverse effects leading to the occurrence of malignant arrhythmias (Jin, 2013; Zhao et al., 1995; Wu and Li, 1988), a meta-analysis revealed that the combined use of TCMi with tonifying qi properties can reduce the risk of malignant arrhythmias during hospitalization in AMI patients. This reduction in risk may be attributed to the clinical effect of TCMi-TQ in improving myocardial ischemia.
Following myocardial infarction, the loss of myocardial cells leads to myocardial remodeling and the development of heart failure (Author Anonymous, 2020), which significantly impacts the patients’ quality of life and long-term prognosis. LVEF is an essential indicator of cardiac function (McDonagh et al., 2021). This study found that the combined use of TCMi-TQ demonstrates clinically relevant improvements in cardiac function, consistent with previous meta-analysis results (Zhu et al., 2018; Wei et al., 2021). The protective effect of TCMi-TQ on ischemic myocardium may explain this improvement. However, significant heterogeneity was observed in the analysis results, and subgroup analysis and sensitivity analysis did not identify a clear source of heterogeneity. This heterogeneity may be attributed to differences in the ultrasound equipment and technical standards used for LVEF assessment. Therefore, caution must be exercised when interpreting the aforementioned results due to the presence of these heterogeneity factors.
Our meta-analysis results demonstrate that the combined administration of TCMi-TQ does not increase the occurrence of adverse events in AMI patients. Nevertheless, TCMi, when administered through direct bloodstream injection, can be influenced by various factors such as co-solvents, particulates during the manufacturing process, and solvents. This often leads to a higher occurrence of adverse reactions compared to other TCM formulations (Zhang and Niu, 2018). Therefore, healthcare providers should exercise caution in prescribing medications, prioritizing oral formulations. For patients with complex or severe conditions requiring traditional TCM injections, intramuscular administration should be preferred. In emergency situations, TCM injections via intravenous infusion may be necessary (Gao et al., 2012). Healthcare providers should strictly adhere to medication guidelines for the rational and standardized use of TCM injections. Providers should carefully prepare medications, standardize dosages and treatment plans, and accurately identify and document the evidence basis for medication use (Yu et al., 2023). Hospitals should enhance quality control and inspection during the procurement of medications. These TCM injections should be classified, stored separately, and subjected to enhanced supervision and consultation to ensure their proper use. Additionally, hospitals should integrate the quality of TCM intravenous formulations into clinical safety monitoring systems to enable traceability (Peng and Li, 2019). Assigning specialized TCM pharmacists to systematically manage these formulations can further enhance oversight and safety. Research has shown that pharmacist involvement in prescription review, dispensing, drug preparation, and patient counseling significantly reduces the incidence of adverse reactions (Deng et al., 2024). Therefore, hospitals should establish standardized management systems for TCMi and foster effective communication between pharmacists, clinical doctors, and patients to reduce the incidence of adverse reactions.
In summary, this study has the following characteristics compared to previous meta-analyses on TCMi (Mensah et al., 2023): The TCMi included in this study all possess the function of tonifying qi. This is because energy metabolism is one of the main therapeutic principles in TCM for treating AMI, reflecting the representativeness of this study (Suzuki et al., 2023). This study primarily focuses on the observing mortality rate. Meta-analyses of TCMi with mortality, a hard endpoint, as the primary outcome have been relatively rare. The conclusions of this study will provide a more valuable reference for clinical decision-making by healthcare professionals.
The present study underwent a rigorous research process, adhering strictly to a pre-registered protocol. Nonetheless, this meta-analysis still has certain limitations (Mensah et al., 2023): Regarding methodological quality, the overall quality of the included studies is suboptimal, particularly due to insufficient reporting of random sequence generation, allocation concealment methods, blinding implementation, medical follow-up, and independent assessment of the purity/potency of the TCMi-TQ utilized in the studies. These factors may introduce risks of selection bias and performance bias. Researchers should adhere to RCT design standards (Chan et al., 2013) and reporting guidelines (Butcher et al., 2022). In future clinical studies, independent collaborative laboratories should be incorporated, utilizing advanced technologies such as HPLC and GC-MS to assess the purity and efficacy of TCMi-TQ, accurately identify and quantitatively analyze active ingredients, and promote the scientific and standardized generation of high-quality clinical evidence in TCM. This will enhance the rigor and reliability of clinical trials (Suzuki et al., 2023). Regarding long-term efficacy, the included studies fail to evaluate long-term mortality, which limits the assessment of the long-term prognosis of AMI patients receiving TCMi-TQs. It is recommended to expand the evaluation of long-term survival outcomes in AMI patients who receive TCMi-TQs. This would provide a more comprehensive assessment of the clinical significance and practical application value of these treatments (National Center Cardiovascular Diseases, 2024). Regarding heterogeneity, there is notable heterogeneity in the results concerning LVEF, thereby affecting the certainty of the outcomes. These discrepancies may stem from variations in ultrasound equipment and technical standards for LVEF evaluation. To minimize the impact of human factors and ensure consistent, reliable results, it is recommended to enhance the standardization of ultrasound equipment and evaluation techniques (Roger et al., 2010). Regarding the generalizability of research results, all the included studies were conducted within China and involved a single ethnic group. While our findings provide a preliminary foundation for multicenter research, further evaluation is necessary to determine the generalizability of the conclusions. We recommend conducting multicenter trials outside of China to generate more reliable and generalizable clinical evidence.
The present study proposes that integrating TCMi-TQ with conventional biomedicine treatment has a favorable impact on reducing mortality rates, the incidence of malignant arrhythmias, the incidence of adverse events, and enhancing cardiac function among patients with AMI. Given the low methodological quality observed in the included studies, it is imperative to approach this conclusion with caution. Nevertheless, these findings hold significant potential for informing clinical practice guidelines, and we look forward to achieving the scientific integration of TCMi-TQ with standard care in the future.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
HwZ: Conceptualization, Formal Analysis, Methodology, Validation, Visualization, Writing–original draft. JC: Conceptualization, Formal Analysis, Methodology, Validation, Writing–original draft. HL: Funding acquisition, Methodology, Supervision, Writing–review and editing. XL: Funding acquisition, Methodology, Supervision, Writing–review and editing. HqZ: Formal Analysis, Investigation, Writing–review and editing. SZ: Investigation, Writing–review and editing. YS: Formal Analysis, Investigation, Writing–review and editing. YL: Investigation, Writing–review and editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Grants from the National Natural Science Foundation of China (No. 82104767, No. 82174315); Beijing major and difficult diseases collaborative research project of traditional Chinese and Western medicine (No. 2023BJSZDYNJBXTGG-011); Beijing “The Fourteenth Five-Year” key specialty of Traditional Chinese Medicine cardiovascular Department (demonstration class) (BJZKLC0011); Research and Translational Application of Clinical Specialized Diagnosis and Treatment Techniques in the Capital (No. Z221100007422127); Scientific Research Program of Hebei Provincial Administration of Traditional Chinese Medicine (No. B2025055); And Training Fund for Open Projects at Clinical Institutes and Departments of Capital Medical University (No. CCMU2024ZKYXY012); Youth Talent Support Project of the Chinese Association of Traditional Chinese Medicine (No. CACM-2024-QNRC2-B20); Beijing Traditional Chinese Medicine New Era 125 Project Promotes Talents. Capital Health Development Research Special Project (No. 2022-1-2231).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1511486/full#supplementary-material
Author Anonymous (2020). Expert consensus on prevention and treatment of heart failure after myocardial infarction. Chin. Cardiocirc. J. Chin. (35), 1166–1180. doi:10.3969/j.issn.1000-3614.2020.12.002
Bai, Y. K., Wang, Y. H., Hao, Y. L., Liang, Y. Q., and Li, X. X. (2002). Clinical observation of 999 Shenmai injection and western medicine on 62 patients with acute myocardial infarction. Mod. J. Integr. Tradit. Chin. West. Med. Chin., 285–286. doi:10.3969/j.issn.1008-8849.2002.04.003
Berg, R. A., Sanders, A. B., Kern, K. B., Hilwig, R. W., Heidenreich, J. W., Porter, M. E., et al. (2001). Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation 104, 2465–2470. doi:10.1161/hc4501.098926
Bo, B. J., Tian, Y. C., Kang, X. Q., Qiao, Y. G., and Zhao, D. (2018). Effect of Shenfu injection on Ca2+ and KATP channels in MIRI rats. Clin. Res. Pract. Chin. 3, 5–6. doi:10.19347/j.cnki.2096-1413.201826002
Butcher, N. J., Monsour, A., Mew, E. J., Chan, A. W., Moher, D., Mayo-Wilson, E., et al. (2022). Guidelines for reporting outcomes in trial reports: the consort-outcomes 2022 extension. JAMA 328, 2252–2264. doi:10.1001/jama.2022.21022
Cao, J. C., Guo, L., and Sun, Q. Y. (2022). Curative effect of shenmai injection combined with western medicine on No-reflow after PCI in patients with acute myocardial infarction and its effect on myocardial injury and oxidative stress. J. New Chin. Med. Chin. 54, 48–52. doi:10.13457/j.cnki.jncm.2022.15.010
Chan, A. W., Tetzlaff, J. M., Gøtzsche, P. C., Altman, D. G., Mann, H., Berlin, J. A., et al. (2013). SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 346 (8), e7586. doi:10.1136/bmj.e7586
Chen, G. L. (2021). Ginseng-assisted intravenous thrombolysis in acute ST-segment elevation myocardial infarction. Practical Clinical J of Integr. Tradit. Chin. West. Med. (Chin.) 21, 64–65. doi:10.13638/j.issn.1671-4040.2021.13.031
Chen, H., Ceng, X. T., Gu, W. J., Bai, Z. G., and Gu, Y. H. (2018). The introduction of using new version of guideline development tool (GRADE pro GDT) in the systematic reviews of the intervention studies. Chin. J. Evid. Based Med. Chin. 18, 1135–1142.
