- Department of Paediatrics, Guang’anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
Background: Traditional Chinese medicine (TCM) is used to treat mycoplasma pneumonia (MP) in children with favorable treatment outcome in China. In the present study, we evaluated the clinical efficacy of TCM combined with azithromycin (AZM) for the treatment of MP among children, providing high evidence-based reference for clinical treatment.
Method: We retrieved eligible randomized controlled trials (RCTs) from CQVIP, CNKI, WanFang, NSTL, PubMed, Embase, and Embase databases from January 2000 to November 2023. Data extraction and quality assessment of the enrolled studies were independently by two reviewers. Review Manager 5.3 was used for meta-analysis.
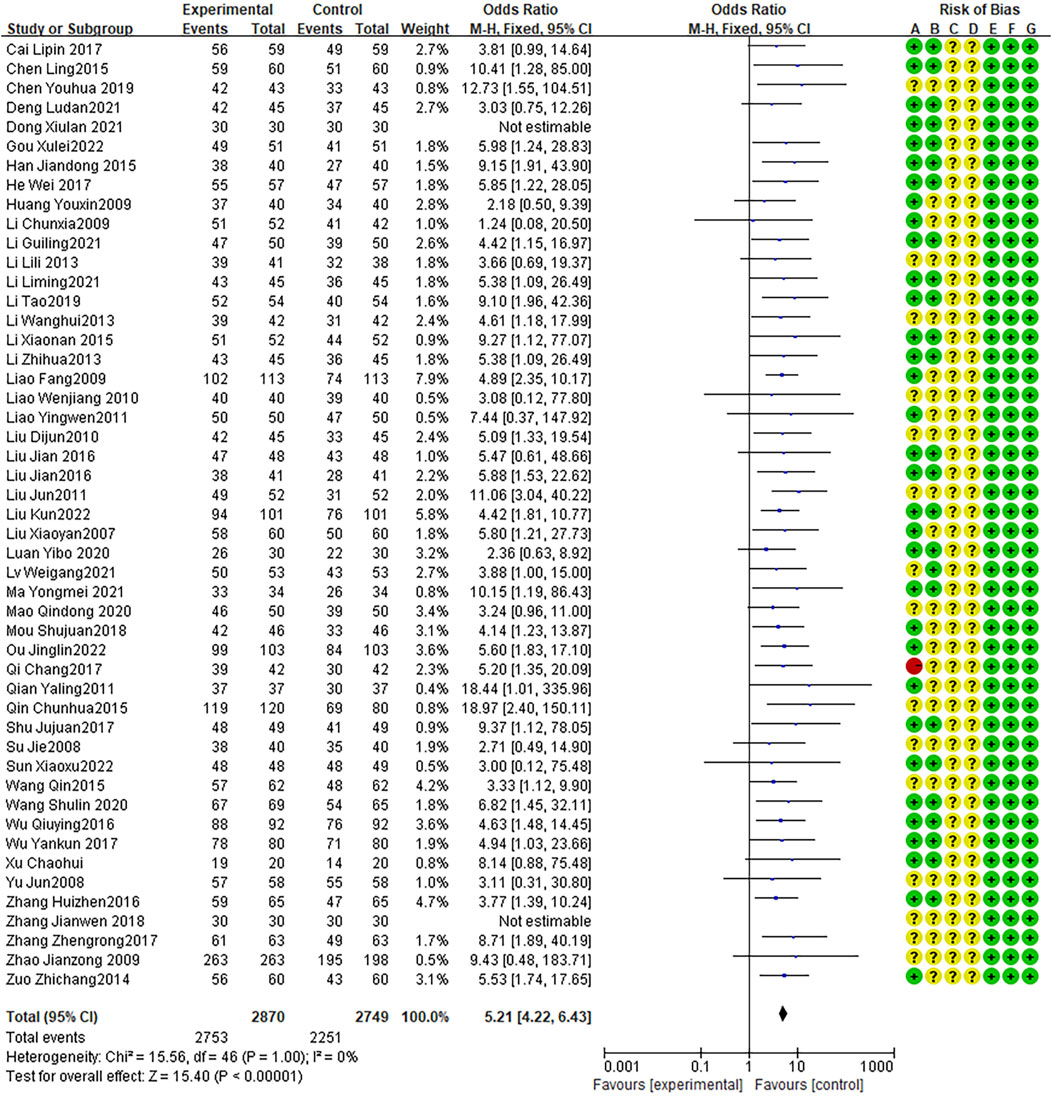
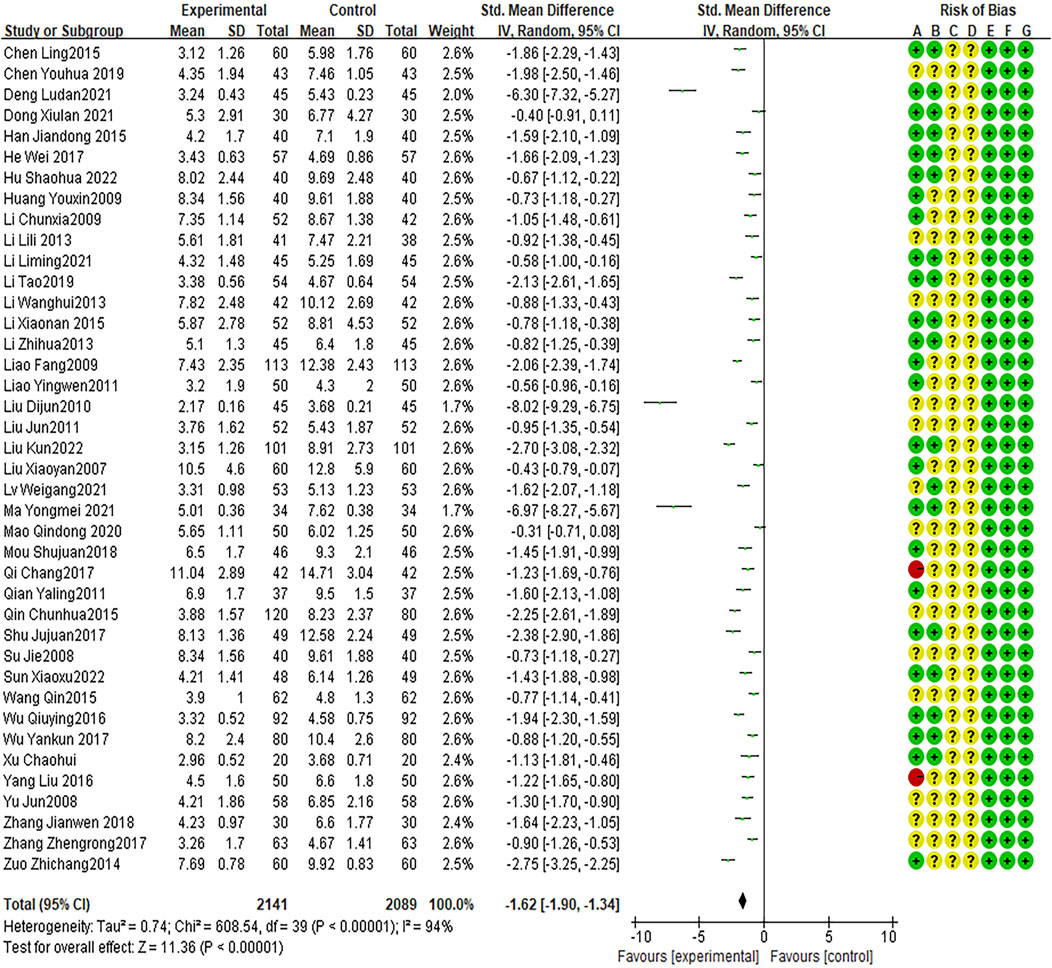
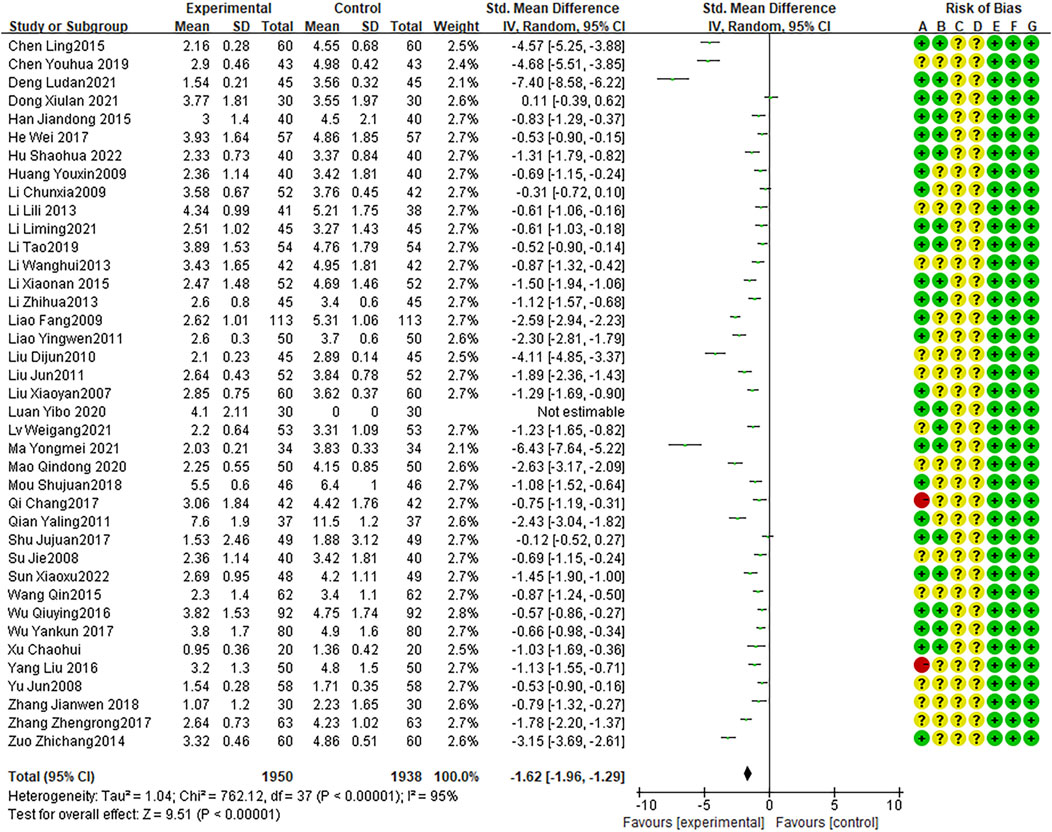
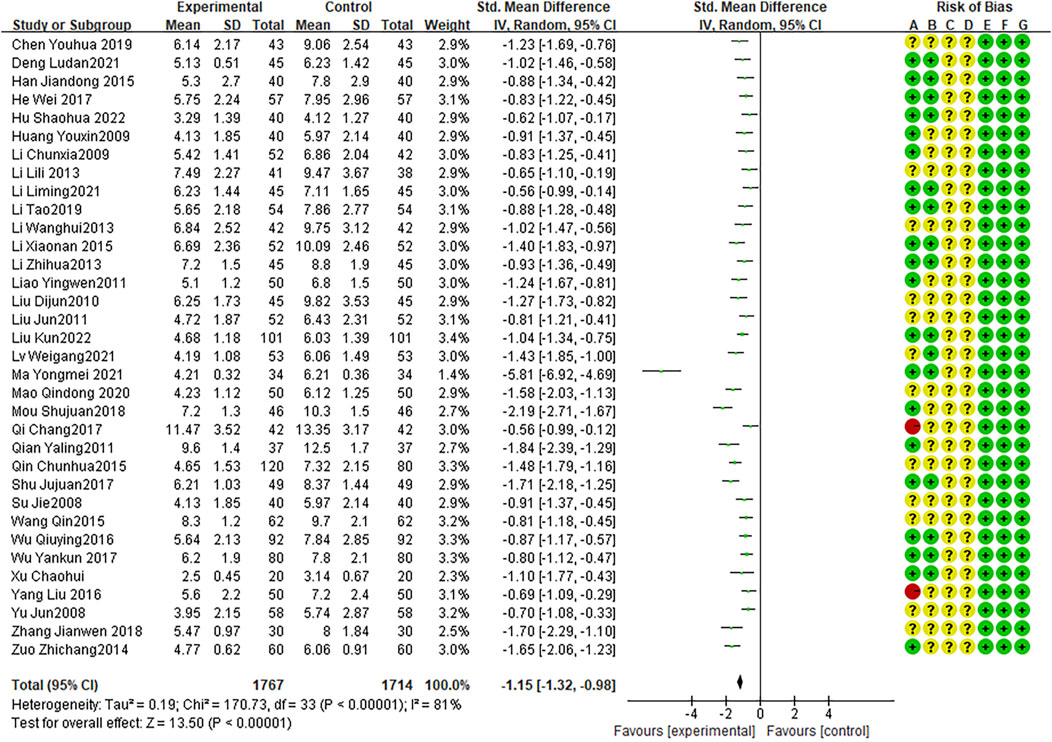
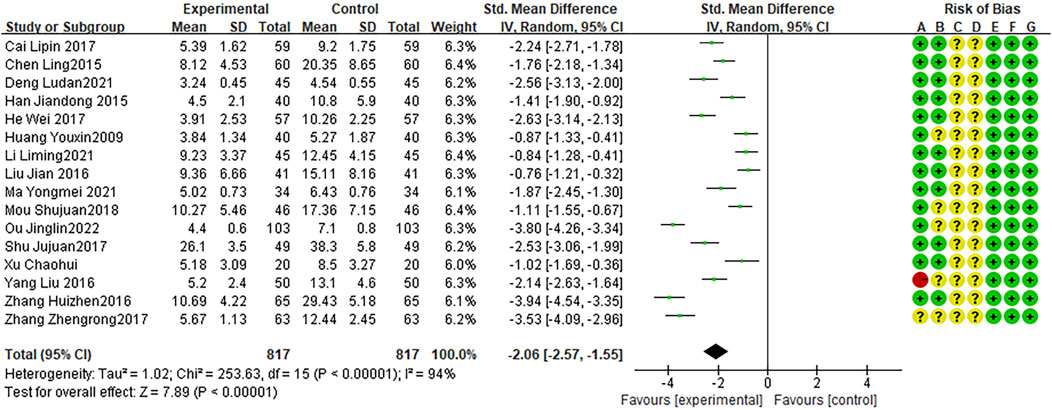
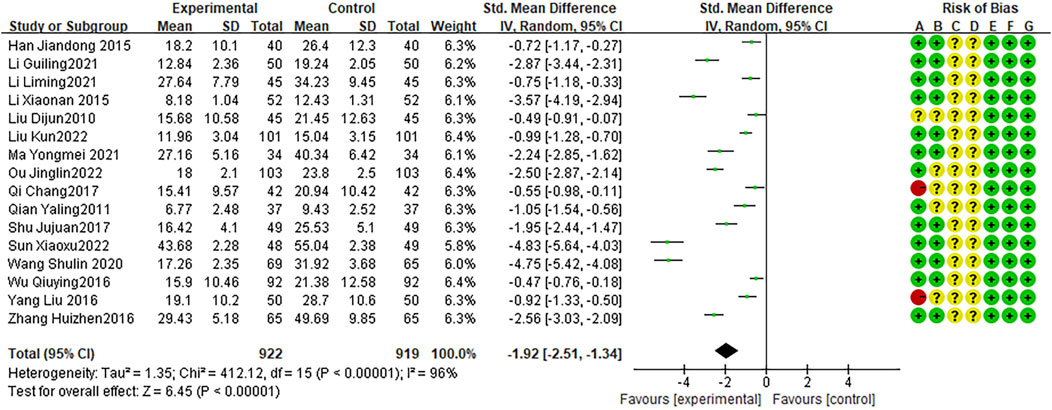
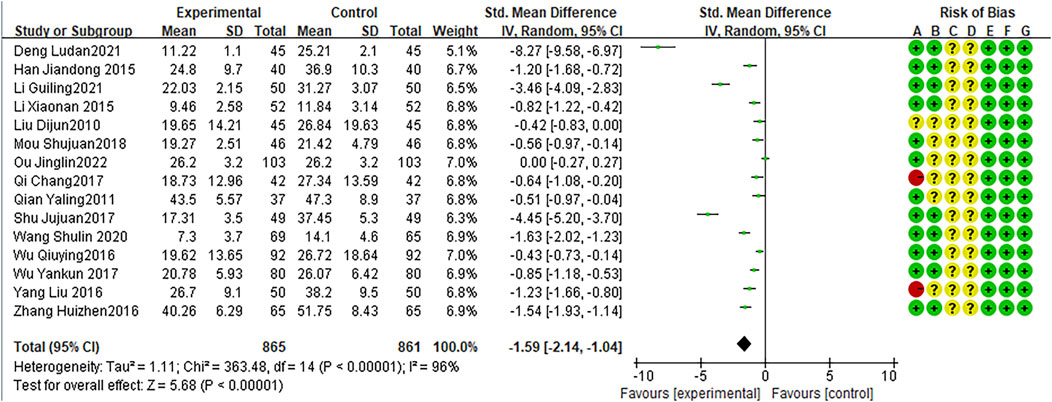
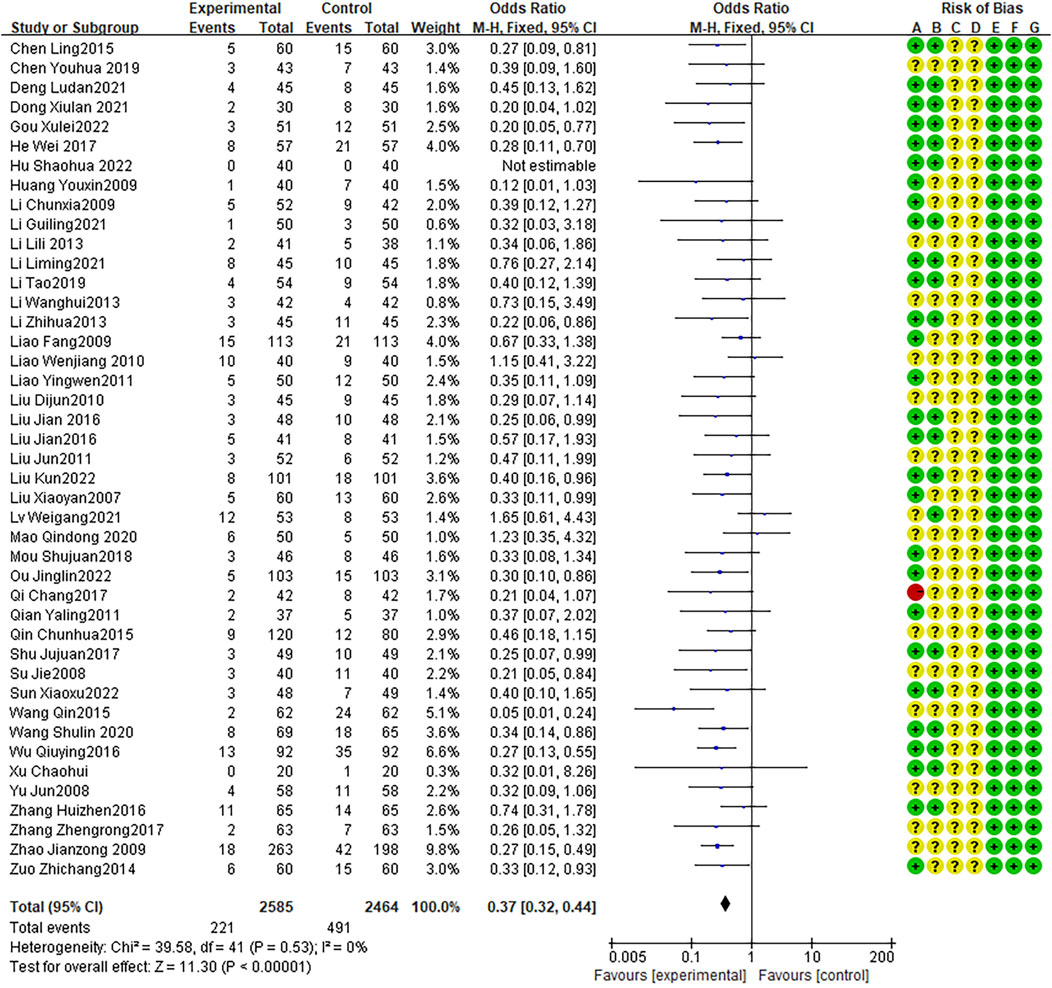
Result: A total of 51 RCTs involving 5,799 children aged 1–14 enrolled. Meta-analysis demonstrated that TCM combined with AZM improved the cure rate (odds ratio [OR] = 2.34, 95% CI: 2.06 to 2.64) and the effective rate (OR = 5.21, 95% CI: 4.22 to 6.43), shorted the disappearance duration of cough (WMD = −1.62, 95% CI: −1.90 to −1.34), the duration of fever (WMD = −1.62, 95% CI: −1.96 to −1.29), and the disappearance time of lung rales (WMD = −1.15, 95% CI: −1.32 to −0.98), improved CRP levels (WMD = −2.06, 95% CI: −2.57 to −1.55), IL-6 levels (WMD = −1.92,95% CI: −2.51 to −1.34), and TNF-α levels (WMD = −1.59, 95% CI: −2.14 to −1.04), and reduced adverse reactions (OR = 0.37, 95% CI: 0.32 to 0.44).
Conclusion: TCM combined with AZM in the treatment of MP among children has favorable clinical efficacy and safety.
Introduction
Mycoplasma pneumonia (MP) is common in children (Li et al., 2023), and its incidence rate has increased significantly in recent years, showing pandemic-level trends.
In traditional Chinese medicine (TCM), the occurrence of MP is associated with wind cold invading the lungs, phlegm heat obstructing the lungs, yin deficiency and lung dryness, and phlegm turbidity accumulation (Poddighe et al., 2022; Tsai et al., 2021). Various treatment methods have been adopted, such as relieving cough and reducing phlegm, strengthening the spleen and