- 1Department of Anesthesiology, The Second Affiliated Hospital of Jiaxing University, Jiaxing, China
- 2Department of Anesthesiology, Women and Children’s Hospital of Jiaxing University, Jiaxing, China
Background: Emergency agitation is a common postoperative complication in pediatric patients after general anesthesia. The aim of this study was to explore the effects of a low dose of esketamine on emergency agitation in children following tonsillectomy.
Materials and Methods: Eighty children were recruited prospectively to this study and divided into the esketamine group and the control group (40 cases in each group). The induction and maintenance of anesthesia were the same in both groups. At the end of surgery, the esketamine group received 0.25 μg/kg esketamine, while the control group received the same volume of normal saline. The extubation time, time to eye opening, Ramsay sedation scale and time to discharge from the post-anesthesia care unit (PACU) were recorded during post-anesthesia care unit. Postoperative complications, such as emergency agitation, respiratory depression, hypertension, tachycardia, nightmares, nausea, and vomiting, were also recorded.
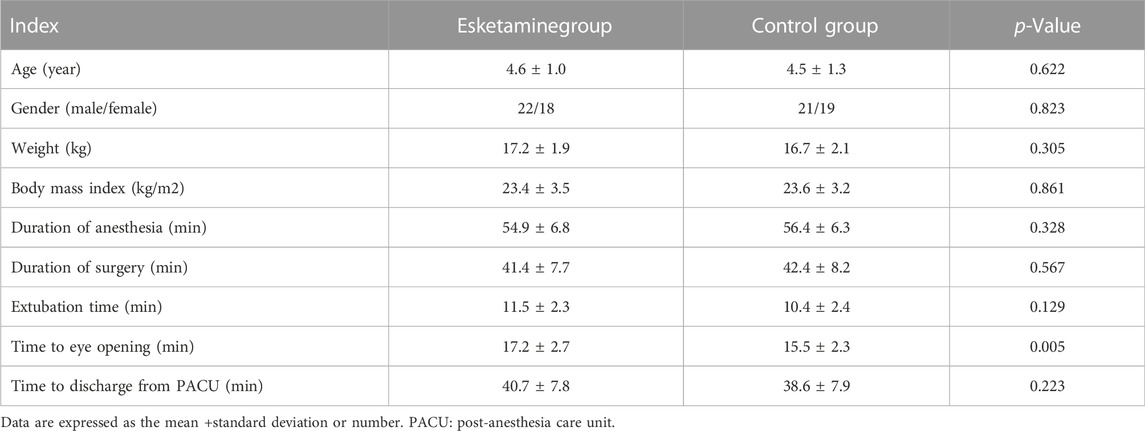
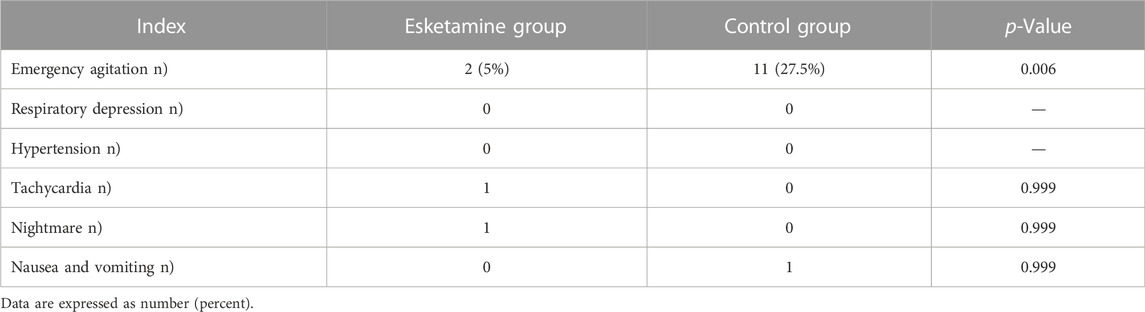
Results: The incidence of emergency agitation was lower in the esketamine group compared with that in the control group (5% vs. 27.5%, p = 0.006). The time to eye opening was longer in the esketamine group than in the control group (17.2 ± 2.7 vs. 15.5 ± 2.3 min, p = 0.005). However, the extubation time and time to discharge from PACU were similar between the two groups.