Chen, J. D., Zhang, L. T., Chen, X. H., and Qian, J. (2015). Clinical observation on Astragalus injection for treatment of acute myocardial infarction after percutaneous coronary intervention. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. Chin. 17, 1924–1926. doi:10.3969/j.issn.1672-1349.2015.17.002
Chen, Q. T. (2017). Effect of Shengmai injection on cardiac function after PCI in patients with ST-segment elevation myocardial infarction. Bachelor’s degree. Qingdao (China): Qingdao University.
Chen, W. J., Zeng, W. T., Hong, J. L., Guo, S. B., and Zhang, M. Y. (2003). The effect of shenfu injection on left heart function in patients with acute myocardial infarction--with a report of 40 cases. New Med. Chin., 746–747. doi:10.3969/j.issn.0253-9802.2003.12.016
Chen, Y. J., and Qiao, W. (2018). Effects of shenfu injection on cardiac function in patients with acute myocardial infarction. J. Rare Uncommon Dis. (Chin.) 25, 11–13. doi:10.3969/j.issn.1009-3257.2018.06.005
Chen, Z. Y., Liu, Y., Wei, Y., Deng, L. Y., and Zhang, Q. (2022). Efficacy of traditional Chinese medicine injection in preventing oxaliplatin-induced peripheral neurotoxicity: an analysis of evidence from 3598 patients. Evid. Based Complement. Altern. Med. 2022, 6875253. doi:10.1155/2022/6875253
Cui, J. D., and Li, X. F. (2006). Clinical observation on 38 cases of acute myocardial infarction treated with auxiliary treatment of Shengmai injection. J. Pract. Med. Tech. Chin., 3598–3599. doi:10.3969/j.issn.1671-5098.2006.20.055
Deeks, J. J., Higgins, J. P. T., and Altman, D. G. (2023). On behalf of the Cochrane statistical methods group Cochrane handbook for systematic reviews of interventions. in Chapter 10: analysing data and undertaking meta-analyses. Available online at: https://training.cochrane.org/handbook/archive/v6.4/chapter-10 (Accessed October 1, 2024).
Deng, S. Q., Luo, X. H., and Xu, D. L. (2024). Analysis of the effect of pharmacist intervention on the rational use of traditional Chinese medicine injections. Chin. Sci. Technol. J. Database (Abstr. Ed.) Med. Health (Chin.) (10), 153–156.
Ding, L., and Xu, M. H. (2006). Clinical observation on the adjuvant treatment of acute myocardial infarction complicated with cardiogenic shock with Shengmai Injection. Gansu Tradit. Chin. Med. Chin. 19, 11. doi:10.3969/j.issn.1004-6852.2006.08.006
Dong, Z., Zhao, P., Xu, M., Zhang, C., Guo, W., Chen, H., et al. (2017). Astragaloside IV alleviates heart failure via activating PPARα to switch glycolysis to fatty acid β-oxidation. Sci. Rep. 7, 2691. doi:10.1038/s41598-017-02360-5
Du, Y. K. (2017). Clinical study of Shenmai injection combined with thrombolytic therapy legislation riverstone anterior wall acute myocardial infarction reperfusion injury. Shaanxi J. Tradit. Chin. Med. Chin. 38, 171–173. doi:10.3969/j.issn.1000-7369.2017.02.015
Egger, M., Davey, S. G., Schneider, M., and Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. doi:10.1136/bmj.315.7109.629
Eldar, M., Ohad, D., Bor, A., Varda-Bloom, N., Swanson, D. K., and Battler, A. (1994). A closed-chest pig model of sustained ventricular tachycardia. Pacing Clin. Electrophysiol. 17, 1603–1609. doi:10.1111/j.1540-8159.1994.tb02353.x
Eryol, N. K., Topsakal, R., Oguzhan, A., Abaci, A., Basar, E., Ergin, A., et al. (2002). Is the change of late potential over time related to enzyme levels? Ischemic burden in acute myocardial infarction. Ann. Noninvasive Electrocardiol. 7, 242–246. doi:10.1111/j.1542-474x.2002.tb00170.x
Feng, J. P., Liang, M. F., Wang, Y. H., and Yan, W. (2019). Effect analysis on Shenfu Injection combined with enoxaparin sodium in treatment of acute myocardial infarction complicated with heart failure. Drug Eval. Res. Chin. 42, 2057–2061. doi:10.7501/j.issn.1674-6376.2019.10.028
Feng, Q. L., Yao, A. Q., and Dang, Y. H. (2011). Effect of shenfu injection on ventricular remodeling in patients with acute myocardial infarction and clinical observations. J. Emerg. Trad. Chin. Med. Chin. 20, 1183–1184. doi:10.3969/j.issn.1004-745X.2011.07.101
Gao, R., Weng, W. L., and Li, R. (2012). The principle and methods of reasonable application of traditional Chinese medicine injection. China licens. Pharm. Chin. 9, 5–8. doi:10.3969/j.issn.1672-5433.2012.12.002
GBD 2013 Mortality and Causes of Death Collaborators (2015). Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385, 117–171. doi:10.1016/S0140-6736(14)61682-2
Guan, J., Huang, F. K., Zhou, Y. L., Li, B. Q., Chen, Y. W., Wang, Y., et al. (2023). Research progress on the mechanism of astragaloside IV in preventing ischemia hypoxia myocardial injury in patients with heart failure. Pract. J. Card. Cereb. Pneumal Vasc. Dis. Chin. 31, 111–114. doi:10.12114/j.issn.1008-5971.2023.00.180
Guo, H., Zhu, M., Yu, R., Li, X. Y., and Zhao, Q. F. (2023). Efficacy of Chinese traditional patent medicines for heart failure with preserved ejection fraction: a Bayesian network meta-analysis of 64 randomized controlled trials. Front. Cardiovasc Med. 10, 1255940. doi:10.3389/fcvm.2023.1255940
Guo, S. (2014). Study on the myocardial protective effect of shenmai injection on patients with acute myocardial infarction after emergency PCI surgery. Bachelor’s degree. Henan (China): Xinxiang Medical University, 7–14.
Guo, S. P., and Zhang, Y. Z. (1999). Antimyocardial thwarting effect of shenmai injection in urokinase thrombolysis for acute myocardial infarction. Acta Acad. Med. Weifang Chin. 21, 271–273.
Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., et al. (2008). GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926. doi:10.1136/bmj.39489.470347.AD
Han, G. J., Ma, Z. X., Xue, X. R., Lu, L. Y., and Zhang, Y. (2000). Effect of astragalus injection on reperfusion injury in acute myocardial infarction treated with intravenous thrombolysis. Chin. J. Integr. Tradit. West. Med. Intensive Crit. Care (Chin), 107–108. doi:10.3321/j.issn:1008-9691.2000.02.015
Han, G. M., Han, X. Y., and Meng, Y. H. (2003). Twenty-one cases of acute myocardial infarction with western and traditional Chinese medicine. Shandong J. Tradit. Chin. Med. Chin., 485–487. doi:10.16295/j.cnki.0257-358x.2003.08.028
Hao, L. N., Pei, G. X., and Li, Y. P. (2021). Effect of shenfu injection on myocardial reinfusion TIMI flow grading and fibrinolytic indexes in patients undergoing PCI for AMI. Chin. J. Conval. Med. Chin. 30, 429–431. doi:10.13517/j.cnki.ccm.2021.04.035
He, C. F., Ji, Q. J., Zhang, L., Xie, X. F., Han, X. L., and Li, C. (2016). Investigate the influence on cardiac structure and function of patients with acute myocardial infarction treated with Shenmai combined with tirofiban after interventional therapy. J. Clin. Emerg. Chin. 17, 671–674. doi:10.13201/j.issn.1009-5918.2016.09.004
Heinrich, M., Jalil, B., Abdel-Tawab, M., Echeverria, J., Kulić, Ž., McGaw, L. J., et al. (2022). Best Practice in the chemical characterisation of extracts used in pharmacological and toxicological research-The ConPhyMP-Guidelines. Front. Pharmacol. 13, 953205. doi:10.3389/fphar.2022.953205
Heusch, G., and Gersh, B. J. (2017). The pathophysiology of acute myocardial infarction and strategies of protection beyond reperfusion: a continual challenge. Eur. Heart J. 38, 774–784. doi:10.1093/eurheartj/ehw224
Higgins, J. P. T., Li, T. J., and Deeks, J. J. (2023). Chapter 6: choosing effect measures and computing estimates of effect. Available online at: https://training.cochrane.org/handbook/archive/v6.4/chapter-06 (Accessed October 1, 2024).
