- 1Department of Psychiatry, University of Campania “L. Vanvitelli”, Naples, Italy
- 2Department of Translational Biomedicine and Neuroscience, University of Bari Aldo Moro, Bari, Italy
- 3Department of Biotechnological and Applied Clinical Sciences, University of L’Aquila, L’Aquila, Italy
- 4Department of Systems Medicine, University of Rome Tor Vergata, Rome, Italy
- 5Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Introduction: Poor adherence to pharmacological treatment is frequent in people with severe mental disorders and it often causes lack of effectiveness of many psychotropic drugs. Thus, efforts should be made to improve adherence to pharmacological treatments in patients with these disorders.
Methods: In this paper, based on the LIFESTYLE randomized, controlled multicentric trial, we aim to: 1) assess the level of adherence in a real-world sample of patients with severe mental disorders; 2) evaluate differences in treatment adherence according to patients’ socio-demographic and clinical characteristics; 3) evaluate the impact of an innovative psychosocial intervention, on patients’ adherence to treatments. The Lifestyle Psychosocial Group Intervention consists of group sessions, focused on different lifestyle behaviours, including healthy diet; physical activity; smoking habits; medication adherence; risky behaviours; and regular circadian rhythms. At end of each session a 20-min moderate physical activity is performed by the whole group.
Results: The sample consists of 402 patients, mainly female (57.1%, N = 229), with a mean age of 45.6 years (±11.8). Less than 40% of patients reported a good adherence to pharmacological treatments. Adherence to treatments was not influenced by gender, age, diagnosis and duration of illness. At the end of the intervention, patients receiving the experimental intervention reported a significant improvement in the levels of adherence to treatments (T0: 35.8% vs. T3: 47.6%, p < 0.005). Patients practicing moderate physical activity reported a two-point improvement in the levels of adherence [odds ratio (OR): 1,542; 95% confidence intervals (CI): 1,157–2,055; p < 0.001], even after controlling for several confounding factors.
Discussion: The experimental lifestyle intervention, which can be easily implemented in the routine clinical practice of mental health centres, was effective in improving adherence to pharmacological treatments.
Background
Adherence to treatment or medication compliance, defined as intake of medications according to the prescribed dosage provided by referring clinician and with persistence over time (World Health Organization, 2003). A different concept is that of medication persistence, referring to the act of continuing the treatment for the prescribed duration (Cramer et al, 2008). Medication adherence is fundamental to prevent relapses, improve long-term clinical and functional outcome, and reduce healthcare costs in people suffering from chronic physical or mental disorders (Davidson and Tondora, 2022; McIntyre et al., 2022). People suffering from severe mental disorders often report non-adherence to prescribed medications, ranging from 28%–52% in people suffering from major depression to 70% in patients with schizophrenia (Baylé et al., 2015). About 40% of patients stop taking their medication within a year, and up to 75% up to 2 years (Semahegn et al., 2020). Poor adherence to pharmacological treatment is also common in people suffering from other chronic diseases, such as diabetes, cardiovascular diseases or chronic obstructive pulmonary disease (COPD) (Vetrano et al., 2017; Marrie and Bernstein et al., 2021), with approximately 50% of patients not taking properly the drugs prescribed for long-term therapies (Brown and Bussell, 2011; Kim et al., 2021; Fusar-Poli et al., 2022; Mirhaj Mohammadabadi et al., 2022; Ostuzzi et al., 2022).
Lack of adherence is one of the causes for low efficacy of many pharmacological treatments and should be carefully evaluated in clinical practice. In fact, the WHO has defined an “invisible epidemic” the poor or lack of adherence to treatments, which should be tackled with any possible effective initiative (WHO, 2003).
Nonadherence to pharmacological and non-pharmacological interventions is considered a multifactorial phenomenon, including causes related to the patient, the healthcare system and the clinician (Lam and Fresco, 2015; Caqueo-Urízar et al., 2021). Patients’ adherence to medications is significantly reduced by lack of insight (Novick et al., 2015), negative beliefs about the efficacy of the medications, concerns about side effects, costs of medications, low educational level, and belonging to ethnic minority (Lemay et al., 2018). In particular, several studies have highlighted that lower insight is associated with lower adherence and a worse therapeutic relationship (Novick et al., 2015; Elowe et al., 2022; Okobi et al., 2022). Healthcare system factors mainly include polypharmacy (particularly in older adults) and care fragmentation provided by different healthcare professionals (Aggarwal et al., 2020). Clinician-related factors include excessive workload, lack of time for patient’s education about treatments, poor adoption of the shared decision-making approach (Dell’Osso et al., 2020; Caqueo-Urízar et al., 2021). Because these factors usually interact and potentiate each other, multilevel and integrated strategies are required to efficiently address poor adherence to medications.
Available interventions for improving treatment adherence have been grouped into four categories: educational, behavioural, cognitive-behavioural, and multicomponent approaches (Torres-Robles et al., 2018; Cuijpers et al., 2021; Leichsenring et al., 2022). The most frequently adopted interventions are psychoeducation (Killaspy et al., 2022; Harmancı and Yıldız, 2023), problem-solving strategies (Chatoo and Lee, 2022), and programmes aiming to promote the adoption of a shared decision-making clinical style (Fiorillo et al., 2020; Fulford and Handa, 2021; Roe et al., 2022). Despite this, adherence rates to treatments remain incredibly low, highlighting the need to develop and implement innovative and effective strategies. One of these innovative strategies is represented by the promotion of healthy lifestyle behaviours, including regular physical activity. A recent study carried out in a cardiology unit involving patients suffering from hypertension has shown the positive effect of regular physical activity on adherence to medications (Fragoulis et al., 2023) after a behavioral activation intervention. Thus, the authors concluded that there is the need for innovative research in this field for further confirmation of the positive relationship between treatments’ adherence and physical activity. Indeed, physical activity defined as any planned, systematic, and repetitive physical exercise that enhances athletic performance by improving body composition, fitness, and motor abilities (Mahindru et al., 2023), is considered a complementary treatment modality in the management and control of non-communicable diseases, including severe mental disorders, and is associated with the reduction of cardiovascular risk, morbidity and mortality (Theofilou and Saborit, 2013; Saqib et al., 2020; Arango et al., 2021; Baron and Noordsy, 2021; Suokas et al., 2022). People with severe mental disorders too often have a sedentary lifestyle and do not perform any kind of physical activity (Sampogna et al., 2022a; Sampogna et al., 2022b; Correll et al., 2022; Højlund et al., 2022). Several psychosocial interventions with a specific focus on physical activity and other healthy lifestyle behaviours—such as quit smoking and balanced diet—have been recently developed for people with severe mental disorders (Masa-Font et al., 2015; Speyer et al., 2016; De Rosa et al., 2017; Swift et al., 2021). These interventions showed promising results in terms of reduction of the long-term morbidity and mortality, but a few data are available on their efficacy on adherence to treatments. Indeed, an emerging body of research has linked both the onset and symptoms of various mental disorders to “lifestyle factors”, a term referring to health behaviors such as physical activity, diet, tobacco smoking and sleep and therefore the innovative field of lifestyle psychiatry is nowadays very active and expanding quickly (Firth et al., 2020).
The present research project entitled “LIFESTYLE trial” is a multicentric, randomized controlled study aiming to test the efficacy of an innovative psychosocial intervention on several lifestyle behavioural domains (Sampogna et al., 2018). This paper aims to: 1) assess the level of adherence in a real-world sample of patients with severe mental disorders; 2) evaluate differences in adherence to pharmacological treatments according to patients’ socio-demographic and clinical characteristics; 3) evaluate the impact of an innovative psychosocial intervention on patients’ adherence to treatments.
