- 1National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, China
- 2Institute of Traditional Chinese Medicine, Tianjin University of Traditional Chinese Medicine, Tianjin, China
Heart failure with preserved ejection fraction accounts for a large proportion of heart failure, and it is closely related to a high hospitalization rate and high mortality rate of cardiovascular disease. Although the methods and means of modern medical treatment of HFpEF are becoming increasingly abundant, they still cannot fully meet the clinical needs of HFpEF patients. Traditional Chinese medicine is an important complementary strategy for the treatment of diseases in modern medicine, and it has been widely used in clinical research on HFpEF in recent years. This article reviews the current situation of HFpEF management, the evolution of guidelines, the clinical evidence and the mechanism of TCM in the treatment of HFpEF. The purpose of this study is to explore the application of TCM for HFpEF, to further improve the clinical symptoms and prognosis of patients and to provide a reference for the diagnosis and treatment of the disease.
1 Introduction
Heart failure (HF) with preserved ejection fraction (HFpEF) refers specifically to left ventricular ejection fraction (LVEF) ≥ 50%. It is a syndrome that accumulates in multiple organs and systems. The main clinical manifestations are exertional dyspnoea and exercise intolerance. According to the latest American Heart Association/American College of Cardiology/Heart Failure Society of America (AHA/ACC/HFSA) guidelines in 2022, heart failure is divided into four categories: heart failure with preserved ejection fraction (HFpEF), heart failure with reduced ejection fraction (HFrEF), heart failure with midrange ejection fraction (HFmrEF) and heart failure with improved ejection fraction (HFimpHF) (Heidenreich et al., 2022). According to the epidemiology in 2019, cardiovascular disease (CVD) accounted for approximately 45% of the causes of death in China, and 2 out of every 5 deaths were from CVD. At present, the number of CVD cases is 330 million, of which heart failure accounts for 8.9 million (Wang, 2021), while HFpEF accounts for between 19% and 55% of HF cases (Teramoto et al., 2022). The risk of death and rehospitalization from HFpEF is similar to that of HFrEF, and its prevalence rate is increasing by 1% per year (Paulus and Tschöpe, 2013). The distribution of HFpEF in the population is more in the United States than in Europe and more in Europe than in Asia. It is more prevalent in women than in men and in the elderly than in the young. With increasing age, the number of comorbidities in patients with HFpEF also increases (Dunlay et al., 2017). Therefore, in hospitalized cases of HFpEF, we cannot only consider cardiovascular problems, which results in the complexity and diversity of doctors’ diagnoses and treatment. The pathogenesis of HFpEF results from impaired cardiac filling and changes in the diastolic function of the left ventricle. In the past, primary myocardial injury was considered to be an important factor triggering HFpEF. Recent studies have shown that myocardial injury in HFpEF is not primary but rather systemic inflammation caused by arterial hypertension or metabolic diseases such as diabetes and obesity. It eventually leads to coronary artery microvascular inflammation, dysfunction, subendocardial ischaemia, myocardial cellular mechanisms and metabolic changes (Heinzel and Shah, 2022).
The 2022 AHA/ACC/HFSA guidelines proposed guideline-directed management and therapy (GDMT) as the cornerstone of drug treatment, and SGLT2i, MRA, and ARNI are included in the recommended drugs according to the guidelines. However, a one-size-fits-all treatment strategy has difficulty solving the real problem. For example, the risk period for HFrEF requires initiating drugs to prevent disease progression, while there is a lack of treatment strategies for the risk period for HFpEF. Given the high mortality and rehospitalization rate of HFpEF (Schrutka et al., 2022), how to use drugs and improve the prognosis of patients has also become the focus of our attention. The current treatments in Western medicine include SGLT-2 inhibitors, which can regulate diabetic comorbid disease and improve the quality of life of patients (Heinzel and Shah, 2022); sacubatril valsartan, which can prevent the deterioration of renal function and reduce the risk of cardiovascular death (Cui et al., 2022); corresponding anti-inflammatory strategies, which can improve systemic microvascular inflammation (Omote et al., 2022); pirfenidone, which can reduce TGF-β and improve myocardial fibrosis (Lewis et al., 2021); and spironolactone, which can regulate cardiac function (Beldhuis et al., 2021). Although its treatment takes into account the comorbidities and prognosis of HFpEF, it also has some limitations. For example, the clinical effect of some drugs is not obvious, or the regulatory mode is relatively simple. Clinical studies have shown that sildenafil (Lam et al., 2018) has no significant effect on haemodynamics and exercise ability, the effect of eplerenone on follow-up mortality is not clear, and the efficacy nitrate of quality of life cannot be evaluated due to the lack of long-term trials (Dong, 2022). Therefore, more effective measures are still needed to intervene in the development of the disease (Zhang et al., 2022). Previous studies have shown that traditional Chinese medicine can reduce the clinical symptoms of HFpEF, improve the quality of life of patients, enhance overall motor function and prevent the development of HFpEF (Bai, 2022; Tan, 2022). This study summarizes the management process of HFpEF and the clinical evidence and mechanism of traditional Chinese medicine in the treatment of HFpEF and reveals the clinical significance and development prospects of TCM in the treatment of HFpEF.
2 Management strategies for HFpEF
In the past, HFpEF was regarded as an early stage of the transition to HFrEF. Modern research shows that the transition from HFpEF to HFrEF is rare. Compared with HFrEF, HFpEF has higher comorbidity and noncardiovascular mortality (Heinzel and Shah, 2022). Therefore, the guide proposes different management models for HFpEF and HFrEF.
At present, HFpEF lacks a specific diagnostic test. Although Doppler echocardiography can support the diagnosis of HF through evidence such as increased ventricular filling pressure or decreased cardiac output, it cannot support the diagnosis of HFpEF (it cannot reflect LVEF or cardiac morphology) (Dunlay et al., 2017). When physical examination, imaging data, and blood tests are unable to provide a clear basis for diagnosis, an invasive exercise test is necessary (Borlaug, 2020). This is undoubtedly a difficult problem in the process of HFpEF research. From the point of view of treatment, the treatment strategy of HFrEF cannot be fully applied to HFpEF, mainly because there is no symptomatic treatment for the aetiology of HFpEF. Some HFpEF patients complain of chest discomfort, which suggests that the disease may be related to coronary artery disease (Rush et al., 2021), abnormal cardiac metabolism (Mishra and Kass, 2021), and myocardial injury. Dizziness and orthostatic intolerance suggest that HFpEF may be caused by cardiac amyloidosis. Peripheral oedema, abdominal distension, loss of appetite, and early satiety are usually symptoms of late HFpEF complicated with right heart failure. In addition to the aforementioned intractable symptoms, complications closely related to HFpEF should also be considered. A history of atrial fibrillation (Reddy et al., 2018), obesity, diabetes, or metabolic syndrome significantly increases the likelihood of HFpEF. Studies have shown that strategies to relieve cardiac congestion can reduce the hospitalization rate of HFpEF (Borlaug, 2020). Strategies include the use of glucocorticoid receptor antagonists, the management of complications, and the promotion of a healthy and active lifestyle. HFpEF is an important issue in the cardiovascular field. In the future, HFpEF will be more strictly classified to achieve individualized treatment.
3 Evolution of guidelines
As shown in Figure 1, the European Diastolic Heart Failure Research Group proposed in 1998 that the diagnosis of primary diastolic heart failure needs to meet three necessary conditions at the same time: 1) signs or symptoms of pulmonary congestion, 2) evidence of left ventricular abnormality and 3) left ventricular systolic function being normal or only mildly abnormal, with a left ventricular ejection fraction ≥45% (Group, 1998). In 2007, the European Society of Cardiology (ESC) proposed that heart failure with normal ejection fraction (HFNEF) cannot be equated with diastolic heart failure (DHF), and systolic heart failure (SHF) can also have diastolic dysfunction. The consensus is that HFNEF may be the early stage of HFpEF, and the following should be satisfied: 1) signs or symptoms of congestive heart failure, 2) evidence of left ventricular diastolic dysfunction and 3) normal or mildly abnormal left ventricular systolic function (Paulus et al., 2007). Since then, HFpEF and HFNEF have been widely used as terms in North America and Europe, and some people are opposed to using HFpEF instead of HFNEF (Sanderson, 2014). In the 2013 American College of Cardiology Foundation/AHA (ACCF/AHA) guidelines (Yancy et al., 2013), standards are proposed for the definition of HFpEF syndrome, including 1) clinical signs or symptoms of heart failure, 2) evidence that left ventricular ejection fraction is preserved or normal and 3) evidence of abnormal left ventricular diastolic function that can be determined by Doppler echocardiography or cardiac catheterization. HFpEF is classified as EF > 40%, >45%, >50%, and ≥55%. The 2016 ESC/Heart failure Association (HFA) guidelines define HFpEF as ≥ 50% (Ponikowski et al., 2016). HF includes a new category called HFmrEF, with an ejection fraction in the range of 40%–49%. In 2019, the ESC formally established the terminology of HFpEF, and its diagnostic conditions have also been updated: diagnosis based on the HFA-PEFF scoring system, including initial evaluation, UCG, and natriuretic peptide scores, functional tests, and aetiological diagnosis (Pieske et al., 2019). In 2021, to promote the wide application of the guidelines, the previous comprehensive diagnosis was simplified, emphasizing some clinically available variables: LA volume index (LAVI) > 32 mL/m2, mitral E velocity >90 cm/s, septal e’ velocity <9 cm/s, and E/e’ ratio >9 (Mcdonagh et al., 2021). In 2022, the ACC/AHA/HFSA announced two scoring systems. In addition to the previous HFA-PEFF diagnostic scoring system, the H2FPEF scoring system identified risk factors for HFpEF: hypertension, obesity, atrial fibrillation, pulmonary hypertension, advanced age, and average filling pressure height. The guidelines also proposed a new classification of HFimpEF. It is unclear which HFimpEF patients will be classified as HFpEF or HFmrEF, and the evidence for the treatment of HFimpEF is limited (Heidenreich et al., 2022).
