
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 16 June 2023
Sec. Ethnopharmacology
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1201240
Background: Few studies have investigated traditional Chinese medicine (TCM) utilization patterns for irritable bowel syndrome (IBS), despite the potential benefits of exploring TCM utilization patterns in optimizing TCM management. This study aimed to evaluate TCM utilization patterns and clinical features for IBS patterns in Taiwan.
Methods: This was a population-based cross-sectional study using claim data from the National Health Insurance Research Database between 2012 and 2018. Patients newly diagnosed with IBS and aged over 20 years were included. The TCM utilization patterns and characteristics, including Chinese herbal medicine (CHM) treatment types and prescription patterns, were evaluated.
Results: A total of 73,306 patients newly diagnosed with IBS used TCM for IBS at least once. Females used TCM for IBS more than males (female-to-male ratio = 1.89: 1). The age distribution showed a peak at 30–39 years (27.29%), followed by 40–49 years (20.74%) and 20–29 years (20.71%). Patients who received Western medications for IBS had a lower tendency to seek TCM. CHM was the most commonly used TCM modality (98.22%), with Jia-wei-xiao-yao-san being the most commonly prescribed Chinese herbal formula and Bai-zhu being the most frequently prescribed single Chinese herb.
Conclusion: This study enhances our understanding of TCM usage patterns for IBS, particularly CHM prescriptions. Further research is needed to investigate commonly used TCM formulas and individual herbs.
Irritable bowel syndrome (IBS) is a prevalent chronic gastrointestinal (GI) disorder affecting around 11.2% of the global population (Lovell and Ford, 2012). In Taiwan, the average annual incidence and prevalence showed a decreasing trend from 2012 to 2018, the use of International Classification of Diseases (ICD) codes rather than rigorous research criteria to identify IBS diagnoses may have led to upcoding or misdiagnosis, which could have affected the reported incidence and prevalence of IBS (Lai et al., 2021). Despite the high prevalence of IBS, its pathophysiology remains incompletely understood (Soares, 2014). The IBS symptoms include chronic or recurring abdominal pain and changes in bowel habits without any structural or biochemical abnormalities or the presence of any organic cause (Masuy et al., 2020). IBS management aims to alleviate symptoms and improve the quality of life, since the condition can negatively impact mental and physical wellbeing (Black and Ford, 2020). Treatment typically involves a combination of psychological support, lifestyle and dietary modifications, physical activity, and pharmaceutical interventions. Non-pharmaceutical treatments are recommended as the first-line approach and can be tailored to the individual’s predominant symptoms such as stress management and dietary modifications for bowel symptoms (Smith, 2006). Pharmaceutical treatment is considered for patients who do not respond to non-pharmaceutical therapies. Beneficial to non-GI symptoms and comorbidities, which can improve health-related quality of life and symptom severity (Gwee et al., 2019; Moayyedi et al., 2019; Masuy et al., 2020; Fukudo et al., 2021; Lacy et al., 2021). Many patients with IBS are unsatisfied with conventional treatment and seek complementary and alternative medicine (CAM) (Li and Li, 2015; Ford et al., 2017), such as traditional Chinese medicine (TCM), which is commonly used in East Asia for IBS treatment (Wu et al., 2021). High-quality studies suggest that TCM formulas, including Tong-xie-yao-fang granule and Shen-ling-bai-zhu-san, effectively manage IBS global symptoms (M Chen et al., 2018; M. Chen et al., 2018; Wang et al., 2020; Xiao et al., 2015), but their use lacks consensus and mainly depends on experiences of TCM practitioners. Thus, this cross-sectional study aimed to investigate TCM utilization patterns and clinical characteristics among patients newly diagnosed with IBS to address the knowledge gap regarding TCM use in IBS treatment in Taiwan.
This was a population-based study using data from the National Health Insurance Research Database (NHIRD) in Taiwan from 2011 to 2018. The National Health Insurance (NHI) program offers universal health insurance to nearly all of the local population, and the NHIRD holds complete and excellent data on demographics, clinical visits, hospitalizations, and prescriptions. The diagnoses are based on the International Classification of Diseases, Ninth and 10th Editions and Clinical Modification (ICD-9-CM and ICD-10-CM) codes. The prescriptions, including Chinese herbal medicine (CHM), contain generic names, brand names, and dosages. This study was approved by the Institutional Review Board (IRB) of Kaohsiung Medical University Chung-Ho Memorial Hospital [KMUHIRB-E(II)-20190359]. Individual identification numbers were encrypted with unique and anonymous identifiers to protect privacy; thus, the requirement for consent was waived by the IRB.
Patients aged 20 years or above with at least one outpatient visit or hospitalization for IBS (ICD-9-CM code: 564.1 and ICD-10-CM code: K58.0 and K58.9) from 2012 to 2017 were enrolled. Exclusion criteria included patients with missing age and gender information and those with a prior IBS diagnosis before 2012 to ensure that all patients were newly diagnosed with IBS. Patients were then categorized as either TCM or non-TCM users. TCM users were defined as those who received an IBS diagnosis after their initial diagnosis and sought for treatment at TCM clinics.
Data, including demographics, comorbidities, and comedications, were collected to analyze the independent variables that influence the use of TCM for IBS. Patients were divided into six age groups for both genders (20–29, 30–39, 40–49, 50–59, 60–69, and ≥70). Urbanization levels in Taiwan were classified into seven tiers, with 1 being the most urbanized and 7 being the least. Residential areas were categorized as levels 1 and 2 (urban areas), levels 3 and 4 (suburban areas), and levels 5 and above (rural areas). Insurance premiums in New Taiwan Dollars (NT$) are determined based on the monthly income of the insured individual and can be used as an indicator of their economic status. The premiums are categorized into three groups: <NT$18,780, NT$18,780–NT$29,000, and >NT$29,000 in this study. This study investigated the comorbidities and prescribed comedication in IBS patients to better understand their disease status. Comorbidities were defined as having at least two ambulatory or outpatient diagnoses or one inpatient diagnosis before IBS diagnosis and identified using the ICD-9-CM and ICD-10-CM codes (Supplementary Table S1). Comedications were defined as the use of medications of interest for a minimum of 14 days before IBS diagnosis and identified using Anatomical Therapeutic Chemical codes, which included laxatives, antidiarrheals, antispasmodics, antidepressants, and probiotics (Supplementary Table S2). The NHIRD provides detailed information on TCM utilization, including TCM diagnoses, CHM prescription, and related claim data. A list of reimbursed CHM was obtained from the Taiwan National Health Insurance Administration website, including NHI codes and names of Chinese herbs and formulas, to identify CHM use in the NHIRD. Treatment codes were extracted from TCM clinical records of patients with IBS to assess the TCM treatment types used, including CHM and acupuncture. CHM prescription patterns were analyzed to identify the most frequently prescribed CHM for patients with IBS, the number of prescriptions, the average duration of prescriptions (in days), the average dose (in grams), and the average daily dose (in grams) was estimated. Average daily dose (g) = Average dose (g)/Average duration for prescriptions (days).