Methods
The LIFESTYLE trial was coordinated by the University of Campania “Luigi Vanvitelli” in Naples and carried out in the mental health units of the Universities of Bari, Genova, L’Aquila, Pisa, and Rome-Tor Vergata (Sampogna et al., 2018; Luciano et al., 2022).
The full methodology of the study is available in Sampogna et al. (2018). Patients were included if they met the following criteria: 1) age between 18 and 65 years; 2) diagnosis of schizophrenia, schizoaffective disorder, delusional disorder, other psychotic disorder, major depressive disorder, or bipolar disorder, according to the DSM-5 criteria and confirmed by the Structured Clinical Interview for DSM-5 (SCID-5); 3) ability to provide written informed consent; 4) BMI ≥ 25; 5) in charge at the local mental health unit for at least 3 months before recruitment. Exclusion criteria were: inability to perform moderate physical activity (i.e., walking at least 150 min per week, or 75 min of vigorous activity twice a week, according to the guidelines of the Italian Ministry of Health); pregnancy or breast-feeding; intellectual disability or severe cognitive impairment; hospital admission in the previous 3 months.
The main outcome measure considered for the present analyses is a change of global score at the Morisky Medication Adherence Scale (MMAS) (Morisky et al., 1986), which evaluates the levels of adherence to pharmacological treatments. The MMAS-4 uses a scoring scheme of “Yes” = 0 and “No” = 1. Therefore, the items were summed up to obtain scores ranging from 0 to 4 (e.g., a score of 0 was considered poor; while a score of 4 was considered complete adherence).
Besides the MMAS, all recruited patients were assessed through the following tests: a) the International Physical Activity Questionnaire (IPAQ)—short form (Craig et al., 2003); b) the Food Frequency Questionnaire—short version (Marventano et al., 2016); c) the 24-item Questionnaire on lifestyle behaviours, developed by the Italian National Institute of Health (ISS, 2010); d) the Fagerström Test for Nicotine Dependence (FTND) (Heatherton et al., 1991); e) the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989); f) the Leeds Dependence Questionnaire (LDQ) (Raistrick et al., 1994); g) the Recovery Style Questionnaire (RSQ) (Drayton et al., 1998); h) the Cumulative Illness Rating Scale (CIRS) (Linn et al., 1968); i) the Manchester Short Assessment of Quality of Life (Priebe et al., 1999); j) the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery (MCCB)—brief version (Kern et al., 2008); k) the Internalized Stigma of Mental Illness (ISMI) (Ritsher et al., 2003); l) an ad hoc questionnaire on sexual health; m) the Pattern of Care Schedule (PCS)—modified version (Morosini et al., 2000); n) the 24-item Brief Psychiatric Rating Scale (BPRS) (Lukoff et al., 1986); o) the Personal and Social Performance Scale (Morosini et al., 2000).
Information on weight, height, BMI, waist circumference, blood pressure, resting heart rate, HDL, LDL and overall levels of cholesterol, blood glucose, triglycerides, and blood insulin were collected by researchers with an Anthropometric schedule.
All patients have been assessed at the baseline (T0); 2 months post-randomization (T1); 4 months post-randomization (T2); 6 months post-randomization (T3); 12 months post-randomization (T4); and 24 months post-randomization (T5). T1 and T2 assessments include only anthropometric tests. For the scope of the present study, only data collected at baseline and 6 monts post-randomization have been considered.
Patients were randomly allocated to receive the Lifestyle Psychosocial Group Intervention (experimental group) or a Brief Psychoeducational Group Intervention (control group).
The Lifestyle Psychosocial Group Intervention consists of group sessions, delivered every 7–10 days for about 6 months, focused on different lifestyle behaviours, including healthy diet; physical activity; smoking habits; medication adherence; risky behaviours; and regular circadian rhythms. At end of each session a 20-min moderate physical activity is performed by the whole group.
The control Brief Psychoeducational Group Intervention consists of group sessions, delivered every 7 days for about 2 months and focusing on healthy lifestyle; early detection of clinical relapses; effects of pharmacological treatment and management of side effects; stress management techniques; and problem-solving techniques. The interventions were delivered by trained psychiatrists, attending an ad hoc brief course on the main characteristics of the interventions. All characteristics of the two interventions are reported in Sampogna et al. (2018).
This study was conducted in accordance with globally accepted standards of good practice, in agreement with the Declaration of Helsinki and with local regulations. The study protocol was formally approved by the Ethics Committee of the Coordinating Center in January 2017 (approval number: 64). Trial registration number is 2015C7374S.
Statistical analyses
Statistical analyses were conducted according to the “Intention To Treat” principle. Missing data were handled using the Last Observation Carried Forward. Descriptive statistics and frequency tables were used to assess patients’ socio-demographic and clinical characteristics. Chi-square with multiple comparisons and ANOVA with Bonferroni corrections were adopted to detect differences in the levels of adherence to treatments. Bivariate analyses were performed in order to evaluate the association between levels of adherence and severity of clinical symptoms. Descriptive statistics (frequency table, means and standard deviation) were calculated for both experimental and control groups at baseline and at the end of the intervention. Differences in sociodemographic and clinical characteristics among the two groups at baseline and at the end of the intervention were tested using χ2 or t-test for independent samples, as appropriate.
Generalized estimating equation (GEE) models were used for evaluating the impact of the experimental intervention on the primary outcome. GEE models allow estimation of population-averaged models in repeated-measures data. Control vs. intervention interaction terms assessed changes between groups over time; Wald tests determined whether joint effects of time-by-group equalled zero. Age and center were included as time-invariant covariates; time-varying covariates included medications, cognitive functioning, age, gender, and diagnosis of mental disorder. GEE models with a normal distribution and identity link were used. Covariate-adjusted results using robust estimates of standard errors are reported. All models were adjusted for diagnosis, pharmacological treatments, duration of illness, and educational level. Pharmacological treatments (i.e., mood stabilizers, tricyclic antidepressants, new-generation antidepressants, first- and second-generation antipsychotics) and psychiatric diagnoses (i.e., depressive disorder, bipolar disorders, psychosis) were included in the regression models as dummy variables.
The level of statistical significance was set at p < 0.05 and statistical analyses were performed using the Statistical Package for Social Sciences (SPSS), version 26.0, and STATA, version 15.
Results
The sample consists of 401 patients, with a mean age of 45.6 years (±11.8), mainly female (57%, N = 227), single (71.4%, N = 287), and unemployed (64.3%, N = 258). The mean duration of illness was 16.3 (±17.8) years, with a median value of 15 years, Inter Quartile Range, INR: 6;23; patients were in charge at the local mental health centre for 5.9 (±6.9) years, with a median value of 3 years (IQR: 1; 9), with a diagnosis of bipolar disorder (43.4%; N = 174), psychotic spectrum disorders (29.6%; N = 120) and major depressive disorder (27.1%; N = 108) (Table 1).
The levels of anxiety/depressive symptoms were moderate (8.8 ± 3.1) as well as the level of personal functioning (65.5 ± 15.1 at the PSP scale). All patients were receiving a pharmacological drug treatment; in particular, 59% (N = 236) were treated with a second-generation antipsychotic and 65.8% (N = 264) with a mood stabilizer.