4 TCM for HFpEF treatment
4.1 Understanding HFpEF in TCM theory
Originally, in TCM theory there was no separate classification of HFpEF or even HF. The disease is treated solely based on symptoms. During the Western Jin dynasty, the concept of HF was mentioned for the first time in the “Mai Jing” written by Wang Shuhe (Wang, 2019): “If heart failure falls, the pulse sinks.” In modern times, the TCM syndrome types of HF can be divided into qi deficiency and blood stasis, qi and yin deficiency, yang qi deficiency and blood stasis, and exhaustion of yin and yang. At present, there is no exact TCM syndrome for HFpEF, and its basic pathogenesis is deficiency in origin and excess in superficiality. In terms of aetiology, different doctors hold different opinions. Liu Jing (Liu and Xu, 2017) believes that the main cause of HFpEF is qi deficiency and blood stasis accompanied by qi stagnation and blood heat. Zhao Zhiqiang (Zhao et al., 2018) believes that the origin is mainly yin deficiency often combined with qi deficiency and yang deficiency, and the superficiality is mainly blood stasis, phlegm, and heat accumulation. Ji Hongyun (Ji et al., 2020) believes that although there are many causes of HFpEF, qi deficiency and blood stasis always underlie the disease. Shen Bin (Shen, 2018) believes that the basic pathogenesis of HF is the deficiency of heart qi and heart yang, while blood stasis is the key link, and other pathological factors are phlegm and water.
4.2 Clinical evidence of TCM for HFpEF
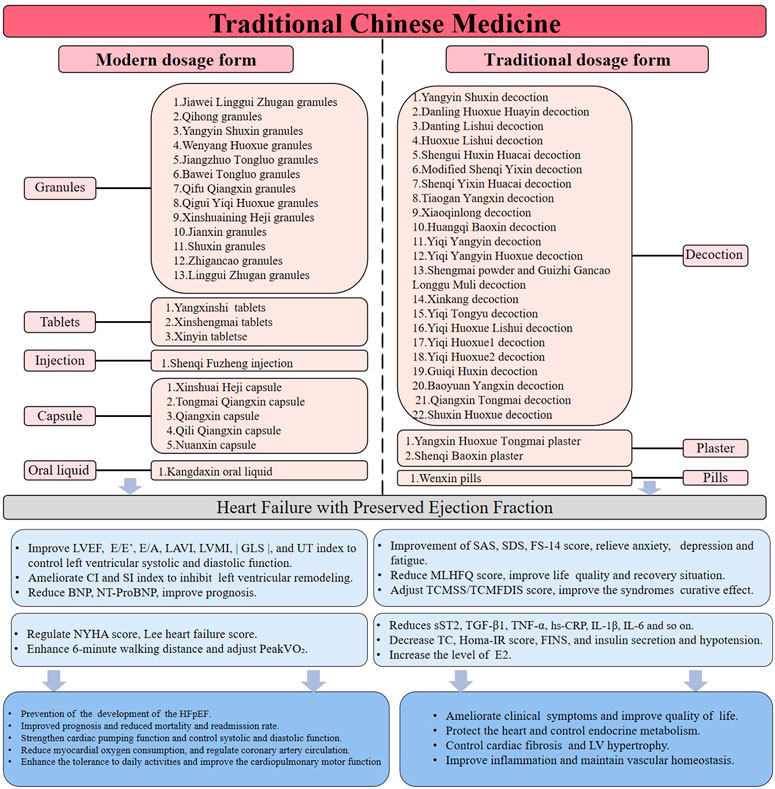
In this paper, 58 clinical randomized controlled trials were collected by VIP, Wanfang, CNKI, SinoMed, PubMed, Embase, Web of Science, Cochrane, and clinical trials. At present, there are a large number of experiments on traditional and modern Chinese medicine dosage forms, as shown in Figure 2. Traditional Chinese medicine dosage forms include decoctions, pills, powders, and plasters. The dosage forms of modern traditional Chinese medicine also include granules, capsules, tablets, suppositories, injections, and so on (Nie et al., 2021). In this paper, 22 different TCM decoctions, 2 different plasters, 1 different pill (Tan, 2022), 13 different granules, 5 different capsules, 3 different tablets (Huang, 2005; Zhang, 2011; Huang et al., 2014; Liu, 2020; Zhu, 2021), 1 different injection (Xu et al., 2020), and 1 different oral liquid (Lin et al., 2016) are discussed as clinical evidence. Supplementary Table S1 analyses and summarizes the clinical evidence of TCM in the treatment of HFpEF, including 1) TCM dosage form, 2) clinical manifestations, and 3) clinical indicators. Based on Supplementary Table S1, Table 1 discusses the experimental mechanism of TCM in the treatment of HFpEF.
4.2.1 Traditional dosage form
4.2.1.1 Decoction
As the most important method of clinical prevention and treatment of diseases in TCM, traditional Chinese medicine decoctions have the characteristics of individual prescription, adding and decreasing with the syndrome, and customizing measures to personal conditions (Chou et al., 2022). At present, it is known that traditional Chinese medicine decoctions can improve clinical symptoms, adjust patients’ cardiac function and prognosis, improve quality of life, regulate abnormal biomarkers, and so on. Most of the decoctions in the study can reduce the TCMSS or TCMFDIS score. Yiqi Yangyin Huoxue decoction (Shen, 2018), Danting Lishui decoction (Chen, 2014; Zou et al., 2014; Zou et al., 2014), Shengui Huxin Huacai decoction (Zhu, 2017), Yiqi Yangyin decoction (Zhang, 2018), Xinkang decoction (Chen, 2019), Shuxin Huoxue decoction (Ma et al., 2020), Guiqi Huxin decoction (Li, 2020), Xiaoqinglong decoction (Zhou, 2020), Shenqi Yixin Huacai decoction (Zhang, 2020), Yiqi Tongyu decoction (Li, 2021), Yiqi Huoxue2 decoction (Liu et al., 2021), Danling Huoxue Huayin decoction (Ji, 2021), Baoyuan Yangxin decoction (Wang, 2021), Tiaogan Yangxin decoction (Sun, 2021) and Modified Shenqi Yixin decoction (Liu et al., 2021) can clearly reduce the clinical symptoms and improve the curative effect of TCM syndrome. Xinkang decoction (Chen and Ye, 2019), Shuxin Huoxue decoction (Ma et al., 2020), Guiqi Huxin decoction (Li, 2020), Danling Huoxue Huayin decoction (Ji, 2021), Yiqi Tongyu decoction (Li, 2021), Yiqi Huoxue2 decoction (Liu et al., 2021), Baoyuan Yangxin decoction (Wang, 2021), Modified Shenqi Yixin decoction (Liu et al., 2021), Huoxue Lishui decoction (Zhou and Hong, 2016), Huangqi Baoxin decoction (Wu, 2018), Yangyin Shuxin decoction (Liu, 2020; Zhao, 2021; Li et al., 2022), Yiqi Huoxue Lishui decoction (Peng et al., 2020), Shengmai powder and Guizhi Gancao Longgu Muli decoction (Yuan, 2021) can increase the 6-min walking distance, improve cardiopulmonary motor function, and enhance the overall motor function of patients. Yiqi Yangyin Huoxue decoction (Shen, 2018), Yiqi Yangyin decoction (Zhang, 2018), Xinkang decoction (Chen and Ye, 2019), Danling Huoxue Huayin decoction (Ji, 2021), Yiqi Tongyu decoction (Li, 2021), Yangyin Shuxin decoction (Liu, 2020), Shengmai powder and Guizhi Gancao Longgu Muli decoction (Yuan, 2021), Qiangxin Tongmai decoction (Zhang, 2019) and Yiqi Huoxue1 decoction (Liu et al., 2020) can reduce the MLHFQ score and improve quality of life. Tiaogan Yangxin decoction (Sun, 2021), Qiangxin Tongmai decoction (Zhang, 2019), and Yiqi Huoxue1 decoction (Liu et al., 2020) can reduce SDS or SAS scores and improve anxiety and depression symptoms. Danting Lishui decoction (Zou et al., 2014), Danling Huoxue Huayin decoction (Ji, 2021), and Baoyuan Yangxin decoction (Wang, 2021) can improve NT-proBNP, prevent the development of HFpEF, improve prognosis, and reduce mortality and rehospitalization rates. Shuxin Huoxue decoction (Ma et al., 2020), Xiaoqinglong decoction (Zhou, 2020), Tiaogan Yangxin decoction (Sun, 2021), and Huoxue Lishui decoction (Zhou and Hong, 2016) can increase the cardiac ejection fraction and improve cardiac function. Huoxue Lishui decoction (Zhou and Hong, 2016) can reduce hs-CRP, improve inflammation, and maintain intravascular homeostasis. Danting Lishui decoction (Zou et al., 2014) can reduce FINS and Homa-IR and interfere with insulin resistance. Guiqi Huxin decoction (Li, 2020) can increase oestradiol, protect the heart, and improve endocrine metabolism. Baoyuan Yangxin decoction (Wang, 2021) reduces TGF-β1 and controls myocardial fibrosis and left ventricular hypertrophy. Danting Lishui decoction (Chen, 2014; Zou et al., 2014), Shengui Huxin Huacai decoction (Zhu, 2017), Baoyuan Yangxin decoction (Wang, 2021), Tiaogan Yangxin decoction (Sun, 2021), and Modified Shenqi Yixin decoction (Liu et al., 2021) can decrease the parameters of E/e’ and LAVI to improve left ventricular diastolic function and inhibit left ventricular remodelling. Yangyin Shuxin decoction (Li et al., 2020) can enhance cardiac pumping function, reduce myocardial oxygen consumption, and improve coronary artery circulation.
