- 1Health Services and Systems Research, Duke-NUS Medical School, Singapore, Singapore
- 2Centre for Population Health Research and Implementation, SingHealth Regional Health System, Singapore, Singapore
- 3Department of Pharmacy, National University of Singapore, Singapore, Singapore
- 4Department of Internal Medicine, Singapore Health Services, Singapore, Singapore
- 5Duke-NUS Medical School, Singapore, Singapore
- 6Population Health and Integrated Care Office (PHICO), Singapore General Hospital, Singapore, Singapore
- 7Post-Acute and Continuing Care, Outram Community Hospital, Singapore, Singapore
- 8Department of Family Medicine and Continuing Care, Singapore General Hospital, Singapore, Singapore
- 9SingHealth Duke-NUS Family Medicine Academic Clinical Program, Singapore, Singapore
Background: Poor medication adherence can lead to adverse health outcomes and increased healthcare costs. Although reasons for medication adherence have been widely studied, less is explored about factors affecting medication adherence for patients in non-Western healthcare setting and from Asian cultures. This study aimed to explore cultural perspectives on factors influencing medication adherence among patients with chronic diseases in a multi-ethnic Asian healthcare setting.
Methods: We conducted a qualitative study involving in-depth interviews with patients with chronic conditions purposively recruited from a community hospital in Singapore until data saturation was achieved. A total of 25 patients participated in this study. Interviews were transcribed and thematically analyzed. Themes were subsequently mapped into the World Health Organization (WHO) Framework of Medication Adherence.
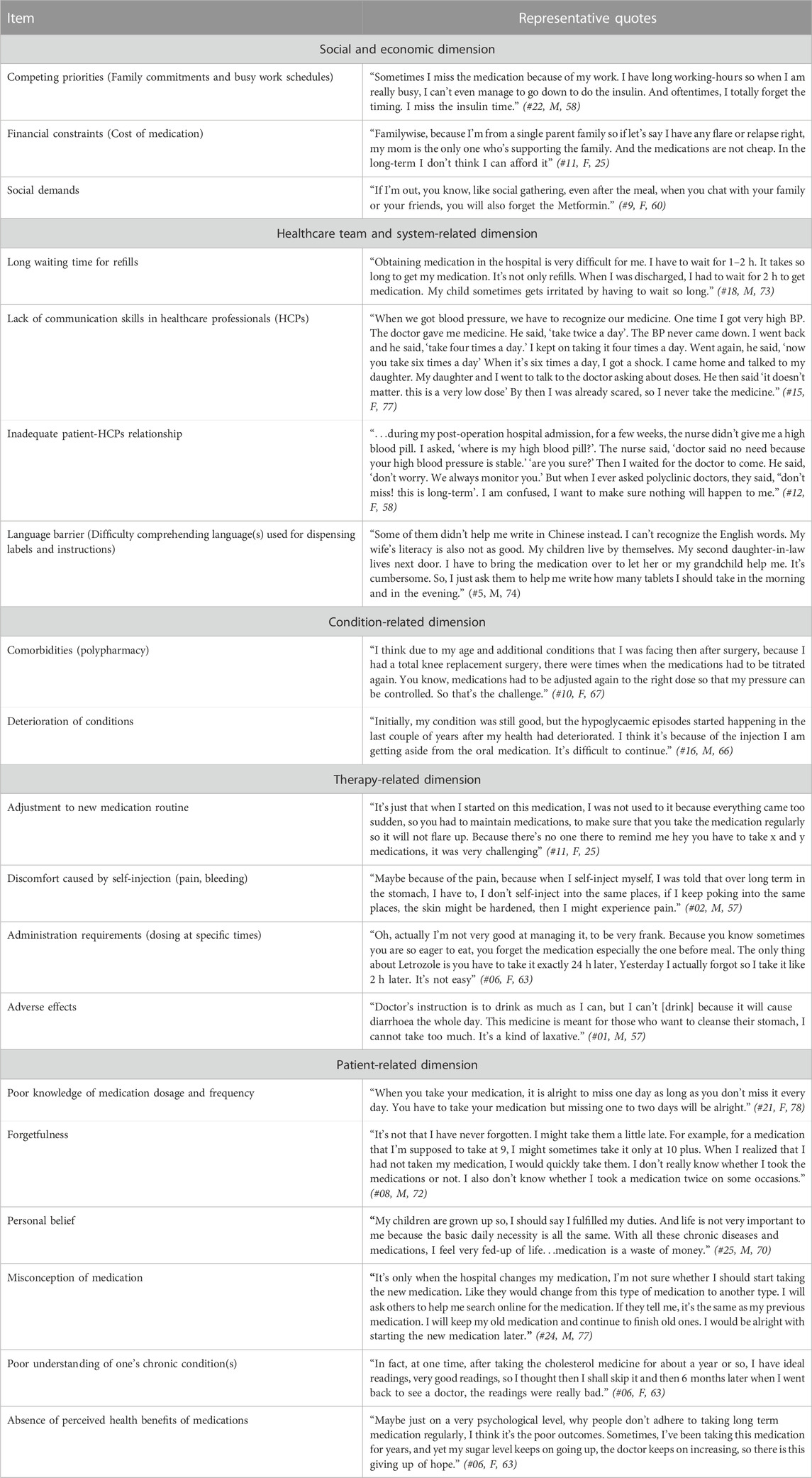
Results: Participants commonly perceived that sides effects (therapy-related dimension), poor understanding of medication (patient-related dimension), limited knowledge of condition (patient-related dimension), forgetfulness (patient-related dimension) and language issues within a multi-ethnic healthcare context (healthcare team and system-related dimension) as the main factors contributing to medication adherence. Importantly, medication adherence was influenced by cultural beliefs such as the notion of modern medicines as harms and fatalistic orientations towards escalation of doses and polypharmacy (patient-related dimension). Participants made various suggestions to foster adherence, including improved patient-physician communication, enhanced care coordination across providers, use of language familiar to patients, patient education and empowerment on the benefits of medication and medication adjustment.
Conclusion: A wide range of factors influenced medication adherence, with therapy- and patient-related dimensions more pronounced compared to other dimensions. Findings demonstrated the importance of cultural beliefs that may influence medication adherence. Future efforts to improve medication adherence should consider a person-centered approach to foster more positive health expectations and self-efficacy on medication adherence, supplemented with routine reviews, development of pictograms and cultural competence training for healthcare professionals.
