
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 24 February 2023
Sec. Drugs Outcomes Research and Policies
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1051350
 Mojtaba Shafiekhani1,2,3
Mojtaba Shafiekhani1,2,3 Farbod Shahabinezhad3†
Farbod Shahabinezhad3† Zahra Tavakoli2†
Zahra Tavakoli2† Tahereh Tarakmeh2
Tahereh Tarakmeh2 Elham Haem4
Elham Haem4 Negar Sari2
Negar Sari2 Shohreh Nasirabadi2
Shohreh Nasirabadi2 Masoud Dehghani1*
Masoud Dehghani1*Purpose: Transplanted organ survival after solid organ transplantation highly correlates with the adherence levels of the patients to their immunosuppressive drugs. On the other hand, one of the main goals of liver transplantation is to increase the overall quality of life (QOL) for the patient. This study is aimed to analyze the relationship between adherence and QOL in adult liver transplant recipients of the biggest liver transplant center in Asia.
Methods: All of the included patients were older than 18 years and at least 6 months had passed from their liver transplantation. The adherence level was measured with BAASIS method and the QOL was assessed by SF-36 questionnaire in real-time interviews. The relationship between adherence and different aspects of QOL in addition to qualitative and quantitative influential factors on these two outcomes was calculated with statistical analysis.
Results: Among the 122 included patients, 41% of the were categorized in the non-adherent group. The most important reasons for non-adherence in these patients included forgetfulness (62%), lack of medication (12%), financial problems for drug supply (9%), and side effects (2%). According to the results of the multivariate linear regression model, rejection was the only influential factor in the occurrence of non-adherence among patients (OR = 8.226 CI (1.404-48.196)). The overall mean QOL score of patients was reported 51.09 ± 21.86. The lowest is given to social functioning, while mental health has achieved the highest score. The mean QOL scores in different dimensions in patients with adherence were higher than non-adherents, which was only significant in mental health (p-value = 0.01). Additionally, in total scores related to Physical Composite Score (PSC) and Mental Composite Score (MCS), the mean MSC scores in adherent patients were significantly higher than non-adherent patients (p-value: 0.02). Although adherent patients have an overall greater QOL, the only meaningful effect on QOL total score was from income level.
Conclusion: The overall QoL score has been in all parameters higher in the adherent group compared with non-adherent patients. The difference in QoL was most meaningfully significant in mental composite score among other parameters of QoL.
Liver transplantation is a lifesaving intervention available for patients suffering from end-stage liver diseases. There is an increasing number of liver transplant centers that provide liver transplant surgeries across the world. According to United Network for Organ Sharing (UNOS), 8,906 liver transplants were performed in the United States in 2020 (Organ transplant trends | More transplants than ever UNOS, 2021). Shiraz Transplant Center is the leader in solid organ transplantation in the Middle East and Asia and one of the largest liver transplant centers in the world, with more than 500 solid organ transplants per year (Malek-Hosseini et al., 2019). The first liver transplantation in Iran was performed in 1992 at Namazee Hospital, Shiraz. Since then more than 6,500 cases of liver transplants have been performed in Iran.
Immunosuppressive medications are still considered a critical component in patients’ post-transplant care. Adherence to an immunosuppressive regimen after liver transplantation guarantees graft survival (Jones and Serper, 2020). Non-adherence is one of the three primary causes of post-transplant organ failure, along with rejection and infection (Moradi et al., 2019). Treatment adherence is defined by the World Health Organization (WHO) as “the extent to which a patient’s behavior coincides with the clinical prescriptions” (Ahmed and Aslani, 2014).
The prevalence of non-adherence in solid organ transplant recipients has been estimated to be between 15% and 30% in various studies (Mehta et al., 2017). Non-adherence increases the risk for graft loss and post-transplant hospitalizations by about 25% (Takemoto et al., 2007). According to WHO the economic impact of non-adherence in solid organ transplant recipients is estimated to be between 15 and 100 million USD annually (Gorevski et al., 2013). Albekairy et al. Reported about 41% of adult liver transplant recipients were non-adherent to their immunosuppressive treatment (Albekairy et al., 2016).
Different adherence levels measurement method has resulted in a wide range of non-adherence reports. Factors that affect a patient’s non-adherence to their treatment have been mentioned in different studies, including age at the time of transplantation, underlying diseases, education level, marital status, employment status, and income (Mehta et al., 2017; Jones and Serper, 2020).
An important goal after transplantation is to increase the quality of life (QoL) in recipients. WHO defines QoL as “an overall sense of wellbeing, including aspects of happiness and satisfaction with life as a whole”. It includes factors such as mental, physical, and social status (Butt et al., 2012; Burra et al., 2018). Several studies have been published on the relationship between liver transplants and factors affecting QoL in them. According to the studies, male gender, model for end-stage liver disease (MELD) score before transplantation, having a supportive family, and marriage are among the factors that improve QoL after liver transplant (Burra et al., 2018; Jones and Serper, 2020). QoL is also measured using questionnaires. One of the well-known questionnaires is the Short Form 36 (SF-36), which measures different physical, mental, social, and pain factors in varied conditions (Ware, 2000). No studies have been written on the relationship between immunosuppressive medication adherence and QoL in adult liver transplant recipients in Iran. Therefore, the goal of this study has been to evaluate the level of adherence and QoL and the association between these two outcomes in adult liver transplant patients of Shiraz Transplant Center as one of the world’s greatest solid organ transplant centers.
