- 1The First Clinical Medical College, Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
- 2Science and Technology Innovation Center, Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
- 3The Basic Medicine College, Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
- 4Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine, Nanchang, Jiangxi, China
- 5Department of Gynecology, The First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
Objective: To systematically evaluate the differences in the efficacy of commonly used topical commercial Chinese polyherbal preparations (CCPPs) for vulvovaginal candidiasis (VVC), and to provide evidence-based reference for clinical drug regimens.
Methods: Computer searched major Chinese and English literature databases, and collected randomized controlled trials (RCTs) of external use of CCPPs combined with conventional treatment (CT, test group) versus CT alone (control group) in patients with VVC. After screening the literature, the quality of the included studies was assessed using the risk of bias assessment tool recommended in 5.3 of the Cochrane Handbook. Outcome data for each outcome measure were extracted and a network meta-analysis was performed using Stata 15.0.
Results: A total of 74 RCTs with a total of 8,151 patients were included, nine interventions were involved. The results of network meta-analysis showed that, Fufang Shajiziyou suppository combined with CT was more effective in improving the negative conversion rate and controlling the recurrence rate of Candida albicans. Kangfu gel combined with CT had the better effect in relieving pruritus. Baofukang suppository combined with CT was the most effective in reducing leukorrhea. Fufukang spray combined with CT had fewer adverse reactions.
Conclusion: The addition of CCPPs to CT may acquire a better curative effect in patients with VVC and external does not significantly increase the occurrence of adverse reactions. However, due to the low quality of the included literature, larger-scale, higher-quality clinical studies are still needed.
Systematic Review Registration: PROSPERO, NO: CRD42023410244.
1 Introduction
Vulvovaginal candidiasis (VVC) is a prevalent inflammatory gynecologic dermatomycosis resulting from an overgrowth of Candida albicans (C. albicans), characterized by a high occurrence and recurrence rate (Saxon Lead Author et al., 2020). Studies indicate that 75% of women will experience at least one episode of VVC in their lifetime, and 40%–50% experiencing multiple episodes (Yano et al., 2019; Sun et al., 2023). Clinical manifestations of VVC include abnormal itching of the vulva and vagina, increased thick leukorrhea resembling tofu curds, and superficial pain during sexual intercourse and so on, all of which significantly impact the quality of life and reproductive health of patients. Current treatment primarily involves oral or intra-vaginal anti-fungal drugs, or through nebulization with ozone insufflation, etc (Denison et al., 2020; Sanjaya et al., 2023). However, these treatments may lead to recurrence of symptoms after cessation and potential side effects such as drug resistance, liver and kidney damage, respiratory irritation, memory loss, or other allergic reactions. Therefore, the need for improved treatment options remains (Satora et al., 2023). Therefore, exploring a better treatment is still the focus of clinical research.
VVC belongs to the category of “vulval pruritus” or “leukorrhagia” based on the theoretical principles of traditional Chinese medicine (TCM), which believes that the core pathogenesis of VVC is dampness-heat in lower jiao, and the therapeutic principle often involves clearing heat and expelling dampness, killing worms and relieving itching (Yang et al., 2018; Feng et al., 2024), the external application of TCM is one of the important treatment methods. As one of the modern TCM preparations, topical commercial Chinese polyherbal preparations (CCPPs) is more stable, easy to store and use, and has been shown in numerous clinical studies to be effective in reducing itching, improving the negative conversion rate and decreasing the recurrence rate of C. albicans (Lijuan et al., 2022). Basic studies have further confirmed the effectiveness, such as the study found that Baofukang suppository (BFKS) can effectively inhibit the adhesion, mycelial formation, and proliferation of C. albicans, restore the morphology and vitality of vaginal epithelial cells, and enhance local immune function (Li et al., 2016). Nevertheless, CCPPs available on the market is booming and there is a lack of research on their relative effectiveness, which is not conducive to their further popularization and application.
Network meta-analysis (NMA) enables simultaneous comparison of three or more interventions for the same disease, offering valuable insights by combining direct comparisons and indirect comparisons and ranking intervention effectiveness, especially when direct comparative studies are insufficient or lacking (Yang et al., 2023). Widely applied in medical research, NMA helped Zhang et al. find Zhibitai capsule as the most effective choice of CCPPs for non-alcoholic fatty liver disease (Zhang et al., 2022). Similarly, Huang et al. found the combination of Shensong Yangxin capsule with Western medicine is presumably the optimal treatment prescription for stable angina through NMA (Huang et al., 2022). Based on these, the study aimed to compare the effectiveness and safety of commonly used topical CCPPs combined with conventional treatment (CT) in treating VVC through NMA to provide evidence for clinical drug use.
2 Methods
The study was registered in the International Systematic Review Prospective Register (PROSPERO, NO: CRD42023410244) and carried out according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews and meta-analyses (Page et al., 2021).
2.1 Inclusion criteria
The Population-Intervention-Comparators-Outcomes-Study design (PICOS) framework was used as the criterion for this study.
2.1.1 Selection of studies
Publicly published randomized controlled trials (RCTs) with no restrictions on allocation concealment and blinding were included. Language was restricted to Chinese and English.
2.1.2 Study populations
Patients diagnosed with VVC, characterized by symptoms such as vulvovaginal pruritus and curd-like vaginal secretions, and confirmed through the detection of fungal spores or mycelium in the secretions, were included in the study (Nyirjesy et al., 2022), and There were no restrictions regarding age, occupation, race, time of onset, or duration of disease.
2.1.3 Intervention measures
The patients in both groups (control group and test group) were given CT, such as oral or intra-vaginal anti-fungal drugs (clotrimazole preparations, miconazole preparations, nystatin preparations,etc.), 5% sodium bicarbonate solution (vulvar wash) or lacidophilin vaginal capsule. Based on a comprehensive literature review and practical clinical application, the test group was treated with one of eight common topical CCPP, including BFKS, Fufang Shajiziyou suppository (FFSJZYS), Kushen gel (KSG), Kangfu gel (KFG), Fufukang spray (FFKS), Honghe Fujie lotion (HHFJL), Bai’an lotion (BAL) and Jieeryin lotion (JEYL) in addition to the control group’s treatment. The dose and course of treatment were not limited for both groups. Composition, extract and extraction process and more information of PPCCs are shown (Supplementary Tables S1–S3).
2.2 Outcomes
1) The negative conversion rate of C. albicans; 2) the recurrence rate of C. albicans; 3) time to resolution of pruritus; 4) time to resolution of secretion; 5) incidence of adverse reactions.
2.3 Exclusion criteria
Articles meeting the following criteria were excluded: non-clinical trials, such as reviews, cell experiments and animal modeling experiments, conference reports, empirical summaries, dissertation, treatment guidelines, etc.; relevant outcome indicators were not provided; the full text could not be obtained; the test group only used CCPPs; the clinical data were incomplete and the request for the data from the original author was fruitless; patients with bacterial or trichomoniasis infection; repeatedly published articles, non-Chinese and English literature.
2.4 Search strategy
PubMed, CNKI, Wanfang Data, VIP, CBM, Web of science, Cochrane Library and Embase database were searched by computer (Song et al., 2024). According to the characteristics of different databases, MeSH terms, free words and keywords were used for retrieval, and the language of the literature was limited to Chinese and English. The retrieval time was from the inception of each database to February 2024. The search strategy’s complete details are displayed (Supplementary Tables S4–S11).
2.5 Data extraction
When screening the literature, the two researchers independently read the titles and abstracts of the articles for primary selection and deduplication, and then read the full text for deciding whether to include or not according to the inclusion and exclusion criteria strictly (Wu et al., 2022). If there is a difference between the two ideas, disagreements were resolved by discussion first or, if necessary, a third-party opinion was consulted to reduce the selection bias. All data were independently extracted through standard tables, including: 1) basic information of the included studies (the first author and year of publication); 2) basic information of the research subjects (sample size and age); 3) intervention measures; 4) course of treatment; 5) outcome indicators (negative conversion rate, recurrence rate, time to improve itching, time to reducing secretion, and occurrence of adverse effects); 6) quality assessment and methodological information of the articles.
2.6 Handling of missing data
If data was missing or incomplete, calculated it if possible; for instance, if the data was presented in graphical form, the data could be extracted using GetData software. If calculation failed, contacted the first or corresponding author. Excluded the data from analysis if it remains unavailable.
2.7 Risk of bias assessment
The quality of the included RCT was assessed using the quality assessment methods recommended in the Cochrane Handbook for Systematic Evaluators 5.3 (Higgins et al., 2011), which include the following seven items: 1) generation of the randomized sequence; 2) allocation concealment; 3) blinding of participants and personnel; 4) blinding of outcome measures; 5) completeness of data on outcome indicators; 6) selective reporting; 7) other bias. For the included articles, each item was judged as “Yes” (low risk), “No” (high risk), or “Unclear” (unclear risk). Methodological quality was assessed independently by two reviewers, and in case of disagreement, a third-party opinion was reached.
2.8 Statistical analysis
Data were statistically analyzed and graphically presented using Stata15.0 software (Shim et al., 2017), and continuous variables were expressed by standardized mean difference (SMD) and 95% confidence interval (CI), and dichotomous variables were expressed by odds ratio (OR) and 95% CI. Heterogeneity test used I2 to test the magnitude of heterogeneity among the studies, if I2 ≤ 50%, it was considered that there was no statistical heterogeneity among the included studies, and the fixed-effects model was used for meta-analysis; if I2 > 50%, it was suggestive of the existence of heterogeneity among the studies, and the random-effects model was selected for meta-analysis. In outcomes with significant heterogeneity, subgroup analyses were performed to identify potential sources of heterogeneity. Descriptive analyses were used when the source of heterogeneity could not be determined.
If there was a closed loop in a network, the consistency between direct and indirect comparisons was first compared using the node-split model, with P > 0.05 indicating good consistency, and the consistency model was employed for analysis, while the inconsistency model was utilized for the converse scenario. In studies where node-split nodes were not produced, the consistency model was first applied for analysis. The cumulative ranking probability of each therapy was determined through the calculation of the surface under the cumulative ranking curve area (SUCRA), with higher SUCRA values indicating superior intervention efficacy. Comparison-corrected funnel plots were drawn with Stata 15.0 to determine whether there was publication bias or small sample effects. Sensitivity analysis was used to evaluate the stability of meta-analysis results.