39.8% of patients reported a good adherence to the prescribed pharmacological treatments (Figure 1). At bivariate analyses, age, gender, duration of illness and type of the disorder did not influence patients’ adherence to medications. A significant inverse correlation was found between adherence and quality of life (Rho di Person: −0.140, p <.005).
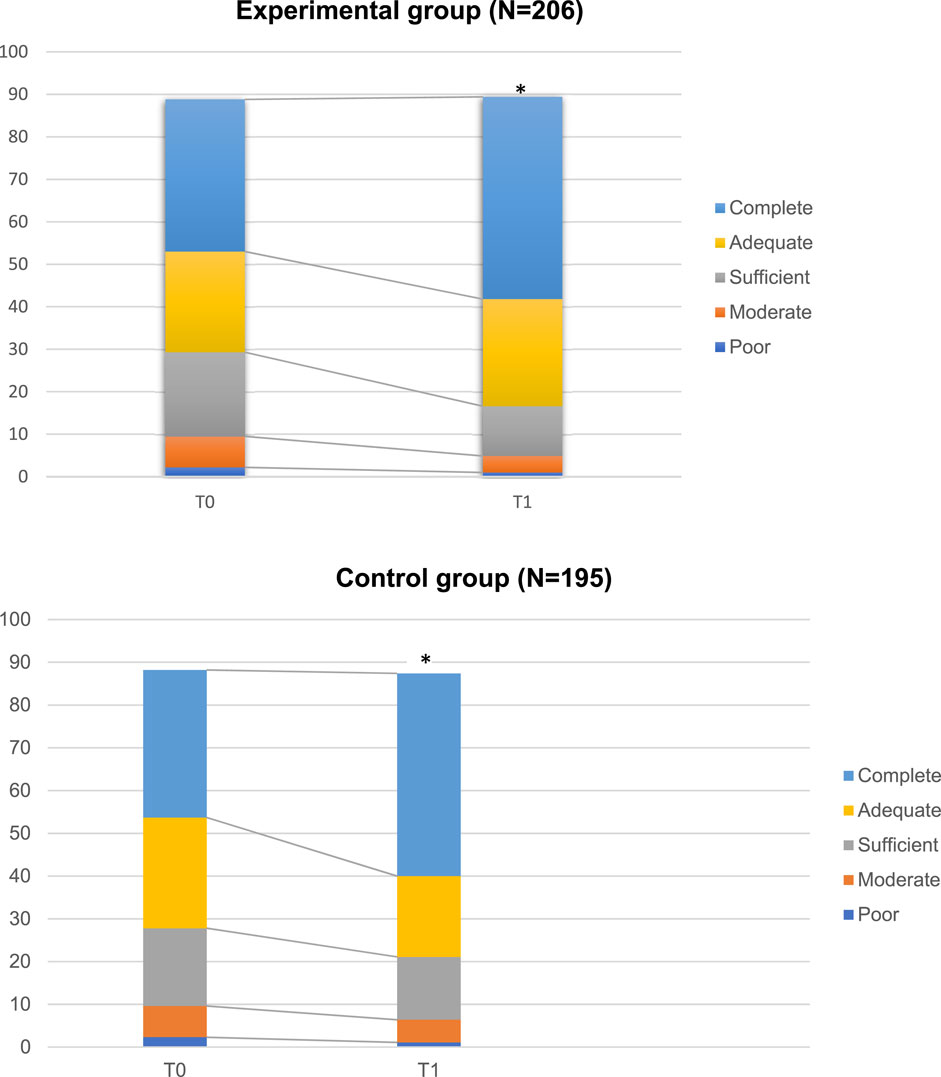
FIGURE 1. Levels of adherence to pharmacological treatments in the study sample. The weight of the different bars corresponds to the frequency of responses in the different categories of adherence, as evaluated at the Morisky scale. In particular, poor category indicates a condition where all items were scored as “yes”, while “complete adherence”, indicates a condition where all items were scored as “no” *p < 0.005.
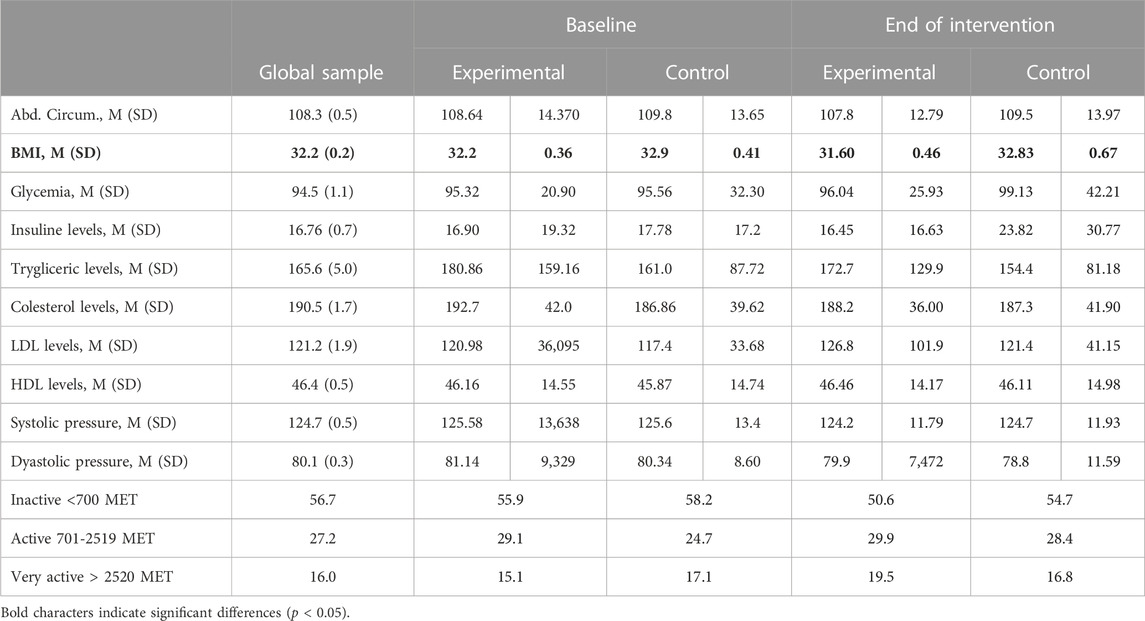
The majority of patients were obese (63.1%, N = 253), with a mean BMI of 32.2 (0.2); 53.4% of them were suffering from the metabolic syndrome. All metabolic parameters have been reported in Table 2. Although 29.4% of patients (N = 118) declared to perform physical activity, only 16.1% were found to be very physically active at the IPAQ scale. The most frequently practiced sport activities were walking (52.1%, N = 62), going to the gym (21.8%, N = 26) and playing football (7.5%, N = 9).
34.5% of patients (N = 138) reported a frequent use of alcohol; 41% of them (N = 163) declared to smoking and 36.3% of them never tried to quit smoking.
There were no significant differences between the experimental (N = 206) and the control (N = 195) groups in any of the considered domains. Further data are available in Supplementary Table S1.
Longitudinal evaluation of levels of physical activity and adherence to treatments
Hundred and three patients from the experimental group and 95 patients from the control group were re-assessed at 6 months, with an attrition rate of 49.4%. Drop-outs were due to lack of time, reduced interest in the intervention, other personal commitments, and clinical relapses.
At 6 months, the levels of adherence to pharmacological treatment changed from 35.8% at baseline to 47.6% at the end of the intervention (p <.005) in the experimental group, while the levels of physical activity did not change between baseline (T0: 6.3%) and 6- month (T1: 9.7%), although a reduction of BMI, weight and other metabolic parameters was found.