Continuous variables were presented as means ± standard deviation, and categorical variables were presented as numbers (percentages). A multivariate logistic regression analysis was performed to examine the clinical characteristics associated with the utilization of TCM. Case was defended as TCM group and control was non-TCM group. Odd ratio (OR) was over 1 means IBS patients prefer to TCM treatment. Statistical significance was defined as a two-sided p-value < 0.05. The statistical analysis was conducted by SAS version 9.4 software program (SAS Institute, Inc., Cary, North. Carolina).
Out of the 1,193,490 patients newly diagnosed with IBS in NHIRD between 2012 and 2017, 73,306 patients (6.14%) used TCM with routine western-medicine care (TCM users) for IBS at least once during their follow-up year (Figure 1). 1,120,184 patients were non-TCM users. The female proportion was higher in both TCM and non-TCM users. Females had a significantly higher ratio of TCM use than males, with a female-to-male ratio of 1.89: 1. Additionally, the mean age of TCM users (42.94 years) was lower than that of non-TCM users (50.40 years). The age distribution of TCM users peaked in the 30–39 age group (27.29%), followed by the 40–49 (20.74%) and 20–29 age groups (20.71%), whereas the age distribution of non-TCM users peaked in the 50–59 age group (19.66%), followed by the 40–49 (17.90%) and 30–39 age groups (17.65%). Patients residing in urban areas or with an income >NT$29,000 were more likely to seek TCM consultation (Table 1).
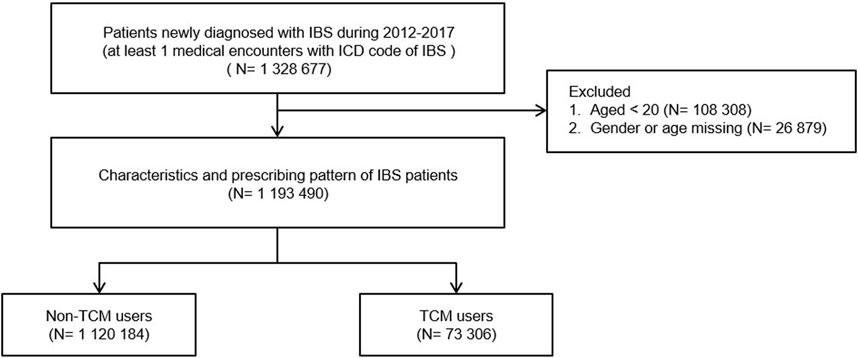
FIGURE 1. Flowchart of study population. NHIRD, National Health Insurance Research Database; ICD code, The International Classification of Diseases, Version 9/10, Clinical Modification (ICD-9-CM code: 564.1 and ICD-10-CM code: K58.0 and K58.9); IBS, Irritable bowel syndrome.
The comorbidities and comedication of patients with IBS receiving TCM care are shown in Table 2. The top three common GI comorbidities were gastritis and duodenitis (16.37%), peptic ulcer (15.05%), and abdominal pain (12.55%) in non-TCM users and constipation (12.17%), gastritis and duodenitis (11.68%), and peptic ulcer (10.53%) in TCM users. The three most common non-GI comorbidities were hypertension (24.84%), dyslipidemia (16.06%), and diabetes (11.8%) in non-TCM users and allergic rhinitis (12.41%), hypertension (11.74%), and dyslipidemia (9.46%) in TCM users. However, the top three psychiatric comorbidities were sleep disorder (13.68% versus 17.13%), anxiety (9.47% versus 8.17%), and depression (4.66% versus 3.41%) in both non-TCM and TCM users. Comedication patterns were similar between non-TCM and TCM users, with antacids (28.78% versus 15.29%), propulsives (24.78% versus 15%), and anxiolytics (21.19% versus 11.90%) being the top three medications.
The multiple regression analysis in Table 3 demonstrated that female (OR = 1.66; 95% confidence interval (CI), 1.63–1.69, p < 0.001) have a higher likelihood of utilizing TCM for IBS treatment compared to males. Otherwise, there were significantly increasing trend for visiting TCM treatments, including urban residents (OR = 1.82), insurance premiums above NT$ 29000 (OR = 1.21), peptic ulcer (OR = 1.06), gastric functional disease (OR = 1.85), intestinal functional disease (OR = 1.37), fibromyalgia (OR = 1.06), chronic obstructive pulmonary disease (OR = 1.25), chronic fatigue syndrome (OR = 1.97), migraine (OR = 1.61), obesity (OR = 1.37), sleep disorder (OR = 1.66). However, there was some factors decreasing visiting TCM treatment, the probability of seeking TCM care for IBS treatment varies among different age groups compared to the reference group (20–29 years), patients in the 30–39 age range showed a non-significant association. However, as age increases exhibited significantly decreasing for visiting TCM treatments for their IBS treatment. Moreover, also a significantly decreasing for visiting TCM treatments, including insurance premiums NT$ 18780–29000 (OR = 0.87), gastritis and duodenitis (OR = 0.84), gastroenteritis and colitis (OR = 0.74), infectious enterocolitis (OR = 0.85), hypertension (OR = 0.76), dyslipidemia (OR = 0.96), diabetes (OR = 0.75), chronic lung disease (OR = 094.), asthma (OR = 0.89), chronic kidney disease (OR = 0.79), depression (OR = 0.84), stress related disorders (OR = 0.81), and all co-medications, except for antidiarrheal drugs.
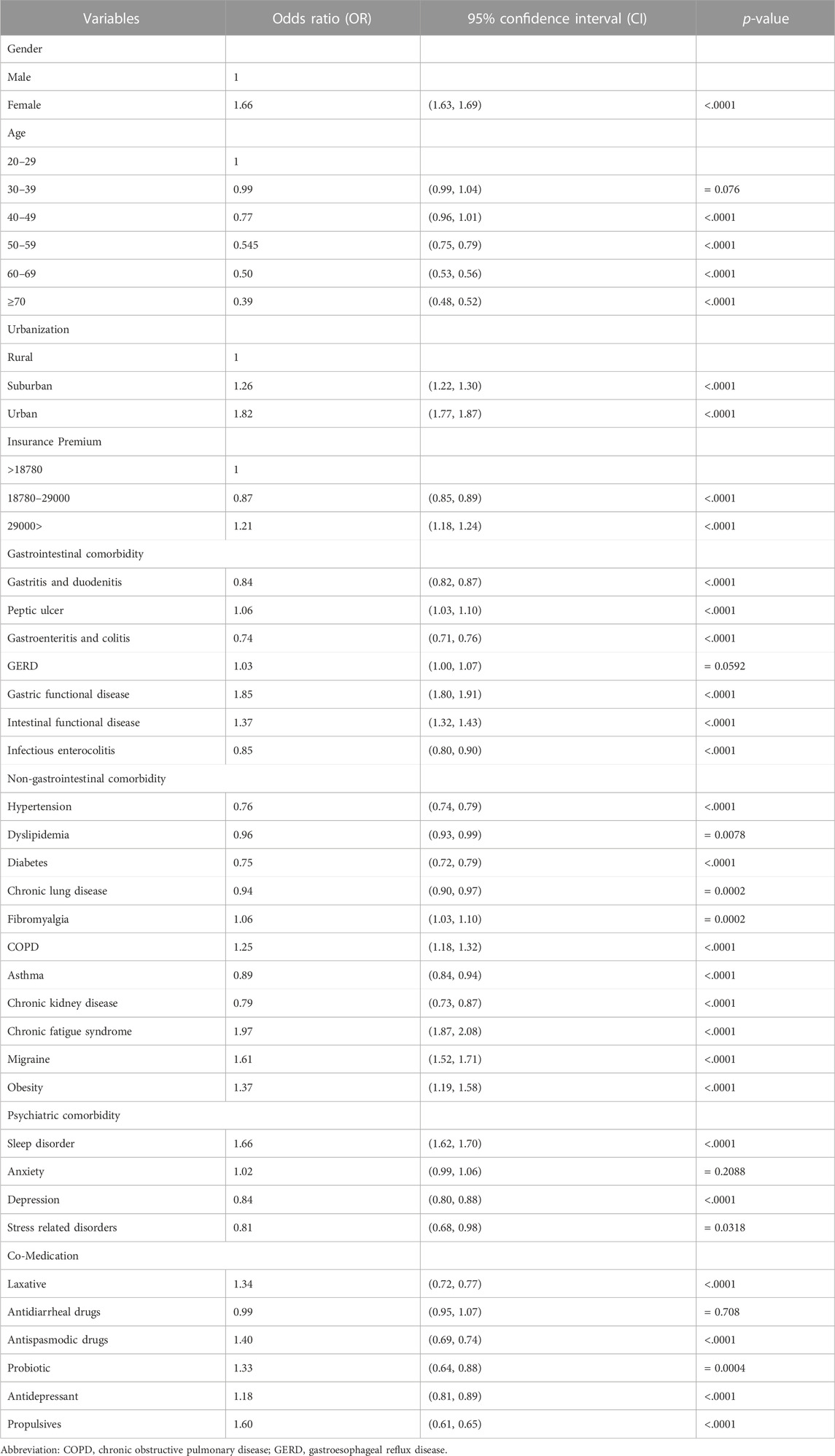
TABLE 3. A multiple regression analysis of factors associated with TCM care in IBS population in Taiwan.