1 Introduction
Medication adherence is defined as “the extent to which a person’s behavior in terms of taking medications corresponds to agreed recommendations from a healthcare provider” (WHO, 2003). Medication adherence can be also viewed as a dynamic process that changes over time and involves three components: initiation, implementation and persistence (Vrijens et al., 2012). Despite the importance of medication adherence, non-adherence to medication remains to be a significant challenge in managing chronic conditions. Studies have shown that up to 50% of patients with chronic diseases fail to take their medications as instructed (WHO, 2003; Kleinsinger, 2018; Foley et al., 2021). In Singapore where this study was conducted, around 60% percent of adults are non-adherent to their chronic disease medication regimen (Lee et al., 2017; Chew et al., 2021). Medication non-adherence creates a considerable economic and clinical burden to individuals and health systems. According to a systematic review by Cutler et al., the annual disease-specific economic cost associated with non-adherence ranged from US$949 to US$44,190 per person (Cutler et al., 2018). In addition, a previous report estimated that poor medication adherence resulted in 200,000 premature deaths in Europe each year (Khan and Socha-Dietrich, 2018). The economic and clinical repercussions of medication non-adherence underscore the importance of developing an optimal mechanism to foster adherence to medication regimen.
Medication adherence is a complex behavior with multiple factors in play. The World Health Organization (WHO) framework for medication adherence categorizes the factors affecting adherence into five major dimensions (WHO, 2003). Social and economic factors include the cost of medication and the impact of medicines on patients’ work and social lives. Healthcare team and system-related factors deal with healthcare workers’ knowledge, the distribution of medication, and the rapport between doctors and patients. Condition-related factors consider the impact of the severity and progression of the illness on medication adherence. Therapy-related factors relate to the complexity of the medication regime and possible adverse effects of medication. Finally, patient-related factors involve forgetfulness on the part of the patients, perceptions of their conditions, and their attitudes and mindsets, among many things.
The extent of and reasons for medication adherence have been empirically studied in different patient groups using various methods of measurement (Krass et al., 2015; Yap et al., 2016; Durand et al., 2017; Cheen et al., 2019). Literature reported that socioeconomic status and social support were found to be positively associated with medication adherence in adult patients with chronic diseases (Gast and Mathes, 2019; Peh et al., 2021). There have also been several meta-syntheses of qualitative studies exploring patients’ perspectives of perceived barriers to adherence (Marshall et al., 2012; Brundisini et al., 2015; Kvarnström et al., 2021). They highlighted that health beliefs, lay understanding of medication and life context contributed medication adherence. Although these factors are well documented and may apply to Asian patient populations, cultural and healthcare system specificities make it difficult to directly extrapolate from literature. Studies on international variations in medication adherence highlight the need to examine health system context of medication adherence (Rabia Khan, 2018). A recent systematic review also underlines the importance of personal and cultural beliefs that shape the adherence behavior (Shahin et al., 2019; McQuaid and Landier, 2018). However, with a few exceptions (Chen et al., 2009; Abdul Wahab et al., 2021), qualitative studies assessing medication adherence of Asian patients tended to focus on Asian minorities within the Western healthcare context (King-Shier et al., 2017; Jalal et al., 2019; Greenhalgh et al., 2015; Kumar et al., 2016; King-Shier et al., 2018).
Building on existing literature, this study aimed to explore factors influencing medication adherence among patients with chronic diseases in multi-ethnic Asian healthcare setting of Singapore. The healthcare system in Singapore employs a mixed model of public and private funding to ensure the optimum balance between individual responsibility and social protection. Although approximately 80% of the population obtain their healthcare services from the public health system that offers subsidized healthcare services (Khoo et al., 2014), the country’s primary care sector is being dominated by private general practices (Foo et al., 2021). The annual healthcare spending (4.08% of GDP) is lower than countries in developed Western economies such as the US (16%) and the United Kingdom (10%), yet health outcomes of Singapore are largely comparable with these countries (WHO, 2022). Recently, Singapore has announced the HealthierSG initiative in which residents are encouraged to anchor themselves with a primary care doctor for regular check-ins for chronic disease management (Abraham et al., 2022). Like many of its neighboring countries in Asia, Singapore is facing an increasingly aging population (Department of Statistics Singapore, 2021), and medication non-adherence is found to be associated with an increased risk of hospital admission and healthcare expenditure (Ling et al., 2020). Understanding patients’ perspectives will therefore enable an identification of challenges of medication adherence faced by multi-ethnic Asian patients with chronic diseases and inform the intervention to foster medication adherence.
2 Methods
2.1 Study design and participant recruitment
We conducted a qualitative study involving in-depth interviews. Patients were eligible if they were 21 years and above (a minor is defined as a person who is below 21 years of age in Singapore) and having one or more of the following chronic diseases: diabetes mellitus, heart disease, cancer, osteoarthritis, asthma, COPD, anxiety or depression, stroke, migraine, vision disorders, or adult-onset hearing loss. These diseases were selected based on the top 20 causes of the total burden of disease in Singapore (Ministry of Health Singapore, 2019). Eligible participants were purposively recruited based on gender, years of medication use, chronic condition, language spoken from inpatient wards at a large Community Hospital in Singapore. Eligible patients were identified from the administrative databases by two of the study team members (medical doctors). Potential participants were approached by a research staff who explained the purpose of the study. Patients in community hospitals generally stay for a few weeks for rehabilitation and discharge planning. Inpatient recruitment enabled the study team to facilitate the process from identification of eligible patients to recruitment to interviews.
2.2 Data collection
A semi-structured interview guide was developed based on existing literature (Marshall et al., 2012; Krass et al., 2015) with open-ended questions to probe the participants on the important aspects of medication adherence and reasons behind non-adherence (Supplementary Material). Topics included the extent and reasons for non-adherence, goals and motivations for medication adherence and chronic disease management, barriers to and facilitators of medication adherence and suggestions for improving medication adherence. Interviews were conducted in either English or Chinese by a female interviewer (ZL) who had credentials in Bachelor of Science and ample experience in in-depth interviews and focus group discussions in various clinical settings. The interviewer had no prior relationship with the participants. The interviews lasted 35 min–65 min in duration. A couple of participants had caregivers in attendance, but caregivers did not participate in the interviews. We originally planned to conduct face-to-face interviews. However, due to the safe distancing measures enforced during the COVID-19 pandemic, we conducted remote interviews via online video conferencing or phone call after the 12th interview. Field notes were taken by the study team member (WY).