This is a cross-sectional study conducted at the Abu-Ali Sina Transplant Hospital in Shiraz, Iran, affiliated to Shiraz University of Medical Sciences, Iran, from April 2020 to February 2021. The study has been approved by the Shiraz University of Medical Sciences Institutional Review Board (#IR.SUMS.REC.1399.494).
We enrolled liver transplant recipients over the age of 18 years, who received at least one immunosuppressive drug treatment and at least 6 months have been passed after their transplantation. Patients who had received other solid organ transplantation in addition to their liver transplant or went through liver re-transplantation were excluded from the study. The considered 6-month period was to ensure achieving a stable level of immunosuppressive medications as well as stabilizing the patient’s clinical condition. Patient enrolment is briefly described in Figure 1.
We collected and recorded socio-demographic data including age, gender, level of education, employment, economic and marital status and living condition, clinical data including the cause of liver failure, donor type, duration of liver transplantation, comorbidities, underlying diseases, and acute rejection episodes, habitual history data including smoking and drug or alcohol consumption and immunosuppressive regimen and other medications history. These data and evaluation of adherence level and QoL were collected from face-to-face interviews, as well as reviewing medical records stored in the hospital database by two registered nurses trained in the field of transplantation under the supervision of a clinical pharmacist and transplant surgeon.
Adherence level to immunosuppressive medications was assessed in face-to-face interviews using the Basel Assessment of Adherence to Immunosuppressive medication Scale criteria (BAASIS) (Dobbels et al., 2010). This criterion consists of four items related to the use of immunosuppressive drugs such as dimension, timing (drug holiday), dose reduction, and continuity of immunosuppressive medication administration. Responses were given on a six-point scale: every day 5), more than once per week 4), every week 3), every second week 2), once per month 1), and never 0). Any answer other than “never” in each of the four questions was considered non-adherent. It was also recorded if a patient used reminders to take their medications, such as timed pillboxes or calendars.
The quality of life (QoL) level was measured by the short-form (SF-36) questionnaire and was confirmed by face-to-face observations made by trained interviewers when the adherence levels were accessed. SF-36 is created and validated as a standardized short-form instrument for measuring health-related QoL and is commonly used in the Medical Outcomes Study to measure essential QoL domains. The SF-36 consists of eight QoL domains: PF, physical functioning (10 questions); RP, role physical (4 questions); BP, bodily pain (2 questions); GH, general health (5 questions); VT, vitality (5 questions); SF, social functioning (2 questions); RE, role emotional (3 questions); and MH, mental health (5 questions) (Lins and Carvalho, 2016).
The standardized scores for each domain range from 0 to 100, where 0 reflects a diminished QoL. The eight scales are summarized in two scores: Physical Composite Score (PCS) for physical health, and Mental Composite Score (MCS) for mental health. The PCS score includes physical functioning, role physical, pain, and general health scales, and the MCS score comprises role emotion, social function, and scales emotional wellbeing scales. A Persian version has already been prepared and validated based on Iranian demographic norms (Motamed et al., 2005).
We reported categorical data as a percentage and continuous variables as means ± standard deviation (SD). To perform the linear regression analysis with odds ratio (OR) and 95% confidence interval (CI), we used a stepwise method to determine the possible relation of different demographic, socio-economic, cultural, clinical factors, and development of acute rejection episodes with adherence. We selected variables with p-values less than 0.3 for the final multivariate logistic regression model, and we considered p-values less than 0.05 statistically significant. Also, to compare between adherent and non-adherent groups, the mean of answers for all questions and each SF-36 domain were calculated using the linear regression model. All the statistical analyses were performed by Social Science Package Statistical Software (SPSS) version16.
A total of 122 patients were included in the study. The mean age was 43.43 ± 13.57 years, and 70 (57.3%) of them were males. Table 1 shows the demographic, social-economical-cultural, and clinical data of the participants.