Hou, Y., Chen, Z. H., Wang, Y., Yang, L., and Wu, Y. X. (2012). Impact of Huangqi injection on inflammation and ventricular remodeling in patients with acute myocardial infarction. J. Clin. Cardiol. Chin. 28, 766–768.
Hu, J., Zhang, L., Fu, F., Lai, Q., Zhang, L., Tao, L., et al. (2022). Cardioprotective effect of ginsenoside Rb1 via regulating metabolomics profiling and AMP-activated protein kinase-dependent mitophagy. J. Ginseng Res. 46, 255–265. doi:10.1016/j.jgr.2021.06.011
Huang, Y., Kwan, K., Leung, K. W., Wang, H., Kong, X. P., Dong, T., et al. (2018). The extracts and major compounds derived from Astragali Radix alter mitochondrial bioenergetics in cultured cardiomyocytes: comparison of various polar solvents and compounds. Int. J. Mol. Sci. 19, 1574. doi:10.3390/ijms19061574
Huang, Y., Zhang, K., Jiang, M., Ni, J., Chen, J., Li, L., et al. (2020). Regulation of energy metabolism by combination therapy attenuates cardiac metabolic remodeling in heart failure. Int. J. Biol. Sci. 16, 3133–3148. doi:10.7150/ijbs.49520
Huang, Y. W., Lin, B., and Zhang, M. Y. (2015). Observation of shenmai injection and atorvastatin in treatment of patients with acute myocardial infarction. Chin. Arch. Tradit. Chin. Med. Chin. 33, 2558–2560. doi:10.13193/j.issn.1673-7717.2015.10.079
Jaiswal, V., Wajid, Z., Suresh, V., Hanif, M., Rajak, K., Halder, A., et al. (2023). Procedural safety of transcatheter aortic valve replacement with Portico valve: a systematic review. Int. J. Surg. 109, 3602–3608. doi:10.1097/JS9.0000000000000645
Ji, F., Ren, Y. L., Zhang, Y. B., and Chen, X. B. (2021). Application of shenmai injection in patients with ST-segment elevation myocardial infarction with deficiency of both qi and yin. World Chin. Med. Chin. 16, 643–647. doi:10.3969/j.issn.1673-7202.2021.04.021
Ji, X. F., Yang, L., Zhang, M. Y., Li, C. S., Wang, S., and Cong, L. H. (2011). Shen-fu injection attenuates postresuscitation myocardial dysfunction in a porcine model of cardiac arrest. Shock 35, 530–536. doi:10.1097/SHK.0b013e31820e2058
Jia, F. Y., Gao, S. W., Zhang, Q., Pang, J. Z., and Xu, Q. (2023). Meta-analysis of efficacy and safety of Shenfu Injection combined with conventional western medicine in treatment of acute myocardial infarction after PCI. Drug Eval. Res. Chin. 46, 1323–1333. doi:10.7501/j.issn.1674-6376.2023.06.021
Jia, P., Zi, H. Y., and Ceng, Y. J. (2016). Influence of Shenfu injection on effect and endothelial function in patients with acute inferior wall ST-elevation myocardial infarction complicated with hypotension after percutaneous coronary intervention. China Med. Chin. 11, 789–792. doi:10.3760/cma.j.issn.1673-4777.2016.06.002
Jiang, M., Kang, L., Wang, Y., Zhao, X., Liu, X., Xu, L., et al. (2014). A metabonomic study of cardioprotection of ginsenosides, schizandrin, and ophiopogonin D against acute myocardial infarction in rats. BMC Complement. Altern. Med. 14, 350. doi:10.1186/1472-6882-14-350
Jiang, M., Wang, Q., Chen, J., Wang, Y., Fan, G., and Zhu, Y. (2017). Comparative metabonomics of Wenxin Keli and Verapamil reveals differential roles of gluconeogenesis and fatty acid β-oxidation in myocardial injury protection. Sci. Rep. 7, 8739. doi:10.1038/s41598-017-09547-w
Jin, Y., Chen, Q., Li, X., Fan, X., and Li, Z. (2014). Astragali Radix protects myocardium from ischemia injury by modulating energy metabolism. Int. J. Cardiol. 176, 1312–1315. doi:10.1016/j.ijcard.2014.07.154
Jin, Y. Y., Gao, H., Yan, Y., and Zhang, H. (2017). The effect of Shenfu injection on IL-6 and TNF - α in patients with acute ST segment elevation myocardial infarction complicated by cardiogenic shock. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. Chin. 15, 59–63. doi:10.3969/j.issn.1672-1349.2017.01.016
Jin, Y. Z. (2013). A case of ventricular tachycardia induced by shengmai injection. Chin. J. Trauma Disabil. Med. Chin. 21, 220–221.
Kang, W. L. (2017). Clinical efficacy analysis of shenfu injection in the treatment of patients with acute myocardial infarction. Chin. Prim. Health Care (Chin) 31, 82–83. doi:10.3969/j.issn.1001-568X.2017.07.0034
Lan, Z., Tuo, P., Gao, Y. G., Li, B., Yan, N. Z., Chen, X. H., et al. (2021). Study on the efficacy of shenfu injection combined with sodium creatine phosphate in the treatment of acute ST-segment elevation inferior wall myocardial infarction. J. Emerg. Trad. Chin. Med. Chin. 30, 1374–1377. doi:10.3969/j.issn.1004-745X.2021.08.014
Li, D. K., Zhu, J., Hu, X. L., Gao, Z., Xing, G., and Yu, L. F. (2017). Clinical efficacy of shenfu injection and reteplase in the treatment of acute ST elevation myocardial infarction. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. (Chin) 15, 3007–3010. doi:10.3969/j.issn.1672-1349.2017.23.019
Li, G. Y. (2013). Clinical study on the intervention of shenfu injection in the formation of ventricular wall tumor in patients with acute myocardial infarction. Chin. Manip. and Rehabilit. Med. (Chin.) 4, 36–39. doi:10.3969/j.issn.1008-1879.2013.03.018
Li, N., and Cheng, W. L. (2014). Clinical research of Shenfu Injection used in treating acute myocardial infarction accompanied right heart failure. China J. Tradit. Chin. Med. Pharm. Chin. 29, 3061–3063.
Li, Q., Zhang, S., Yang, G., Wang, X., Liu, Y., Chen, Y., et al. (2023). Energy metabolism: a critical target of cardiovascular injury. Biomed. Pharmacother. 165, 115271. doi:10.1016/j.biopha.2023.115271
Li, Q. H., Deng, X., Zhou, X. Y., and Jiang, H. M. (2016). Influence of shenmai injection on myocardia of patients with acute myocardial infarction after PCI operation. Henan tradit. Chin. Med. Chin. 36, 430–433. doi:10.16367/j.issn.1003-5028.2016.03.0187
Li, R., and Hou, A. J. (2017). Clinical study of shenfu injection in the treatment of acute myocardial infarction with pump failure. Clin. J. Tradit. Chin. Med. Chin. 29, 1874–1877. doi:10.16448/j.cjtcm.2017.0622
Li, S. G. (2016). Clinical study on the treatment of combined cardiogenic shock after PCI for acute myocardial infarction with shenfu injection. Asia-Pacific Tradit. Med. Chin. 12, 140–141. doi:10.11954/ytctyy.201617067
Li, W. D. (2015a). Treatment of acute myocardial infarction with heart failure with injection of reference. Jilin J. Tradit. Chin. Med. Chin. 35, 901–903. doi:10.13463/j.cnki.jlzyy.2015.09.011
Li, Y., Ruan, X., Xu, X., Li, C., Qiang, T., Zhou, H., et al. (2019). Shengmai injection suppresses angiotensin II-induced cardiomyocyte hypertrophy and apoptosis via activation of the AMPK signaling pathway through energy-dependent mechanisms. Front. Pharmacol. 10, 1095. doi:10.3389/fphar.2019.01095
Li, Y. F. (2015b). Analysis of the clinical efficacy of ginseng injection applied to rescue the early stage of acute extensive anterior wall myocardial infarction in emergency medical treatment. China Health Care and Nutr. (Chin) 25, 120–121.
