
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 20 September 2022
Sec. Gastrointestinal and Hepatic Pharmacology
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.956392
This article is part of the Research Topic Advances in the Potential Treatments of Gastrointestinal and Liver Diseases: Addressing the Public Health Burden View all 21 articles
Objective: This study aimed to determine the optimal dose of propofol combined with esketamine to inhibit the response to gastroscope insertion in elderly patients.
Methods: This is a prospective, non-controlled, non-randomized, single-center study. Elderly patients aged 65–80 years were enrolled in the study with the American society of anesthesiologists (ASA) physical status I or II undergoing elective gastroscopy. All patients were administered propofol after an intravenous esketamine at the dosage of 0.3 mg/kg 30 s, the subsequent dose of propofol was determined by the response of the previous patient to gastroscope insertion (choking, body movement, etc.) using Dixon’s up-and-down method. The initial dose of propofol administered to the first elderly patient was 3.0 mg/kg, and the standard ratio of propofol dose in adjacent patients was 0.9. At least six crossover points were obtained before the conclusion of the study. By using Probit analysis the median effective dose (ED50), 95% effective dose (ED95), and the corresponding 95% confidence interval (CI) for propofol were determined.
Results: The study continued until we obtained seven crossover points and 32 elderly patients (17 males and 15 females) were collected. The ED50 of propofol combined with esketamine inhibiting response to gastroscope insertion in elderly patients were found to be 1.479 mg/kg (95% CI 1.331–1.592 mg/kg), and ED95 was found to be 1.738 mg/kg (95% CI 1.614–2.487 mg/kg).
Conclusion: According to the present study, propofol combined with 0.3 mg/kg esketamine is safe and effective for elderly patients undergoing gastroscopy. The ED50 and ED95 doses of propofol inhibiting response to gastroscope insertion in elderly patients when combined with 0.3 mg/kg esketamine were 1.479 and 1.738 mg/kg, respectively, without apparent adverse effects.
During upper gastrointestinal endoscopy, the endoscope probe stimulates the pharynx when it enters the esophagus. As the pharynx is highly sensitive, patients tend to have nausea, vomiting, choking cough, and even laryngospasm, which can be considerably reduced with an adequate painless procedure. Appropriate sedation enables patients to pass the examination process without difficulty and improves the completion rate and accuracy of endoscopic examination with an enhanced patient and endoscopist satisfaction (Padmanabhan et al., 2017; Nishizawa and Suzuki, 2018). Propofol is a short-acting sedative-hypnotic drug with the characteristics of rapid onset of action, quick recovery, and fewer adverse effects that have been widely used in painless digestive endoscopy (Padmanabhan et al., 2017). Nevertheless, propofol has been reported to possess dose-dependent adverse effects, where overdose increases the risk of respiratory and circulatory depression, while underdose causes airway irritation, pain, limb twitching, and even gastroscopy interruption (Vaessen and Knape, 2016; Delgado et al., 2019), mostly in older patients. In many cases, adjuvants are required because co-administration could not only decrease the required dose of propofol but also reduces the incidence of adverse drug reactions (Nam et al., 2022).
Esketamine is the s-enantiomer of ketamine, and its anesthetic effect is approximately threefold that of R (-) -ketamine (Zanos et al., 2018). Due to the dose-dependent adverse effects of ketamine, low-dose esketamine can decrease the incidence of anesthesia-related adverse events (Bowdle et al., 1998; Zhan et al., 2022). Due to its sympathomimetic properties and less respiratory and circulatory depression, esketamine could better maintain the hemodynamic stability of elderly patients during induction of anesthesia (Yang et al., 2022b; Li et al., 2022). Therefore, it is an ideal candidate to be used in combination with propofol for gastroscopic examination (Wang et al., 2019). However, there is no clear evidence on the effective dose of propofol in combination with esketamine for elderly patients undergoing gastroscopy. Therefore, we conducted this prospective study intending to assess the ED50 and ED95 of propofol combined with 0.3 mg/kg esketamine for a gastroscopy to inhibit the gastroscope insertion (from the pharynx into the esophagus) reaction in elderly patients, thereby providing clinical advice and medication guidance.