3 Results
3.1 Literature retrieval and basic information
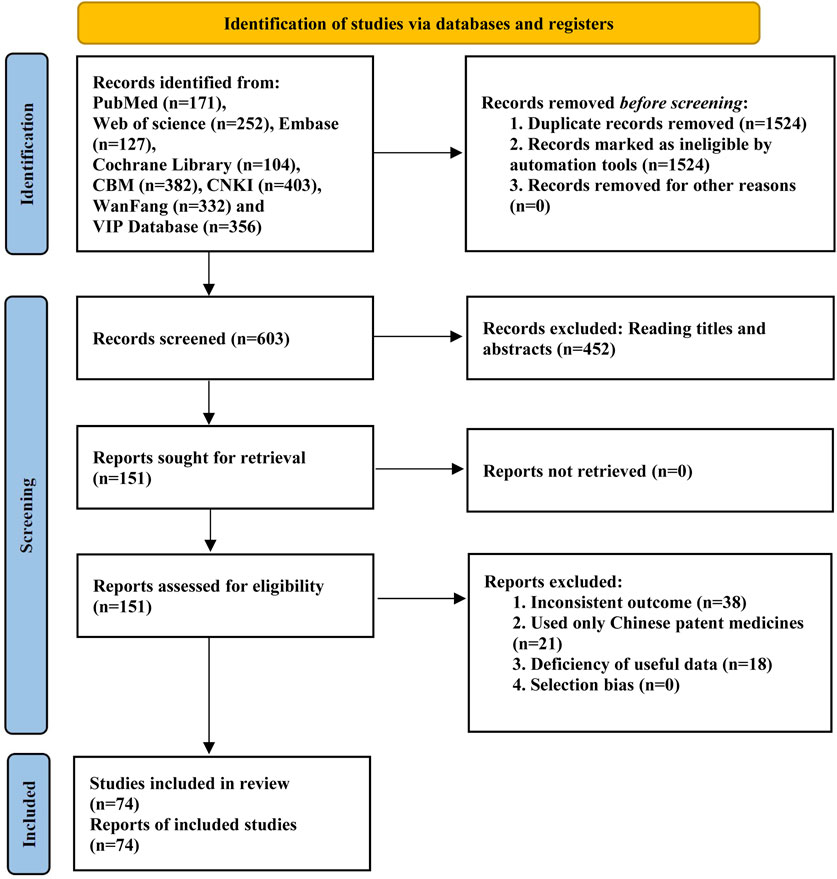
After the reading of the title, abstract and full text, a total of 74 RCTs were finally included (Wang, 2005; Song, 2011; Yang G., 2011; Yang R., 2011; Huang, 2012; Zhang, 2013; Lei, 2014; Wang He et al., 2015; Wang Namei et al., 2015; Sun and Fang, 2015; Wang and Hu, 2016; Song, 2016; Wang, 2016; Zhang et al., 2016; Alimu, 2017; Chen, 2017; Gong, 2017; Chen et al., 2017; Guo, 2017; Hao, 2017; Huang, 2017; Li C., 2017; Li Y., 2017; Sang, 2017; Wen, 2017; Yu, 2017; Cao, 2018; Hu and Liu, 2018; Hua and Dai, 2018; Cang et al., 2018; Wang J., 2018; Wang L., 2018; Zhao, 2018; Ban, 2019; Zhang, 2019; Deng, 2020; Lei, 2020; Li, 2020; Shang and Shang, 2020; Shi and Zhang, 2020; Wang, 2020; Liu and Feng, 2020; Xu, 2020; Zhang, 2020; Dong et al., 2021; Lei and Yang, 2021; Quan and Huang, 2021; Wan and Hu, 2021; Yang, 2021; Yin, 2021; Zeng, 2021; Chunyang and Song, 2022; Hu, 2022; Tong and Zhang, 2022; Li, 2022; Ma and Xu, 2022; Ma, 2022; Wang et al., 2022; Xiong, 2022; Xu, 2022; Xue, 2022; Yang, 2022; Yuqing and Yu, 2022; Zhao, 2022; Ji, 2023; Jia, 2023; Feng et al., 2023; Liu et al., 2023; Xiao and Chen, 2023; Xu, 2023; Xiao and Chen, 2023; Yu, 2023; Zeng, 2023; Zhang, 2023). The literature screening process is shown in Figure 1, and the basic information of the included studies is shown in Table 1.
A total of 8,151 patients were involved: KSG (26 RCTs), HHFJL (17 RCTs), 26 BFKS (15 RCTs), KFG (4 RCTs), FFKS (4 RCTs), BAL (3 RCTs), FFSJZYS (3 RCTs), JEYL (2 RCTs). The number of sample sizes in the included literature ranges from 20 to 210, with an average of 55. The range of age is from 23 to 51, with a mean age of 34. The course of treatment ranges from 6 d to 30d, and around 7d or 14d for most studies.
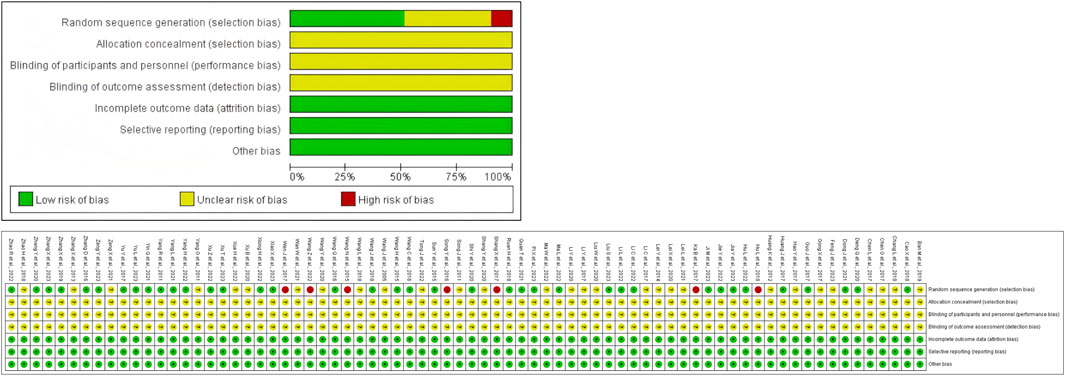
3.2 Quality evaluation of the included articles
All studies were RCTs, of which 35 used random number table; three used random drawing; seven used the order of participation, the remaining studies only mentioned randomization. None of the studies mentioned blinding and allocation concealment. All studies had complete data. The risk of bias assessment of the included studies is shown in Figure 2.
3.3 Negative conversion rate of C. albicans
A total of 68 RCTs reported negative conversion rate of C. albicans, all nine interventions were involved. It was found that the overall I2 between the two-arm studies was 0.0%, indicating that the heterogeneity was small, and thus the fixed-effects model was used for NMA. As shown in Figure 3A, the larger the circle in the graph, the more patients in this measure; the thicker the line, the more studies in which directly the two interventions were directly compared. The results of NMA (Figure 3B) showed that compared with CT, CT combined with JEYL (OR = 0.73, 95% CI [-0.41, 1.87]) and FFKS (OR = 0.40, 95% CI [-0.07, 0.88]) could not significantly improve the conversion rate, but the rest of the test groups could significantly improve the negative conversion rate (P < 0.05). The analysis among test groups showed that compared with CT combined with FFKS, CT combined with FFSJZYS, BFKS, KSG, HHFJL, KFG or BAL could significantly improve the negative conversion rate (P < 0.05). The ranking results of each intervention measure were shown in Figure 3C. The percentage represented the surface under the cumulative ranking curve (SUCRA). The larger the area, the higher the efficiency. The results showed that the ranking of the nine interventions in improving the negative conversion rate was FFSJZYS + CT > HHFJL + CT > KFG + CT > KSG + CT > BAL + CT > BFKS + CT > JEYL + CT > FFKS + CT > CT.
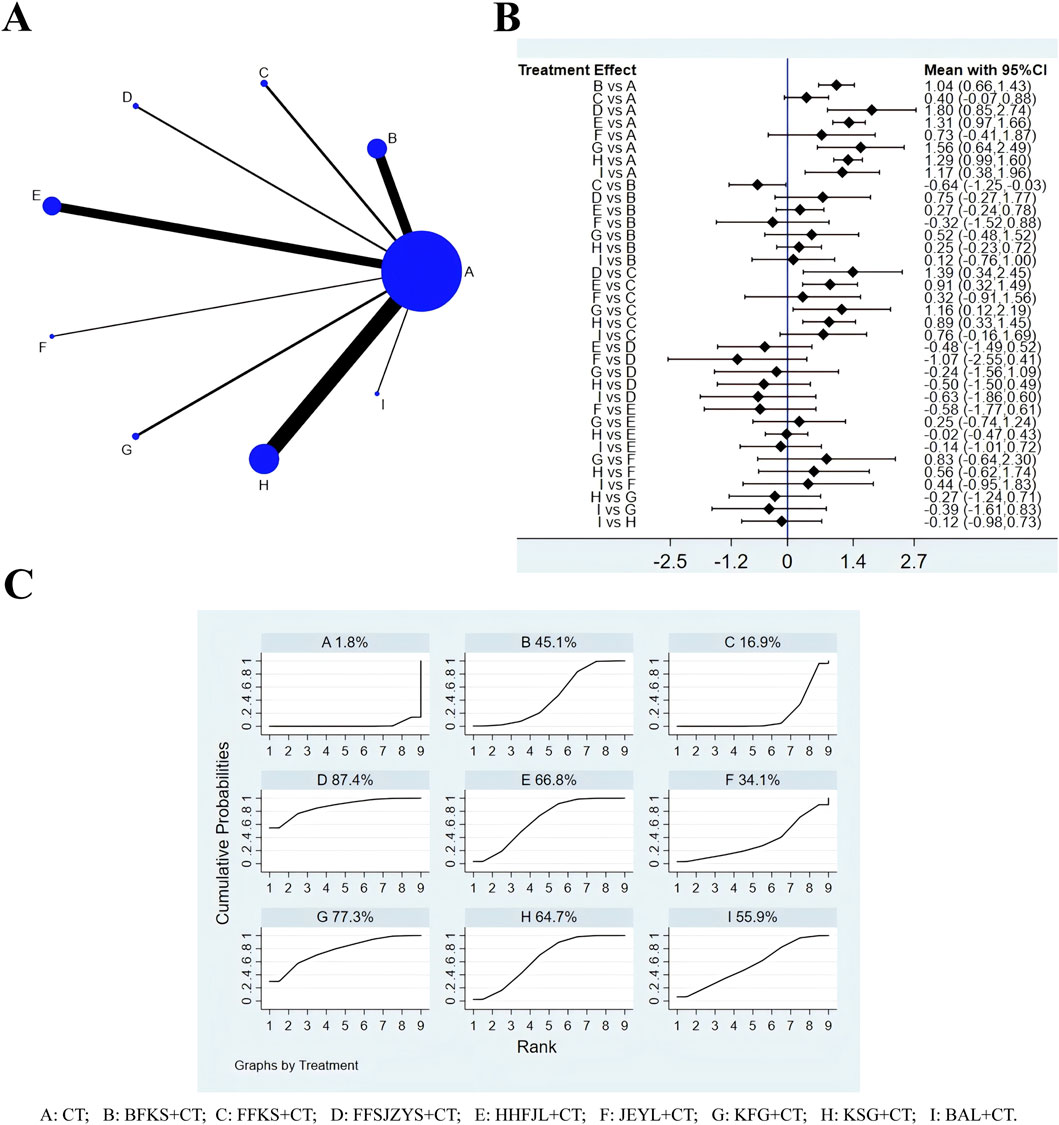
Figure 3. Evidence relationship (A), forest plot (B) and SUCRA (C) of negative conversion rate of C. albicans. CT, conventional treatment; BFKS, Baofukang suppository; FFKS, Fufukang spray; FFSJZYS, Fufang Shajiziyou suppository; HHFJL, Honghe Fujie lotion; JEYL, Jieeryin lotion; KFG, Kangfu gel; KSG, Kushen gel; BAL, Bai’an lotion.