2.3 Data analysis
All interviews were audio-recorded with the consent of the participants and transcribed verbatim. Transcriptions were not returned to participants due to time constraints. Interviews in Chinese were translated into English and verified for accuracy by the bilingual study team members. Data analysis involved a hybrid approach of data-driven inductive coding (Boyatzis, 1998) and template-based deductive coding (Crabtree and Miller, 1999), supported by iterative study team meetings. Inductive coding was first performed independently by two coders (WY, ZL). The coders first familiarize themselves with the data. The interview data was then coded through open and line-by-line coding by naming or defining concepts through close examination of the data. The data was grouped according to various provisional categories and subcategories of factors influencing medication adherence. For example, provisional categories such as being difficult to reconcile work and medication due to long working hours, caregiving responsibility, and house chores were later merged into a category of competing priorities. Each category was constantly reviewed and refined, with any discrepancies being iteratively discussed and resolved with the third study team member (SY).
The categories and sub-categories identified were then mapped into the WHO Framework of Medication Adherence to explore similarities and differences (WHO, 2003). WHO framework is useful for understanding factors contributing medication adherence in the context of chronic disease management in a holistic manner as it recognizes that issues surrounding medication adherence are not limited to a personal dimension but include a wider environment such as healthcare systems. Hence, this study used the framework as a reference point to explore how inductive results were aligned with different dimensions of adherence and whether there were any categories that did not fit one of the dimensions. The WHO framework provides descriptions of five dimensions of medication adherence which facilitated comparing of inductive coding categories with the framework’s dimensions and subsequently assigning them to these dimensions. Consensus meetings involving all study team members were held in an iterative manner to conduct peer review and validation of the overarching dimensions. The study team employed member checking, detailed audit trail and reflexivity at each step to ensure credibility and improve trustworthiness of the data (Lincoln and Guba, 1985). All data analysis was performed using a data management software, NVivo 12. For rigor and transparency, we anchored our methodology according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) (Supplementary Material) (Tong et al., 2007). Participant feedback was not sought due to difficulty contacting patients after discharge.
2.4 Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
2.5 Ethics
This study was approved by the SingHealth Centralized Institutional Review Board (Ref: 2020/2200). Written consent, which included publication of anonymized responses from the participants, was obtained prior to each interview.
3 Results
3.1 Participant characteristics
A total of 25 interviews were conducted. Data saturation was reached with 23 participants with no new themes emerging from subsequent interviews. We undertook two additional interviews to ensure that point of information redundancy was achieved. Of 33 patients purposively approached, eight patients rejected participation for reasons of speech impairment, time constraints and physical discomfort due to chronic conditions. The mean age was 66.4 years and 76% were Chinese. Participants had multiple chronic conditions: the majority of the participants had hypertension (68%), followed by hyperlipidemia (60%), diabetes mellitus (40%) and ischemic heart disease (20%). More than half of the participants (61.3%) had been on medication for more than ten years. (Table 1).
3.2 Factors influencing medication adherence
The factors influencing medication adherence, grouped according to the five dimensions of the WHO framework, are summarized in Table 2. Below, selected quotes were presented based on the representativeness of the themes identified and their informative nature.
3.2.1 Social and economic dimension
Participants mentioned that they had missed their medications due to competing priorities such as busy work schedules and family commitments. Having to attend social gatherings was also cited by participants. These activities served as an inadvertent distraction from a daily medication routine and resulted in failure to take the medication as prescribed. For example, participants described that social gathering could be considered as a barrier to medication non-adherence.
Although financial issues were not mentioned as a factor substantially hindering medication adherence, a minority of participants expressed that paying for regular prescriptions could be a burden for the family in the long term and hence would likely to impede medication adherence. As one participant described:
“The new oral medication for my diabetes was so costly as it was not covered by subsidies. My family is not well-off. So I stopped the medication.” (#4, M, 71)
3.2.2 Healthcare team and system-related dimension
The most common factors under the healthcare team and system-related domain included a perceived lack of communication skills in healthcare professionals (HCPs), long waiting times for refills and inadequate relationship between patients and healthcare professionals. Participants commonly stated having to wait for a long time to refill their medication or limited communication skills of HCPs to communicate with patients to elicit their needs and challenges in managing medications. As one participant highlighted, a lack of coordination across multiple physicians prescribing medications along with suboptimal quality of communication made it difficult to manage medications which could result in poor adherence:
“There are some doctors who will take time with the patient if they see that the previous doctor has done something and if they're not very comfortable with it, they will explain why. If they want to take off a medication or add a new medication, they spend the time to explain. Then there are some that are in a rush. You know they just like to briefly glance at the notes. I've had some doctors like this. Although it's written there that I can’t take a certain medication, they still prescribe that exact same medication.” (#15, F, 77)
Another item emerged from the data was the language-related issue. In the multi-ethnic society of Singapore, the primary working language in the healthcare system is English and thus written information is typically generated in English alone. Many older participants mentioned that they had difficulty understanding the instructions because they were not proficient in the language used in the prescription medication labels.
3.2.3 Condition-related dimension
The main challenges under condition-related dimension were the deterioration of conditions and presence of comorbidities. Participants commonly described the complexity of adherence to multiple medications with their comorbid health conditions. For example, a participant spoke of the medications having to be constantly titrated, which she found it challenging to keep up with the changes.