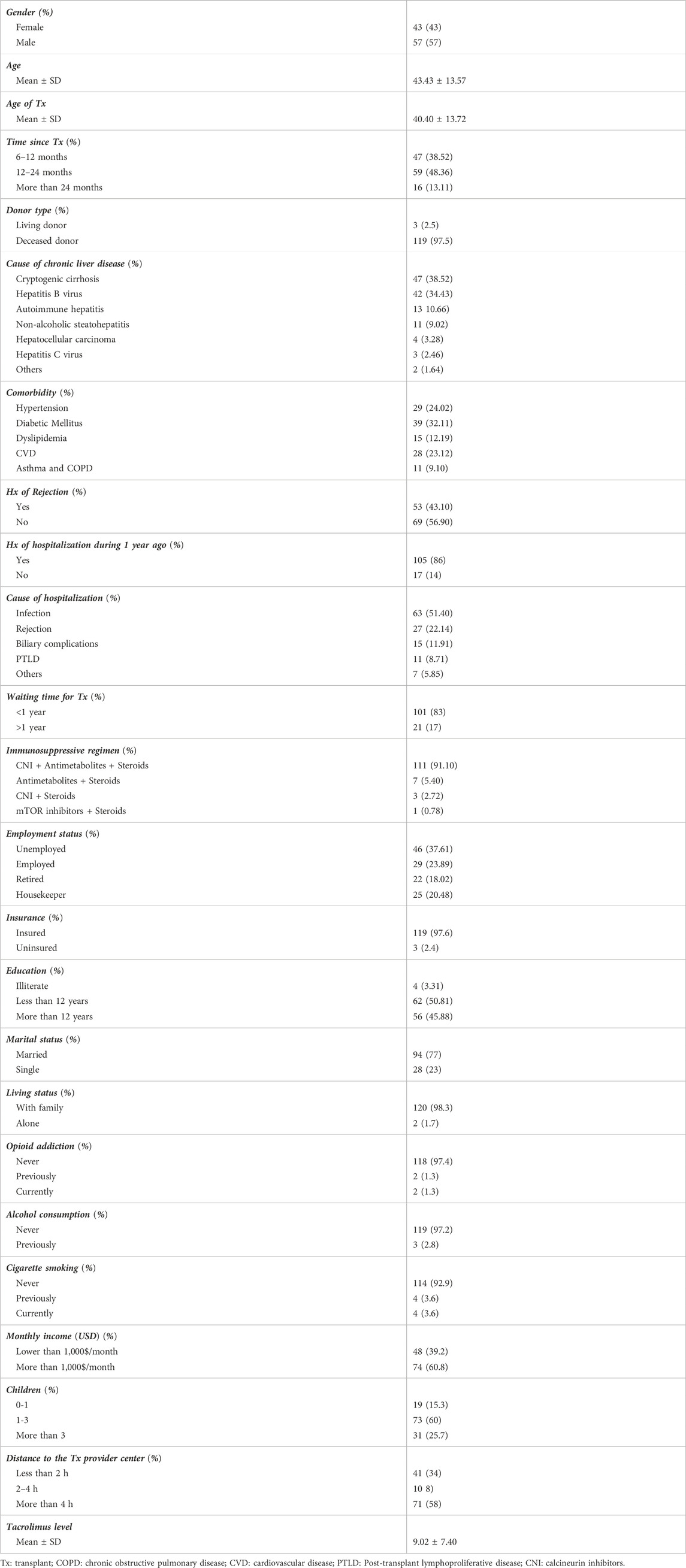
TABLE 1. Demographic, clinical, and social-economical-cultural properties of the liver transplant recipients (N = 122).
The most common indications for liver transplantation were cryptogenic cirrhosis (38.52%), Hepatitis B (34.43%), and autoimmune hepatitis (10.66%). The most important comorbidities were diabetes mellitus (32.11%), hypertension (24.02%), and cardiovascular disease (23.12%). Of the included patients, 96.7% were literate, 23.89% were employed, while 98.3% lived with family and 1.7% lived alone.
History of alcohol or drug use was positive in 2.8% and 2.6% respectively. None of them did mention any continued use of alcohol during the study period, while 1.3% admitted being on opioid drugs in that period. Of the subjects of the study, 48.3% had participated in the study in 12–24 months and 13.11% in more than 2 years after their transplantation. In total, 43.1 percent of patients experienced at least one episode of rejection after liver transplantation. 91.10% of the participants received a triple immunosuppressive regimen including antimetabolite, Calcineurin inhibitor (CNI), and steroids. Among all patients, 41% (50 patients) were categorized in the non-adherent group. The most important reasons for non-adherence in these patients included forgetfulness (62%), lack of medication (12%), financial problems for drug supply (9%), and side effects (2%). The most common causes of drug holiday were:COVID-19 infection and discontinuation of several concurrent doses, in spite that there has been no presciptions for discontinuation. Forgetfulness and Travel and limited access to enough amounts of the medications.
Table 2 shows the relationship between quantitative and qualitative risk factors and the occurrence of non-adherence. Patients’ age, age of transplant, income level, history of hospitalization, and transplant rejection were among the main factors impacting non-adherence. Of those factors, according to the results of the multivariate linear regression model, rejection was the only influential factor in the occurrence of non-adherence among patients (OR = 8.226 CI(1.404-48.196)).