3.4 Recurrence rate of C. albicans
According to the evidence network (Figure 4A), a total of 42 studies reported recurrence rates, excluding FFKS, the remaining eight intervention measures were involved. Because the overall I2 between the two-arm studies was 0.0%, the fixed-effects model was used for NMA. The results of NMA (Figure 4B) showed that compared with CT, CT combined with JEYL (OR = −1.21, 95% CI [-2.88, 0.46]) could not significantly reduce the recurrence rate (P > 0.05), but the other test groups were significantly different from the CT groups (P < 0.05). Comparisons were made between the test groups, there was no significant difference. The SUCRA probability ranking of eight interventions (Figure 4C) in reducing the recurrence rate was FFSJZYS + CT > KFG + CT > BAL + CT > KSG + CT > BFKS + CT > JEYL + CT > HHFJL + CT > CT.
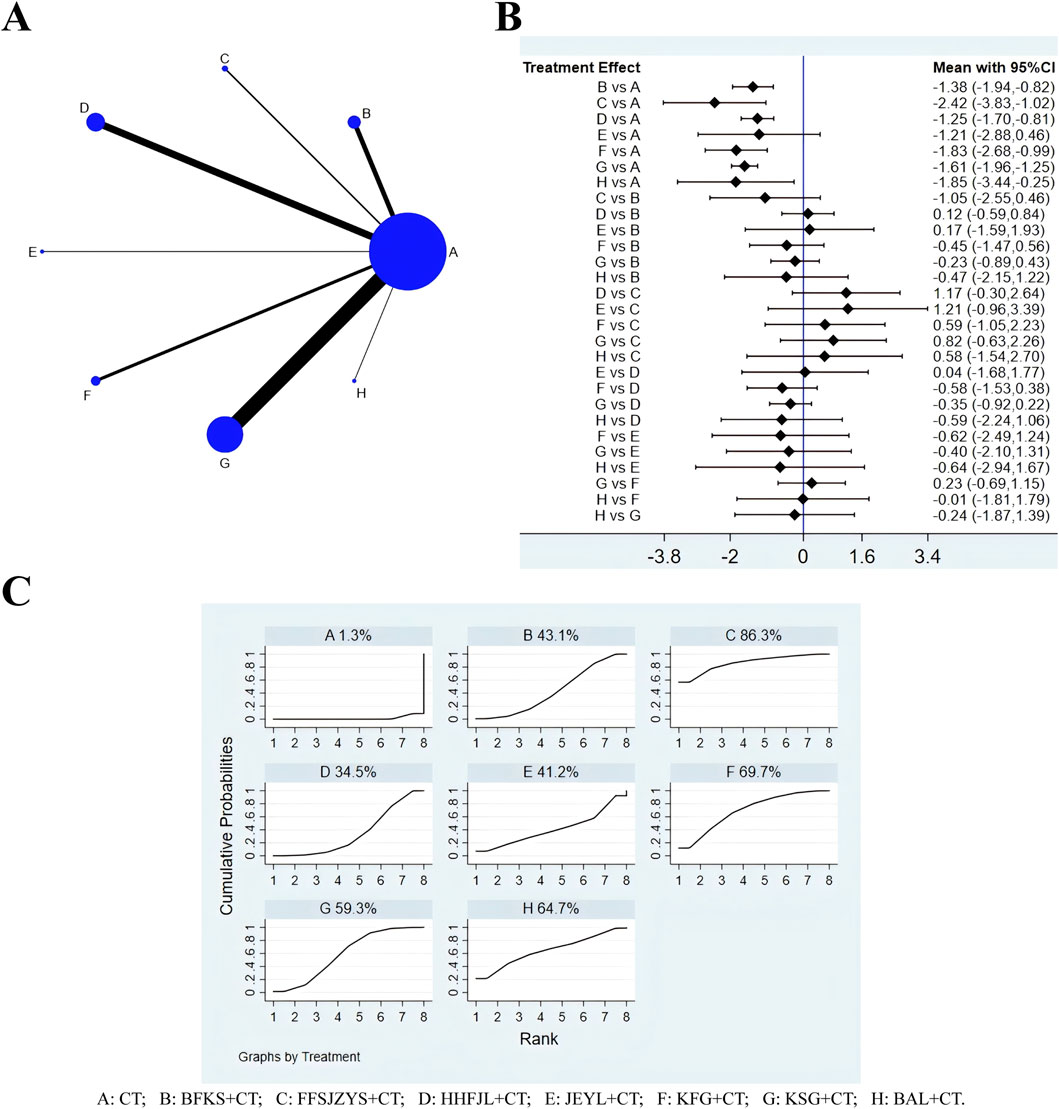
Figure 4. Evidence relationship (A), forest plot (B) and SUCRA (C) of recurrence rate. CT, conventional treatment; BFKS, Baofukang suppository; FFSJZYS, Fufang Shajiziyou suppository; HHFJL, Honghe Fujie lotion; JEYL, Jieeryin lotion; KFG, Kangfu gel; KSG, Kushen gel; BAL, Bai’an lotion.
3.5 Time to resolution of pruritus
There were 36 studies whose outcome measures included time to resolution of pruritus, including six interventions: CT, BFKS, KSG, HHFJL, KFG, and BAL (Figure 5A). The results showed that the overall I2 between the two-arm studies was 94.0%, indicating that the heterogeneity was large, and thus the random-effects model was used for NMA. The results of NMA (Figure 5B) showed that compared with CT, CT combined with KFG (SMD = −7.27, 95%CI [-9.57, −4.98]), KSG (SMD = −3.22, 95%CI [-3.90, −2.54]), BFKS (SMD = −3.00, 95%CI [-4.55, −1.44]), BAL (SMD = −2.43, 95%CI [-4.61, −0.26]), or HHFJL (SMD = −2.44, 95%CI [-3.60, −1.27]) significantly shortened the time to resolution of pruritus (P < 0.05). When comparisons were made between the test groups, compared with CT combined with KSG (SMD = −4.05, 95%CI [-6.45, −1.66]), BFKS (SMD = −4.28, 95%CI [-7.05, −1.51]), BAL (SMD = −4.84, 95%CI [-8.00, −1.68]), HHFJL (SMD = −4.84, 95%CI [-7.41, −2.27]), CT combined with KFG could reduce pruritus more effectively (P < 0.05). The ranking of SUCRA (Figure 5C) probability was KFG + CT > KSG + CT > BFKS + CT > BAL + CT > HHFJL + CT > CT.
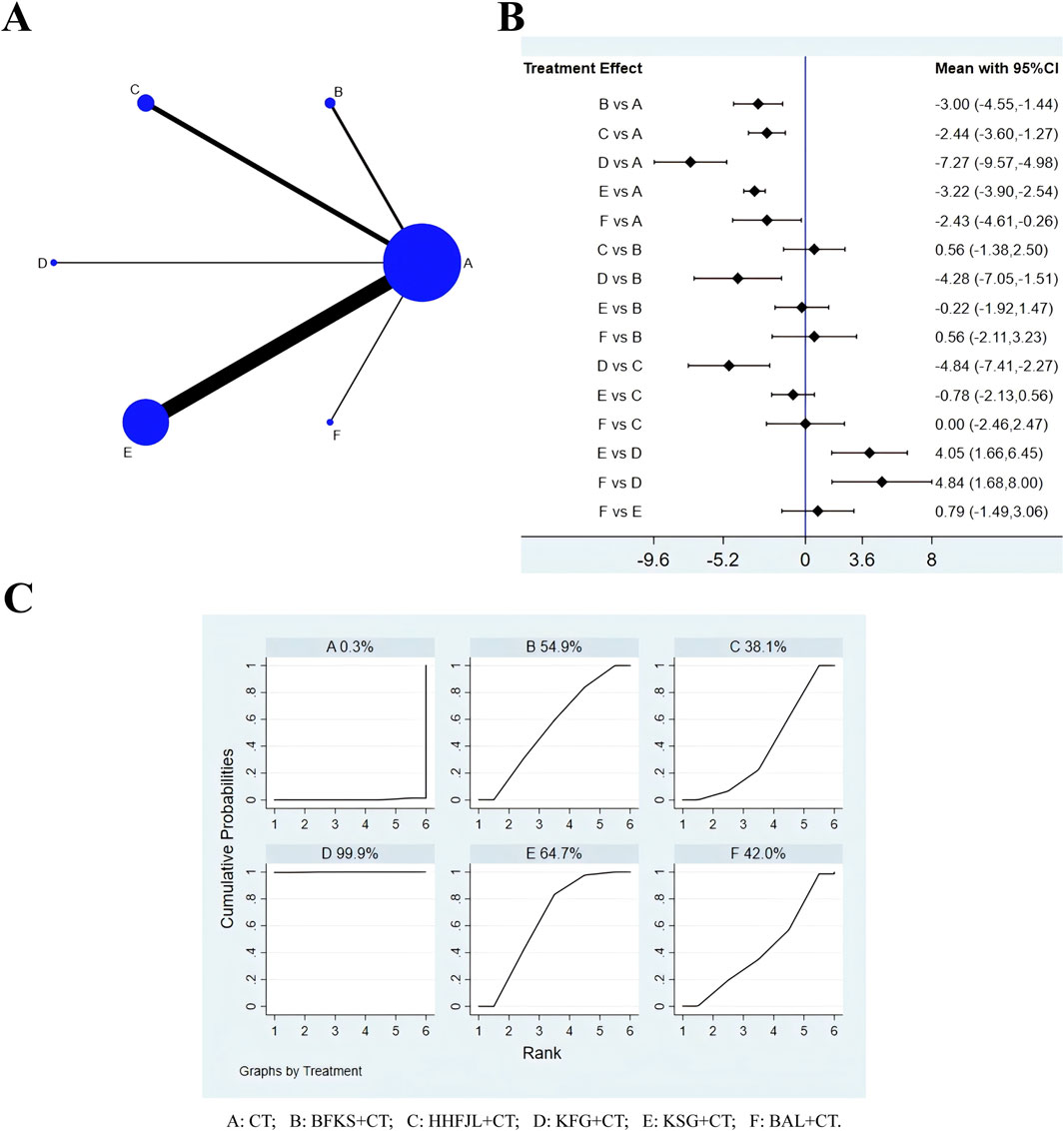
Figure 5. Evidence relationship (A), forest plot (B) and SUCRA (C) of time to resolution of pruritus. CT, conventional treatment; BFKS, Baofukang suppository; HHFJL, Honghe Fujie lotion; KFG, Kangfu gel; KSG, Kushen gel; BAL, Bai’an lotion.