Li, Z. E. (2006). A clinical study on the treatment of acute myocardial infarction (ST elevation type) complicated with left heart failure by different dosage of shenfu injection. J. New Chin. Med. Chin., 19–20. doi:10.13457/j.cnki.jncm.2006.06.012
Li, Z. M., Hu, Q., Mao, Y., and Li, H. J. (2010). Effect of shenfu injection with conventional therapy on heart failure in elderly patients with myocardial infarction. Chin. J. Integr. Med. Chin. 30, 996–998.
Liang, W. S. (2006). Clinical study on the treatment of acute myocardial infarction in the elderly by combining Chinese and Western medicine. China Med. Chin., 275–277. doi:10.3760/cma.j.issn.1673-4777.2006.05.010
Lin, F., Guo, L. L., and Wang, J. (2014). Explaining the role of qi in Chinese medicine based on the function of mitochondria. Chin. J. Integr. Med. Chin. 34, 903–906. doi:10.7661/CJIM.2014.08.0903
Liu, B. F. (2012). Clinical efficacy of 20 cases of acute inferior wall combined right ventricular myocardial infarction treated with traditional Chinese and western medicines. World Health Dig. Chin. 9, 118–119. doi:10.3969/j.issn.1672-5085.2012.29.108
Liu, G. S. (2016). Effectiveness and pharmacologic analysis of shenmai injection in the treatment of acute myocardial infarction. Strait Pharm. J. Chin. (28), 99–100. doi:10.3969/j.issn.1006-3765.2016.01.042
Liu, L. L. (2018). Effect of shenfu injection combined with simvastatin on cardiac function indexes in patients with acute myocardial infarction combined with diabetes mellitus. J. Pract. Diabetology (Chin.) 14, 23–24.
Liu, L. L., and Tu, X. X. (2016). Observation on the effect of using shenmai injection before percutaneous coronary intervention in patients with acute myocardial infarction. J. New Chin. Med. Chin. 48, 24–26. doi:10.13457/j.cnki.jncm.2016.10.010
Liu, S. K., Liu, Y., and Wang, Y. Y. (2004). Study of effect of Shen Mai injection on acute myocardial infarction. China J. Mod. Med. Chin., 108–109. doi:10.3969/j.issn.1005-8982.2004.05.035
Long, S. E. (2007). Clinical observation on 32 cases of acute myocardial infarction combined with heart failure treated with the aid of shenmai injection. Guizhou Med. J. Chin., 1009–1010. doi:10.3969/j.issn.1000-744X.2007.11.025
Long, Z., Liu, W., Zhao, Z., Tong, S., Wang, L., Zhou, M., et al. (2022). Case fatality rate of patients with acute myocardial infarction in 253 chest pain centers - China, 2019-2020. China CDC Wkly. 4, 518–521. doi:10.46234/ccdcw2022.026
Lopaschuk, G. D., and Jaswal, J. S. (2010). Energy metabolic phenotype of the cardiomyocyte during development, differentiation, and postnatal maturation. J. Cardiovasc Pharmacol. 56, 130–140. doi:10.1097/FJC.0b013e3181e74a14
Lu, D. X., and Yao, W. Y. (2022). Analysis of the effect of Shengwei injection combined with dobutamine injection in the treatment of heart failure after acute myocardial infarction. Proc. Clin. Med. (Chin.) 31, 504–507. doi:10.16047/j.cnki.cn14-1300/r.2022.07.018
Lu, F. P., Su, N., Zheng, Z. M., Zhu, M. M., Shen, Y. J., Shi, H. F., et al. (2018). Shengmai Injection combined with conventional treatment for acute myocardial infarction: a systematic review and Meta-analysis. Chin. Tradit. Herb. Drugs. (Chin.) 49, 1201–1210. doi:10.7501/j.issn.0253-2670.2018.05.032
Lu, J. M. (2011). Application of shengmai injection and urokinase in acute myocardial infarction with thrombolytic therapy. Natl. Med. Front. China (Chin.) 6, 32–37. doi:10.3969/j.issn.1673-5552.2011.08.0018
Lu, M., Jiang, Y. Z., Zhang, X. H., Zhang, B. M., and Fu, S. P. (2005). Protective effects of Shengmai injection on myocardial ischemic reperfusion injury. J. Jilin Univ. Med. Ed. Chin. 3, 446–448. doi:10.3969/j.issn.1671-587X.2005.03.038
Lu, S. Q., and Xiang, C. Q. (2023). Protective effect of Shenfu injection based on mitochondrial target on myocardial injury. China Med. Pharm. Chin. 13, 51–54. doi:10.3969/j.issn.2095-0616.2023.06.014
Lu, Y., Li, S., Wu, H., Bian, Z., Xu, J., Gu, C., et al. (2015). Beneficial effects of astragaloside IV against angiotensin II-induced mitochondrial dysfunction in rat vascular smooth muscle cells. Int. J. Mol. Med. 36, 1223–1232. doi:10.3892/ijmm.2015.2345
Lu, Y. H. (2009). Clinical observation on the effect of urokinase combined with shengmai injection on left ventricular function in patients with acute myocardial infarction. J. Clin. Exp. Med. Chin. 8, 86–87. doi:10.3969/j.issn.1671-4695.2009.02.049
Luan, G. X., Zhao, X. L., and Zheng, X. (2022). Levosimendan combined with Shengmai injection for the treatment of pump failure in 55 patients with acute myocardial infarction. Chin. J. Prim. Med. Pharm. Chin. 29, 23–27. doi:10.3760/cma.j.issn.1008-6706.2022.01.006
Luo, S. (2016). Clinical study on the treatment of acute myocardial infarction by shenmai injection together with conventional therapy of western medicine. Asia-Pacific Tradit. Med. Chin. 12, 150–151. doi:10.11954/ytctyy.201618074
Ma, X. G., Wang, W. Q., and Zhang, J. L. (2019). Clinical efficacy of shenfu injection in the treatment of acute myocardial infarction combined with heart failure. Gansu Med. J. Chin. 38, 916–917.
Ma, X. S., Wang, Y. N., Peng, B., Cui, J., Wang, H. C., and Dong, Z. H. (2022). Effect of shenfu injection on serum sST2 in patients with acute myocardial infarction. J. Emerg. Trad. Chin. Med. Chin. 31, 2187–2190. doi:10.3969/j.issn.1004-745X.2022.12.030
McDonagh, T. A., Metra, M., Adamo, M., Gardner, R. S., Baumbach, A., Bohm, M., et al. (2021). 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42 (42), 3599–3726. doi:10.1093/eurheartj/ehab368
Meng, F. S. (2014). Clinical observation on the treatment of acute extensive anterior wall myocardial infarction combined with left heart failure by shenfu injection. J. Emerg. Trad. Chin. Med. Chin. 23, 2002–2031. doi:10.3969/j.issn.1004-745X.2014.11.015
Mensah, G. A., Fuster, V., Murray, C. J. L., and Roth, G. A. (2023). Global burden of cardiovascular diseases and risks, 1990-2022. J. Am. Coll. Cardiol. 82, 2350–2473. doi:10.1016/j.jacc.2023.11.007
Mi, Z. Y., Li, Y. X., and Zhang, D. B. (2009). Observation on the efficacy of Astragalus injection in the treatment of acute myocardial infarction complicated with cardiogenic shock. J. Emerg. Trad. Chin. Med. Chin. 18, 1621–1647. doi:10.3969/j.issn.1004-745X.2009.10.032
Mo, C. R., and Zhao, K. M. (2002). Adjuvant treatment of acute myocardial infarction with heart failure by shenfu injection in 36 cases. Chin. J. Integr. Med. Chin., 812. doi:10.7661/CJIM.2002.11.812
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1. doi:10.1186/2046-4053-4-1
Nasution, S. A., Alwi, I., Subekti, I., Yamin, M., Suhendro, S., Harimurti, K., et al. (2020). The role of acute hyperglycemia on the risk of malignant arrhythmia in acute myocardial infarction patients: a study of myocardial damage, ion channel changes and inflammatory factors. Acta Med. Indones. 52, 102–110.
