
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol. , 22 July 2022
Sec. Drugs Outcomes Research and Policies
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.953341
 Wan Nur Liyana Hazwani Wan Rohimi
Wan Nur Liyana Hazwani Wan Rohimi Nurul Ain Mohd Tahir*
Nurul Ain Mohd Tahir*Aims: Educational interventions are effective to improve peoples’ self-efficacy in managing diabetes complications and lifestyle changes. This systematic review aims to assess and compare various aspects of educational interventions and to provide updated pharmacoeconomics data.
Methods: Literature searches were conducted using databases such as EBSCOhost, Ovid, PubMed, Scopus, and Web of Science. Outcomes such as study characteristics, costs, medication adherence, effectiveness and were narratively summarized, and the quality of each article was assessed.
Results: A total of 27 studies were retrieved. The types of educational interventions were classified as face-to-face strategy, structured programs, telemedicine health education, a combination approach, and others. All types of educational interventions (N = 24, 89%) were reported to be cost-effective. The cost-effectiveness of the other two studies was considered to be not cost-effective while the outcome of one study could not be determined. The majority of the studies (N = 24, 89%) had moderate-quality evidence whereas thirteen (48%) studies were regarded to provide high-quality economic evaluations.
Conclusion: All types of educational interventions are highly likely to be cost-effective. The quality of economic evaluations is moderate but the most cost-effective types of educational interventions could not be determined due to variations in the reporting and methodological conduct of the study. A high-quality approach, preferably utilizing the societal perspective over a long period, should be standardized to conduct economic evaluations for educational interventions in T2DM.
Systematic Review Registration: website, identifier registration number.
Diabetes affects 422 million people globally, with the majority living in low-and middle-income countries (WHO, 2021). This number has significantly increased as 170 million people were diagnosed in the 2000s, and currently, it has exceeded the projected number of 366 million people having diabetes by 2030 (Wild et al., 2004). Out of these, type II diabetes mellitus (T2DM) usually accounted for nine out of every ten people (Zimmet, 2003). T2DM is commonly associated with obesity and other comorbidities, including hypertension, cardiovascular-related diseases, and microvascular disorders that could lead to complications that may impact people’s quality of life (Keith Campbell, 2009). A study in South Australia reported that 56.6% of cases of mortality of T2DM people were caused by cardiovascular-related diseases, followed by 15.0 and 10.9% due to unnatural deaths and infections, respectively (Zhou and Byard, 2018). The economic burden of diabetes mellitus is equally substantial. International Diabetes Federation (IDF) reported enormous expenses of US$850 billion for the management of diabetes mellitus globally in 2017, and it was projected to increase up to US$958 billion by 2045 (Cho et al., 2018). In the United States, an estimated cost of $327 billion was for diabetes, accounting for 25% of all healthcare spending (ADA, 2018). The burden of expenses is amplified in T2DM people requiring an additional cost of US$9,643 as compared to non-diabetes people and the difference can increase up to US$18,057 after 8 years of diagnosis (Zimmet, 2003). The high cost of diabetes care is a significant problem in today’s healthcare system as well as a burden on people.
Educational interventions are useful and successful strategies that can contribute to positive outcomes in peoples’ knowledge and attitude in managing their T2DM as well as effectively improving people’s glycaemic control (Ahmed et al., 2015). The effectiveness of these interventions which includes various forms and components in preventing the onset and delaying the progression of complications of T2DM have always been widely studied and reported in an abundant number of studies (Merakou et al., 2015; Zhang and Chu, 2018; Mohamed et al., 2019). Various beneficial methods of delivering educational interventions had been accomplished in improving diabetes self-care, however, these studies revealed inconsistency in the determination of the elements of educational interventions and thus became the major barrier to understanding the outcomes of educational research in diabetes (Sigurdardottir et al., 2007). Furthermore, a diversity of educational programs did not yield consistent results on measures of metabolic control (Loveman et al., 2003). For example, the diversity of theories concerning delivery, teaching methods, content, and depth of educational interventions may have an impact on the HbA1c and metabolic outcomes of T2DM patients (Loveman et al., 2003; Sigurdardottir et al., 2007).
Similarly, numerous systematic reviews of the cost-effectiveness of educational interventions have resulted in equivocal conclusions (Loveman et al., 2003; Odnoletkova et al., 2014). Furthermore, it ignores the variety of educational intervention aspects and economic evaluation methodological conducts that could influence the cost-effectiveness decision. This evidence could potentially fill in the existing gaps and provide updated pharmacoeconomics data for the healthcare policymakers in determining which elements of educational interventions are effective and economically practical to be implemented in the provision of health care for T2DM people.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used as a guide in reporting the economic evaluation outcomes in this systematic review (Moher et al., 2009).Search strategy
Major databases selected in generating the search included EBSCOhost, Ovid, PubMed, Scopus, and Web of Science. The main search terms such as “cost-effectiveness”, “educational interventions”, “medication adherence”, and “type II diabetes mellitus” were used. The medical subject heading (MeSH) was employed where applicable. Subsequent keywords were added in conjunction to the main keywords by connecting them using Boolean Operator “OR” to broaden the search. The subsequent keywords were as follows (“costs” OR “cost analysis” OR “cost utility” OR “cost benefit” OR “health economics” OR “economic evaluation” OR “cost minimi?ation”) (“educational strategies” OR “patient education”) (“medication compliance” OR “medication nonadherence” OR “medication noncompliance” OR “persistence” OR “constancy”) (“diabetes mellitus type II” OR “metabolic disease” OR “non-insulin dependent diabetes” OR “T2DM” OR “NIDDM”). Boolean Operator “AND” was used to connect all the keywords to narrow down and retrieve all the relevant studies. The language of all the literature selected was limited to English. The database was searched for all articles published between the start of the database and the last search date of 28 October 2020.
