- 1Department of Anesthesiology, Qilu Hospital of Shandong University, Jinan, China
- 2Department of Anesthesiology, Qilu Hospital (Qingdao), Cheeloo College of Medicine, Shandong University, Qingdao, China
Background: Postoperative nausea and vomiting (PONV) is a common complication, that can reduce patient satisfaction and may lead to serious consequences, such as wound dehiscence. Many strategies have been proposed to prevent PONV; however, it remains common, especially in high-risk surgeries such as gynecological surgery. In recent years, opioid-free anesthesia has been widely studied because it minimizes adverse reactions of opioids, such as nausea, vomiting, and itching; however, conclusions have been inconsistent. Therefore, we conducted this meta-analysis to investigate the effects of opioid-free anesthesia on PONV in patients undergoing gynecological surgery.
Methods: A systematic search of the PubMed, Web of Science, Cochrane Library, and Embase databases, from inception to 28 August 2023, was performed. Keywords and other free terms were used with Boolean operators (OR and, AND) to combine searches. This review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Results: Six studies involving 514 patients who underwent gynecological surgery were included. The forest plot revealed that the incidence of PONV (risk ratio = 0.52; p < 0.00001) and consumption of postoperative antiemetics use (risk ratio = 0.64; p = 0.03) were significantly lower in the opioid-free anesthesia group. In addition, opioid-free anesthesia improved the quality of recovery (mean difference = 4.69; p < 0.0001). However, there were no significant differences in postoperative pain scores (mean difference = 0.05; p = 0.85), analgesic use (risk ratio = 1.09; p = 0.65), and the time of extubation (mean difference = −0.89; p = 0.09) between the opioid-free anesthesia and control groups.
Conclusion: OFA reduces PONV and the use of antiemetic drugs. In addition, it improves the quality of postoperative recovery. However, OFA can not reduce the postoperative pain scores, analgesic use and the time of extubation. Due to the strength of the evidence, we cannot support OFA as an ideal anesthesia method in gynecological surgery, and the implementation of anesthesia strategies should be case-by-case.
Systematic Review Registration: [https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=462044], identifier [CRD42023462044]
Introduction
As an important part of general anesthesia, opioids exert a strong intraoperative anti-nociceptive stimulus and analgesic effect, and ensure stable vital signs in patients undergoing surgical procedures (Shinoda et al., 2013; Adams et al., 2023). However, improper use of opioids can also cause many adverse reactions such as postoperative nausea and vomiting (PONV), hyperalgesia, respiratory depression, and inflammatory responses, which prolong the length of postoperative hospital stay and increases medical costs (Macintyre et al., 2022). Moreover, opioid use for postoperative analgesia can lead to opioid addiction and abuse (Vadivelu et al., 2018). The incidence of PONV in patients undergoing gynecological surgery involving opioids is 50%–80%, and patients often experience postoperative hypoxemia and bradycardia due to opioid residue (Madej and Simpson, 1986; Zorrilla-Vaca et al., 2022).
With the emerging concept of enhanced recovery after surgery, opioid-free anesthesia (OFA) has been gradually introduced in an increasing number of surgeries (Moningi et al., 2019). OFA is a multimodal anesthesia method, which combines multiple drugs or methods such as sedatives, N-methyl-D-aspartate receptor antagonists, local anesthetics, anti-inflammatory drugs and α2 receptor agonists to enhance intraoperative analgesia and minimize the use of opioids during the perioperative period. Elkassabany et al. defines OFA as a perioperative treatment strategy from admission to discharge, that is, to perform anesthesia and analgesia in a non-opioid mode as far as possible, and reserve opioids for pain that cannot be relieved by other methods (Elkassabany and Mariano, 2019). Forget et al. believes that OFA can be defined as a combination of different opioid-sparing techniques to achieve opioid-free anesthesia (Forget, 2021). Mulier et al. distinguishes OFA from opioid-free analgesia, and believes that OFA means that opioids are not used before or during surgery until the patient is awake (Mulier and Dekock, 2017). It can reduce the risk for common opioid-related adverse reactions, such as postoperative respiratory depression, and PONV, and reduce the potential for dependence and addiction of patients to opioids (Feenstra et al., 2023). OFA has been widely used in bariatric and thoracic surgeries, and ideal results have been obtained (Selim et al., 2022; Mieszczański et al., 2023).
We conducted this systematic review and meta-analysis to compare and summarize postoperative outcomes, including PONV, antiemetic use, pain scores, and analgesic use, time of extubation and QoR-40 score between OFA and opioid-based anesthesia in gynecological surgery.
Methods
This review was performed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic review (Page et al., 2021). This systematic review and meta-analysis were included in PROSPERO (registration number: CRD42023462044).
Search strategy
The PubMed, Web of Science, Cochrane Library, and Embase databases were systematically searched from inception to 28 August 2023, for relevant studies published in English. The search terms used were as follows: ((opioid free [Title/Abstract]) OR (opioid-free [Title/Abstract])) AND ((“Gynecologic Surgical Procedures" [Mesh]) OR (((((((((((((((((((Procedures, Gynecologic Surgical [Title/Abstract]) OR (Surgical Procedure, Gynecologic [Title/Abstract])) OR (Surgery, Gynecological [Title/Abstract])) OR (Gynecological Surgeries [Title/Abstract])) OR (Gynecological Surgery [Title/Abstract])) OR (Surgeries, Gynecological [Title/Abstract])) OR (Gynecologic Surgical Procedure [Title/Abstract])) OR (Surgical Procedures, Gynecologic [Title/Abstract])) OR (Gynecological Surgical Procedure [Title/Abstract])) OR (Gynecological Surgical Procedures [Title/Abstract])) OR (Procedure, Gynecological Surgical [Title/Abstract])) OR (Procedures, Gynecological Surgical [Title/Abstract])) OR (Surgical Procedure, Gynecological [Title/Abstract])) OR (Surgical Procedures, Gynecological [Title/Abstract])) OR (Procedure, Gynecologic Surgical [Title/Abstract])) OR (Gynecologic Surgery [Title/Abstract])) OR (Gynecologic Surgeries [Title/Abstract])) OR (Surgeries, Gynecologic [Title/Abstract])) OR (Surgery, Gynecologic [Title/Abstract])))
All retrieved citations were downloaded and imported into a reference management tool (EndNote, Clarivate, London, United Kingdom) (Bramer et al., 2017). Duplicate studies were eliminated, titles and abstracts were reviewed to exclude studies that did not meet the inclusion criteria, and the remaining articles were analyzed and further screened according to the inclusion and exclusion criteria.
