
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Pharmacol., 07 March 2023
Sec. Neuropharmacology
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1149511
This article is part of the Research TopicBiomarkers of Mental Well-being Continuum across Life Span: from Excelling to CrisisView all 8 articles
A correction has been applied to this article in:
Corrigendum: Could peripheral 5-HT level be used as a biomarker for depression diagnosis and treatment? A narrative minireview
The serotonin hypothesis of depression is still influential, but the relationship between peripheral 5-HT levels and depression is still unknown. This review aimed to verify whether peripheral 5-HT levels could be used as a biomarker for depression diagnosis and treatment. PubMed and EMBASE were searched using terms appropriate to the area of research. Articles from 1957 to 2022 in the following terms were identified: depression, 5-HT, serotonin and peripheral (serum, plasma, blood platelets). 33 studies were included: seven clinical trials about periphery 5-HT levels in depressive patients compared to normal subjects, 15 clinical trials about changes of peripheral 5-HT levels in patients with depression after drug treatment and 11 animal experiments about peripheral 5-HT levels in animal models of depression. Peripheral 5-HT levels presented three different outcomes before and after antidepressant treatments: increased, decreased and no significant change. In conclusion, changes in peripheral 5-HT levels did not show consistent results among these studies. Peripheral 5-HT level could not be used as a biomarker both for depression diagnosis and for antidepressant efficacy evaluation.
Depression is a common mental disorder. Patients with depression tend to exhibit slowness of thought, agitation and sustained low mood. Those with major depressive disorder (MDD) may suffer from a range of other symptoms such as psychomotor disorders and cognitive impairment, even suicide (Kandola et al., 2019). According to a World Health Organization report, approximately 280 million people (about 3.8% of the total population) are suffering from depression worldwide. More than 75% of depression patients in developing countries do not receive proper diagnosis and treatment (Herrman et al., 2022).
Decades of studies on the pathological mechanisms of depression have not yet led to a complete elucidation. The development of depression is usually considered to be related to numerous factors including genetic, environmental, immune, endocrine and neurogenesis (Jesulola et al., 2018), and many pathogenetic hypotheses have been proposed up to the present.
As early as 1956, Coppen A et al. advanced a novel serotonin (5-HT) hypothesis on depression pathogenesis. In the central nervous system (CNS), 5-HT is an inhibitory neurotransmitter synthesized in the presynaptic neuron. 5-HT synthesis reduction, release reduction, or reuptake increase leads to a decrease of the 5-HT level in the synaptic cleft, and thus induces the onset of depression (Coppen, 1967). Based on this hypothesis, the selective serotonin reuptake inhibitors (SSRIs, such as fluoxetine and citalopram) have been developed and have been shown to improve symptoms in depression patients (Delgado, 2000).
In peripheral system, 5-HT as one of autacoids is synthesized and distributed in enterochromaffin cells, and stored in cell granules with ATP. Under the effect of stimulation factors, 5-HT is released from the granules, diffused into the blood, and absorbed and stored by platelets, accounting for about 8% of the total 5-HT in the body.
In this context, the correlation between 5-HT synaptic level and peripheral 5-HT level has become a curious concern of pharmacologists. Could the peripheral 5-HT level reflect the synaptic 5-HT level to some extent? Could the peripheral 5-HT level be used to diagnosis, to assess treatment efficacy of antidepressants? Many scientists have been efforted to better clarify the association, however, the efforts have been greatly hindered by the difficulty of direct measuring 5-HT level in patients’ synaptic cleft. Despite all this, researchers have conducted numerous studies on 5-HT level in plasma, serum and platelets in the diagnosis and treatment of depression, trying to confirm the possibility of the peripheral 5-HT level as a biomarker for depression diagnosis and treatment.
Unfortunately, as literature review found, no consistent evidence has been presented yet to clarify the relationship between peripheral 5-HT level and depression development. In this article, we reviewed the current evidence with the hope of providing ideas for the follow-up research on the relationship between 5-HT level and depression diagnosis and treatment.