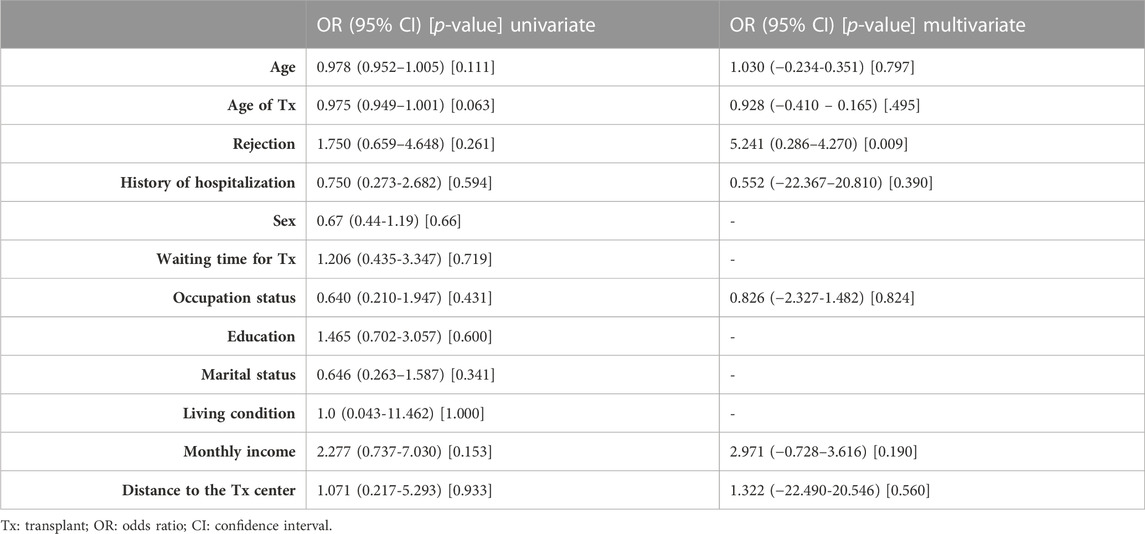
TABLE 2. Quantitative and qualitative risk factors regarding adherence among the liver transplant recipients (N = 122).
The overall mean QoL score of patients was reported 51.09 ± 21.86. Accordingly, the lowest score is given to social functioning, while mental health has achieved the highest score (Table 3). The mean QoL scores in different dimensions in patients with adherence were higher than non-adherents, which was only significant in mental health (p-value = 0.01). Additionally, in total scores related to PSC and MCS, the mean MSC scores in adherent patients were significantly higher than non-adherent patients (p-value: 0.02).
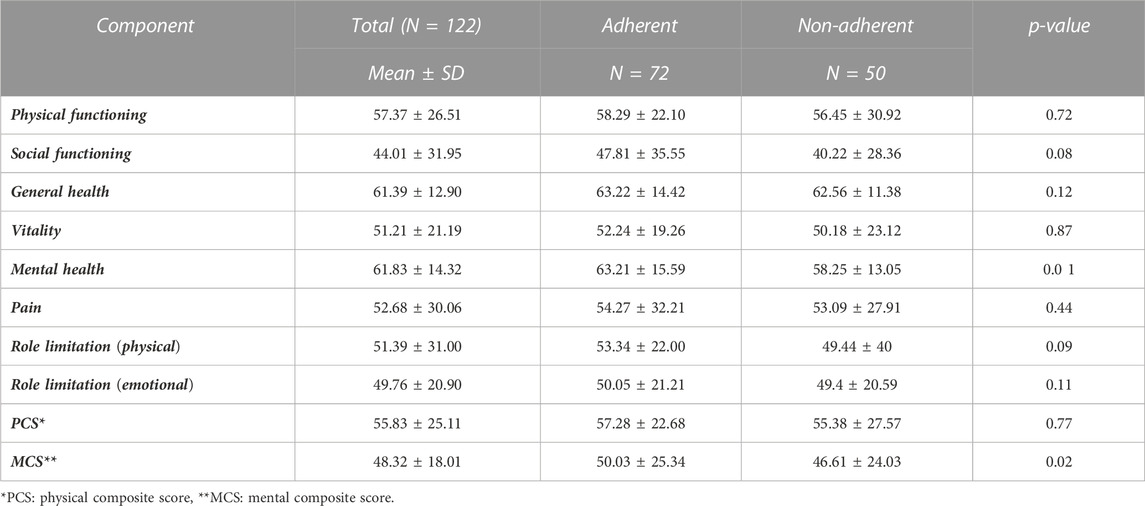
TABLE 3. Different components of quality of life between adherent and non-adherent liver transplant recipients (N = 122).
Based on the results of Table 4, which evaluated the relationship between quantitative and qualitative variables affecting the total score of QoL, the only meaningful effect on QoL total score was of income level. Although adherent patients have an overall greater QoL compared with the others, the differences are not statistically significant.