Selection criteria
The inclusion criteria were developed based on the “PICOS” principle: Patients, those underwent gynecological surgery or examination; Intervention, opioid-free anesthesia; Comparison, opioid-based anesthesia; Outcomes, incidence of the opioid-free anesthesia group and the control group; and Study design, randomized controlled trial.
Studies with no available or incomplete data, meta-analysis, systematic reviews, or retrospective studies, and those addressing pediatric or emergency surgery were excluded.
Data collection and assessment of risk of bias
Two researchers independently extracted and collected the following information: ZZ extracted the title; name of first author; year of publication; type of surgery; number of patients in both groups; CW L collected the characteristics of the patients, and the required outcomes in the two groups. The data extraction author was blinded.
ZZ used the Cochrane Risk of Bias 2.0 to assess the quality of the included studies (Higgins et al., 2011). CW L used the Begg test and Egger test in Stata 16.0 software to analyze publication bias. Any disagreement was resolved through discussion with another author.
Data analysis
Data analysis was performed using Review Manager 5.4 (Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020). Pooled risk ratio (RR) and 95% confidence interval (CI) for dichotomous results were calculated using the Mantel-Haenszel method. For continuous outcomes, mean difference (MD) and 95% CI were calculated using inverse-variance method. If only the median and interquartile range (IQR) were available, the Wan methods was used to converted data expressed as medians (interquartile range) to means ± standard deviations (Wan et al., 2014). The statistical heterogeneity was assessed using the chi-square test, and the I2 statistic was calculated. I2 values of approximately 25%, 50%, and 75% were considered low, moderate, and severe heterogeneity, respectively (I2 > 50% was used as the threshold to indicate significant heterogeneity in individual studies). Data analysis of the collated data was performed using a fixed-effects model when I2 ≤ 50, and a randomized-effects model when I2 > 50. p < 0.05 