National Center For ADR Monitoring C (2024). National adverse drug reaction surveillance annual report (2023). Chin. J. Viral Dis. Chin. 14, 204–210. doi:10.16505/j.2095-0136.2024.3002
National Center for Cardiovascular Diseases (2024). China DI. Report on cardiovascular health and diseases in China 2023: an updated summary. Chin. Cardiocirc. J. Chin. 39, 625–660. doi:10.3969/j.issn.1000-3614.2024.07.001
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 88, 105906. doi:10.1016/j.ijsu.2021.105906
Pei, J. N., Liu, J., Liang, Z. F., Wang, X. L., Li, W., and Guo, P. (2019). Clinical efficacy of combined Chinese and Western medicine in the treatment of acute anterior wall ST-segment elevation myocardial infarction. Med. Inf. Chin. 32, 166–167. doi:10.3969/j.issn.1006-1959.2019.08.052
Peng, G. P., and Li, C. Y. (2019). Thinking and analysis on the safety of traditional Chinese medicine injection. J. Nanjing Univ. Tradit. Chin. Med. Chin. 35, 744–751. doi:10.14148/j.issn.1672-0482.2019.0744
Piccini, J. P., Schulte, P. J., Pieper, K. S., Mehta, R. H., White, H. D., Van de Werf, F., et al. (2011). Antiarrhythmic drug therapy for sustained ventricular arrhythmias complicating acute myocardial infarction. Crit. Care Med. 39, 78–83. doi:10.1097/CCM.0b013e3181fd6ad7
Qi, Y. W., Wu, Z. R., and Feng, Z. Y. (2015a). Clinical observation on 60 cases of acute myocardial infarction treated with shenmai injection. Guid. J. Tradit. Chin. Med. Pharmacol. Chin. 21, 93–95. doi:10.13862/j.cnki.cn43-1446/r.2015.06.033
Qi, Y. W., Wu, Z. R., Ma, Z. G., Feng, Z. Y., and Liu, Y. X. (2015b). Treatment of acute myocardial infarction of ST-segment elevation type by shenmai combined with ritonril and its effect on ventricular function and plasma brain natriuretic peptide level. Shaanxi J. Tradit. Chin. Med. Chin. 36, 562–564. doi:10.3969/j.issn.1000-7369.2015.05.021
Qi, Y. W., Wu, Z. R., Ma, Z. G., Feng, Z. Y., Liu, Y. X., and Liu, B. L. (2015c). Action mechanism of adjuvant therapy of shenmai injection in treating acute ST-segment elevation myocardial infarction. Chin. J. Exp. Tradit. Med. Formulae Chin. 21, 195–198. doi:10.13422/j.cnki.syfjx.2015100195
Qin, G. Q. (2021). Clinical observation of left ximengdan combined with shenmai injection in the treatment of acute myocardial infarction with cardiogenic shock. Chin. Health Care (Chin.) 39, 83–85.
Qu, Y. Z. (2007). Effect of shenmai injection on Q-T dispersion in patients with acute myocardial infarction. Mod. J. Integr. Tradit. Chin. West. Med. Chin., 916–917. doi:10.3969/j.issn.1008-8849.2007.07.037
Roger, V. L., Weston, S. A., Gerber, Y., Killian, J. M., Dunlay, S. M., Jaffe, A. S., et al. (2010). Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation 121, 863–869. doi:10.1161/CIRCULATIONAHA.109.897249
Shen, Y. X., Gao, H., and Ruan, G. A. (2006). Observation on the efficacy of shenfu injection in the treatment of acute myocardial infarction. J. Qiqihar Univ. Med. Chin., 1038–1039. doi:10.3969/j.issn.1002-1256.2006.09.009
Shi, B. Z., Yang, M. H., Dong, Y., Dong, X., Wang, L., Li, Y. T., et al. (2018). Effect and mechanism study of Shenmai injection in treating acute ST-elevation myocardial infarction with cardiogenic shock. Chin. J. Hosp. Pharm. Chin. 38, 2459–2463. doi:10.13286/j.cnki.chinhosppharmacyj.2018.23.16
Shi, J., and Li, S. F. (2016). Clinical study on the adjuvant treatment of acute myocardial infarction with shenmai injection. Chin. J. Clin. Pharmacol. (Chin.) 32, 2222–2224. doi:10.13699/j.cnki.1001-6821.2016.24.003
Shi, L., and Lin, L. (2019). The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Med. Baltim. 98, e15987. doi:10.1097/MD.0000000000015987
Song, C. J. (2018). Effect of Shengmai injection combined with routine treatment on cardiogenic shock after AMI and its influence on cardiac function, serum cTnI, cTnI-mRNA, CaM and urine volume. Clin. Res. Pract. (Chin.) 3, 108–110. doi:10.19347/j.cnki.2096-1413.201806052
Spatz, E. S., Wang, Y., Beckman, A. L., Wu, X., Lu, Y., Du, X., et al. (2018). Traditional Chinese medicine for acute myocardial infarction in western medicine hospitals in China. Circ. Cardiovasc Qual. Outcomes 11, e004190. doi:10.1161/CIRCOUTCOMES.117.004190
Sterne, J., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., et al. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898. doi:10.1136/bmj.l4898
Su, N., Lu, F. P., Zhu, M. M., Zheng, Z. M., Shi, H. F., and Shen, Y. J. (2017). Meta-analysis of Astragalus injection in the treatment of myocardial infarction. Lishizhen Med. Mater. Medica Res. Chin. 28, 3009–3013.
Sun, L. (2019). Shenmai injection as an adjunct in the treatment of acute myocardial infarction. Chin. Pract. Med. Chin. 14, 102–104. doi:10.14163/j.cnki.11-5547/r.2019.36.054
Suzuki, T., Kataoka, Y., Shiozawa, M., Morris, K., Kiyoshige, E., Nishimura, K., et al. (2023). Heart-brain team approach of acute myocardial infarction complicating acute stroke: characteristics of guideline-recommended coronary revascularization and antithrombotic therapy and cardiovascular and bleeding outcomes. J. Am. Heart Assoc. 12, e027156. doi:10.1161/JAHA.122.027156
Tang, F. N. (2019). Effect of treatment with Shengmai Injection combined with tirofiban on vascular endothelial and fibrinolytic function in patients with acute myocardial infarction. Med. J. Commun. Chin. 33, 48–49. doi:10.19767/j.cnki.32-1412.2019.01.017
Thiele, H., Akin, I., Sandri, M., Fuernau, G., de Waha, S., Meyer-Saraei, R., et al. (2017). PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N. Engl. J. Med. 377, 2419–2432. doi:10.1056/NEJMoa1710261
Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Alonso, A., Beaton, A. Z., Bittencourt, M. S., et al. (2022). Heart disease and stroke statistics-2022 update: a report from the American heart association. Circulation 145, e153–e639. doi:10.1161/CIR.0000000000001052
Wang, A., Song, Q., Li, Y., Fang, H., Ma, X. J., Li, Y. X., et al. (2024a). Effect of traditional Chinese medicine on metabolism disturbance in ischemic heart diseases. J. Ethnopharmacol. 329, 118143. doi:10.1016/j.jep.2024.118143
Wang, A. J., Sun, L., Li, M., Li, J., Lu, S. Q., and Zhang, F. B. (2021a). Study on the efficacy and mechanism of shenmai injection combined with western drugs in patients with acute myocardial infarction. Prog. Mod. Biomed. Chin. 21, 100–103. doi:10.13241/j.cnki.pmb.2021.01.021
Wang, C. L., and Qing, L. J. (2017). Clinical observation on the treatment of combined pump failure after PCI for acute myocardial infarction by shenfu injection combined with dopamine continuous sedation. J. Guangxi Univ. Chin. Med. Chin. 20, 7–09. doi:10.3969/j.issn.2095-4441.2017.02.003
Wang, G. H. (2019). Effects of shenmai injection on acute myocardial infarction and serum hs-CRP and PCT levels. Clin. Res. Chin. 27, 123–124.
Wang, G. Y., Yang, H. X., Wang, X. H., Ma, Y., Mei, X. Y., and Wu, H. X. (2023). Research approaches and methods of basic theory of traditional Chinese medicine. China J. Tradit. Chin. Med. Pharm. Chin. 38, 691–694.
Wang, H., Liu, J. S., and Xu, S. X. (2017). Myocardial and microvascular protection by shenmai injection after percutaneous coronary intervention in patients with acute myocardial infarction. Mod. J. Integr. Tradit. Chin. West. Med. Chin. 26, 1201–1203. doi:10.3969/j.issn.1008-8849.2017.11.019
Wang, H. Y., Zhang, F. C., Zhang, L. M., Li, T. T., and Zhang, M. L. (2018a). Effect of recombinant human brain natriuretic peptide combined with Shenfu injection in the treatment of acute myocardial infarction complicated with acute heart failure. J. Bengbu Med. Coll. Chin. 43, 59–64. doi:10.13898/j.cnki.issn.1000-2200.2018.01.018
Wang, J. (2016). Effects of shenmai injection combined with rehabilitation training on cardiac function and left ventricular remodeling in patients with acute myocardial infarction and its mechanism. J. Tradit. Chin. Med. Univ. Hunan Chin. 36, 498–499.
