
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol. , 02 June 2023
Sec. Obstetric and Pediatric Pharmacology
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1138968
This article is part of the Research Topic Safety of Drugs and CAM Products in Pregnancy and Breastfeeding: Evidence From Clinical Toxicology View all 9 articles
Background: Despite some progress has been made in the pathogenesis and treatment of threatened miscarriage (TM), conventional treatment remains suboptimal. Thus, complementary medicine gradually become a new treatment option for treating threatened miscarriage. Gushen Antai Pills (GAP), a classic prescription of Traditional Chinese medicine (TCM), has became a popular complementary therapy to conventional western medicine (dydrogesterone) in treating threatened miscarriage in recent years. However, a systematic summary and analysis for its therapeutic effects is lacking. This meta-analysis aimed to systematically evaluate the effectiveness and safety of Gushen Antai Pills combined with dydrogesterone in the treatment of threatened miscarriage.
Methods: A systematic search across seven electronic databases was conducted from inception to 17 September 2022. Studies were included if they were randomized controlled trials (RCTs) evaluating the effect of integrating Gushen Antai Pills and dydrogesterone in patients with threatened miscarriage, and reported the outcomes of interest. All statistical analyses were conducted using the Revman5.3 and Stata 13 software. The GRADE system was used to evaluate the quality of evidence.
Results: Ten eligible randomized controlled trials involving 950 participants were contained in this meta-analysis. The pooled analysis showed that Gushen Antai Pills combined with dydrogesterone can significantly reduce the incidence of early pregnancy loss (RR: 0.29; 95% CI: 0.19–0.42; p < 0.00001) and alleviate clinical symptoms (RR: 1.39; 95% CI: 1.22–1.59; p < 0.00001), compared with treatment of dydrogesterone alone. Also, meta-analysis indicated that integrating Gushen Antai Pills and dydrogesterone is more effective than using dydrogesterone alone in improving hormone levels (serum levels of progesterone, β-HCG and estradiol) for women with threatened miscarriage (all p < 0.00001). Meanwhile, the combined effects with significant heterogeneity also showed favorable consistency in the sensitivity analyses, indicating a good stability of present results. Moreover, no significant differences between Gushen Antai Pills combined with dydrogesterone and control group on adverse events was identified. The overall GRADE qualities were low to moderate.
Conclusion: The overall available evidence suggested that Gushen Antai Pills combined with dydrogesterone had significant effects in improving pregnancy success rate, clinical symptoms and hormone levels for women with threatened miscarriage, with considerable safety and reliability. However, due to the partial heterogeneity, suboptimal quality and high risk of bias of some included studies, further rigorously designed randomized controlled trials are required.
Systematic Review Registration: identifier https://INPLASY2022120035, https://inplasy.com/inplasy-2022-12-0035/.
Threatened miscarriage (TM) is a common complication of all pregnancies worldwide, occurring in approximately 20% in the first half of pregnancy (Lee et al., 2017). Unfortunately, owing to the complex pathogenesis and unsatisfied treatment in TM, nearly half of TM patients may progress to inevitable or incomplete miscarriage (Everett, 1997; Weiss et al., 2004). The miscarriage could bring physical and mental harms to the most of sufferers and their families, as well as a medical expense burden on patients’ families and society (Yang et al., 2013). Hence, identifying a prompt and effective treatment for TM is of significantly clinical and social importance (Sotiriadis et al., 2004).
Current evidence supposed that lacking progesterone due to the endocrine dysfunction is the most common factor (Ku et al., 2018; Dang et al., 2022). Progesterone is vital to maintain normal pregnancy in the first trimester, which enhances endogenous progesterone and chorionic gonadotropin secretion, as well as placental trophoblast activity (Chen et al., 2022). In this context, hormonal supplementation with progesterone was commonly used as the conventional western medicine for TM treatment, especially oral dydrogesterone (Coomarasamy et al., 2020). Dydrogesterone, pharmacologically comparable to endogenous progesterone, has highly selective progesterone action and good oral bioavailability and can be used at lower oral doses to exert curative effects (Omar et al., 2005). More importantly, dydrogesterone does not have an androgenic effect on fetuses and don't hinder progesterone synthesis in the placenta (Carp, 2015). With the wide use of dydrogesterone in treating TM, a number of studies had shown promising outcome that dydrogesterone can partially lower the incidence of subsequent miscarriage (Carp, 2012). However, dydrogesterone remedy also accompanied with some side effects such as nausea, headache, and sleepiness. Besides, solitary treatment with dydrogesterone rarely relieved all the symptoms of TM and yielded a limited therapeutic effect in some TM patients, especially those with multiple or complex causes (Lou et al., 2021). Presently, the clinical effect of dydrogesterone alone for treating TM remains suboptimal due to the considerable individual heterogeneity and poor prognosis of TM (Zhou et al., 2021). Thus, it is extremely essential to seek for more effective treatment options to treat TM. Recently, complementary and alternative medicine gradually becomes a new treatment option for treating TM. Especially, Traditional Chinese medicine (TCM) has became a popular complement to dydrogesterone in maintaining successful pregnancy preservation and the prevention of miscarriage in recent years (Chen et al., 2022).
According to the theory of TCM, the pathogenesis of TM included deficient kidney essence, deficiency of spleen-Qi, and liver depression (Ye et al., 2021; Zeng et al., 2021). Gushen Antai Pills (GAP), based on the treatment principles of tonifying kidney, invigorating spleen, and regulating liver, has been clinically applied for decades to treat TM (Ma et al., 2021). GAP included ten kinds of Chinese herbal medicines (Dipsaci, Cuscutae Semen, Herba Taxilli, Polygonum Multiflori, Rehmannia Glutinosa, Cistanche Deserticola, Atractylodes, Scutellariae, Paeoniae, and Uncaria), and each of its ingredients had respective therapeutical effects (Ma et al., 2021). Among the herbal formula, Dipsaci, Cuscutae Semen, and Herba Taxilli are the monarch drug, which play the role of tonifying the kidney, replenishing essence, nourishing blood, and consolidating Chong Vessel (Ye et al., 2021). On this basis, Rehmannia Glutinosa, Cistanche Deserticola, and Polygonum Multiflori were appended to boost the effects of strengthening kidney, invigorating spleen and liver, and nourishing blood (Ding et al., 2018; Ma et al., 2021; Chen et al., 2022). Meanwhile, Atractylodes, Uncaria, and Scutellariae are functional at Qi-invigorating, heat-clearing, harmonizing Qi, soothing liver, and detoxifying (Yang et al., 2021; Y. Xu, 2021, S.P. Ge, 2020). In brief, all the herbal components will be mutually reinforcing, achieving a more harmonious effect of tranquilizing the fetus to prevent miscarriage. Meanwhile, emerging clinical studies showed that applying dydrogesterone combined with GAP has a beneficial effect in the treatment of TM. However, a comprehensive and systematic assessment of this issue is lacking. Hence, this systematic review was conducted to comprehensively evaluate the efficacy and safety of integrating GAP and dydrogesterone for treating TM through summarizing available evidence, aiming to emphasize the therapeutic potential and feasibility of GAP in conjunction with dydrogesterone and highlight its safety and implications for practice in treating TM. Moreover, this topic will provide better evidence to guide the rational therapy in clinical practice and develop the new guidelines, further promoting the clinical treatment and understanding for TM.