PubMed and EMBASE were searched to collect relevant publications on peripheral 5-HT level and depression. The search formula of PubMed was (“Depression” [MeSH Terms] OR “Depress*” [tiab] OR “chronic mild stress” [tiab]) AND (“Serotonin/blood” [Mesh] OR “Serotonin” [Tiab] OR 5-HT [Tiab] OR “hydroxytryptamine” [Tiab]) AND (“peripheral” [tiab] OR “serum” [MeSH Terms] OR “serum” [tiab] OR “plasma” [MeSH Terms] OR “plasma” [tiab] OR “blood platelets” [MeSH Terms] OR “platelet*” [tiab] OR “blood” [tiab]) AND 1957:2022 [pdat]. And the search formula of EMBASE was (“depression”/mj OR “depress*”:ab,ti) AND (“serotonin”/mj OR “5-ht”:ab, ti OR “serotonin”:ab, ti OR “5-hydroxytryptamine”:ab,ti) AND (“serum”/mj OR “plasma”/mj OR “thrombocyte”/mj OR “serum”:ab, ti OR “plasma”:ab, ti OR “thrombocyte”:ab, ti OR “platelet”:ab,ti) AND ([animals]/lim OR [randomized controlled trial]/lim OR “controlled clinical trial”/de) AND [<1957-2022]/py. The detailed processes were shown in Figure 1.
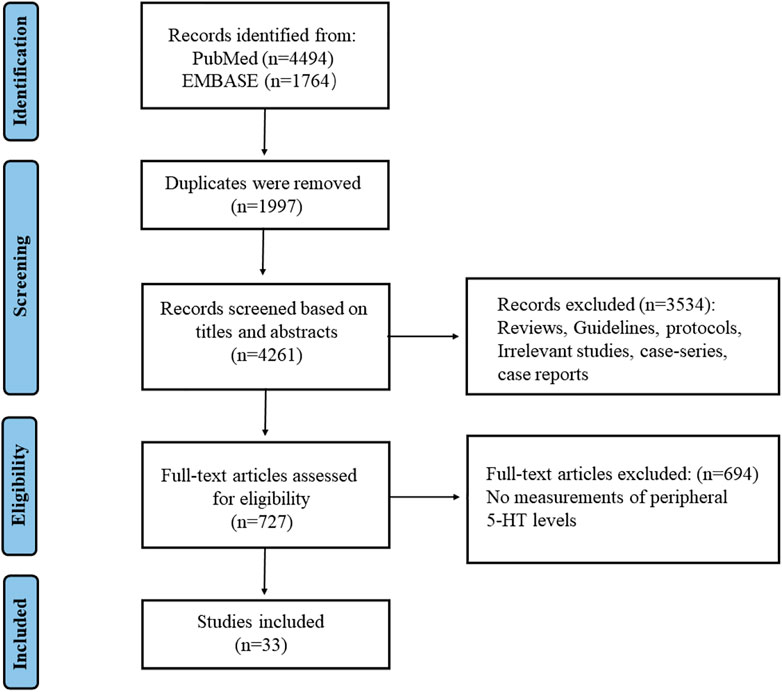
FIGURE 1. The search process and the screening of the articles for identifying the eligible studies.
Briefly, the MADRS, HAMD, HDRS and HAMA are the most commonly used scales for assessing depression symptoms and for assessing antidepressants efficacy in clinical practice (Zimmerman et al., 2013; Obeid et al., 2018; Paketci, 2021). The depression score criteria are respectively as follows. The MADRS offers scores on the following scale: <12 (normal/remission), 12 to 22 (mild depression), 22 to 30 (moderate depression), 30 to 35 (major depression), >35 (extreme depression). The HAMD has two types of scoring: the HAMD-17 and the HAMD-24. The HAMD-17 is scored on a scale of 7–17 (probably depressed), 18 to 24 (depressed) and >24 (severely depressed); the HAMD-24 is scored on a scale of 9–20 (probably depressed), 21 to 35 (depressed) and >35 (severely depressed). The HDRS is rated on a scale of 0 (normal), 1 (mild depression), 2 (moderate depression), 3 (major depression) and 4 (very severe depression). The HAMA is scored on a scale as follows: <7 (no anxiety symptoms), 7 to 14 (possible anxiety symptoms), 14 to 21 (anxiety symptoms), 21 to 29 (significant anxiety symptoms), and ≥29 (severe anxiety symptoms).