The majority of TCM users (n = 71,999; 98.22%) received CHM, which includes both Chinese single herbs and herbal formulas (Table 4). A smaller proportion of patients (n = 1,082; 1.48%) received a combination of CHM and acupuncture, whereas only 92 (0.13%) patients received acupuncture alone. A total of 133 (0.18%) patients received other TCM treatments, such as moxibustion and traumatology.
The top 10 Chinese single herbs were Bai-zhu (n = 9,123; 12.45%), Hou-pu (6,784; 9.25%), Chen-pi (6,391; 8.72%), Dan-shen (6,379; 8.7%), Yan-hu-suo (6,320; 8.62%), Fu-ling (6,098; 8.32%), Hai-piao-xiao (5,819; 7.94%), Bai-shao (5,468; 7.46%), Xiang-fu (5,280; 7.2%), and Fang-feng (5,267; 7.18%). Bai-zhu was the most frequently prescribed Chinese single herb, and Hai-piao-xiao had the longest average duration of use (90.59 days), highest average dose (114.77 g), and highest average daily dose (1.827 g) (Table 5). Jia-wei-xiao-yao-san (n = 16,755; 22.86%) was the most frequently prescribed Chinese herbal formula. Ban-xia-xie-xin-tang (n = 11,469; 14.1%) and Xiang-sha-liu-jun-zi-tang (n = 9,977; 12.6%) were the second and third most commonly used formulas, respectively (Table 6). Among complex formulas and sigle herbs, Jia-wei-xiao-yao-san (n = 16,755; 22.86%) was the most commonly used herbal medicine, and Ma-zi-ren-wan had the longest average duration of use (90.59 days) and the highest average dose (300.47 g). TCM prefers the uses of complex formuals. However, Shen-ling-bai-zhu-san had the highest average daily dose (4.817 g) (Table 6) in the treatments.
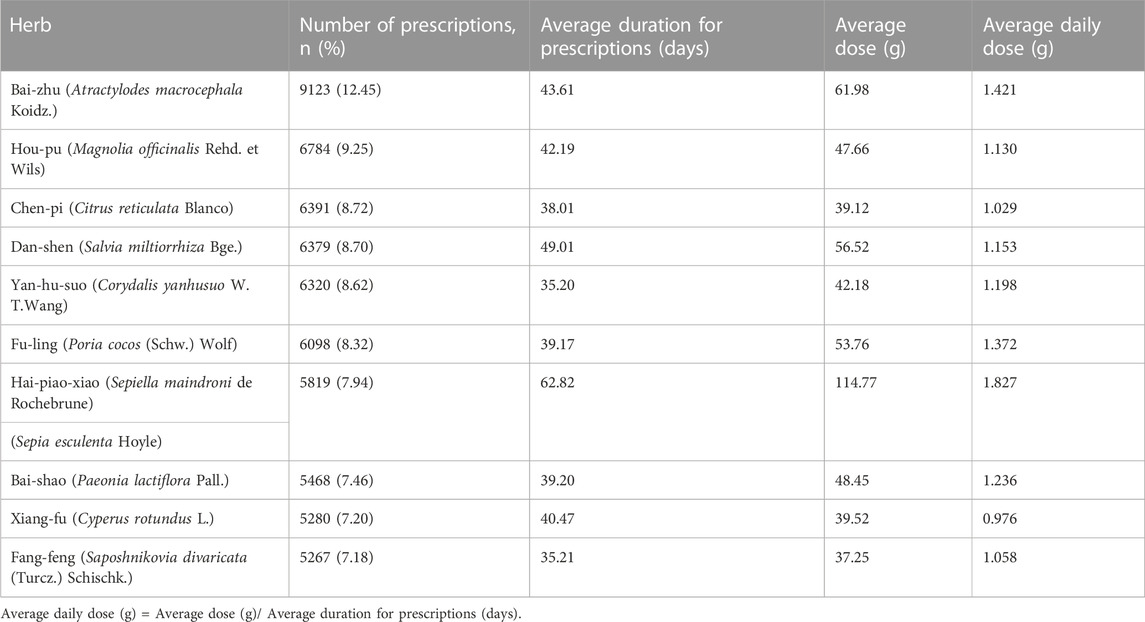
TABLE 5. Top 10 Chinese single herbs prescribed per person within 1 year for IBS in Taiwan (N = 73306).