This meta-analysis was performed according to the criteria of the PRISMA statement and the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2011; Moher et al., 2015). This protocol has been registered in the INPLASY (https://inplasy.com/), with the registered number INPLASY2022120035.
A systematic search was conducted to identify relevant studies, which included seven databases of China National Knowledge Infrastructure (CNKI), the Chinese BioMedical database (CBM), Chinese Scientific Journal Database, PubMed, Cochrane Library, Embase, and the Wanfang database. The retrieval deadline was 17 September 2022. We applied a combination of free-text and medical subject heading (MeSH) terms to search (“Gushen Antai” AND “dydrogesterone” OR “duphaston” AND “threatened abortion” OR “threatened miscarriage”). Search strategy taking PubMed as an example were as follows: [threatened miscarriage OR threatened miscarriage (MeSH) OR threatened abortion (Title/Abstract) OR threatened miscarriage (Title/Abstract)] AND [dydrogesterone OR dydrogesterone (MeSH) OR dydrogesterone (Title/Abstract) OR duphaston (Title/Abstract)] AND [Gushen Antai OR Gushen Antai (MeSH) OR Gushen Antai (Title/Abstract)]. Furthermore, we also manually checked the references from the retrieved articles to seek the potential studies.
Two investigators (KC and XL) selected the studies and extract data from selected studies independently. Disagreements were resolved by group consensus. For literature with insufficient data, we will attempt to contact the corresponding author to obtain raw data. Firstly, the literatures retrieved from the initial searching was imported in the Endnote software and removed the duplication. Secondly, literature titles and abstracts were reviewed for further screening subsequently. Thirdly, full texts were screened in accordance with the inclusion and exclusion criteria. Inclusion criteria: 1) Participants: Pregnant women diagnosed with TM in the first trimester, regardless of underlying causes; 2) Intervention: Treatment with GAP combined with dydrogesterone; 3) Controls: Treated with dydrogesterone or progesterone alone; 4) Outcomes: The incidence of early pregnancy loss was the primary outcome. Secondary outcomes involved serum β-human chorionic gonadotropin (β-HCG), progesterone, and estradiol (E2) levels, as well as the rate of alleviation of clinical symptoms and adverse events (AEs); 5) Design: All randomized controlled trials (RCTs) were included. Exclusion criteria were listed as follows: I) Repetitive studies; II) Non-RCTs studies, retrospective studies, conferences, and reviews; III) Studies lacked the outcomes of interest or the valid data. The basic information were extracted from the included trails: study design, first author, published year, sample sizes of treatment and intervention groups, drug intervention strategy, treatment of control group, duration of treatment, main outcomes, and the modified Jadad score.
Two investigators (KC and XL) independently assessed the risk of bias of the included RCTs using the risk of bias tool of the Cochrane Handbook (Higgins et al., 2011). The next characteristics were evaluated: random (selection bias), allocation concealment, blinding (performance bias), incomplete outcome (attrition bias), reporting bias, and other possible biases. The modified Jadad score was also applied to assess the quality of all RCTs, ranging from 0 to 7 points. The 0 to 3 points stood for a low quality, while the RCTs with 4–7 points are named as a high quality (Jadad et al., 1996).
RevMan 5.3 (Nordic Cochrane Centre) and Stata 13.0 (Stata Corp LP) softwares were used for statistical analyses. Dichotomous data were expressed as relative risk (RR) with 95% confidence interval (CI) and continuous data were presented as Standardized mean differences (SMD) or mean differences (MD) with 95% CI. Descriptive approach would be used if the data were insufficient. Chi-squared test and the I2 statistic were used to assess the heterogeneity (I2 > 50% for a significant heterogeneity) (Higgins et al., 2003). Meta-analyses were conducted using fixed-effect or random-effect model (if I2 > 50%) where appropriate. If obvious heterogeneities were observed, sensitivity or subgroup analysis would be used to investigate potential sources of heterogeneity through sequentially omitting trials. Funnel plot and the Begg´s regression test were performed to check the publication bias. The trial sequential analysis (TSA) was used to decide whether sample sizes were adequate to evaluate outcomes of this meta-analysis (Gu et al., 2022). Two-sided p < 0.05 was deemed statistically significant.
Two independent reviewers (K. C and XX. L) assessed the quality of the evidence for each outcome using the GRADE approach (Guyatt et al., 2008). Divergences were discussed with and solved by the third reviewer. The evidence grade was classified as very low, low, moderate, or high based on the characteristics of study limitations, inconsistency, indirectness, imprecision, and reporting bias.
Initially, a total of 71 relevant studies were retrieved from the systemic search. 38 records were excluded for duplicates, then 33 records were filtered by screening the titles and abstracts. 20 records were eliminated for specific reasons according to the inclusion and exclusion criteria. Subsequently, the remaining 13 trails were assessed for eligibility, and 3 were further removed for inappropriate intervention, participants or data. Finally, 10 RCTs were included in this meta-analysis (X.Y. Zhang, 2020; Y. Gu, 2019; Huang and Xu, 2020; Y. Yang, 2020; S.P. Ge, 2020; Zhang and Qian, 2016; L.Y. Zhang et al., 2014; L.P. Li et al., 2018; Y. Xu, 2021; Y.Y. Lu et al., 2017). The selection process was summarized in Figure 1.
The basic characteristics were shown in Table 1. All studies were published from 2014 to 2021 and came from China. Totally, this meta-analysis involved 950 participants, of which 495 participants were designated to the experimental group while 495 patients were assigned to the control group. Patients in the experimental group were treated with GAP in combination with dydrogesterone. The control group adopted the therapy of western medicine alone, among which nine trails used dydrogesterone and one with intramuscular injection of progesterone. Treatment durations were all 2 weeks. According to the assessment of the modified Jadad score, six RCTs were defined as low quality, while four RCTs were named as high quality.