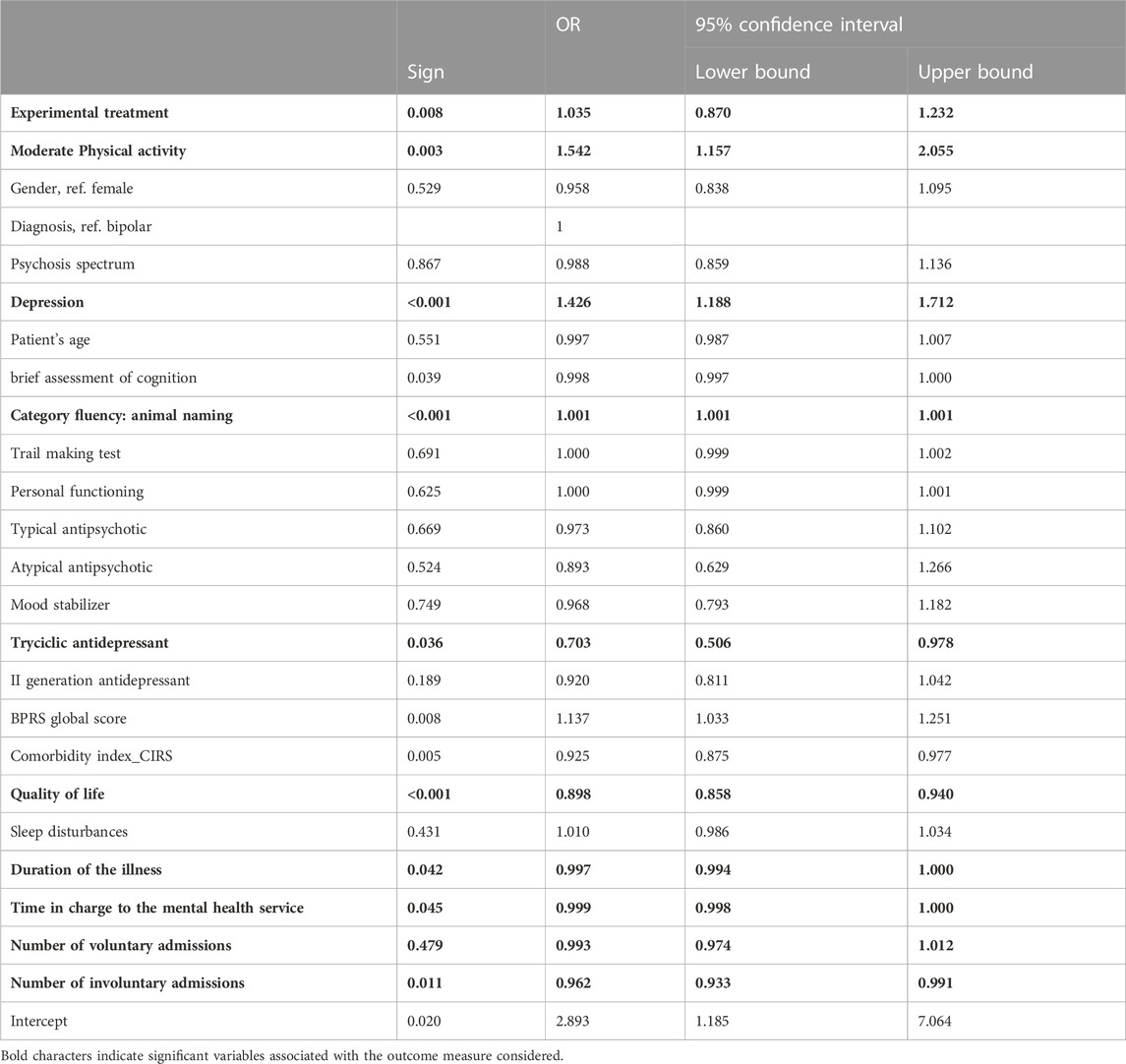
The GEE model showed a significant effect of physical activity on adherence to treatments. In particular, at the end of the intervention, patients performing moderate physical activity reported a two-point improvement of adherence to pharmacological treatments (odds ratio [OR]: 1,542; 95% confidence intervals [CI]: 1,157–2,055; p < 0.001). Other factors positively influencing adherence were having a diagnosis of major depression (p < 0.001), a better cognitive functioning (p < 0.001) and quality of life (p < 0.05), a shorter duration of illness (p < 0.001) and time in contact with the local mental health centre (p < 0.001). Surprisingly, treatment adherence was not influenced by symptom severity and type of pharmacological treatment (Table 3).
Discussion
Patients’ adherence to treatments is a complex phenomenon posing a significant burden on health professionals, users and carers, and on the healthcare system in general (Atreja et al., 2005).
Lack of adherence is associated with negative consequences on patients’ outcomes, including lack of efficacy of treatments, poor clinical outcome, and worsening of patient health status. This clinical worsening usually requires the subsequent prescription of more drugs, increasing dosages of current drugs, cross-titration of more drugs and other add-on or replacement strategies, which can lead to increased healthcare costs, more frequent consultations, higher rates of emergency services and of hospitalization rates (Semahegn et al., 2020; Gosh et al., 2022; McCutcheon et al., 2022).
Several strategies have been developed in recent years to enhance patient adherence, although the target of “complete adherence” to treatments has not been reached yet (Loots et al., 2021).
In our study on real-world patients suffering from severe mental disorders, 40% of participants reported a good adherence to pharmacological treatments. This finding is slightly lower compared to that reported by the WHO in developed countries, who found that “adherence among patients suffering from chronic diseases averages 50%” (WHO, 2003). However, both our and WHO findings highlight the need to improve medication adherence among patients with chronic physical and mental illnesses (Fernandez-Lazaro et al., 2019; Laranjeira et al., 2023). The lower adherence rates found in people with severe mental disorders compared to those reported by people suffering from other chronic conditions can be due to the presence of specific symptoms, such as cognitive impairment in schizophrenia (El-Missiry et al., 2015; Mendes et al., 2019; Senner et al., 2023); inflated mood in bipolar disorder or hopelessness in major depressive disorder (Chauhan et al., 2021). Indeed, in our sample having a psychiatric diagnosis of schizophrenia and/or bipolar disorder did not influence patients’ adherence to treatments, which is partially in line with findings from Ghosh et al. (2022). This would imply that all psychiatric symptoms have the same weight on adherence rates, and that other causes common to all mental disorders can play a role, such as stigma, prejudices and misconceptions against psychiatric treatments (Kamaradova et al., 2016). Informative campaigns should be carried out at the population level in order to reduce such misconceptions, helping people who take these medications not to feel stigmatized (Corrigan, 2022; Sum et al., 2022).
No significant association was found between illness severity and medication non-adherence. However, lack or poor adherence to medications usually worsens illness severity which, in turn, reduces insight into the illness and has significant adverse clinical outcomes (Wu and Moser, 2018).
Moreover, several socio-demographic variables, including patient’s age and gender, as well as levels of personal functioning and presence of any physical comorbidities did not have any specific impact in modifying the levels of medication adherence. In particular, studies evaluating gender-based difference in medication adherence have highlighted that women are consistently less likely than men to be adherent with their diabetes and cardiovascular medications (Venditti et al., 2023). Some authors argued that this difference may be explained by the fact that women experience more drug side effects than men, while others pointed out that differences in medication adherence are largely due to the type of disorders considered. It should be that the core psychopathological features of different mental disorders play a crucial role in modifying medication adherence, more than socio-demographic features (Semahegn et al., 2020).