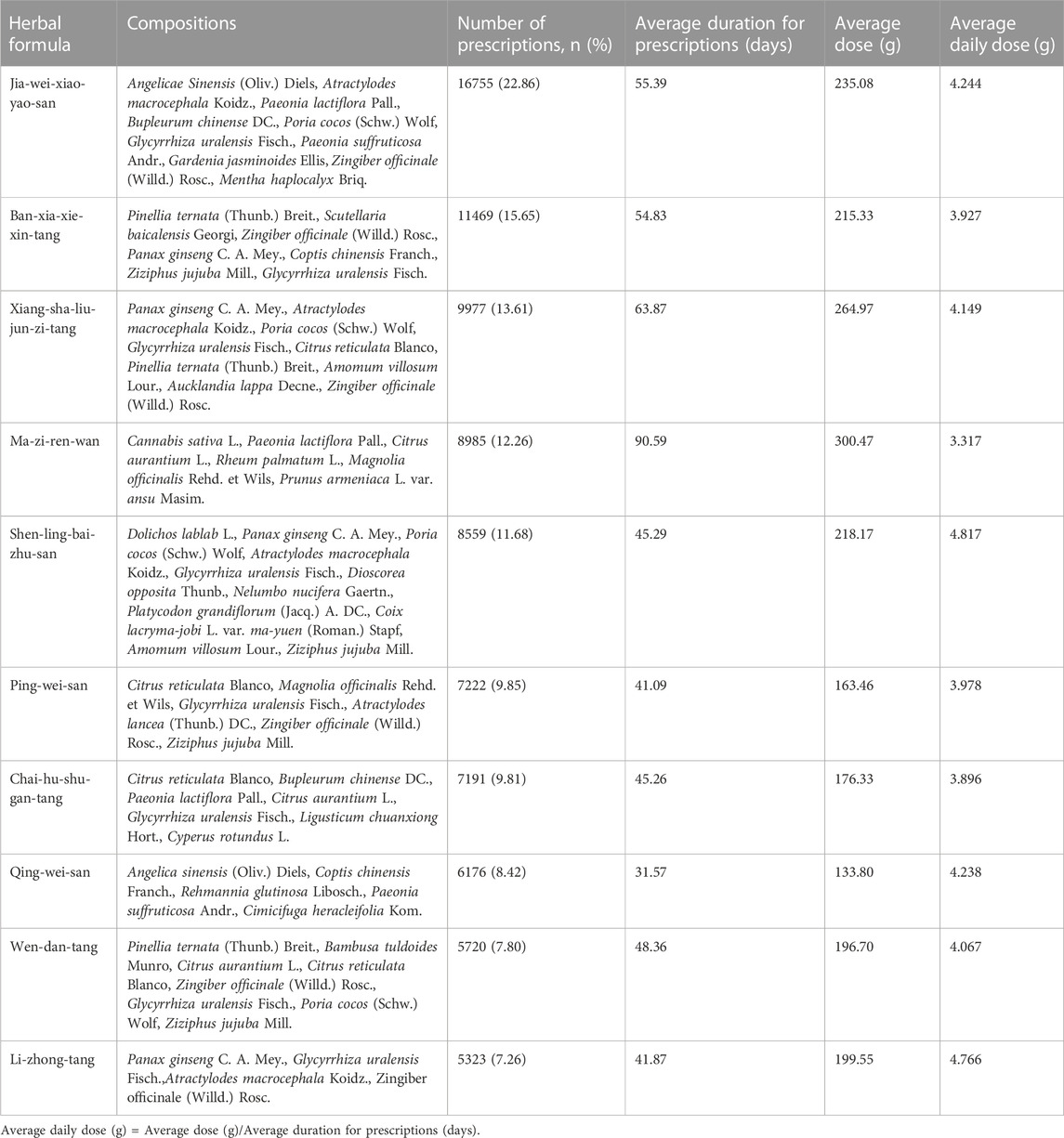
TABLE 6. Top 10 Chinese herbal formulas prescribed per person within 1 year for IBS in Taiwan (N = 73306).
This study conducted the first population-based research demonstrated the TCM prescription patterns and clinical characteristics among patients with IBS in Taiwan. 73,306 patients (6.14%) of TCM treatment with routine western-medicine care (TCM users) and 1,120,184 patients with routine western-medicine (non-TCM users) for IBS were involved. This finding is similar to that reported by Fan et al., who reported that 6.8% of patients used TCM for IBS in China (Fan et al., 2017). In Taiwan, western medicine continues to be the predominant treatment for IBS. However, TCM plays an important role in additional to western medicine, and is covered by national health insurance in Taiwan.
As a previous study in Taiwan, Chinese herbal remedies were found to be the primary choice of TCM with a utilization rate of 85.9% (Chen et al., 2007a). Similarly, CHM was the preferred treatment option for 98.22% of IBS patients. Females with IBS syndromes were more likely to seek for TCM treatment than males. This finding is consistent with previous studies (Chang & Lu, 2009; Chen et al., 2007b; C. C; Shih et al., 2012). However, the reasons behind this phenomenon were not fully explained in the earlier reports. Nevertheless, the results of previous studies proposed that independent or affluent females may have a strong belief in TCM for gynecologic problems and chronic diseases (C.-C. Shih et al., 2012). Age distribution of TCM users peaked in the 30 s. Young age has also been found to be representative of a positive attitude toward CAM in a survey of German hospitals (Huber et al., 2004). This might be because age 30 s people are mainly the breadwinners in their families, and they have more stress and possible disposable money to care for IBS since the NHI does not cover Chinese herbal pieces. Additionally, living in urbanized areas with abundant public facilities, such as easy access to public transportation, and a high density of TCM practitioners was associated with the likelihood of TCM uses (Shih et al., 2010; Yeh et al., 2016). Furthermore, choosing TCM might also be attributed to the higher expectations of patients and the fact that it allows better long-term clinical outcomes and might improve their quality of life (Figueira et al., 2010). TCM was more likely to be chosen by elderly patients for improving health conditions (Pun, 2022). For IBS patients, the morbidity for age 30–60 s are a higher plateau (>200000 patients). However, IBS patients in their 30 s had the highest visit rate to TCM clinics, and visit rates to TCM clinics for patients over 40 years old decreased obviously with age (Table 1). In sleep disorder was found to be the most prevalent, followed by anxiety and depression. Moreover, TCM can be an alternative therapy for improving sleep quality and emotional wellbeing (Aung et al., 2013). TCM practitioners typically evaluate patients’ sleep and emotions during treatment, so patients with mental health conditions are more likely to seek TCM as a healthcare option (Gureje et al., 2015).
Over 10% of IBS patients will have allergy related syndromes, such as allergic rhinitis, asthma, atopic dermatitis, etc. In diagnostic theories of TCM, the “Fei” (lungs) are believed to govern the body’s “Qi” and aid in bowel movement by regulating metabolism and waterways, Additionally, the “Fei” are closely associated with the skin. The “Da-chang” (large intestine) smoothly transport and lower waste. The “Fei” and the “Da-chang” are believed to have a close relationship in terms of their functions and interactions within the body. This connection allows for the exchange of “Qi” and other substances between the two organs, and helps to maintain balance and harmony within the body. When there is an imbalance or dysfunction in either the “Fei” or “Da-chang”, it can affect the function of the other organ as well (Wang and Zhu, 2011). While “Da-chang” is not functioning properly, such as IBS, a higher incidences of allergy related syndromes will also company (Table 2). The core patterns of these allergic syndromes can be characterized by “Fei” and “Qi” deficiencies (Tai et al., 2007; Yang et al., 2012).
Most frequently prescribed single herb for patients with IBS in Taiwan was “Bai-zhu” (Table 5), which has similar results reported as an effective agent for diarrhea-predominant IBS (IBS-D) (Park et al., 2015). Most top 10 single herbs were selected because of “Qi” circulation and reduce bloating and relieve pain caused by abdominal or muscle spasms. Research has verified the effectiveness of Tong-Xie-Yao-Fang in reducing IBS-D symptoms (M Chen et al., 2018). This formula comprises four herbals, Bai-zhu, Chen-pi, Bai-shao, and Fang-feng, which are among the top 10 Chinese single herbs prescribed for patients with IBS in Taiwan. In a previous study, it showed that Hai-piao-xiao was the most commonly prescribed single herb for patients with peptic ulcers in Taiwan (C.-Y. Huang et al., 2015). Its main component is calcium carbonate (Li et al., 2010), which may act as an antacid, helping to relieve discomfort caused by excess gastric acid. It has a significant antacid effect and is most likely to have a gratifying outcome.