4.2.1.2 Plaster
Traditional Chinese medicine plasters are divided into edible black plasters and external applications of white plasters. This article only considers the black plaster prescriptions. Compared with decoctions, black plaster prescriptions can reduce gastrointestinal reactions, enhance the safety of drug use, and help to improve the compliance of patients (Jiang and Tong, 2022). Yangxin Huoxue Tongmai plaster (Wang, 2019; Li, 2020) and Shenqi Baoxin plaster (Chen, 2019) can improve TCM clinical symptoms, enhance TCM efficacy, increase 6-min walking distance, enhance exercise endurance, improve NT-proBNP, prevent the development of HFpEF, improve prognosis, and reduce mortality and rehospitalization rates. Shenqi Baoxin plaster (Chen, 2019) can also reduce MLHFQ scores and improve quality of life.
4.2.2 Modern dosage form
4.2.2.1 Granules
The main advantage of granules is that they have the same curative effect as a decoction, and they are easy to carry and take orally; thus, they are widely used in TCM clinics (Qin et al., 2022). Qifu Qiangxin granules (Bai, 2022), Yangyin Shuxin granules (Zhao et al., 2018), Wenyang Huoxue granules (Gu, 2016), Bawei Tongluo granules (Zhang, 2017), Xinshuaining Heji granules (Wan, 2017), Shuxin granules (Chen, 2018), Jiangzhuo Tongluo granules (Yin et al., 2019), Qigui Yiqi Huoxue granules (Liu, 2020), Jiawei Linggui Zhugan granules (Wang, 2021), Qihong granules (Li, 2021), Zhigancao granules (Zhang et al., 2021), and Jianxin granules (Xin, 2015; Chen et al., 2022) can improve the clinical symptoms of TCM, reduce the scores of TCM syndrome, improve the prognosis, and reduce the mortality and rehospitalization rate. Qifu Qiangxin granules (Bai, 2022), Yangyin Shuxin granules (Zhao et al., 2018), Bawei Tongluo granules (Zhang, 2017), Shuxin granules (Chen, 2018), Jiangzhuo Tongluo granules (Yin et al., 2019), Jiawei Linggui Zhugan granules (Wang, 2021), Qihong granules (Li, 2021), Jianxin granules (Xin, 2015), and Linggui Zhugan granules (Niu, 2021) can lower the MLHFQ score and improve quality of life. Jianxin granules (Chen et al., 2022) can reduce CRP, IL-1β, and IL-6 inflammatory factors to improve inflammation, maintain intravascular homeostasis, reduce BNP to improve prognosis and reduce mortality and rehospitalization rates. Qifu Qiangxin granules (Bai, 2022), Yangyin Shuxin granules (Zhao et al., 2018), Wenyang Huoxue granules (Gu, 2016), Xinshuaining Heji granules (Wan, 2017), Jiangzhuo Tongluo granules (Yin et al., 2019), Qigui Yiqi Huoxue granules (Liu, 2020), and Jianxin granules (Xin, 2015) can improve parameters such as E/e’, E/A, LVEF and LVMI to adjust the left ventricular diastolic function; enhance the cardiac pumping function; reduce myocardial oxygen consumption; inhibit the left ventricular remodelling; and improve coronary artery circulation. Yangyin Shuxin granules (Zhao et al., 2018), Wenyang Huoxue granules (Gu, 2016), Bawei Tongluo granules (Zhang, 2017), and Jiawei Linggui Zhugan granules (Wang, 2021) can increase the 6-min walking distance, enhance tolerance of daily activities and improve cardiopulmonary motor function. Yangyin Shuxin granules (Liu, 2020; Li et al., 2022) can increase the PeakVO index, |GLS| index, and UT index to regulate left ventricular systolic function and systolic synchronization and inhibit myocardial fibrosis and left ventricular hypertrophy.
4.2.2.2 Capsule
TCM capsules are suitable for elderly patients and patients with diabetes. It has high bioavailability and can be rapidly disintegrated and absorbed into the intestines and stomach to achieve effective blood concentration (Zhang et al., 2012). Qili Qiangxin capsule (Lu et al., 2013), Tongmai Qiangxin capsule (Guan et al., 2015), Xinshuai Heji capsule (Gao et al., 2016), Qiangxin capsule (Wu, 2020), and Nuanxin capsule (Lou, 2021) can improve TCM symptoms and reduce the TCM syndrome score. Xinshuai Heji capsule (Gao et al., 2016) and Qiangxin capsule (Wu, 2020) can enhance tolerance of daily activities and improve cardiopulmonary motor function. Qili Qiangxin capsule (Lu et al., 2013), Tongmai Qiangxin capsule (Guan et al., 2015), Qiangxin capsule (Wu, 2020), and Nuanxin capsule (Lou, 2021) improve parameters such as E/e', E/A, LVEF and LAVI to adjust left ventricular systolic and diastolic function; inhibit left ventricular remodelling; enhance cardiac pumping function; reduce myocardial oxygen consumption; and improve coronary artery circulation. Qili Qiangxin capsule (Lu et al., 2013; Gao et al., 2019), Tongmai Qiangxin capsule (Guan et al., 2015), Xinshuai Heji capsule (Gao et al., 2016), and Nuanxin capsule (Lou, 2021) improve NT-proBNP, prevent the development of HFpEF, improve prognosis, and reduce mortality and rehospitalization rates.
In summary, the clinical evidence shows that the main clinical manifestations of TCM in the treatment of HFpEF are as follows: 1) improving the TCM symptoms and the exerting a curative effect on TCM syndrome; improving the quality of life, anxiety, depression, and fatigue of patients, including the MLHFQ score, SAS score, SDS score, and FS-14 score; 2) enhancing tolerance of daily activities and improving cardiopulmonary motor function, including NYHA grade, Lee’s heart failure score, 6-min walk test (6 MWT) and cardiopulmonary exercise test (CPET); 3) strengthening cardiac pumping function, improving systolic and diastolic function, reducing myocardial oxygen consumption, and improving coronary artery circulation. By improving parameters echocardiography such as E/e', E/A, LAVI, LVEF and LVMI, regulating left ventricular systolic function and systolic synchrony by adjusting STI parameters such as |GLS| and UT, and improving haemodynamics by increasing the CI and SI index; and 4) maintaining intravascular homeostasis, including reducing sST2 and hs-CRP to improve systemic inflammation; reducing CRP, IL-1β, IL-6, and other inflammatory factors and decreasing ET, TGF-β1, TNF-α, and AngII to control myocardial fibrosis and left ventricular hypertrophy; improving blood fat and blood pressure, such as total cholesterol (TC) and diastolic blood pressure; improving endocrine metabolism, including by increasing oestrogen E2 levels, interfering with insulin resistance, and reducing Homa-IR and FINS; reducing BNP and NT-proBNP to improve prognosis; and lowering mortality and rehospitalization rates, and preventing the development of HFpEF.
5 Potential mechanisms of TCM for HFpEF
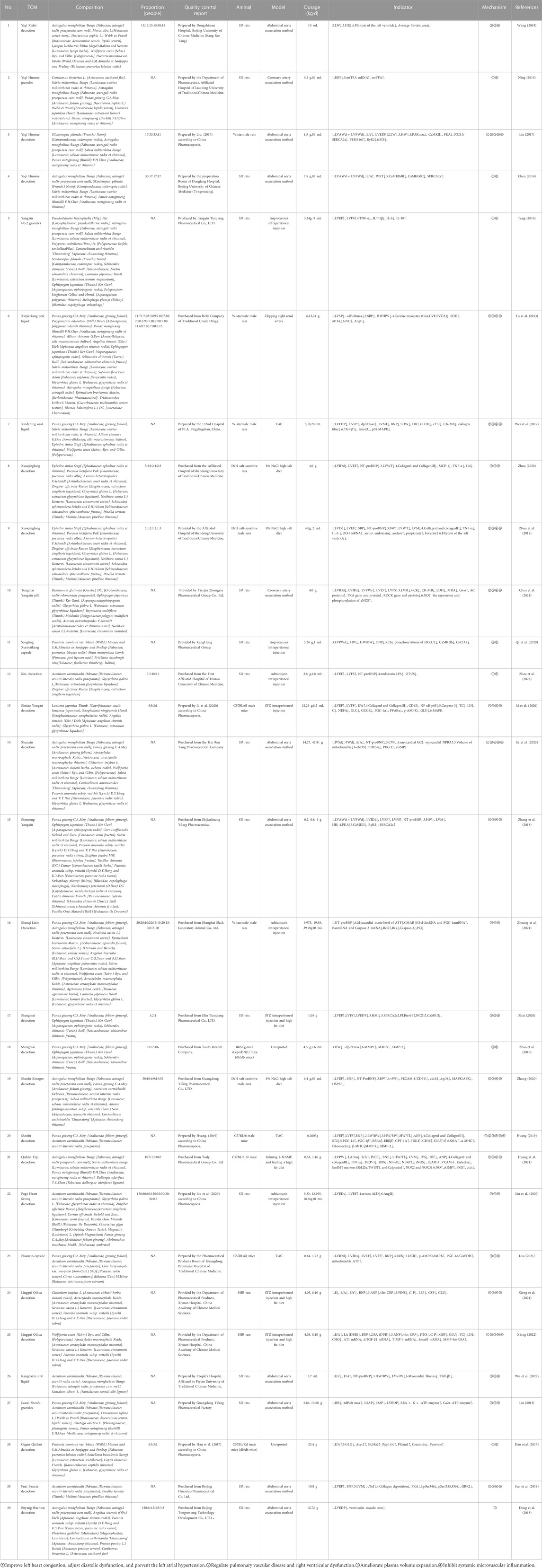
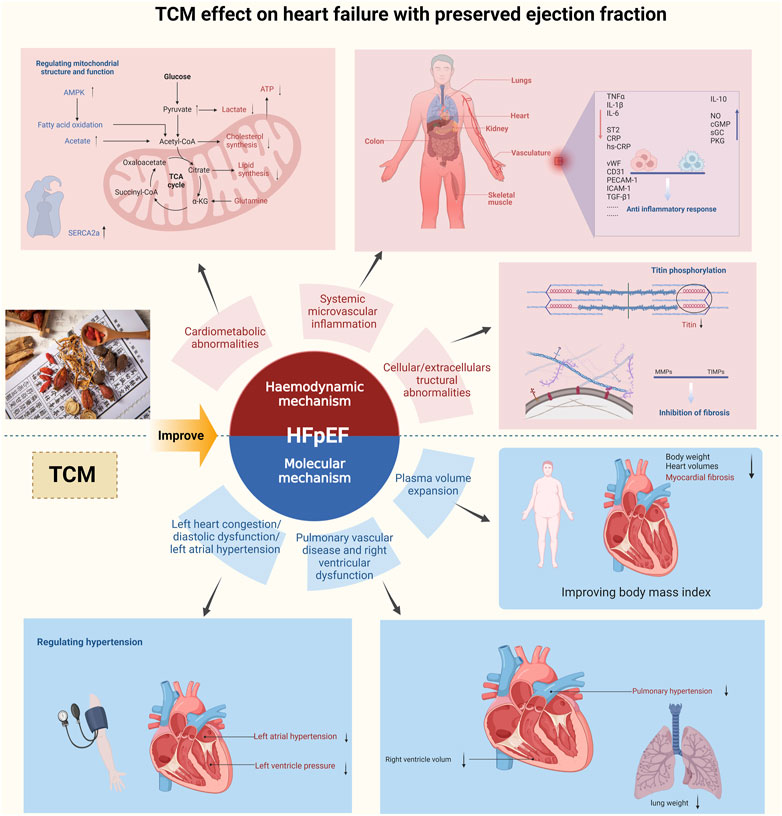
There is no unified conclusion on the specific mechanism of HFpEF. At present, it is widely believed that it is a multisystem disease involving the heart, lung, kidney, skeletal muscle, adipose tissue, immune/inflammatory signals, and vascular system (Mishra and Kass, 2021). According to haemodynamics and cellular and molecular mechanisms, HFpEF is divided into six types (Lam et al., 2018), as shown in Figure 3. There are few articles about the experimental types of HFpEF. In this paper, 12 articles about the experimental types of HFpEF were collected, and the other 18 articles were summarized concerning the similar mechanisms of haemodynamics or cellular molecular science in diastolic heart failure and chronic heart failure.