At the end of the psychosocial intervention, patients showing a significant improvement in treatments’ adherence also reported increased moderate physical activity. This association can be explained considering the multiple components of our experimental intervention, that include specific sessions dedicated to treatment adherence and to physical activity, with a synergic positive effect of both sessions. Several studies showed that patient’s knowledge about treatments is the strongest predictor of adherence (Jankowska-Polańska et al., 2016; López-Pintor et al., 2021; Kanyongo and Ezugwu, 2023), particularly in patients with severe mental disorders, who can have more difficulties than other patients in understanding the need for taking pharmacological drugs. It can be that the improved adherence found in our sample at the end of the intervention is due to the inclusion of psychoeducational components, motivational interview and cognitive-behavioral techniques (Vieta, 2005; Depp et al., 2008; Okazaki et al., 2023). However, this finding deserves confirmation in long-term studies with larger samples.
The positive association between improved adherence and higher levels of moderate physical activity highlights that physical activity improves global health and functional status. Moreover, it also shows that exercise/physical activity training shall be included in the multilevel personalized treatment for people with severe mental disorders, as already happens in other chronic conditions, such as cardiovascular disease and diabetes mellitus. As recently pointed out by the European Association for Sport and Mental Health (EASMH), the dissemination of sport-based psychosocial interventions for people with severe mental disorders in routine clinical practice is still very low, although considerable evidence is accumulating regarding their efficacy (Sampogna et al., 2022c).
The present study has some limitations, which should be acknowledged. First, the inclusion of patients in a stable phase of the disorder might have biased the results, since they may not be the patients usually seen in routine clinical practice. However, this potential bias has been managed by adopting the GEE model for evaluating the effect of the interventions on the primary outcome (i.e., medication adherence); moreover, all statistical analyses have been controlled for confounding variables, such as type of pharmacological treatment and severity of clinical symptoms. Second, adherence to pharmacological treatments has been evaluated only through a self-reported questionnaire, without other objective measures, which might have led to a potential recall bias. However, introducing more sophisticated biological and clinical evaluations might have hampered the conduction of the study, also because the experimental intervention was developed with the aim to be easily used in routine clinical practice, without a sophisticated training for mental health professionals and high costs. A final limitation is the high drop-out of almost 50%. Reasons for such a high attrition rate vary including the duration of the interventions (which are considered too long by many patients), too structured and manualized approaches (which are considered difficult to follow by many patients), difficulties to travel to the place where the intervention is provided or clinical relapses. In particular, the high attrition should have biased towards those patients more prone to follow recommendations regarding medications as well as practicing physical activity. However, the attrition rate found in our study is similar to that found in other studies on psychosocial interventions. Moreover, the sample size was adequate according to the power analysis, which supports the evidence that the moderate physical activity can improve the levels of adherence.
Thus, future approaches should consider to have a lower total number of sessions, a less structured approach, and the inclusion of online sessions to reduce the need to travel biweekly.
Conclusion
The poor rate of adherence to treatment reported by patients affected from chronic mental and physical disorders is considered by the WHO an “invisible epidemic”. Poor adherence to treatments is one of the most important—yet modifiable—causes of low efficacy of medications, treatment failure, re-hospitalization, delayed remission and recovery. Therefore, the identification of innovative, multilevel, integrated strategies is essential for overcoming this public health emergency (Kestel, 2022). The promotion of moderate physical activity, which was integrated in our experimental intervention, can represent a valid approach to improve treatment adherence in patients with severe mental disorders. Physical activity exercises, which can be easily implemented in routine clinical practice, are associated with improved outcome. Further studies are needed in larger samples and in acutely severe patients with mental disorders.
LIFESTYLE working group
Giulia Amatori, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; Ileana Andriola, Department of Translational Biomedicine and Neuroscience, University of Bari Aldo Moro; Emanuela Bianciardi, Department of Systems Medicine, University of Rome Tor Vergata, Rome, Italy; Laura Capobianco, Section of Psychiatry, Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Italy; Pierluigi Catapano, Department of Psychiatry, University of Campania “L. VanvitellI”, Naples, Italy; Salvatore Cipolla, Department of Psychiatry, University of Campania “L. VanvitellI”, Naples, Italy; Ivan Cremone, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; Bianca Della Rocca, Department of Psychiatry, University of Campania “L. VanvitellI”, Naples, Italy; Giorgio Di Lorenzo, Department of Systems Medicine, University of Rome Tor Vergata, Rome, Italy; Ramona Di Stefano, Department of Biotechnological and Applied Clinical Sciences, University of L’Aquila, Italy; Francesca Pacitti, Department of Biotechnological and Applied Clinical Sciences, University of L’Aquila, Italy; Pierluigi Selvaggi, Department of Translational Biomedicine and Neuroscience, University of Bari Aldo Moro; Domenico Zampogna, Section of Psychiatry, Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Italy.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethical review Board University of Campania Vanvitelli. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GS: Conceptualization, Formal Analysis, Methodology, Writing–original draft. ML: Writing–review and editing. MDV: Data curation, Writing–review and editing. CT: Methodology, Writing–review and editing. ED: Writing–review and editing, Validation. AnR: Investigation, Writing–review and editing. AlR: Writing–review and editing. RR: Writing–review and editing. MA: Writing–review and editing. PC: Writing–review and editing. AS: Writing–review and editing. CN: Writing–review and editing. LD: Writing–review and editing. BC: Writing–review and editing. LG: Writing–review and editing. AF: Writing–review and editing, Conceptualization, Investigation, Writing–original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1285383/full#supplementary-material
References
Aggarwal, P., Woolford, S. J., and Patel, H. P. (2020). Multi-morbidity and polypharmacy in older people: challenges and opportunities for clinical practice. Geriatr. (Basel) 5 (4), 85. doi:10.3390/geriatrics5040085
Arango, C., Dragioti, E., Solmi, M., Cortese, S., Domschke, K., Murray, R. M., et al. (2021). Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World Psychiatry 20 (3), 417–436. doi:10.1002/wps.20894
Atreja, A., Bellam, N., and Levy, S. R. (2005). Strategies to enhance patient adherence: making it simple. MedGenMed 7 (1), 4.