Assessment of risk biases were displayed in Figure 2. In general, the overall methodological qualities of the included RCTs were poor to moderate. In terms of random sequence generation, four RCTs reported proper random methods and were designated as low risk; five trials supplied unclear randomization procedure, assessed as unclear risk; one trial did not mention the randomization, identified as a high risk. In terms of the allocation concealment and blinding assessment, all RCTs did not mention it clearly and were ranked as unclear risk. With respect to the incomplete outcome data, all included RCTs didn’t report the bias of selective reporting, thus assessing as low risk.
All of included RCTs stated the rate of early pregnancy loss. A fixed-effect model was adopted owing to the low heterogeneity between studies (I2 = 0%). Pooled analysis indicated that the GAP combined with dydrogesterone group had a significantly lower rate of early pregnancy loss when comparing with the dydrogesterone treatment alone (RR: 0.29; 95% CI: 0.19–0.42; p < 0.00001) (Figure 3).
Eight studies comprising 762 patients compared the changes of serum β-HCG levels. There was obvious heterogeneity among these studies (I2 = 98%). The pooled result using a random effects model revealed that serum β-HCG levels in the experimental group were significantly higher after adjuvant treatment (SMD = 4.06; 95% CI: 2.54–5.58, p < 0.00001) (Figure 4A). The sensitivity analysis demonstrated a stable result with pooling outcomes ranging from SMD2.63 (95% CI: 1.38–3.88; I2 = 97%) to SMD4.67 (95% CI:2.87–6.48; I2 = 98%) (Figure 4B).
The serum progesterone levels were highlighted in 8 studies involving 762 patients. Random-effect model was applied owing to the significant heterogeneity (I2 = 93%). The pooling result revealed that the serum progesterone levels in the combined treatment group were significantly higher after treatment (SMD = 1.89; 95% CI: 1.24–2.55, p < 0.00001) (Figure 5A). The sensitivity analysis suggested that single study could not obviously affect the pooled results, ranging from SMD1.77 (95% CI:1.10–2.44; I2 = 93%) to SMD2.08 (95% CI:1.42–2.73; I2 = 91%) (Figure 5B).
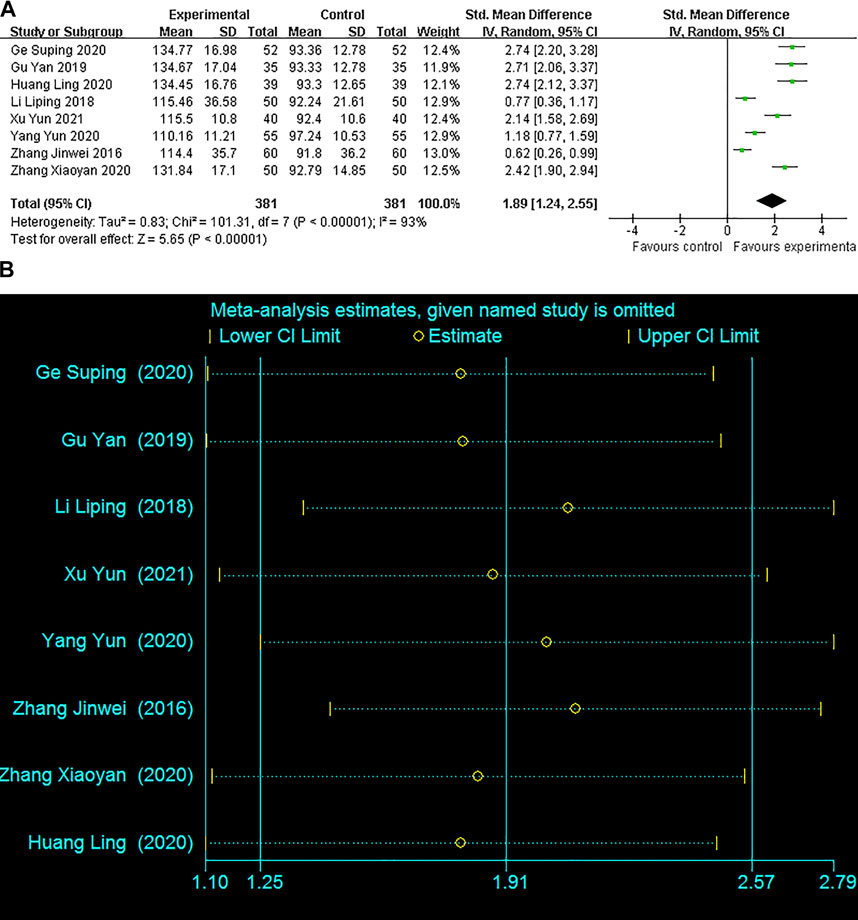
FIGURE 5. Forest plots with: (A) Serum progesterone levels; (B)Sensitivity analysis for the progesterone levels.
Only two studies reported serum E2 levels. The fixed-effect model was adopted to analyze based on the low heterogeneity (I2 = 0%). The pooled outcome indicated comparing with the control group, E2 has a significant improvement in the experimental group (MD = 222.60, 95% CI 203.03–242.16, p < 0.00001) as shown in Figure 6.
Eight studies assessed the alleviation of clinical symptoms. The pooled result showed that combined medicines treatment was more effective in alleviating clinical symptoms than dydrogesterone treatment alone (RR: 1.39; 95% CI: 1.22–1.59; p < 0.00001), with low heterogeneity (I2 = 13%). (Figure 7).
Of the ten included studies, only three studies reported minor AEs in the treatment group, including one case of urticaria, two cases of nausea, and two cases of vomiting. However, the remaining seven studies lacked the information of AEs. Furthermore, based on the available data, the pooled analysis showed that AEs had no significant difference between 2 groups (RR = 1.0, 95% CI: 0.30–3.37, p = 1.00), without heterogeneity (I2 = 0%) (Figure 8).
Publication bias was expressed based on the data of the primary outcome. Although the funnel plot was asymmetrically distributed, the result of Begg’s test (p = 0.107) indicated no significant publication bias (Figure 9). All of sensitivity analysis results (including the evaluation of serum β-HCG and progesterone levels) remained stable, supporting the robustness of the pooled outcomes.
We used TSA to estimate the required sample size (greater than 117) for meta-analysis cumulative data, supporting the present sample size was adequately powered to evaluate outcomes. Briefly, the overall quality was moderate for the early pregnancy loss rate and alleviation rate of clinical symptoms; low for serum progesterone, β-HCG, E2 levels, and adverse events. The GRADE evaluations were displayed in Table 2.