Conclusion: Low-dose of esketamine decreases the incidence of emergency agitation in children after tonsillectomy without delaying extubation time and increasing the postoperative side effects. (www.chictr.org.cn, registration number: ChiCTR2100054178).
1 Introduction
Emergence agitation is a well-known phenomenon in children after general anesthesia, (Mohkamkar et al., 2014; Cao et al., 2016), especially in those undergoing adenotonsillectomy. (Fattahi-Saravi et al., 2021). The incidence of emergence agitation varies from 0.25% to 90.5%. (Lee and Sung, 2020). Emergence agitation might cause injury, accidental removal of intravenous cannulation, self-extubation, post-operative wound bleeding, and increase the nursing requirements in the post-anesthesia care unit (PACU).. (Zhu et al., 2021).
Intravenous administration of a subhypnotic dose of midazolam, propofol, and ketamine combined with fentanyl is usually performed to decrease the incidence of emergence agitation in children undergoing sevoflurane anesthesia. (Chen et al., 2010). Although intravenous administration of fentanyl at the end of surgery could reduce the incidence of emergence agitation in children undergoing general anesthesia, it was associated with a prolonged PACU stay and an increased incidence of postoperative nausea or vomiting. (Kim et al., 2017). The literature reported that dexmedetomidine decreased the incidence of emergence agitation in children after general anesthesia, but it was accompanied by delayed extubation time. (Yang et al., 2020).
Ketamine is an antagonist of the N-methyl-d-aspartate receptor. In recent years, it has been used widely in clinical anesthesia, pain management, and resistant depression. (Frey et al., 2019; Salloum et al., 2019). Esketamine is a more potent S-isomer of ketamine. Its potency is approximately two times higher than that of ketamine, but with fewer side effects. (Jonkman et al., 2018; Wang et al., 2019). Moreover, esketamine offers a shorter recovery time and orientation recovery time compared with ketamine. (Wang et al., 2019). To date, there have been no studies on the use of esketamine to prevent emergency agitation. Therefore, the present study aimed to investigate the efficacy of esketamine in reducing emergency agitation in children undergoing tonsillectomy.
2 Materials and methods
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethical Committee of the Jiaxing Children’s Hospital (approval number: 201836, Chairman: Prof L. Xia). Written informed consent was obtained from the guardians of the children (www.chictr.org.cn, registration number: ChiCTR2100054178).
From 1 December 2021 to 1 March 2022, a total of 80 children undergoing tonsillectomy with American Society of Anesthesiologists (ASA) stage I–II, weighing between 10 and 50 kg, and aged from 2 to 7 years were included this study. Children with cardiovascular diseases, psychosis, or mental diseases were excluded. The children were randomly divided into the control group and the esketamine group (40 cases in each group). The investigators, anesthesiologists, surgeons, and nurses were blinded to the group allocation.
The children, who did not receive premedication, were fasted for 8 h. After entering the operating center, venous access was established. The electrocardiogram, pulse oxygen saturation (SPO2), non-invasive blood pressure, and heart rate (HR) were monitored. Anesthesia was induced using intravenous fentanyl at 3 μg/kg, propofol at 3 mg/kg, and cis-atracurium at 0.12 mg/kg. Endotracheal intubation was performed under direct laryngoscopy. Subsequently, the lungs were ventilated in the pressure-controlled ventilation mode. The ventilation parameters were set as follows: a driving pressure of 15–18 cmH2O, a breathing rate of 14–20 breaths/min, an oxygen flow rate of 2 L/min, a fraction of inspired oxygen of 0.5, an inspiratory expiratory ratio of 1:1.5, and a positive end-expiratory pressure of zero.