was considered statistically significant. Subgroup analysis of primary outcomes was performed by Stata 16.0 and divided into groups according to type of intraoperative opioid use (remifentanil vs sufentanil, fentanyl), methods used for maintenance of opioid-free anesthesia (volatile anesthesia combined with propofol vs propofol vs epidural anesthesia) in opioid-free anesthesia, methods of implementation of opioid-free anesthesia (epidural vs general anesthesia), and whether dexmedetomidine is used in opioids anesthesia (yes vs no). Sensitivity analysis was used for secondary outcomes with high heterogeneity and it was performed by removing one study at a time to estimate the effect of an individual study on the pooled results.
Results
Literature search and screening
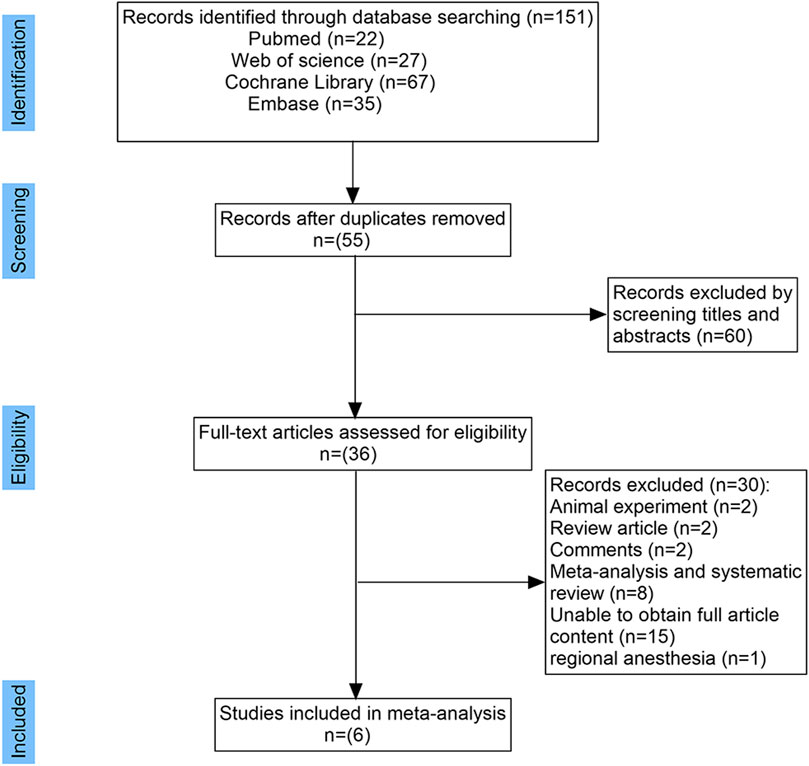
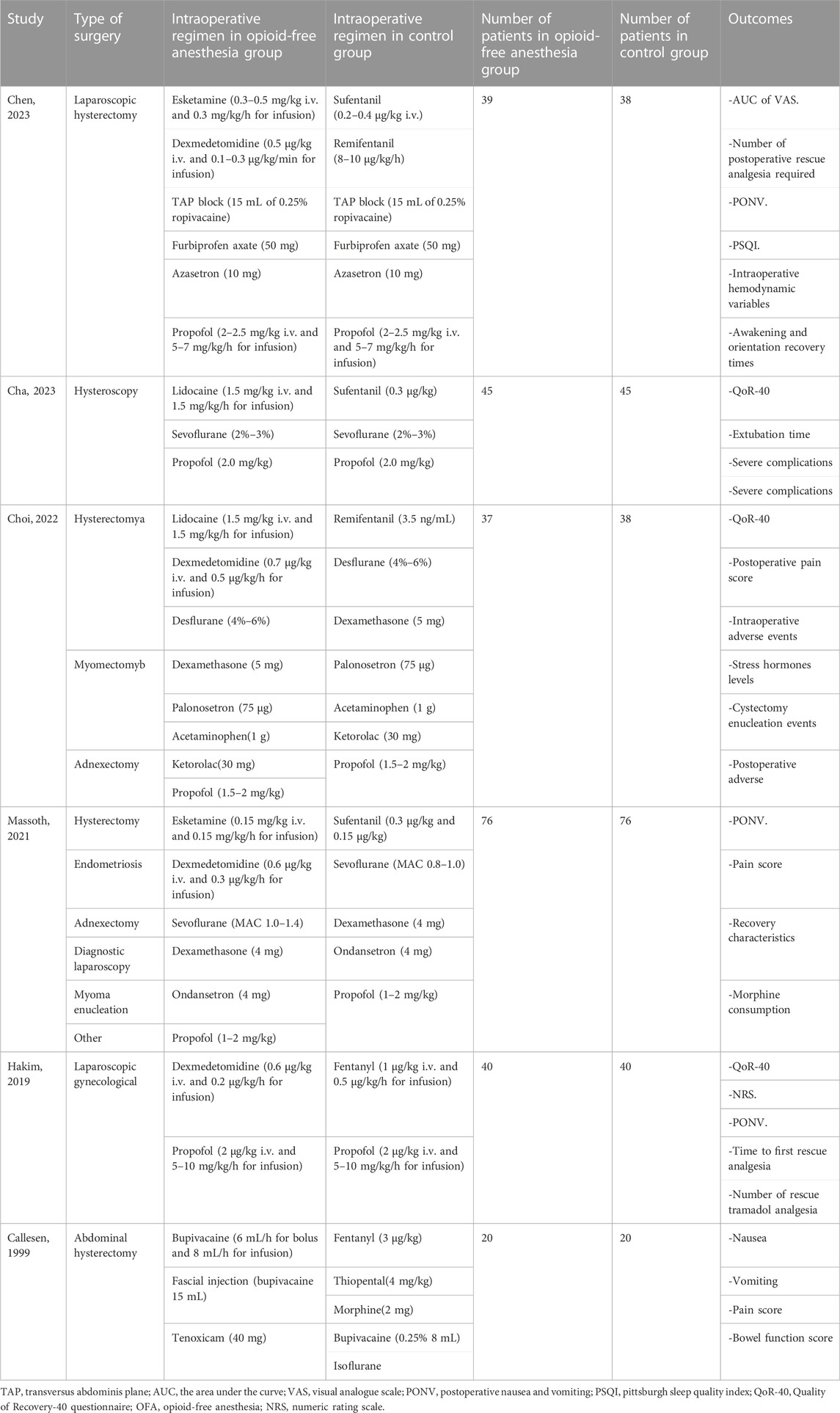
A total of 151 relevant studies were retrieved, and 115 were excluded. After reviewing the remaining 36 studies, 30 were excluded for reasons shown in Figure 1. Six studies involving 514 adult patients undergoing gynecological surgery or examination were included in this meta-analysis (Callesen et al., 1999; Hakim and Wahba, 2019; Massoth et al., 2021; Chen et al., 2022; Choi et al., 2022; Cha et al., 2023). Of the 6 included studies, 2 reported the use of fentanyl in the control group (Callesen et al., 1999; Hakim and Wahba, 2019), 3 reported the use of sufentanil (Massoth et al., 2021; Chen et al., 2022; Cha et al., 2023), and 1 reported the use of remifentanil in the control group (Choi et al., 2022). However, the OFA groups reported in the six studies used different regimens. The characteristics of the included studies are presented in Table 1.
Quality assessment
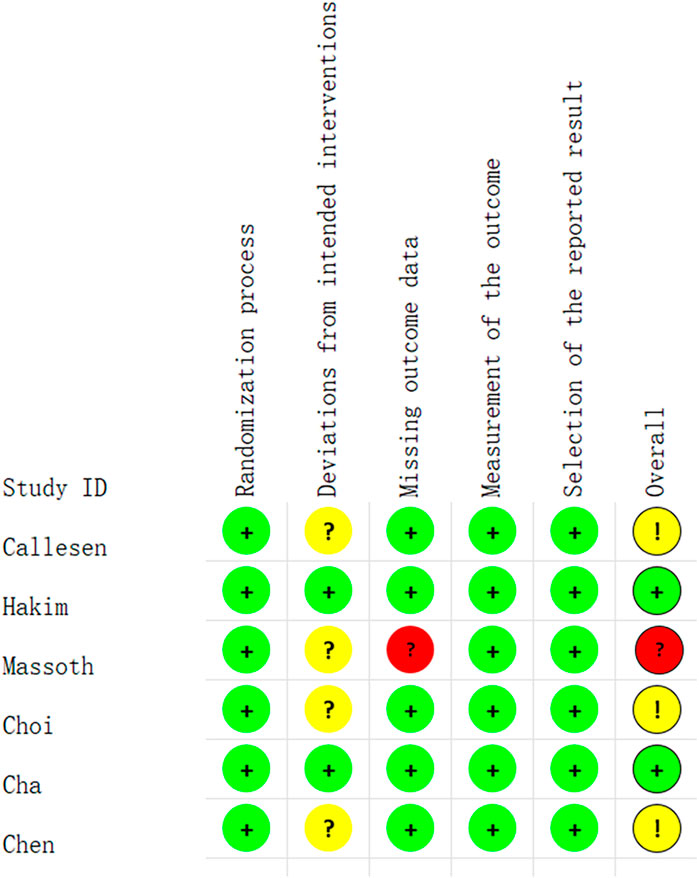
Of the 6 studies, 2 studies were considered to have a low risk of bias (Hakim and Wahba, 2019; Cha et al., 2023). The study by Massoth et al. was considered likely to have a high attrition bias (Massoth et al., 2021). In addition, three studies were considered to have an unclear risk of bias (Callesen et al., 1999; Chen et al., 2022; Choi et al., 2022). The quality evaluation of the included studies was shown in Figure 2.