The eligibility criteria for inclusion of the article include: 1) the study population is those diagnosed with T2DM, 2) The intervention is an educational intervention defined as the number of approaches aim to improve disease knowledge and management skills 3) the comparator is the usual care or any control group specified in the study, 4) the main outcome is the comparative cost-effectiveness value. The primary outcomes mainly focused on the cost-effectiveness of the educational interventions meanwhile the secondary outcomes included the costs, medication adherence, and health effects of the interventions such as HbA1c level and T2DM complications. Only original articles will be included in the review. Articles with study design such as study protocol, pilot study, case reports, editorial, comments, and notes were excluded from the review.
All the article generated was entered into a reference management software (EndNote) to be screened. Duplicates of the article were excluded beforehand. The remaining articles were screened against the inclusion and exclusion criteria based on the titles, followed by the abstracts to obtain the qualified articles. The articles that were relevant to the research topics and fulfilled all the eligibility criteria were selected to be read in full text. The articles that did not meet the criteria were removed and the remaining articles were included in the systematic review. The whole study selection process was conducted by the first reviewer (LH) and further checked by the second reviewer (NAMT) to ensure that an appropriate assessment for inclusion was done.
Characteristics of the studies including the type of economic evaluation, study design, the intervention, comparator, perspective, year and type of costs, sources of data, time horizon, and main economic outcomes were extracted.
The information related to the primary and secondary outcomes of the study such as the prevalence of medication adherence, the effectiveness measured by clinical measures or health effects, costs, the outcomes measures, and the cost-effectiveness ratio were further extracted. The costs, medication adherence, and the health effects of the educational interventions were considered the secondary outcomes of the study. The data extracted were analyzed, grouped, and summarized narratively by the first reviewer (LH). The second reviewer (NAMT) was in charge of making sure that the data entered was relevant to the interest of the study.
The methodological quality of the retrieved studies was assessed against ten items indicated in the ten-point Drummond checklist (Drummond et al., 2015). The checklist concisely formulated all the essential aspects needed for the judgment of the studies such as follows: the research question, the study description, the effectiveness of the intervention, the identification of health effects and its measurements, the valuation and effects of the interventions, discounting, incremental costs analysis, the determination of uncertainty by sensitivity analysis and discussion relevant to the available health policies. Each item in the checklist was scaled from a score of 1–10, where a score ranging from 1 to 3 indicates poor quality, followed by a score ranging from 4 to 7 reflects a modest-quality while a high-quality score of 8–10 (Doran, 2008). The quality assessment was performed by the first reviewer (LH) and the second reviewer (NAMT) will further validate the quality of the studies.
The study selection process was summarized in Figure 1. A total of 2,117 articles were generated from the database searches. 1858 records of duplicates were eliminated, and the title of the remaining records was screened. 1,572 records were excluded due to the irrelevance of the title, leaving 286 records to be screened based on their abstracts. This led to the further exclusion of 231 articles and a full-text assessment was performed on the remaining 55 articles. 28 articles were excluded for reasons as stated in Figure 1. As a result, 27 articles that were deemed to fulfill the inclusion criteria were included in the review.
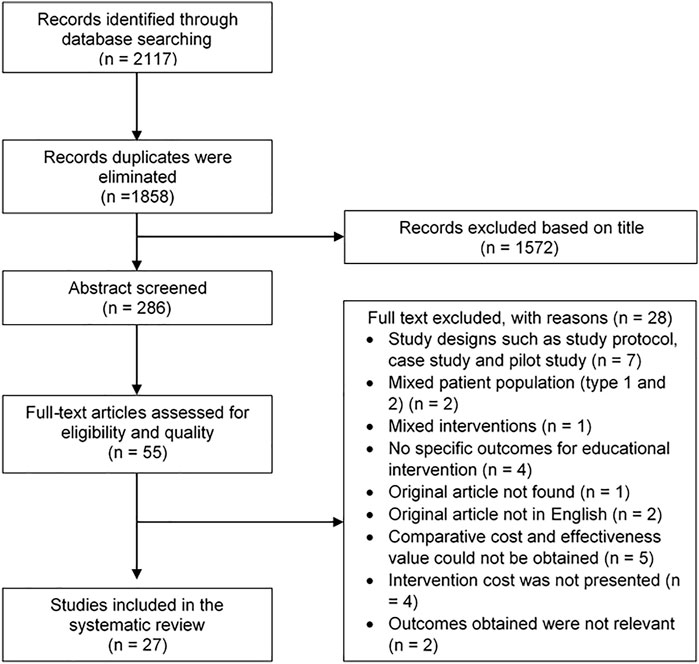
FIGURE 1. Flow diagram for selection of articles of a systematic review of the cost-effectiveness of different types of educational interventions in type II diabetes mellitus.
The characteristics of the included study are tabulated in Table 1. Out of twenty-seven studies selected, thirteen were performed in European countries (Davies et al., 2001; Trento et al., 2002; Keers et al., 2005; Dijkstra et al., 2006; Simon et al., 2008; Molsted et al., 2012; Tao et al., 2015; Elliott et al., 2016; Odnoletkova et al., 2016; Elliott et al., 2017; Johansson et al., 2017; Oksman et al., 2017; Wu et al., 2018), eight studies were conducted in the United States (Banister et al., 2004; Handley et al., 2008; Brownson et al., 2009; Brennan et al., 2012; Schechter et al., 2012; Hendrie et al., 2014; Prezio et al., 2014; Schechter et al., 2016), while the remaining were in South Africa (n = 1) (Mash et al., 2015), India (n = 1) (Kesavadev et al., 2012), Australia (n = 2) (Gillett et al., 2010; Varney et al., 2016) and Hong Kong (n = 2) (Lian et al., 2017; Lian et al., 2019). The articles were published from 2001 to 2019, where most (N = 15, 56%) of the articles were published within the 10 years of the study.