“It's like, if you started by taking, let's say, a very low dose of amlodipine, only one type of medication to control the blood pressure. But later, more and more medications were added to control the pressure. You know, where the medications need to be adjusted because the body's not controlling the blood pressure as well.” (#14, M, 62)
3.2.4 Therapy-related dimension
The most prominent item mentioned under therapy-related dimension was the presence of adverse effects. Those who experienced adverse effects from medications tended to stop their medications. Participants noted that often, they were not informed about the adverse effects and what they should do to counter the medication’s adverse reactions. A participant described:
“Sometimes when the doctor prescribes me some medication, I don’t think they are suitable for me. Sometimes I get a nosebleed when I take the medication. So, I let my daughter-in-law see the medication and she said I cannot take the medication. I will get a nosebleed if I take them. [Interviewer: Then what did you do?] I stop taking the medication and I don’t get a nosebleed.” (#17, M, 73)
Other participants mentioned that they did not adhere to their medications when they did not see any improvement in their chronic conditions. Participants also experienced difficulties when they first started a new medication or had to take medication at specific times.
3.2.5 Patient-related dimension
Across five WHO dimensions for medication adherence, patient-related dimension appeared to be markedly salient in our data. They included poor knowledge of medication dosage and frequency, forgetfulness, personal perception, misconception of medication, poor understanding of one’s chronic condition(s) and absence of perceived health benefits of medications. For example, lack of perceived improvement in one’s condition represented giving up of hope, resulting in cessation of medication intake.
Some participants expressed a fatalistic outlook by stating that they had achieved everything they needed in life and did not see the need to continue taking medications. Similarly, ‘Karma’ was highlighted by a non-adherent participant who believed that having to manage multiple medications was a punishment for his past wrongdoings.
“The number of medicines keeps increasing. I am living alone, and it becomes difficult to keep track of medicines. I don’t know when this [taking medication] will end, so I kind of give up [taking medication]. In my religion, it is called Karma. I think I am punished for my wrongdoings.” (#03, M, 61)
Others had cultural beliefs about Western medication as ‘harm’, making decisions to stop medications or lowering doses at their own discretion.
“To me, medicine is also a poison. So don’t depend on too much. I believe that medicine is not really good for the health. It’s good for the sickness, but it’s not good for the health.” (#04, M, 71)
3.3 Suggestions for improving medication adherence
Participants were asked what could help them to adhere to medication. Most of the suggestions were centered around four dimensions of the WHO framework. A summary of factors influencing medication adherence and suggestions to improve medication adherence based on WHO Framework of Medication Adherence can be found in Supplementary Material. For the social and economic dimension, participants would like to receive more subsidies from the government to help cover the cost of medical expenses. Participants also felt that reminders from family and friends and assistance from patient support groups would improve their adherence to medications.
Patient support groups can help improve medication adherence. As a patient and also part of patient support group, I always share (with patients) that it is important to adhere to the timing of the medications. The timing has to be very precise. It is very nerve-wracking. And we should always have our medications with us at all times.” (#12, F, 58)
Under the healthcare team and system-related dimension, there was agreement that adequate education by HCPs would be important in improving medication adherence. Other suggestions made by participants included improved patient-doctor relationships and enhanced care coordination across the healthcare systems and providers.
“I feel it is important how doctors explain and educate patients. For example, my doctor one day told me, although I am under control, once I start taking the high blood pill, I must take it for life. I didn’t understand, then the doctor drew a diagram on how medicine works and how skipping medications will affect my kidney long-term. From then, I always take the medicine. So, it’s important how doctors educate patients.” (#25, M, 70)
The use of a language that is familiar with patients would be critical for medication adherence.
“I would need someone who can write in Chinese whenever I collect my medications. Some of them write in English but I cannot understand. I would ask them what the medication is for and request them to write down how many tablets I have to take in the morning and in the evening in Chinese.” (#21, F, 78)
For the therapy-related dimension, an adjustment to the medication regimen in accordance with one’s lifestyle was found to be helpful.
My previous medication for hypercholesterolemia was supposed to be taken at night but I kept forgetting. I spoke to my doctor, and he changed the medication to one that can be taken in the morning together with my other medications. In this way, I will never forget the medication. So, it is important to find out how best to adjust (the medication regimen) to improve adherence.” (#06, F, 63)
Under the patient-related dimension, participants felt that increasing patient motivation and a good understanding of one’s own conditions could help achieve better medication adherence.
“What is important is to understand your own chronic conditions and your medications. You will also need to be motivated to be healthy. I think the hospital, the doctors and pharmacists can talk to patients who are not so compliant and encourage them to stay healthy. Every time I take medication, I always talk to myself ‘I want to be healthy, so I have to obey. I got to keep reminding me of the medication.” (#14, M, 62)
4 Discussion
4.1 Principal findings
This study sought to understand the factors contributing to medication adherence among multi-ethnic Asian patients with chronic diseases, using the WHO framework of medical adherence. We found that a broad range of factors influenced medication adherence, with therapy- and patient-related dimensions more pronounced compared to other dimensions. In particular, findings from this study demonstrated the importance of cultural beliefs that may contribute to medication adherence. Participants made several suggestions to improve adherence. They included improved patient-HCP relationships and enhanced care coordination across levels, use of language familiar to patients, patient education and empowerment on the benefit medication and medication adjustment.
4.2 Implications for research and practice
In our study, therapy-related dimension was the most prominent. In particular, the fear of adverse effects when taking medication was cited as the main barrier. The adverse effects ranged from gastrointestinal discomfort to joint pain and epistaxis; participants commonly reported that they stopped taking medications to prevent unpleasant or harmful reactions to medications. This may be an important factor to consider in a multi-ethnic society since adverse effects can vary with ethnicity (Hsu et al., 2010). Previous studies have found that adverse effects were one of the important reasons for lower rates of medication adherence (Marshall et al., 2012; Ju et al., 2018). A possible strategy to address non-adherence arising from adverse effects would be a benefit-risk counselling whereby physicians evaluate counseling needs of patients, educate steps needed to minimize risks and support patients in the treatment decision making (Kooy et al., 2014). Past research suggests that patients benefit greatly from routine medication reviews through re-evaluation of the patient’s experience at subsequent patient-physician interactions (Zaugg et al., 2018; Xu et al., 2020; Schindler et al., 2020). In addition, a collaborative effort between physicians and pharmacists was found to help patients cope with adverse effects of their medications (Shim et al., 2018). Further research is needed to determine the value of such programs and the most feasible way to implement them in a multi-ethnic Asian healthcare setting to enhance patient adherence.