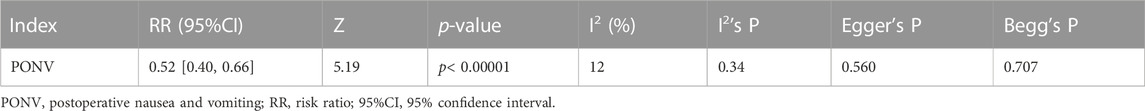
Publication bias
According to the principle of publication bias, we counted the research reports with PONV (Callesen et al., 1999; Hakim and Wahba, 2019; Massoth et al., 2021; Chen et al., 2022; Choi et al., 2022; Cha et al., 2023) as the outcome (Begg’s p = 0.707, Egger’s p = 0.560), suggesting that the articles included in the research report had no publication bias. The result was shown in Table 2.
PONV and rescue antiemetics
Six studies including 514 patients undergoing gynecological surgery or examination, reported the incidence of PONV (Callesen et al., 1999; Hakim and Wahba, 2019; Massoth et al., 2021; Chen et al., 2022; Choi et al., 2022; Cha et al., 2023). The incidence of PONV was significantly lower in the OFA group than that in the control group (RR = 0.52; M-H, Fixed, 95% CI = 0.40–0.66; p < 0.00001; I2 = 12%) (Figure 3A). The heterogeneity of result was low.
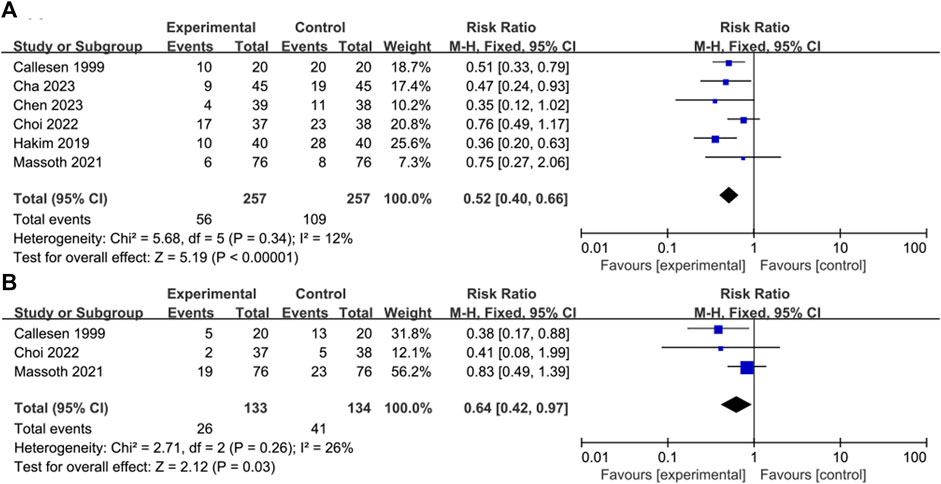
FIGURE 3. Forest plot of the (A) incidence of postoperative nausea and/or vomiting (PONV) (B) rescue antiemetics: opioid-free anesthesia vs control.
Three of the 6 studies reported the use of postoperative antiemetics (Callesen et al., 1999; Massoth et al., 2021; Choi et al., 2022). The use of postoperative antiemetics was significantly lower in the intervention group than that in the control group (RR = 0.64; M-H, Fixed, 95% CI = 0.42–0.97; p = 0.03; I2 = 26%) (Figure 3B). The heterogeneity of result was moderate.
Pain score and analgesic use
Three of the 6 studies reported specific pain scores (Hakim and Wahba, 2019; Massoth et al., 2021; Choi et al., 2022) and there was no significant difference in postoperative pain scores between the control and OFA groups (MD = 0.05; IV, Fixed, 95% CI = −0.44–0.54; p = 0.85; I2 = 0%) (Figure 4A). The heterogeneity of result was low.
Four of the 6 studies reported the use of postoperative analgesics (Callesen et al., 1999; Hakim and Wahba, 2019; Chen et al., 2022; Choi et al., 2022); the use of postoperative analgesics in the intervention group was not significantly lower than that in the control group (RR = 1.09; M-H, Random, 95% CI = 0.76–1.55; p = 0.65; I2 = 70%) (Figure 4B). The heterogeneity of result was high.
Time of extubation and QoR-40
Three of the 6 studies reported the time of extubation (Hakim and Wahba, 2019; Choi et al., 2022; Cha et al., 2023); the time of extubation in the OFA group was not significantly shorter than that in the control group (MD = −0.89; IV, Random, 95% CI = −1.94–0.16; p = 0.09; I2 = 71%) (Figure 5A). The heterogeneity of result was high.