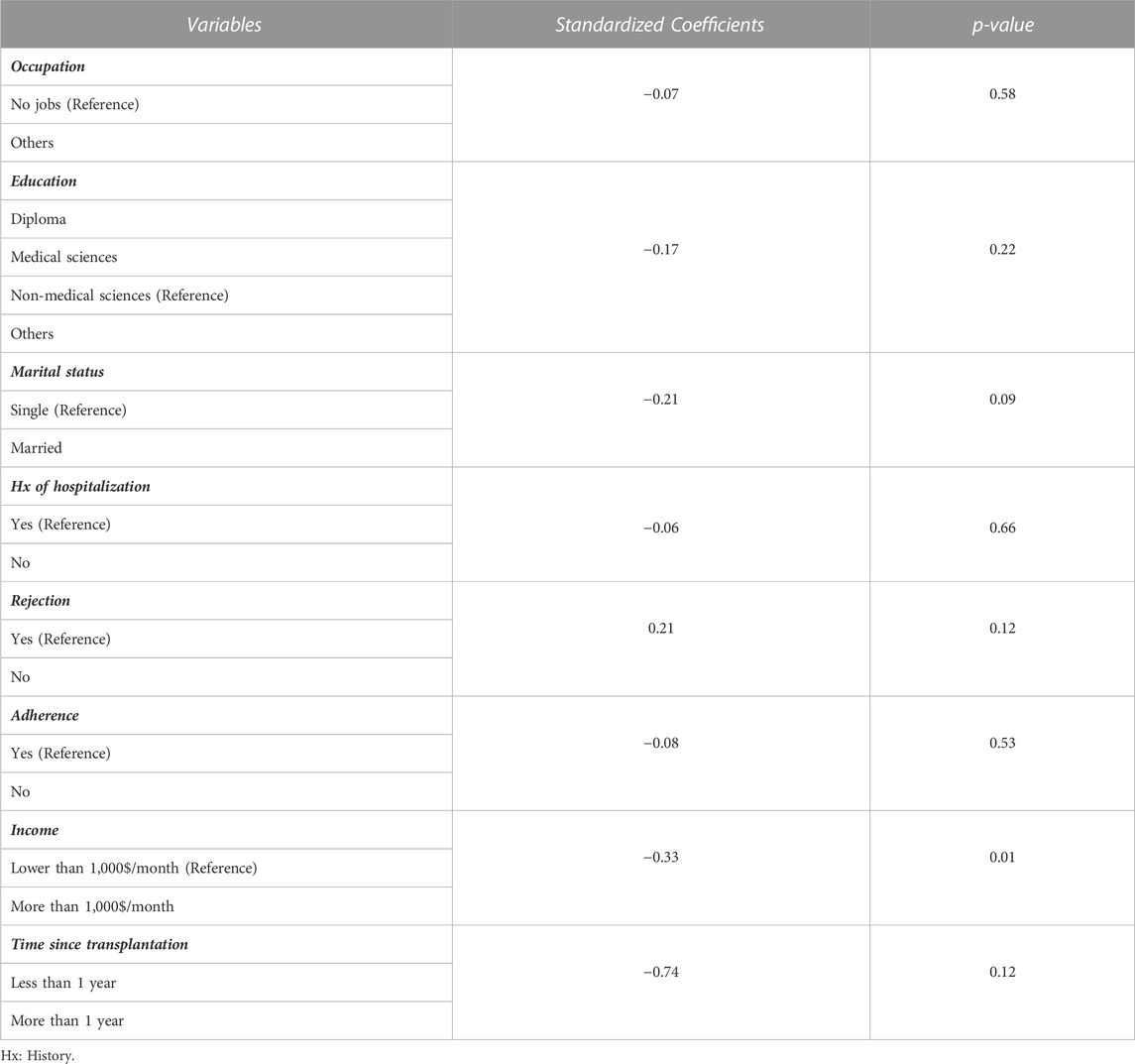
TABLE 4. Different demographic, socio-economic, cultural, and clinical factors concerning the quality of life among liver transplant recipients.
Adherence to immunosuppressive drugs is one of the most critical factors in the success of the organ transplant process. On the other hand, one of the most important issues, which is often one of the main goals of the transplant process, is to improve the QoL after organ transplantation. This study aimed to determine the relationship between patients’ adherence to immunosuppressive drugs and QoL levels after liver transplantation, following similar earlier on kidney transplantation (Ganjali et al., 2019; Moradi et al., 2019). The non-adherence rate in our study was 41%. In some other studies on liver transplant patients, different ranges such as 32%–50.8% have been reported for non-adherence levels (Serper et al., 2015; Leven et al., 2017). One of the most important factors explaining this wide range of reported levels is the different methods used for adherence evaluation. For example, in our study, the measurement was based on the BAASIS method, while in the study of Serper et al., the plasma level of Tacrolimus was used as an adherence criterion (Serper et al., 2015). Therefore, due to the difference in measurement methods, diverse studies are not easily compared. Moreover, to name another causing factor, the time elapsed from the transplantation is effective on adherence as well. It has been shown that the more time passes from the transplantation, the less is that particular patient’s adherence. Thus, considering the heterogeneity of diverse studies with different study group populations and times elapsed since the transplantations, this wide range is expectable.
Patient forgetfulness was the most important cause of non-adherence in our study. In addition, the lack of medications was another major cause of non-adherence. Noteworthy, in the study of Moradi et al. and Cossart et al., forgetfulness has been considered the most important cause of non-adherence as well (Cossart et al., 2019; Moradi et al., 2019). Due to the dependence of Iran’s pharmaceutical industry on imported raw materials to supply the pharmaceutical industry and the existence of international sanctions against trade with Iran in the past decade, there are shortages of immunosuppressive medications at times (Setayesh and Mackey, 2016), explaining the second cause of non-adherence among the patients in our study.
History of re-hospitalization, history of rejection, younger age at the time of transplantation, low income, and unemployment were among the risk factors affecting non-adherence in univariate analysis. Ultimately, the history of rejection is calculated to be the only factor influencing the incidence of non-adherence in our study. In some studies, ages less than 40 years, psychiatric disorders, immunosuppressive side effects, and having beliefs that medications were harmful have been among the risk factors for non-adherence (Ghods et al., 2003; Drent et al., 2009). In the study of Ghods et al. (Ghods et al., 2003), which examined the risk factors for non-compliance among kidney transplant patients, the number of transplant rejections was one of the factors affecting non-adherent incidence.