Lots of evidences found that the negative life events are highly precipitating factors in developing depression. Chronic stress is the primary trigger for depression. An optimal animal model should replicate the signs, symptoms and behavioral manifestations of the disease observed in the clinic. Therefore, many chronic stress-induced depressive-like behavior animal model has been developed by using a range of mild, variable and random stimulus stressors on rats/mice. Among them CUMS (chronic unpredictable mild stress) animal model was a representative which was first designed in rats by Katz (Katz, 1982), and later improved by Papp and Willner (Papp et al., 1991; Willner et al., 1992). Besides, the chronic mild stress model of mice were first using by Monleon et al. (1995). Because of its effectiveness in perfectly simulating the clinical symptoms of depression to a large extent, this model is now the most widely used and appropriate animal model in depression research (Hao et al., 2019). A series of behavioral tests are widely used to assess depression severity, including sucrose preference test (SPT), tail suspension test (TST), forced swimming test (FST) and open field test (OFT) and so on (Hao et al., 2019). There is no recognized and objective biomarker for depression diagnosis in animal experiments.
5-HT level in the cerebrospinal fluid (CSF) has been measured and documented its association with depression severity in patients with MDD (Hou et al., 2006). However, since it is not easy to obtain CSF sample from patients as well as brain tissue biopsy, few work directly measures the 5-HT level in the CNS up to date. The peripheral serum, plasma and platelet in circulation system therefore become accessible sample to test 5-HT level.
Various peripheral samples display different 5-HT level. For rough estimation, the 5-HT in serum equals to 5-HT in plasma and 5-HT in platelet (Lee et al., 2014; Choi et al., 2020), it is unclear that which sample of 5-HT is more related to the degree of depression. Based on results in 1,094 outpatients with depression, Choi et al. (2021) believed that serum 5-HT level could be used as a biomarker of antidepressants response . However, Mück-Seler et al. (2002) suggested that platelet 5-HT level could predict the therapeutic effect of paroxetine in depression patients. Bianchi et al. (2002) furthermore considered that platelet 5-HT might reflect 5-HT level in neuron in CNS, while plasma 5-HT reflect the 5-HT in synaptic cleft in experimental animal. The alterations of peripheral 5-HT level might have a ripple effect on 5-HT levels in the CNS (Bordukalo-Niksic et al., 2010). In fact, as the inhibition of platelet 5-HT uptake by antidepressants is highly consistent with the inhibition of synaptic 5-HT uptake (Da Prada et al., 1988), it is reasonable to consider that possibility of peripheral serum, plasma or platelet 5-HT to be used as biomarker of depression (Read et al., 2017).
In terms of group-comparison results, peripheral 5-HT level in depression patients demonstrated different outcome compared to normal healthy counterparts (shown in Table 1). Four studies showed that peripheral 5-HT level in depression patients were higher than normal subjects, one study reported peripheral 5-HT level in depression patients were lower than normal subjects, meanwhile two studies showed no significant difference.
Fifteen papers on the relevance between peripheral 5-HT level and the drug treatment response in depression patients were retrieved (Table 2). The samples were whole blood, serum, plasma and platelets from depression patients. In terms of self-comparison results, five researches reported an increase in peripheral 5-HT levels after drug treatment. Nine researches reported a diametrically opposite result. The remaining one work reported no definite changes in peripheral 5-HT levels after drug treatment.
Since it is relatively easy to obtain sample from animal brain tissue, many studies were conducted to explore the association between central 5-HT level and depressive behavioral performance in animals. Most studies seem to support the 5-HT hypothesis. The 5-HT level in the hippocampus, cortex and prefrontal cortex (PFC) of depression-phenotype mice or rats were significantly reduced compared to the normal groups, and after antidepressant treatment, the 5-HT levels were increased and the animals’ depressive behaviors were significantly improved. Of course, there was report of contrary results. One study showed that the 5-HT levels of depression-phenotype rats in hippocampus were significantly increased compared to the normal group, while decreased after treating with citalopram, a SSRI (Li et al., 2015).