The most commonly prescribed herbal formula For IBS was “Jia-wei-xiao-yao-san.” It is also commonly used to treat psychological disorders, including depression and insomnia (F. P. Chen et al., 2011; Chen et al., 2015; Park et al., 2014; Su et al., 2019). Additionally, it has been reported to be effective in regulating abnormal gastric motility and myoelectrical activity in IBS patients with functional dyspepsia (FD) (Qu et al., 2010) and ameliorating depression-like behaviors induced by chronic stress in mice by regulating the gut microbiome and brain metabolome in relation to purine metabolism (Ji et al., 2022). Brain-gut interaction is definitely affected by IBS, and numerous studies that firmly established the existence of microbiota and brain-gut interaction (Lydiard, 2001; Coss-Adame and Rao, 2014; Serafini et al., 2022). Furthermore, several studies showed a correlation among IBS with anxiety, depression, and antidepressant use (Wessely et al., 1999; Posserud et al., 2004; Lee et al., 2015). Furthermore, it may soothe the “Gan” (liver) and regulates “Qi” in TCM theories, which is beneficial for individuals aged 30–39, who are mostly working under high levels of stress. In this study, these comorbidities were common for TCM consultation, which may lead to the higher prescription rate of Jia-wei-xiao-yao-san in patients with IBS.
Ma-zi-ren-wan was reported to be effective in treating constipation and is the most commonly prescribed Chinese herbal formula for patients with this syndrome in Taiwan (Jong et al., 2010; Yang et al., 2021). The average duration of Ma-zi-ren-wan was used for the longest time and the highest dosage in average. Additionally, Ban-xia-xie-xin-tang was the second most commonly prescribed (Zeng et al., 2019). It not only relieves IBS symptoms but also provides greater benefits to FD and peptic ulcer symptoms. Consequently, it has become widely used in Taiwan for treating peptic ulcers (C. Y. Huang et al., 2015). Furthermore, Xiang-sha-liu-jun-zi-tang is frequently used for allergic related syndromes, functional abdominal pain syndrome and yields significant improvements in FD symptoms compared with prokinetic agents (Xiao et al., 2012; Liu et al., 2016). In an animal model, it promoted the expression of anti-inflammatory factors, enhanced immune response, and regulated intestinal flora, and modulated the ERK/p38 MAPK signaling pathway (Ma et al., 2019). Treatments using Shen-ling-bai-zhu-san and Chai-hu-shu-gan-tang showed significantly higher total effective rates than those of western medicine in IBS (Li et al., 2013). Moreover, an antacid effect had been reported for Shen-ling-bai-zhu-san (Wu et al., 2010). However, Ping-wei-san showed beneficial effects in reducing colonic damage in patients with colorectal cancer (Yeh et al., 2020), inhibiting inflammatory cytokine production and pathway activation of the NF-κB pathway and the NLRP3 inflammasome in mice (Zhang et al., 2019). Magnolia officinalis in Ping-wei-san can impede neuroinflammation and oxidative stress in the prefrontal cortex. Additionally, in a rodent model of depression, it could boost brain-derived neurotrophic factor protein levels in the hippocampus (Cheng et al., 2018; Zhang et al., 2020).
Qing-wei-san was used to treat various conditions related to heat in the stomach and blood, such as oral ulcers, periodontitis, and upper GI bleeding. It exerted anti-inflammatory effects by improving the pathological morphologies of gastric and oral mucosa in mice, reducing the levels of proinflammatory cytokines, and inhibiting the TLR4/MyD88/NF-κB signaling pathway (Shi et al., 2022). Wen-dan-tang had the potential to treat neurological and psychiatric disorders and digestive disorders (Pradhan et al., 2022). Most studies focused on insomnia and psychotic symptoms (Wu et al., 1999; Che et al., 2016; Deng and Xu, 2017; Yan et al., 2017). In Taiwan, Wen-dan-tang is commonly used for insomnia (F.-P. Chen et al., 2011). An animal study decrease insomnia-related anxiety (Wang et al., 2014). Furthermore, the inhibitory modulation of NF-κB and NLRP3 inflammasome activation by Wen-dan-tang may mediate its antidepressant effect (Jia et al., 2018). Overall, gastroesophageal reflux disease was reported to be associated with IBS (Ruigómez et al., 2009; Yarandi et al., 2010; de Bortoli et al., 2018). Wen-dan-tang consistently demonstrated significant improvement in symptom relief, and this efficacy was sustained over time in gastroesophageal reflux disease (Ling et al., 2015).
Li-zhong-tang enhanced antioxidative defense and improved mucosal immunity through the TLR-2/MyD88 signaling pathway (Song et al., 2020), it significantly restored intestinal microflora in Spleen-“Qi” deficient rats (Peng et al., 2008).
In this real-world survey, Chinese single herbs and complex formulas were suggested and may improve IBS. They are commonly prescribed to patients because they effectively alleviate comorbidities associated with IBS related disorders in physical and psychological aspects.
This study has some limitations. First, NHI covers Chinese herbal remedies that come in scientific granular or powder forms (extraction and preparation forms with drug certificates). Thus, the traditional form of Chinese herbal remedies (crude drugs and their complex formulas) is not covered by reimbursement and hence was excluded from this study. Second, self-pay patients were excluded from this study. Thus, the uses of TCM may be underestimated in this study. Third, as the NHIRD did not include data on the severity of IBS and specific subtypes, TCM utilization might reflect IBS clinical symptoms to a certain extent.
This ethnopharmacological study reveals the prescription patterns of TCM for treating patients with IBS. The study benefits from the involvement of licensed physicians responsible for diagnosis and TCM prescriptions, increasing its credibility. Further research is needed to explore commonly used TCM formulas and single herbs. TCM can be considered for treating patients with IBS or GI disorders, as well as addressing their psychological conditions. However, clinical trials are required to support these findings.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Institutional Review Board of Kaohsiung Medical University Chung-Ho Memorial Hospital [KMUHIRB-E(II)-20190359]. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The research was also supported by grants from the National Science and Technology Council of Taiwan (NSTC 111-2320-B-037-022) awarded to C-YC. The research was also supported by grants from the National Science and Technology Council of Taiwan (NSTC 111-2321-B-037-004, and 111-2320-B-037-020-MY3) awarded to F-RC. In addition, this research was partially supported by the Drug Development and Value Creation Research Center, Kaohsiung Medical University and Department of Medical Research, Kaohsiung Medical University Hospital.