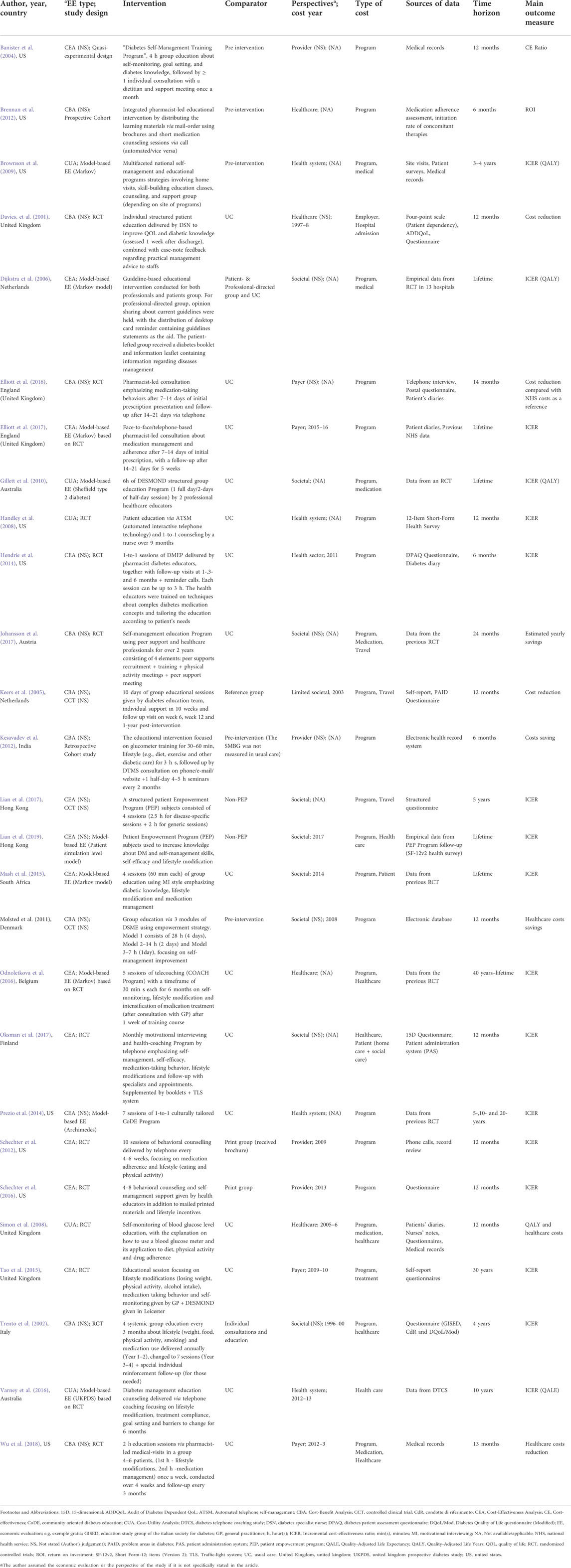
TABLE 1. Study characteristics of a systematic review of the cost-effectiveness of different types of educational interventions in type II diabetes mellitus.
Most of the studies compared the intervention group with the usual care practice, as well as the pre-intervention group (Banister et al., 2004; Brownson et al., 2009; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012) except for a few which compared them to their designated control group (Trento et al., 2002; Keers et al., 2005; Dijkstra et al., 2006; Schechter et al., 2012; Schechter et al., 2016; Lian et al., 2017; Lian et al., 2019).
The study design of economic evaluation incorporated in this study was model-based economic evaluation (n = 9) (Dijkstra et al., 2006; Brownson et al., 2009; Gillett et al., 2010; Prezio et al., 2014; Mash et al., 2015; Odnoletkova et al., 2016; Varney et al., 2016; Elliott et al., 2017; Lian et al., 2019), randomized controlled trial (n = 12) (Davies et al., 2001; Trento et al., 2002; Handley et al., 2008; Simon et al., 2008; Schechter et al., 2012; Hendrie et al., 2014; Tao et al., 2015; Elliott et al., 2016; Schechter et al., 2016; Johansson et al., 2017; Oksman et al., 2017; Wu et al., 2018) and prospective cohort studies (n = 2) (Brennan et al., 2012; Kesavadev et al., 2012). Another four studies were classified as quasi-experimental design (n = 1) (Banister et al., 2004) and controlled clinical trials (n = 3) (Keers et al., 2005; Molsted et al., 2012; Lian et al., 2017) as the authors did not explicitly clarify the nature of allocation of the participants in the study.
Eight studies were reported as cost-effectiveness analysis (CEA) (Dijkstra et al., 2006; Schechter et al., 2012; Mash et al., 2015; Tao et al., 2015; Odnoletkova et al., 2016; Schechter et al., 2016; Elliott et al., 2017; Oksman et al., 2017), while five studies were cost-utility analysis (CUA) with QALYs measured obtained as the results (Handley et al., 2008; Simon et al., 2008; Brownson et al., 2009; Gillett et al., 2010; Varney et al., 2016). Other studies (N = 14) did not mention the type of economic evaluation that was performed (Davies et al., 2001; Trento et al., 2002; Banister et al., 2004; Keers et al., 2005; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012; Hendrie et al., 2014; Prezio et al., 2014; Elliott et al., 2016; Johansson et al., 2017; Lian et al., 2017; Wu et al., 2018; Lian et al., 2019).