Currently, although great progress has been achieved in the understanding and treatment of TM, no definitely effective treatment is available for clinical management of TM. Growing studies have found that the therapeutic strategy of dydrogesterone combined with GAP has a potentially beneficial effect in treating TM. Herein, our study systematically integrated the existing RCTs and evaluated the efficacy and safety of GAP in conjunction with dydrogesterone in the treatment of TM, providing an evidence-based framework for further clinical application and research. Pooled results indicated that GAP combined with dydrogesterone can significantly decrease the rate of early pregnancy loss in pregnant women experiencing TM without increasing the incidence of AEs. Also, combined treatment was more efficient than dydrogesterone alone in relieving the clinical symptoms of TM, mainly including vaginal bleeding and abdominal pain. Furthermore, our meta-analysis showed that integrated GAP and dydrogesterone treatment was superior to dydrogesterone alone in improving serum progesterone, β-HCG and E2 levels.
TCM has unique treatment theories and practical experiences gradually formed in long-term medical practice, made indelible contributions in maintaining maternal and child health. Based on the TCM theory, TM belonged to the categories of fetal leakage with pathogenesis being commonly dominated by the kidney-Qi deficiency (Zeng et al., 2021). Moreover, other pathogenesis were also involved in the development of TM, including insufficiency of spleen-Qi, liver depression, and blood deficiency. Therefore, the rational treatment was focused on tonifying kidney, enhancing spleen, nourishing blood, as well as soothing liver (Li HF. et al., 2020a). GAP formula, adapted from the Shennong’s classic of materia medica and innovated by modern pharmaceutical technology, has a history-proven therapeutic efficacy (L.Y.Zhang et al., 2014). Among the herbal formula of GAP, Dipsaci, Cuscutae Semen and Herba Taxilli played the role of tonifying the kidney, nourishing blood, replenishing essence, and consolidating Chong Vessel (Ye et al., 2021). Moreover, Rehmannia Glutinosa, Cistanche Deserticola, and Polygonum Multiflori reinforced the effects of strengthening kidney, invigorating spleen and liver, and nourishing blood (Ding et al., 2018; Ma et al., 2021; Chen et al., 2022). In addition, Atractylodes, Uncaria, and Scutellariae would be beneficial to the Qi-invigorating and harmonizing, heat-clearing, soothing liver, and detoxifying (Yang et al., 2021, Y; Xu, 2021, S.P; Ge, 2020). Briefly, the herbal components of GAP can be mutually strengthened, yielding a more harmonious effect of tranquilizing the fetus to prevent miscarriage.
Evidence clarifying the effectiveness of GAP for TM can be identified in modern pharmacological studies. Holistically, pharmacological researches indicated that GAP benefited TM potentially through multiple mechanisms including enhance vascular function, improve immune activity, and regulate ovarian endocrine function, etc (Wang et al., 2021; Chen et al., 2022). In addition, modern pharmacological researches have pointed that baicalein, flavanone, norwogonin, rhynchophylline, polysaccharides, methoxyflavone, acacetin, anthraquinone glycosides and triterpenoid saponins are the main active components in GAP, which can improve blood circulation and placental blood supply, regulate disordered cellular immunity and humoral immunity, and improve endocrine dysfunction (Cao et al., 2020; Dang et al., 2022). For instance, baicalein and norwogonin can ameliorate the uterine blood circulation to nourish the embryo and strengthen the immunomodulation and inhibit allergic reactions to protect the fetus (Liao et al., 2021; Wu et al., 2022). Moreover, flavanone, acacetin, and methoxyflavone can suppress the formation of TNF-α through mitogen-activated protein kinase (MAPK) signaling pathway to attain the bactericidal and anti-inflammatory effects, maintaining the stabilization of intrauterine environment and reducing the miscarriage (Chang et al., 2017; Singh et al., 2021; Dang et al., 2022). Meanwhile, dydrogesterone also influence the cytokine balance and inhibit the immune activity at the fetal-maternal interface. As a result, GAP in conjunction with dydrogesterone can reinforce each other and reduce the occurrence of miscarriage (Y.Yang, 2020).
Recently, some pharmacological studies targeting the mechanisms of single herb or herb pair also provided indirect evidence for the anti-abortive effects of GAP. Wu HW found that Cuscutae Semen may prevent miscarriage by inhibiting the MAPK signaling pathway (Wu et al., 2018). Evidences have shown that during the implantation of embryo, the MAPK signal pathway will be activated and improve the invasion and proliferation of trophoblast cells and decidual stromal cells (DSCs), which play the key role in the maintenance of normal pregnancy (Paliga et al., 2005; Yang et al., 2020). Besides, it was believed that the Th1/Th2 imbalance and natural killer (NK) cell-regulated immunity significantly affect the development of miscarriage. More specifically, excessive expression of Th1 cytokines [interleukin-2 (IL-2), interferon-γ (IFN-γ), and tumor necrosis factor-α (TNF-α)] would lead to pregnancy failure, while low expression of Th2 cytokines (IL-4, IL-5, IL-6, IL-10, and IL-13) indicated a weak immunoprotective effect to maintain normal pregnancy (Calleja-Agius et al., 2011; Dong et al., 2017). Moreover, Zhong XH speculated that Scutellariae and Atractylodescan inhibited the maternal-fetal interface immunity and reduced the early embryo loss, which may be associated with its ability to the infiltration of NK cells and the production of IL-2, and upregulate the IL-10 in the uterus (Zhong et al., 2002; Zhong et al., 2008). Similarly, Ma AT showed that Scutellariae can play an anti-abortive effect by reducing the IFN-γ and increasing the progesterone (Ma et al., 2009).
Progress on network pharmacology provided some valuable clues about the molecular mechanisms of the holy herb pair Cuscutae Semen- Herba Taxilli (the main ingredients of GAP) in treating TM, which identified three key pathways directly related to TM, including MAPK, phosphatidylinositol-3-kinase/protein kinase B (PI3K-AKT), and transforming growth factor-β (TGF-β) (Yang et al., 2020). Identically, both PI3K-AKT and TGF-β signaling pathways participates in the proliferation, migration and apoptosis of trophoblast cells that are vital for establishing and persisting normal pregnancy (Latifi et al., 2019). Additionally, the TGF-β signal pathway is also involved in immune and inflammatory responses to promote immune tolerance of the maternal-fetal interface, maintaining the fetus in a stable state (Liu et al., 2017; Yang et al., 2020).
Network pharmacological analysis further found some valuable genes and signaling pathway of GAP for treating TM, including AKT 1, vascular endothelial growth factor A (VEGFA), Signal transducer and activator of transcription 3 (STAT3), and hypoxia-inducible factor 1(HIF-1) signaling pathway (Dang et al., 2022). AKT1, a heterodimer of AKT, mediates many PI3K-regulated downstream pathways (Gillani et al., 2021). Also, PI3K-AKT pathway can promote the growth of trophoblast cells and regulate the function of chorionic trophoblast cells, thus exerting a prominent effect on the embryonic development and pregnancy maintenance (Zhu et al., 2013). VEGFA, an important member of the VEGF family, can positively increase the vascular permeability and promote the formation of endometrial microvasculature and placenta through the upregulated expression AKT signaling pathway, thereby promoting embryonic growth and development (Amirchaghmaghi et al., 2015; Li Y. et al., 2020b).