This study was based in part on data from the NHIRD provided by the Bureau of National Health Insurance (BNHI) of the Ministry of Health and Welfare. The conclusion presented in this study are those of the authors and do not necessarily reflect the views of the BNHI, the Ministry of Health and Welfare. We thank the Center for Medical Informatics and Statistics of Kaohsiung Medical University for providing administrative and funding support. We would specially thank the Center for Research Resources and Development in Kaohsiung Medical University for the assistance.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1201240/full#supplementary-material
Aung, S. K., Fay, H., and Hobbs, R. F. (2013). Traditional Chinese medicine as a basis for treating psychiatric disorders: A review of theory with illustrative cases. Med. Acupunct. 25 (6), 398–406. doi:10.1089/acu.2013.1007
Black, C. J., and Ford, A. C. (2020). Global burden of irritable bowel syndrome: Trends, predictions and risk factors. Nat. Rev. Gastroenterol. Hepatol. 17, 473–486. doi:10.1038/s41575-020-0286-8
Chang, F. Y., and Lu, C. L. (2009). Treatment of irritable bowel syndrome using complementary and alternative medicine. J. Chin. Med. Assoc. 72 (6), 294–300. doi:10.1016/s1726-4901(09)70375-2
Che, Y.-w., Yao, K.-y., Xi, Y.-p., Chen, Z.-j., Li, Y.-l., Yu, N., et al. (2016). Wendan decoction (温胆汤) for treatment of schizophrenia: A systematic review of randomized controlled trials. Chin. J. Integr. Med. 22, 302–310. doi:10.1007/s11655-015-2047-z
Chen, F.-P., Chen, T.-J., Kung, Y.-Y., Chen, Y.-C., Chou, L.-F., Chen, F.-J., et al. (2007a). Use frequency of traditional Chinese medicine in Taiwan. BMC health Serv. Res. 7 (1), 26–11. doi:10.1186/1472-6963-7-26
Chen, F.-P., Chen, T.-J., Kung, Y.-Y., Chen, Y.-C., Chou, L.-F., Chen, F.-J., et al. (2007b). Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv. Res. 7 (1), 26. doi:10.1186/1472-6963-7-26
Chen, F.-P., Jong, M.-S., Chen, Y.-C., Kung, Y.-Y., Chen, T.-J., Chen, F.-J., et al. (2011). Prescriptions of Chinese herbal medicines for insomnia in Taiwan during 2002. Evidence-Based Complementary Altern. Med. 2011, 236341. doi:10.1093/ecam/nep018
Chen, M., Tang, T. C., Wang, Y., Shui, J., Xiao, X. H., Lan, X., et al. (2018). Randomised clinical trial: Tong-Xie-Yao-Fang granules versus placebo for patients with diarrhoea-predominant irritable bowel syndrome. Alimentary Pharmacol. Ther. 48 (2), 160–168. doi:10.1111/apt.14817
Chen, Y.-L., Lee, C.-Y., Huang, K.-H., Kuan, Y.-H., and Chen, M. (2015). Prescription patterns of Chinese herbal products for patients with sleep disorder and major depressive disorder in Taiwan. J. Ethnopharmacol. 171, 307–316. doi:10.1016/j.jep.2015.05.045
Cheng, J., Dong, S., Yi, L., Geng, D., and Liu, Q. (2018). Magnolol abrogates chronic mild stress-induced depressive-like behaviors by inhibiting neuroinflammation and oxidative stress in the prefrontal cortex of mice. Int. Immunopharmacol. 59, 61–67. doi:10.1016/j.intimp.2018.03.031
Coss-Adame, E., and Rao, S. S. (2014). Brain and gut interactions in irritable bowel syndrome: New paradigms and new understandings. Curr. Gastroenterol. Rep. 16, 379. doi:10.1007/s11894-014-0379-z
de Bortoli, N., Tolone, S., Frazzoni, M., Martinucci, I., Sgherri, G., Albano, E., et al. (2018). Gastroesophageal reflux disease, functional dyspepsia and irritable bowel syndrome: Common overlapping gastrointestinal disorders. Ann. gastroenterology 31 (6), 639–648. doi:10.20524/aog.2018.0314
Deng, H., and Xu, J. (2017). Wendan decoction (Traditional Chinese medicine) for schizophrenia. Cochrane Database Syst. Rev. 6 (6), CD012217. doi:10.1002/14651858.CD012217.pub2
Fan, W. J., Xu, D., Chang, M., Zhu, L. M., Fei, G. J., Li, X. Q., et al. (2017). Predictors of healthcare-seeking behavior among Chinese patients with irritable bowel syndrome. World J. Gastroenterol. 23 (42), 7635–7643. doi:10.3748/wjg.v23.i42.7635
Figueira, H. A., Figueira, O. A., Figueira, A. A., Figueira, J. A., Giani, T. S., and Dantas, E. H. (2010). Elderly quality of life impacted by traditional Chinese medicine techniques. Clin. interventions aging 5, 301–305. doi:10.2147/CIA.S10615
Ford, A. C., Lacy, B. E., and Talley, N. J. (2017). Irritable bowel syndrome. N. Engl. J. Med. 376 (26), 2566–2578. doi:10.1056/NEJMra1607547
Fukudo, S., Okumura, T., Inamori, M., Okuyama, Y., Kanazawa, M., Kamiya, T., et al. (2021). Evidence-based clinical practice guidelines for irritable bowel syndrome 2020. J. Gastroenterol. 56 (3), 193–217. doi:10.1007/s00535-020-01746-z
Gureje, O., Nortje, G., Makanjuola, V., Oladeji, B. D., Seedat, S., and Jenkins, R. (2015). The role of global traditional and complementary systems of medicine in the treatment of mental health disorders. Lancet Psychiatry 2 (2), 168–177. doi:10.1016/S2215-0366(15)00013-9
Gwee, K. A., Gonlachanvit, S., Ghoshal, U. C., Chua, A. S. B., Miwa, H., Wu, J., et al. (2019). Second asian consensus on irritable bowel syndrome. J. Neurogastroenterol. Motil. 25 (3), 343–362. doi:10.5056/jnm19041
Huang, C.-Y., Lai, W.-Y., Sun, M.-F., Lin, C.-C., Chen, B.-C., Lin, H.-J., et al. (2015). Prescription patterns of traditional Chinese medicine for peptic ulcer disease in taiwan: A nationwide population-based study. J. Ethnopharmacol. 176, 311–320. doi:10.1016/j.jep.2015.11.002
Huber, R., Koch, D., Beiser, I., Zschocke, I., and Luedtke, R. (2004). Experience and attitudes towards CAM-a survey of internal and psychosomatic patients in a German University hospital. Altern. Ther. Health & Med. 10 (1), 32–36.