As to peripheral 5-HT level, elevenpapers on the relevance between peripheral 5-HT level and the antidepressant treatment response in depression-phenotype mice or rats were retrieved (Table 3). Eight experiments showed that the peripheral 5-HT level in depression-phenotype mice or rats were lower than normal ones, and after antidepressant treatments, the 5-HT levels were increased combined with improvements in depressive-like behavior. Two studies showed that the peripheral 5-HT levels were decreased after antidepressant treatments. The remaining one study reported no significant differences in peripheral 5-HT levels after antidepressant treatments, although the depressive-like behavior in animal were improved. These different or contradictory results may be explained by different animal species, modelling methods, drugs (including doses and period), sample and sampling methods, measuring methods, and so on.
Many SSRIs based on 5-HT hypothesis have made a significant contribution to the treatments of depressive disorders. 5-HT level has been used to guide clinical decision on whether to use or continue to use, or even discontinue antidepressants (Maund et al., 2019). Here 5-HT level should be 5-HT in synaptic cleft rather than in peripheral system. Just due to the difficulty in sampling from CNS, peripheral sample has to be adopted to replace in measuring central 5-HT level (van Buel et al., 2019). From the evidence listed above, unfortunately, it does not work. Peripheral 5-HT level could not be used as a biomarker both for depression diagnosis and for antidepressant efficacy evaluation.
The inconsistent results suggested that the onset of depressive disorders might not be solely induced by a deficiency of 5-HT. It might be related to many other factors such as receptors on dendrites, the receptive apparatus of nerve cells, various subtypes of 5-HT receptors for various antidepressant drugs (Yohn et al., 2017). A combination of factors such as dosing cycles, patient’s age, race, gender, environment and dietary habits might have contribution to this inconsistence.
The peripheral 5-HT levels showed inconsistent results before and after antidepressant treatments both in clinical trials and animal experiments. In summary, peripheral 5-HT level could not be used as a biomarker both for depression diagnosis and for antidepressant efficacy evaluation..
This research determined that peripheral 5-HT level could not be used as a biomarker both for depression diagnosis and for antidepressant efficacy evaluation, and plasma 5-HT level might be a possible biomarker to demonstrate its association with depression. However, our samples so small that perhaps with larger samples, the conclusions—especially those relating to animal data—might change. This study will help researchers pay more attention to the relationship between plasma 5-HT and depression. In future, more and more work should be efforted to achieve comparability of data.
CL and QC drafted the manuscript; ZS, ZC, and JC provided intellectual input; FX revised the manuscript and all approved the final version.
We are grateful to the Sixth People’s Hospital South Campus, Shanghai Jiaotong University and Shanghai Municipal Science Commission, for providing the funding to perform this project. [Grant number 19411971700].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alvarez, J. C., Gluck, N., Arnulf, I., Quintin, P., Leboyer, M., Pecquery, R., et al. (1999a). Decreased platelet serotonin transporter sites and increased platelet inositol triphosphate levels in patients with unipolar depression: Effects of clomipramine and fluoxetine. Clin. Pharmacol. Ther. 66 (6), 617–624. doi:10.1053/cp.1999.v66.103402001
Alvarez, J. C., Gluck, N., Fallet, A., Grégoire, A., Chevalier, J. F., Advenier, C., et al. (1999b). Plasma serotonin level after 1 day of fluoxetine treatment: A biological predictor for antidepressant response? Psychopharmacology 143 (1), 97–101. doi:10.1007/s002130050924
Bianchi, M., Moser, C., Lazzarini, C., Vecchiato, E., and Crespi, F. (2002). Forced swimming test and fluoxetine treatment: In vivo evidence that peripheral 5-HT in rat platelet-rich plasma mirrors cerebral extracellular 5-HT levels, whilst 5-HT in isolated platelets mirrors neuronal 5-HT changes. Exp. Brain Res. 143 (2), 191–197. doi:10.1007/s00221-001-0979-3
Bismuth-Evenzal, Y., Gonopolsky, Y., Gurwitz, D., Iancu, I., Weizman, A., and Rehavi, M. (2012). Decreased serotonin content and reduced agonist-induced aggregation in platelets of patients chronically medicated with SSRI drugs. J. Affect. Disord. 136 (1-2), 99–103. doi:10.1016/j.jad.2011.08.013
Bordukalo-Niksic, T., Mokrovic, G., Stefulj, J., Zivin, M., Jernej, B., and Cicin-Sain, L. (2010). 5HT-1A receptors and anxiety-like behaviours: Studies in rats with constitutionally upregulated/downregulated serotonin transporter. Behav. Brain Res. 213 (2), 238–245. doi:10.1016/j.bbr.2010.05.002
Castrogiovanni, P., Blardi, P., De Lalla, A., Dell'Erba, A., and Auteri, A. (2003). Can serotonin and fluoxetine levels in plasma and platelets predict clinical response in depression? Psychopharmacol. Bull. 37 (2), 102–108.