As the research developed, it was shown that inhibiting STAT3 pathway expression will decrease the Cyclin D1 expression (Tang et al., 2018). Relevant studies have also confirmed that the downregulation of Cyclin D1 can decreased the number of trophoblast cells and increased the cell apoptosis, thus affecting the proliferation and differentiation of endometrial and trophoblast cells in first-trimester pregnancy (Cai et al., 2016). In addition, the inhibition of STAT3 also influences the VEGF expression and Th17 cells differentiation, and decrease the levels of related Th1/Th2 cytokines, resulting in immune imbalance and reduced angiogenesis, which affects the stability of the intrauterine immune environment and embryonic development (Lee et al., 2016). HIF-1 was also involved in the early miscarriage, which affect the receptivity of endometrium to the embryo. The overexpression of HIF-1 protein will cause endometrium to be infiltrated by inflammatory cells, thereby making the trophoblast cells difficult to invade the uterine spiral artery and reducing the placental blood perfusion, which lead to the placental angiogenesis deficiency and embryonic ischemia and hypoxia (Zhi et al., 2018; Colson et al., 2020; Zhao et al., 2021). Meaningfully, the Scutellariae-Atractylodes herb pair of GAP can rationally regulate the aforementioned target genes and signaling pathway to maintain stable pregnancy and prevent miscarriage (Dang et al., 2022). Although several mechanisms have been proposed, the precise mechanism of complementary GAP-treated TM has not fully elucidated owing to the multi-components and multi-effects of GAP. More researches involving in vitro and in vivo are needed to uncover the detailed mechanism.
The present results also documented that GAP combined with dydrogesterone can effectively improve endocrine levels of serum P, E2, and β-HCG. Remarkably, it’s well known that sex hormones of P, E2, and β-HCG play a crucial role in maintaining the maternal-fetal response and stability of the internal environment (Cha et al., 2012). Patients with TM usually had lower levels of serum P, β-HCG, and E2, which increased the risk of early pregnancy loss and miscarriage (Osmanağaoğlu et al., 2010). Therefore, improving serum hormone levels highly associated with the progression of TM is of great significance. As expected, modern pharmacological studies provided evidence that GAP can improve the sex hormones through a multiple-target pathway and holistic effect, especially the estrogen-like effect (Cao et al., 2020). Likewise, pharmacological studies have reported that Dipsaci and Cuscutae Semen could regulate the immune balance of maternal-fetal interface and the expression of Th2 cytokines to stabilize pregnancy, which also attributed to its estrogen-like activities (Yang et al., 2021). In addition, mounting studies had shown that Cuscutae Semen and some active compounds in the GAP could improve the secretion of β-HCG, which promote the generation of progesterone and secretion of estrogen, and inhibit the production of oxytocin to decrease the intensity of uterine contractions (Ma et al., 2021; Maharajan et al., 2021; Ye et al., 2021; Chen et al., 2022). Generally, dydrogesterone itself can replenish the inadequate endogenous progesterone (Carp, 2012). Furthermore, the application of GAP collaborate with dydrogesterone tend to yield a more harmonious and enhanced effect on regulating the relevant sex hormone levels (Y.Gu, 2019). Additionally, the present study also showed that GAP combined with dydrogesterone is more effective in reliving the clinical symptoms of pain and bleeding of TM patients, whose mechanisms are possibly related to exert estrogen-like effects, adjust the body’s immunity and endocrine disorders, and improve the intrauterine environment (Zhang and Qian, 2016; Zhang, 2020). However, improving the curative outcome of TM is a long-term and complex process and need systematic pharmacological examinations to fully verify.
Meanwhile, the safety assessment is also a concern in the clinical application of TCM. Based on the available data, our study showed that there were no obvious AEs with the combined treatment, indicating that GAP in conjunction with dydrogesterone may be safe and well-tolerated. In particular, GAP was processed through international quality control of natural medicinal herbs and permitted by the Chinese State Food and Drug Administration, which make it to be more rationalizing and standardizing (Ma et al., 2021). Although GAP has the characteristics of multiple herbs, optimized compatibility will decrease the side effects of the other herbs (Liu et al., 2015). However, it must be noted that most of the include trials did not report the data of AEs. It may be because the incidence of AEs was indeed too rare or ignore the awareness on the AEs. Presently, the systematic data regarding the potential harm to the mothers and fetuses in the utilization of GAP is insufficient. In the near future, we hope that detailed pharmacotoxicity studies assessing the AEs of GAP will be conducted, providing sufficient evidence of safety.
To our knowledge, this is the first meta-analysis to quantitatively estimate the beneficial effect of GAP adjuvant therapy for TM, providing better evidence-based evaluation for the domestic and international researchers to understand this issue. Moreover, most of the pooled results had low heterogeneity and were generally consistent with the sensitivity analyses, showing a good stability. Additionally, the current quality of overall evidence assessed by GRADE can offer a comprehensive and transparent framework for promoting clinical practice guidelines. Importantly, extensive and in-depth data mining in applying TCM to the treatment of TM is conducive to inherit the clinical experience of ancient TCM, boost the understanding of the theory and practice of TCM in TM treatment and enrich the treatment options for treating TM.
Despite our critical evaluation of the currently available evidence, some potential limitations should not be ignored. Firstly, limitations included the low quality of some of included RCTs owing to the unclear allocation concealment and attrition bias, reducing the strength of evidence. Therefore, the present results should be interpreted with cautious owing to the aforementioned limitations and further high-quality, well-designed RCTs on this theme are urgently needed. Secondly, Notwithstanding we performed a thoroughgoing literature search with no language restriction, all included trails were entirely conducted in China, which likely limits their representativeness and generalizability. Thirdly, very few trials included have reported the outcomes of serum E2 levels and AEs, thus the objective influence to E2 value and safety must be evaluated by more rigorous RCTs. Additionally, although no obvious heterogeneity existed across the studies, some confounding factors (age and miscarriage history) affecting the pooled results could not fully adjusted based on the present information.