3.6 Time to resolution of secretion
A total of 36 studies reported time to resolution of secretion, including six interventions (Figure 6A): CT, BFKS, KSG, HHFJL, KFG, and BAL. Because the overall I2 was 97.3%, so the random-effects model was used for analysis. The results (Figure 6B) showed that compared with CT, CT combined with BFKS (SMD = −4.03, 95% CI [-6.40, −1.67]), KSG (SMD = −3.04, 95% CI [-4.22, −1.85]), or HHFJL (SMD = −2.58, 95% CI [-4.57, - 0.59]) could reduce abnormal leucorrhea more quickly (P < 0.05), but there was no significant difference between the test groups. The ranking of SUCRA probability in decreasing time to resolution of secretion was BFKS + CT > KFG + CT > KSG + CT > HHFJL + CT > BAL + CT > CT (Figure 6C).
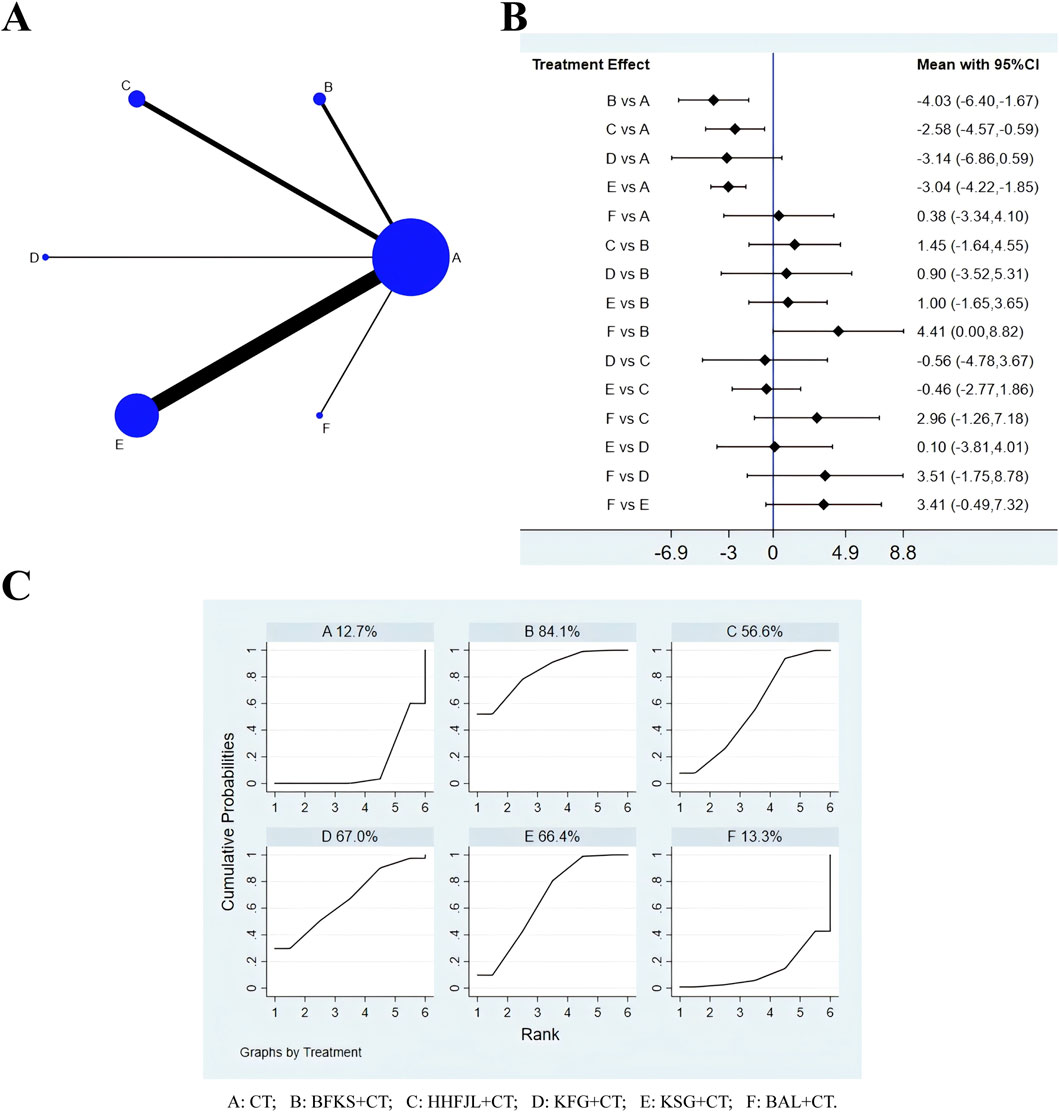
Figure 6. Evidence relationship (A), forest plot (B) and SUCRA (C) of time to resolution of secretion. CT, conventional treatment; BFKS, Baofukang suppository; HHFJL, Honghe Fujie lotion; KFG, Kangfu gel; KSG, Kushen gel; BAL, Bai’an lotion.
3.7 Adverse reaction
A total of 36 studies reported adverse reactions, including eight interventions (Figure 7A): CT, BFKS, KSG, HHFJL, FFKS, FFSJZYS, BAL, and JEYL. Because the overall I2 was 0.0%, the fixed-effects model was used for NMA. The results of this analysis (Figure 7B) suggested that compared with CT, CT combined with FFKS (OR = −1.61, 95% CI [-2.91, −0.32]) had fewer side effects (P < 0.05). Compared with CT combined with BFKS, CT combined with FFKS (SMD = −1.62, 95% CI [-3.17, −0.08]) could significantly reduce adverse reactions (P < 0.05). The ranking of SUCRA probability in reducing adverse reactions was JEYL + CT > FFKS + CT > BAL + CT > HHFJL + CT > KSG + CT > FFSJZYS + CT > BFKS + CT > CT (Figure 7C).
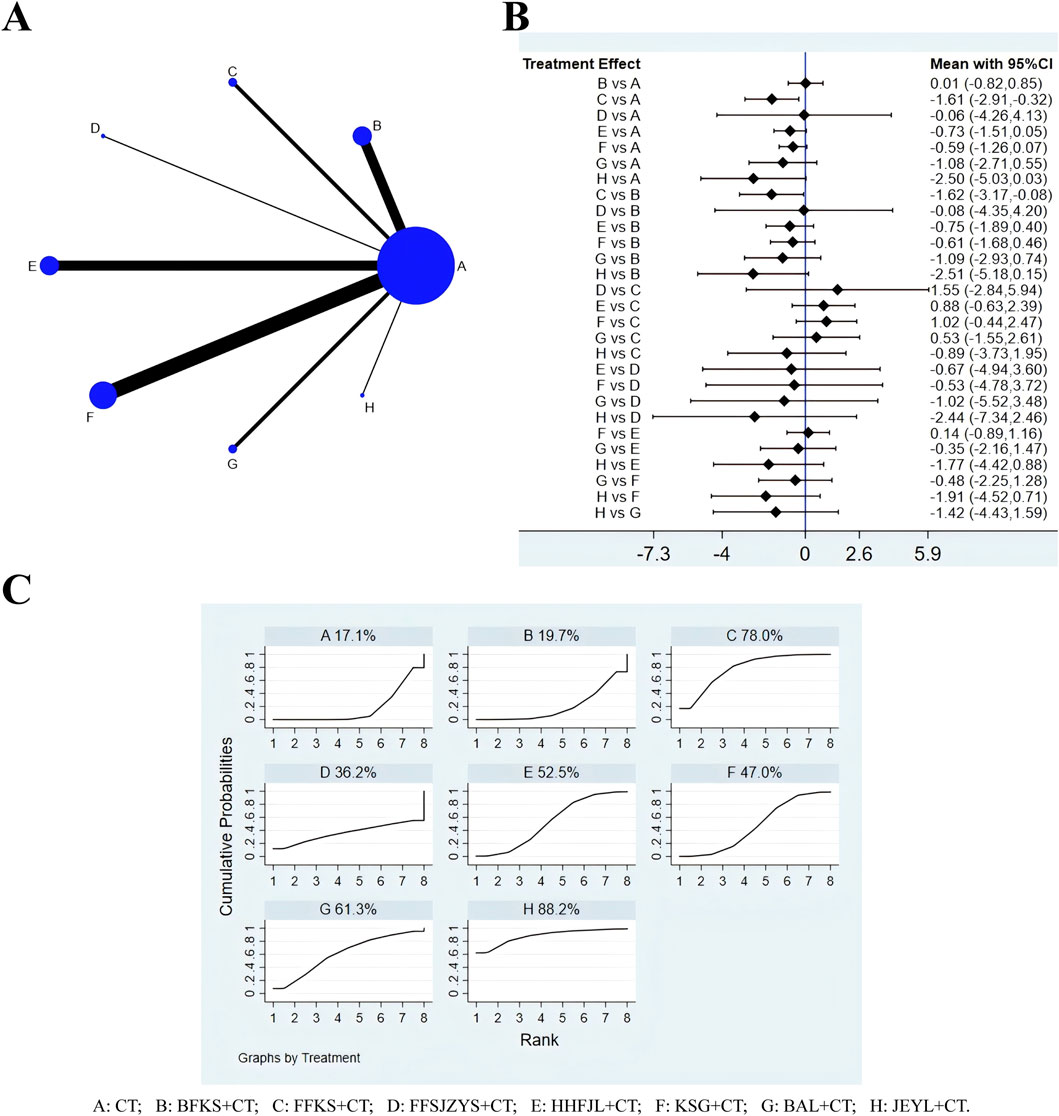
Figure 7. Evidence relationship (A), forest plot (B) and SUCRA (C) of adverse reactions. CT, conventional treatment; BFKS, Baofukang suppository; FFKS, Fufukang spray; FFSJZYS, Fufang Shajiziyou suppository; HHFJL, Honghe Fujie lotion; KSG, Kushen gel; BAL, Bai’an lotion; JEYL, Jieeryin lotion.
3.8 Publication bias analysis
With the effect size of each indicator as the abscissa and the standard error as the ordinate, a comparison-corrected funnel plot was drawn. Each dot represents a direct comparison of different interventions, and the number of dots in the same color represents the number of pairwise comparisons in the study. The results (Figure 8) demonstrated that the scattering points related to negative conversion rate, recurrence rate, and adverse reaction were basically within the range of the inverted funnel plot, and the graph was basically symmetrical about the zero line, indicating that the possibility of publication bias was small. Some scattering points involving time to resolution of pruritus and secretion were outside the range of the inverted funnel plot, suggesting that there was a high possibility of publication bias.