Chen, Y., Wan, M., Zhong, Y., Gao, T., Zhang, Y., Yan, F., et al. (2021a). Partially hydrolyzed guar gum modulates gut microbiota, regulates the levels of neurotransmitters, and prevents CUMS-induced depressive-like behavior in mice. Mol. Nutr. Food Res. 65 (16), e2100146. doi:10.1002/mnfr.202100146
Cheng, R., Xu, W., Wang, J., Tang, Z., and Zhang, M. (2021c). The outer membrane protein Amuc_1100 of Akkermansia muciniphila alleviates the depression-like behavior of depressed mice induced by chronic stress. Biochem. Biophys. Res. Commun. 566, 170–176. doi:10.1016/j.bbrc.2021.06.018
Choi, W., Kim, J. W., Kang, H. J., Kim, H. K., Kang, H. C., Lee, J. Y., et al. (2021). Interaction effect of serum serotonin level and age on the 12-week pharmacotherapeutic response in patients with depressive disorders. Sci. Rep. 11 (1), 24226. doi:10.1038/s41598-021-03753-3
Choi, W., Moon, J. H., and Kim, H. (2020). Serotonergic regulation of energy metabolism in peripheral tissues. J. Endocrinol. 245 (1), R1-R10. doi:10.1530/JOE-19-0546
Coppen, A. (1967). The biochemistry of affective disorders. Br. J. Psychiatry J. Ment. Sci. 113 (504), 1237–1264. doi:10.1192/bjp.113.504.1237
Da Prada, M., Cesura, A. M., Launay, J. M., and Richards, J. G. (1988). Platelets as a model for neurones? Experientia 44 (2), 115–126. doi:10.1007/BF01952193
Delgado, P. L. (2000). Depression: The case for a monoamine deficiency. J. Clin. Psychiatry 61 (6), 7–11.
Dvojkovic, A., Nikolac Perkovic, M., Sagud, M., Nedic Erjavec, G., Mihaljevic Peles, A., Svob Strac, D., et al. (2021). Effect of vortioxetine vs. escitalopram on plasma BDNF and platelet serotonin in depressed patients. Prog. Neuro-psychopharmacology Biol. Psychiatry 105, 110016. doi:10.1016/j.pnpbp.2020.110016
Figueras, G., Pérez, V., San Martino, O., Alvarez, E., and Artigas, F. (1999). Pretreatment platelet 5-HT concentration predicts the short-term response to paroxetine in major depression. Grupo de Trastornos Afectivos. Biol. Psychiatry 46 (4), 518–524. doi:10.1016/s0006-3223(98)00344-8
Franke, L., Schewe, H. J., Müller, B., Campman, V., Kitzrow, W., Uebelhack, R., et al. (2000). Serotonergic platelet variables in unmedicated patients suffering from major depression and healthy subjects: Relationship between 5HT content and 5HT uptake. Life Sci. 67 (3), 301–315. doi:10.1016/s0024-3205(00)00620-2
Greaney, J. L., Dillon, G. A., Saunders, E. F. H., and Alexander, L. M. (2020). Peripheral microvascular serotoninergic signaling is dysregulated in young adults with major depressive disorder. J. Appl. Physiology 128 (1), 100–107. doi:10.1152/japplphysiol.00603.2019
Hao, Y., Ge, H., Sun, M., and Gao, Y. (2019). Selecting an appropriate animal model of depression. Int. J. Mol. Sci. 20 (19), 4827. doi:10.3390/ijms20194827