Patient-related dimension was equally a leading cause of medication non-adherence in our study. Specifically, patient’s cultural perception regarding medication significantly influenced their decision for non-adherence. A specific belief brought up by participants was that Western medications were detrimental to one’s health in the long-term; for this reason, participants often intentionally self-adjusted medication dose or discontinued medications without consulting their doctors. However, we did not observe cultural beliefs on the superiority of traditional medication over Western medication or concurrent intake of both Western and complementary medications, a common belief and practice found in studies of Asian patients in a Western healthcare setting (Li et al., 2006; Eh et al., 2016; Jamil et al., 2022). Our findings are also in contrast with studies in Western healthcare settings where spirituality and religious beliefs were culturally significant factors that were shown to have a considerable effect on medication adherence (Albargawi et al., 2017; McQuaid and Landier, 2018; Shahin et al., 2019). Our finding, together with results from other studies, underlines the importance of understanding cultural perceptions in medication adherence. HCPs should consider the impact of cultural beliefs on medication adherence in diverse ethnic patients when implementing appropriate education strategies (Saha et al., 2013; Bosworth et al., 2017). Developing a program to train HCPs in cultural competence might serve to further promote communication with diverse patients, engaging them as collaborative partners in their care in a multi-ethnic and multi-cultural healthcare setting. Studies have shown that targeted interventions to address specific concerns of cultural groups can enhance adherence and health outcomes (Zolnierek and Dimatteo, 2009; Zeh et al., 2012). Indeed, effective patient education and empowerment were desired by many of our participants. It is therefore timely to implement ongoing support and culturally sensitive educational programs to achieve better medication adherence.
Another culturally relevant factor under the patient-related dimension was patients’ belief about fatalism in our multi-ethnic Asian setting. We found that for some patients, the escalation of medication doses or having to take multiple medications was viewed as meaningless or losing hope, and consequently, there was a gradual sense of aversion to medication intake. Destiny, that seems to be more acceptable in Asian culture, may account for this non-adherent behavior (Heiniger et al., 2015; Kim and Lwin, 2021). Clinicians and healthcare teams should consider how cultural background can impact on health beliefs about medication to ensure that more sensitive care is provided to diverse ethnic patient groups. We also suggest that patients with fatalistic cultural beliefs may benefit from a person-centered approach to foster more positive health expectations, self-efficacy, and health locus of control (extent of an individual’s perceived control over health outcomes on medication adherence) (Bosworth et al., 2017; Gerland and Prell, 2021).
When comparing our results on healthcare team and system-related dimension to recent reviews which assessed factors associated with medication non-adherence (Konstantinou et al., 2020; Kvarnström et al., 2021), we found that language issue was more prominent in our healthcare settings. Having difficulty in understanding the language used by HCPs or written instructions used for medication labels can result in poor communication and suboptimal clinical outcomes. Prior studies reported that limited language proficiency leads to poor medication adherence in migrant or less acculturated minority patients in a Western setting (Kumar et al., 2016; Jalal et al., 2019), What is different in our study is that the language barriers were commonly reported across the board, indicating that patients particularly of older age experienced language issues regardless of ethnic minority status. Greater effort is therefore required to ensure that a language familiar with the patient is used to deliver messages regarding instruction, a suggestion also made by our participants. A combination of pictograms and bilingual text should also be considered to assist communication of medication use as evidenced by previous intervention literature (Berthenet et al., 2016; Malhotra et al., 2019).
Lastly, under social and economic dimensions, financial constraints were acknowledged by some participants who suggested the extension of government subsidies to offset cost concerns. Yet, it should be noted that the majority of participants did not see financial commitments as a determining factor influencing medication non-adherence. This is in contrast to previous studies where cost of medications was a commonly cited factor affecting medication adherence (Briesacher et al., 2007; Khera et al., 2019). A key reason for this difference may be that many medications for common chronic diseases in Singapore are heavily subsidized in public healthcare institutions through various schemes available to patients (e.g., Medisave, MediShield, MediFund and the Community Healthcare Assistance Scheme) that help ease their financial burden (Ministry of Health Singapore, 2021). However, physicians should be aware that a small number of patients might still face cost-related adherence issues so that prescription planning could be done to minimize the cost barriers.
4.3 Strengths and limitations
All participants interviewed in this study had at least one disease that falls under the top 20 causes of the total burden of disease in Singapore. Our participants also represented a broad spectrum of the patient population with chronic diseases in terms of the level of education, number of years of taking medications and language spoken. Hence, by obtaining their perspectives on medication adherence, the results of this study provided a meaningful insight into the complexity of factors influencing medication adherence in multi-ethnic Asian patients with chronic diseases.
This study is not without its limitations. First, as participants were recruited from a single intermediary healthcare institution, their experiences might not be generalizable to the spectrum of healthcare services in Singapore. However, many participants recounted their experiences of public primary care services in relation to the topic of medication adherence and hence their perspectives would be relevant. The format of interviews used in this study was limited to individual interviews due to difficulty in scheduling a group discussion. While the questions asked in individual interviews facilitated in-depth open discussions, focus groups would have allowed for a better exchange of views and experiences amongst participants that could have brought about other unique themes (Kitzinger, 1995). While the WHO framework has the benefits of considering a diverse range of factors related to medication adherence, use of other relevant frameworks could have engendered unique insights on medication adherence (e.g., ABC taxonomy for process-oriented medication adherence behavior) (Vrijens et al., 2012). Therefore, more research should be done using different frameworks to explain complex pattens of medication behavior and associated factors. Lastly, despite our efforts to recruit a balanced sample, there was a limited representation of Indian participants in this study, which might have introduced a selection bias in the findings. Nevertheless, the proportion of ethnicity was similar to the distribution of ethnicity in Singapore although Indian participants were slightly under-represented (Department of Statistics Singapore, 2021).
5 Conclusion
This study identified a wide range of factors that contributed to medication adherence. Our findings shed light on the importance of cultural beliefs that may affect medication adherence in a multi-ethnic Asian healthcare setting. The factors identified in this study can enable clinicians to understand multiple underlying determinants that promote or hinder medication adherence and incorporate patient concerns and perspectives into appropriate strategies to enhance adherence. healthcare professionals should pay more attention to addressing language barriers and patient’s cultural beliefs through patient education by language-concordant healthcare professionals, succinct written instructions and involvement of trained medical interpreters. In addition, interventions aimed at improving medication adherence will benefit from considering a person-centered approach to foster positive health expectations, locus of control and self-efficacy, along with routine reviews, development of pictograms and cultural competence training for healthcare professionals.