Overall, the type of costs identified in the studies includes the program costs, health care costs, travel costs, drug costs as well as out-of-pocket costs that needed to be paid by the people such as for home and social care. Most of the studies estimated the costs from a single site or multi-site evaluation, with the exclusion of three studies that generalizes the cost estimates from nationwide data (Gillett et al., 2010; Lian et al., 2017; Lian et al., 2019). Twelve studies were performed over 6 months up to 12 months (Davies et al., 2001; Banister et al., 2004; Keers et al., 2005; Handley et al., 2008; Simon et al., 2008; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012; Schechter et al., 2012; Hendrie et al., 2014; Schechter et al., 2016; Oksman et al., 2017), and 3 studies were conducted in the range of 13 months up to 24 months (Elliott et al., 2016; Johansson et al., 2017; Wu et al., 2018). Of these, the remaining twelve studies (Trento et al., 2002; Dijkstra et al., 2006; Brownson et al., 2009; Gillett et al., 2010; Prezio et al., 2014; Mash et al., 2015; Tao et al., 2015; Odnoletkova et al., 2016; Varney et al., 2016; Elliott et al., 2017; Lian et al., 2017; Lian et al., 2019) were extrapolated between 3 years to a lifetime horizon in estimating the long-term cost-effectiveness of the educational interventions.
This section summarized the cost-effectiveness of each type of educational intervention. The types of educational interventions were divided into face-to-face education, structured education programs, telemedicine health education, others (peer education via discussion; self-management education, and support), and combination. To sum it up generally, out of the 27 studies included, only two educational interventions (Simon et al., 2008; Tao et al., 2015) were considered not cost-effective. The cost-effectiveness of one study (Davies et al., 2001) was not determined and the remaining economic evaluations have shown evidence of the cost-effectiveness of educational interventions delivered to T2DM people. Except for these three studies, the interventions were found to be cost-effective when compared to the comparator.
In general, seventeen studies have reported positive health outcomes linked to educational interventions. The changes in the HbA1c level were the most common health effect observed. The studies that utilized the HbA1c level as their main parameter demonstrated positive health benefits either a significant reduction of HbA1c level are achieved or the level remained controlled throughout the studies. Other significant positive outcomes include a reduction in the number of days of hyperglycaemic episodes, the development of complications, hospitalization rates, and mortality due to T2DM.
Furthermore, educational interventions were associated with cost reduction to obtain health benefits in nine studies (Davies et al., 2001; Banister et al., 2004; Keers et al., 2005; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012; Elliott et al., 2016; Johansson et al., 2017; Wu et al., 2018). Medication adherence assessments were only found to be performed in two studies (Brennan et al., 2012; Elliott et al., 2016). These details can be briefly viewed in Table 2.
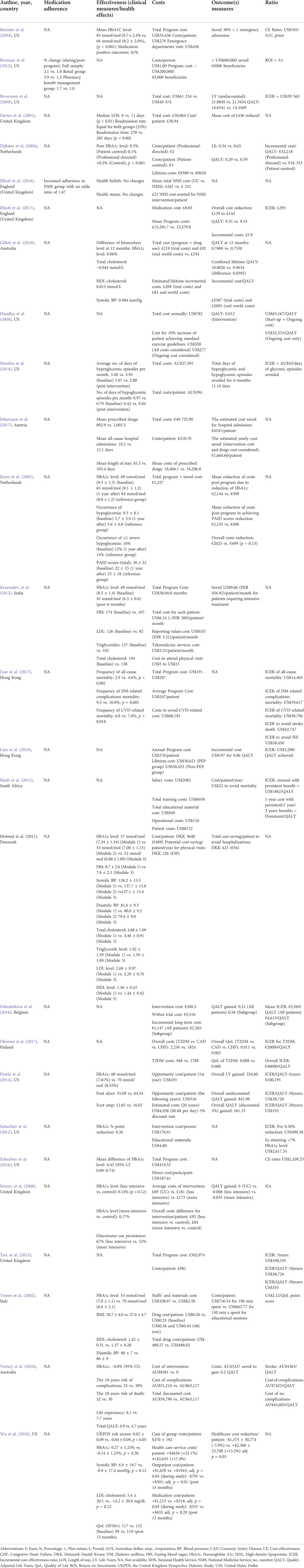
TABLE 2. Effectiveness and economic outcomes of a systematic review of the cost-effectiveness of different types of educational interventions in type II diabetes mellitus.
There are a total of four studies that conducted group-based education, while the remaining three interventions performed the education session individually. All studies were reported to be cost-effective and cost-saving (Banister et al., 2004; Keers et al., 2005; Wu et al., 2018) along with their positive clinical effects. The clinical findings showed a reduction in HbA1c levels (Trento et al., 2002; Banister et al., 2004; Keers et al., 2005; Prezio et al., 2014), hyperglycaemic and hypoglycaemic episodes (Hendrie et al., 2014), diabetes-related stress scores (Keers et al., 2005), and other biomarkers level (Trento et al., 2002). However, Mash et al. (2015) did not report the clinical effects resulting from the intervention given, and no clinical benefits were gained from one study (Wu et al., 2018). Medication adherence assessments were not conducted in any of the studies.
A total of six studies assessed the structured education programs delivered in the management of T2DM people with the majority (n = 5) reporting favorable cost-effectiveness outcomes. A study reported an inconclusive cost-effectiveness result (Davies et al., 2001). The study by Moldsted et al. (2012) presented a cost reduction associated with the implementation of the program (Molsted et al., 2012). The health advantages obtained from this component of intervention include a shorter readmission rate (Davies et al., 2001), lower HbA1c level (Dijkstra et al., 2006), other biomarkers levels (Gillett et al., 2010), mortality (Lian et al., 2017; Lian et al., 2019), and fewer physical visits (Molsted et al., 2012).
A total of six studies incorporated in the review discussed the implementation of the telemedicine approach to provide health education. Only one study reported a higher medication adherence (Brennan et al., 2012). Besides that, telemedicine health education was considered cost-effective in four studies and cost reduction was observed in two studies (Brennan et al., 2012; Kesavadev et al., 2012). T2DM people receiving this intervention were presented with reduced blood glucose and other biomarker levels (Kesavadev et al., 2012; Schechter et al., 2012; Varney et al., 2016); a lower risk of complications (Varney et al., 2016), and a higher quality of life (Oksman et al., 2017). Two studies did not report any clinical changes (Brennan et al., 2012; Oksman et al., 2017).