This is a prospective, non-controlled, non-randomized, single-center study. The study was registered at the Chinese Clinical Trial Registry (www.chictr.org.cn; registration number: ChiCTR2000038242) on 15/09/2020. The registration of clinical trial includes different age groups (pediatric group, young-middle-aged group and elderly group) and the present study enrolled only elderly patients (age range from 65 to 80). The study was approved by the Medical Ethics Committee of the Shunde Hospital of Southern Medical University (Number: 20200903). All patients undergoing elective gastroscopy from March to May 2021 were enrolled in the study.
Patients were included if they met the following criteria: age between 65 and 80 years, body mass index (BMI) between 18 and 27 kg/m2, perform elective gastroscopy, diagnostic gastroscopy, and ASA physical status I or II.
The following exclusion criteria were implemented in this study: refuse to participate; known allergy to either propofol or esketamine; evident difficult airway; chronic pain; mental-related diseases; symptomatic cardiovascular or pulmonary diseases; severe hepatic and kidney function problems; alcohol abuse; those with increased intracranial pressure or intraocular pressure; history of hyperthyroidism; hemostasis, polypectomy or other require any treatments before/during the examination; chronic use of sedative or analgesic drugs.
Before the painless gastroscopy, all patients were kept fasted for at least 6 h and were then transferred to the examination room and put on oxygen at the rate of 4 L/min through a nasal straw. The Anesthesiologist also measured the mean arterial pressure (MAP), heart rate (HR), and blood oxygen saturation (SpO2) of all patients. After opening the patient’s peripheral venous access, 500 ml of lactated ringer’s solution was infused at a rate of 250 ml/h.
All Anesthesia operations were performed by the same anesthesiologist. Patients were administered intravenous 0.3 mg/kg esketamine (2 ml: 50 mg, Jiangsu Hengrui Medicine China, lot number: 200403BL) and propofol for sedation (20 ml: 0.2 g, Propofol 1% MCT Fresenius Kabi St. Wendel Germany, lot number: 2003085). The dose of propofol administered to elderly patients after 30 s of intravenous esketamine was determined by the response of the previous patient to gastroscope insertion (choking cough, body movement, etc.) using Dixon’s up-and-down method. The dose of propofol was increased in the subsequent patient due to an increase in choking cough, body movement, and effect on operations by endoscopists when the gastroscope inserted into the esophagus was deemed “responsive.” The dose of propofol was decreased in the subsequent patient if there was no choking cough and no body movement. The initial dose of propofol administered to the first elderly patient was 3.0 mg/kg, and the average ratio of propofol dose in adjacent patients was 0.9. At least six crossover points were obtained before the conclusion of the study.
Following the administration of propofol, an endoscope (OLYMPUS Lucera LCV-260SL) was inserted. All gastroscopic examinations were performed by endoscopists with at least five years of experience. If the patient was “responsive”, a single dose of 20–50 mg of propofol was administered intravenously and repeated to complete the gastroscopy.
Following gastroscopy, the patients were transferred to the post-anesthesia care unit (PACU), where the anesthetist awakened the elderly patient. Similarly, the HR, MAP, and SpO2 levels were also monitored. The recovery time was recorded. The patient spent at least 30 min in PACU. The criteria for discharge or transfer from PACU to the inpatient unit were typical vital signs, the ability to walk without assistance, and the absence of evident side effects.
The adverse medical events were handled as follows: hypotension (MAP decreased by 30% over the baseline value) was treated with a bolus of 5–10 mg ephedrine; bradycardia (HR < 50 beats/min) was treated with an intravenous injection of 0.25–0.5 mg atropine; respiratory depression (SpO2<90%) was treated with a mask pressurized or laryngeal mask to maintain ventilation; and in event of nausea and vomiting, a bolus of 2 mg tropisetron was administered.
The primary outcome of the current study was the dose of propofol determined for each elderly patient using Dixon’s up-and-down method.
The secondary outcome: HR, MAP, and SpO2 were measured at the following time points: 5 min after entering the gastroscopy room (T1), immediately after intravenous injection of ketamine (T2), immediately after intravenous injection of propofol (T3), and immediately after the Endoscope was passed into the esophagus (T4), and 1 min after the patient’s recovery (T5). Hypotension, bradycardia, injection pain, post-operative nausea and vomiting (PONV), respiratory depression (SpO2<90%), emergence agitation, and psychiatric symptoms 24 h following anesthesia were also recorded. Additionally, each dose of propofol used, the duration of the gastroscope insertion and gastroscopy, and the recovery time were recorded. If the patient frowned or complained of arm pain or ipsilateral limb escape response, this was defined as injection pain. Gastroscope insertion time was defined as the duration from the pharynx into the esophagus. Recovery time was defined as the duration between propofol cessation and eye-opening on command.