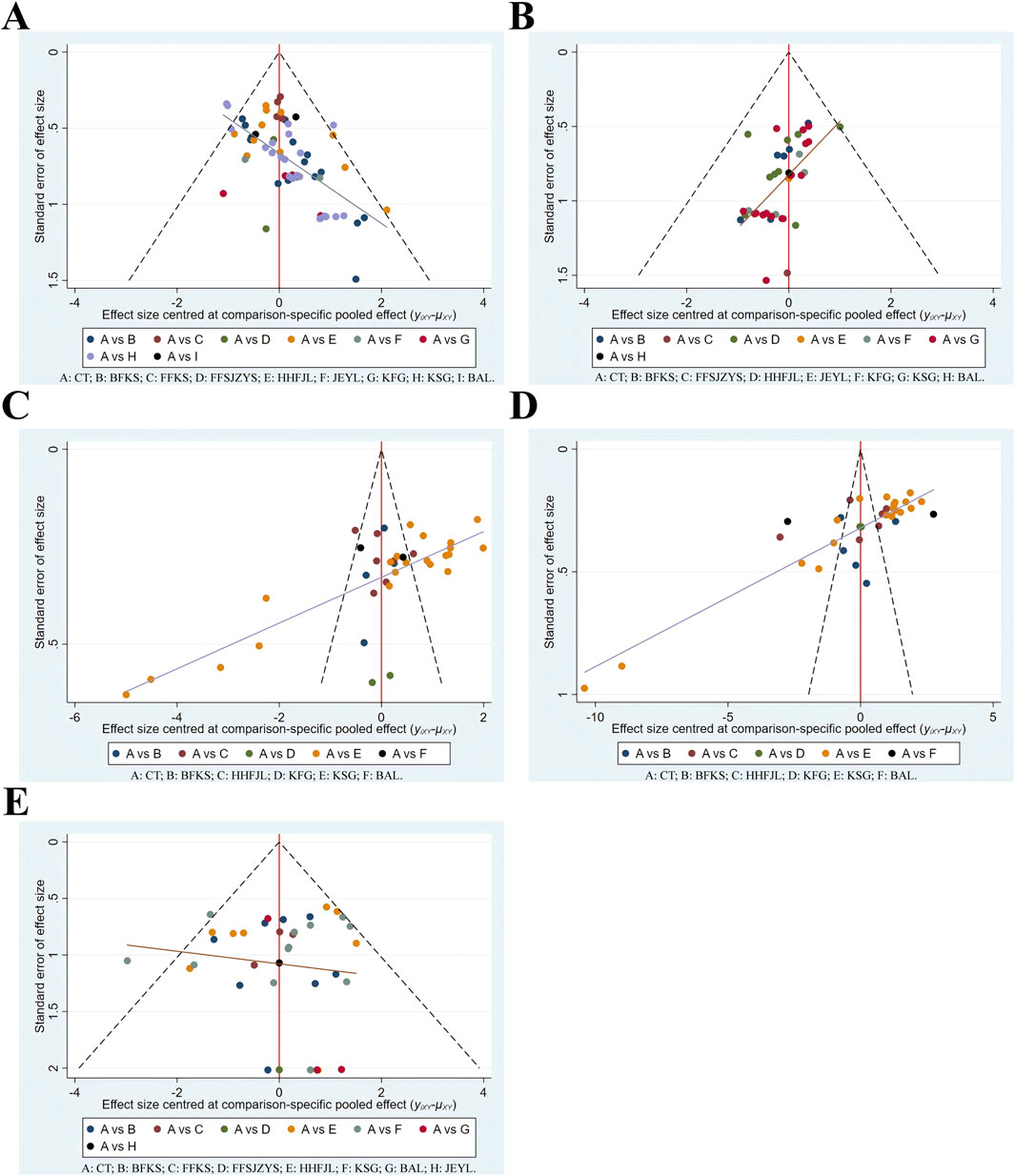
Figure 8. Funnel plots. (A) negative conversion rate; (B) recurrence rate; (C) time to resolution of pruritus; (D) time to resolution of secretion; (E) adverse reaction. CT, conventional treatment; BFKS, Baofukang suppository; FFKS, Fufukang spray; FFSJZYS, Fufang Shajiziyou suppository; HHFJL, Honghe Fujie lotion; JEYL, Jieeryin lotion; KFG, Kangfu gel; KSG, Kushen gel; BAL, Bai’an lotion.
3.9 Inconsistency, subgroup and sensitivity analysis
Because five outcomes in this NMA were non-closed loops, the consistency hypothesis was not applicable in this study. Analyses revealed heterogeneity in the time to resolve pruritus and secretion, however, results of subgroup analyses based on age, course of disease, sample size, and course of treatment showed the heterogeneity did not been decreased (Supplementary Figure S1, S2). Sensitivity analyses were performed on the negative conversion rate of C. albicans, recurrence rate, time to resolution of pruritus, time to resolution of secretion, and incidence of adverse reactions. The results indicated that the sensitivity analyses for all outcomes were stable, with no significant bias detected, thereby affirming the stability of the meta-analysis results (Supplementary Figure S3).
4 Discussion
In the study, NMA was used for the first time to compare the efficacy of eight commonly used CCPPs for VVC. The analysis suggested that CT combined with FFSJZYS had better effect in both increasing the negative conversion rate and lowering recurrence rate of C. albicans. The underlying pharmacological mechanism may be related to its composition. FFSJZYS contains seven botanical drugs. Matrine and Osthole has been proved to reduce yeast to hypha transition of C. albicans (Shao et al., 2014; Li et al., 2017). Boswellia sacra Flück. [Burseraceae, Olibanum] and Commiphora myrrha (T.Nees) Engl. [Burseraceae, Myrrha] activate blood circulation and relieve pain, Smithsonite [Calamina] and Dryobalanops aromatica C.F.Gaertn [Dipterocarpaceae, Borneolum]. astringe sores and promote granulation. Most importantly, Hippophae rhamnoides L. [Elaeagnaceae, Seabuckthorn Seed Oil] is rich in carbohydrates, lipids and isoflavones (Zuchowski, 2023). Carbohydrates can provide nutrients for the growth of normal lactobacillus and lower vaginal pH; lipids aid in repairing vaginal tissues; and isoflavones can stimulate vaginal epithelial hyperplasia and keratosis. Taken together, FFSJZYS effectively addresses the heat, dampness, blood stasis and deficiency associated with VVC pathogenesis. Modern pharmacological studies have shown that FFSJZYS can regulate the local immune function of vaginal mucosa, repair the damaged epithelium, enhance the body resistance and improve the long-term prognosis of patients (Niu. et al., 2017; Zhao. et al., 2019).
In terms of improving pruritus, CT combined with KFG was more effective. KFG is composed of five botanical drugs. The extracts of Angelica dahurica (Hoffm.) Benth. and Hook.f. ex Franch. and Sav. [Apiaceae, Angelicae Dahuricae Radix] may exert analgesic effect by suppressing TRPV1 channel and reducing NO level (Li and Wu, 2017). Zanthoxylum bungeanum Maxim. [Rutaceae, Zanthoxyli Pericarpium] disperses cold and removes dampness, its volatile oil had the antipruritic effect via the GRPR pathway (Zhou et al., 2022). The total sesquiterpene lactones isolated from Inula helenium L. [Asteraceae, Inulae Radix] reduced epidermis/dermis thickening and dermal inflammatory infiltration (Wang et al., 2018). Borneolum can induce a cooling sensation and has significant antipruritic effects in the chronic pruritus models (Yin, 2019). In addition, the gel also has a lubricating and protective function. In summary, KFG has the effects of warming Yang and drying dampness, dispelling wind and relieving itching, has been shown to reduce the level of inflammatory factors such as IL-6, reduce the pruritus, pain and mucosal congestion of vulvovagina (Lei and Wang, 2021; Chunyang LI and Song, 2022).
In terms of resolving secretion, CT combined with BFKS ranked first. BFKS contains 8.2 mg Curcuma zedoaria (Christm.) Rosc. [Zingiberaceae, Zedoary Turmeric oil] and 7.5 mg borneolum. Zedoary turmeric oil can promote the regeneration of damaged mucosa and reduce inflammatory secretions (Kamazeri et al., 2012). Borneolum can also accelerate percutaneous drug absorption and improve the bioavailability of zedoary turmeric oil in vagina. Studies have shown that BFKS promotes the repair of vaginal epithelial cells, reduce IL-2, increase the cytokine IL-4, and upregulate the level of IgG secreted by the treated VK2/E6E7 cells (Li et al., 2016). The adverse reactions mainly involved vaginal dryness or heat, aggravated itching, rash, nausea, etc., which could be alleviated by stopping treatment. CT combined with FFKS, which includes Rostellularia procumbens (L.) Nees [Acanthaceae, Rostellulariae procumbentis herba], Senecio scandens Buch.-Ham. ex D.Don [Acanthaceae, Senecionis scandentis herba], has fewer adverse effects and can be used for pregnant patients (Duan et al., 2023). In addition, JEYL, BAL and HHFJL also rank high on reducing adverse reactions, it may be also related to liquid preparations that can be metabolized faster and are milder than suppositories. However, the difference is not statistically significant, it may be associate with the small sample size.
In addition, some mechanisms of other CCPPs in treating VVC have been studied. HHFJL is made from dry distillation liquid of Crataegus pinnatifida Bunge. [Rosaceae, Crataegus Semen], it could inhibit C. albicans biofilm formation (JIN et al., 2017), a meta-analysis indicates improvement of effectiveness and safety of combination medication with HHFJL in VVC, especially among pregnant women (Lijuan et al., 2022). KSG are composed of Sophora flavescens Aiton. [Fabaceae, Total Alkaloids of Sophorae flavescentis Radix], the results of meta-analysis by Du et al. showed that KSG could increase the negative conversion rate of pathogenic bacteria, reduce the recurrence rate and clinical symptoms, which was superior to that of antifungal drug alone (Du. et al., 2021). JEYL contains key components such as matrine, osthole, baicalein, quercetin, a study confirmed that the synergistic effect of baicalein and quercetin could effectively inhibit the adherence of Candida cells by down-regulating ALS3, HYR1 and so on (Janeczko et al., 2022). Phellodendron chinense C.K.Schneid. [Rutaceae, Phellodendri Chinensis Cortex] is the sovereign drug in the BAL. Modern studies show that Berberine can inhibit biofilm formation and the adhesion of C. albicans to vaginal epithelial cells by decreasing the ICAM-1 and mucin1 expressions, balancing IL-2 and IL-4 expressions (Huang et al., 2020; Zhao et al., 2022).
To sum up, considering the clinical implications and recommendations, FFSJZYS may be the preferred treatment for patients with serious imbalance in the vaginal micro-ecological environment or those who are not cured for a long time and often relapse. KFG demonstrates strong anti-itch properties, and may be a good choice for VVC patients with severe pruritus. BFKS may be a preferred choice when it comes to reducing leukorrhea. In the incidence of adverse reactions, FFKS may have more advantages. For pregnant women, HHFJL and FFKS are safer and clinically proven. Since JEYL is contraindicated, FFSJZYS and KSG should be used with caution according to the instructions; TCM advises against borneolum (in KFG and BAL) and warns that blood-activating drugs (in BFK and FFSJZYS) are risky during pregnancy. Finally, in terms of daily cost, lotions like BAL are more economical, while suppositories and gels are pricier, with BFKS being the more affordable option among them. The above discussions were made from the TCM theory, pharmacological research and clinical experience in gynecology, but it is still crucial to choose the appropriate CCPPs based on the results of this study and the actual situation of patients in clinical practice.