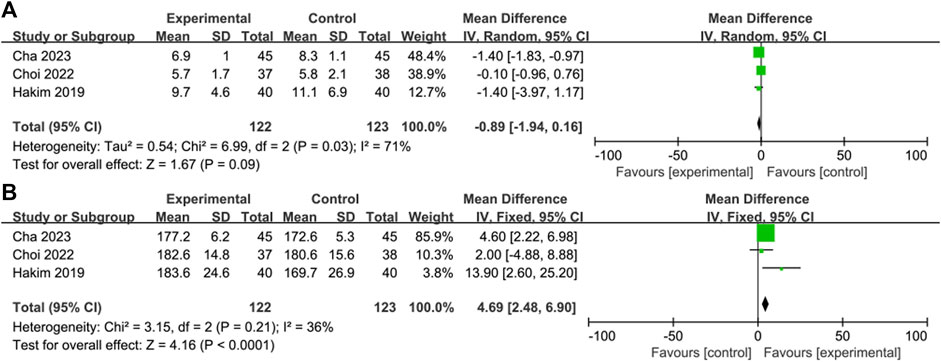
FIGURE 5. Forest plot of the (A) time of extubation: opioid-free anesthesia vs control (B) the QoR-40: opioid-free anesthesia vs control.
Three of the 6 studies reported QoR-40 scores (Hakim and Wahba, 2019; Choi et al., 2022; Cha et al., 2023). The score of QoR-40 in the OFA was significantly higher than that in the control group (MD = 4.69; IV, Fixed, 95% CI = 2.48–6.90; p < 0.0001; I2 = 36%) (Figure 5B). The heterogeneity of result was moderate.
Subgroup analysis
Subgroup analysis of intraoperative opioid use showed that the heterogeneity of each subgroup was reduced (Figure 6A). When it based on intraoperative maintenance of opioid-free anesthesia also showed a decrease in heterogeneity among subgroups (Figure 6B). However, subgroup analysis according to methods of implementation of opioid-free anesthesia did not show a reduction in heterogeneity across subgroups (Figure 7A), nor did subgroup analysis according to whether dexmedetomidine was used in the opioid-free anesthesia group (Figure 7B).
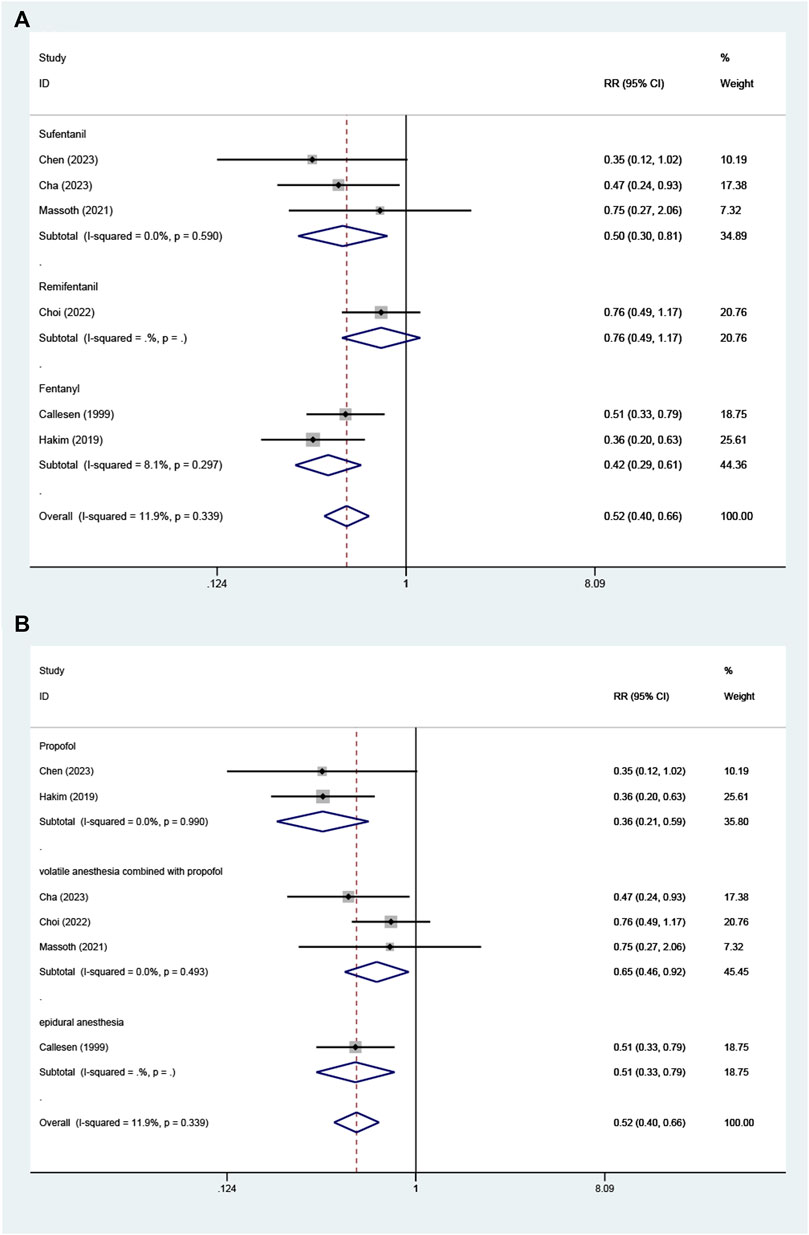
FIGURE 6. Subgroup analysis. Forest plot of the (A) according to type of intraoperative opioid use (remifentanil vs sufentanil, fentanyl) (B) according to methods used for maintenance of opioid-free anesthesia (volatile anesthesia combined with propofol vs propofol vs epidural anesthesia).

FIGURE 7. Subgroup analysis. Forest plot of the (A) according to methods of implementation of opioid-free anesthesia (epidural vs general anesthesia) (B) according to whether dexmedetomidine is used in opioids anesthesia (yes vs no).
Sensitivity analysis
For the outcome of postoperative analgesic use, when the study by Callesen et al. (Callesen et al., 1999)was removed, the heterogeneity of the meta-analysis was reduced; however, the conclusion keeps consistent (I2 = 0%; p = 0.13) (Figure 8A). For time of extubation, when the study by Choi et al. (Choi et al., 2022) was removed, the heterogeneity decreased; however, the conclusion did change (I2 = 0%; p < 0.00001) (Figure 8B). When the study by Cha et al. (Cha et al., 2023) was removed, the heterogeneity was also reduced, but the conclusion did not change (I2 = 0%; p = 0.58) (Figure 8C).