The sample size calculation: The total number of participants depends on Dixon’s up-and-down method (Dixon, 1991). This method requires at least six crossover points (non-responsive to responsive) for statistical analysis.
All the statistical analysis were performed using SPSS (version 17.0, SPSS Inc. Chicago, Illinois, United States). Data were checked for normality using Shapiro-Wilk test, and the appropriate test was next applied as indicated. Data were expressed as mean ± standard deviation (SD), median [range] or n. Using repeated measures analysis of variance, the data collected at various time points within the group were analyzed. p < 0.05 indicates a statistically significant difference. The ED50 and ED95 of propofol and their corresponding CI were analyzed using the Probit test. Microsoft excel software was used to draw a sequential graph and dose-response curve.
A total of 35 elderly patients were enrolled from March to May 2021. Three elderly patients were excluded, and a total of 32 elderly patients successfully completed the study (Figure 1). Table 1 depicts the demographic data of all the elderly enrolled patients. Gastroscopy time was (5.9 ± 1.2) min, recovery time was (11.2 ± 4.3) min, and propofol dose was (119.4 ± 18.3) mg.
Our study was conducted until data of seven crossover points were collected. Figure 2 shows the sequential response of 32 elderly patients to the up-and-down method of gastroscope insertion. There were 12 elderly patients who were responsive and given propofol as a remedy.
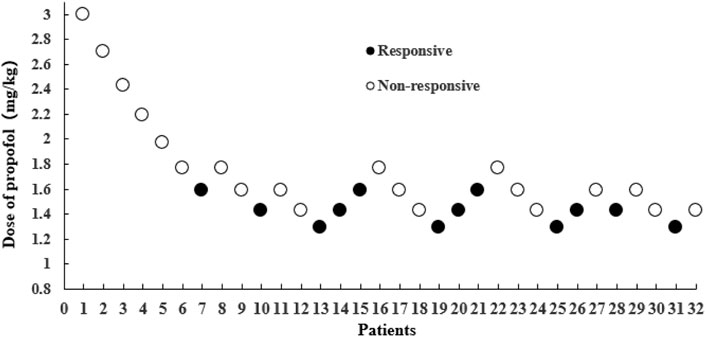
FIGURE 2. The sequential response of 32 elderly patients to gastroscope insertion with the up-and-down method. The black dot represents “responsive,” and the white dot represents “non-responsive".
The ED50 of propofol combined with esketamine inhibiting response to gastroscope insertion in elderly patients was found to be 1.479 mg/kg (95% CI: 1.331–1.592 mg/kg), while the ED95 was found to be 1.738 mg/kg (95% CI: 1.614–2.487 mg/kg) (Figure 3).
According to repeated measures analysis of variance, MAP and HR fluctuated significantly (p < 0.05) over time. MAP significantly increased immediately after intravenous injection of ketamine (T2) time point and dropped significantly immediately after intravenous injection of propofol (T3) time point in comparison to 5 min after entering the gastroscopy room (T1) time point without a significant change in HR and SpO2 (Table 2).
The overall incidence of anesthesia-related adverse events was recorded to be 23.3% (Table 3).
The primary objective of this study was to evaluate the effect of low-dose esketamine on the dose of propofol required to achieve the desired degree of sedation without body movement for gastroscopy in elderly patients and its safety and efficacy. Our research revealed that the ED50 and ED95 values for propofol inhibiting the response to gastroscope insertion in patients when combined with 0.3 mg/kg esketamine were found to be 1.479 and 1.738 mg/kg, respectively. The incidence of anesthesia-related complications was recorded to be 23.3% among all patients. All adverse reactions returned rapidly to normal following treatment, and there was no severe cardiovascular incident during gastroscopy. No significant psychiatric symptoms occurred during the telephone follow-up 24 h after the gastroscopy. Thus, the combinational use of propofol and 0.3 mg/kg esketamine is regarded as safe and effective for elderly patients undergoing gastroscopy.