Wang, J., Lin, F., Zeng, M., Liu, M., Zheng, M., Ren, Y., et al. (2024b). Intraoperative blood pressure and cardiac complications after aneurysmal subarachnoid hemorrhage: a retrospective cohort study. Int. J. Surg. 110, 965–973. doi:10.1097/JS9.0000000000000928
Wang, J., Wang, T., Yang, B., Chen, Y., Gao, P., Wang, Y., et al. (2024c). Impact of acute silent ischemic lesions on clinical outcomes of carotid revascularization. Int. J. Surg. 110, 974–983. doi:10.1097/JS9.0000000000000925
Wang, J. B., and Huang, Y. T. (2017). Clinical effect of urokinase thrombolysis combined with Shenmai injection in the treatment of acute anterior wall infarction. J. Logist. Univ. Pap. Med. Sci. Chin. 26, 584–586. doi:10.16548/j.2095-3720.2017.07.009
Wang, L. M., Gao, C. J., Xie, L. C., and Gao, B. (2019a). Clinical study on the treatment of acute myocardial infarction with heart failure by Shengmai Injection combined with lyophilized recombinant human brain natriuretic peptide. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. (Chin.) 17, 3553–3556. doi:10.12102/j.issn.1672-1349.2019.22.026
Wang, Q., Yang, X., Song, Y., Sun, X., Li, W., Zhang, L., et al. (2021c). Astragaloside IV-targeting miRNA-1 attenuates lipopolysaccharide-induced cardiac dysfunction in rats through inhibition of apoptosis and autophagy. Life Sci. 275, 119414. doi:10.1016/j.lfs.2021.119414
Wang, R. L., Wang, H. Q., Fan, X. H., Duan, M. X., Li, H. Y., and Wang, S. F. (2020). Analysis of chemical constituents in shenmai injection by LC-Q-TOF-MS and LC-IT-MS. Chin. J. Chin. Mater. Med. Chin. 45, 555–564. doi:10.19540/j.cnki.cjcmm.20191002.308
Wang, S., Ye, L., and Wang, L. (2019c). Protective mechanism of shenmai on myocardial ischemia-reperfusion through the energy metabolism pathway. Am. J. Transl. Res. 11, 4046–4062.
Wang, S. M., Yang, L. F., and Wang, L. H. (2022). Traditional Chinese medicine enhances myocardial metabolism during heart failure. Biomed. Pharmacother. 146, 112538. doi:10.1016/j.biopha.2021.112538
Wang, X., Miao, H., Yan, Y., Guo, R., Gong, W., He, Y., et al. (2021b). Effect of shenfu injection on reperfusion injury in patients undergoing primary percutaneous coronary intervention for st segment elevation myocardial infarction: a pilot randomized clinical trial. Front. Cardiovasc Med. 8, 736526. doi:10.3389/fcvm.2021.736526
Wang, X., Wang, Y., Feng, X., Lu, Y., Zhang, Y., Wang, W., et al. (2016). Systematic review and meta-analysis of randomized controlled trials on Wenxin Keli. Drug Des. Devel Ther. 10, 3725–3736. doi:10.2147/DDDT.S112333
Wang, X., Wu, Y., Shen, L., Guo, Z. Q., Wang, X. F., Cui, X. Y., et al. (2010). Clinical study of prevention and treatment for reperfusion injury with Shengmai injection after acute myocardial infarction PCI. Mod. J. Integr. Tradit. Chin. West. Med. Chin. 19, 3553–3554. doi:10.3969/j.issn.1008-8849.2010.28.002
Wang, X. F. (2008). Clinical study on the prevention and treatment of reperfusion injury after acute myocardial infarction intervention with Shengmai injection. Bachelor’s degree. Beijing (China): Beijing University of Chinese Medicine.
Wang, X. Y., Liu, D. J., and Yin, Q. L. (2019b). Efficacy of shenmai injection in acute myocardial infarction and its effect on BNP, cTnT and cardiac function of patients. J. Med. Theory Pract. (Chin.) 32, 3443–3444. doi:10.19381/j.issn.1001-7585.2019.21.016
Wang, Y., Zhao, Y., Jiang, W., Zhao, X., Fan, G., Zhang, H., et al. (2018b). iTRAQ-based proteomic analysis reveals recovery of impaired mitochondrial function in ischemic myocardium by shenmai formula. J. Proteome Res. 17, 794–803. doi:10.1021/acs.jproteome.7b00450
Wang, Y. T. (2018). Recent efficacy and safety of recombinant human brain natriuretic peptide combined with shenfu injection in the treatment of acute myocardial infarction with heart failure. World J. Integr. Tradit. West. Med. Chin. 13, 108–111. doi:10.13935/j.cnki.sjzx.180130
Wang, Z. (2017). Exploration of the clinical value of Shengmai injection combined with alteplase in the treatment of acute myocardial infarction. J. Med. Theory Pract. Chin. 30, 193–194. doi:10.19381/j.issn.1001-7585.2017.02.015
Wang, Z., Ju, J. Q., and Li, Y. L. (2015). Systematic evaluation of the effect of shenmai injection on acute myocardial infarction morbidity and mortality and sequential analysis of the trial. Chin. J. Exp. Tradit. Med. Formulae Chin. 21, 189–193. doi:10.13422/j.cnki.syfjx.2015190189
Wei, D. X., and Liu, M. (2001). Treatment of acute myocardial infarction with intravenous thrombolysis plus intravenous shenmai injection. Chin. J. Inf. Tradit. Chin. Med. Chin., 45–46.
Wei, J. J., Li, B., Zhu, M. J., Wang, Y. X., and Yu, R. (2021). Meta-analysis and trial sequential analysis of Shenmai Injection in the treatment of heart failure after acute myocardial infarction. Chin. J. Hosp. Pharm. Chin. 41, 2082–2090. doi:10.13286/j.1001-5213.2021.20.08
Wen, B. C. (2014). The efficacy of shenfu injections in combination with r-TPA intravenous thrombolysis in the treatment of acute myocardial infarction. Int. Med. Health Guid. News Chin. 20, 1738–1740. doi:10.3760/cma.j.issn.1007-1245.2014.12.033
Wu, M. X., and Li, Y. X. (1988). A case of ventricular arrhythmia and neck edema caused by intravenous danshen injection. J. Henan Univ. Chin. 356.
Wu, R. M., Jiang, B., Li, H., Bang, W. Z., Bao, W. L., Li, H. D., et al. (2020). A network pharmacology approach to discover action mechanisms of Yangxinshi Tablet for improving energy metabolism in chronic ischemic heart failure. J. Ethnopharmacol. 246, 112227. doi:10.1016/j.jep.2019.112227
Wu, Y. F., Chen, J. Q., and Liang, H. T. (2022). Effect of shenmai injection combined with ritongli in the treatment of acute myocardial infarction and its effect on patients' cardiac function and serum inflammatory factor. J. N. Pharm. Chin. 19, 64–66. doi:10.3969/j.issn.1672-8351.2022.05.020
Wu, Z. R., Qi, Y. W., and Li, H. Q. (2016). Effect of shenmai injection combined with ritongli on serum IL-6, TNF-α, and CRP in patients with acute ST-segment elevation myocardial infarction. Shaanxi J. Tradit. Chin. Med. Chin. 37, 29–30. doi:10.3969/j.issn.1000-7369.2016.01.015
Xian, W. (2019). Influence of recombinant human BNP combined Astragalus injection on heart function and serum levels of inflammatory factors in AMI patients with post-PCI heart failure. Chin. J. Cardiovasc. Rehabilit. Med. Chin. 28, 424–428. doi:10.3969/j.issn.1008-0074.2019.04.09
Xie, H. (2018). Effect of shenmai injection with thrombolytic therapy on AMI: impact on ventricular function, level of CRP, BNP, and IL -6. World J. Integr. Tradit. West. Med. Inf. Tradit. Chin. Med. Chin. 35, 94–97. doi:10.19656/j.cnki.1002-2406.180027
Xu, K. (2022). Clinical efficacy of Sheng Vein Injection after emergency PCI in patients with acute myocardial infarction. Bachelor’s degree. Qingdao (China): Qingdao University.