Baron, D., and Noordsy, D. (2021). The lifestyle psychiatry project of the WPA section on medicine, psychiatry and primary care. World Psychiatry 20 (3), 454–455. doi:10.1002/wps.20898
Baylé, F. J., Tessier, A., Bouju, S., and Misdrahi, D. (2015). Medication adherence in patients with psychotic disorders: an observational survey involving patients before they switch to long-acting injectable risperidone. Patient Prefer Adherence 9, 1333–1341. doi:10.2147/PPA.S89748
Brown, M. T., and Bussell, J. K. (2011). Medication adherence: WHO cares? Mayo Clin. Proc. 86 (4), 304–314. doi:10.4065/mcp.2010.0575
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi:10.1016/0165-1781(89)90047-4
Caqueo-Urízar, A., Urzúa, A., Mena-Chamorro, P., and Bravo de la Fuente, J. (2021). Effects of adherence to pharmacological treatment on the recovery of patients with schizophrenia. Healthc. (Basel) 9 (9), 1230. doi:10.3390/healthcare9091230
Chatoo, A., and Lee, S. (2022). Association of coping strategies and medication adherence: a systematic review. Innov. Pharm. 13 (3), 10. doi:10.24926/iip.v13i3.4991
Chauhan, N., Chakrabarti, S., and Grover, S. (2021). Identifying poor adherence in outpatients with bipolar disorder: a comparison of different measures. J. Neurosci. Rural. Pract. 13 (1), 12–22. doi:10.1055/s-0041-1736155
Correll, C. U., Solmi, M., Croatto, G., Schneider, L. K., Rohani-Montez, S. C., Fairley, L., et al. (2022). Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry 21 (2), 248–271. doi:10.1002/wps.20994
Corrigan, P. W. (2022). Coming out proud to erase the stigma of mental illness. World Psychiatry 21 (3), 388–389. doi:10.1002/wps.21016
Craig, C. L., Marshall, A. L., Sjöström, M., Bauman, A. E., Booth, M. L., Ainsworth, B. E., et al. (2003). International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
Cramer, J. A., Roy, A., Burrell, A., Fairchild, C. J., Fuldeore, M. J., Ollendorf, D. A., et al. (2008). Medication compliance and persistence: terminology and definitions. Value Health 11 (1), 44–47. doi:10.1111/j.1524-4733.2007.00213.x
Cuijpers, P., Quero, S., Noma, H., Ciharova, M., Miguel, C., Karyotaki, E., et al. (2021). Psychotherapies for depression: a network meta-analysis covering efficacy, acceptability and long-term outcomes of all main treatment types. World Psychiatry 20 (2), 283–293. doi:10.1002/wps.20860
Davidson, L., and Tondora, J. (2022). Person-centred care planning as foundational to clinical practice. World Psychiatry 21 (1), 1–2. doi:10.1002/wps.20922
Dell'Osso, B., Albert, U., Carrà, G., Pompili, M., Nanni, M. G., Pasquini, M., et al. (2020). How to improve adherence to antidepressant treatments in patients with major depression: a psychoeducational consensus checklist. Ann. Gen. Psychiatry 19, 61. doi:10.1186/s12991-020-00306-2
Depp, C. A., Moore, D. J., Patterson, T. L., Lebowitz, B. D., and Jeste, D. V. (2008). Psychosocial interventions and medication adherence in bipolar disorder. Dialogues Clin. Neurosci. 10 (2), 239–250. doi:10.31887/DCNS.2008.10.2/cadepp
De Rosa, C., Sampogna, G., Luciano, M., Del Vecchio, V., Pocai, B., Borriello, G., et al. (2017). Improving physical health of patients with severe mental disorders: a critical review of lifestyle psychosocial interventions. Expert Rev. Neurother. 17 (7), 667–681. doi:10.1080/14737175.2017.1325321
Drayton, M., Birchwood, M., and Trower, P. (1998). Early attachment experience and recovery from psychosis. Br. J. Clin. Psychol. 37, 269–284. doi:10.1111/j.2044-8260.1998.tb01385.x
El-Missiry, A., Elbatrawy, A., El Missiry, M., Moneim, D. A., Ali, R., and Essawy, H. (2015). Comparing cognitive functions in medication adherent and non-adherent patients with schizophrenia. J. Psychiatr. Res. 70, 106–112. doi:10.1016/j.jpsychires.2015.09.006
Elowe, J., Ramain, J., Solida, A., Conus, P., and Golay, P. (2022). Dynamics between insight and medication adherence in first-episode psychosis: study of 3-year trajectories. Eur. Psychiatry 65 (1), e49. doi:10.1192/j.eurpsy.2022.2305
Fernandez-Lazaro, C. I., García-González, J. M., Adams, D. P., Fernandez-Lazaro, D., Mielgo-Ayuso, J., Caballero-Garcia, A., et al. (2019). Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study. BMC Fam. Pract. 20 (1), 132. doi:10.1186/s12875-019-1019-3
Fiorillo, A., Barlati, S., Bellomo, A., Corrivetti, G., Nicolò, G., Sampogna, G., et al. (2020). The role of shared decision-making in improving adherence to pharmacological treatments in patients with schizophrenia: a clinical review. Ann. Gen. Psychiatry 19, 43. doi:10.1186/s12991-020-00293-4
Firth, J., Solmi, M., Wootton, R. E., Vancampfort, D., Schuch, F. B., Hoare, E., et al. (2020). A meta-review of "lifestyle psychiatry": the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry 19 (3), 360–380. doi:10.1002/wps.20773
Fragoulis, C., Prentakis, A. G., Kontogianni, E., Polyzos, D., Tsioufis, P. A., Fragouli, D., et al. (2023). Medication adherence in relation with physical activity in hypertensive patients: data from a behavioral cardiology unit. Eur. J. Prev. Cardiol. 30, 2023doi. doi:10.1093/eurjpc/zwad125.132
Fulford, K. W. M., and Handa, A. (2021). New resources for understanding patients' values in the context of shared clinical decision-making. World Psychiatry 20 (3), 446–447. doi:10.1002/wps.20902
Fusar-Poli, P., Estradé, A., Stanghellini, G., Venables, J., Onwumere, J., Messas, G., et al. (2022). The lived experience of psychosis: a bottom-up review co-written by experts by experience and academics. World Psychiatry 21 (2), 168–188. doi:10.1002/wps.20959
Ghosh, P., Balasundaram, S., Sankaran, A., Chandrasekaran, V., Sarkar, S., and Choudhury, S. (2022). Factors associated with medication non-adherence among patients with severe mental disorder - a cross sectional study in a tertiary care centre. Explor Res. Clin. Soc. Pharm. 7, 100178. doi:10.1016/j.rcsop.2022.100178
Harmancı, P., and Yıldız, E. (2023). The effects of psychoeducation and motivational interviewing on treatment adherence and functionality in individuals with bipolar disorder. Arch. Psychiatr. Nurs. 45, 89–100. doi:10.1016/j.apnu.2023.04.026
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., and Fagerström, K. O. (1991). The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 (9), 1119–1127. doi:10.1111/j.1360-0443.1991.tb01879.x
Højlund, M., Andersen, K., Ernst, M. T., Correll, C. U., and Hallas, J. (2022). Use of low-dose quetiapine increases the risk of major adverse cardiovascular events: results from a nationwide active comparator-controlled cohort study. World Psychiatry 21 (3), 444–451. doi:10.1002/wps.21010
Jankowska-Polańska, B., Uchmanowicz, I., Dudek, K., and Mazur, G. (2016). Relationship between patients' knowledge and medication adherence among patients with hypertension. Patient Prefer Adherence 10, 2437–2447. doi:10.2147/PPA.S117269