The remaining six studies utilized the combinations of educational interventions mentioned above for the management of people with T2DM. The majority of the studies demonstrated cost-effectiveness and cost reduction except for one study that concluded that the intervention is not cost-effective (Tao et al., 2015). Only one study recorded a reduction in HbA1c level (Schechter et al., 2016) while the remainder of the papers did not provide clinical effectiveness estimates. Improvements in medication adherence were also observed in a study by Elliott et al. (2016).
Only one study assessed peer discussions related to the management and treatment of T2DM as a type of health educational strategy (Johansson et al., 2017). It was found to be cost-saving and associated with positive health outcomes including hospital admissions. Another study found that integrating self-management education and people support had negative health outcomes and was not cost-effective for T2DM people (Simon et al., 2008).
The results of the quality assessment were presented in Table 3. About half of the studies (n = 13) included in the review were classified as high quality (Dijkstra et al., 2006; Simon et al., 2008; Brownson et al., 2009; Gillett et al., 2010; Hendrie et al., 2014; Prezio et al., 2014; Tao et al., 2015; Odnoletkova et al., 2016; Schechter et al., 2016; Varney et al., 2016; Elliott et al., 2017; Lian et al., 2017; Lian et al., 2019), while the other half (n = 13) demonstrated a modest-quality (Davies et al., 2001; Trento et al., 2002; Keers et al., 2005; Handley et al., 2008; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012; Mash et al., 2015; Elliott et al., 2016; Schechter et al., 2016; Johansson et al., 2017; Oksman et al., 2017; Wu et al., 2018). Only one study was subjected to poor quality (Banister et al., 2004).
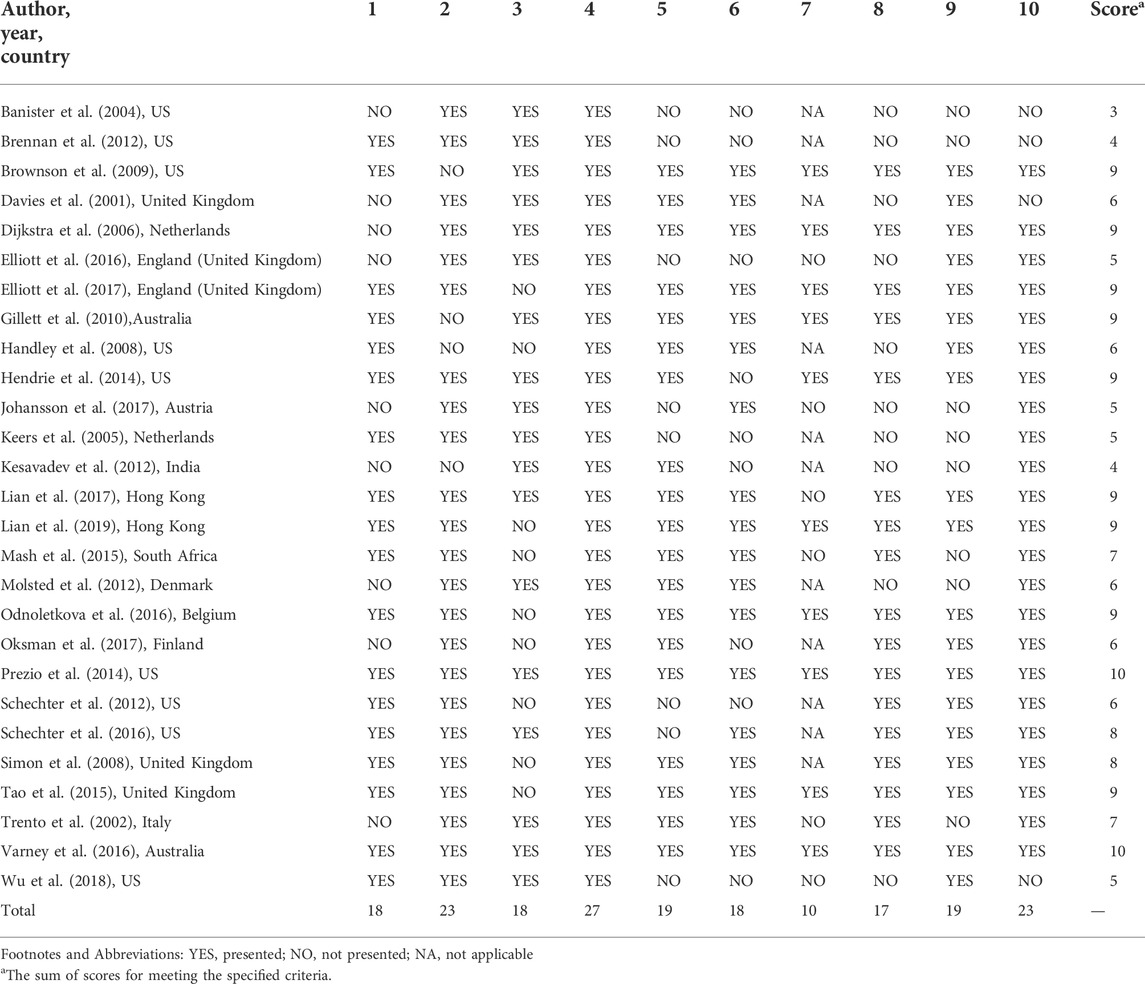
TABLE 3. Quality assessment of a systematic review of the cost-effectiveness of different types of educational interventions in type II diabetes mellitus.