5.1 Haemodynamic mechanism
At present, three main haemodynamic mechanisms of HFpEF are observed according to the cardiac ultrasound parameters and the improvement of BNP and NT-proBNP.
5.1.1 Left heart congestion/diastolic dysfunction/left atrial hypertension
As HFpEF was originally named after diastolic heart failure, most of the experimental studies in this paper have improved the problem of left ventricular diastolic dysfunction by regulating parameters such as E/e', E/A, LVEDP, BNP, and NT-proBNP. For example, Yiqihuoxue decoction (Chen, 2014; Liu, 2017) can improve diastolic function parameters by adjusting calcium ion homeostasis. Nuanxin capsule (Lou, 2021), Yangxin No. 2 granules (Tang, 2016), Shensong Yangxin decoction (Zhang et al., 2018), Fuzi Banxia decoction (Sun et al., 2019), Shenfu decoction (Huang, 2019), Xiaoqinglong decoction (Zhou et al., 2019; Zhou, 2020), Shengmai decoction (Zhai, 2020), Shenfu Xiongze decoction (Zhang, 2020), Simiao Yongan decoction (Li et al., 2020), Tongmai Yangxin pill (Chen et al., 2021), Sini decoction (Zhao et al., 2022), and Buyang Huanwu decoction (Dong et al., 2018) can improve left ventricular congestion and systolic function by regulating LVID d, LVID s, LVMI, LVEF, and LVFS. Qishen Yiqi decoction (Huang et al., 2021) and Linggui Qihua decoction (Xiong, 2022) can ameliorate left atrial hypertension by regulating LADI/R and LA/Ao.
5.1.2 Pulmonary vascular disease and right ventricular dysfunction
Pulmonary vascular disease and right ventricular dysfunction are rare, the prognosis is poor, and the mortality is high (Lam et al., 2018). Shenfu decoction (Huang, 2019), Linggui Qihua decoction (Xiong, 2022), Yiqi Huoxue decoction (Liu, 2017), and Yiqi Xiefei decoction (Wang, 2019) can improve the lung weight index, lung weight, lung-to-body ratio, and corresponding ultrasound parameters. Among them, Linggui Qihua decoction (Xiong, 2022) can regulate the right atrial volume and reduce stress.
5.1.3 Plasma volume expansion
The expansion of plasma volume is mainly related to right heart dilatation and total cardiac volume expansion. Shengmai decoction (Zhao et al., 2016; Zhai, 2020), Qishen Yiqi decoction (Huang et al., 2021), Linggui Qihua decoction (Xiong, 2022), Yiqi Huoxue decoction (Liu, 2017), Xinjierkang oral liquid (Yu et al., 2013), Xindening oral liquid (Wei et al., 2017), Shensong Yangxin Songling Xuemaikang capsule (Qi et al., 2020) and Kangdaxin oral liquid (Wu et al., 2022) can improve ANP, heart weight, the heart-to-body ratio, the myocardial ratio, and corresponding problems. Fuzi Banxia decoction (Sun et al., 2019), Xiaoqinglong decoction (Zhou et al., 2019; Zhou, 2020), Shenfu Xiongze decoction (Zhang, 2020), Sini decoction (Zhao et al., 2022), Qishen Yiqi decoction (Huang et al., 2021), Yiqi Xiefei decoction (Wang, 2019), Linggui Qihua decoction (Xiong et al., 2021), and Shunxin decoction (Jia et al., 2022) can improve myocardial hypertrophy, myocardial fibrosis, and other myocardial problems. Qishen Yiqi decoction (Huang et al., 2021) and Shengmai decoction (Zhai, 2020) can improve plasma volume expansion by reducing obesity or regulating diabetes.
5.2 Cellular and molecular mechanism
5.2.1 Systemic microvascular inflammation
The comorbidity of HFpEF leads to systemic microvascular inflammation, including circulatory inflammation, myocardial inflammation, extracardiac organ inflammation (e.g., lung, kidney, and skeletal muscle inflammation), and diseases associated with inflammation (such as obesity and hyperlipidaemia).
The problems caused by systemic microvascular inflammation include endothelial dysfunction, oxidative stress, and decreased bioavailability. Experimental research shows that the TCM YangxinNo.2 Granules (Tang, 2016), Shenfu decoction (Huang, 2019), Xiaoqinglong decoction (Zhou et al., 2019; Zhou, 2020), Qishen Yiqi decoction (Huang et al., 2021) and Linggui Qihua decoction (Xiong et al., 2021; Xiong, 2022) can reduce pro-inflammatory cytokines TNF-α, IL-6, IL-1β, MCP-1, soluble ST2, CRP, and hs-CRP. YangxinNo.2 granules (Tang, 2016) can also increase the expression of the anti-inflammatory factor IL-10. Xindening oral liquid (Wei et al., 2017), Xiaoqinglong decoction (Zhou et al., 2019; Zhou, 2020), Shenfu Xiongze decoction (Zhang, 2020), Simiao Yongan decoction (Li et al., 2020), Qishen Yiqi decoction (Huang et al., 2021), Linggui Qihua decoction (Xiong, 2022) and Kangdaxin oral liquid (Wu et al., 2022) can reduce collagen I, collagen III, vWF, CD31, ICAM-1, VCAM-1, TGF-β1, and CD45 to improve myocardial inflammation. In addition, Xiaoqinglong decoction (Zhou et al., 2019) and Sini decoction (Zhao et al., 2022) can also regulate intestinal flora, reduce serum endotoxin, and increase acetate, propionate, and butyrate to improve extracardiac inflammation.
Systemic microvascular inflammation can activate ROS and reduce the utilization of NO and cGMP, which leads to an increase in cAMP or PKA, and an imbalance in intracellular Ca2+. Low availability of cGMP leads to low expression of PKG, inhibition of titin phosphorylation, and decreased myocardial compliance. On the one hand, TCM improves oxidative stress: Nuanxin capsule (Lou, 2021) and Qishen Yiqi decoction (Huang et al., 2021) can reduce the activities of ROS and MDA. Xinjierkang oral liquid (Yu et al., 2013) and Shenqi Lixin decoction (Zhuang et al., 2021) can increase the availability of NO and cGMP, improve the PKG channel, and enhance the protein and gene expression of SOD and Bcl-2. Poge Heart-Saving decoction (Liu et al., 2020) inhibits the RASS system to reduce the production of AngII. On the other hand, to improve endothelial dysfunction, Fuzi Banxia decoction (Sun et al., 2019), Shenfu Xiongze decoction (Zhang, 2020), and Xindening oral liquid (Wei et al., 2017) can inhibit important molecules P38 and MAPKAPK in the VEGF pathway. Xinjierkang oral liquid (Yu et al., 2013), Tongmai Yangxin pill (Chen et al., 2021), and Shunxin decoction (Jia et al., 2022) can enhance myocardial compliance by increasing NPRA, GC, and eNOS in the cGMP/PKG signalling pathway to increase cGMP and PKG in cardiomyocytes. Shensong Yangxin decoction (Zhang et al., 2018) can decrease PKA, RyR2, NOX2, and NOX3 to maintain Ca2+ homeostasis.
5.2.2 Cardiometabolic abnormalities
Abnormal Cardiac metabolism is mainly due to myocardial energy damage, which is caused by three mechanisms: 1) abnormal structure and function of mitochondria, 2) changes in substrate utilization, and 3) intracellular calcium overload. The structural and functional abnormalities of mitochondria are reflected in organelle dyspnoea, shrinkage, enlargement, a decrease in membrane potential, and other problems, resulting in a decrease in ATP synthesis. Due to the change in mitochondrial function and structure, the utilization of substrate changes accordingly, the heart changes from fatty acid metabolism to glucose metabolism, glucose oxidation decreases, glucose degradation occurs, and lactic acid increases. At the same time, SERCA2a deficiency eventually leads to intracellular calcium overload.