regulating qi, moistening dryness and resolving phlegm, nourishing yin and clearing the lungs, clearing heat, and detoxification, and are selected based on the pathway of occurrence (Koenen et al., 2023; Li et al., 2022). Clinical and related studies have shown that TCM has high cure and effective rates in treating MP, though treatment efficacy remains low in some patients (Liu et al., 2022; Ling, 2015; Liu, 2016; Wan et al., 2022). Azithromycin (AZM) is a first-line drug for the treatment of MP, although AZM shows good therapeutic effects, its efficacy is reduced over time, and some patients present gastrointestinal adverse reactions (Heidary et al., 2022). Previous studies found that the combination of TCM formulas and AZM can effectively improve the clinical symptoms in children and reduce adverse reactions (Wang et al., 2021; Zhang et al., 2021). However, existing studies have limited sample size and clinical translatability. Consequently, we performed a systematic evaluation and meta-analysis to evaluate the efficacy and safety of TCM combined with AZM in the treatment of pediatric MP, and provide an evidence-based outlook on its clinical applicability.
Methods
The study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2015).
Search strategy
Two reviewers independently searched seven databases including four Chinese databases such as China’s Knowledge Infrastructure (http://www.cnki.net,CNKI), the Chinese periodical service platform (http://www.cqvip.com,CQVIP), Wanfang knowledge service platform (http://www.wanfangdata.com,WF), China National Science and Technology Library and documentation center (http://www.nstl.cn,NSTL), and three English databases such as PubMed, Cochrane Library, and EMBASE.English. Following search terms: (“Traditional Chinese medicine” OR “TCM”) AND (“children” OR “pediatric”) AND (“Azithromycin”) AND (“mycoplasma pneumonia”) between January 1, 2000 and November 1, 2023. The detailed search strategies can be showed in Supplementary Table S1.
Eligibility
Inclusion criteria: 1) The research topic was MP; 2) subjects were aged ≤14 years; 3) study design was a randomized controlled trial; 4) clear reporting of no significant difference between the baseline data of the experimental and control groups; 5) intervention measures were TCM decoction combined with AZM sequential therapy, and symptomatic treatment was given; 6) control measure was AZM sequential therapy combined with symptomatic treatment; and 7) reporting of at least one clear efficacy indicator or adverse reaction observation.