This systematic review provided evidence to the clinical practice that GAP combined with dydrogesterone may be effective and safe for treating patients with TM. However, the present results should be carefully interpreted because of the partial heterogeneity, suboptimal quality and high risk of bias of some included studies. In the future, further high-quality RCTs are required to ensure reliable effects of GAP adjuvant therapy for TM.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
KC, XL, and XW designed the research and the study concept. KC and XL performed the data extraction. KC, XL, and XM analyzed and interpreted the data. XL, XM, KC, and CY performed the quality and risk assessment. KC, XL, CY, XM, HL, and XW wrote the article. All authors contributed to the article and approved the submitted version.
This research was supported by grants from the Science Foundation of Jinan health commission (Grant No. 20204141) and Jinan City People’s Hospital.
Many thanks to Caiyan Liang for assistance in the format of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Amirchaghmaghi, E., Rezaei, A., Moini, A., Roghaei, M. A., Hafezi, M., and Aflatoonian, R. (2015). Gene expression analysis of VEGF and its receptors and assessment of its serum level in unexplained recurrent spontaneous abortion. Cell. J. 16 (4), 538–545. doi:10.22074/cellj.2015.498
Cai, J., Li, M., Huang, Q., Fu, X., and Wu, H. (2016). Differences in cytokine expression and STAT3 activation between healthy controls and patients of unexplained recurrent spontaneous abortion (URSA) during early pregnancy. PLoS One 11 (9), e0163252. doi:10.1371/journal.pone.0163252
Calleja-Agius, J., Schembri-Wismayer, P., Calleja, N., Brincat, M., and Spiteri, D. (2011). Obstetric outcome and cytokine levels in threatened miscarriage. Gynecol. Endocrinol. 27 (2), 121–127. doi:10.3109/09513590.2010.487614
Cao, X. L., Song, J. Y., Zhang, X. X., Chen, Y. H., Teng, Y. L., Liu, H. P., et al. (2020). Effects of a Chinese patent medicine gushen'antai pills on ongoing pregnancy rate of hormone therapy fet cycles: A multi-center, randomized, double-blind, placebo-controlled clinical trial. Front. Endocrinol. (Lausanne). 11, 581719. doi:10.3389/fendo.2020.581719
Carp, H. (2015). A systematic review of dydrogesterone for the treatment of recurrent miscarriage. Gynecol. Endocrinol. 31 (6), 422–430. doi:10.3109/09513590.2015.1006618
Carp, H. (2012). A systematic review of dydrogesterone for the treatment of threatened miscarriage. Gynecol. Endocrinol. 28 (12), 983–990. doi:10.3109/09513590.2012.702875
Cha, J., Sun, X., and Dey, S. K. (2012). Mechanisms of implantation: Strategies for successful pregnancy. Nat. Med. 18 (12), 1754–1767. doi:10.1038/nm.3012
Chang, W., Wu, Q. Q., Xiao, Y., Jiang, X. H., Yuan, Y., Zeng, X. F., et al. (2017). Acacetin protects against cardiac remodeling after myocardial infarction by mediating MAPK and PI3K/Akt signal pathway. J. Pharmacol. Sci. 135 (4), 156–163. doi:10.1016/j.jphs.2017.11.009
Chen, X., Qiu, X., and Jin, Y. (2022). Effects of dydrogesterone tablets combined with zishen yutai pills on threatened abortion in early pregnancy and pregnancy outcomes. Comput. Math. Methods Med. 2022, 4593637. doi:10.1155/2022/4593637
Colson, A., Depoix, C. L., Baldin, P., Hubinont, C., Sonveaux, P., and Debiève, F. (2020). Hypoxia-inducible factor 2 alpha impairs human cytotrophoblast syncytialization: New insights into placental dysfunction and fetal growth restriction. Faseb J. 34 (11), 15222–15235. doi:10.1096/fj.202001681R
Coomarasamy, A., Devall, A. J., Brosens, J. J., Quenby, S., Stephenson, M. D., Sierra, S., et al. (2020). Micronized vaginal progesterone to prevent miscarriage: A critical evaluation of randomized evidence. Am. J. Obstet. Gynecol. 223 (2), 167–176. doi:10.1016/j.ajog.2019.12.006
Dang, C. X., Wang, D., Liu, P. F., Liu, J. X., and Yu, X. (2022). Network pharmacological analysis and molecular docking of Huangqin-Baizhu herb pair in the treatment of threatened abortion. Med. Baltim. 101 (36), e30417. doi:10.1097/md.0000000000030417
Ding, J., Tan, X., Song, K., Ma, W., Xiao, J., Song, Y., et al. (2018). Bushen huoxue recipe alleviates implantation loss in mice by enhancing estrogen-progesterone signals and promoting decidual angiogenesis through FGF2 during early pregnancy. Front. Pharmacol. 9, 437. doi:10.3389/fphar.2018.00437
Dong, P., Wen, X., Liu, J., Yan, C. Y., Yuan, J., Luo, L. R., et al. (2017). Simultaneous detection of decidual Th1/Th2 and NK1/NK2 immunophenotyping in unknown recurrent miscarriage using 8-color flow cytometry with FSC/Vt extended strategy. Biosci. Rep. 37 (3). doi:10.1042/bsr20170150
Everett, C. (1997). Incidence and outcome of bleeding before the 20th week of pregnancy: Prospective study from general practice. BMJ 315 (7099), 32–34. doi:10.1136/bmj.315.7099.32
Ge, S. P. (2020). Effect of Gushen Antai Pill Combined with dydrogesterone on quality of life in treatment of threatened abortion. Renow Doct (10), 337–338.
Gillani, S. Q., Nisa, M. U., Sarwar, Z., Reshi, I., Bhat, S. A., Nabi, N., et al. (2021). Regulation of PCTAIRE1 protein stability by AKT1, LKB1 and BRCA1. Cell. Signal 85, 110032. doi:10.1016/j.cellsig.2021.110032
Gu, W. J., Huang, J., and Jiang, H. Y. (2022). Efficacy and safety of antiviral therapy in critically ill patients with mechanical ventilation: A meta-analysis with trial sequential analysis of randomized controlled trials. Clin. Microbiol. Infect. 28 (6), 792–800. doi:10.1016/j.cmi.2021.12.002
Gu, Y. (2019). Effect of Gushen Antai Pill Combined with dydrogesterone on serum hCG,P and E_2 in Patients with early threatened abortion. Mater Chil. Heal Care Chin. 34 (9), 2093–2096.
Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., et al. (2008). Grade: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336 (7650), 924–926. doi:10.1136/bmj.39489.470347.AD
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. doi:10.1136/bmj.d5928
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327 (7414), 557–560. doi:10.1136/bmj.327.7414.557
Huang, L., and Xu, D. (2020). Effect of Gushen Antai pill combined with dydrogesterone on serum endocrine hormone level and pregnancy outcome in patients with early threatened abortion. Guan J. Chin. Med. 35 (24), 3969–3971.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghan, D. J., et al. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials 17 (1), 1–12. doi:10.1016/0197-2456(95)00134-4
Ku, C. W., Allen, J. C., Lek, S. M., Chia, M. L., Tan, N. S., and Tan, T. C. (2018). Serum progesterone distribution in normal pregnancies compared to pregnancies complicated by threatened miscarriage from 5 to 13 weeks gestation: A prospective cohort study. BMC Pregnancy Childbirth 18 (1), 360. doi:10.1186/s12884-018-2002-z
Latifi, Z., Nejabati, H. R., Abroon, S., Mihanfar, A., Farzadi, L., Hakimi, P., et al. (2019). Dual role of TGF-β in early pregnancy: Clues from tumor progression. Biol. Reprod. 100 (6), 1417–1430. doi:10.1093/biolre/ioz024
Lee, H. J., Park, T. C., Kim, J. H., Norwitz, E., and Lee, B. (2017). The influence of oral dydrogesterone and vaginal progesterone on threatened abortion: A systematic review and meta-analysis. Biomed. Res. Int. 3616875, 3616875. doi:10.1155/2017/3616875
Lee, S. Y., Min, H. K., Lee, S. H., Shin, H. J., Lee, W. Y., Cho, Y. G., et al. (2016). IL-1 receptor antagonist (IL-1Ra)-Fc ameliorate autoimmune arthritis by regulation of the Th17 cells/Treg balance and arthrogenic cytokine activation. Immunol. Lett. 172, 56–66. doi:10.1016/j.imlet.2016.02.011
Li, H. F., Shen, Q. H., Li, X. Q., Feng, Z. F., Chen, W. M., Qian, J. H., et al. (2020). The efficacy of traditional Chinese medicine shoutai pill combined with western medicine in the first trimester of pregnancy in women with unexplained recurrent spontaneous abortion: A systematic review and meta-analysis. Biomed. Res. Int. 2020, 7495161. doi:10.1155/2020/7495161
Li, L. P., Wu, D. R., and Feng, L. P. (2018). Applied value of Gushen Antai pill combined with dydrogesterone tablets in the treatment of early threatened abortion. Str. Pharm. J. 30 (3), 106–107.
Li, Y., Xu, Q., Shi, M., Gan, P., Huang, Q., Wang, A., et al. (2020). Low-level laser therapy induces human umbilical vascular endothelial cell proliferation, migration and tube formation through activating the PI3K/Akt signaling pathway. Microvasc. Res. 129, 103959. doi:10.1016/j.mvr.2019.103959
Liao, H., Ye, J., Gao, L., and Liu, Y. (2021). The main bioactive compounds of scutellaria baicalensis georgi. For alleviation of inflammatory cytokines: A comprehensive review. Biomed. Pharmacother. 133, 110917. doi:10.1016/j.biopha.2020.110917
Liu, S. H., Chuang, W. C., Lam, W., Jiang, Z., and Cheng, Y. C. (2015). Safety surveillance of traditional Chinese medicine: Current and future. Drug Saf. 38 (2), 117–128. doi:10.1007/s40264-014-0250-z
Liu, W., Huang, Y., Huang, G., Zhou, C., Zeng, X., Zhao, S., et al. (2017). Relationship of SOCS3 and TGF-β with Ido expression in early pregnancy chorionic villi and decidua. Exp. Ther. Med. 14 (5), 4817–4824. doi:10.3892/etm.2017.5142
Lou, C., Wang, C., Zhao, Q., and Jin, F. (2021). Effect of dydrogesterone and progesterone on threatened miscarriage due to corpus luteum insufficiency. Am. J. Transl. Res. 13 (5), 4544–4552.
Lu, Y. Y., Zhu, Y., and Tian, G. (2017). Clinical observation on 50 cases of threatened abortion treated with Gushen Antai pill and dydrogesterone. Chin. Prac. Med. 12 (20), 126–127. doi:10.14163/j.cnki.11-5547/r.2017.20.068
Ma, A. T., Zhong, X. H., Liu, Z. M., Shi, W. Y., Du, J., Zhai, X. H., et al. (2009). Protective effects of baicalin against bromocriptine induced abortion in mice. Am. J. Chin. Med. 37 (1), 85–95. doi:10.1142/s0192415x09006709
Ma, Y. J., Cao, X. L., Ma, T., Song, J. Y., Yu, L. Y., Yu, Y. Y., et al. (2021). Study protocol: A multi-center, double-blind, randomized, 6-month, placebo-controlled trial to investigate the effect of supplementing hormone therapy FET cycles with gushen'antai pills on the outcomes of in vitro fertilization. Trials 22 (1), 657. doi:10.1186/s13063-021-05614-w
Maharajan, K., Xia, Q., Duan, X., Tu, P., Zhang, Y., and Liu, K. (2021). Therapeutic importance of zishen yutai pill on the female reproductive health: A review. J. Ethnopharmacol. 281, 114523. doi:10.1016/j.jep.2021.114523
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4 (1), 1. doi:10.1186/2046-4053-4-1
Omar, M. H., Mashita, M. K., Lim, P. S., and Jamil, M. A. (2005). Dydrogesterone in threatened abortion: Pregnancy outcome. J. Steroid Biochem. Mol. Biol. 97 (5), 421–425. doi:10.1016/j.jsbmb.2005.08.013
Osmanağaoğlu, M. A., Erdoğan, I., Eminağaoğlu, S., Karahan, S. C., Ozgün, S., Can, G., et al. (2010). The diagnostic value of beta-human chorionic gonadotropin, progesterone, CA125 in the prediction of abortions. J. Obstet. Gynaecol. 30 (3), 288–293. doi:10.3109/01443611003605286
Paliga, A. J., Natale, D. R., and Watson, A. J. (2005). p38 mitogen-activated protein kinase (MAPK) first regulates filamentous actin at the 8-16-cell stage during preimplantation development. Biol. Cell. 97 (8), 629–640. doi:10.1042/bc20040146
Singh, S., Meena, A., Luqman, S., and Meena, A. (2021). Acacetin and pinostrobin as a promising inhibitor of cancer-associated protein kinases. Food Chem. Toxicol. 151, 112091. doi:10.1016/j.fct.2021.112091