Experimental studies have shown that the TCM Nuanxin capsule (Lou, 2021), Shenfu decoction (Huang, 2019), Simiao Yongan decoction (Li et al., 2020), Shunxin decoction (Jia et al., 2022), Shenqi Lixin decoction (Zhuang et al., 2021), Jiawei Shenfu granules (Liu, 2013), and Yiqihuoxue granules (Ning, 2019) can regulate the volume of mitochondria and enhance the gene and protein expression of PGC-1α, PGC-1β, ERR-α and ERR-β to protect the ultrastructure. They can also activate the AMPK pathway to inhibit phosphorylation, inhibit caspase3 and increase Bcl-2 to prevent mitochondrial apoptosis and enhance OCR and ATP to improve respiratory function. Shenfu decoction (Huang, 2019) and Gegen Qinlian decoction (Han et al., 2017) optimize the metabolism and utilization of fatty acids, glucose, and pyruvate to different degrees and enhance the expression of carnitine palmitoyltransferase 1A (CPT-1A), pyruvate dehydrogenase kinase-4 (PDK4), fatty acid translocase (CD36) and glucose transporter (GLUT4). Simiao Yongan decoction (Li et al., 2020) increases PGam1, pyruvate to reduce sugar degradation, PPAR-α, and ceramide. Linggui Qihua decoction (Xiong et al., 2021) can reduce FINS, GSP, and GLU to regulate glucose and lipid metabolism. Shensong Yangxin decoction (Zhang et al., 2018), Shengmai decoction (Zhai, 2020), Jiawei Shenfu granules (Liu, 2013), Yiqi Huoxue decoction (Chen, 2014; Liu, 2017), and Songling Xuemaikang capsule (Qi et al., 2020) can increase the expression of SERCA2a and NCX1 to reduce intracellular Ca2+ overload. In addition, they can inhibit RyR2 and CaMKII to reduce the release of Ca2+, and inhibit ERK1/2, leading to downregulation of GATA4 and improvement of BNP.
5.2.3 Cellular/extracellular structural abnormalities
PKG, cGMP, and Titin phosphorylation in cardiomyocytes jointly regulate myocardial contractile motion, and the high expression of Titin in cardiomyocytes reflects the decrease in Titin phosphorylation. TCM Fuzibanxia decoction (Sun et al., 2019), Tongmai Yangxin pill (Chen et al., 2021), Qishen Yiqi decoction (Huang et al., 2021), Yiqi Huoxue decoction (Liu, 2017), and Shunxin decoction (Jia et al., 2022) can reduce PDE5A or PKA to increase eNOS and cGMP, activate the PKG pathway, regulate Titin phosphorylation to inhibit Titin, and improve myocardial compliance.
Structural abnormalities of myocardial extracellular matrix (ECM), including fibrosis and amyloid protein, can occur. ECM mainly depends on the balance of MMPs and TIMPs. If the balance is lost, myocardial fibrosis will occur. In addition, TGF-β/Smads, p38MAPK, the G protein-coupled receptor kinase (GRK) signal pathway, and TGF-β1 expression induced by AngII can all lead to the development of fibrosis. TCM Shenfu decoction (Huang, 2019), Linggui Qihua decoction (Xiong, 2022), and Shengmai decoction (Zhao et al., 2016) can regulate ECM deposition and balance the relationship between MMP-9, MMP2, TIMP-1, and TIMP-2. Xiaoqinglong decoction (Zhou et al., 2019) and Yiqi Xiefei decoction (Wang, 2019) can reduce the area of fibrosis. Shenfu Xiongze decoction (Zhang, 2020), Simiao Yongan decoction (Li et al., 2020), Linggui Qihua decoction (Xiong, 2022), Xindening oral liquid (Wei et al., 2017), Songling Xuemaikang capsule (Qi et al., 2020), and Kangdaxin oral liquid (Wu et al., 2022) can inhibit P38, MAPK, Smad3, TGF-β1, and AngII.
6 Conclusion and perspectives
The number of deaths caused by HFpEF worldwide is gradually increasing every year, and increasing attention has been given to the prevention and treatment of HFpEF. Western medicine treatment can control the development of HFpEF, but it still faces the bottleneck problem. While developing new drugs and devices, modern medicine has recognized the individual treatment advantages and overall regulatory effects of TCM.
At present, the integration of traditional Chinese and Western medicine has become an objective and generally accepted medical model in the treatment of HFpEF. TCM treatment can improve the clinical symptoms of HFpEF, enhance the quality of life of patients, lower the poor prognosis of patients, reduce mortality and rehospitalization rates, and provide new ideas and methods for the treatment strategy of HFpEF. However, due to the diversity of TCM syndrome types and the strong subjectivity of dialectical analysis, TCM lacks certain convincing power in the process of development. The relationship between TCM and botanical drugs lacks a rigorous scientific research system, and the relationship between the ‘monarch’ and ‘minister’ in the compound prescription of TCM is seldom discussed. In addition, most of the studies on the treatment of HFpEF with TCM have a small sample size, short observation time, and lack of rigor in design. Therefore, the research results cannot be widely applied and popularized. In the future, research on TCM in the treatment of HFpEF should start from the following three angles 1) In terms of theory, it is convenient to distinguish syndrome types by setting an objective threshold for dialectical analysis. The purpose of the research is to analyse the relationship between the existing compound prescriptions of TCM and botanical drugs. 2) From a clinical perspective, we need to standardize the clinical design; perform large-sample, multicentre randomized clinical controlled trials; enhance the observation and follow-up time; and evaluate the effectiveness and safety of TCM on HFpEF. 3) In terms of experiments, people should identify the subtypes of HFpEF and expand different modelling methods to consider different mechanisms of TCM treatment to provide new ideas for improving HFpEF.
In summary, HFpEF is still a thorny clinical disease. TCM has great potential for HFpEF. However, more extensive and rigorous clinical and animal experiments are needed to promote the application of TCM in HFpEF.
Author contributions
YF, ZY, and LW performed the literature search, selected relevant articles, interpreted data, and wrote the report; YaL, YS, and YuL revised the manuscript; XW, ZZ, and JM designed and supervised this work. YF and ZY contributed equally to this work and shared the first authorship; All authors have read and approved the final submission.
Funding
This work was supported by the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine (No: ZYYCXTD-C-202203), the “Innovation Team Development Plan” of the Ministry of Education-Research on the prevention and treatment of cardiovascular diseases in traditional Chinese medicine (No: IRT_16R54). We also thank Biorender (https://biorender.com/) for design of the online figures by Biorender and its linguistic assistance during the preparation of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1154167/full#supplementary-material
References
Bai, Z. X. (2022). Clinical study on Qifu Qiangxin decoction in the treatment of Heart Yang deficiency, blood stasis and fluid retention syndrome of heart failure with preserved ejection fraction. Changsha: Hunan University of Chinese Medicine.
Beldhuis, I. E., Myhre, P. L., Bristow, M., Claggett, B., Damman, K., Fang, J. C., et al. (2021). Spironolactone in patients with heart failure, preserved ejection fraction, and worsening renal function. J. Am. Coll. Cardiol. 77 (9), 1211–1221. doi:10.1016/j.jacc.2020.12.057
Borlaug, B. A. (2020). Evaluation and management of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 17 (9), 559–573. doi:10.1038/s41569-020-0363-2
Chen, C., Zhang, W. S., Yang, Y. H., Chen, L., and Li, X. (2022). Clinical efficacy observation of Jianxin granule on elderly heart failure with preserved ejection fraction of qi deficiency and blood stasis type. Shanxi J. Traditional Chin. Med. 38 (01), 16–19. doi:10.20002/j.issn.1000-7156.2022.01.006
Chen, H. (2018). Study on the clinical efficacy of Shuxin decoction in the treatment of heart failure with preserved ejection fraction. Hefei: Anhui University of Chinese Medicine.
Chen, L. P., and Ye, X. H. (2019). Therapeutic effect of Xinkang decoction for heart failure with preserved ejection fraction differentiated as qi deficiency, blood stasis and fluid retention syndrome. J. Guangzhou Univ. Traditional Chin. Med. 36 (4), 471–475. doi:10.13359/j.cnki.gzxbtcm.2019.04.005
Chen, R., Chen, T., Wang, T., Dai, X., Zhang, S., Jiang, D., et al. (2021). Tongmai Yangxin pill reduces myocardial No-reflow via endothelium-dependent NO-cGMP signaling by activation of the cAMP/PKA pathway. J. Ethnopharmacol. 267, 113462. doi:10.1016/j.jep.2020.113462
Chen, T. (2019). Clinical observation of Shenqi Baoxin decoction in treating heart failure preserved ejection fraction (Qi deficiency and blood stasis). ChengTu: Chengdu University of Traditional Chinese Medicine.
Chen, X. H. (2014). The effect of Blood Activating Water Relieving method on cardiac diastolic function in patients with HFpEF. Harbin: Heilongjiang University Of Chinese Medicine.
Chen, X. J. (2014). Study on the effect of Yiqi Huoxue drugs on calcium transport related gene and protein expression in rats with diastolic dysfunction. Beijing: Beijing University of Chinese Medicine.
Chinese Cardiovascular Health and Disease Reporting Group (2022). Summary of Chinese cardiovascular health and disease report 2021. Chin. Circulation J. 37 (06), 553–578. doi:10.3969/j.issn.1000-3614.2022.06.001
Chou, M., Yang, J., and Wang, X. Y. (2022). Suitability of traditional Chinese medicine decoction mate for inhibiting bitterness and masking taste in classic famous prescriptions. Chin. Traditional Herb. Drugs 53 (08), 2292–2301. doi:10.7501/j.issn.0253-2670.2022.08.005
Cui, X. J., Xie, B., Yi, X. Q., Chen, Z. J., Lei, Y., Huang, X. F., et al. (2022). Progress in pharmacological therapy for heart failure with preserved ejection fraction, 1–12.Her. Med.