Exclusion criteria: 1) duplicate published literature; 2) full-text literature unavailable; 3) missing results or obvious errors in the literature.
Literature quality assessment and data extraction
Two independent reviewers used the Cochrane risk-of-bias tool to assess the quality of the literature. Random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases were evaluated, and the risk of bias was determined as low, unclear,or high (Higgins et al., 2011). In case of disagreement, the outcome was determined after discussion with a third reviewer.
We designed a structured data extraction procedure to extract the first author, publication year, population of each group, patient characteristics, treatment measures, drug composition, and treatment results. The treatment outcomes included cure, effectiveness, fever disappearance time, cough disappearance time, pulmonary rales disappearance time, untoward reaction, and C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF- α) levels. “Cure” was defined as the disappearance of asthma, fever, cough, dry/wet lung rales and other post-treatment signs, and recovery in chest X-rays. “Effective” referred to a significant improvement in cough, asthma, fever, and dry/wet lung rales after treatment. Data extraction was performed by two independent reviewers, and any disagreements were resolved through discussion with the third reviewer.
Statistical analysis
We summarized the results of the included studies and calculated the sample size, mean, and standard deviation. For dichotomous variables, such as cure, effectiveness, and untoward reaction after treatment, we calculated the odds ratio (OR) with 95% confidence interval (CI). For continuous variables, such as fever disappearance time, cough disappearance time, CRP, and IL-6 levels, we calculated the mean difference (MD) with 95% CI. Review Manager 5.3 (The Cochrane Collaboration, London, UK) was used for analysis, and I2 was calculated to estimate heterogeneity. Generally, an I2 of 25% indicates low heterogeneity, 50% indicates moderate heterogeneity, and 75% indicates high heterogeneity (Higgins et al., 2011). If the heterogeneity of multiple studies is low (I2 < 25%), a fixed effect model is used, and if the heterogeneity is high (I2 ≥ 25%), a random effects model is used. We assessed the risk of publication bias using funnel plots.