This study has the following shortcomings: 1) The quality of the included studies needs to be improved, because the studies were all conducted in China, high-quality English literature is lacking, and none of them mentioned blinding and allocation concealment, so there might be bias. 2) There are differences in the number of studies and sample sizes included for each CCPP, this increases the difference in the test efficacy. There is a lack of RCTs with pairwise comparison among different CCPPs, and the evidence relationship fails to form a closed loop, these can affect the reliability and stability of the conclusions to a certain extent. 3) There was some heterogeneity in the reduction of pruritus and secretion, but the subgroup network meta-analysis of age, course of disease, sample size, and duration of treatment showed that the heterogeneity did not decrease, which may be related to many interventions and differences in patients’ subjective consciousness, etc.
In view of the limitations, the recommendations are as follows: 1) Large-sample and multi-center RCTs of international cooperation should be organized, the research plan should be registered in advance and blinding and allocation concealment should be implemented strictly to reduce risk of bias (Yue et al., 2024). 2) the quality and quantity of articles included in meta-analysis should be increased, and the baseline differences should be controlled to avoid excessive heterogeneity that affects the stability and generalizability of the results; 3) for CCPPs with limited evidence (e.g., BAL), more clinical studies are needed to further verify their efficacy, and more RCTs for direct comparison between CCPPs can be conducted to improve the level of indirect comparative evidence. 4) The treatment of VVC is challenging, future research should undertake comprehensive analyses to investigate the impact of variables such as dosage, dosage form on treatment. This will help further offer better guidance.
5 Conclusion
The NMA showed that addition of CCPPs to CT may acquire a better curative effect in patients with VVC. FFSJZYS combined with CT is more effective in improving the negative conversion rate and controlling the recurrence rate of C. albicans. KFG combined with CT had the better effect in relieving pruritus. BFKS combined with CT were the most effective in reducing leukorrhea. FFKS combined with CT had fewer adverse reactions. The conclusions aforementioned are limited to the data analysis of literature, and cannot fully explain the clinical efficacy of CCPPs, larger sample sizes and more quality RCTs are needed in future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
LW: Conceptualization, Writing–original draft, Writing–review and editing. SJ: Writing–review and editing. NL: Writing–review and editing. DC: Data curation, Writing–review and editing. FP: Supervision, Writing–review and editing. YL: Data curation, Methodology, Writing–review and editing. XC: Data curation, Writing–review and editing. YH: Software, Visualization, Writing–review and editing. CZ: Funding acquisition, Supervision, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Nos 82305288, 82374500, and 81904233), Chinese special Research fund for obstetrics and Gynecology of integrated Traditional Chinese and Western medicine (FCK-ZSYTW-03), Research Project of Inheritance and innovation of National traditional Chinese medicine (2022QN22 and 2023ZD05), National TCM inheritance innovation development demonstration pilot project (GZYZS2024XKG02), and the Young Talent Program of the First Afffliated Hospital of Guangzhou University of Chinese Medicine (No. ZYYY[2023]186).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1484325/full#supplementary-material
References
Alimu, K. (2017). Efficacy of Baofukang suppository combined with lacidophilin vaginal capsules in the treatment of patients with mycotic vaginitis. Women's Health Res. (21), 28–29.
Ban, M. (2019). Effects of Honghe Fujie lotion combined with nifuratel and nysfungin vaginal soft capsules in treatment of pregnant patients complicated with mycotic vaginitis Guide of China medicine 17(18), 177. doi:10.15912/j.cnki.gocm.2019.18.143
Cang, L., Xi, Y., and Wu, J. (2018). Application effect of clotrimazole vaginal tablets combined with Honghe Fujie lotion in the treatment of mycotic vaginitis. Clin. Res. Pract. 3 (36), 81–83. doi:10.19347/j.cnki.2096-1413.201836034
Cao, X. (2018). Study on the effect of Kushen gel combined with fluconazole capsule in fungal vaginitis. ournal Pract. Gynecol. Endocrinol. 5 (28), 27–28. doi:10.16484/j.cnki.issn2095-8803.2018.28.015
Chen, G., Guo, P., and Zhang, Y. (2017). Observation of kushen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. Nei Mongol J. Traditional Chin. Med. 36 (12), 78. doi:10.16040/j.cnki.cn15-1101.2017.12.081
Chen, L. (2017). Observation of the efficacy of clotrimazole associated with jerrying the treatment of vulvovaginal candidacies (VVC). Nei Mongol J. Traditional Chin. Med. 36 (10), 47–48. doi:10.16040/j.cnki.cn15-1101.2017.10.048
Chunyang, L. I., and Song, Y. (2022). Clinical study on Kangfu gei combined with Clotrimazole Suppouitorie in treatment of mycotic vaginitis. J. Pract. Traditional Chin. Med. 38 (07), 1184–1186.
Deng, Q. (2020). Curative effect of kushen gel combined with fluconazole capsules on fungal vaginitis. Med. Inf. 33 (07), 162–164. doi:10.3969/j.issn.1006-1959.2020.07.054
Denison, H. J., Worswick, J., Bond, C. M., Grimshaw, J. M., Mayhew, A., Gnani Ramadoss, S., et al. (2020). Oral versus intra-vaginal imidazole and triazole anti-fungal treatment of uncomplicated vulvovaginal candidiasis (thrush). Cochrane Database Syst. Rev. 8 (8), Cd002845. doi:10.1002/14651858.CD002845.pub3
Dong, J.-xiang, Wang, Z.-zhen, and Ying-hua, C. (2021). Clinical study on Bai'an Lotion combined with nifuratel and nysfungin in treatment of mycotic vaginitis Drugs and Clinic 36(03), 525–529. doi:10.7501/j.issn.1674-5515.2021.03.022
Du, H., Song, Y., and Chen, J. (2021). Meta-analysis of Kushen Gel combined with antifungal drugs in treatmentof vulvovaginal candidiasis. Chin. Traditional Herb. Drugs 52 (16), 4973–4985. doi:10.7501/j.issn.0253-2670.2021.16.022
Duan, F., Jin, W., Fu, R., Leng, X., and Chen, J. (2023). Effects of Fufukang spray combined with Clotrimazole suppositories in treatment of pregnant patients complicated with vulvovaginal candidiasis. Med. J. Chin. People's Health 35 (19), 71–74. doi:10.3969/j.issn.1672-0369.2023.19.022
Feng, J., Feng, P., and Yi, X. (2023). Analysis of clinical efficacy of fluconazole combined with KuShen gel in the treatment of mycotic vaginitis. Chin. Sci. Technol. J. Database 6.
Feng, X., Zhang, H., Hu, K., Shi, G., Wu, D., Shao, J., et al. (2024). Longdan Xiegan decoction ameliorates vulvovaginal candidiasis by inhibiting the NLRP3 inflammasome via the Toll-like receptor/MyD88 pathway. J. Ethnopharmacol. 318 (Pt A), 116869. doi:10.1016/j.jep.2023.116869
Gong, X. (2017). Clinical effect of kushen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. J. North Pharm. 14 (07), 12–13.
Guo, J. (2017). Effects of kushen gel combined with fluconazole on fungal vaginitis and vaginal microecology. Shenzhen J. Integr. Traditional Chin. West. Med. 27 (23), 23–25. doi:10.16458/j.cnki.1007-0893.2017.23.011
Hao, Y. (2017). Clinical observation on the treatment of mycotic vaginitis with traditional Chinese medicine and western medicine. J. Pract. Traditional Chin. Med. 33 (12), 1396–1397.
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Bmj 343, d5928. doi:10.1136/bmj.d5928
Hu, L. (2022). Efficacy of Baofukang suppository and lactobacillus vaginal capsule in patients with vaginitis during pregnancy. Women's Health Res. (9).
Hu, L., and Liu, F. (2018). Clinical efficacy of fluconazole capsules combined with Baofukang suppository in the treatment of mycotic vaginitis. Maternal Child Health Care China 33 (10), 2228–2229. doi:10.7620/zgfybj.j.issn.1001-4411.2018.10.22
Hua, R., and Dai, Y. (2018). Clinical efficacy of Baofukang suppository combined with miconazole in the treatment of patients with vulvovaginal candidiasis. Anti-Infection Pharm. 15 (08), 1421–1423. doi:10.13493/j.issn.1672-7878.2018.08-048
Huang, J. (2017). Clinical observation of kushen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. Electron. J. Clin. Med. Literature 4 (92), 18178–18179. doi:10.16281/j.cnki.jocml.2017.92.089
Huang, K. (2012). Effect of itraconazole combined with Bafukang Suppository in the treatment of candidal vaginitis. ournal Youjiang Med. Univ. Natl. 34 (04), 493–494. doi:10.3969/j.issn.1001-5817.2012.04.026
Huang, P., Li, Z., Chen, L., Zeng, J., Zhao, S., Tang, Y., et al. (2022). The comparative effects of oral Chinese patent medicines combined with western medicine in stable angina: a systematic review and network meta-analysis of 179 trials. Front. Pharmacol. 13, 918689. doi:10.3389/fphar.2022.918689
Huang, X., Zheng, M., Yi, Y., Patel, A., Song, Z., and Li, Y. (2020). Inhibition of berberine hydrochloride on Candida albicans biofilm formation. Biotechnol. Lett. 42 (11), 2263–2269. doi:10.1007/s10529-020-02938-6
Janeczko, M., Gmur, D., Kochanowicz, E., Górka, K., and Skrzypek, T. (2022). Inhibitory effect of a combination of baicalein and quercetin flavonoids against Candida albicans strains isolated from the female reproductive system. Fungal Biol. 126 (6-7), 407–420. doi:10.1016/j.funbio.2022.05.002
Ji, M. (2023). Application value of kushen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. Chinese science and technology journal database 8, 102–104.
Jia, Y. (2023). Clinical efficacy of Honghe Fujie lotion combined with clotrimazole vaginal tablets in the treatment of mycotic vaginitis. New Mom and new born 3, 67–69.
Jin, Z., Feng, Y. A. O., Chen-xu, SHANG, hong, L. J.-, Fei, Mo, Yun-fang, X. A. O., et al. (2017). Study on the antifungal activity of Honghefujie lotion against Candida Albicans biofilmand pathogen of superficial mycoses in vitro. Chin. J. Clin. Pharmacol. 33 (16), 1556–1560. doi:10.13699/j.cnki.1001-6821.2017.16.012
Kamazeri, T. S., Samah, O. A., Taher, M., Susanti, D., and Qaralleh, H. (2012). Antimicrobial activity and essential oils of Curcuma aeruginosa, Curcuma mangga, and Zingiber cassumunar from Malaysia. Asian Pac J. Trop. Med. 5 (3), 202–209. doi:10.1016/s1995-7645(12)60025-x
Lei, L., and Wang, H. (2021). Observation on the curative effect of Kangfu gel in the treatment of bacterial vaginitis and fungal vaginitis. China Contin. Med. Educ. 13 (18), 162–165. doi:10.3969/j.issn.1674-9308.2021.18.046
Lei, L., and Yang, S. (2021). Clinical observation on the treatment of recurrent Candida vaginitis with traditional Chinese medicine and western medicine. China Contin. Med. Educ. 13 (06), 157–160.