Dong, G. J. (2022). Interpretation of updated key points of heart failure with preserved ejection fraction in the 2022 AHA/ACC/HFSA guideline for the management of heart failure. Chin. J. Evidence-based Med. 22 (10), 1117–1124.
Dong, X., Wang, Z., Li, J. B., and Shen, X. X. (2018). Effect of Buyang Huanwu decoction on cardiac diastolic function in rats with diastolic heart failure. Int. J. Traditional Chin. 40 (11), 1055–1058. doi:10.3760/cma.j.issn.1673-4246.2018.11.013
Dunlay, S. M., Roger, V. L., and Redfield, M. M. (2017). Epidemiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 14 (10), 591–602. doi:10.1038/nrcardio.2017.65
Gao, C., Jin, L. Z., Wen, L., Wang, Q., and Liu, Z. P. (2019). Clinical study on Qili Qiangxin capsule for treatment of chronic heart failure with preserved ejection fraction. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis. 17 (17), 2621–2623. doi:10.12102/j.issn.1672-1349.2019.17.018
Gao, S. M., He, D. Y., Liu, H. Y., Liu, F., and Peng, J. (2016). The effect of Xinshuai Heji on improvement of symptoms in patients with chronic heart failure and NT-proBNP. J. Emerg. Traditional Chin. 25 (6), 1090–1092. doi:10.3969/j.issn.1004-745X.2016.06.044
Group, E. S. (1998). How to diagnose diastolic heart failure. European study Group on diastolic heart failure. Eur. Heart J. 19 (7), 990–1003. doi:10.1053/euhj.1998.1057
Gu, J. L. (2016). Clinical observation of the intervention of Wenyang Huoxue method in heart failure with preserved ejection fraction. Shanghai: Shanghai University of Traditional Chinese Medicine.
Guan, H., He, J., Luo, H. L., Huang, J. H., and Li, S. H. (2015). Effect of Tongmai Qiangxin capsule on cardiac function and serum NT-proBNP level in patients with heart failure with normal ejection fraction. Med. Forum.
Han, J., Wang, Z., Xing, W., Yuan, Y., Zhang, Y., Lv, T., et al. (2017). Effect of gegen qinlian decoction on cardiac gene expression in diabetic mice. Int. J. Genomics 2017, 7421761. doi:10.1155/2017/7421761
Heidenreich, P. A., Bozkurt, B., Aguilar, D., Allen, L. A., Byun, J. J., Colvin, M. M., et al. (2022). 2022 AHA/ACC/HFSA guideline for the management of heart failure. J. Card. Fail. 28 (5), e1–e167. doi:10.1016/j.cardfail.2022.02.010
Heinzel, F. R., and Shah, S. J. (2022). The future of heart failure with preserved ejection fraction: Deep phenotyping for targeted therapeutics. Herz 47 (4), 308–323. doi:10.1007/s00059-022-05124-8
Huang, Q. (2005). The study of influence of XinShengmai tablets on related vasoactive substances in patients with heart failure. Tianjin: Tianjin University of Traditional Chinese Medicine.
Huang, Q., Zhang, Y., and Zhen, Y. (2014). Effect of Xinshengmai tablets on cardiovascular risk factors in HFNEF patients. Chin. J. Integr. Med. Cardio Cerebrovasc. Dis. 12 (01), 20–21. doi:10.3969/j.issn.1672-1349.2014.01.0011
Huang, Y. T. (2019). Study on the mechanism of the effect of Shenfu compatibility on energy metabolism in chronic heart failure in mice. Tianjin: Tianjin University of Traditional Chinese Medicine.
Huang, Y., Zhang, K., Liu, M., Su, J., Qin, X., Wang, X., et al. (2021). An herbal preparation ameliorates heart failure with preserved ejection fraction by alleviating microvascular endothelial inflammation and activating NO-cGMP-PKG pathway. Phytomedicine 91, 153633. doi:10.1016/j.phymed.2021.153633
Ji, H. Y. (2021). Observation on curative effect of danling huoxue Huayin decoction in treating chronic heart failure with preserved ejection fraction (blood stasis and fluid retention). Changsha: Hunan University of Chinese Medicine.
Ji, H. Y., Yu, Z. K., Cheng, X. N., Zhou, Z. X., and Zhai, S. Y. (2020). Research on medication rules of Chinese medicine for the treatment of heart failure with preserved ejection fraction based on data mining. Clin. J. Traditional Chin. Med. 32 (11), 2104–2108. doi:10.16448/j.cjtcm.2020.1132
Jiang, Y., and Tong, J. Y. (2022). Clinical study on bushen Huoxue paste for premature ovarian insufficiency of kidney deficiency and blood stasis type. New Chin. Med. 54 (18), 92–96. doi:10.13457/j.cnki.jncm.2022.18.021
Jiaying, Z., Xiangxiang, W., Xuefeng, L. I., Yang, Y., Yinghuan, D., Yanbin, S., et al. (2022). Shunxin decoction improves diastolic function in rats with heart failure with preserved ejection fraction induced by abdominal aorta constriction through cyclic guanosine monophosphate-dependent protein kinase Signaling Pathway. J. Tradit. Chin. Med. 42 (5), 764–772. doi:10.19852/j.cnki.jtcm.20220519.003
Lam, C. S. P., Voors, A. A., de Boer, R. A., Solomon, S. D., and van Veldhuisen, D. J. (2018). Heart failure with preserved ejection fraction: From mechanisms to therapies. Eur. Heart J. 39 (30), 2780–2792. doi:10.1093/eurheartj/ehy301
Lewis, G. A., Dodd, S., Clayton, D., Bedson, E., Eccleson, H., Schelbert, E. B., et al. (2021). Pirfenidone in heart failure with preserved ejection fraction: A randomized phase 2 trial. Nat. Med. 27 (8), 1477–1482. doi:10.1038/s41591-021-01452-0
Li, B., Liu, W. H., Li, X. S., Shi, L., and Shao-Ke, G. U. (2020). Using Speckle tracking imaging to evaluate the left ventricular systolic function of heart failure with preserved ejection fraction by treatment of Yangyin Shuxin decoction. Chin. J. Integr. Traditional West. Med. 40 (9), 1064–1069. doi:10.7661/j.cjim.20200817.285
Li, G. (2021). Efficacy of Qihong granules on heart failure with preserved ejection fraction of Qi Deficiency and Blood Stasis. Urumqi: Xinjiang medical university.
Li, J. (2020). Effect of Yangxin Huoxue Tongmai plaster on quality of life in patients with HFpEF (Heart-qi deficiency, phlegm and blood stasis blocking collaterals). Changsha: Hunan University of Chinese Medicine.
Li, J. J. (2021). Clinical observation of Yiqi Tongyu decoction in treating heart failure with preserved ejection fraction. Harbin: Heilongjiang University of Traditional Chinese Medicine.
Li, L., Chen, X., Su, C., Wang, Q., Li, R., Jiao, W., et al. (2020). Si-Miao-Yong-An decoction preserves cardiac function and regulates GLC/AMPK/NF-κB and GLC/PPARα/PGC-1α pathways in diabetic mice. Biomed. Pharmacother. 132, 110817. doi:10.1016/j.biopha.2020.110817
Li, Q., Su, L., Zhou, R., Tang, E., Liu, Y., Cheng, T., et al. (2022). Efficacy and safety of Yangyin Shuxin decoction-a Chinese herbal medicine formula for heart failure with preserved ejection fraction: A randomized controlled trial. Med. 2022, 1486366. doi:10.1155/2022/1486366
Li, X. Y. (2020). To observe the clinical effect of Guiqi Huxin decoction in the treatment of heart failure with preserved ejection fraction (Qi deficiency and blood stasis type) and its effect on estradiol. Harbin: Heilongjiang University Of Chinese Medicine.
Lin, C., Yan, P., Li, C. Y., Zhen, F., Qiao, J. F., and Xiong, S. Q. (2016). Prevalence and factors of elevated alanine aminotransferase in central Taiwan - a retrospective study. Fujian J. Traditional Chin. Med. 47 (04), 11–12+15. doi:10.7603/s40681-016-0011-7
Liu, J. (2017). Study on the mechanism of Yiqi Huoxue drugs in preventing and treating diastolic dysfunction based on calcium homeostasis of cardiomyocytes. Beijing: Beijing University of Chinese Medicine.
Liu, J., and Xu, H. (2017). Discuss the prevention and treatment of heart failure with preserved ejection fraction from the theory of qi and blood. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis. 15 (17), 2210–2213. doi:10.3969/j.issn.1672-1349.2017.17.041
Liu, L., Mo, Y., Wu, B., Yu, Z., and Sun, B. (2020). Effect of traditional Chinese medicine poge heart-saving decoction on cardiac function in heart failure rat model. Evid.-based Complement. Altern. Med. 2020, 8762509. doi:10.1155/2020/8762509
Liu, L., Yang, Y., Zou, G. L., Wu, X., Zhang, P. P., and Han, Y. B. (2021). Clinical observation of Modified Shenqi Yixin decoction in the treatment of heart failure and Heart-kidney Yang deficiency syndrome with HFpEF. Chin. J. Integr. Med. Cardio Cerebrovasc. Dis. 19 (18), 3061–3063. doi:10.12102/j.issn.1672-1349.2021.18.002
Liu, L., Zhang, J., Zou, G. L., Sui, Y. B., and Han, Y. B. (2021). Determining the kinetics of break-induced replication (BIR) by the assay for monitoring BIR elongation rate (AMBER). Liaoning J. Traditional Chin. Med. 48 (11), 139–154. doi:10.1016/bs.mie.2021.09.004
Liu, Q. (2020). Clinical effect of Qigui Yiqi Huoxue granules on elderly patients with chronic HFpEF. Guiyang: Guizhou University of Traditional Chinese Medicine.