Results
Systematic literature search results
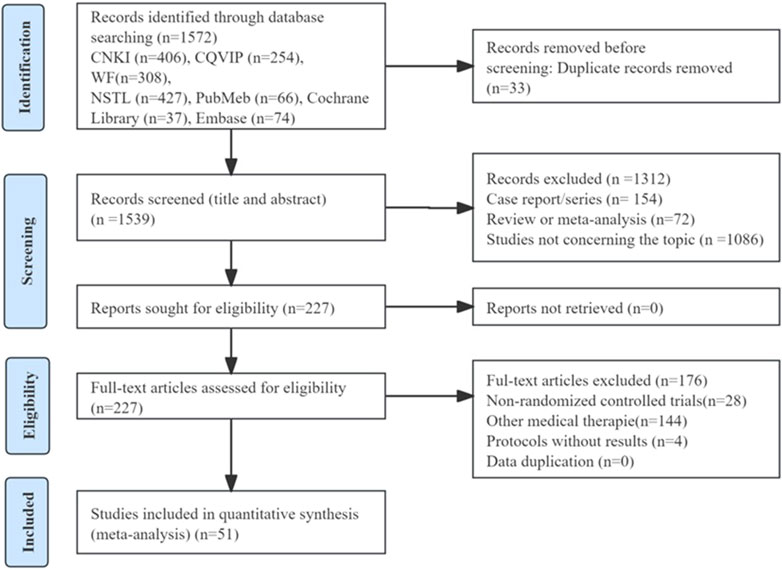
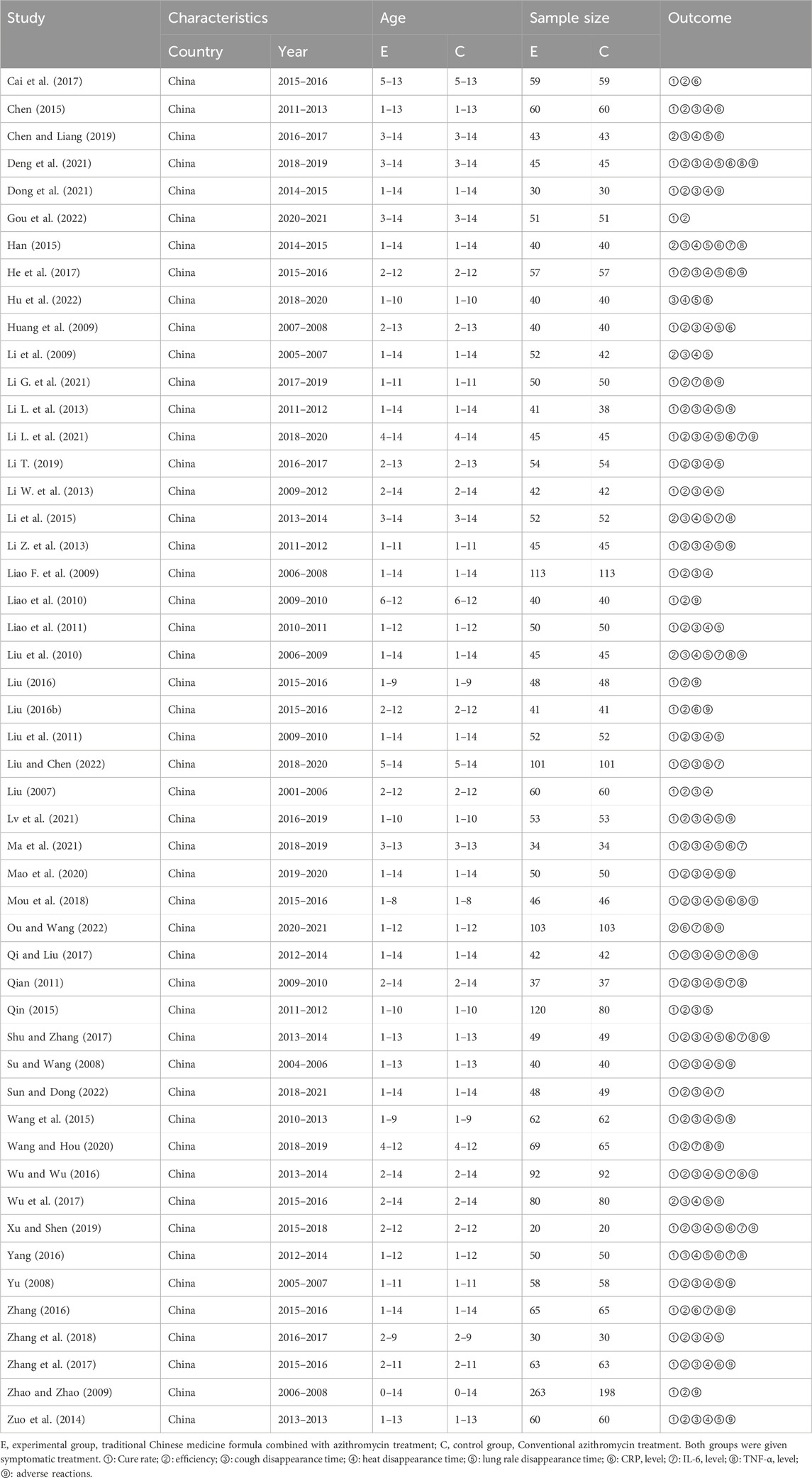
A total of 774 potentially relevant publications were searched by electronic searching approaches. After eliminating duplicates of 1,539 records were screened. Then after excluding abstracts, the titles, case report/series, and full text of 1,539 records, finally, we included 51 RCTs with 5,799 children for systematic evaluation and meta-analysis. The screening process was shown in Figure 1. Main characteristics of the RCTs were shown in Table 1.
Literature quality evaluation
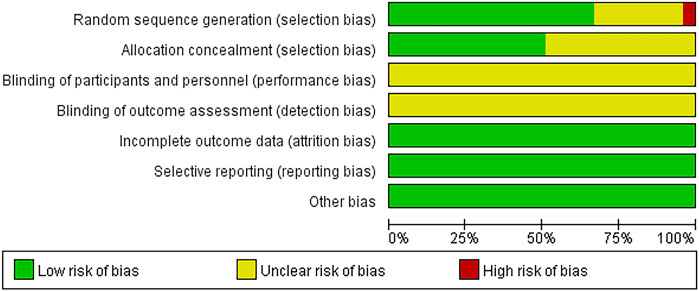
Among the 51 RCTs, 38 studies used the random number table method, 11 studies only mentioned random grouping without specifying specific methods, and 2 studies performed grouping according to the order of subject visits. None of the literature explicitly mentioned the blinding method of implementers and participants, or the blinding method used in outcome evaluation. All literature had complete outcome data, selective reporting of outcome indicators, or no other biases (Figure 2).
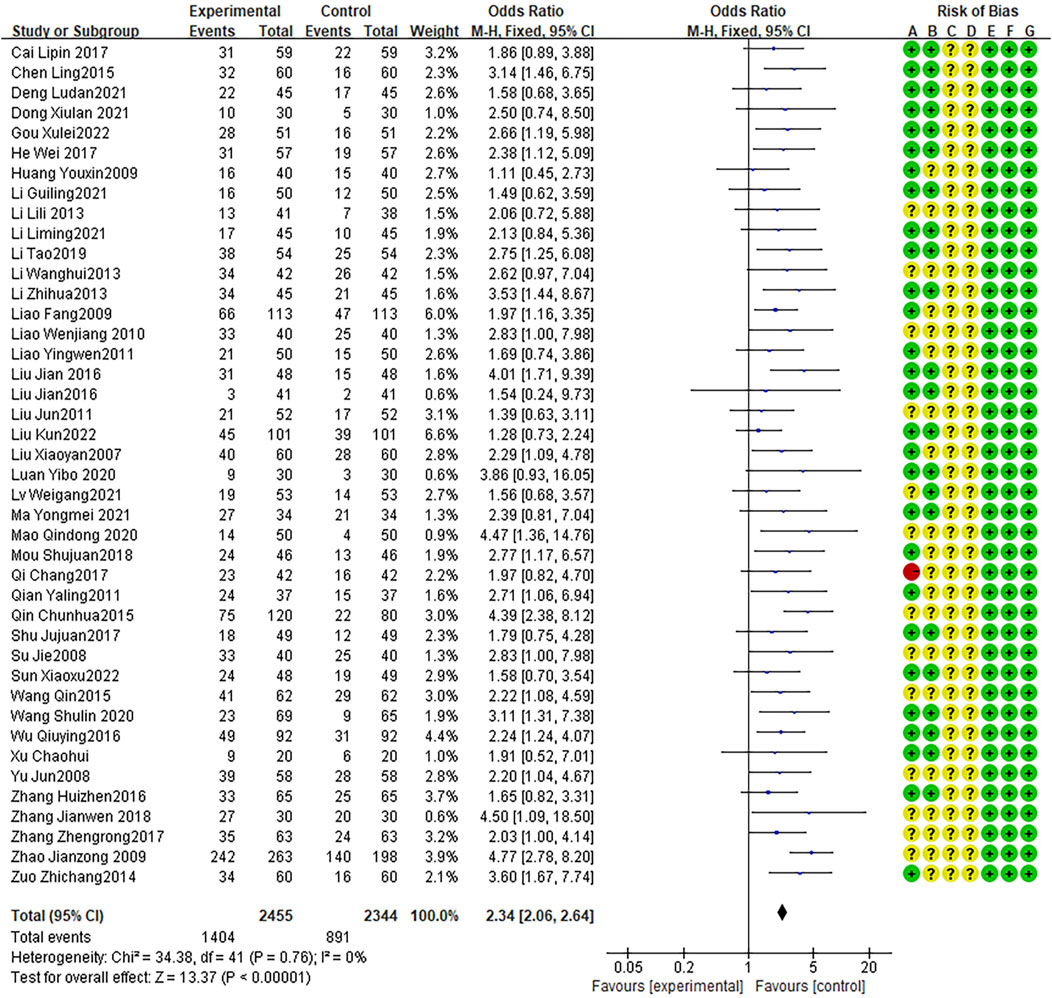
Treatment effect
Forty-two articles reported cure rates, with no heterogeneity between studies (I2 = 0%, P = 0.76). The fixed effects model indicated that the therapeutic effect of the combination therapy was better than that of AZM alone (OR = 2.34, 95% CI: 2.06 to 2.64, P < 0.0001; Figure 3). In addition, 49 RCTs reporting effective rates, with no heterogeneity between studies (I2 = 0%, P = 1.00). The fixed effects model indicated that the effective rate of the combination therapy was higher than that of the AZM treatment (OR = 5.21, 95% CI: 4.22 to 6.43, P < 0.0001; Figure 4).