Kamaradova, D., Latalova, K., Prasko, J., Kubinek, R., Vrbova, K., Mainerova, B., et al. (2016). Connection between self-stigma, adherence to treatment, and discontinuation of medication. Patient Prefer Adherence 10, 1289–1298. doi:10.2147/PPA.S99136
Kanyongo, W., and Ezugwu, A. E. (2023). Feature selection and importance of predictors of non-communicable diseases medication adherence from machine learning research perspectives. Inf. Med. Unlocked 38, 101232, 101232. doi:10.1016/j.imu.2023.101232
Kern, R. S., Nuechterlein, K. H., Green, M. F., Baade, L. E., Fenton, W. S., Gold, J. M., et al. (2008). The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. Am. J. Psychiatry 165, 214–220. doi:10.1176/appi.ajp.2007.07010043
Kestel, D. (2022). Transforming mental health for all: a critical role for specialists. World Psychiatry 21 (3), 333–334. doi:10.1002/wps.21030
Killaspy, H., Harvey, C., Brasier, C., Brophy, L., Ennals, P., Fletcher, J., et al. (2022). Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry 21 (1), 96–123. doi:10.1002/wps.20940
Kim, H., Turiano, N. A., Forbes, M. K., Kotov, R., Krueger, R. F., and Eaton, N. R.HiTOP Utility Workgroup (2021). Internalizing psychopathology and all-cause mortality: a comparison of transdiagnostic vs. diagnosis-based risk prediction. World Psychiatry 20 (2), 276–282. doi:10.1002/wps.20859
Lam, W. Y., and Fresco, P. (2015). Medication adherence measures: an overview. Biomed. Res. Int. 2015, 217047. doi:10.1155/2015/217047
Laranjeira, C., Carvalho, D., Valentim, O., Moutinho, L., Morgado, T., Tomás, C., et al. (2023). Therapeutic adherence of people with mental disorders: an evolutionary concept analysis. Int. J. Environ. Res. Public Health 20 (5), 3869. doi:10.3390/ijerph20053869
Leichsenring, F., Steinert, C., Rabung, S., and Ioannidis, J. P. A. (2022). The efficacy of psychotherapies and pharmacotherapies for mental disorders in adults: an umbrella review and meta-analytic evaluation of recent meta-analyses. World Psychiatry 21 (1), 133–145. doi:10.1002/wps.20941
Lemay, J., Waheedi, M., Al-Sharqawi, S., and Bayoud, T. (2018). Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adherence 12, 1687–1698. doi:10.2147/PPA.S169236
Linn, B. S., Linn, M. W., and Gurel, L. (1968). Cumulative illness rating scale. J. Am. Geriatr. Soc. 16, 622–626. doi:10.1111/j.1532-5415.1968.tb02103.x
Loots, E., Goossens, E., Vanwesemael, T., Morrens, M., Van Rompaey, B., and Dilles, T. (2021). Interventions to improve medication adherence in patients with schizophrenia or bipolar disorders: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 18 (19), 10213. doi:10.3390/ijerph181910213
López-Pintor, E., Grau, J., and Lumbreras, B. (2021). Patient's awareness on COPD is the strongest predictor of persistence and adherence in treatment-naïve patients in real life: a prospective cohort study. BMC Pulm. Med. 21 (1), 388. doi:10.1186/s12890-021-01754-6
Luciano, M., Sampogna, G., Amore, M., Bertolino, A., Dell'Osso, L., Rossi, A., et al. (2022). Improving physical activity and diet in patients with severe mental disorders: results from the LIFESTYLE multicentric, real-world randomized controlled trial. Psychiatry Res. 317, 114818. doi:10.1016/j.psychres.2022.114818
Lukoff, D., Nuechterlein, K. H., and Ventura, J. (1986). Appendix A: manual for expanded brief psychiatric rating scale (BPRS). Schizophre Bull. 12, 594–602.
Mahindru, A., Patil, P., and Agrawal, V. (2023). Role of physical activity on mental health and well-being: a review. Cureus 15 (1), e33475. doi:10.7759/cureus.33475
Marrie, R. A., and Bernstein, C. N. (2021). Psychiatric comorbidity in immune-mediated inflammatory diseases. World Psychiatry 20 (2), 298–299. doi:10.1002/wps.20873
Marventano, S., Mistretta, A., Platania, A., Galvano, F., and Grosso, G. (2016). Reliability and relative validity of a food frequency questionnaire for Italian adults living in Sicily, Southern Italy. Int. J. Food Sci. Nutr. 67, 857–864. doi:10.1080/09637486.2016.1198893
Masa-Font, R., Fernández-San-Martín, M. I., Martín López, L. M., Alba Muñoz, A. M., Oller Canet, S., Martín Royo, J., et al. (2015). The effectiveness of a program of physical activity and diet to modify cardiovascular risk factors in patients with severe mental illness after 3-month follow-up: CAPiCOR randomized clinical trial. Eur. Psychiatry 30 (8), 1028–1036. doi:10.1016/j.eurpsy.2015.09.006
McCutcheon, R. A., Pillinger, T., Efthimiou, O., Maslej, M., Mulsant, B. H., Young, A. H., et al. (2022). Reappraising the variability of effects of antipsychotic medication in schizophrenia: a meta-analysis. World Psychiatry 21 (2), 287–294. doi:10.1002/wps.20977
McIntyre, R. S., Alda, M., Baldessarini, R. J., Bauer, M., Berk, M., Correll, C. U., et al. (2022). The clinical characterization of the adult patient with bipolar disorder aimed at personalization of management. World Psychiatry 21 (3), 364–387. doi:10.1002/wps.20997
Mendes, R., Martins, S., and Fernandes, L. (2019). Adherence to medication, physical activity and diet in older adults with diabetes: its association with cognition, anxiety and depression. J. Clin. Med. Res. 11 (8), 583–592. doi:10.14740/jocmr3894
Mirhaj Mohammadabadi, M. S., Mohammadsadeghi, H., Eftekhar Adrebili, M., Partovi Kolour, Z., Kashaninasab, F., Rashedi, V., et al. (2022). Factors associated with pharmacological and psychotherapy treatments adherence in patients with borderline personality disorder. Front. Psychiatry 13, 1056050. doi:10.3389/fpsyt.2022.1056050
Morisky, D. E., Green, L. W., and Levine, D. M. (1986). Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 24, 67–74. doi:10.1097/00005650-198601000-00007
Morosini, P. L., Magliano, L., Brambilla, L., Ugolini, S., and Pioli, R. (2000). Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social funtioning. Acta Psychiatr. Scand. 101, 323–329. doi:10.1111/j.1600-0447.2000.tb10933.x
Novick, D., Montgomery, W., Treuer, T., Aguado, J., Kraemer, S., and Haro, J. M. (2015). Relationship of insight with medication adherence and the impact on outcomes in patients with schizophrenia and bipolar disorder: results from a 1-year European outpatient observational study. BMC Psychiatry 15, 189. doi:10.1186/s12888-015-0560-4
Okazaki, T., Nakatsu, K., Asaoka, S., and Okamura, H. (2023). Factors associated with long-term medication adherence in patients who participated in a short-term group psychoeducation program for bipolar disorder. Psychiatr. Q. 94 (2), 265–280. doi:10.1007/s11126-023-10031-0
Okobi, O. E., Agazie, O., Ayisire, O. E., Babalola, F., Dick, A. I., Akinsola, Z., et al. (2022). Approaches to medication administration in patients with lack of insight. Cureus 14 (7), e27143. doi:10.7759/cureus.27143
Ostuzzi, G., Bertolini, F., Tedeschi, F., Vita, G., Brambilla, P., Del Fabro, L., et al. (2022). Oral and long-acting antipsychotics for relapse prevention in schizophrenia-spectrum disorders: a network meta-analysis of 92 randomized trials including 22,645 participants. World Psychiatry 21 (2), 295–307. doi:10.1002/wps.20972