Twenty-three studies (excluding (Handley et al., 2008; Brownson et al., 2009; Gillett et al., 2010; Kesavadev et al., 2012)) successfully provided a detailed explanation regarding the comparator in the studies. The relevant costs and effects of the interventions were sufficiently established in all studies (n = 27). Almost 70% of the studies (excluding (Banister et al., 2004; Keers et al., 2005; Brennan et al., 2012; Schechter et al., 2012; Elliott et al., 2016; Schechter et al., 2016; Johansson et al., 2017; Wu et al., 2018)) expressed the outcomes according to their appropriate physical units, while another 67% (excluding (Banister et al., 2004; Keers et al., 2005; Brennan et al., 2012; Kesavadev et al., 2012; Schechter et al., 2012; Hendrie et al., 2014; Elliott et al., 2016; Oksman et al., 2017; Wu et al., 2018)) were able to report the credible value of its overall costs and effects. Only six studies (6/16, 37.5%) were unable to report the use of discounting approach for studies longer than 12 months in duration that required timing adjustments (Trento et al., 2002; Mash et al., 2015; Elliott et al., 2016; Johansson et al., 2017; Lian et al., 2017; Wu et al., 2018). Meanwhile, the robustness of the outcomes of the study cannot be confirmed in eight studies as sensitivity analyses were not conducted (Trento et al., 2002; Banister et al., 2004; Keers et al., 2005; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012; Mash et al., 2015; Johansson et al., 2017). Twenty-three studies (excluding (Davies et al., 2001; Banister et al., 2004; Brennan et al., 2012; Wu et al., 2018)) took into consideration the transferability of the outcomes concerning the use of interventions in the real world. The explicit incremental cost-effectiveness ratio (ICER) value was presented in seventeen studies [excluding (Davies et al., 2001; Banister et al., 2004; Keers et al., 2005; Handley et al., 2008; Brennan et al., 2012; Kesavadev et al., 2012; Molsted et al., 2012; Elliott et al., 2016; Johansson et al., 2017; Wu et al., 2018)].
Eighteen studies described the view of economic perspectives such as health care and health system (Handley et al., 2008; Simon et al., 2008; Brownson et al., 2009; Brennan et al., 2012; Hendrie et al., 2014; Prezio et al., 2014; Odnoletkova et al., 2016; Varney et al., 2016), societal (Keers et al., 2005; Gillett et al., 2010; Mash et al., 2015; Lian et al., 2017; Lian et al., 2019), provider (Schechter et al., 2012; Schechter et al., 2016) and payer (Tao et al., 2015; Elliott et al., 2017; Wu et al., 2018).
Furthermore, fourteen studies presented the year where the costs were indexed, ranging from 1997 up to 2017 (Davies et al., 2001; Trento et al., 2002; Keers et al., 2005; Simon et al., 2008; Molsted et al., 2012; Schechter et al., 2012; Hendrie et al., 2014; Mash et al., 2015; Tao et al., 2015; Schechter et al., 2016; Varney et al., 2016; Elliott et al., 2017; Wu et al., 2018; Lian et al., 2019). The study by Banister et al. (2004) was still included because they adequately documented the comparative outcomes between the costs and health benefits despite the poor methodology conduct (Banister et al., 2004).
Successful and cost-effective strategies to prevent or delay the onset and progression of T2DM are necessary to relieve the clinical and economic burden borne by the health care system and the people. Few studies reported promising outcomes over the implementation of health education for T2DM people. This systematic review gathers available evidence in providing updated information on the cost-effectiveness of types of educational interventions in improving peoples’ medication adherence and treatment compliance. The inclusion of various types of educational interventions is regarded as one of the strengths in this review for providing a more holistic view of its cost-effectiveness values. To summarize, 24 studies have shown to be cost-effective while the remaining three studies yielded a different conclusion. A study classified as a combined type of approach (Tao et al., 2015) and other types utilizing self-management education and people support (Simon et al., 2008) were determined to be not cost-effective. Davies et al. (2001) found the cost-effectiveness of structured programs to be inconclusive, owing to insufficient economic assessment (Davies et al., 2001). The majority of the studies were classified as having moderate-to-high quality studies.
Overall, the most cost-effective type of educational intervention cannot be determined due to the differences in the adopted perspective and methods in those studies. The differences in the reported outcomes of the studies cannot be compared directly across the categories of interventions because each study employed a different approach to economic evaluations, each with a specific purpose, comprising of various descriptions of perspectives and intended outcomes. The preferences, values, and criteria of the stakeholders requiring health economic assessment data are responsible for the selection of types of economic evaluation. The types of economic evaluations will address a wide range of objectives such as productive efficiency, allocative efficiency, social welfare, and policy depending on the description of the value of health from the perspective of the specified stakeholders. In this review, about half of the studies were in the form of either CEA or CUA, which mainly focuses on the productive efficiency of the interventions and some issues of allocative efficiency. This will also have an impact on the costing methods such as identification, measurement, precision, and valuation of the cost estimates as well as the weighting of various aspects of health outcomes. Although the societal perspective is recommended to be used for economic evaluation because it encompasses a wider range of viewpoints, only Keers et al. (2005) applied this perspective. Still, Keers et al. (2005) did not consider all costs such as intangible costs that are necessary to represent the social value. Furthermore, the level of precision of estimates varies widely for the program costs. For example, the program costs in a study by Banister et al. (2004) include the costs of educators’ salaries, glucometer kits, testing strips, and room rentals while Molsted et al. (2012) cover the costs for the educators’ salary, education materials, and maintenance. This, in turn, leads to different results and recommendations depending on the perspective attributed to the analysis. A larger number of studies should be included in the next review to allow for the comparison of studies using similar economic evaluation approaches to produce more homogeneous results. Furthermore, researchers are recommended to use standard guidelines to conduct an economic evaluation to improve the reliability of the outcomes. Furthermore, improving transparency and reporting in original studies and developments of frameworks and tools will further aid in the assessment of transferability issues in health economic evaluations (Kim et al., 2019; García-Mochón et al., 2021; Weise et al., 2022). Additionally, multi-national economic evaluations, international cost catalogues, and an open-source platform are prospective approaches to improving the transferability (Kim et al., 2019).