Ji, S., Han, S., Yu, L., Du, L., You, Y., Chen, J., et al. (2022). Jia Wei Xiao Yao San ameliorates chronic stress-induced depression-like behaviors in mice by regulating the gut microbiome and brain metabolome in relation to purine metabolism. Phytomedicine 98, 153940. doi:10.1016/j.phymed.2022.153940
Jia, K.-K., Ding, H., Yu, H.-W., Dong, T.-J., Pan, Y., and Kong, L.-D. (2018). Huanglian-wendan decoction inhibits NF-κb/NLRP3 inflammasome activation in liver and brain of rats exposed to chronic unpredictable mild stress. Mediat. Inflamm. 2018, 3093516, doi:10.1155/2018/3093516
Jong, M. S., Hwang, S. J., Chen, Y. C., Chen, T. J., Chen, F. J., and Chen, F. P. (2010). Prescriptions of Chinese herbal medicine for constipation under the national health insurance in Taiwan. J. Chin. Med. Assoc. 73 (7), 375–383. doi:10.1016/s1726-4901(10)70081-2
Lacy, B. E., Pimentel, M., Brenner, D. M., Chey, W. D., Keefer, L. A., Long, M. D., et al. (2021). ACG clinical guideline: Management of irritable bowel syndrome. Am. J. Gastroenterol. 116 (1), 17–44. doi:10.14309/ajg.0000000000001036
Lai, Y.-T., Chen, C.-Y., and Bair, M.-J. (2021). Epidemiology, clinical features, and prescribing patterns of irritable bowel syndrome in Taiwan. Front. Pharmacol. 12, 788795. doi:10.3389/fphar.2021.788795
Lee, Y.-T., Hu, L.-Y., Shen, C.-C., Huang, M.-W., Tsai, S.-J., Yang, A. C., et al. (2015). Risk of psychiatric disorders following irritable bowel syndrome: A nationwide population-based cohort study. Plos one 10 (7), e0133283. doi:10.1371/journal.pone.0133283
Li, C.-Y., and Li, S.-C. (2015). Treatment of irritable bowel syndrome in China: A review. World J. Gastroenterol. 21 (8), 2315–2322. doi:10.3748/wjg.v21.i8.2315
Li, Q., Yang, G.-Y., and Liu, J.-P. (2013). Syndrome differentiation in Chinese herbal medicine for irritable bowel syndrome: A literature review of randomized trials. Evidence-Based Complementary Altern. Med., 2013, 232147, doi:10.1155/2013/232147
Li, Y.-Z., Pan, H., Xu, J., Fan, X.-W., Song, X.-C., Zhang, Q., et al. (2010). Characterization of metal removal by os sepiae of Sepiella maindroni Rochebrune from aqueous solutions. J. Hazard. Mater. 179 (1-3), 266–275. doi:10.1016/j.jhazmat.2010.03.001
Ling, W., Huang, Y., Xu, J.-H., Li, Y., Huang, Y.-M., Ling, H.-B., et al. (2015). Consistent efficacy of Wendan decoction for the treatment of digestive reflux disorders. Am. J. Chin. Med. 43 (05), 893–913. doi:10.1142/S0192415X15500524
Liu, T., Wang, N., Zhang, L., and Zhong, L. (2016). Chinese herbal medicine for functional abdominal pain syndrome: From clinical findings to basic understandings. Evid. Based Complement. Altern. Med., 2016, 8652523. doi:10.1155/2016/8652523
Lovell, R. M., and Ford, A. C. (2012). Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin. gastroenterology hepatology 10 (7), 712–721. doi:10.1016/j.cgh.2012.02.029
Lydiard, R. B. (2001). Irritable bowel syndrome, anxiety, and depression: What are the links? J. Clin. Psychiatry 62, 38–45.
Ma, Q., Ouyang, Y., Meng, F., Noolvi, M. N., Avvaru, S. P., More, U. A., et al. (2019). A review of pharmacological and clinical studies on the application of Shenling Baizhu San in treatment of Ulcerative colitis. J. Ethnopharmacol. 244, 112105. doi:10.1016/j.jep.2019.112105
Masuy, I., Pannemans, J., and Tack, J. (2020). Irritable bowel syndrome: Diagnosis and management. Minerva Gastroenterol. Dietol. 66 (2), 136–150. doi:10.23736/s1121-421x.19.02640-0
Moayyedi, P., Andrews, C. N., MacQueen, G., Korownyk, C., Marsiglio, M., Graff, L., et al. (2019). Canadian association of gastroenterology clinical practice guideline for the management of irritable bowel syndrome (IBS). J. Can. Assoc. Gastroenterol. 2 (1), 6–29. doi:10.1093/jcag/gwy071
Park, D.-M., Kim, S.-H., Park, Y.-C., Kang, W.-C., Lee, S.-R., and Jung, I.-C. (2014). The comparative clinical study of efficacy of gamisoyo-san (jiaweixiaoyaosan) on generalized anxiety disorder according to differently manufactured preparations: Multicenter, randomized, double blind, placebo controlled trial. J. Ethnopharmacol. 158, 11–17. doi:10.1016/j.jep.2014.10.024
Park, J. J., Chon, N. R., Lee, Y. J., and Park, H. (2015). The effects of an extract of Atractylodes Japonica rhizome, SKI3246 on gastrointestinal motility in Guinea pigs. J. Neurogastroenterol. Motil. 21 (3), 352–360. doi:10.5056/jnm14112
Peng, Y., Jin, J., Wu, C.-F., Yang, J.-Y., and Li, X.-B. (2008). Regulation of three Jianpi Buqi recipes on intestinal microflora of Piqi-deficiency rat. Zhongguo Zhong yao za zhi= Zhongguo zhongyao zazhi= China J. Chin. materia medica 33 (21), 2530–2534.
Posserud, I., Agerforz, P., Ekman, R., Björnsson, E., Abrahamsson, H., and Simrén, M. (2004). Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. Gut 53 (8), 1102–1108. doi:10.1136/gut.2003.017962
Pradhan, S. K., Li, Y., Gantenbein, A. R., Angst, F., Lehmann, S., and Shaban, H. (2022). Wen dan tang: A potential jing fang decoction for headache disorders? Medicines 9 (3), 22. doi:10.3390/medicines9030022
Pun, J., Yu, Q. J., and Lee, M. K. C. (2022). The active participation of elderly patients in traditional Chinese medicine consultations as means to creating a community of practice: A case study in Hong Kong. Front. Psychol. 13, 943840. doi:10.3389/fpsyg.2022.943840
Qu, Y., Gan, H. Q., Mei, Q. B., and Liu, L. (2010). Study on the effect of jia-wei-xiao-yao-san decoction on patients with functional dyspepsia. Phytotherapy Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 24 (2), 245–248. doi:10.1002/ptr.2920
Ruigómez, A., Wallander, M.-A., Johansson, S., and Rodríguez, L. A. G. (2009). Irritable bowel syndrome and gastroesophageal reflux disease in primary care: Is there a link? Dig. Dis. Sci. 54, 1079–1086. doi:10.1007/s10620-008-0462-0
Serafini, N., Jarade, A., Surace, L., Goncalves, P., Sismeiro, O., Varet, H., et al. (2022). Trained ILC3 responses promote intestinal defense. Science 375 (6583), 859–863. doi:10.1126/science.aaz8777
Shi, L., An, Y., Cheng, L., Li, Y., Li, H., Wang, C., et al. (2022). Qingwei San treats oral ulcer subjected to stomach heat syndrome in db/db mice by targeting TLR4/MyD88/NF-κB pathway. Chin. Med. 17, 1–16. doi:10.1186/s13020-021-00565-5
Shih, C.-C., Liao, C.-C., Su, Y.-C., Tsai, C.-C., and Lin, J.-G. (2012). Gender differences in traditional Chinese medicine use among adults in Taiwan. Plos one 7 (4), e32540. doi:10.1371/journal.pone.0032540
Shih, C.-C., Su, Y.-C., Liao, C.-C., and Lin, J.-G. (2010). Patterns of medical pluralism among adults: Results from the 2001 national health interview survey in taiwan. BMC health Serv. Res. 10, 191–199. doi:10.1186/1472-6963-10-191
Smith, G. D. (2006). Irritable bowel syndrome: Quality of life and nursing interventions. Br. J. Nurs. 15 (21), 1152–1156. doi:10.12968/bjon.2006.15.21.22371
Soares, R. L. (2014). Irritable bowel syndrome: A clinical review. World J. Gastroenterology WJG 20 (34), 12144–12160. doi:10.3748/wjg.v20.i34.12144
Song, H., Hou, X., Zeng, M., Chen, X., Chen, X., Yang, T., et al. (2020). Traditional Chinese Medicine Li-Zhong-Tang accelerates the healing of indomethacin-induced gastric ulcers in rats by affecting TLR-2/MyD88 signaling pathway. J. Ethnopharmacol. 259, 112979. doi:10.1016/j.jep.2020.112979
Su, R., Fan, J., Li, T., Cao, X., Zhou, J., Han, Z., et al. (2019). Jiawei xiaoyao capsule treatment for mild to moderate major depression with anxiety symptoms: A randomized, double-blind, double-dummy, controlled, multicenter, parallel-treatment trial. J. Tradit. Chin. Med. 39 (3), 410–417.