Lei, X. (2020). Clinical observation of Bai'an lotion combined with Nifuratel capsule in the treatment of mycotic vaginitis. Kang Yi (13), 241. doi:10.12332/j.issn.2095-6525.2020.13.235
Lei, Y. (2014). Clinical efficacy of compound sea buckthorn seed oil suppository combined with miconazole nitrate suppositories in the treatment of mycotic vaginitis qinghai medical journal 44(05), 25–26.
Li, C. (2017a). Clinical efficacy of Baofukang suppository in the treatment of mycotic vaginitis during pregnancy world latest medicine information 17(92), 95. doi:10.19613/j.cnki.1671-3141.2017.92.074
Li, D., and Wu, L. (2017). Coumarins from the roots of Angelica dahurica cause anti-allergic inflammation. Exp. Ther. Med. 14 (1), 874–880. doi:10.3892/etm.2017.4569
Li, D.-D., Chai, D., Huang, X.-W., Guan, S.-X., Du, J., Zhang, H.-Y., et al. (2017). Potent in vitro synergism of fluconazole and osthole against fluconazole-resistant Candida albicans. Antimicrob. Agents Chemother. 61 (8). doi:10.1128/AAC.00436-17
Li, L. (2022). Clinical study of clotrimazole combined with kushen gel in the treatment of recurrent fungal vaginitis. Chin. Sci. and Technol. J. database 4.
Li, T., Niu, X., Zhang, X., Wang, S., and Liu, Z. (2016). Baofukang suppository promotes the repair of vaginal epithelial cells in response to Candida albicans. Amb. Express 6 (1), 109. doi:10.1186/s13568-016-0281-1
Li, Y. (2017b). Effects of Honghe Fujie Lotion in treatment of pregnant patients complicated with vulvovaginal candidiasis. Guide China Med. 15 (21), 175. doi:10.15912/j.cnki.gocm.2017.21.142
Li, Y. (2020). Effects of Fufukang spray combined with mico nazole nitrate suppositories in treatment of mycotic vaginitis smart healthcare 6(28), 75–77. doi:10.19335/j.cnki.2096-1219.2020.28.031
Lijuan, D., Lu, Y., Liping, W., Yaya, S., Xiaoyun, L., and Xiangrong, L. I. (2022). Effectiveness of redcore lotion in patients with vulvovaginal candidiasis: a systematic review and Meta-analysis. J. Tradit. Chin. Med. 42 (4), 487–492. doi:10.19852/j.cnki.jtcm.2022.04.001
Liu, S., Fan, Y., and Jiang, M. (2023). Effect of Honghe Fujie lotion combined with nifuratel nystatin on symptom improvement time and vaginal cleanliness in patients with candidal vaginitis drug evaluation 20(01), 72–74. doi:10.19939/j.cnki.1672-2809.2023.01.19
Liu, W., and Feng, Q. (2020). Clinical study on kushen gels combined with metronidazole, clotrimazole and chlorhexidine acetate vagina gels in treatment of mycotic vaginitis drugs and clinic 35(02), 239–242.
Ma, L., and Xu, X. (2022). Clinical study of kushen gel combined with microwave and fluconazole on mycotic vaginitis new Chinese medicine 54(02), 114–117. doi:10.13457/j.cnki.jncm.2022.02.031
Ma, W. (2022). Clinical analysis of KuShen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. Bao Jian Wen Hui 23 (14), 4–6.
Niu, X., Li, T., and Liu, C. (2017). The repair effect of Fufang Shajiziyou suppository in vaginal epithelial mucosa damage. Chin. J. Pract. Gynecol. Obstetrics 33 (02), 195–199. doi:10.19538/j.fk2017020116
Nyirjesy, P., Brookhart, C., Lazenby, G., Schwebke, J., and Sobel, J. D. (2022). Vulvovaginal candidiasis: a review of the evidence for the 2021 centers for disease control and prevention of sexually transmitted infections treatment guidelines. Clin. Infect. Dis. 74, S162–s168. doi:10.1093/cid/ciab1057
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj 372, n71. doi:10.1136/bmj.n71
Pi, X. (2023). The clinical effect of Matrine gel combined with fluconazole capsule in the treatment of vulvovaginal candidiasis. Contemp. Med. 29 (10). doi:10.3969/j.issn.1009-4393.2023.10.008
Quan, T., and Huang, L. (2021). Effect of combined Chinese and western medicine in the treatment of patients with vulvovaginal candidiasis. Acta Med. Sin. 34 (04), 125–128. doi:10.19296/j.cnki.1008-2409.2021-04-032
Sang, X. (2017). Clinical Efficacy of kushen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. ournal Pract. Gynecol. Endocrinol. 4 (28), 29–31. doi:10.16484/j.cnki.issn2095-8803.2017.28.019
Sanjaya, H., and Pemayun, C. (2023). Vaginal ozone insufflation in management of vaginal candidiasis. EJMHS 5(5), 13–16. doi:10.24018/ejmed.2023.5.5.1414
Satora, M., Grunwald, A., Zaremba, B., Frankowska, K., Żak, K., Tarkowski, R., et al. (2023). Treatment of vulvovaginal candidiasis-an overview of guidelines and the latest treatment methods. J. Clin. Med. 12 (16), 5376. doi:10.3390/jcm12165376
Saxon Lead Author, G., Edwards, A., Rautemaa-Richardson, R., Owen, C., Nathan, B., Palmer, B., et al. (2020). British Association for Sexual Health and HIV national guideline for the management of vulvovaginal candidiasis (2019). Int. J. STD AIDS 31 (12), 1124–1144. doi:10.1177/0956462420943034
Shang, Y., and Shang, w. (2020). Effects of fluconazole combined with kushen gel on serum IL-1β and PH levels in patients with mycotic vaginitis. Mod. Diagnosis and Treat. 31 (08), 1213–1214.
Shao, J., Wang, T., Yan, Y., Shi, G., Cheng, H., Wu, D., et al. (2014). Matrine reduces yeast-to-hypha transition and resistance of a fluconazole-resistant strain of Candida albicans. J. Appl. Microbiol. 117 (3), 618–626. doi:10.1111/jam.12555
Shi, Y., and Zhang, A. (2020). Effects of Honghe Fujie lotion in the treatment of mycotic vaginitis and its influences on serum inflammatory indexes and quality of life. Maternal Child Health Care China 35 (12), 2203–2206. doi:10.19829/j.zgfybj.issn.1001-4411.2020.12.019
Shim, S., Yoon, B. H., Shin, I. S., and Bae, J. M. (2017). Network meta-analysis: application and practice using Stata. Epidemiol. Health 39, e2017047. doi:10.4178/epih.e2017047
Song, J. (2011). Effects of Jieeryin lotion combined withNystatin tablets in treatment of mycotic vaginitis Chinese and foreign medical research 9(18), 120. doi:10.14033/j.cnki.cfmr.2011.18.104
Song, Y. (2016). Clinical study on the treatment of mycotic vaginitis with traditional Chinese medicine and western medicine. Women's Health Res. (22), 154–158.
Song, Y., Song, N., Jia, L., and Pei, Y. (2024). Effectiveness and safety of Danshen injections in treatment of cardiac failure: a network meta-analysis. Front. Pharmacol. 15, 1319551. doi:10.3389/fphar.2024.1319551
Sun, Y., and Fang, Y. (2015). Clinical efficacy of Honghe Fujie Lotion combined with Clotrimazole suppositories in treatment of pregnant patients complicated with vulvovaginal candidiasis New Chinese Medicine 47(02), 148–149. doi:10.13457/j.cnki.jncm.2015.02.071
Sun, Z., Ge, X., Qiu, B., Xiang, Z., Jiang, C., Wu, J., et al. (2023). Vulvovaginal candidiasis and vaginal microflora interaction: microflora changes and probiotic therapy. Front. Cell Infect. Microbiol. 13, 1123026. doi:10.3389/fcimb.2023.1123026
Tong, J., and Zhang, J. (2022). Clinical efficacy of fluconazole capsules combined with Baofukang suppository in the treatment of recurrent mycotic vaginitis. Chin. Sci. Technol. J. Database Abstract Ed. Med. Health (1).
Wan, W., and Hu, Y. (2021). Clinical study of vulvovaginal candidiasis during pregnancy treated with Kangfu gel combined with nifuratel nysfungin vaginal soft capsules. ournal Jiangxi Univ. Traditional Chin. Med. 33 (05), 51–53.
Wang, C., and Hu, D. (2016). Therapeutic effect of KuShen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. New Chin. Med. 48 (08), 180–181. doi:10.13457/j.cnki.jncm.2016.08.078
Wang, He, Han, X., and Lang, G. (2015a). Efficacy and safety of honghefujie lotion plus nifuratel nysfungin vaginal soft capsules for Candida vaginitis in pregnant women. Eval. Analysis Drug-Use Hosp. China 15 (03), 306–308. doi:10.14009/j.issn.1672-2124.2015.03.007
Wang, J. (2005). Clinical efficacy of Baofukang suppository combined with sporanox in the treatment of patients with recurrent vulvovaginal candidiasis. Modern Journal of integrated traditional Chinese and western medicine 13, 1717–1718.
Wang, J. (2018a). Clinical efficacy of Honghe Fujie Lotion in treatment of pregnant patients complicated with vulvovaginal candidiasis. J. Pract. Gynecol. Endocrinol. 5 (32), 99–100. doi:10.16484/j.cnki.issn2095-8803.2018.32.073
Wang, L. (2018b). Analysis of clinical efficacy of Baofukang suppository in the treatment of mycotic vaginitis smart healthcare 4(19), 69–70. doi:10.19335/j.cnki.2096-1219.2018.19.031
Wang, N., Cui, L., Ma, C., and Wang, H. (2015b). Clinical observation on treatment of mycotic vaginitis with Sophora gel combined with Fluconazole capsules China Journal of Chinese Materia Medica 40(05), 978–980.
Wang, Q. (2016). Clinical observation on the treatment of recurrent vulvovaginal candidiasis withLacidophilin Vaginal Capsules combined with Baofukang suppository New Chinese Medicine 48(03), 140–141. doi:10.13457/j.cnki.jncm.2016.03.055
Wang, Q., Gao, S., Wu, G. Z., Yang, N., Zu, X. P., Li, W. C., et al. (2018). Total sesquiterpene lactones isolated from Inula helenium L. attenuates 2,4-dinitrochlorobenzene-induced atopic dermatitis-like skin lesions in mice. Phytomedicine 46, 78–84. doi:10.1016/j.phymed.2018.04.036
Wang, Y. (2020). Clinical analysis of Sophora flavescens gel and fluconazole capsule in the treatment of mycotic vaginitis. Syst. Med. 5 (02), 22–24. doi:10.19368/j.cnki.2096-1782.2020.02.022
Wang, Z., Wu, N., Ma, Y., Cai, R., and Xu, X. (2022). Migration and transformation of Cd in pig manure-insect frass (Hermetia illucens)-Soil-Maize system. Women's Health Res. 20(9), 60–61. doi:10.3390/ijerph20010060
Wen, J. (2017). Clinical effect on treatment of mycotic vaginitis with Sophora gel combined with Fluconazole capsules. Women's Health Res. (23), 69–70.