Data availability statement
The datasets presented in this article are not readily available because of participant confidentiality and participant privacy. Requests to access the datasets should be directed to low.lian.leng@singhealth.com.sg.
Ethics statement
The studies involving human participants were reviewed and approved by SingHealth Centralized Institutional Review Board (Ref: 2020/2200). The patients/participants provided their written informed consent to participate in this study.
Author contributions
SY, YK, and LL contributed to the conception of the study. SY and YK designed the work. WY, ZYL, YL, JA, and LL contributed to the acquisition of the data. All authors contributed to the analysis and interpretation of data. SY drafted the manuscript. All authors revised the manuscript critically for important intellectual content and approved the final version.
Funding
This research is supported by the National Medical Research Council (NMRC) through the SingHealth PULSES Centre Grant (NMRC/CG/027/2017) and the SingHealth PULSES II Centre Grant (CG21APR1013).
Acknowledgments
The authors thank all participants who provided valuable insights for the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1124297/full#supplementary-material
References
Abdul Wahab, N. A., Makmor Bakry, M., Ahmad, M., Mohamad Noor, Z., and Mhd Ali, A. (2021). Exploring culture, religiosity and spirituality influence on antihypertensive medication adherence among specialised population: A qualitative ethnographic approach. Patient Prefer Adherence 15, 2249–2265. doi:10.2147/ppa.S319469
Abraham, M., Lim, M. J., Tan, W. S., and Cheah, J. (2022). Global trends towards population health management and key lessons and initiatives in the Singapore context. Int. J. Integr. Care 22 (3), 19. doi:10.5334/ijic.7016
Albargawi, M., Snethen, J., Al Gannass, A., and Kelber, S. (2017). Relationship between person's health beliefs and diabetes self-care management regimen. J. Vasc. Nurs. 35 (4), 187–192. doi:10.1016/j.jvn.2017.07.002
Berthenet, M., Vaillancourt, R., and Pouliot, A. (2016). Evaluation, modification, and validation of pictograms depicting medication instructions in the elderly. J. Health Commun. 21, 27–33. doi:10.1080/10810730.2015.1133737
Bosworth, H. B., Fortmann, S. P., Kuntz, J., Zullig, L. L., Mendys, P., Safford, M., et al. (2017). Recommendations for providers on person-centered approaches to assess and improve medication adherence. J. general Intern. Med. 32 (1), 93–100. doi:10.1007/s11606-016-3851-7
Boyatzis, R. E. (1998). Transforming qualitative information: Thematic analysis and code development. Thousand Oaks, CA: Sage.
Briesacher, B. A., Gurwitz, J. H., and Soumerai, S. B. (2007). Patients at-risk for cost-related medication nonadherence: A review of the literature. J. Gen. Intern Med. 22 (6), 864–871. doi:10.1007/s11606-007-0180-x
Brundisini, F., Vanstone, M., Hulan, D., DeJean, D., and Giacomini, M. (2015). Type 2 diabetes patients' and providers' differing perspectives on medication nonadherence: A qualitative meta-synthesis. BMC Health Serv. Res. 15, 516. doi:10.1186/s12913-015-1174-8
Cheen, M. H. H., Tan, Y. Z., Oh, L. F., Wee, H. L., and Thumboo, J. (2019). Prevalence of and factors associated with primary medication non-adherence in chronic disease: A systematic review and meta-analysis. Int. J. Clin. Pract. 73 (6), e13350. doi:10.1111/ijcp.13350
Chen, S. L., Tsai, J. C., and Lee, W. L. (2009). The impact of illness perception on adherence to therapeutic regimens of patients with hypertension in Taiwan. J. Clin. Nurs. 18 (15), 2234–2244. doi:10.1111/j.1365-2702.2008.02706.x
Chew, S. M., Lee, J. H., Lim, S. F., Liew, M. J., Xu, Y., and Towle, R. M. (2021). Prevalence and predictors of medication non-adherence among older community-dwelling people with chronic disease in Singapore. J. Adv. Nurs. 77 (10), 4069–4080. doi:10.1111/jan.14913
Crabtree, B. F., and Miller, W. F. (1999). “A template approach to text analysis: Developing and using codebooks,” in Doing qualitative research. Editors B. Crabtree, and W. Miller (Newbury Park, CA: Sage).