Xu, X. J. (2018). Clinical effect of shenmai injection combined with clopidogrel in the treatment of acute myocardial infarction and the effect on cardiac function. J. Guangxi Med. Univ. Chin. 35, 255–257. doi:10.16190/j.cnki.45-1211/r.2018.02.031
Xuan, J. J., Gao, C. X., Guan, H. M., Jie, J. H., Chen, Y. S., Luo, M. H., et al. (2015). Long-term clinical efficacy of shenmai injection in the treatment of patients with heart failure after acute myocardial infarction. Chin. Tradit. Pat. Med. Chin. 37, 465–467. doi:10.3969/j.issn.1001-1528.2015.02.054
Yan, H., Hu, Z. Q., and Xu, G. (2017). Effect of shenfu injection on left ventricular remodeling and cardiac function in patients with early acute myocardial infarction. Mod. J. Integr. Tradit. Chin. West. Med. Chin. 26, 52–54. doi:10.3969/j.issn.1008-8849.2017.01.017
Yan, J., Cheng, M. Y., Duan, Y., Wang, Z. R., Feng, H., and Xie, B. (2018). A clinical study on shenmai injection combined with batroxobin in the treatment of acute myocardial infarction. Prog. Mod. Biomed. Chin. 18, 4294–4297. doi:10.13241/j.cnki.pmb.2018.22.021
Yan, P. (2018). Protective effect on myocardial injury after thrombolytic therapy of acute ST-segment elevation myocardial infarction assisted by shenmai injection. Mod. J. Integr. Tradit. Chin. West. Med. Chin. 27, 2788–2791.
Yang, F. F., Xing, Y. B., Guo, H. Y., Peng, F., Qiu, Y. F., Yuan, M., et al. (2017b). The intervention effect of Shenmai injection on endothelial dysfunction and apoptosis factors in non-ST elevation acute myocardial infarction. Zhejiang J. Tradit. Chin. Med. Chin. 5, 68–69. doi:10.3969/j.issn.0411-8421.2017.01.049
Yang, H. Y., Liu, M. L., Luo, P., Yao, X. S., and Zhou, H. (2022). Network pharmacology provides a systematic approach to understanding the treatment of ischemic heart diseases with traditional Chinese medicine. Phytomedicine 104, 154268. doi:10.1016/j.phymed.2022.154268
Yang, J. W., Hong, J. N., Fang, J., Xue, F., Ceng, X. P., and Jin, W. X. (2017a). Effect of shenmai injection combined with revascularization on cardiac function in patients with acute myocardial infarction complicated with heart failure. Mod. Diagn. and Treat. (Chin.) 28, 3346–3347. doi:10.3969/j.issn.1001-8174.2017.18.008
Yang, M. N., and Wang, P. P. (2021). Effect of Shenmai injection combined with levocarnitine on cardiac function and myocardial microcirculation in patients with ischemic cardiomyopathy and heart failure. Clin. Res. Pract. Chin. 6, 140–142. doi:10.19347/j.cnki.2096-1413.202115047
Yang, S. Q. (2014). Effect of shenfu injection on ultrasound cardiogram in patients of acute myocardial infarction combined with pump failure. Chin. J. Postgrad. Med. Chin. 37, 56–58. doi:10.3760/cma.j.issn.1673-4904.2014.19.020
Yang, X. Z., Zheng, Y., Guo, S. Q., Li, J. J., and Shang, S. Z. (2014). Clinical observation on intracoronary injection with shenmai injection and western medicine for No-reflow after percutaneous coronary intervention in patients with acute myocardial infarction. J. Tradit. Chin. Med. Chin. 55, 854–857. doi:10.13288/j.11-2166/r.2014.10.013
Yang, Y., Li, X., Chen, G., Xian, Y., Zhang, H., Wu, Y., et al. (2023). Traditional Chinese medicine compound (Tongxinluo) and clinical outcomes of patients with acute myocardial infarction: the CTS-AMI randomized clinical trial. JAMA 330, 1534–1545. doi:10.1001/jama.2023.19524
Yang, Z. Q., and Cai, L. L. (2016). Effects of Sheng Mai Injection on blood rheology and cardiac pump function in patients with myocardial infarction complicated with cardiac shock. J. Clin. Emerg. Chin. 17, 948–951. doi:10.13201/j.issn.1009-5918.2016.12.015
Ye, D. J. (2010). Effect of Shen Mai injection to prognosis and hemorheology on acute myocardial infarction. Nei Mong. J. Tradit. Chin. Med. Chin. 29, 1–02. doi:10.16040/j.cnki.cn15-1101.2010.16.023
You, S., and Wang, Y. M. (2019). Effects of Shenfu injection on hemorheology and neuroendocrine hormones in the treatment of acute myocardial infarction with acute heart failure. Acta Med. Sin. Chin. 32, 53–57. doi:10.19296/j.cnki.1008-2409.2019-01-015
Yu, H., Hu, Q., Sun, J., Feng, R., Zhang, S., Zhang, J. X., et al. (2019a). Analysis of chemical constituents in Astragalus injection based on ultra performance liquid chromatography-quadrupole-time of flight mass spectrometry. World Chin. Med. Chin. 14, 809–817. doi:10.3969/j.issn.1673-7202.2019.04.005
Yu, H. B., Yu, X. W., and Wu, N. B. (2010). Adjuvant therapeutic effect of shenmai injection in non-ST-segment elevation acute myocardial infarction. Clin. J. Tradit. Chin. Med. Chin. 22, 133–134. doi:10.16448/j.cjtcm.2010.02.035
Yu, S., Guo, Y. Y., Cao, J. W., and Zhai, X. F. (2023). Analysis of adverse reaction characteristics of Huoxue Huayu traditional Chinese medicine injection based on literature research. Chin. J. Clin. Ration. Drug Use Chin. 16, 9–13. doi:10.15887/j.cnki.13-1389/r.2023.10.003
Yu, X. P., Li, P. S., and Chen, K. Q. (2021). Exploration of the efficacy of shenmai injection combined with beta-blockers in the treatment of acute myocardial infarction and the effect on the QTd degree of electrocardiography. Knowl. Cardiovasc. Dis. Prev Treat. (Chin.) 11, 20–22. doi:10.3969/j.issn.1672-3015(x).2021.04.007
Yu, Y., Spatz, E. S., Tan, Q., Liu, S., Lu, Y., Masoudi, F. A., et al. (2019b). Traditional Chinese medicine use in the treatment of acute heart failure in western medicine hospitals in China: analysis from the China PEACE retrospective heart failure study. J. Am. Heart Assoc. 8, e012776. doi:10.1161/JAHA.119.012776
Yuan, X. H. (2009). Therapeutic efficacy of intravenous thrombolysis combined with shenmai injection in the treatment of acute myocardial infarction. Chin. Mod. Med. Chin. 16, 56–59. doi:10.3969/j.issn.1674-4721.2009.10.034
Zang, Y., Wan, J., Zhang, Z., Huang, S., Liu, X., and Zhang, W. (2020). An updated role of astragaloside IV in heart failure. Biomed. Pharmacother. 126, 110012. doi:10.1016/j.biopha.2020.110012
Zeng, Y. L. (2005). Adjuvant treatment of acute myocardial infarction with heart failure in 54 cases with shenfu injection. Chin. Pract. J. Rural. Dr. Chin., 31–32. doi:10.3969/j.issn.1672-7185.2005.01.019
Zhan, D. S., and Cui, X. Y. (2023). Effect of Shenmai Injection combined with Ticagrelor in patients with acute myocardial infarction. Chin. Mod. Med. Chin. 30, 118–121. doi:10.3969/j.issn.1674-4721.2023.32.030
Zhan, S., Fan, X., Zhang, F., Wang, Y., Kang, L., and Li, Z. (2016). Correction: a proteomic study of Shengmai injection's mechanism on preventing cardiac ischemia-reperfusion injury via energy metabolism modulation. Mol. Biosyst. 12, 674–677. doi:10.1039/c5mb90052b
Zhan, Z. A., Yuan, H., Sun, H., Liu, S. T., Zhang, S., Jiang, S., et al. (2024). Effect of shenfu injection of anti-myocardial ischemia-reperfusion injury via modulating HIF-1α/BNIP3 pathway-mediated mitophagy. Chin. J. Integr. Med. Chin. 44, 1086–1093.