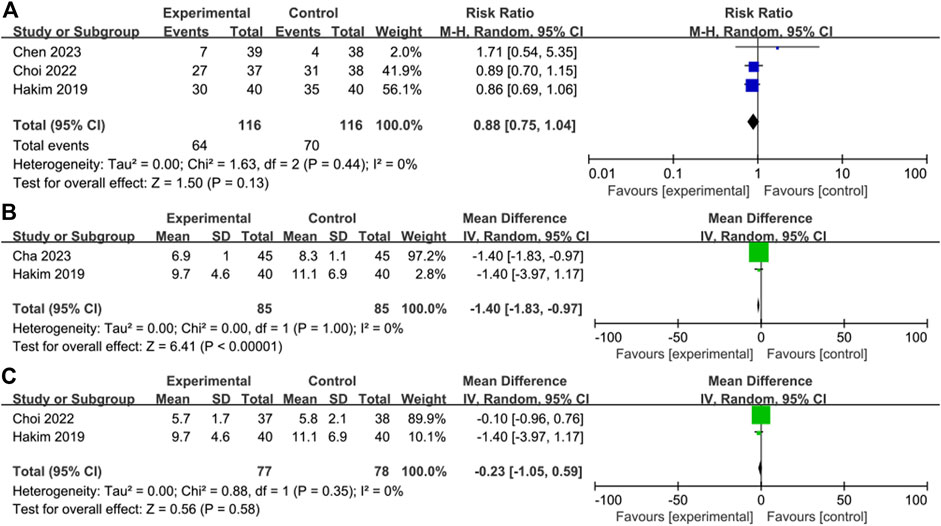
FIGURE 8. Sensitivity analysis. Forest plot comparing the (A) analgesic use without Callesen’s report (B) time of extubation without Choi’s report (C) time of extubation without Cha’s report.
Discussion
Although many previous studies have investigated the postoperative outcomes of OFA and opioid-based anesthesia, there is a lack of systematic reviews and meta-analyses addressing a particular type of surgery. In this meta-analysis, we defined opioid-free anesthesia as the absence of opioid use during surgery, and regional anesthesia was also defined as a technique of opioid-free anesthesia, which was ultimately included in six studies. The results revealed that, in gynecological surgery, compared with opioid-based anesthesia, OFA reduced the incidence of PONV and the use of postoperative antiemetics, improved the quality of recovery but did not affect postoperative pain and the time of extubation.
Previous studies have found that opioid-free anesthesia can reduce postoperative nausea and vomiting in patients (Frauenknecht et al., 2019; Salomé et al., 2021; Feenstra et al., 2023; Malo-Manso et al., 2023; Zhang et al., 2023) and improve the quality of postoperative recovery (Feenstra et al., 2023), which is consistent with the results of this meta-analysis of opioid-free gynecological surgery. But two meta-analyses found that opioid-free anesthesia reduced postoperative pain in patients (Malo-Manso et al., 2023; Zhang et al., 2023) and one showed that opioid-free anesthesia reduced extubation time (Zhang et al., 2023), which is different from our results.
PONV remains a major challenge. Female sex is an independent risk factor for PONV, and the incidence of PONV in gynecological surgery is high among various types of surgery (Apfel et al., 2012). A study by Apfel et al. reported that the incidence of PONV can reach 80% in gynecological surgery involving opioid-based anesthesia (Madej and Simpson, 1986; Wesmiller et al., 2017). Opioids are commonly used perioperative analgesics with good analgesic effect; however, they also have adverse reactions such as nausea and vomiting (Gustafsson et al., 2023). Opioids may induce nausea and vomiting by direct action on chemo-trigger zone receptors in the brainstem (Andrews, 1992). The effect of perioperative opioid use on PONV has been extensively studied, and there is strong evidence supporting that the incidence and severity of PONV are dose-dependent with perioperative opioids. (Roberts et al., 2005). OFA replaces opioids with other drugs or anesthetic techniques during anesthesia, thus minimizing perioperative opioid use, thus may reduce the incidence of PONV, which is consistent with the conclusions of this meta-analysis. Among the 6 included studies, Callesen et al. used combined spinal-epidural anesthesia in the OFA group, and regional anesthesia may have a different risk of PONV compared with general anesthesia, which may affect the accuracy of the results. (Liu et al., 2005). However, when we excluded this study, the conclusions did not change. And through subgroup analysis, we found that the sources of heterogeneity were differences in intraoperative opioid use and methods of intraoperative anesthesia maintenance. Of the included studies, 4 selected dexmedetomidine as part of OFA, and previous studies have shown that dexmedetomidine, as an α2 receptor agonist, can reduce the occurrence of PONV by modulating the release of 5-hydroxytryptamine and dopamine (Zhao et al., 2023). Despite inconsistent combinations of anesthetic drugs, we concluded that OFA is beneficial in reducing PONV during gynecological surgery.
The effect of OFA on postoperative pain is controversial; in this meta-analysis, there were no statistical differences in postoperative pain scores and postoperative analgesic consumption between the two groups. Our results support the use of multimodal analgesia to minimize opioids use and achieve adequate analgesia. However, due to differences in postoperative analgesia and multi-modal analgesia protocols, the confidence of this conclusion is limited, and more trials are needed to explore the relationship between OFA and postoperative pain. There was no difference in extubation time between the two groups. It is generally expected that opioid use will enhance sedation and thus prolong extubation time, but this result is contrary. This may be due to the fact that the insufficient sample size makes this conclusion less reliable. In addition, this meta-analysis concluded that OFA improved the quality of recovery. The included studies selected the QoR-40 as the assessment tool for quality of recovery, and PONV is an important component of QoR-40; thus, a lower incidence of PONV may lead to a better postoperative quality of recovery. However, due to the small number of included studies and high heterogeneity, the confidence of secondary outcomes is limited.