Tai, C.-J., Chang, C.-P., Huang, C.-Y., and Chien, L.-Y. (2007). Efficacy of sanfujiu to treat allergies: Patient outcomes at 1 year after treatment. Evidence-Based Complementary Altern. Med. 4 (2), 241–246. doi:10.1093/ecam/nel082
Wang, H., and Zhu, B. (2011). Basic theories of traditional Chinese medicine. London, United Kingdom: Singing Dragon.
Wang, L., Song, Y., Li, F., Liu, Y., Ma, J., Mao, M., et al. (2014). Effects of Wen Dan Tang on insomnia-related anxiety and levels of the brain-gut peptide Ghrelin. Neural Regen. Res. 9 (2), 205–212. doi:10.4103/1673-5374.125351
Wang, Y., Zhang, S., Zhou, Q., Meng, M., and Chen, W. (2020). Efficacy of shenlingbaizhu formula on irritable bowel syndrome: A systematic review. J. Tradit. Chin. Med. 40 (6), 897–907. doi:10.19852/j.cnki.jtcm.2020.06.001
Wessely, S., Nimnuan, C., and Sharpe, M. (1999). Functional somatic syndromes: One or many? Lancet 354 (9182), 936–939. doi:10.1016/S0140-6736(98)08320-2
Wu, J., An, H., Li, Y., and Duan, L. (1999). TCM treatment with the modified wendan tang in 40 cases of melancholia. J. Traditional Chin. Medicine= Chung i tsa Chih Ying wen pan 19 (4), 296–297.
Wu, T.-H., Chen, I.-C., and Chen, L.-C. (2010). Antacid effects of Chinese herbal prescriptions assessed by a modified artificial stomach model. World J. Gastroenterology WJG 16 (35), 4455–4459. doi:10.3748/wjg.v16.i35.4455
Wu, Y.-b., Dai, Y.-k., Zhang, L., Pan, H.-g., Chen, W.-j., Li, R.-l., et al. (2021). Pharmacological treatments of Chinese herbal medicine for irritable bowel syndrome in adults: A network meta-analysis of randomized controlled trials. Plos one 16 (8), e0255665. doi:10.1371/journal.pone.0255665
Xiao, H. T., Zhong, L., Tsang, S. W., Lin, Z. S., and Bian, Z. X. (2015). Traditional Chinese medicine formulas for irritable bowel syndrome: From ancient wisdoms to scientific understandings. Am. J. Chin. Med. 43 (1), 1–23. doi:10.1142/S0192415X15500019
Xiao, Y., Liu, Y.-Y., Yu, K.-Q., Ouyang, M.-Z., Luo, R., and Zhao, X.-S. (2012). Chinese herbal medicine Liu jun zi tang and Xiang sha Liu jun zi tang for functional dyspepsia: meta-analysis of randomized controlled trials. Evid. Based Complement. Altern. Med., 2012, 936459–936459. doi:10.1155/2012/936459
Yan, X., Wang, Y., Li, X., Li, Z., Zhang, Y., Cai, X., et al. (2017). Wendan decoction for primary insomnia: Protocol for a systematic review and meta-analysis. Medicine 96 (47), e8906. doi:10.1097/MD.0000000000008906
Yang, M., Feng, Y., Zhang, Y. L., Smith, C. M., Hou, Y. N., Wang, H., et al. (2021). Herbal formula MaZiRenWan (hemp seed pill) for constipation: A systematic review with meta-analysis. Phytomedicine 82, 153459. doi:10.1016/j.phymed.2021.153459
Yang, S., Chen, H., Lin, Y., and Chen, Y. (2012). The exploration of disease pattern, zheng, for differentiation of allergic rhinitis in traditional Chinese medicine practice. Evidence-Based Complementary Altern. Med., 2012, 521780, doi:10.1155/2012/521780
Yarandi, S. S., Nasseri-Moghaddam, S., Mostajabi, P., and Malekzadeh, R. (2010). Overlapping gastroesophageal reflux disease and irritable bowel syndrome: Increased dysfunctional symptoms. World J. Gastroenterol. 16 (10), 1232–1238. doi:10.3748/wjg.v16.i9.1232
Yeh, M.-H., Chiu, H.-P., Wu, M.-C., Koo, M., Lin, N.-W., Liao, K.-K., et al. (2020). Integrated Chinese herbal medicine and Western medicine on the survival in patients with colorectal cancer: A retrospective study of medical records. Evidence-Based Complementary Altern. Med., 2020, 4561040, doi:10.1155/2020/4561040
Yeh, Y.-H., Chou, Y.-J., Huang, N., Pu, C., and Chou, P. (2016). The trends of utilization in traditional Chinese medicine in taiwan from 2000 to 2010: A population-based study. Medicine 95 (27), e4115. doi:10.1097/MD.0000000000004115
Zeng, G., Huang, Y.-f., Xiao, C.-x., and Xie, R.-s. (2019). Efficacy and safety of banxia xiexin decoction in the treatment of irritable bowel syndrome: A meta - analysis. China Pharm. 28 (13), 69–72. doi:10.3969/j.issn.1006-4931.2019.13.022
Zhang, Z., Cao, H., Shen, P., Liu, J., Cao, Y., and Zhang, N. (2020). Ping weisan alleviates chronic colitis in mice by regulating intestinal microbiota composition. J. Ethnopharmacol. 255, 112715. doi:10.1016/j.jep.2020.112715
Keywords: traditional Chinese medicine, irritable bowel syndrome (IBS), Chinese herbal medicine, utilization patterns, real-world data
Citation: Gu Y, Lai Y-T, Chang F-R and Chen C-Y (2023) Utilization patterns and prescription characteristics of traditional Chinese medicine among patients with irritable bowel syndrome in Taiwan. Front. Pharmacol. 14:1201240. doi: 10.3389/fphar.2023.1201240
Received: 06 April 2023; Accepted: 05 June 2023;
Published: 16 June 2023.
Edited by:
Juei-Tang Cheng, Chang Jung Christian University, TaiwanReviewed by:
Jianye Yuan, Shanghai University of Traditional Chinese Medicine, ChinaCopyright © 2023 Gu, Lai, Chang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang-Rong Chang, YWFyb25mcmNAa211LmVkdS50dw==; Chung-Yu Chen, amsyOTc1NTI1QGhvdG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.