Liu, Q. J. (2013). Study on chronic heart failure and myocardial energy metabolism with Jiawei Shenfu granules. Guiyang: Guangzhou University of Chinese Medicine.
Liu, S. Y., and Zhang, Y. (2020). Research of the clinical efficacy of Yiqi Huoxue decoction in the treatment of heart failure with preserved ejection fraction. Clin. J. Traditional Chin. Med. 32 (11), 2141–2145. doi:10.16448/j.cjtcm.2020.1140
Liu, W. H. (2020). Effect of Yangyin Shuxin decoction on cardiac function and exercise tolerance in patients with heart failure with ejection fraction. Tianjin: Tianjin University of Traditional Chinese Medicine.
Liu, X. M. (2020). Intervention study of Yangxinshi tablets on exercise intensity and quality of life on heart failure with preserved ejection fraction. Jinan: Shandong University of Traditional Chinese Medicine.
Lou, T. T. (2021). Study on the effect of Nuanxin capsule on energy metabolism in patients with HFpEF. Guangzhou: Guangzhou University of Chinese Medicine.
Lu, T. Q., Zhao, Y., Meng, Q. H., Li, Y., and Feng, S. J. (2013). Clinical research on the Qili Qiangxin capsule in the adjuvant treatment of heart failure with preserved ejection fraction. Prog. Mod. Biomed. 13 (22), 4292–4294+4301. doi:10.13241/j.cnki.pmb.2013.22.009
Ma, A. L., Huang, Q. S., and Huang, X. Y. (2020). Effect of Shuxin Huoxue recipe on TCM syndrome and related cardiac function indexes of patients with heart failure with preserved ejection fraction and qi-deficiency and blood-stasis syndrome. Shanxi J. Traditional Chin. Med. 36(8), 8–10. doi:10.3969/j.issn.1000-7156.2020.08.004
Mcdonagh, T. A., Metra, M., Adamo, M., Gardner, R. S., Baumbach, A., Böhm, M., et al. (2021). 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42 (36), 3599–3726. doi:10.1093/eurheartj/ehab368
Mishra, S., and Kass, D. A. (2021). Cellular and molecular pathobiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 18 (6), 400–423. doi:10.1038/s41569-020-00480-6
Nie, H. Y., Xu, L. X., and Li, G. (2021). Current situation and discussion on the development of modern dosage forms of traditional Chinese patent medicines. China J. Traditional Chin. Med. Pharm. 36 (11), 6347–6351.
Ning, X. (2019). Experimental study on the effect of Yiqi Huoxue compound on mitochondrial metabolism in rats with chronic heart failure. Shenyang: Liaoning University of Traditional Chinese Medicine.
Niu, J. X. (2021). Clinical observation of Linggui Zhugan decoction in the treatment of chronic heart failure with preserved ejection fraction. Tianjin: Tianjin University of Traditional Chinese Medicine.
Omote, K., Verbrugge, F. H., and Borlaug, B. A. (2022). Heart failure with preserved ejection fraction: Mechanisms and treatment strategies. Annu. Rev. Med. 73, 321–337. doi:10.1146/annurev-med-042220-022745
Paulus, W. J., and Tschöpe, C. (2013). A novel paradigm for heart failure with preserved ejection fraction: Comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 62 (4), 263–271. doi:10.1016/j.jacc.2013.02.092
Paulus, W. J., Tschöpe, C., Sanderson, J. E., Rusconi, C., Flachskampf, F. A., Rademakers, F. E., et al. (2007). How to diagnose diastolic heart failure: A consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the European society of Cardiology. Eur. Heart J. 28 (20), 2539–2550. doi:10.1093/eurheartj/ehm037
Peng, L., B, L. X., Mei, Y. B., Liu, J. J., and Ni, W. (2020). Effect of Yiqi Huoxue Lishui Prescription combined with Spironolactone in the treatment of heart failure with preserved ejection fraction in the elderly. China Med. Her. 17 (17), 57–61.
Pieske, B., Tschöpe, C., de Boer, R. A., Fraser, A. G., Anker, S. D., Donal, E., et al. (2019). How to diagnose heart failure with preserved ejection fraction: The HFA–PEFF diagnostic algorithm: A consensus recommendation from the heart failure association (HFA) of the European society of Cardiology (ESC). Eur. Heart J. 40 (40), 3297–3317. doi:10.1093/eurheartj/ehz641
Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G. F., Coats, A. J. S., et al. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37 (27), 2129–2200. doi:10.1093/eurheartj/ehw128
Qi, J., Tan, Y., Fan, D., Pan, W., Yu, J., Xu, W., et al. (2020). Songling Xuemaikang Capsule inhibits isoproterenol-induced cardiac hypertrophy via CaMKIIδ and ERK1/2 pathways. J. Ethnopharmacol. 253, 112660. doi:10.1016/j.jep.2020.112660
Qin, L., Yu, M., Zhang, H., Jia, H., Ye, X., and Zou, Z. (2022). Quality markers of Baizhu dispensing granules based on multi-component qualitative and quantitative analysis combined with network pharmacology and chemometric analysis. J. Ethnopharmacol. 288, 114968. doi:10.1016/j.jep.2022.114968
Reddy, Y. N. V., Obokata, M., Gersh, B. J., and Borlaug, B. A. (2018). High prevalence of occult heart failure with preserved ejection fraction among patients with atrial fibrillation and dyspnea, 534–535.
Rush, C. J., Berry, C., Oldroyd, K. G., Rocchiccioli, J. P., Lindsay, M. M., Touyz, R. M., et al. (2021). Prevalence of coronary artery disease and coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 6 (10), 1130–1143. doi:10.1001/jamacardio.2021.1825
Sanderson, J. E. (2014). HFNEF, HFpEF, HF-PEF, or DHF. JACC Heart Fail. 2 (1), 93–94. doi:10.1016/j.jchf.2013.09.006
Schrutka, L., Seirer, B., Rettl, R., Dachs, T., Binder, C., Duca, F., et al. (2022). Heart failure with preserved ejection fraction: Calculating the risk of future heart failure events and death. Front. Cardiovasc. Med. 9, 921132. doi:10.3389/fcvm.2022.921132
Shen, B. (2018). Clinical study on the treatment of heart failure with preserved ejection fraction (Qi Yin deficiency) with Qiyin huoxue decoction. Jinan: Shandong University of Traditional Chinese Medicine.
Sun, F., Huang, Y., Li, L., Wang, Y., Zhuang, P., and Zhang, Y. (2019). PKA/β2-AR-Gs/Gi signaling pathway is associated with anti-inflammatory and pro-apoptotic effects of Fuzi and Banxia combination on rats subjected to pressure overload. J. Ethnopharmacol. 235, 375–384. doi:10.1016/j.jep.2019.02.011
Sun, S. Y. (2021). Clinical observation of self-designed Tiaogan Yangxin decoction in the treatment of HFpEF accompanied by anxiety. Jinan: Shandong University of Traditional Chinese Medicine.
Tan, J. L. (2022). Effect of Wenxin pills on heart failure with preserved ejection fraction (Yang deficiency and water flooding syndrome). Shijiazhuang: Hubei University of Chinese Medicine.
Tang, L. P. (2016). Experimental study on the effect of Yangxin No.2 granules on serum inflammatory cytokines of rats with chronic heart failure model. Nanjing: Nanjing University Of Chinese Medicine.
Teramoto, K., Teng, T. K., Chandramouli, C., Tromp, J., Sakata, Y., and Lam, C. S. (2022). Epidemiology and clinical features of heart failure with preserved ejection fraction. Card. Fail. Rev. 8, e27. doi:10.15420/cfr.2022.06
Wan, H. (2017). Clinical efficacy observation of Xinshuaining Heji granules in treating heart failure with preserved ejection fraction (Heart-kidney Yang deficiency, water and blood stasis type). GuiYang Coll. Traditional Chin. Med.
Wang, C. (2019). Effect of Yiqi Xiefei decoction on cardiac diastolic function of rats with heart failure with preserved ejection fraction. Beijing: Beijing University of Chinese Medicine.
Wang, Q. X. (2019). Clinical observation on Yangxin Huoxue Tongmai plaster in treating heart failure with preserved ejection fraction of Heart-Qi deficiency and phlegm and blood stasis syndrome. Changsha: Hunan University of Chinese Medicine.
Wang, S. C. (2021). Clinical study on the treatment of heart failure with preserved ejection fraction (Yang deficiency and blood stasis type) of Jiawei Linggui Zhugan Decoction. Kunming: Yunnan University of Chinese Medicine.
Wang, Z. P. (2021). To observe the clinical efficacy of Baoyuan Yangxin decoction in treating heart failure with preserved ejection fraction (QI deficiency and blood stasis syndrome) and its fffect on TGF-β1 level. Harbin: Heilongjiang University Of Chinese Medicine.
Wei, Y., Guo, C., Zhao, J., Yang, J., Yi, W., Liu, H., et al. (2017). X indening oral liquid improves cardiac function of rats with chronic cardiac failure via TGF-ß1/Smad3 and p38 MAPK pathway. Anat. J. Cardiol. 17 (5), 367–373. doi:10.14744/AnatolJCardiol.2016.7438
Wu, W. (2018). Clinical observation of Huangqi Baoxin Decoction in the treatment of heart failure with preserved ejection fraction. Nanjing: Nanjing University of Chinese Medicine.
Wu, X. (2020). Effect of Qiangxin capsule on left ventricular diastolic function in elderly patients with HFpEF (Yang deficiency and water flooding). Kunming: Yunnan University of Chinese Medicine.
Wu, X., Zhang, T., Qiao, J., Li, C., Lin, C., and Xiong, S. (2022). Effects of Kangdaxin on myocardial fibrosis in heart failure with preserved ejection fraction rats. J. Thorac. Dis. 14 (4), 1157–1163. doi:10.21037/jtd-22-198
Xin, L. (2015). Clinical study of improving quality of life on patients with HFpEF by Jianxin granules. Fuzhou: Fujian University of Traditional Chinese Medicine.