Cough disappearance time
Forty RCTs reported cough disappearance time, with high heterogeneity between studies (I2 = 94%, P < 0.0001). The random effects model indicated that the average cough disappearance time was shorter with combination therapy than that with AZM therapy (WMD = −1.62, 95% CI: −1.90 to −1.34, P < 0.0001; Figure 5).
Duration of fever
Twenty-four RCTs presented the duration of fever, with high heterogeneity between studies (I2 = 95%, P < 0.0001). The random effects model indicated that the average duration of fever was shorter with combination therapy than that with AZM therapy (WMD = −1.62, 95% CI: −1.96 to −1.29, P < 0.0001; Figure 6).
Disappearance time of lung rales
Twenty-two RCTs presented the disappearance time of lung rales, with high heterogeneity among RCTs (I2 = 81%, P < 0.0001). The random effects model indicated that the average disappearance time of lung rales was shorter with combination therapy than that with AZM therapy (WMD = −1.15, 95% CI: −1.32 to −0.98, P < 0.0001; Figure 7).
Post-treatment CRP levels
Sixteen RCTs reported CRP levels after treatment, with high heterogeneity among studies (I2 = 94%, P < 0.0001). The random effects model indicated that the average CRP level after treatment was lower after combination therapy than that after AZM therapy (WMD = −2.06, 95% CI: −2.57 to −1.55, P < 0.0001; Figure 8).
Post-treatment IL-6 levels
Sixteen RCTs reported IL-6 levels after treatment, with high heterogeneity among studies (I2 = 96%, P < 0.0001). The random effects model indicated that the average IL-6 level in was lower after combination treatment than that after AZM treatment (WMD = −1.92,95% CI: −2.51 to −1.34, P < 0.0001; Figure 9).
Post-treatment TNF-α levels
Fifteen RCTs reported post-treatment TNF-α levels, with high heterogeneity between studies (I2 = 96%, P < 0.0001). The random effects model indicated that the average TNF-α level was lower after combination therapy than that after AZM therapy (WMD = −1.59, 95% CI: −2.14 to −1.04 P < 0.0001; Figure 10).
Adverse reactions
Forty-three RCTs demonstrated adverse reactions, with no heterogeneity between studies (I2 = 0%, P = 0.53). The fixed effects model indicated that the number of adverse reactions was lower with combination therapy than that with AZM therapy (OR = 0.37, 95% CI: 0.32 to 0.44, P < 0.0001; Figure 11).
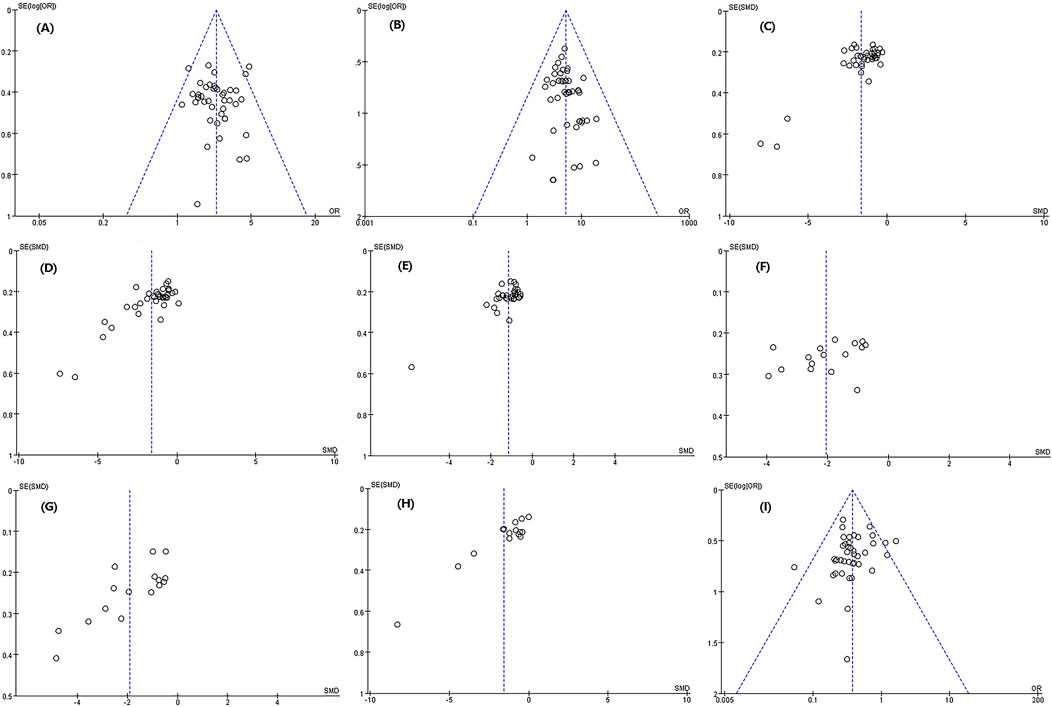
Publication bias
The publication bias between cure rate, effective rate, disappearance time of lung gong sounds, post-treatment CRP level, and incidence of adverse reactions was relatively small. There was a certain degree of publication bias in cough disappearance time, fever disappearance time, IL-6 level after treatment, and TNF-α level after treatment (Figure 12).
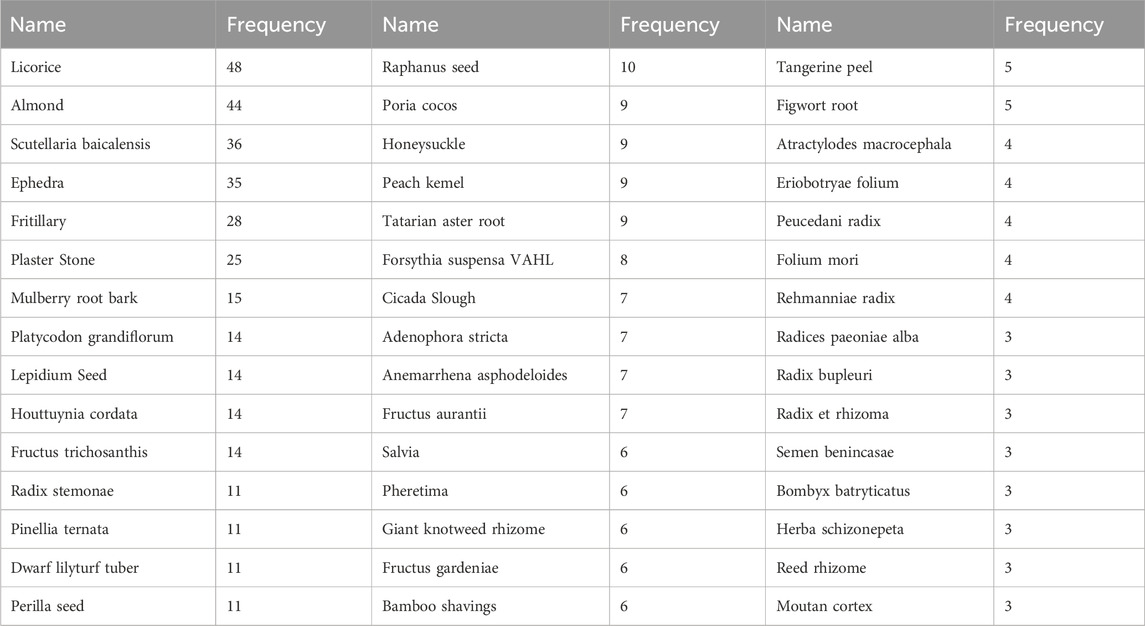
Usage of Chinese Medicinal materials
Among the 51 RCTs, a total of 115 Chinese medicinal herbs were used in the combination therapy. The top ten Chinese medicinal herbs with the highest frequency of use were Licorice, almond, Scutellaria baicalensis, Ephedra, Fritillaria, plaster stone, mulberry root bark, Platycodon grandiflorus, Lepidium seed, Houttuynia cordata, and Gualou. The statistical results of the main Chinese medicinal materials and their usage frequency are shown in Table 2.