The driving pressure was adjusted to keep the end-tidal carbon dioxide partial pressure (PETCO2) between 35 and 45 mmHg. Anesthesia was maintained using 2%–4% sevoflurane to keep the systolic blood pressure within a 20% range of baseline. Anesthetics were stopped 5 min before the end of surgery. The esketamine group received 0.25 mg/kg esketamine (Jiangsu Hengrui pharmaceutical company, Jiangsu, China) at the end of surgery and the control group received the same volume of normal saline, after which all the children were transferred to the PACU. These medications were prepared by nurses who were blinded to the grouping.
The systolic blood pressure (SBP), diastolic blood pressure (DBP), and HR were recorded at 3 min after drug administration. The extubation time, time to eye opening, Ramsay sedation scale (RSS) in the PACU, and time to discharge from the PACU were also noted. The adverse events (emergency agitation, respiratory depression, tachycardia, hypotension, nightmares, nausea, and vomiting) were recorded. The endotracheal tube was extubated when the tidal volumes were >6 ml/kg, SPO2 was >96%, and PETCO2 was <45 mmHg during air inhalation. The standards of discharge from the PACU were as follows: a. Awake. b. Air breathing SpO2 > 94%. c. Moving the arms, legs, and head with commands. d. Breathing with a normal respiratory rate. Respiratory depression was defined as SpO2 < 94% whilst receiving oxygen and a breathing rate <10 times per minute. Hypertension was defined as an SBP above 20% from the baseline values and tachycardia was defined as an HR above 20% from the baseline values. The children were given 1 mg/kg propofol by intravenous injection if emergency agitation occurred.
The level of sedation was assessed using the Ramsay sedation scale (RSS) (1, patients were anxious, agitated, or restless, or both. 2, patients were cooperative, oriented, and tranquil. 3, patients responded to commands only. 4, patients were asleep but had a brisk response to a light glabellar tap or loud auditory stimulus. 5, patients were asleep with a sluggish response to a light glabellar tap or loud auditory stimulus. 6, patients were asleep and not responsive). Emergency agitation was defined as an RSS value of 1.
2.1 Statistical analysis
In this study, the primary outcome was the incidence of emergency agitation. A priori power analysis using two-sided analysis with an α error of 0.05 and a power of 0.8 showed that 32 patients were needed to detect a statistical difference in the incidence of emergency agitation between the two groups for this study. The sample size was increased to 40 to allow for dropout in each group. Data analysis was performed with the SPSS 20.0 statistical software (IBM Corp., Armonk, NY, United States). Data are presented as the mean ± standard deviation. Comparison of the numerical variables between the two groups was performed using a t-test for independent samples. The categorical data were compared using a Chi-squared test or Fisher’s exact test. p-values <0.05 were considered statistically significant.