Similar research evaluated the median effective concentration (EC50) of propofol and ketamine in elderly gastrointestinal endoscopy patients (Yang et al., 2022b). To determine the EC50 in their study, propofol was administered using a computer-controlled target-controlled infusion (TCI) pump. We believe that the use of TCI has certain advantages for painless gastrointestinal endoscopy. Still, because gastroscopy requires less time than gastrointestinal endoscopy in the present study, direct injection is simple, convenient, and quick, saving anesthesia time and equipment requirements compared to TCI. Thus, direct injection of propofol is appropriate for gastroscopy. The effective dose of propofol obtained using Dixon’s up-and-down method can be utilized to be a better immediate clinically applied medication for gastroscopy.
Like Ketamine, esketamine is an N-methyl-D-aspartate receptor antagonist with analgesic, anesthetic, and sympathomimetic properties and can reduce the incidence of cardiopulmonary depression; however, there is a correlation between effect and dosage, and a small dose of esketamine has greater sedative and analgesic effects than a larger dose (Perez-Ruixo et al., 2021; Yang et al., 2022b; Zheng et al., 2022). Esketamine can be used safely and effectively in elderly patients due to its stable hemodynamics and low incidence of adverse events properties (Yang et al., 2022b). Impaired physical function, the type of surgical procedure, and old age are risk factors for propofol-induced circulatory and respiratory depression (Quine et al., 1995; Eckardt et al., 1999; Bhananker et al., 2006). Therefore, advanced age is also a significant risk factor for adverse events associated with propofol sedation during gastroscopy. Because propofol reduces cardiac output (CO) and systemic vascular resistance (SVR) and causes respiratory depression, it should be administered with caution to elderly patients (Han et al., 2017). After injection of low-dose esketamine, our study revealed that MAP was significantly higher than the baseline blood pressure but had almost no effect on HR and SpO2. This transient blood pressure increase could be eliminated by the injection of propofol. Our results were consistent with results reported by Eberl et al, (2020). We believed that it might be due to the sympathomimetic effect of esketamine, which makes it an optimal analgesic and sedative drug for anesthesia in hemodynamically compromised patients. Furthermore, it has been regarded as the drug of choice for elderly patients, in the event of a pre-hospital emergency, burn, and cardiogenic shock patients, as an adjunct to propofol use for sedation (Trimmel et al., 2018; Eberl et al., 2020).
Due to the potential for apnea with propofol, propofol-related respiratory depression occurs frequently reported adverse effects. Ketamine has the unique characteristics of maintaining stable oxygen saturation owing to its ability to exert direct smooth muscle relaxation, bronchodilation effect, and preserve the laryngeal reflex (Cortinez and Anderson, 2018; Iqbal et al., 2022). However, it should be noted that ketamine-induced sedation can also result in the adverse airway and respiratory events, with an incidence of 1.4%–6.6% (Green et al., 2009). In our study, the incidence and severity of hemodynamic and respiratory adverse events were lower than in other reported studies (Akhondzadeh et al., 2016; Bahrami Gorji et al., 2016). Ketamine is a psychoactive drug that can cause neurological and psychiatric complications, including delirium, hallucinations, and dissociative symptoms. None of patients in our study developed psychiatric symptoms during the follow-up by telephone after 24 h. Propofol may inhibit ketamine-induced expression of c-fos in the posterior cingulate cortex, and that overexpression of c-fos leads to psychotomimetic side effects of ketamine (Nagata et al., 1998).
With increasing age, the effective dose range of propofol gradually decreases (Yang et al., 2022a). Researchers estimated that the mean induction dose of propofol for elderly patients was 1.7 mg/kg (Schonberger et al., 2021), which was comparable to the outcomes of our study. Opioids such as remifentanil, sufentanil, or fentanyl combined with propofol were the most frequently used agents in painless gastroenteroscopy, which can reduce the administered dose of propofol (Zhao et al., 2015; Doganay et al., 2017). Compared to propofol alone or in combination with opioids, propofol combined with ketamine provides sedation and analgesia in addition to the reduction in the risk of cardiovascular and respiratory adverse events (Shah et al., 2011; Nazemroaya et al., 2018). It was observed that propofol used in combination with esketamine reduced the therapeutic dose of propofol in comparison to its lone use for producing similar results during gastrointestinal endoscopy in elderly patients. With the increase in esketamine dose (0–0.5 mg/kg), there was no obvious hypotension, and the recovery time was shortened (Yang et al., 2022b). We, therefore, believed that the low incidence of adverse events in this study was associated with a lower propofol induction dose.