Priebe, S., Huxley, P., Knight, S., and Evans, S. (1999). Application and results of the manchester short assessment of quality of life (MANSA). Int. J. Soc. Psychiatry 45, 7–12. doi:10.1177/002076409904500102
Raistrick, D., Bradshaw, J., Tober, G., Weiner, J., Allison, J., and Healey, C. (1994). Development of the Leeds Dependence Questionnaire (LDQ): a questionnaire to measure alcohol and opiate dependence in the context of a treatment evaluation package. Addiction 89, 563–572. doi:10.1111/j.1360-0443.1994.tb03332.x
Ritsher, J., Otilingam, P. G., and Grajales, M. (2003). Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 121, 31–49. doi:10.1016/j.psychres.2003.08.008
Roe, D., Slade, M., and Jones, N. (2022). The utility of patient-reported outcome measures in mental health. World Psychiatry 21 (1), 56–57. doi:10.1002/wps.20924
Sampogna, G., Borgi, M., Collacchi, B., Cirulli, F., Cerino, S., Rullo, S., et al. (2022c). Using sport-based interventions for people with severe mental disorders: results from the European EASMH study. Int. Rev. Psychiatry 34 (7-8), 837–847. doi:10.1080/09540261.2022.2106122
Sampogna, G., Di Vincenzo, M., Della Rocca, B., Mancuso, E., Volpicelli, A., Perris, F., et al. (2022b). Physical comorbidities in patients with severe mental disorders: a brief narrative review on current challenges and practical implications for professionals. Riv. Psichiatr. 57 (6), 251–257. doi:10.1708/3922.39071
Sampogna, G., Fiorillo, A., Luciano, M., Del Vecchio, V., Steardo, L., Pocai, B., et al. LIFESTYLE Working Group (2018). A randomized controlled trial on the efficacy of a psychosocial behavioral intervention to improve the lifestyle of patients with severe mental disorders: study protocol. Front. Psychiatry 9, 235. doi:10.3389/fpsyt.2018.00235
Sampogna, G., Luciano, M., Di Vincenzo, M., Andriola, I., D'Ambrosio, E., Amore, M., et al. Working Group LIFESTYLE (2022a). The complex interplay between physical activity and recovery styles in patients with severe mental disorders in a real-world multicentric study. Front. Psychiatry 13, 945650. doi:10.3389/fpsyt.2022.945650
Saqib, Z. A., Dai, J., Menhas, R., Mahmood, S., Karim, M., Sang, X., et al. (2020). Physical activity is a medicine for non-communicable diseases: a survey study regarding the perception of physical activity impact on health wellbeing. Risk Manag. Healthc. Policy 13, 2949–2962. doi:10.2147/RMHP.S280339
Semahegn, A., Torpey, K., Manu, A., Assefa, N., Tesfaye, G., and Ankomah, A. (2020). Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst. Rev. 9 (1), 17. doi:10.1186/s13643-020-1274-3
Senner, F., Hiendl, L., Bengesser, S., Adorjan, K., Anghelescu, I. G., Baune, B. T., et al. (2023). Medication adherence and cognitive performance in schizophrenia-spectrum and bipolar disorder: results from the PsyCourse Study. Transl. Psychiatry 13 (1), 99. doi:10.1038/s41398-023-02373-x
Speyer, H., Christian Brix Nørgaard, H., Birk, M., Karlsen, M., Storch Jakobsen, A., Pedersen, K., et al. (2016). The CHANGE trial: no superiority of lifestyle coaching plus care coordination plus treatment as usual compared to treatment as usual alone in reducing risk of cardiovascular disease in adults with schizophrenia spectrum disorders and abdominal obesity. World Psychiatry 15 (2), 155–165. doi:10.1002/wps.20318
Sum, M. Y., Chan, S. K. W., Suen, Y. N., Cheung, C., Hui, C. L. M., Chang, W. C., et al. (2022). The role of education level on changes in endorsement of medication treatment and perceived public stigma towards psychosis in Hong Kong: comparison of three population-based surveys between 2009 and 2018. BMC Psychiatry 22 (1), 641. doi:10.1186/s12888-022-04288-1
Suokas, K., Hakulinen, C., Sund, R., Kampman, O., and Pirkola, S. (2022). Mortality in persons with recent primary or secondary care contacts for mental disorders in Finland. World Psychiatry 21 (3), 470–471. doi:10.1002/wps.21027
Swift, J. K., Mullins, R. H., Penix, E. A., Roth, K. L., and Trusty, W. T. (2021). The importance of listening to patient preferences when making mental health care decisions. World Psychiatry 20 (3), 316–317. doi:10.1002/wps.20912
Theofilou, P., and Saborit, A. R. (2013). Adherence and physical activity. Health Psychol. Res. 1 (1), e6. doi:10.4081/hpr.2013.e6
Torres-Robles, A., Wiecek, E., Tonin, F. S., Benrimoj, S. I., Fernandez-Llimos, F., and Garcia-Cardenas, V. (2018). Comparison of interventions to improve long-term medication adherence across different clinical conditions: a systematic review with network meta-analysis. Front. Pharmacol. 9, 1454. doi:10.3389/fphar.2018.01454
Venditti, V., Bleve, E., Morano, S., and Filardi, T. (2023). Gender-related factors in medication adherence for metabolic and cardiovascular health. Metabolites 13 (10), 1087. doi:10.3390/metabo13101087
Vetrano, D. L., Bianchini, E., Onder, G., Cricelli, I., Cricelli, C., Bernabei, R., et al. (2017). Poor adherence to chronic obstructive pulmonary disease medications in primary care: role of age, disease burden and polypharmacy. Geriatr. Gerontol. Int. 17 (12), 2500–2506. doi:10.1111/ggi.13115
Vieta, E. (2005). Improving treatment adherence in bipolar disorder through psychoeducation. J. Clin. Psychiatry 66 (Suppl. 1), 24–29.
World Health Organisation (2003). Adherence to long-term therapies: evidence for action. Geneva: WHO. Available from http://www.who.int/chp/knowledge/publications/adherence_report/en.
Keywords: adherence, physical activity, severe mental disorder, lifestyle, personalization
Citation: Sampogna G, Luciano M, Di Vincenzo M, Toni C, D’Ambrosio E, Rampino A, Rossi A, Rossi R, Amore M, Calcagno P, Siracusano A, Niolu C, Dell’Osso L, Carpita B, LIFESTYLE Working Group and Fiorillo A (2023) Physical activity influences adherence to pharmacological treatments in patients with severe mental disorders: results from the multicentric, randomized controlled LIFESTYLE trial. Front. Pharmacol. 14:1285383. doi: 10.3389/fphar.2023.1285383
Received: 29 August 2023; Accepted: 20 November 2023;
Published: 11 December 2023.
Edited by:
Maria Teresa Herdeiro, University of Aveiro, PortugalReviewed by:
Renato de Filippis, University Magna Graecia of Catanzaro, ItalyDiego Quattrone, King’s College London, United Kingdom
Ana Plácido, Instituto Politécnico da Guarda, Portugal
Copyright © 2023 Sampogna, Luciano, Di Vincenzo, Toni, D’Ambrosio, Rampino, Rossi, Rossi, Amore, Calcagno, Siracusano, Niolu, Dell’Osso, Carpita, LIFESTYLE Working Group and Fiorillo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gaia Sampogna, Z2FpYS5zYW1wb2duYUBnbWFpbC5jb20=
 Gaia Sampogna
Gaia Sampogna Mario Luciano
Mario Luciano Matteo Di Vincenzo
Matteo Di Vincenzo Claudia Toni1
Claudia Toni1 Enrico D’Ambrosio
Enrico D’Ambrosio Antonio Rampino
Antonio Rampino Alessandro Rossi
Alessandro Rossi Rodolfo Rossi
Rodolfo Rossi Mario Amore
Mario Amore Alberto Siracusano
Alberto Siracusano Barbara Carpita
Barbara Carpita Andrea Fiorillo
Andrea Fiorillo