3 Results
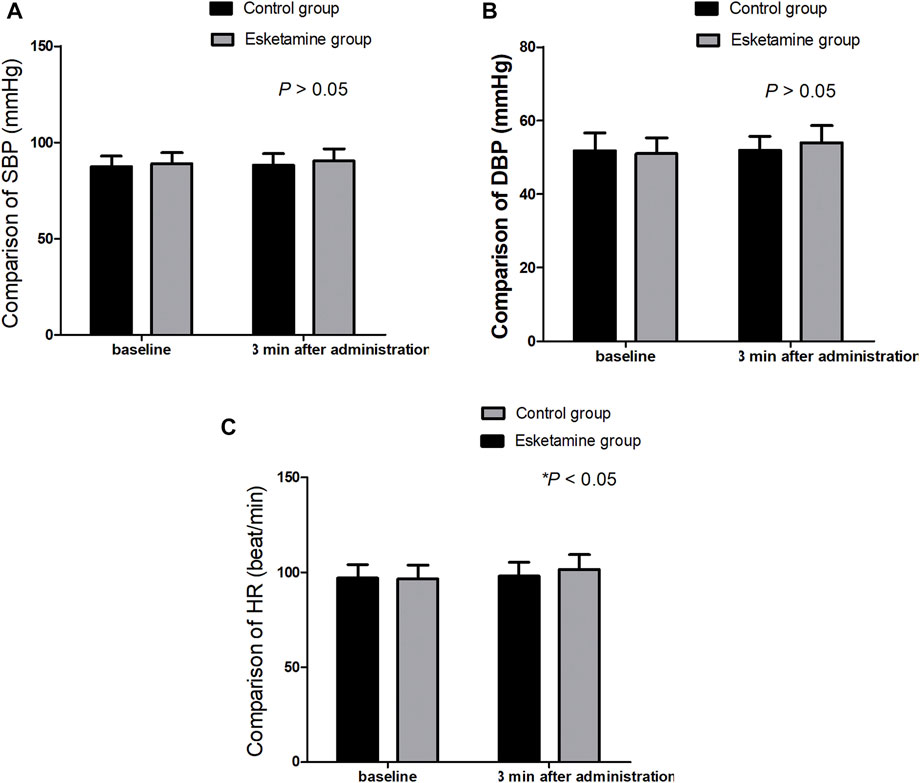
A total of 80 children were enrolled in this trial (Figure 1). There were no significant differences in terms of the age, sex, weight, body mass index, duration of operation, and duration of anesthesia between the two groups (p > 0.05) (Table 1). The extubation time and time to discharge from the PACU were similar between the two groups (p > 0.05); however, the time to eye opening was longer in the esketamine group than in the control group (17.2 ± 2.7 vs.15.5 ± 2.3 min, p = 0.005) (Table 1). The SBP and DBP at 3 min after drug administration were similar between the two groups (p > 0.05); however, the HR at 3 min after drug administration was greater in the esketamine group than in the control group (p = 0.042) (Figure 2).
There were two case of emergency agitation in the esketamine group, while 11 cases of emergency agitation were reported in the control group (5% vs. 27.5%, p = 0.006). There were no statistical differences in the incidence of respiratory depression, hypotension, tachycardia, nightmare, nausea, and vomiting between the two groups (p > 0.05) (Table 2).
4 Discussion
This study showed that low-dose esketamine reduced the incidence of emergency agitation in children after tonsillectomy without delaying extubation time and increasing postoperative side effects.
Esketamine can produce an analgesic effect by activating the N-methyl-d-aspartate (NMDA) receptor. (Jonkman et al., 2018). In the present study, the incidence of emergency agitation in the PACU was lower in the esketamine group than in the control group. There are many factors related to emergency agitation in patients undergoing general anesthesia, including the use of inhalation anesthetics, rapid recovery, type of surgical procedure, postoperative pain, hypoxia, and airway obstruction. (Kim et al., 2015; Wei et al., 2021). Postoperative pain or discomfort is the main factor in emergency agitation. (Zhong et al., 2018). Esketamine could provide long-term sedation and analgesia, and good sedation and analgesic effects could decrease the incidence of emergency agitation in children after tonsillectomy. Chen, et al. (Chen et al., 2010) reported that low doses of midazolam-fentanyl or propofol-fentanyl were both effective to decrease the incidence of emergency agitation in children undergoing cataract extraction after general anesthesia, without significantly delaying recovery time and time to PACU discharge. Lee, et al. (Lee et al., 2010) found that ketamine was decreased the incidence of emergency agitation in children undergoing tonsillectomy and adenoidectomy after sevoflurane general anesthesia without increasing the extubation time and delivery time from the PACU. Their findings agreed with those of the present study. Ni, et al. (Ni et al., 2015) reported that intravenous dexmedetomidine significantly reduced the incidence of emergency agitation; however, it increased the time to eye-opening and the time to discharge from the PACU.