The limitations encountered during the study were: First, considering the safety of the drugs in exploratory trials in elderly patients, we only included patients with ASA I or II and excluded high-risk patients with ASA III and IV. Therefore, the results and conclusions of this study may not apply to other high-risk patients. Second, gastroscopies were performed by 3 different operators (with>5 years of experience), and skills and manipulations of gastroscope insertion may affect the results; therefore, these results may have limited applicability. Thirdly, considering that esketamine may have a greater impact on the effect of general anesthesia and hemodynamics in elderly patients, the anesthesiologists were not blinded to the dose of esketamine used, which may have impacted our findings. Consequently, the current findings require further investigation.
In conclusion, it was discovered that combining 1.738 mg/kg of propofol with 0.3 mg/kg of esketamine inhibits the response to gastroscope insertion in 95% of elderly patients without noticeable adverse reactions. In the future, we aim to further investigate the optimal dose of propofol for elderly patients in combination with other doses of esketamine for gastroscopy.
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Medical Ethics Committee of the Shunde Hospital of Southern Medical Universit. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
In this work, ZZ conceived the study and designed the study. YX, BH and YM contributed to the data collection, performed the data analysis and interpreted the results. YZ wrote the manuscript. YZ (5th author) contributed to the critical revision of article. All authors read and approved the final manuscript.
Beijing Medical Award Foundation, Grant/Award Number: YXJL-2021–0307–0584; Guangdong Hospital Pharmacy Research Fund (Medical Special Fund of Xinchen), Grant/Award Number: 2020XC14. Key medical talents training project of Shunde District.
We thank Home for Researchers editorial team (www.home-for-researchers.com) for language editing service.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Akhondzadeh, R., Ghomeishi, A., Nesioonpour, S., and Nourizade, S. (2016). A comparison between the effects of propofol-fentanyl with propofol-ketamine for sedation in patients undergoing endoscopic retrograde cholangiopancreatography outside the operating room. Biomed. J. 39, 145–149. doi:10.1016/j.bj.2015.11.002
Bahrami Gorji, F., Amri, P., Shokri, J., Alereza, H., and Bijani, A. (2016). Sedative and analgesic effects of propofol-fentanyl versus propofol-ketamine during endoscopic retrograde cholangiopancreatography: A double-blind randomized clinical trial. Anesth. Pain Med. 6, e39835. doi:10.5812/aapm.39835
Bhananker, S. M., Posner, K. L., Cheney, F. W., Caplan, R. A., Lee, L. A., and Domino, K. B. (2006). Injury and liability associated with monitored anesthesia care: A closed claims analysis. Anesthesiology 104, 228–234. doi:10.1097/00000542-200602000-00005
Bowdle, T. A., Radant, A. D., Cowley, D. S., Kharasch, E. D., Strassman, R. J., and Roy-Byrne, P. P. (1998). Psychedelic effects of ketamine in healthy volunteers: Relationship to steady-state plasma concentrations. Anesthesiology 88, 82–88. doi:10.1097/00000542-199801000-00015
Cortinez, L. I., and Anderson, B. J. (2018). Advances in pharmacokinetic modeling: Target controlled infusions in the obese. Curr. Opin. Anaesthesiol. 31, 415–422. doi:10.1097/ACO.0000000000000619
Delgado, A. a. A., De Moura, D. T. H., Ribeiro, I. B., Bazarbashi, A. N., Dos Santos, M. E. L., Bernardo, W. M., et al. (2019). Propofol vs traditional sedatives for sedation in endoscopy: A systematic review and meta-analysis. World J. Gastrointest. Endosc. 11, 573–588. doi:10.4253/wjge.v11.i12.573