Sotiriadis, A., Papatheodorou, S., and Makrydimas, G. (2004). Threatened miscarriage: Evaluation and management. BMJ 329 (7458), 152–155. doi:10.1136/bmj.329.7458.152
Tang, J. C., Ren, Y. G., Zhao, J., Long, F., Chen, J. Y., and Jiang, Z. (2018). Shikonin enhances sensitization of gefitinib against wild-type EGFR non-small cell lung cancer via inhibition PKM2/stat3/cyclinD1 signal pathway. Life Sci. 204, 71–77. doi:10.1016/j.lfs.2018.05.012
Wang, P., Jiang, G., Ju, W., Cai, Y., Wang, J., and Wu, F. (2021). Influence of bushen tiaochong cycle therapy on Th1/Th2 deviation, sex hormone level, and pregnancy outcome of alloimmune recurrent spontaneous abortion. Evid. Based Complement. Altern. Med. 2021, 8624414. doi:10.1155/2021/8624414
Weiss, J. L., Malone, F. D., Vidaver, J., Ball, R. H., Nyberg, D. A., Comstock, C. H., et al. (2004). Threatened abortion: A risk factor for poor pregnancy outcome, a population-based screening study. Am. J. Obstet. Gynecol. 190 (3), 745–750. doi:10.1016/j.ajog.2003.09.023
Wu, H. W., Feng, Y. H., Wang, D. Y., Qiu, W. Y., Yu, Q. Y., Yang, L. L., et al. (2018). Effect of total flavones from cuscuta chinensis on anti-abortion via the MAPK signaling pathway. Evid. Based Complement. Altern. Med. 2018, 2018, 6356190. doi:10.1155/2018/6356190
Wu, L., Yang, F. R., Xing, M. L., Lu, S. F., Chen, H. L., Yang, Q. W., et al. (2022). Multi-material basis and multi-mechanisms of the Dahuang Zhechong pill for regulating Treg/Th1 balance in hepatocellular carcinoma. Phytomedicine 100, 154055. doi:10.1016/j.phymed.2022.154055
Xu, Y. (2021). Clinical observation of Gushen Antai pill combined with dydrogesterone in the treatment of early threatened abortion. Heal Horiz. (18), 98. doi:10.19347/j.cnki.2096-1413.201902062
Yang, G. Y., Luo, H., Liao, X., and Liu, J. P. (2013). Chinese herbal medicine for the treatment of recurrent miscarriage: A systematic review of randomized clinical trials. BMC Complement. Altern. Med. 13, 320. doi:10.1186/1472-6882-13-320
Yang, M., Luo, J., Li, Y., and Xu, L. (2020). Systems pharmacology-based research on the mechanism of tusizi-sangjisheng herb pair in the treatment of threatened abortion. Biomed. Res. Int. 4748264, 4748264. doi:10.1155/2020/4748264
Yang, M., Luo, J., Yang, Q., and Xu, L. (2021). Research on the medication rules of Chinese herbal formulas on treatment of threatened abortion. Complement. Ther. Clin. Pract. 43, 101371. doi:10.1016/j.ctcp.2021.101371
Yang, Y. (2020). Clinical effect of Gushen Antai pill combined with dydrogesterone tablets in the treatment of threatened abortion. Clin. Res. Prac. 5 (22), 134–135. doi:10.19347/j.cnki.2096-1413.202022050
Ye, M., Fang, R., Lun, S., and Fang, J. (2021). Effects of Gushen Antai decoction on serum homocysteine and anticardiolipin antibodies levels in patients with unexplained recurrent spontaneous abortion. Int. J. Clin. Exp. Med. 14(1), 340–346.
Zeng, P., Zhou, H., Guo, P., Xia, W., Huang, J., and Zeng, Q. (2021). Efficacy and safety of traditional Chinese herbal medicine in the treatment of threatened abortion: A protocol for systematic review and meta-analysis. Med. Baltim. 100 (5), e23288. doi:10.1097/md.0000000000023288
Zhang, J. W., and Qian, L. (2016). Clinical effect of Gushen Antai Pill combined with Dydrogesterone in the treatment of early threatened abortion. 3(3), 51–52. doi:10.16484/j.cnki.issn2095-8803.2016.03.029
Zhang, L. Y., Li, H., and Xiong, Y. (2014). Clinical observation of Gushen Antai pill combined with dydrogesterone in the treatment of early threatened abortion. J. Ytz Univ. 11 (30), 76–77. doi:10.16772/j.cnki.1673-1409.2014.30.034
Zhang, X. Y. (2020). The efficacy of dydrogesterone combined with Gushen antai pills in treatment of threatened abortion. Elec J. Prac. Gyn Endo 7 (20), 17+19. doi:10.16484/j.cnki.issn2095-8803.2020.20.010
Zhao, H., Wong, R. J., and Stevenson, D. K. (2021). The impact of hypoxia in early pregnancy on placental cells. Int. J. Mol. Sci. 22 (18), 9675. doi:10.3390/ijms22189675
Zhi, Z., Yang, W., Liu, L., Jiang, X., and Pang, L. (2018). Early missed abortion is associated with villous angiogenesis via the HIF-1α/VEGF signaling pathway. Arch. Gynecol. Obstet. 298 (3), 537–543. doi:10.1007/s00404-018-4802-9
Zhong, X. H., Shi, W. Y., Ma, A. T., Gong, X. C., Zhai, X. H., Zhang, T., et al. (2008). Effects of Radix scutellariae and Rhizoma atractylodis on LPS-induced abortion and the uterine IL-10 contents in mice. Am. J. Chin. Med. 36 (1), 141–148. doi:10.1142/s0192415x08005655
Zhong, X. H., Zhou, Z. X., Li, T. S., Wang, E. Q., Shi, W. Y., and Chu, S. M. (2002). Anti-abortive effect of Radix scutellariae and Rhizoma atractylodis in mice. Am. J. Chin. Med. 30 (1), 109–117. doi:10.1142/s0192415x02000120
Zhou, H., Yang, Y., Deng, L., Yao, Y., and Liao, X. (2021). A potential mechanism of kidney-tonifying herbs treating unexplained recurrent spontaneous abortion: Clinical evidence from the homogeneity of embryo implantation and tumor invasion. Front. Pharmacol. 12, 775245. doi:10.3389/fphar.2021.775245
Keywords: threatened miscarriage, Gushen Antai Pills, dydrogesterone, complementary therapy, meta-analysis
Citation: Chen K, Liu X, Meng X, Li H, Yang C and Wang X (2023) Efficacy and safety of Gushen Antai Pills combined with dydrogesterone in the treatment of threatened miscarriage: a systematic review and meta-analysis. Front. Pharmacol. 14:1138968. doi: 10.3389/fphar.2023.1138968
Received: 06 January 2023; Accepted: 22 May 2023;
Published: 02 June 2023.
Edited by:
Giada Crescioli, University of Florence, ItalyReviewed by:
Tian Xia, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, ChinaCopyright © 2023 Chen, Liu, Meng, Li, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohong Wang, eGlhb2hvbmd3YW5nbHdAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.