Discussion
In this study, we conducted a meta-analysis and evaluation of 51 RCTs with 5,799 MP among children, the findings showed that TCM combined with AZM in fighting to pediatric MP had favorable efficacy and safety. We also found that the combination treatment can improve the cure and effective rates, shorten the disappearance time of cough, fever, and lung rales, and reduce CRP, IL-6, and TNF-α levels, representing an overall positive treatment effect in children with MP.
Previous meta-analyses on the treatment of pediatric MP with TCM combined with AZM mostly focused on the efficacy and safety of traditional Chinese patent medicines and simple preparations (He et al., 2020; Sun et al., 2020; Wei et al., 2020). To our knowledge, this is the first meta-analysis to evaluate the efficacy of various TCM combined with AZM in the treatment of pediatric MP. Although traditional Chinese patent medicines, simple preparations, and TCM are prescribed according to the etiology, pathogenesis, and clinical symptoms, there are some differences between traditional Chinese patent medicines/simple preparations and TCM. In traditional Chinese patent medicines and simple preparations, the ingredients are basically fixed, while the ingredients in TCM are adjusted according to patient symptoms for personalized targeted treatment (Zhang et al., 2021). Although the meta-analysis of traditional Chinese patent medicines and simple preparations combined with AZM in the treatment of pediatric MP can aid in clinical decision-making, it does not identify the most effective.
Chinese herbal formulas. Changes in the composition of TCM pose potential risks (Salmerón et al., 2021). In the 51 RCTs, some TCM ingredients were identified with potential safety effects, such as almonds, Scutellaria baicalensis, ephedra, Pinellia ternata, Tianlizi, and rhubarb, among others. Although these drugs may promote adverse reactions (Sun et al., 2020), we found that the combination of TCM and AZM did not correspond with an increase in adverse reactions—the incidence of adverse reactions was reduced compared with using AZM alone, and there were no cases of liver dysfunction. The reason is that all TCM ingredients are processed and produced, and the amount prescribed in treatment is relatively small. Therefore, adverse reactions are unlikely without excessive intake (Doan et al., 2020).
The main types of Chinese medicinal materials in the 51 RCTs were prescribed for lung clearing, phlegm resolving, cough relieving, heat clearing, and antiviral effects. These medicinal herbs contain active ingredients that can inhibit the production of the fever mediators PGE2 and GAMP, promote Th2 cell differentiation, increase anti-inflammatory factor levels, and regulate immune function, thereby enhancing physical function (Hart et al., 2022). The TCMs might play a role in accelerating symptom relief, promoting disease recovery, and reducing the gastrointestinal discomfort caused by AZM.
Our study has several limitations. Firstly, the selection of subjects was based on children admitted to hospitals where the investigators worked. The lack of multicenter research may promote bias in the selection of subjects. Secondly, some indicators had high heterogeneity such as CRP, IL-6, and TNF-a, which may be related to the inconsistent baseline data of each RCT, such as patient age, disease duration, and severity. In addition, the differences in TCM components and biochemical detection techniques used in different RCTs might also lead to high heterogeneity of the above indicators.
Conclusions
The combination of TCM and AZM in the treatment of pediatric MP could significantly improve the cure and effective rates, promote symptom relief, reduce the concentration of inflammatory factors, and reduce the occurrence of adverse reactions. It may be the best treatment choice for pediatric MP. More high-quality multicenter researches should need to be conducted in the future, and further confirm the findings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
JnL: Conceptualization, Writing–original draft, Writing–review and editing. FF: Conceptualization, Writing–original draft, Writing–review and editing. JiL: Data curation, Writing–original draft. QW: Data curation, Writing–original draft. XT: Data curation, Writing–original draft. JX: Formal Analysis, Writing–original draft. SZ: Data curation, Formal Analysis, Writing–original draft. BW: Funding acquisition, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study was supported by high Level Chinese Medical Hospital Promotion Project (HLCMHPP2023093; HLCMHPP2023021; No. ZZ17-XRZ-043).
Acknowledgments
We would like to thank all the members in the present study, and we also thank Prof. Yan Ma from China Academy of Chinese Medical Sciences, and Prof. Fei Huang from Chinese Center for Disease Control and Prevention for language editing of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1431706/full#supplementary-material
References
Cai, L., Song, H., and Wang, B. (2017). Qingfei antispasmodic method combined with azithromycin for the treatment of 59 children with mycoplasma pneumonia. Glob. Tradit. Chin. Med. 10 (6), 653–655. doi:10.3969/j.issn.1674-1749.2017.06.034
Chen, L. (2015). Observations on the efficacy of the treatment of paediatric Mycoplasma pneumoniae with the addition and subtraction of Ma Xing Shi Gan Tang. Shaanxi J. Traditional Chin. Med. 36 (12), 1586–1587. doi:10.3969/j.issn.1000-7369.2015.12.008
Chen, Y., and Liang, J. (2019). Azithromycin combined with modified wuhu decoction orally and xiaohuang san in the the treatment of mycoplasma pneumonia in children. Jilin J. Chin. Med. 39 (1), 60–63. doi:10.13463/j.cnki.jlzyy.2019.01.017
Deng, L., Li, Y., Zhao, C., Song, P., and Wang, M. Q. (2021). Observation on the clinical efficacy of azithromycin sequential therapy combined with wuhu decoction in the treatment of mycoplasma pneumonia in children. World J. Integr. Traditional West. Med. 1 (16), 7–11. doi:10.13935/j.cnki.sjzx.210102
Doan, T., Worden, L., Hinterwirth, A., Arzika, A. M., Maliki, R., Abdou, A., et al. (2020). Macrolide and nonmacrolide resistance with mass azithromycin distribution. N. Engl. J. Med. 383, 1941–1950. doi:10.1056/NEJMoa2002606
Dong, X., Xu, H., Zhang, X., Liu, H., Ye, J. Y., and Chen, Y. B. (2021). Effect of modified jiawei wuhu decoction on clinical curative effect and T cell subsets in children with mycoplasma pneumonia. World Chin. Med. 16 (3), 458–462. doi:10.3969/j.issn.1673-7202.2021.03.017
Gou, X., Wei, L., Zhang, Z., and Zhang, L. (2022). Observation on the effect of Qingfei Yin combined with azithromycin on children with mycoplasma pneumoniae pneumonia (syndrome of phlegm-heat blocking the lung). Jilin J. Chin. Med. 42 (8), 913–916. doi:10.13463/j.cnki.jlzyy.2022-08.012
Han, J. (2015). Effects of Chinese medicine combined with azithromycin on children of mycoplasma pneumonia and their serum inflammatory factors. West. J. Traditional Chin. Med. 28 (3), 121–123. doi:10.3969/j.issn.1004-6852.2015.03.039
Hart, J. D., Samikwa, L., Meleke, H., Burr, S. E., Cornick, J., Kalua, K., et al. (2022). Prevalence of nasopharyngeal Streptococcus pneumoniae carriage and resistance to macrolides in the setting of azithromycin mass drug administration: analysis from a cluster-randomised controlled trial in Malawi, 2015-17. Lancet Microbe 3, e142–e150. doi:10.1016/S2666-5247(21)00279-2
He, H., Wang, X., Xiao, Y., Zheng, J., Wang, J., and Zhang, B. (2020). Comparative efficacy and safety of traditional Chinese patent medicine in the treatment of Mycoplasma pneumoniae pneumonia in children: a protocol for systematic review and meta-analysis. Med. Baltim. 99, e23747. doi:10.1097/MD.0000000000023747