Xiong, S. (2022). Clinical study on the distribution of TCM syndromes in patients with HFpEF and the mechanism of Linggui Qihua Decoction in the intervention of HFpE. Beijing: China Academy of Chinese Medical Science.
Xiong, S., Liu, J. G., Dong, G. J., Ma, L., Tang, R., and Cheng, Y. (2021). Effects of Linggui Qihua Decoction on cardiac function and glucose and lipid metabolism in rats with heart failure with preserved ejection fraction. Tianjin J. Traditional Chin. Med. 38 (07), 909–916. doi:10.11656/j.issn.1672-1519.2021.07.2
Xu, Z. Q., Zhang, Y., Lian, M., Gu, H. H., and Wang, J. (2020). A preliminary study on the mechanism of clinical efficacy of Shenqi Fuzheng injection in the treatment of the elderly patients with HFpEF. Geriatrics Health Care 26 (4), 537–541. doi:10.3969/j.issn.1008-8296.2020.04.008
Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey, D. E. J., Drazner, M. H., et al. (2013). 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology foundation/American heart association task force on practice guidelines. J. Am. Coll. Cardiol. 62 (16), e147–e239. doi:10.1016/j.jacc.2013.05.019
Yin, J., Niu, T., Liu, T., Li, J., Qi, H., Geng, Q., et al. (2019). Clinical observation on Jiangzhuo Tongluo Granules combined with Western medicine in the treatment of 36 cases of heart failure with preserved ejection fraction of intermingled phlegm and blood stasis type. J. Tradit. Chin. Med. 60(2019), 1832–1836. doi:10.13288/j.11-2166/r.2019.21.006
Yu, T. T., Guo, K., Chen, H. C., Lan, C. Z., Wang, J., Huang, L. L., et al. (2013). Effects of traditional Chinese medicine Xinjierkang formula on 2K1C hypertensive rats: Role of oxidative stress and endothelial dysfunction. BMC Complement. Altern. Med. 13, 173. doi:10.1186/1472-6882-13-173
Yuan, S. M. (2021). Shengmai powder and Guizhi Gancao Longgu Muli decoction in the treatment of the elderly heart failure with preserved ejection fraction. Nanjing: Nanjing University of Chinese Medicine.
Zhai, Q. (2020). Study on protective mechanism of Shengmai decoction on cardiac function in diabetic rats. Beijing: China Academy of Chinese Medical Science.
Zhang, C. H., Gong, L. M., and Wang, W. M. (2012). “Review on preparation of Chinese medicine soft capsules,” in The third annual conference of Chinese traditional medicine commodities and the first seminar on kudzu international industry development. The third annual conference of Chinese traditional medicine commodities and the first seminar on kudzu international industry development (Changsha, Hunan, China, 295–303.
Zhang, D. D. (2020). The clinical efficacy of Yiqi Huoxue method and its influences of myocardial energy expenditure. Harbin: Heilongjiang University Of Chinese Medicine.
Zhang, G. Y., Wang, Z. H., Fan, J. R., and Li, L. (2022). Research progress of traditional Chinese medicine in treatment of heart failure with preserved ejection fraction. Med. Recapitulate 28 (13), 2679–2683. doi:10.3969/j.issn.1006-2084.2022.13.032
Zhang, H. (2017). Clinical study of heart failure with preserved ejection fraction treated with Yiqi Yangyin Tongluo treatment. Taiyuan: Shanxi Provincial Institute of Traditional Chinese Medicine.
Zhang, H. F. (2018). Clinical observation of Yiqi Yangyin Decoction in treating heart failure with preserved ejection fraction (Qi Yin deficiency). Xian: Shaanxi University of Chinese Medicine.
Zhang, N., Zhao, Y., Liu, Y., Tang, N., Zheng, W., Mao, M., et al. (2021). A double-blinded, placebo-controlled randomized trial evaluating the efficacy and safety of Zhigancao tang granules for treating HFpEF: Study protocol for a randomized controlled trial. Trials 22 (1), 293. doi:10.1186/s13063-021-05232-6
Zhang, W., Sun, Q., Chen, H., and Zhang, Q. (2018). Effect of shensong yangxin on heart failure in preserved ejection fraction rat model. Trop. J. Pharm. Res. 17 (12), 2427–2432. doi:10.4314/tjpr.v17i12.17
Zhang, X. Q. (2020). Study on the protection and mechanism of Shenfu Xiongze decoction on cardiac microvessels in HFpEF rats. Xian: Shaanxi University of Chinese Medicine.
Zhang, Y. (2011). Clinical observation of Xinshengmai tablets in treating heart failure with preserved ejection fraction. Chin. J. Inf. Traditional Chin. Med. 18 (05), 75–76. doi:10.3969/j.issn.1005-5304.2011.05.033
Zhang, Y. (2019). The clinical efficacy of Yiqi Huoxue Chinese medicine in treating patients with HFpEF and depression. Shenyang: Liaoning University of Traditional Chinese Medicine, 40.
Zhao, J., Cao, T., Tian, J., Chen, H., Zhang, C., Wei, H., et al. (2016). Shengmai san ameliorates myocardial dysfunction and fibrosis in diabetic db/db mice. Evid.-based Complement. Altern. Med. 2016, 4621235–4621239. doi:10.1155/2016/4621235
Zhao, Y. Y. (2021). Correlation analysis between TCM syndrome elements and cardiopulmonary exercise test indexes in patients with heart failure with preserved ejection fraction. Tianjin: Tianjin University of Traditional Chinese Medicine.
Zhao, Z., Liu, J., Hu, Y., Zhang, X., Cao, L., Dong, Z., et al. (2022). Bacterial diversity in the intestinal mucosa of heart failure rats treated with Sini Decoction. BMC Complement. Med. Ther. 22 (1), 93. doi:10.1186/s12906-022-03575-4
Zhao, Z. Q., Wang, X. L., Zhang, P., Bi, Y. F., Zhou, R. J., and Li, D. (2018). Effect of Yangyin Shuxin granules on quality of life in heart failure with normal ejection fraction. J. Tradit. Chin. Med. 59 (21), 1843–1847. doi:10.13288/j.11-2166/r.2018.21.011
Zhou, G. F. (2020). Clinical observation and experimental study of the Xiaoqinglong decoction on heart failure with preserved ejection fraction of harmful fluid retention. Jinan: Shandong University of Traditional Chinese Medicine.
Zhou, G., Jiang, Y., Ma, D., Wang, Y., Yang, J., Chen, J., et al. (2019). Xiao-qing-long tang prevents cardiomyocyte hypertrophy, fibrosis, and the development of heart failure with preserved ejection faction in rats by modulating the composition of the gut microbiota. Biomed. Res. Int. 2019, 9637479. doi:10.1155/2019/9637479
Zhou, L. G., and Hong, Y. F. (2016). Effects of Chinese botanical drugs for activating blood and eliminating water on cardiac function and serum proBNP, hs-CRP and TNF-α of patients with HFNEF. Beijing J. Traditional Chin. Med. 35 (02), 109–112. doi:10.16025/j.1674-1307.2016.02.004
Zhu, H. L. (2021). The clinical study of xinyin tablet in treatment of qi yin deficiency and blood stasis syndrome in heart failure with preserved ejection fraction. Guangzhou: Guangzhou University of Chinese Medicine.
Zhu, K. H. (2017). The clinical observation of the Shengui Huxin decoction to treat HFpEF (Heart-Yang Deficiency). Harbin: Heilongjiang University Of Chinese Medicine.
Zhuang, J., Zhu, J., Dou, Y., Chen, X., Chen, H., Liu, X., et al. (2021). Shenqi Lixin Decoction improves cardiac function in rats with adriamycin-induced heart failure through modulation of PGC-1α and mitochondrial apoptosis pathway. Ann. Transl. Med. 9 (20), 1592. doi:10.21037/atm-21-5350
Zou, G. L., Zhong, W. L., Jin, J., Sui, Y. B., and Liu, L. (2014). Intervention effect of activating blood circulation and promoting diuresis on insulin resistance in patients with heart failure with normal ejection fraction. Acta Chin. Med. Pharmacol. 42 (02), 123–124. doi:10.19664/j.cnki.1002-2392.2014.02.045
Zou, G. L., Zhong, W. L., Sui, Y. B., Jin, J., and Liu, L. (2014). Effect of blood activating water relieving method on heart functions and serum levels of NT-proBNP in patients with heart failure with normal ejection fraction. Chin. J. Integr. Traditional West. Med. 34 (2), 146–148. doi:10.7661/CJIM.2014.02.0146
Glossary
Keywords: heart failure with preserved ejection fraction, traditional Chinese medicine, clinical evidence, potential mechanisms, cardiovascular disease
Citation: Fan Y, Yang Z, Wang L, Liu Y, Song Y, Liu Y, Wang X, Zhao Z and Mao J (2023) Traditional Chinese medicine for heart failure with preserved ejection fraction: clinical evidence and potential mechanisms. Front. Pharmacol. 14:1154167. doi: 10.3389/fphar.2023.1154167
Received: 30 January 2023; Accepted: 24 April 2023;
Published: 10 May 2023.
Edited by:
Yaozu Xiang, Tongji University, ChinaReviewed by:
Youhua Wang, Shanghai University of Traditional Chinese Medicine, ChinaYujuan Li, Tongji University, China
Copyright © 2023 Fan, Yang, Wang, Liu, Song, Liu, Wang, Zhao and Mao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianliang Wang, eGx3YW5nMTk4MUAxMjYuY29t; Zhiqiang Zhao, cXVhbm1pbmd6aGFvQDEyNi5jb20=; Jingyuan Mao, anltYW9AMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yujian Fan1†
Yujian Fan1† Zhihua Yang
Zhihua Yang Lin Wang
Lin Wang Yu Liu
Yu Liu Xianliang Wang
Xianliang Wang Jingyuan Mao
Jingyuan Mao