Our study’s average total QoL score was about 51, which is much lower than the average QoL score reported in developed countries among adult liver transplant recipients. Fredericks et al. reported a total QoL score of close to 60.3, also in a study by Masala et al., it was estimated to be 63 (Fredericks et al., 2008; Masala et al., 2012). Different methods for measuring QoL and the dissimilarity between the average time elapsed since the time of transplantation between diverse studies have led to an unalike range for the average QoL in distinct studies, making comparisons between these studies more difficult. In this regard, some studies believe that QoL of liver transplant patients has an upward trend in the first 6 months after transplantation. However, in long-term follow-ups (5 years and 10 years), the upward trend has stopped, and over time since the transplant, QoL takes a decreasing trend (Telles-Correia et al., 2009; Burra and Germani, 2013). In conclusion, the factor of time elapsed after transplantation can be an essential influencer in comparing QoL measurements between different studies.
Based on our data, patients with poor psychological scores in the study period were the most non-adherent. However, there is no visible cause and effect association in this manner. In other words, it is still unclear whether non-adherence has caused a lower score in psychological factors, or it is psychological factors affecting the trend of patients to non-adherence. It is also possible for these factors to induce a positive loop for each other, as if, non-adherent patients will become less emotionally stable, which might cause more non-adherence in this population. Additionally, as mentioned earlier, there are limitations in Iran for these patients to freely access the desired medications, such as lower income or unavailable medications in the market. Such obstacles might induce both psychological distress and non-adherence trends, without any needed causal effect between the two.
While studies have mentioned the impacts of pre-transplant depression in non-adherence of liver and kidney transplant recipients (Scheel et al., 2018; Golfieri et al., 2019), they have suggested the positive impact of psychological interventions in adherence. It is also noticeable that in some studies, poor psychological scores before transplantation did not significantly modify patient adherence to immunosuppressive regimens when compared with psychologically stable patients (Michaud et al., 2016). This suggests further attention to considering the causal relationship between non-adherence and poor psychological scores. However, a major challenge in assessing post-transplant patients is the small size of study groups in many studies, including ours.
Our data suggest that the adherent patients have a higher overall QoL score, which is statistically significant in mental factors. Yet, differentiating QoL-affecting factors from adherence-affecting factors is not an easy task, as most of them such as age, the time elapsed after the transplantation, pre-transplant psychological status, and similar ones are common in both. Some of the prior studies indicate that the most adherent patients had lower complications such as organ rejection. Hence, they experience fewer re-hospitalizations, both in frequency and in duration, improving their QoL. Also, it has been reported that the patients who had spent more time on an organ waiting list had poorer QoL and adherence due to depression (Santos et al., 2012; Benzing et al., 2016). Our center is more focused on cadaver organs than living donors, which would result in more waiting time for most of the patients in this study, affecting the QoL and adherence after transplantation. This should be considered in further studies that these patients are more likely to suffer from post-transplant depression and lower QoL scores. What was shown in this study is that the only factor that significantly affected QoL total score has been income level. Although poor scores in multiple factors such as adherence, job status, re-hospitalization, and education level have resulted in lower overall QoL scores in the patients, the difference has not been statistically significant. Hence, it is challenging to draw the causal link between QoL and adherence as well. It is interesting that normally it is assumed that a higher patient survival rate as a result of higher adherence leads to higher QoL, which might not be true in all situations. In a study regarding HIV patients, it was surprisingly concluded that not always higher adherence would result in higher overall QoL (Geocze et al., 2010). The authors further explained that patients with the highest levels of adherence would suffer more from the side effects of their HAART medications. In other words, although these patients survived more than the average, their QoL was lower. The same conclusion may be expected in liver transplant patients as their immunosuppressive medication too can induce severe side effects as do HAART medications. However, such interpretations need to be further investigated in larger study groups considering multiple factors such as self-care, which was not included in our study. The authors suggested a more convenient medication regimen that induces less interference with daily activities would increase the QoL scores in HIV/AIDS patients, which can be generalized to other chronic conditions such as liver transplant recipients.
In conclusion, it seems that QoL is a multifactorial outcome, with such diverse and interacting affecting components. While our data suggest a statistically significant relationship between forgetfulness and income level with adherence and overall QoL scores, respectively, policymakers and researchers should not view these two factors in an oversimplified manner. In order to achieve a better QoL, there must be multiple support systems for the patients, including better access to suitable medications, psychological supports, educational devices, and a reliable system for the patients to ask for help.
Our results have to be thoroughly evaluated prior to being used in any policymaking, as this study is challenged by some limitations. Some studies have mentioned that using extended or sustained released forms of some immunosuppressive medications, such as Tacrolimus, can help improve patients’ adherence (Beckebaum et al., 2011). As this particular dosage form is not available in our country, it was impossible to assess its effects on patient adherence in this study. Another limitation of this study is the subject group size and it being single-center. The limited group size was due to the decrease in physical visits of the patients during COVID-19 lockouts. In order to establish a firm decision on the effects of QoL on adherence and vice versa, larger multi-central studies must be performed.
Non-adherence is calculated to be 41% in the subjects of this study, for which the main influencing factors were forgetfulness, drug shortages, and economic difficulties for medication provision. The overall QoL score has been in all parameters higher in the adherent group compared with non-adherent patients. The difference in QoL was most meaningfully significant in mental composite score among other parameters of QoL.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Shiraz University of Medical Sciences (#IR.SUMS.REC.1399.494). The patients/participants provided their written informed consent to participate in this study.