Herrman, H., Patel, V., Kieling, C., Berk, M., Buchweitz, C., Cuijpers, P., et al. (2022). Time for united action on depression: A lancet-world psychiatric association commission. Lancet (London, Engl. 399, 957–1022. doi:10.1016/S0140-6736(21)02141-3
Hou, C., Jia, F., Liu, Y., and Li, L. (2006). CSF serotonin, 5-hydroxyindolacetic acid and neuropeptide Y levels in severe major depressive disorder. Brain Res. 1095 (1), 154–158. doi:10.1016/j.brainres.2006.04.026
Jesulola, E., Micalos, P., and Baguley, I. J. (2018). Understanding the pathophysiology of depression: From monoamines to the neurogenesis hypothesis model - are we there yet? Behav. Brain Res. 341, 79–90. doi:10.1016/j.bbr.2017.12.025
Kandola, A., Ashdown-Franks, G., Hendrikse, J., Sabiston, C. M., and Stubbs, B. (2019). Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 107, 525–539. doi:10.1016/j.neubiorev.2019.09.040
Katz, R. J. (1982). Animal model of depression: Pharmacological sensitivity of a hedonic deficit. Pharmacol. Biochem. Behav. 16 (6), 965–968. doi:10.1016/0091-3057(82)90053-3
Lee, G. S., Simpson, C., Sun, B.-H., Yao, C., Foer, D., Sullivan, B., et al. (2014). Measurement of plasma, serum, and platelet serotonin in individuals with high bone mass and mutations in LRP5. J. Bone Mineral Res. Official J. Am. Soc. Bone Mineral Res. 29 (4), 976–981. doi:10.1002/jbmr.2086
Li, H., Wang, P., Huang, L., Li, P., and Zhang, D. (2019). Effects of regulating gut microbiota on the serotonin metabolism in the chronic unpredictable mild stress rat model. Neurogastroenterol. Motil. 31 (10), e13677. doi:10.1111/nmo.13677
Li, X., Fan, Y., Xiao, S., Peng, S., Dong, X., Zheng, X., et al. (2015). Decreased platelet 5-hydroxytryptamin (5-HT) levels: A response to antidepressants. J. Affect. Disord. 187, 84–90. doi:10.1016/j.jad.2015.08.025
Li, Y., Sun, Y., Ma, X., Xue, X., Zhang, W., Wu, Z., et al. (2013). Effects of Sini San used alone and in combination with fluoxetine on central and peripheral 5-HT levels in a rat model of depression. J. Tradit. Chin. Med. 33 (5), 674–681. doi:10.1016/s0254-6272(14)60041-8
Liu, M., Wei, W., Stone, C. R., Zhang, L., Tian, G., and Ding, J. N. (2018a). Beneficial effects of trimetazidine on expression of serotonin and serotonin transporter in rats with myocardial infarction and depression. Neuropsychiatr. Dis. Treat. 14, 787–797. doi:10.2147/NDT.S157441
Liu, P., Li, P., Li, Q., Yan, H., Shi, X., Liu, C., et al. (2021). Effect of pretreatment of S-ketamine on postoperative depression for breast cancer patients. J. Investigative Surg. Official J. Acad. Surg. Res. 34 (8), 883–888. doi:10.1080/08941939.2019.1710626
Liu, Y., Feng, H., Mao, H., Mo, Y., Yin, Y., Liu, W., et al. (2015). Impact on serum 5-HT and TH1/TH2 in patients of depressive disorder at acute stage treated with acupuncture and Western medication. Zhongguo Zhen Jiu = Chin. Acupunct. Moxibustion 35 (6), 539–543.