In the present study, the extubation time and time to discharge from the PACU were similar between the two groups; however, the time to eye opening was longer in the esketamine group compared with that in the control group. A study reported that esketamine countered opioid-induced respiratory depression, (Jonkman et al., 2018), and the clinical dose of esketamine did not cause respiratory depression; therefore, it did not result in prolongation of the extubation time. Low-dose esketamine did not result in extension of the time to discharge from the PACU. This effect was dose-dependent and a high dose of esketamine led to delayed time to PACU discharge. In this study, we found that esketamine increased the time to eye opening, which was associated with the anesthetic effect of esketamine.
No significant differences were observed in the incidence of respiratory depression, hypertension, tachycardia, nightmares, nausea, and vomiting between the two groups in the present study. Hypertension, tachycardia, and nightmares are common side effects of esketamine administration. Low-dose esketamine did not increase the incidence of these side effects. In our study, low-dose esketamine (0.25 mg/kg) did not affect the blood pressure, but led to HR increases (p < 0.05).
4.1 Limitations
Nightmares cannot be assessed accurately in children. Furthermore, a large sample study is needed to investigate the side effects of esketamine.
5 Conclusion
This study indicated that low-dose esketamine reduced the incidence of emergency agitation in children undergoing tonsillectomy without delaying extubation time and increasing the postoperative side effects.
Data Availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethical Committee of the Jiaxing Children’s Hospital. Written informed consent to participate in this study was provided by the participant’s legal guardian/next of kin.
Author contributions
Study design and data analysis: QL, JF and WZ. Patient recruitment and data collection: QL. Writing of the paper: WZ.
Acknowledgments
We would like to thank our colleagues for their valuable contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Cao, J. L., Pei, Y. P., Wei, J. Q., and Zhang, Y. Y. (2016). Effects of intraoperative dexmedetomidine with intravenous anesthesia on postoperative emergence agitation/delirium in pediatric patients undergoing tonsillectomy with or without adenoidectomy: A CONSORT-prospective, randomized, controlled clinical trial. Med. Baltim. 95 (49), e5566. doi:10.1097/MD.0000000000005566
Chen, J., Li, W., Hu, X., and Wang, D. (2010). Emergence agitation after cataract surgery in children: A comparison of midazolam, propofol and ketamine. Paediatr. Anaesth. 20 (9), 873–879. doi:10.1111/j.1460-9592.2010.03375.x
Fattahi-Saravi, Z., Jouybar, R., Haghighat, R., and Asmarian, N. (2021). Comparison of the effect of ketamine, ketamine-midazolam and ketamine-propofol on post-tonsillectomy agitation in children. Malays J. Med. Sci. 28 (5), 72–81. doi:10.21315/mjms2021.28.5.7
Frey, T. M., Florin, T. A., Caruso, M., Zhang, N., Zhang, Y., and Mittiga, M. R. (2019). Effect of intranasal ketamine vs fentanyl on pain reduction for extremity injuries in children: The PRIME randomized clinical trial. JAMA Pediatr. 173 (2), 140–146. doi:10.1001/jamapediatrics.2018.4582
Jonkman, K., van Rijnsoever, E., Olofsen, E., Aarts, L., Sarton, E., van VelzenM., , et al. (2018). Esketamine counters opioid-induced respiratory depression. Br. J. Anaesth. 120 (5), 1117–1127. doi:10.1016/j.bja.2018.02.021
Kim, H. J., Kim, D. K., Kim, H. Y., Kim, J. K., and Choi, S. W. (2015). Risk factors of emergence agitation in adults undergoing general anesthesia for nasal surgery. Clin. Exp. Otorhinolaryngol. 8 (1), 46–51. doi:10.3342/ceo.2015.8.1.46
Kim, N., Park, J. H., Lee, J. S., Choi, T., and Kim, M. S. (2017). Effects of intravenous fentanyl around the end of surgery on emergence agitation in children: Systematic review and meta-analysis. Paediatr. Anaesth. 27 (9), 885–892. doi:10.1111/pan.13181
Lee, S. J., and Sung, T. Y. (2020). Emergence agitation: Current knowledge and unresolved questions. Korean J. Anesthesiol. 73 (6), 471–485. doi:10.4097/kja.20097
Lee, Y. S., Kim, W. Y., Choi, J. H., Son, J. H., Kim, J. H., and Park, Y. C. (2010). The effect of ketamine on the incidence of emergence agitation in children undergoing tonsillectomy and adenoidectomy under sevoflurane general anesthesia. Korean J. Anesthesiol. 58 (5), 440–445. doi:10.4097/kjae.2010.58.5.440
Mohkamkar, M., Farhoudi, F., Alam-Sahebpour, A., Mousavi, S. A., Khani, S., and Shahmohammadi, S. (2014). Postanesthetic emergence agitation in pediatric patients under general anesthesia. Iran. J. Pediatr. 24 (2), 184–190.