He, W., Huang, W., and Zeng, W. (2017). Clinical application of azithromycin combined with traditional Chinese medicine syndrome differentiation in the treatment of children with mycoplasma pneumonia. J. Liaoning Univ. Traditional Chin. Med. 19 (7), 195–197. doi:10.13194/j.issn.1673-842x.2017.07.053
Heidary, M., Ebrahimi Samangani, A., Kargari, A., Kiani Nejad, A., Yashmi, I., Motahar, M., et al. (2022). Mechanism of action, resistance, synergism, and clinical implications of azithromycin. J. Clin. Lab. Anal. 36, e24427. doi:10.1002/jcla.24427
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928. doi:10.1136/bmj.d5928
Hu, S. H., Shi, J., and Wang, J. (2022). Curative effect of modified Sangxing Decoction combined with azithromycin on mycoplasma pneumonia infection in children. Northwest Pharm. J. 37 (2), 140–143. doi:10.3969/j.issn.1004-2407.2022.02.027
Huang, Y., Wang, J., and Peng, J. (2009). Observation on the therapeutic effect of integrated traditional Chinese and Western medicine in the treatment of pediatric mycoplasma pneumonia. Guid. J. Traditional Chin. Med. Pharm. 15 (2), 45–46. doi:10.3969/j.issn.1672-951X.2009.02.021
Koenen, M. H., de Groot, R. C. A., de Steenhuijsen Piters, W. A. A., Chu, M. L. J. N., Arp, K., Hasrat, R., et al. (2023). Mycoplasma pneumoniae carriage in children with recurrent respiratory tract infections is associated with a less diverse and altered microbiota. EBioMedicine 98, 104868. doi:10.1016/j.ebiom.2023.104868
Li, C., Fang, H., Wang, J., and Wang, Y. T. (2009). Clinical observation on the integrated Chinese traditional and westem medicine in 94 cases of mycoplasmal pneumonia in children. Occup. Health J. 25 (10), 1101–1102. doi:10.13329/j.cnki.zyyjk.2009.10.051
Li, G., Zheng, T., and Li, L. (2021). Clinical observation and analysis of maxing shigan decoction(maxing shigan decoction) combined with azithromycin in treatment of pediatric mycoplasma pneumonia. Chin. J. Traditional Chin. Med. 39 (09), 73–75. doi:10.13193/j.issn.1673-7717.2021.09.019
Li, J., Luu, L. D. W., Wang, X., Cui, X., Huang, X., Fu, J., et al. (2022). Metabolomic analysis reveals potential biomarkers and the underlying pathogenesis involved in Mycoplasma pneumoniae pneumonia. Emerg. Microbes Infect. 11, 593–605. doi:10.1080/22221751.2022.2036582
Li, L., Liu, W., Chen, H., and Gong, S. Q. (2013). Analysis on advantages and long - term effect of integrated traditional Chinese and western medicine on treating children mycoplasma pneumonia. Liaoning J. Traditional Chin. Med. 40 (10), 3. doi:10.13192/j.issn.1000-1719.2013.10.072
Li, L., Wang, Y., and Xu, Z. (2021). Efficacy and safety of Qingfei Tongfu Xietan Decoction combined with azithromycin in the treatment of mycoplasma pneumonia complicated with atelectasis of type of phlegm-heat congesting the lung. J. Mod. Integr. Chin. West. Med. 30 (14), 1516–1520. doi:10.3969/j.issn.1008-8849.2021.14.008
Li, T. (2019). Clinical study of TCM syndrome differentiation combined with azithromycin in the treatment of mycoplasma pneumonia in children. Clin. J. Chin. Med. 11 (15), 51–52. doi:10.3969/j.issn.1674-7860.2019.15.021
Li, W., Xu, X., Song, L., and Qiang, R. X. (2013). Treatment of 42 cases of pediatric mycoplasma pneumonia with the method of clearing the lungs, resolving phlegm, and unblocking collaterals. Shaanxi J. Traditional Chin. Med. 34 (007), 787–788. doi:10.3969/j.issn.1000-7369.2013.07.013
Li, X., Li, T., Chen, N., Kang, P., and Yang, J. (2023). Changes of Mycoplasma pneumoniae prevalence in children before and after COVID-19 pandemic in Henan, China. J. Infect. 86, 256–308. doi:10.1016/j.jinf.2022.12.030
Li, X. L., Li, X. J., and Lu, J. (2015). Clinical analysis of azithromycin combined Qibaiqingfei pill in treatment of children mycoplasma pneumoniae infection. Chin. J. Difficult Complicat. Cases (11), 1169–1172. doi:10.3969/j.issn.1671-6450.2015.11.022
Li, Z., Xiong, Y., and Zhang, H. (2013). Observation of efficacy of Chinese and western medicine in the treatment of infantile mycoplasma pneumonia. Acta Chin. Med. 28 (7), 2. doi:10.16368/j.issn.1674-8999.2013.07.062
Liao, F., Zheng, D., Yu, G., and Zhou, W. (2009). Clinical observation of integrated traditional Chinese and Western medicine in the treatment of pediatric mycoplasma pneumonia. China Med. Her. 6 (3), 60–61. doi:10.3969/j.issn.1673-7210.2009.03.040
Liao, W., Huang, T., Yuan, A., Meng, Y., Fu, X., and He, J. (2010). Traditional Chinese medicine combined with azithomycin in the treatment of mycoplasma pneumoniae pneumonia in chlidren. Hainan Med. J. 21 (20), 40–41. doi:10.3969/j.issn.1003-6350.2010.20.017
Liao, Y., Chen, N., and Wu, Z. (2011). Clinical observation of 50 cases of pediatric mycoplasma pneumonia treated with modified Ma Xing Shi Gan Tang. Guid. J. Traditional Chin. Med. Pharm. 17 (11), 51–52. doi:10.3969/j.issn.1672-951X.2011.11.021
Ling, C. (2015). Observation on the therapeutic effect of modified ma xing shi Gan tang on mycoplasma pneumoniae in children. Shaanxi J. Traditional Chin. Med. 36 (12), 1586–1587. doi:10.3969/j.issn.1000-7369-2015.12.008
Liu, D., Zheng, B., Cai, B., Zhou, W. M., and Yu, B. X. (2010). Traditional Chinese and Western medicine treatment of mycoplasmal pneumonia in children and the serum cytokine changes. J. South. Med. Univ. 30 (3), 626–627. doi:10.12122/j.issn.1673-4254.2010.03.064
Liu, J. (2016). Observation on the therapeutic effect of Qingfei Zhishi Huoxue Fang combined with Azithromycin in the treatment of phlegm heat closed lung syndrome in children with Mycoplasma pneumonia. Shaanxi J. Traditional Chin. Med. 37 (8), 1035–1037. doi:10.3969/j.issn.1000-7369.2016.08.046
Liu, J. (2016). The therapeutic effect of Jiawei Wuhu Tang on children with phlegm heat closed lung type Mycoplasma pneumonia and the regulatory effect of T lymphocyte subsets and cytokines. Shaanxi J. Traditional Chin. Med. 37 (10), 1307–1309. doi:10.3969/j.issn.1000-7369.2016.10.017
Liu, J., Wu, R., and Feng, B. (2011). Yin Qiao Qin Bai Tang combined with azithromycin in the treatment of 52 cases of pediatric mycoplasma pneumonia. Shaanxi J. Traditional Chin. Med. 32 (9), 1155–1157. doi:10.3969/j.issn.1000-7369.2011-09.037
Liu, K., and Chen, C. (2022). Effect of modified sangju decoctionon chronic cough after mycoplasma pneumoniae infection in children. World J. Integr. Traditional West. Med. 17 (9). doi:10.13935/j.cnki.sjzx.220923
Liu, X. (2007). Qingfei Zhenke Tang combined with antibiotics for the treatment of 60 cases of pediatric mycoplasma pneumonia. Shaanxi J. Traditional Chin. Med. 28 (10), 1346–1347. doi:10.3969/j.issn.1000-7369.2007.10.052
Liu, X., Wang, M., Kan, Q., Lin, Y., and Jiang, Z. (2022). Qingfei tongluo formula mitigates mycoplasma pneumoniae infection via the PERK signaling pathway. Dis. Markers 2022, 9340353. doi:10.1155/2022/9340353
Lv, W., Zhang, Y., Song, G., Guan, Z. W., Yu, S. P., Guo, Y. R., et al. (2021). Effect of modified qianjin weijing decoction combined with azithromycin on mycoplasma pneumonia in children with phlegm heat obstructing fei and blood stasis syndrome. Chin. J. Integr. Traditional West. Med. 41 (10), 1192–1196. doi:10.7661/j.cjim.20210902-211
Ma, Y., Ren, X., Ma, C. H., and Mu, Y. N. (2021). Clinical efficacy observation of azithromycin combined with Chinese medicine immune-enhancing formulae in the treatment of mycoplasma pneumoniae infection in children. J. Guangzhou Univ. Traditional Chin. Med. 38 (7), 1351–1356. doi:10.13359/j.cnki.gzxbtcm.2021.07.010
Mao, Qi., Gu, M., Pan, B., and Chen, Q. F. (2020). Observation on the curative effect of maxingshigan decoction combined with azithromycin in the treatment of wheezing of InFantile pneumonia. Res. Pract. Chin. Med. 34 (3), 4. doi:10.13728/j.1673-6427.2020.03.015
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1. doi:10.1186/2046-4053-4-1