Cutler, R. L., Fernandez-Llimos, F., Frommer, M., Benrimoj, C., and Garcia-Cardenas, V. (2018). Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open 8 (1), e016982. doi:10.1136/bmjopen-2017-016982
Durand, H., Hayes, P., Morrissey, E. C., Newell, J., Casey, M., Murphy, A. W., et al. (2017). Medication adherence among patients with apparent treatment-resistant hypertension: Systematic review and meta-analysis. J. Hypertens. 35 (12), 2346–2357. doi:10.1097/hjh.0000000000001502
Eh, K., McGill, M., Wong, J., and Krass, I. (2016). Cultural issues and other factors that affect self-management of Type 2 Diabetes Mellitus (T2D) by Chinese immigrants in Australia. Diabetes Res. Clin. Pract. 119, 97–105. doi:10.1016/j.diabres.2016.07.006
Foley, L., Larkin, J., Lombard-Vance, R., Murphy, A. W., Hynes, L., Galvin, E., et al. (2021). Prevalence and predictors of medication non-adherence among people living with multimorbidity: A systematic review and meta-analysis. BMJ Open 11 (9), e044987. doi:10.1136/bmjopen-2020-044987
Foo, C. D., Surendran, S., Tam, C. H., Ho, E., Matchar, D. B., Car, J., et al. (2021). Perceived facilitators and barriers to chronic disease management in primary care networks of Singapore: A qualitative study. BMJ Open 11 (5), e046010. doi:10.1136/bmjopen-2020-046010
Gast, A., and Mathes, T. (2019). Medication adherence influencing factors-an (updated) overview of systematic reviews. Syst. Rev. 8 (1), 112. doi:10.1186/s13643-019-1014-8
Gerland, H. E., and Prell, T. (2021). Association between the health locus of control and medication adherence: An observational, cross-sectional study in primary care. Front. Med. (Lausanne) 8, 705202. doi:10.3389/fmed.2021.705202
Greenhalgh, T., Clinch, M., Afsar, N., Choudhury, Y., Sudra, R., Campbell-Richards, D., et al. (2015). Socio-cultural influences on the behaviour of south asian women with diabetes in pregnancy: Qualitative study using a multi-level theoretical approach. BMC Med. 13, 120. doi:10.1186/s12916-015-0360-1
Heiniger, L. E., Sherman, K. A., Shaw, L. K., and Costa, D. (2015). Fatalism and health promoting behaviors in Chinese and Korean immigrants and Caucasians. J. Immigr. Minor Health 17 (1), 165–171. doi:10.1007/s10903-013-9922-5
Hsu, Y. H., Mao, C. L., and Wey, M. (2010). Antihypertensive medication adherence among elderly Chinese Americans. J. Transcult. Nurs. 21 (4), 297–305. doi:10.1177/1043659609360707
Jalal, Z., Antoniou, S., Taylor, D., Paudyal, V., Finlay, K., and Smith, F. (2019). South asians living in the UK and adherence to coronary heart disease medication: A mixed-method study. Int. J. Clin. Pharm. 41 (1), 122–130. doi:10.1007/s11096-018-0760-3
Jamil, A., Jonkman, L. J., Miller, M., Jennings, L., and Connor, S. E. (2022). Medication adherence and health beliefs among south asian immigrants with diabetes in the United States: A qualitative study. JACCP J. Am. Coll. Clin. Pharm. 5 (8), 829–836. doi:10.1002/jac5.1668
Ju, A., Hanson, C. S., Banks, E., Korda, R., Craig, J. C., Usherwood, T., et al. (2018). Patient beliefs and attitudes to taking statins: Systematic review of qualitative studies. Br. J. Gen. Pract. 68 (671), e408–e419. doi:10.3399/bjgp18X696365
Khan, R., and Socha-Dietrich, K. (2018). Investing in medication adherence improves health outcomes and health system efficiency: Adherence to medicines for diabetes, hypertension, and hyperlipidaemia. Germany: OECD.
Khera, R., Valero-Elizondo, J., Das, S. R., Virani, S. S., Kash, B. A., de Lemos, J. A., et al. (2019). Cost-related medication nonadherence in adults with atherosclerotic cardiovascular disease in the United States, 2013 to 2017. Circulation 140 (25), 2067–2075. doi:10.1161/circulationaha.119.041974
Khoo, H. S., Lim, Y. W., and Vrijhoef, H. J. (2014). Primary healthcare system and practice characteristics in Singapore. Asia Pac Fam. Med. 13 (1), 8. doi:10.1186/s12930-014-0008-x
Kim, H. K., and Lwin, M. O. (2021). Cultural determinants of cancer fatalism and cancer prevention behaviors among asians in Singapore. Health Commun. 36 (8), 940–949. doi:10.1080/10410236.2020.1724636
King-Shier, K. M., Singh, S., Khan, N. A., LeBlanc, P., Lowe, J. C., Mather, C. M., et al. (2017). Ethno-cultural considerations in cardiac patients' medication adherence. Clin. Nurs. Res. 26 (5), 576–591. doi:10.1177/1054773816646078
King-Shier, K., Quan, H., Mather, C., Chong, E., LeBlanc, P., and Khan, N. (2018). Understanding ethno-cultural differences in cardiac medication adherence behavior: A Canadian study. Patient Prefer Adherence 12, 1737–1747. doi:10.2147/ppa.S169167
Kitzinger, J. (1995). Qualitative research. Introducing focus groups. Bmj 311 (7000), 299–302. doi:10.1136/bmj.311.7000.299
Kleinsinger, F. (2018). The unmet challenge of medication nonadherence. Perm. J. 22, 18–033. doi:10.7812/TPP/18-033
Konstantinou, P., Kassianos, A. P., Georgiou, G., Panayides, A., Papageorgiou, A., Almas, I., et al. (2020). Barriers, facilitators, and interventions for medication adherence across chronic conditions with the highest non-adherence rates: A scoping review with recommendations for intervention development. Transl. Behav. Med. 10 (6), 1390–1398. doi:10.1093/tbm/ibaa118
Kooy, M. J., van Geffen, E. C., Heerdink, E. R., van Dijk, L., and Bouvy, M. L. (2014). Effects of a TELephone counselling intervention by pharmacist (TelCIP) on medication adherence, patient beliefs and satisfaction with information for patients starting treatment: Study protocol for a cluster randomized controlled trial. BMC Health Serv. Res. 14, 219. doi:10.1186/1472-6963-14-219
Krass, I., Schieback, P., and Dhippayom, T. (2015). Adherence to diabetes medication: A systematic review. Diabet. Med. 32 (6), 725–737. doi:10.1111/dme.12651
Kumar, K., Greenfield, S., Raza, K., Gill, P., and Stack, R. (2016). Understanding adherence-related beliefs about medicine amongst patients of south asian origin with diabetes and cardiovascular disease patients: A qualitative synthesis. BMC Endocr. Disord. 16 (1), 24. doi:10.1186/s12902-016-0103-0
Kvarnström, K., Westerholm, A., Airaksinen, M., and Liira, H. (2021). Factors contributing to medication adherence in patients with a chronic condition: A scoping review of qualitative research. Pharmaceutics 13 (7), 1100. doi:10.3390/pharmaceutics13071100
Lee, C. S., Tan, J. H. M., Sankari, U., Koh, Y. L. E., and Tan, N. C. (2017). Assessing oral medication adherence among patients with type 2 diabetes mellitus treated with polytherapy in a developed asian community: A cross-sectional study. BMJ Open 7 (9), e016317. doi:10.1136/bmjopen-2017-016317
Li, W. W., Stewart, A. L., Stotts, N., and Froelicher, E. S. (2006). Cultural factors associated with antihypertensive medication adherence in Chinese immigrants. J. Cardiovasc Nurs. 21 (5), 354–362. doi:10.1097/00005082-200609000-00005
Ling, R. Z. Q., Jiao, N., Hassan, N. B., He, H., and Wang, W. (2020). Adherence to diet and medication and the associated factors among patient with chronic heart failure in a multi-ethnic society. Heart Lung 49 (2), 144–150. doi:10.1016/j.hrtlng.2019.11.003
Malhotra, R., Bautista, M. A. C., Tan, N. C., Tang, W. E., Tay, S., Tan, A. S. L., et al. (2019). Bilingual text with or without pictograms improves elderly Singaporeans' understanding of prescription medication labels. Gerontologist 59 (2), 378–390. doi:10.1093/geront/gnx169
Marshall, I. J., Wolfe, C. D., and McKevitt, C. (2012). Lay perspectives on hypertension and drug adherence: Systematic review of qualitative research. Bmj 345, e3953. doi:10.1136/bmj.e3953
McQuaid, E. L., and Landier, W. (2018). Cultural issues in medication adherence: Disparities and directions. J. Gen. Intern Med. 33 (2), 200–206. doi:10.1007/s11606-017-4199-3
Ministry of Health Singapore (2021). Drug subsidies and schemes. Available: https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/drug-subsidies-schemes (Accessed February 17, 2021).