The timing issue is the main thing to be addressed in the study design, to have a good approximation and relevance of specified costs and health outcomes with T2DM disease progression. This is especially important and relevant in the case of T2DM because their financial and clinical implications become apparent only after years of interventions. In contrast to clinical trials, model-based economic evaluation is generally useful in providing evidence of long-term cost-effectiveness (Brownson et al., 2009). Long-term effects and costs are excluded from a trial design (Elliott et al., 2017), and performing a trial for long-term assessment could lead to a very costly and impractical intervention (Brownson et al., 2009). The employed time horizon also affected the value of health and economic outcomes, whereby in this review, the shortest time horizon recorded was 6 months (Kesavadev et al., 2012; Hendrie et al., 2014). The relatively short time horizon could not adequately evaluate the full potential of the cost-effectiveness of the diabetes management education program (Hendrie et al., 2014). For example, the emergence of T2DM complications and mortality better represent the overall and long-term effectiveness of interventions, and these outcomes could only be captured in a long-term study design. A longer time horizon may yield the opposite outcomes, where costs associated with reductions in disease progression to improve quality of life can be captured, proving the robustness of the cost-effectiveness in a pragmatic long-term duration (Brownson et al., 2009). The positive cost-effectiveness of all model-based studies in this review, with some even projecting to the lifetime horizon, may represent that the cost-effectiveness of educational intervention can be sustained over time. However, the cost-effectiveness results from the model-based design should be interpreted with caution considering a few assumptions and limitations made for the projection of the outcomes.
To date, the closest review to our study would be the systematic review of the cost-effectiveness of people education models by Loveman et al. (2003) in the management of DM. This review includes both type I and type II diabetes mellitus, and the author concluded that education as part of intensified treatment intervention in type I people could result in improvement in metabolic control and decrease the risk of developing diabetes-related complications. In contrast, inconsistent results were obtained for T2DM mainly due to a diversity of educational programs. In comparison to our study, the studies included were outdated as most of them were published in the 1990s, ranging from 1985 up to 2002. The authors also concluded that the quality of reporting and methodology of the studies was generally poor by today’s standards. Even, the most recent systematic review identified includes articles up to the publication date of 2014 and concludes that there are growing numbers of studies during the study period (Odnoletkova et al., 2014). Our review further updated the evidence where all the articles were published in the 2000s, which most concentrated from the year 2010. With further improvement and acceptance of the guidelines to conduct economic evaluation, we found that most of the articles published in past years adequately satisfy the quality standards of methodological conduct. Apart from updating the current evidence and quality standards of published articles, our review comprises all study designs including trials, cohort, and model-based studies, to provide a comprehensive overview of the shreds of evidence on educational interventions.
Another issue worth mentioning is regarded to publication bias, in the context of the study’s settings. The majority of the studies were concentrated in developed countries, where resources and skills for implementing educational interventions are well established. The need to provide training and development of materials for the program in low- and middle-income countries may require extra costs and resources. This may have an impact on the cost-effectiveness values of educational programs in this setting. Furthermore, the hypothetical study design of some model-based economic evaluations may limit the transferability of the findings in a real-world setting.
Nonetheless, there were some limitations to this review. The exclusion of non-English articles due to language barriers and Grey literature may reduce the number of articles retrieved, eventually affecting the quantity and comprehensiveness of evidence.
This systematic review sheds light on the cost-effectiveness of educational interventions in achieving optimal and planned diabetes care in managing T2DM. An appropriate and adequate knowledge and skills to manage T2DM and its complications are the necessary elements to achieve the effects of educational intervention, regardless of the type of educational intervention. Enhancement of awareness, knowledge, attitude and self-care are the main elements of educational interventions in helping people to manage diabetes and its complications as well as the need to adopt a positive lifestyle. Although the characteristics and magnitude of implementation of educational interventions are different, most of the interventions are considered cost-effective to improve the health benefits and quality of life of the people. The identified educational interventions would result in positive health benefits, lowering the risk of complications and improving the quality of life eventually leading to a significant reduction in the burden cost of this disease on the people and the health care system. Good quality and preferably long-term health economic studies utilizing societal perspectives are still needed. High-quality evidence will help in guiding and improving the healthcare decision-making process and allow the proper allocation of healthcare resources in the effort of maximizing the health benefits. More research that correlates the economic evaluation and aspects of educational interventions is needed to allow a more comprehensive implication of these interventions on the people’s awareness, knowledge, attitude, and self-enhancement toward T2DM care.