Mou, S., Sun, S., and Shen, H. (2018). The effect of Ma Xing Shi Gan Tang combined with Su Ting Ding Chuan Wan on symptom relief and serum factor levels of Mycoplasma pneumonia in children with phlegm heat closed lung syndrome. Glob. Tradit. Chin. Med. 11 (11), 1809–1812. doi:10.3969/j.issn.1674-1749.2018.11.051
Ou, J., and Wang, W. (2022). Clinical efficacy of Xuanfei Zhike Tang combined with azithromycin in the treatment of pediatric mycoplasma pneumonia and its impact on inflammatory indicators. Shanxi Med. J. 51 (13), 1475–1477. doi:10.3969/j.issn.0253-9926.2022.13.010
Poddighe, D., Demirkaya, E., Sazonov, V., and Romano, M. (2022). Mycoplasma pneumoniae infections and primary immune deficiencies. Int. J. Clin. Pract. 2022, 6343818. doi:10.1155/2022/6343818
Qi, C., and Liu, X. (2017). Clinical analysis of the efficacy of Chinese herbs combined with azithromycin anti-mycoplasma infection of mycoplasma pneumonia in children. J. Basic Chin. Med. 23 (11), 1590–1592. doi:10.19945/j.cnki.issn.1006-3250.2017.11.033
Qian, Y. (2011). Integrated traditional Chinese and Western medicine for the treatment of refractory Mycoplasma pneumoniae pneumonia in children. Chin. J. Exp. Traditional Med. Formulae 17 (21), 268–270. doi:10.13422/j.cnki.syfjx.2011.21.082
Qin, C. (2015). The effect of combining traditional Chinese and Western medicine on the treatment of pulmonary fever and cough after Mycoplasma pneumoniae infection in children. J. Clin. Med. Pract. 19 (3), 149–150. doi:10.7619/jcmp.201503052
Salmerón, P., Moreno-Mingorance, A., Trejo, J., Amado, R., Viñado, B., Cornejo-Sanchez, T., et al. (2021). Emergence and dissemination of three mild outbreaks of Neisseria gonorrhoeae with high-level resistance to azithromycin in Barcelona, 2016-18. J. Antimicrob. Chemother. 76, 930–935. doi:10.1093/jac/dkaa536
Shu, J., and Zhang, X. (2017). Clinical effect study on bronchitis in infantile pneumonia mycoplasma infection treated with the therapy for clearing heat and resolving phlegm and azithromycin. World J. Integr. Traditional West. Med. 12 (02), 226–229. doi:10.13935/j.cnki.sjzx.170222
Su, J., and Wang, Y. (2008). Observation on 40 cases of children mycoplasmal pneumonia treated by TCM and WM combined in clinic. Liaoning J. Traditional Chin. Med. 35 (8), 1210–1211. doi:10.3969/j.issn.1000-1719.2008.08.053
Sun, J. H., Sun, F., Yan, B., Li, J. Y., and Xin, D. L. (2020). Data mining and systematic pharmacology to reveal the mechanisms of traditional Chinese medicine in Mycoplasma pneumoniae pneumonia treatment. Biomed. Pharmacother. 125, 109900. doi:10.1016/j.biopha.2020.109900
Sun, X., and Dong, Y. (2022). Modified qianjin weijing decoction in treatment of mycoplasma pneumonia with wind-heat closed lung syndrome in children. Acta Chin. Med. 37 (06), 1326–1330. doi:10.16368/j.issn.1674-8999.2022.06.240
Tsai, T. A., Tsai, C. K., Kuo, K. C., and Yu, H. R. (2021). Rational stepwise approach for Mycoplasma pneumoniae pneumonia in children. J. Microbiol. Immunol. Infect. 54, 557–565. doi:10.1016/j.jmii.2020.10.002
Wan, R., Jia, M., Dou, H., Tu, P., Shi, D., Yuan, Q., et al. (2022). Mechanism of infantile feire kechuan oral solution against mycoplasma pneumoniae infection of A549 cells. Biomed. Pharmacother. 145, 112366. doi:10.1016/j.biopha.2021.112366
Wang, M., Li, H., Yang, J., Wang, M., and Liu, J. (2021). Clinical efficacy enhancement of a Chinese herbal injection in the treatment of mycoplasma pneumonia in children: a protocol of randomized controlled trial. Med. Baltim. 100, e25135. doi:10.1097/MD.0000000000025135
Wang, Q., Zhu, S., Zhao, Y., and Wang, H. (2015). Treatment of intractable pediatric mycoplasma pneumonia by qingfei huoxue recipe combined azithromycin: a random parallel control study. Chin. J. Integr. Traditional West. Med. 35 (5), 545–548. doi:10.7661/CJIM.2015.05.0545
Wang, S., and Hou, J. (2020). Clinical effects of Modified Qingjin Jianghuo Decoction combined with azithromycin on patients with pediatric mycoplasma pneumoniae pneumonia due to Phlegm-Dampness Accumulation. Chin. Tradit. Pat. Med. 42 (4), 908–912. doi:10.3969/j.issn.1001-1528.2020.04.016
Wei, L., Guo, Y., Fei, Y., Luo, L., Wang, C., Wang, X., et al. (2020). A randomized, double-blind, placebo-controlled, multicenter clinical trial for efficacy and safety of traditional Chinese medicine combined with antibiotics in the treatment of bacterial pneumonia in children. Med. Baltim. 99, e23217. doi:10.1097/MD.0000000000023217
Wu, Q., and Wu, Y. (2016). Azithromycin combined with traditional Chinese medicine treatment of pediatric mycoplasma pneumoniae pneumonia. Chin. J. Integr. Traditional West. Med. 34 (03), 754–757. doi:10.13193/j.issn.1673-7717.2016.03.072
Wu, Y., Liu, Q., and Ma, X. (2017). Clinical study on the effect of oral and acupoint application of traditional Chinese medicine combined with azithromycin for the children with mycoplasma pneumonia. Int. J. Traditional Chin. Med. 39 (2), 124–127. doi:10.3760/cma.j.issn.1673-4246.2017.02.008
Xu, C., and Shen, R. (2019). Comparative study on maxing shigan decoction combined with azithromycin on serum C-reactive protein in children with mycoplasma pneumoniae pneumonia and its clinical efficacy. World Chin. Med. 14 (12), 3257–3259. doi:10.3969/j.issn.1673-7202.2019.12.034
Yang, L. (2016). Effects of Chinese medicine combined with azithromycin on children with mycoplasma pneumonia and their serum inflammatory factors. Int. Med. Health Guid. News 22 (4), 535–536. doi:10.3760/cma.j.issn.1007-1245.2016.04.031
Yu, J. (2008). Clinical observation on the treatment of 58 cases of mycoplasma pneumonia in children with self drafted qingzhi tang combined with azithromycin. Guid. J. Traditional Chin. Med. Pharmacol. 14 (02), 23–24. doi:10.3969/j.issn.1672-951X.2008.02.011
Zhang, H. (2016). Clinical study on combination of Chinese and western medicine in the treatment of mycoplasma pneumonia in children. Acta Chin. Med. 31 (10), 1623–1624. doi:10.16368/j.issn.1674-8999.2016.10.415
Zhang, H., Li, X., Wang, J., Cheng, Q., Shang, Y., and Wang, G. (2021). Baicalin relieves Mycoplasma pneumoniae infection-induced lung injury through regulating microRNA-221 to inhibit the TLR4/NF-κB signaling pathway. Mol. Med. Rep. 24, 571. doi:10.3892/mmr.2021.12210
Zhang, J., Xiang, L., Gui, J., Xu, Z. H., Fei, W. J., and Shang, L. L. (2018). Clinical effect of modified sangju decoction combined with azithromycin in treatment of children with wind-heat cough caused by mycoplasma pneumoni-ae infection. J. Anhui Univ. Chin. Med. 37 (5), 19–21. doi:10.3969/j.issn.2095-7246.2018.05.006
Zhang, Z., Xing, G., and Zhao, Y. (2017). Observation on the therapeutic effect of modified Shansan Tang on Mycoplasma pneumoniae infection in children. Shaanxi J. Traditional Chin. Med. 38 (10), 1356–1357. doi:10.3969/j.issn.1000-7369.2017.10.018
Zhao, J., and Zhao, Y. (2009). Clinical study on treatment of mycoplasma pneumonia with XinLiang QingFei tang a report of 263 cases. West. J. Traditional Chin. Med. 22 (9), 23–24. doi:10.3969/j.issn.1004-6852.2009.09.015
Keywords: Mycoplasma pneumonia, children, traditional Chinese medicine formula, azithromycin, meta-analysis, randomized controlled trial
Citation: Lyu J, Fan F, Li J, Wang Q, Tian X, Xu J, Zhang S and Wang B (2024) Efficacy and safety of traditional Chinese medicine combined with azithromycin sequential therapy for mycoplasma pneumonia among children: a meta-analysis of randomized controlled trials. Front. Pharmacol. 15:1431706. doi: 10.3389/fphar.2024.1431706
Received: 12 May 2024; Accepted: 30 September 2024;
Published: 17 October 2024.
Edited by:
Dongshan Zhu, Shandong University, ChinaReviewed by:
Yuntao Liu, Guangzhou University of Chinese Medicine, ChinaFei Huang, Chinese Center For Disease Control and Prevention, China
Copyright © 2024 Lyu, Fan, Li, Wang, Tian, Xu, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Wang, ZXJrZXdhbmdib0AxNjMuY29t
 Jing Lyu
Jing Lyu Fei Fan
Fei Fan Ji Li
Ji Li Qiong Wang
Qiong Wang