All authors contributed to the study’s conception and design. Data collection and interviews were performed by TT, SHN, SN, EH, and MH. Data were analyzed by EH, MSH, and MD. The first draft of the manuscript was written by ZT, FH, MH, and MD All authors have read and approved the final manuscript.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
The authors would like to thank Shiraz University of Medical Science, Shiraz, Iran.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ahmed, R., and Aslani, P. (2014). What is patient adherence? A terminology overview. Int. J. Clin. Pharm. 36, 4–7. doi:10.1007/s11096-013-9856-y
Albekairy, A. M., Alkatheri, A. M., Jarab, A., Khalidi, N., Althiab, K., Alshaya, A., et al. (2016). Adherence and treatment satisfaction in liver transplant recipients. Saudi J. Gastroenterol. 22, 127–132. doi:10.4103/1319-3767.164209
Beckebaum, S., Iacob, S., Sweid, D., Sotiropoulos, G. C., Saner, F., Kaiser, G., et al. (2011). Efficacy, safety, and immunosuppressant adherence in stable liver transplant patients converted from a twice-daily tacrolimus-based regimen to once-daily tacrolimus extended-release formulation. Transpl. Int. 24, 666–675. doi:10.1111/j.1432-2277.2011.01254.x
Benzing, C., Krezdorn, N., Förster, J., Hinz, A., Krenzien, F., Atanasov, G., et al. (2016). Health-related quality of life and affective status in liver transplant recipients and patients on the waiting list with low MELD scores. Hpb 18, 449–455. doi:10.1016/j.hpb.2016.01.546
Burra, P., Ferrarese, A., and Feltrin, G. (2018). Quality of life and adherence in liver transplant recipients. Minerva Gastroenterol. Dietol. 64, 180–186. doi:10.23736/S1121-421X.17.02459-X
Burra, P., and Germani, G. (2013). Long-term quality of life for transplant recipients. Liver Transpl. 19, S40–S43. doi:10.1002/lt.23725
Butt, Z., Parikh, N. D., Skaro, A. I., Ladner, D., and Cella, D. (2012). Quality of life, risk assessment, and safety research in liver transplantation: New frontiers in health services and outcomes research. Curr. Opin. Organ Transpl. 17, 241–247. doi:10.1097/MOT.0b013e32835365c6
Cossart, A. R., Staatz, C. E., Campbell, S. B., Isbel, N. M., and Cottrell, W. N. (2019). Investigating barriers to immunosuppressant medication adherence in renal transplant patients. Nephrology 24, 102–110. doi:10.1111/nep.13214
Dobbels, F., Berben, L., De Geest, S., Drent, G., Lennerling, A., Whittaker, C., et al. (2010). The psychometric properties and practicability of self-report instruments to identify medication nonadherence in adult transplant patients: A systematic review. Transplantation 90, 205–219. doi:10.1097/TP.0b013e3181e346cd
Drent, G., De Geest, S., Dobbels, F., Kleibeuker, J. H., and Haagsma, E. B. (2009). Symptom experience, nonadherence and quality of life in adult liver transplant recipients. Neth. J. Med. 67, 161–168.
Fredericks, E. M., Magee, J. C., Opipari-Arrigan, L., Shieck, V., Well, A., and Lopez, M. J. (2008). Adherence and health-related quality of life in adolescent liver transplant recipients. Pediatr. Transpl. 12, 289–299. doi:10.1111/j.1399-3046.2008.00901.x
Ganjali, R., Ghorban Sabbagh, M., Nazemiyan, F., Mamdouhi, F., Badiee Aval, S., Taherzadeh, Z., et al. (2019). Factors associated with adherence to immunosuppressive therapy and barriers in asian kidney transplant recipients. ImmunoTargets Ther. 8, 53–62. doi:10.2147/itt.s212760<
Geocze, L., Mucci, S., de Marco, M. A., Nogueira-Martins, L. A., and de Albuquerque Citero, V. (2010). Quality of life and adherence to HAART in HIV-infected patients. Rev. Saude Publica 44, 743–749. doi:10.1590/s0034-89102010000400019
Ghods, A. J., Nasrollahzadeh, D., and Argani, H. (2003). Risk factors for noncompliance to immunosuppressive medications in renal transplant recipients. Transplant. Proc. 35, 2609–2611. doi:10.1016/j.transproceed.2003.09.047
Golfieri, L., Gitto, S., Vukotic, R., Andreone, P., Marra, F., Morelli, M. C., et al. (2019). Impact of psychosocial status on liver transplant process. Ann. Hepatol. 18, 804–809. doi:10.1016/j.aohep.2019.06.011
Gorevski, E., Succop, P., Sachdeva, J., Cavanaugh, T. M., Volek, P., Heaton, P., et al. (2013). Is there an association between immunosuppressant therapy medication adherence and depression, quality of life, and personality traits in the kidney and liver transplant population? Patient prefer. Adherence 7, 301–307. doi:10.2147/PPA.S34945
Jones, L. S., and Serper, M. (2020). Medication non-adherence among liver transplant recipients. Curr. Hepatol. Rep. 19, 327–336. doi:10.1007/s11901-020-00545-7