Mann, J. J., McBride, P. A., Anderson, G. M., and Mieczkowski, T. A. (1992). Platelet and whole blood serotonin content in depressed inpatients: Correlations with acute and life-time psychopathology. Biol. Psychiatry 32 (3), 243–257. doi:10.1016/0006-3223(92)90106-a
Maund, E., Dewar-Haggart, R., Williams, S., Bowers, H., Geraghty, A. W. A., Leydon, G., et al. (2019). Barriers and facilitators to discontinuing antidepressant use: A systematic review and thematic synthesis. J. Affect. Disord. 245, 38–62. doi:10.1016/j.jad.2018.10.107
Monleon, S., D'Aquila, P., Parra, A., Simon, V. M., Brain, P. F., and Willner, P. (1995). Attenuation of sucrose consumption in mice by chronic mild stress and its restoration by imipramine. Psychopharmacology 117 (4), 453–457. doi:10.1007/BF02246218
Mück-Seler, D., Pivac, N., Sagud, M., Jakovljević, M., and Mihaljević-Peles, A. (2002). The effects of paroxetine and tianeptine on peripheral biochemical markers in major depression. Prog. Neuro-psychopharmacology Biol. Psychiatry 26 (7-8), 1235–1243. doi:10.1016/s0278-5846(02)00259-2
Obeid, S., Abi Elias Hallit, C., Haddad, C., Hany, Z., and Hallit, S. (2018). Validation of the Hamilton Depression Rating Scale (HDRS) and sociodemographic factors associated with Lebanese depressed patients. L'Encephale 44 (5), 397–402. doi:10.1016/j.encep.2017.10.010
Oh, N. S., Joung, J. Y., Lee, J. Y., Song, J. G., Oh, S., Kim, Y., et al. (2020). Glycated milk protein fermented with Lactobacillus rhamnosus ameliorates the cognitive health of mice under mild-stress condition. Gut Microbes 11 (6), 1643–1661. doi:10.1080/19490976.2020.1756690
Paketci, S. (2021). Interpretation of the montgomery-åsberg depression rating scale (MADRS). Br. J. Psychiatry J. Ment. Sci. 219 (5), 620–621. doi:10.1192/bjp.2021.162
Papp, M., Willner, P., and Muscat, R. (1991). An animal model of anhedonia: Attenuation of sucrose consumption and place preference conditioning by chronic unpredictable mild stress. Psychopharmacology 104 (2), 255–259. doi:10.1007/BF02244188
Pfeffer, C. R., McBride, P. A., Anderson, G. M., Kakuma, T., Fensterheim, L., and Khait, V. (1998). Peripheral serotonin measures in prepubertal psychiatric inpatients and normal children: Associations with suicidal behavior and its risk factors. Biol. Psychiatry 44 (7), 568–577. doi:10.1016/s0006-3223(98)00020-1
Pivac, N., Mück-Seler, D., Sagud, M., Jakovljević, M., Mustapić, M., and Mihaljević-Peles, A. (2003). Long-term sertraline treatment and peripheral biochemical markers in female depressed patients. Prog. Neuro-psychopharmacology Biol. Psychiatry 27 (5), 759–765. doi:10.1016/S0278-5846(03)00105-2
Read, J. R., Sharpe, L., Modini, M., and Dear, B. F. (2017). Multimorbidity and depression: A systematic review and meta-analysis. J. Affect. Disord. 221, 36–46. doi:10.1016/j.jad.2017.06.009
Schins, A., Hamulyák, K., Scharpé, S., Lousberg, R., Van Melle, J., Crijns, H., et al. (2004). Whole blood serotonin and platelet activation in depressed post-myocardial infarction patients. Life Sci. 76 (6), 637–650. doi:10.1016/j.lfs.2004.04.060
Tyano, S., Zalsman, G., Ofek, H., Blum, I., Apter, A., Wolovik, L., et al. (2006). Plasma serotonin levels and suicidal behavior in adolescents. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 16 (1), 49–57. doi:10.1016/j.euroneuro.2005.05.005
van Buel, E. M., Meddens, M. J. M., Arnoldussen, E. A., van den Heuvel, E. R., Bohlmeijer, W. C., den Boer, J. A., et al. (2019). Major depressive disorder is associated with changes in a cluster of serum and urine biomarkers. J. Psychosomatic Res. 125, 109796. doi:10.1016/j.jpsychores.2019.109796