Dixon, W. J. (1991). Staircase bioassay: The up-and-down method. Neurosci. Biobehav. Rev. 15, 47–50. doi:10.1016/s0149-7634(05)80090-9
Doganay, G., Ekmekci, P., Kazbek, B. K., Yilmaz, H., Erkan, G., and Tuzuner, F. (2017). Effects of alfentanil or fentanyl added to propofol for sedation in colonoscopy on cognitive functions: Randomized controlled trial. Turk. J. Gastroenterol. 28, 453–459. doi:10.5152/tjg.2017.16489
Eberl, S., Koers, L., Van Hooft, J., De Jong, E., Hermanides, J., Hollmann, M. W., et al. (2020). The effectiveness of a low-dose esketamine versus an alfentanil adjunct to propofol sedation during endoscopic retrograde cholangiopancreatography: A randomised controlled multicentre trial. Eur. J. Anaesthesiol. 37, 394–401. doi:10.1097/EJA.0000000000001134
Eckardt, V. F., Kanzler, G., Schmitt, T., Eckardt, A. J., and Bernhard, G. (1999). Complications and adverse effects of colonoscopy with selective sedation. Gastrointest. Endosc. 49, 560–565. doi:10.1016/s0016-5107(99)70382-2
Green, S. M., Roback, M. G., Krauss, B., Brown, L., Mcglone, R. G., Agrawal, D., et al. (2009). Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: An individual-patient data meta-analysis of 8, 282 children. Ann. Emerg. Med. 54, 158–168154. doi:10.1016/j.annemergmed.2008.12.011
Han, S. J., Lee, T. H., Park, S. H., Cho, Y. S., Lee, Y. N., Jung, Y., et al. (2017). Efficacy of midazolam- versus propofol-based sedations by non-anesthesiologists during therapeutic endoscopic retrograde cholangiopancreatography in patients aged over 80 years. Dig. Endosc. 29, 369–376. doi:10.1111/den.12841
Iqbal, A. U., Shuster, M. E., and Baum, C. R. (2022). Ketofol for procedural sedation and analgesia in the pediatric population. Pediatr. Emerg. Care 38, 28–33. doi:10.1097/PEC.0000000000002599
Li, J., Wang, Z., Wang, A., and Wang, Z. (2022). Clinical effects of low-dose esketamine for anaesthesia induction in the elderly: A randomized controlled trial. J. Clin. Pharm. Ther. 47, 759–766. doi:10.1111/jcpt.13604
Nagata, A., Nakao, S., Miyamoto, E., Inada, T., Tooyama, I., Kimura, H., et al. (1998). Propofol inhibits ketamine-induced c-fos expression in the rat posterior cingulate cortex. Anesth. Analg. 87, 1416–1420. doi:10.1097/00000539-199812000-00040
Nam, J. H., Jang, D. K., Lee, J. K., Kang, H. W., Kim, B. W., Jang, B. I., et al. (2022). Committees of quality, M., and conscious sedation of Korean society of gastrointestinal, EPropofol alone versus propofol in combination with midazolam for sedative endoscopy in patients with paradoxical reactions to midazolam. Clin. Endosc. 55, 234–239. doi:10.5946/ce.2021.126
Nazemroaya, B., Majedi, M. A., Shetabi, H., and Salmani, S. (2018). Comparison of propofol and ketamine combination (ketofol) and propofol and fentanyl combination (fenofol) on quality of sedation and analgesia in the lumpectomy: A randomized clinical trial. Adv. Biomed. Res. 7, 134. doi:10.4103/abr.abr_85_18
Nishizawa, T., and Suzuki, H. (2018). Propofol for gastrointestinal endoscopy. United Eur. Gastroenterol. J. 6, 801–805. doi:10.1177/2050640618767594
Padmanabhan, A., Frangopoulos, C., and Shaffer, L. E. T. (2017). Patient satisfaction with propofol for outpatient colonoscopy: A prospective, randomized, double-blind study. Dis. Colon Rectum 60, 1102–1108. doi:10.1097/DCR.0000000000000909
Perez-Ruixo, C., Rossenu, S., Zannikos, P., Nandy, P., Singh, J., Drevets, W. C., et al. (2021). Population pharmacokinetics of esketamine nasal spray and its metabolite noresketamine in healthy subjects and patients with treatment-resistant depression. Clin. Pharmacokinet. 60, 501–516. doi:10.1007/s40262-020-00953-4
Quine, M. A., Bell, G. D., Mccloy, R. F., Charlton, J. E., Devlin, H. B., and Hopkins, A. (1995). Prospective audit of upper gastrointestinal endoscopy in two regions of england: Safety, staffing, and sedation methods. Gut 36, 462–467. doi:10.1136/gut.36.3.462