Zhang, C., and Niu, S. M. (2018). Analysis and discussion of the adverse drug reactions induced by traditional Chinese medicine injections in 86 cases of patients. Shanghai Med. and Pharm. J. (Chin.) 39, 41–43. doi:10.3969/j.issn.1006-1533.2018.13.014
Zhang, D., and Jia, X. F. (2019). Clinical study on the adjuvant treatment of acute myocardial infarction with shenmai injection. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. (Chin.) 17, 1890–1894. doi:10.12102/j.issn.1672-1349.2019.12.037
Zhang, D. L., Yin, L., Jiang, F., Guo, F., Hao, W. H., Yang, H. J., et al. (2018a). Clinical study on the treatment of acute myocardial infarction combined with cardiogenic shock in the elderly with shenmai injection combined with levosimendan. Mod. J. Integr. Tradit. Chin. West. Med. Chin. 27, 1453–1457. doi:10.3969/j.issn.1008-8849.2018.13
Zhang, D. M., Sun, D. X., Sun, C. L., Du, L. L., Yao, K. J., and Liu, Y. (2018b). Effects of pressurized rapid intravenous infusion of Shenfu on hemodynamics in patients with acute inferior myocardial infarction. J. Hebei Med. Univ. Chin. 39, 882–886. doi:10.3969/j.issn.1007-3205.2018.08.004
Zhang, H., Zhao, Y. H., Xia, Z. X., Du, H. L., Gao, Y., Xue, D., et al. (2018c). Metabolic profiles revealed anti-ischemia-reperfusion injury of Yangxinshi tablet in Rats. J. Ethnopharmacol. 214, 124–133. doi:10.1016/j.jep.2017.09.003
Zhang, H. X. (2011). The efficacy of shenfu injection in the treatment of heart failure after acute myocardial infarction. Chin. J. Ethnomed. Ethnopharm. Chin. 20, 75. doi:10.3969/j.issn.1007-8517.2011.05.055
Zhang, L., Wang, W., and Xie, Y. M. (2023). Effect of Shenfu Injection on polysaccharide inclusion in patients with acute myocardial infarction complicated by hypotension. Drug Eval. Res. Chin. 46, 2408–2414. doi:10.7501/j.issn.1674-6376.2023.11.017
Zhang, M., Chen, K., and Yang, Q. Q. (2011). Effect of shenmai injection on malignant cardiac events and morbidity and mortality in patients with acute massive myocardial infarction. Shandong Med. J. Chin. 51, 92–93. doi:10.3969/j.issn.1002-266X.2011.03.056
Zhang, M. L., Zhang, L. T., Qiu, X. F., and Zhou, A. F. (2001). On the relationship between mitochondria and qi in Chinese medicine. Chin. J. Basic Med. Tradit. Chin. Med. Chin., 60–61. doi:10.3969/j.issn.1006-3250.2001.04.024
Zhang, W. J., Cao, Y., Zhang, Y., Ge, Y., Wang, S., Kang, C. Z., et al. (2021). Current status and prospects of implementing GAP in Chinese medicine injection materials. Chin. J. Chin. Mater. Med. Chin. 46, 5166–5172. doi:10.19540/j.cnki.cjcmm.20210528.601
Zhang, Y. H., Cheng, R. L., Shang, Y. D., Qu, X. Y., Wang, T. T., Lv, X. Y., et al. (2019). Clinical observation on the treatment of acute myocardial infarction combined with heart failure by shenfu injection. J. Emerg. Trad. Chin. Med. Chin. 28, 317–319. doi:10.3969/j.issn.1004-745X.2019.02.037
Zhang, Z. L. (2017). Clinical study on the treatment of acute anterior wall myocardial infarction by intravenous thrombolysis with shenmai injection combined with urokinase. Asia-Pacific Tradit. Med. Chin. 13, 124–125. doi:10.11954/ytctyy.201710055
Zhao, C. H. (2020). Analysis of the effects of shenmai injection combined with clopidogrel on cardiac function and prognosis in patients with acute myocardial infarction. Chin. Remedies and Clin. (Chin.) 20, 566–568. doi:10.11655/zgywylc2020.04.032
Zhao, J., Zhao, Q., and Wu, T. G. (2016a). Evaluation of the efficacy of recombinant human brain natriuretic peptide combined with shenfu in the treatment of acute myocardial infarction with pump failure. Mod. J. Integr. Tradit. Chin. West. Med. Chin. 25, 1413–1416. doi:10.3969/j.issn.1008-8849.2016.13.016
Zhao, L. F., and Sun, F. J. (2021). Effect of coronary artery injection of tirofiban combined with sensitized wheat injection on cardiac function after PCI in patients with acute STEMI. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. (Chin.) 19, 4337–4339. doi:10.12102/j.issn.1672-1349.2021.24.028
Zhao, X. L., Li, J. Y., and Wang, Y. (1995). A case of polymorphic ventricular tachycardia induced by shengmai injection. Chin. J. Cardiol. Chin. 295.
Zhao, X. P., Chen, J., and Guo, S. A. (2005). Research on repurfusion injury after thrombolysis in vein of acute myocardial infarction treated by shenmai injection. J. Pract. Tradit. Chin. Med. Chin., 195–196. doi:10.3969/j.issn.1004-2814.2005.04.001
Zhao, Y., Zhang, Y. G., Wang, H. B., Ren, S. H., Cao, Q. M., Jiang, C. Y., et al. (2016b). One hundred and five cases of related heart failure due to acute myocardial infarction treated with ginseng and Radix ophiopogonis injection. Henan tradit. Chin. Med. Chin. 36, 1730–1732. doi:10.16367/j.issn.1003-5028.2016.10.0700
Zheng, Q., Wang, X. Y., Liu, J., Peng, C., Xiong, L., Zhu, Y. N., et al. (2022). Identification of the chemical constituents of shenfu injection and the anti-inflammatory activity of its acetylenic compounds. China Pharm. Chin. 33, 1931–1936. doi:10.6039/j.issn.1001-0408.2022.16.03
Zheng, Y. (2016). Clinical effect analysis of shenmai injection in the treatment of patients with heart failure after acute myocardial infarction. Chin. J. Mod. Drug Appl. Chin. 10, 171–172. doi:10.14164/j.cnki.cn11-5581/r.2016.08.132
Zhou, J. Y., Liu, Y. C., and Guo, D. C. (2019). Effect of Astragalus injection on the improvement of cardiac function and vascular endothelial function in patients with acute myocardial infarction. Chin. J. Pharm. Biotechnol. Chin. 26, 236–239. doi:10.19526/j.cnki.1005-8915.20190310
Zhou, R. S. (2017). Evaluation of the effect and safety of shenmai injection combined with thrombolytic drugs in the treatment of acute ST-segment elevation myocardial infarction. J. China Prescr. Drug (Chin.) 15, 77–78.
Zhou, S. J. (2024). The effect of sensitized wheat injection combined with tegretol in patients with acute myocardial infarction. Pract. Clin. J. Integr. Tradit. Chin. West. Med. (Chin.) 24, 95–97. doi:10.13638/j.issn.1671-4040.2024.02.028
Zhu, C. Z., Wang, X. H., Liu, X., Xue, J. H., Zhao, L., Song, Y. F., et al. (2019). The efficacy of shenfu injection combined with aspirin and clopidogrel in the treatment of acute myocardial infarction. Eval. Anal. Drug-Use Hosp. China (Chin) 19, 950–952. doi:10.14009/j.issn.1672-2124.2019.08.015
Zhu, G. J. (2006). Clinical study on the myocardial protective effect of ginseng and auxiliary injection on patients with acute myocardial infarction. Chin. Med. Theory Pract. (Chin.) 16, 827–828.
Zhu, X. H., Ye, H. F., and Yang, L. (2020). Effect of shenfu injection on myocardial TIMI flow grading during PCI in patients with acute myocardial infarction and major adverse cardiac events in the immediate postoperative period. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. (Chin.) 18, 2107–2111. doi:10.12102/j.issn.1672-1349.2020.13.023
Zhu, Y. H., Shen, X. X., Han, Q. Q., and Zhao, J. (2018). Meta-analysis of the clinical efficacy of shenfu injection in the treatment of myocardial infarction with heart failure. Chin. J. Evid.-Bases Cardiovasc. Med. Chin. 10, 402–406. doi:10.3969/j.issn.1674-4055.2018.04.04
Zhuo, D. Q., Min, L., Zhang, D. Y., and Ren, W. Q. (2018). Observation of the hemodynamic intervention effect of Shenfu injection on patients with acute myocardial infarction and cardiogenic shock. Chin. J. Tradit. Med. Sci. Technol. Chin. 25, 381–382.
Zong, X. L., Du, A. F., and Zhao, L. M. (2014). Clinical analysis of ginseng injection with urokinase thrombolysis therapy in anterior wall acute myocardial infarction. Hainan Med. J. Chin. 25, 2822–2824. doi:10.3969/j.issn.1003-6350.2014.19.1112
Keywords: Chinese medicine injections, acute myocardial infarction, meta-analysis, traditional Chinese medicine, energy metabolism
Citation: Zhou H, Chen J, Liu H, Li X, Zong H, Zhang S, Shi Y and Li Y (2025) Traditional Chinese medicine injections with Tonifying Qi, equivalent effect of regulating energy metabolism, for acute myocardial infarction: a systematic review and meta-analysis of randomized clinical trials. Front. Pharmacol. 16:1511486. doi: 10.3389/fphar.2025.1511486
Received: 15 October 2024; Accepted: 10 March 2025;
Published: 28 March 2025.
Edited by:
Chen Huei Leo, National University of Singapore, SingaporeReviewed by:
Yuxiang Fei, China Pharmaceutical University, ChinaCopyright © 2025 Zhou, Chen, Liu, Li, Zong, Zhang, Shi and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongxu Liu, bGh4X0AyNjMubmV0; Xiang Li, bGl4aWFuZzExODk3QGJqemhvbmd5aS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.