This meta-analysis had some limitations. First, we included only 6 studies, and the sample size was small. Second, the types of procedures included in the study were not broad enough. Third, the end point of our outcome indicators was the last time period, and the relevant outcome indicators occurring in the middle time period were not extracted and analyzed; thus, confidence of secondary outcomes was limited.
Conclusion
OFA reduces PONV and the use of antiemetic drugs. In addition, it improves the quality of postoperative recovery. However, OFA can not reduce the postoperative pain scores, analgesic use and the time of extubation. Due to the strength of the evidence, we cannot support OFA as an ideal anesthesia method in gynecological surgery, and the implementation of anesthesia strategies should be case-by-case.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
ZZ: Data curation, Formal Analysis, Software, Visualization, Writing–original draft, Methodology. CL: Supervision, Writing–original draft, Writing–review and editing. LX: Writing–review and editing, Data curation. XS: Data curation, Writing–review and editing, Formal Analysis. XL: Data curation, Formal Analysis, Writing–review and editing. PW: Conceptualization, Funding acquisition, Writing–review and editing, Methodology, Project administration. JL: Conceptualization, Funding acquisition, Project administration, Supervision, Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Support for this study was provided from the Natural Science Foundation of Shandong Province (ZR2020QH291 and ZR2020MH126), the Qingdao Key Health Discipline Development Fund (QDZDZK2022094) and the Qingdao Outstanding Health Professional Development Fund (2023).
Acknowledgments
We thank all the participants and study staffs involved in this study for their great contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adams, T. J., Aljohani, D. M., and Forget, P. (2023). Perioperative opioids: a narrative review contextualising new avenues to improve prescribing. Br. J. Anaesth. 130, 709–718. doi:10.1016/j.bja.2023.02.037
Andrews, P. L. (1992). Physiology of nausea and vomiting. Br. J. Anaesth. 69, 2S–19S. doi:10.1093/bja/69.supplement_1.2s
Apfel, C. C., Heidrich, F. M., Jukar-Rao, S., Jalota, L., Hornuss, C., Whelan, R. P., et al. (2012). Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br. J. Anaesth. 109, 742–753. doi:10.1093/bja/aes276
Bramer, W. M., Milic, J., and Mast, F. (2017). Reviewing retrieved references for inclusion in systematic reviews using EndNote. J. Med. Libr. Assoc. JMLA 105, 84–87. doi:10.5195/jmla.2017.111
Callesen, T., Schouenborg, L., Nielsen, D., Guldager, H., and Kehlet, H. (1999). Combined epidural-spinal opioid-free anaesthesia and analgesia for hysterectomy. Br. J. Anaesth. 82, 881–885. doi:10.1093/bja/82.6.881
Cha, N. H., Hu, Y., Zhu, G. H., Long, X., Jiang, J. J., and Gong, Y. (2023). Opioid-free anesthesia with lidocaine for improved postoperative recovery in hysteroscopy: a randomized controlled trial. BMC Anesthesiol. 23, 192. doi:10.1186/s12871-023-02152-7
Chen, J., Luo, Q., Huang, S., and Jiao, J. (2022). Effect of opioid-free anesthesia on postoperative analgesia after laparoscopic gynecologic surgery. Minerva Anestesiol. 88, 439–447. doi:10.23736/S0375-9393.22.15850-5
Choi, H., Song, J. Y., Oh, E. J., Chae, M. S., Yu, S., and Moon, Y. E. (2022). The effect of opioid-free anesthesia on the quality of recovery after gynecological laparoscopy: a prospective randomized controlled trial. J. pain Res. 15, 2197–2209. doi:10.2147/JPR.S373412
Elkassabany, N. M., and Mariano, E. R. (2019). Opioid-free anaesthesia - what would Inigo Montoya say? Anaesthesia 74, 560–563. doi:10.1111/anae.14611
Feenstra, M. L., Jansen, S., Eshuis, W. J., van Berge Henegouwen, M. I., Hollmann, M. W., and Hermanides, J. (2023). Opioid-free anesthesia: a systematic review and meta-analysis. J. Clin. Anesth. 90, 111215. doi:10.1016/j.jclinane.2023.111215
Forget, P. (2021). Opioid treatment for non-cancer pain: we need a comprehensive approach. BMJ 375, n3045. doi:10.1136/bmj.n3045
Frauenknecht, J., Kirkham, K. R., Jacot-Guillarmod, A., and Albrecht, E. (2019). Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia 74, 651–662. doi:10.1111/anae.14582
Gustafsson, M., Matos, C., Joaquim, J., Scholl, J., and van Hunsel, F. (2023). Adverse drug reactions to opioids: a study in a national pharmacovigilance database. Drug Saf. 46, 1133–1148. doi:10.1007/s40264-023-01351-y
Hakim, K. Y. K., and Wahba, W. Z. B. (2019). Opioid-free total intravenous anesthesia improves postoperative quality of recovery after ambulatory gynecologic laparoscopy. Anesth. Essays Res. 13, 199–203. doi:10.4103/aer.AER_74_19
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. doi:10.1136/bmj.d5928
Liu, S. S., Strodtbeck, W. M., Richman, J. M., and Wu, C. L. (2005). A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth. Analg. 101, 1634–1642. doi:10.1213/01.ANE.0000180829.70036.4F
Macintyre, P. E., Quinlan, J., Levy, N., and Lobo, D. N. (2022). Current issues in the use of opioids for the management of postoperative pain: a review. JAMA Surg. 157, 158–166. doi:10.1001/jamasurg.2021.6210