Wang, J., Wang, Y., Xu, X., Peng, S., Xu, F., and Liu, P. (2020a). Use of various doses of S-ketamine in treatment of depression and pain in cervical carcinoma patients with mild/moderate depression after laparoscopic total hysterectomy. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 26, e922028. doi:10.12659/MSM.922028
Willner, P., Muscat, R., and Papp, M. (1992). Chronic mild stress-induced anhedonia: A realistic animal model of depression. Neurosci. Biobehav. Rev. 16 (4), 525–534. doi:10.1016/s0149-7634(05)80194-0
Wu, G. F., Ren, S., Tang, R. Y., Xu, C., Zhou, J. Q., Lin, S. M., et al. (2017). Antidepressant effect of taurine in chronic unpredictable mild stress-induced depressive rats. Sci. Rep. 7 (1), 4989. doi:10.1038/s41598-017-05051-3
Wulsin, L. R., Musselman, D., Otte, C., Bruce, E., Ali, S., and Whooley, M. A. (2009). Depression and whole blood serotonin in patients with coronary heart disease from the Heart and Soul Study. Psychosom. Med. 71 (3), 260–265. doi:10.1097/PSY.0b013e31819cc761
Yang, Z., Li, Z., Guo, Z., Ren, Y., Zhou, T., Xiao, Z., et al. (2021). Antitumor effect of fluoxetine on chronic stress-promoted lung cancer growth via suppressing kynurenine pathway and enhancing cellular immunity. Front. Pharmacol. 12, 685898. doi:10.3389/fphar.2021.685898
Yohn, C. N., Gergues, M. M., and Samuels, B. A. (2017). The role of 5-HT receptors in depression. Mol. Brain 10 (1), 28. doi:10.1186/s13041-017-0306-y
Zhang, Z.-J., Wang, D., Man, S. C., Ng, R., McAlonan, G. M., Wong, H. K., et al. (2014). Platelet 5-HT(1A) receptor correlates with major depressive disorder in drug-free patients. Prog. Neuro-psychopharmacology Biol. Psychiatry 53, 74–79. doi:10.1016/j.pnpbp.2014.03.004
Zhang, Z., Shao, S., Zhang, Y., Jia, R., Hu, X., Liu, H., et al. (2020). Xiaoyaosan slows cancer progression and ameliorates gut dysbiosis in mice with chronic restraint stress and colorectal cancer xenografts. Biomed. Pharmacother. 132, 110916. doi:10.1016/j.biopha.2020.110916
Zhao, Y., Wang, Q., Jia, M., Fu, S., Pan, J., Chu, C., et al. (2019). (+)-Sesamin attenuates chronic unpredictable mild stress-induced depressive-like behaviors and memory deficits via suppression of neuroinflammation. J. Nutr. Biochem. 64, 61–71. doi:10.1016/j.jnutbio.2018.10.006
Zhou, X., Li, Y., Zhou, Z., and Pan, S. (2015). Clinical observasion of acupuncture in patients with depression and its impact on serum 5-HT. Zhongguo Zhen Jiu = Chin. Acupunct. Moxibustion 35 (2), 123–126.
Zhuang, X., Xu, H., Fang, Z., Xu, C., Xue, C., and Hong, X. (2018). Platelet serotonin and serotonin transporter as peripheral surrogates in depression and anxiety patients. Eur. J. Pharmacol. 834, 213–220. doi:10.1016/j.ejphar.2018.07.033
Keywords: 5-HT, peripheral, depression, biomarker, plasma, platelet
Citation: Li C, Cai Q, Su Z, Chen Z, Cao J and Xu F (2023) Could peripheral 5-HT level be used as a biomarker for depression diagnosis and treatment? A narrative minireview. Front. Pharmacol. 14:1149511. doi: 10.3389/fphar.2023.1149511
Received: 22 January 2023; Accepted: 24 February 2023;
Published: 07 March 2023.
Edited by:
Kyoko Koshibu, DSM Nutrition Products Ltd., SwitzerlandReviewed by:
Paul Willner, Swansea University, United KingdomCopyright © 2023 Li, Cai, Su, Chen, Cao and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Xu, eHVmQHNtdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.