Ministry of Health Singapore (2019). The burden of disease in Singapore, 1999-2017: An overview of the global burden of disease study 2017 results. Available: https://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Singapore_Report.pdf (Accessed November 1, 2021).
Peh, K. Q. E., Kwan, Y. H., Goh, H., Ramchandani, H., Phang, J. K., Lim, Z. Y., et al. (2021). An adaptable framework for factors contributing to medication adherence: Results from a systematic review of 102 conceptual frameworks. J. Gen. Intern Med. 36 (9), 2784–2795. doi:10.1007/s11606-021-06648-1
Rabia Khan, K. S.-D. (2018). “Investing in medication adherence improves health outcomes and health system efficiency: Adherence to medicines for diabetes, hypertension and hyperlipidemia,” in OECD health working paper (France: Organisation for Economic Co-peration and Development).
Saha, S., Korthuis, P. T., Cohn, J. A., Sharp, V. L., Moore, R. D., and Beach, M. C. (2013). Primary care provider cultural competence and racial disparities in HIV care and outcomes. J. Gen. Intern Med. 28 (5), 622–629. doi:10.1007/s11606-012-2298-8
Schindler, E., Hohmann, C., and Culmsee, C. (2020). Medication review by community pharmacists for type 2 diabetes patients in routine care: Results of the DIATHEM-study. Front. Pharmacol. 11, 1176. doi:10.3389/fphar.2020.01176
Shahin, W., Kennedy, G. A., and Stupans, I. (2019). The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: A systematic review. Patient Prefer Adherence 13, 1019–1035. doi:10.2147/ppa.S212046
Shim, Y. W., Chua, S. S., Wong, H. C., and Alwi, S. (2018). Collaborative intervention between pharmacists and physicians on elderly patients: A randomized controlled trial. Ther. Clin. Risk Manag. 14, 1115–1125. doi:10.2147/tcrm.S146218
Department of Statistics Singapore (2021). Population trends 2021. Available: https://www.singstat.gov.sg/-/media/files/publications/population/population2021.pdf (Accessed December 26, 2021).
Tong, A., Sainsbury, P., and Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 19 (6), 349–357. doi:10.1093/intqhc/mzm042
Vrijens, B., De Geest, S., Hughes, D. A., Przemyslaw, K., Demonceau, J., Ruppar, T., et al. (2012). A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 73 (5), 691–705. doi:10.1111/j.1365-2125.2012.04167.x
WHO (2022). World health organization global health expenditure database. Available: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=SG [Accessed].
WHO (2003). “Adherence to long-term therapies: Evidence for action,” in Eduardo sabaté] (Geneva: World Health Organization).
Xu, H. Y., Yu, Y. J., Zhang, Q. H., Hu, H. Y., and Li, M. (2020). Tailored interventions to improve medication adherence for cardiovascular diseases. Front. Pharmacol. 11, 510339. doi:10.3389/fphar.2020.510339
Yap, A. F., Thirumoorthy, T., and Kwan, Y. H. (2016). Systematic review of the barriers affecting medication adherence in older adults. Geriatr. Gerontol. Int. 16 (10), 1093–1101. doi:10.1111/ggi.12616
Zaugg, V., Korb-Savoldelli, V., Durieux, P., and Sabatier, B. (2018). Providing physicians with feedback on medication adherence for people with chronic diseases taking long-term medication. Cochrane Database Syst. Rev. 1 (1), Cd012042. doi:10.1002/14651858.CD012042.pub2
Zeh, P., Sandhu, H. K., Cannaby, A. M., and Sturt, J. A. (2012). The impact of culturally competent diabetes care interventions for improving diabetes-related outcomes in ethnic minority groups: A systematic review. Diabet. Med. 29 (10), 1237–1252. doi:10.1111/j.1464-5491.2012.03701.x
Keywords: medication adherence, chronic disease, Asian patients, multi-ethnic setting, WHO framework
Citation: Yoon S, Kwan YH, Yap WL, Lim ZY, Phang JK, Loo YX, Aw J and Low LL (2023) Factors influencing medication adherence in multi-ethnic Asian patients with chronic diseases in Singapore: A qualitative study. Front. Pharmacol. 14:1124297. doi: 10.3389/fphar.2023.1124297
Received: 15 December 2022; Accepted: 17 February 2023;
Published: 09 March 2023.
Edited by:
Grigorios L. Kyriakopoulos, National Technical University of Athens, GreeceReviewed by:
Mojtaba Vaismoradi, Nord University, NorwayNejc Horvat, University of Ljubljana, Slovenia
Copyright © 2023 Yoon, Kwan, Yap, Lim, Phang, Loo, Aw and Low. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lian Leng Low, bG93LmxpYW4ubGVuZ0BzaW5naGVhbHRoLmNvbS5zZw==
†These authors have contributed equally to this work and share first authorship
 Sungwon Yoon
Sungwon Yoon Yu Heng Kwan
Yu Heng Kwan Wei Liang Yap
Wei Liang Yap Zhui Ying Lim6
Zhui Ying Lim6 Jie Kie Phang
Jie Kie Phang Junjie Aw
Junjie Aw Lian Leng Low
Lian Leng Low