Madej, T. H., and Simpson, K. H. (1986). Comparison of the use of domperidone, droperidol and metoclopramide in the prevention of nausea and vomiting following major gynaecological surgery. Br. J. Anaesth. 58, 884–887. doi:10.1093/bja/58.8.884
Malo-Manso, A., Fontaneda-Heredia, A., Romero-Molina, S., Sepúlveda-Haro, E., Escalona-Belmonte, J. J., and Guerrero-Orriach, J. L. (2023). Opioid-free anaesthesia improves anaesthesia recovery when compared with that of opioid-based anaesthesia. Systematic review and meta-analysis of clinical trials. Curr. Med. Chem. 30, 1667–1681. doi:10.2174/0929867329666220907155612
Massoth, C., Schwellenbach, J., Saadat-Gilani, K., Weiss, R., Pöpping, D., Küllmar, M., et al. (2021). Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy - a randomised controlled trial. J. Clin. Anesth. 75, 110437. doi:10.1016/j.jclinane.2021.110437
Mieszczański, P., Górniewski, G., Ziemiański, P., Cylke, R., Lisik, W., and Trzebicki, J. (2023). Comparison between multimodal and intraoperative opioid free anesthesia for laparoscopic sleeve gastrectomy: a prospective, randomized study. Sci. Rep. 13, 12677. doi:10.1038/s41598-023-39856-2
Moningi, S., Patki, A., Padhy, N., and Ramachandran, G. (2019). Enhanced recovery after surgery: an anesthesiologist's perspective. J. Anaesthesiol. Clin. Pharmacol. 35, S5–S13. doi:10.4103/joacp.JOACP_238_16
Mulier, J., and Dekock, M. (2017). Opioid free general anesthesia, a new paradigm? Best. Pract. Res. Clin. Anaesthesiol. 31, 441–443. doi:10.1016/j.bpa.2017.11.005
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ Clin. Res. ed.) 372, n71. doi:10.1136/bmj.n71
Roberts, G. W., Bekker, T. B., Carlsen, H. H., Moffatt, C. H., Slattery, P. J., and McClure, A. F. (2005). Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth. Analg. 101, 1343–1348. doi:10.1213/01.ANE.0000180204.64588.EC
Salomé, A., Harkouk, H., Fletcher, D., and Martinez, V. (2021). Opioid-free anesthesia benefit-risk balance: a systematic review and meta-analysis of randomized controlled trials. J. Clin. Med. 10, 2069. doi:10.3390/jcm10102069
Selim, J., Jarlier, X., Clavier, T., Boujibar, F., Dusséaux, M.-M., Thill, J., et al. (2022). Impact of opioid-free anesthesia after video-assisted thoracic surgery: a propensity score study. Ann. Thorac. Surg. 114, 218–224. doi:10.1016/j.athoracsur.2021.09.014
Shinoda, T., Murakami, W., Takamichi, Y., Iizuka, H., Tanaka, M., and Kuwasako, Y. (2013). Effect of remifentanil infusion rate on stress response in orthopedic surgery using a tourniquet application. BMC Anesthesiol. 13, 14. doi:10.1186/1471-2253-13-14
Vadivelu, N., Kai, A. M., Kodumudi, V., Sramcik, J., and Kaye, A. D. (2018). The opioid crisis: a comprehensive overview. Curr. Pain Headache Rep. 22, 16. doi:10.1007/s11916-018-0670-z
Wan, X., Wang, W., Liu, J., and Tong, T. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14, 135. doi:10.1186/1471-2288-14-135
Wesmiller, S. W., Bender, C. M., Conley, Y. P., Bovbjerg, D. H., Ahrendt, G., Bonaventura, M., et al. (2017). A prospective study of nausea and vomiting after breast cancer surgery. J. Perianesthesia Nurs. Official J. Am. Soc. PeriAnesthesia Nurses 32, 169–176. doi:10.1016/j.jopan.2015.12.009
Zhang, Y., Ma, D., Lang, B., Zang, C., Sun, Z., Ren, S., et al. (2023). Effect of opioid-free anesthesia on the incidence of postoperative nausea and vomiting: a meta-analysis of randomized controlled studies. Med. Baltim. 102, e35126. doi:10.1097/MD.0000000000035126
Zhao, W., Li, J., Wang, N., Wang, Z., Zhang, M., Zhang, H., et al. (2023). Effect of dexmedetomidine on postoperative nausea and vomiting in patients under general anaesthesia: an updated meta-analysis of randomised controlled trials. BMJ Open 13, e067102. doi:10.1136/bmjopen-2022-067102
Zorrilla-Vaca, A., Ramirez, P. T., Iniesta-Donate, M., Lasala, J. D., Wang, X. S., Williams, L. A., et al. (2022). Opioid-sparing anesthesia and patient-reported outcomes after open gynecologic surgery: a historical cohort study. Can. J. Anaesth. = J. Can. D'anesthesie 69, 1477–1492. doi:10.1007/s12630-022-02336-8
Keywords: opioid-free anesthesia, postoperative nausea and vomiting, gynecological surgery, quality of recovery, pain
Citation: Zhang Z, Li C, Xu L, Sun X, Lin X, Wei P and Li J (2024) Effect of opioid-free anesthesia on postoperative nausea and vomiting after gynecological surgery: a systematic review and meta-analysis. Front. Pharmacol. 14:1330250. doi: 10.3389/fphar.2023.1330250
Received: 30 October 2023; Accepted: 14 December 2023;
Published: 04 January 2024.
Edited by:
Francisco Lopez-Munoz, Camilo José Cela University, SpainReviewed by:
Lyrics Noba, University of Leeds, United KingdomDavid Mayheu, National Health Service, United Kingdom
Copyright © 2024 Zhang, Li, Xu, Sun, Lin, Wei and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Penghui Wei, d2VpcGVuZ2h1aWh1aUBzaW5hLmNvbQ==; Jianjun Li, bGpqOTU3M0AxNjMuY29t
†These authors share first authorship
 Zheng Zhang
Zheng Zhang Chengwei Li1†
Chengwei Li1† Lin Xu
Lin Xu Penghui Wei
Penghui Wei Jianjun Li
Jianjun Li