Leven, E. A., Annunziato, R., Helcer, J., Lieber, S. R., Knight, C. S., Wlodarkiewicz, C., et al. (2017). Medication adherence and rejection rates in older vs younger adult liver transplant recipients. Clin. Transpl. 31, e12981. doi:10.1111/ctr.12981
Lins, L., and Carvalho, F. M. (2016). SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 4, 205031211667172. doi:10.1177/2050312116671725
Malek-Hosseini, S. A., Habibzadeh, F., and Nikeghbalian, S. (2019). Shiraz organ transplant center: The largest liver transplant center in the world. Transplantation 103, 1523–1525. doi:10.1097/TP.0000000000002581
Masala, D., Mannocci, A., Unim, B., Del Cimmuto, A., Turchetta, F., Gatto, G., et al. (2012). Quality of life and physical activity in liver transplantation patients: Results of a case-control study in Italy. Transpl. Proc. 44, 1346–1350. doi:10.1016/j.transproceed.2012.01.123
Mehta, P., Steinberg, E. A., Kelly, S. L., Buchanan, C., and Rawlinson, A. R. (2017). Medication adherence among adolescent solid-organ transplant recipients: A survey of healthcare providers. Pediatr. Transpl. 21, e13018. doi:10.1111/petr.13018
Michaud, L., Ludwig, G., Berney, S., Rodrigues, S., Niquille, A., Santschi, V., et al. (2016). Immunosuppressive therapy after solid-organ transplantation: Does the intermed identify patients at risk of poor adherence? Pharm. Pract. (Granada) 14, 822. doi:10.18549/PharmPract.2016.04.822
Moradi, O., Karimzadeh, I., Davani-Davari, D., Shafiekhani, M., and Sagheb, M. M. (2019). Pattern and associated factors of adherence to immunosuppressive medications in kidney transplant recipients at a referral center in Iran. Patient Prefer Adherence 13, 729–738. doi:10.2147/PPA.S198967
Motamed, N., Ayatollahi, A. R., Zare, N., and Sadeghi-Hassanabadi, A. (2005). Validity and reliability of the Persian translation of the SF-36 version 2 questionnaire. East. Mediterr. heal. J. 11, 349–357.
Santos, G. G., Gonçalves, L. C., Buzzo, N., Mendes, T. A., Dias, T. P., da Silva, R. C., et al. (2012). Quality of life, depression, and psychosocial characteristics of patients awaiting liver transplants. Transpl. Proc. 44, 2413–2415. doi:10.1016/j.transproceed.2012.07.046
Scheel, J. F., Schieber, K., Reber, S., Stoessel, L., Waldmann, E., Jank, S., et al. (2018). Psychosocial variables associated with immunosuppressive medication non-adherence after renal transplantation. Front. Psychiatry 9, 23. doi:10.3389/fpsyt.2018.00023
Serper, M., Patzer, R. E., Reese, P. P., Przytula, K., Koval, R., Ladner, D. P., et al. (2015). Medication misuse, nonadherence, and clinical outcomes among liver transplant recipients. Liver Transpl. 21, 22–28. doi:10.1002/lt.24023
Setayesh, S., and Mackey, T. K. (2016). Addressing the impact of economic sanctions on Iranian drug shortages in the joint comprehensive plan of action: Promoting access to medicines and health diplomacy. Glob. Health 12, 31. doi:10.1186/s12992-016-0168-6
Takemoto, S. K., Pinsky, B. W., Schnitzler, M. A., Lentine, K. L., Willoughby, L. M., Burroughs, T. E., et al. (2007). A retrospective analysis of immunosuppression compliance, dose reduction and discontinuation in kidney transplant recipients. Am. J. Transpl. 7, 2704–2711. doi:10.1111/j.1600-6143.2007.01966.x
Telles-Correia, D., Barbosa, A., Mega, I., Mateus, E., and Monteiro, E. (2009). When does quality of life improve after liver transplantation? A longitudinal prospective study. Transpl. Proc. 41, 904–905. doi:10.1016/j.transproceed.2009.01.051
UNOS (2021). Organ transplant trends | More transplants than ever | UNOS. Available at: https://unos.org/data/transplant-trends/(Accessed December 24, 2021).
Keywords: solid organ transplantation, quality of life, adherence, immunosuppressive medication, liver transplantation
Citation: Shafiekhani M, Shahabinezhad F, Tavakoli Z, Tarakmeh T, Haem E, Sari N, Nasirabadi S and Dehghani M (2023) Quality of life associated with immunosuppressant treatment adherence in liver transplant recipients: A cross-sectional study. Front. Pharmacol. 14:1051350. doi: 10.3389/fphar.2023.1051350
Received: 22 September 2022; Accepted: 13 February 2023;
Published: 24 February 2023.
Edited by:
Wenji Li, Yangzhou University, ChinaReviewed by:
Godfrey Mutashambara Rwegerera, University of Botswana, BotswanaCopyright © 2023 Shafiekhani, Shahabinezhad, Tavakoli, Tarakmeh, Haem, Sari, Nasirabadi and Dehghani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masoud Dehghani, ZGVoZ2hhbmlnaEBzdW1zLmFjLmly
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.