Schonberger, R. B., Bardia, A., Dai, F., Michel, G., Yanez, D., Curtis, J. P., et al. (2021). Variation in propofol induction doses administered to surgical patients over age 65. J. Am. Geriatr. Soc. 69, 2195–2209. doi:10.1111/jgs.17139
Shah, A., Mosdossy, G., Mcleod, S., Lehnhardt, K., Peddle, M., and Rieder, M. (2011). A blinded, randomized controlled trial to evaluate ketamine/propofol versus ketamine alone for procedural sedation in children. Ann. Emerg. Med. 57, 425–433. doi:10.1016/j.annemergmed.2010.08.032
Trimmel, H., Helbok, R., Staudinger, T., Jaksch, W., Messerer, B., Schochl, H., et al. (2018). S(+)-ketamine : Current trends in emergency and intensive care medicine. Wien. Klin. Wochenschr. 130, 356–366. doi:10.1007/s00508-017-1299-3
Vaessen, H. H., and Knape, J. T. (2016). Considerable variability of procedural sedation and analgesia practices for gastrointestinal endoscopic procedures in europe. Clin. Endosc. 49, 47–55. doi:10.5946/ce.2016.49.1.47
Wang, J., Huang, J., Yang, S., Cui, C., Ye, L., Wang, S. Y., et al. (2019). Pharmacokinetics and safety of esketamine in Chinese patients undergoing painless gastroscopy in comparison with ketamine: A randomized, open-label clinical study. Drug Des. devel. Ther. 13, 4135–4144. doi:10.2147/DDDT.S224553
Yang, H., Deng, H. M., Chen, H. Y., Tang, S. H., Deng, F., Lu, Y. G., et al. (2022a). The impact of age on propofol requirement for inducing loss of consciousness in elderly surgical patients. Front. Pharmacol. 13, 739552. doi:10.3389/fphar.2022.739552
Yang, H., Zhao, Q., Chen, H. Y., Liu, W., Ding, T., Yang, B., et al. (2022b). The median effective concentration of propofol with different doses of esketamine during gastrointestinal endoscopy in elderly patients: A randomized controlled trial. Br. J. Clin. Pharmacol. 88, 1279–1287. doi:10.1111/bcp.15072
Zanos, P., Moaddel, R., Morris, P. J., Riggs, L. M., Highland, J. N., Georgiou, P., et al. (2018). Ketamine and ketamine metabolite Pharmacology: Insights into therapeutic mechanisms. Pharmacol. Rev. 70, 621–660. doi:10.1124/pr.117.015198
Zhao, Y. J., Liu, S., Mao, Q. X., Ge, H. J., Wang, Y., Huang, B. Q., et al. (2015). Efficacy and safety of remifentanil and sulfentanyl in painless gastroscopic examination: A prospective study. Surg. Laparosc. Endosc. Percutan. Tech. 25, e57–60. doi:10.1097/SLE.0000000000000064
Zheng, X. S., Shen, Y., Yang, Y. Y., He, P., Wang, Y. T., Tao, Y. Y., et al. (2022). ED50 and ED95 of propofol combined with different doses of esketamine for children undergoing upper gastrointestinal endoscopy: A prospective dose-finding study using up-and-down sequential allocation method. J. Clin. Pharm. Ther. 47, 1002–1009. doi:10.1111/jcpt.13635
Zhan, Y., Liang, S., Yang, Z., Luo, Q., Li, S., Li, J., et al. (2022). Efficacy and safety of subanesthetic doses of esketamine combined with propofol in painless gastrointestinal endoscopy: A prospective, double-blind, randomized controlled trial. BMC Gastroenterol. 22 (1), 391. doi:10.1186/s12876-022-02467-8
Keywords: propofol, esketamine, effective dose, gastroscopy, dose-response relationship
Citation: Zheng Y, Xu Y, Huang B, Mai Y, Zhang Y and Zhang Z (2022) Effective dose of propofol combined with a low-dose esketamine for gastroscopy in elderly patients: A dose finding study using dixon’s up-and-down method. Front. Pharmacol. 13:956392. doi: 10.3389/fphar.2022.956392
Received: 30 May 2022; Accepted: 06 September 2022;
Published: 20 September 2022.
Edited by:
Adina Turcu-Stiolica, University of Medicine and Pharmacy of Craiova, RomaniaReviewed by:
Kessarin Thanapirom, Royal Free Hospital, United KingdomCopyright © 2022 Zheng, Xu, Huang, Mai, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongqi Zhang, anh6enExMUAxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.