Wu, L. Z., Ke, Y., Huang, L., Lin, L. W., Huang, Y. J., Pei, F. L., et al. (2022). Network Meta-analysis of peroral Chinese patent medicines for activating blood and resolving stasis in treatment of endometriosis. Zhongguo Zhong Yao Za Zhi 47 (11), 3073–3087. doi:10.19540/j.cnki.cjcmm.20220224.501
Xiao, X., and Chen, X. (2023). Effects of fluconazole tablets combined with HongHe FuJie lotion on patients with vulvovaginal candidiasis. J. China Prescr. Drug 21 (7), 115–118. doi:10.3969/j.issn.1671-945X.2023.07.031
Xiong, H. (2022). Effects of Fufukang spray combined with clotrimazole suppositories in treatment of mycotic vaginitis. Women's Health Res. (6), 59–61.
Xu, B. (2020). Clinical efficacy of Fufukang spray combined with mico nazole nitrate suppositories in theTreatment of mycotic vaginitis electronic Journal of practical gynecological endocrinology 7(35), 13–14. doi:10.16484/j.cnki.issn2095-8803.2020.35.010
Xu, T. (2023). Clinical efficacy of Baofukang suppository combined with lacidophilinvaginal capsules in the treatment of patients with mycotic vaginitis. Chinese Science and technology journal database (abstract edition) Medical and health 10, 16–19.
Xu, Z. (2022). Clinical efficacy and recurrence rate analysis of kushen gel combined with Metronidazole,Clotrimazole and Chlorhexidine Acetate Vagina Gel in the treatment of mycotic vaginitis. Med. Diet Health 20 (12), 60–63.
Xue, H. (2022). Clinical effect of Honghefujie lotion in the treatment of vulvovaginal candidiasis. Chin. J. Urban Rural Enterp. 37 (02), 142–144. doi:10.16286/j.1003-5052.2022.02.057
Yang, G. (2011a). Clinical efficacy of Baofukang suppository combined with ketoconazole in the treatment of 47 patients with vulvovaginal candidiasis. China Pharm. 20 (18), 63.
Yang, H. (2022). Clinical effect of Baofukang suppository combined with clotrimazole suppository in treatment of monilial vaginitis. J. Chin. FOREIGN Med. Pharm. Res. 1 (15), 82–84. doi:10.3969/j.issn.2096-6229.2022.15.027
Yang, L. (2021). Clinical study of sophora flavescens gel combined with nitrofurtail vaginal soft capsule in the treatment of fungal vaginitis. Tianjin Pharm. 33 (05), 53–55.
Yang, L., Wu, H., Qiu, W., Guo, L., Du, X., Yu, Q., et al. (2018). Pulsatilla decoction inhibits Candida albicans proliferation and adhesion in a mouse model of vulvovaginal candidiasis via the Dectin-1 signaling pathway. J. Ethnopharmacol. 223, 51–62. doi:10.1016/j.jep.2018.05.018
Yang, R. (2011b). Clinical efficacy of compound sea buckthorn seed oil suppository combined with miconazole nitrate suppositories in the treatment of 180 patients with mycotic vaginitis Chinese Journal of modern drug application 5(19), 91–92. doi:10.14164/j.cnki.cn11-5581/r.2011.19.094
Yang, Z., Li, J., Zhou, B., Ji, X., Yuan, J., Yan, J., et al. (2023). Efficacy and safety of oral Chinese patent medicines in the treatment of coronary heart disease combined with hyperlipidemia: a systematic review and network meta-analysis of 78 trials. Chin. Med. 18 (1), 162. doi:10.1186/s13020-023-00866-x
Yano, J., Sobel, J. D., Nyirjesy, P., Sobel, R., Williams, V. L., Yu, Q., et al. (2019). Current patient perspectives of vulvovaginal candidiasis: incidence, symptoms, management and post-treatment outcomes. BMC Womens Health 19 (1), 48. doi:10.1186/s12905-019-0748-8
Yin, L. (2019). Anti-inflammatory and antipruritic effects of (+)borneol and the molecular mechanisms M, South-Central University for Nationalities.
Yin, Q. (2021). Effect of ketoconazole combined with sophora gel on symptom and inflammatory factor level in patients with recurrent mycotic vaginitis Chinese Journal of Human Sexuality 30(04), 131–134.
Yu, L. (2023). Clinical effect of Honghefujie lotion on vaginal candidiasis. Cap. Med. 30 (3), 146–148. doi:10.3969/j.issn.1005-8257.2023.03.051
Yu, Y. (2017). Clinical efficacy of Honghe Fujie lotion in the treatment of vulvovaginal candidiasi. Contemp. Med. 23 (36), 111–112. doi:10.3969/j.issn.1009-4393.2017.36.048
Yue, L., Xiao, L., Zhang, X., Niu, L., Wen, Y., Li, X., et al. (2024). Comparative efficacy of Chinese herbal injections in patients with cardiogenic shock (CS): a systematic review and Bayesian network meta-analysis of randomized controlled trials. Front. Pharmacol. 15, 1348360. doi:10.3389/fphar.2024.1348360
Yuqing, J., and Yu, J. (2022). Clotrimazole suppository combined with kushen gel patients of 37 cases with candidal vaginitis. Drug Eval. 19 (04), 233–235. doi:10.19939/j.cnki.1672-2809.2022.04.11
Zeng, X. (2021). Clinical efficacy of Baofukang suppository combined with clotrimazole vaginal tablets in the treatment of patients with recurrent vulvovaginal candidiasis. China J. Pharm. Econ. 16 (11), 49–52. doi:10.12010/j.issn.1673-5846.2021.11.009
Zeng, Y. (2023). Clinical study on Kushen Gel combined with policresulen in treatment of vaginal candida. Drugs and Clinic 38 (05), 1213–1217. doi:10.7501/j.issn.1674-5515.2023.05.032
Zhang, D., Lin, H., Zhaohui, L. I. U., Li, GENG, Wang, W., Bei, X. I. A., et al. (2016). Compound sea buckthorn seed oil suppository improves the microecological environment of vagina. Chin. J. Microecology 28 (10), 1201–1205. doi:10.13381/j.cnki.cjm.201610023
Zhang, L., Liu, S., Gu, Y., Li, S., Liu, M., and Zhao, W. (2022). Comparative efficacy of Chinese patent medicines for non-alcoholic fatty liver disease: a network meta-analysis. Front. Pharmacol. 13, 1077180. doi:10.3389/fphar.2022.1077180
Zhang, X. (2013). Effects of Fufukang spray in the treatment of mycotic vaginitis. Med. Inform. 28, 229.
Zhang, X. (2019). Clinical experience of Honghe Fujie lotion combined with clotrimazole vaginal tablets inthe treatment of fungal vaginitis. Drug and Clinic 16(21), 13–14.
Zhang, X. (2023). Effect of Bai'an lotion combined with Metronidazole,Clotrimazole and chlorhexidine acetate vagina gel on mycotic vaginitis practical clinical Journal of integrated traditional Chinese and western medicine 23(14), 62–64+83. doi:10.13638/j.issn.1671-4040.2023.14.018
Zhang, Y. (2020). Clinical efficacy of Honghe Fujie lotion combined with nystatin tablets in the treatment of mycotic vaginitis strait pharmaceutical journal 32(07), 120–121.
Zhao, H. (2018). Clinical efficacy of KuShen gel combined with fluconazole capsules in the treatment of mycotic vaginitis. Med. Forum 22 (07), 930–931. doi:10.19435/j.1672-1721.2018.07.039
Zhao, R. (2022). Effects of Honghe Fujie lotion combined with Lacidophilin vaginal capsules in the treatment of mycotic vaginitis and its influences on inflammatory indexes of vaginal secretions and vaginal flora. Clin. Res. Pract. 7 (26), 94–96. doi:10.19347/j.cnki.2096-1413.202226025
Zhao, T., Zhang, K., Shi, G., Ma, K., Wang, B., Shao, J., et al. (2022). Berberine inhibits the adhesion of Candida albicans to vaginal epithelial cells. Front. Pharmacol. 13, 814883. doi:10.3389/fphar.2022.814883
Zhao, X., Jin, L., Cang, C., and Wei, H. (2019). Linical effect of compound seabuckthorn seed oil suppository combined with recombinant human interferon-α2b suppository on human papillomavirus infection complicated with chronic cervicitis,immune function and inflammatory factors. China Med. 14 (11), 1689–1693. doi:10.3760/i.issn.1673-4777.2019.11.023
Zhou, X. L., Chen, L. L., and Wang, J. F. (2022). Study on the antipruritic mechanism of Zanthoxylum bungeanum and Zanthoxylum schinifolium volatile oil on chronic eczema based on H1R and PAR-2 mediated GRPR pathway. Allergol. Immunopathol. Madr. 50 (4), 83–96. doi:10.15586/aei.v50i4.486
Keywords: vulvovaginal candidiasis, commercial Chinese polyherbal preparation (CCPP), Chinese patent medicine, traditional Chinese medicine (TCM), anti-fungal drugs, network meta-analysis, a review
Citation: Wu L, Jing S, Li N, Cao D, Pei F, Luo Y, Chen X, Huang Y and Zeng C (2025) Comparative efficacy of topical commercial Chinese polyherbal preparation for vulvovaginal candidiasis: a network meta-analysis. Front. Pharmacol. 16:1484325. doi: 10.3389/fphar.2025.1484325
Received: 21 August 2024; Accepted: 06 January 2025;
Published: 03 February 2025.
Edited by:
Miao Liu, Harvard Medical School, United StatesReviewed by:
Dongwei Sun, University of California, Riverside, United StatesXinran Qi, Dana–Farber Cancer Institute, United States
Hui Wang, University of California, Los Angeles, United States
Xi Xu, University of Toronto, Canada
Copyright © 2025 Wu, Jing, Li, Cao, Pei, Luo, Chen, Huang and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fangli Pei, cGVpZmFuZ2xpNTM2OUBnenVjbS5lZHUuY24=; Cheng Zeng, ZHJ6Y2hlbmdAZ3p1Y20uZWR1LmNu
†These authors have contributed equally to this work
 Lizheng Wu
Lizheng Wu Shangwen Jing
Shangwen Jing Na Li3
Na Li3 Dandan Cao
Dandan Cao Fangli Pei
Fangli Pei Xiaoxin Chen
Xiaoxin Chen Cheng Zeng
Cheng Zeng