Ni, J., Wei, J., Yao, Y., Jiang, X., Luo, L., and Luo, D. (2015). Effect of dexmedetomidine on preventing postoperative agitation in children: A meta-analysis. PLoS One 10 (5), e0128450. doi:10.1371/journal.pone.0128450
Salloum, N. C., Fava, M., Freeman, M. P., Flynn, M., Hoeppner, B., Hock, R. S., et al. (2019). Efficacy of intravenous ketamine treatment in anxious versus nonanxious unipolar treatment-resistant depression. Depress. Anxiety 36 (3), 235–243. doi:10.1002/da.22875
Wang, J., Huang, J., Yang, S., Cui, C., Ye, L., Wang, S. Y., et al. (2019). Pharmacokinetics and safety of esketamine in Chinese patients undergoing painless gastroscopy in comparison with ketamine: A randomized, open-label clinical study. Drug Des. Devel Ther. 13, 4135–4144. doi:10.2147/DDDT.S224553
Wei, B., Feng, Y., Chen, W., Ren, D., Xiao, D., and Chen, B. (2021). Risk factors for emergence agitation in adults after general anesthesia: A systematic review and meta-analysis. Acta Anaesthesiol. Scand. 65 (6), 719–729. doi:10.1111/aas.13774
Yang, X., Hu, Z., Peng, F., Chen, G., Zhou, Y., Yang, Q., et al. (2020). Effects of dexmedetomidine on emergence agitation and recovery quality among children undergoing surgery under general anesthesia: A meta-analysis of randomized controlled trials. Front. Pediatr. 8, 580226. doi:10.3389/fped.2020.580226
Zhong, H. Y., Deng, X. B., and Wang, Z. (2018). Effects of fascia iliaca compartment block combined with general laryngeal mask airway anesthesia in children undergoing femoral fracture surgery: A randomized trial. J. Pain Res. 11, 2821–2826. doi:10.2147/JPR.S177122
Keywords: esketamine, emergency agitation, children, tonsillectomy, general anesthesia
Citation: Li Q, Fan J and Zhang W (2022) Low-dose esketamine for the prevention of emergency agitation in children after tonsillectomy: A randomized controlled study. Front. Pharmacol. 13:991581. doi: 10.3389/fphar.2022.991581
Received: 02 August 2022; Accepted: 12 December 2022;
Published: 20 December 2022.
Edited by:
Zhongcong Xie, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Ali Saffaei, Shahid Beheshti University of Medical Sciences, IranSantosh Kumar Swain, Siksha O Anusandhan University, India
Copyright © 2022 Li, Fan and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiaming Fan, ZmptMTk4OTAxMDFAc2luYS5jb20=; Wangping Zhang, emhhbmc2NTA2NzlAMTYzLmNvbQ==
 Qi Li1
Qi Li1 Wangping Zhang
Wangping Zhang