All types of educational interventions are highly likely to be cost-effective. The quality of economic evaluations is moderate but the most cost-effective types of educational interventions could not be determined due to variations in the reporting and methodological conduct of the study. A high-quality approach, preferably utilizing the societal perspective over a long period, should be standardized to conduct economic evaluations for educational interventions in T2DM.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The authors (WW and NAMT) contributed equally to this work. WW and NAMT contributed to the design of the study, literature search, and data analysis. WW identified eligible trials, extracted the data, and assessed the quality of clinical trials and NAMT further review the process. WW and NAMT provided some ideas for this study. WW processed the data and generated the tables and figures and NAMT further review the data, tables, and figures. WW and NAMT contributed to the interpretation of the data. WW drafted the manuscript and NAMT critically revised the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ADA (2018). Economic costs of diabetes in the us in 2017. Diabetes Care 41, 917–928. doi:10.2337/dci18-0007
Ahmed, M. M., El Degwy, H. M., Ali, M. I., and Hegazy, N. H. (2015). The effect of educational intervention on knowledge, attitude and glycemic control in patients with type 2 diabetes mellitus. Int. J. Community Med. Public Health, 302–307. doi:10.18203/2394-6040.ijcmph20150487
Banister, N. A., Jastrow, S. T., Hodges, V., Loop, R., and Gillham, M. B. (2004). Diabetes self-management training program in a community clinic improves patient outcomes at modest cost. J. Am. Diet. Assoc. 104, 807–810. doi:10.1016/j.jada.2004.02.027
Brennan, T. A., Dollear, T. J., Hu, M., Matlin, O. S., Shrank, W. H., Choudhry, N. K., et al. (2012). An integrated pharmacy-based program improved medication prescription and adherence rates in diabetes patients. Health Aff. 31, 120–129. doi:10.1377/hlthaff.2011.0931
Brownson, C. A., Hoerger, T. J., Fisher, E. B., and Kilpatrick, K. E. (2009). Cost-effectiveness of diabetes self-management programs in community primary care settings. Diabetes Educ. 35, 761–769. doi:10.1177/0145721709340931
Cho, N. H., Shaw, J. E., Karuranga, S., Huang, Y., Da Rocha Fernandes, J. D., Ohlrogge, A. W., et al. (2018). IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 138, 271–281. doi:10.1016/j.diabres.2018.02.023
Davies, M., Dixon, S., Currie, C. J., Davis, R. E., and Peters, J. R. (2001). Evaluation of a hospital diabetes specialist nursing service: A randomized controlled trial. Diabet. Med. 18, 301–307. doi:10.1046/j.1464-5491.2001.00470.x
Dijkstra, R. F., Niessen, L. W., Braspenning, J. C., Adang, E., and Grol, R. T. (2006). Patient-centred and professional-directed implementation strategies for diabetes guidelines: A cluster-randomized trial-based cost-effectiveness analysis. Diabet. Med. 23, 164–170. doi:10.1111/j.1464-5491.2005.01751.x
Doran, C. M. (2008). Economic evaluation of interventions to treat opiate dependence : A review of the evidence. Pharmacoeconomics 26, 371–393. doi:10.2165/00019053-200826050-00003
Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., and Torrance, G. W. (2015). Methods for the economic evaluation of health care programmes. Oxford University Press.
Elliott, R. A., Boyd, M. J., Salema, N. E., Davies, J., Barber, N., Mehta, R. L., et al. (2016). Supporting adherence for people starting a new medication for a long-term condition through community pharmacies: A pragmatic randomised controlled trial of the new medicine service. BMJ Qual. Saf. 25, 747–758. doi:10.1136/bmjqs-2015-004400
Elliott, R. A., Tanajewski, L., Gkountouras, G., Avery, A. J., Barber, N., Mehta, R., et al. (2017). Cost effectiveness of support for people starting a new medication for a long-term condition through community pharmacies: An economic evaluation of the new medicine service (NMS) compared with normal practice. Pharmacoeconomics 35, 1237–1255. doi:10.1007/s40273-017-0554-9
García-Mochón, L., Rovira Forns, J., and Espin, J. (2021). Cost transferability problems in economic evaluation as a framework for an European health care and social costs database. Cost. Eff. Resour. Alloc. 19, 43. doi:10.1186/s12962-021-00294-4
Gillett, M., Dallosso, H. M., Dixon, S., Brennan, A., Carey, M. E., Campbell, M. J., et al. (2010). Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: Cost effectiveness analysis. BMJ 341, c4093. doi:10.1136/bmj.c4093
Handley, M. A., Shumway, M., and Schillinger, D. (2008). Cost-effectiveness of automated telephone self-management support with nurse care management among patients with diabetes. Ann. Fam. Med. 6, 512–518. doi:10.1370/afm.889
Hendrie, D., Miller, T. R., Woodman, R. J., Hoti, K., and Hughes, J. (2014). Cost-effectiveness of reducing glycaemic episodes through community pharmacy management of patients with type 2 diabetes mellitus. J. Prim. Prev. 35, 439–449. doi:10.1007/s10935-014-0368-x
Johansson, T., Keller, S., Sönnichsen, A. C., and Weitgasser, R. (2017). Cost analysis of a peer support programme for patients with type 2 diabetes: A secondary analysis of a controlled trial. Eur. J. Public Health 27, 256–261. doi:10.1093/eurpub/ckw158
Keers, J. C., Groen, H., Sluiter, W. J., Bouma, J., and Links, T. P. (2005). Cost and benefits of a multidisciplinary intensive diabetes education programme. J. Eval. Clin. Pract. 11, 293–303. doi:10.1111/j.1365-2753.2005.00536.x
Keith Campbell, R. (20092003). Type 2 diabetes: Where we are today: An overview of disease burden, current treatments, and treatment strategies. J. Am. Pharm. Assoc. 49, S3–S9. doi:10.1331/JAPhA.2009.09077
Kesavadev, J., Shankar, A., Pillai, P. B., Krishnan, G., and Jothydev, S. (2012). Cost-effective use of telemedicine and self-monitoring of blood glucose via Diabetes Tele Management System (DTMS) to achieve target glycosylated hemoglobin values without serious symptomatic hypoglycemia in 1, 000 subjects with type 2 diabetes mellitus--a retrospective study. Diabetes Technol. Ther. 14, 772–776. doi:10.1089/dia.2012.0088
Kim, D. D., Bacon, R. L., and Neumann, P. J. (2019). “Assessing the transferability of economic evaluations: A decision framework,” in Non-communicable disease prevention: Best buys, wasted buys and contestable buys. Editors W. Isaranuwatchai, R. A. Archer, Y. Teerawattananon, and A. J. Culyer (United Kingdom: Open Book Publishers), 91–117. doi:10.11647/OBP.0195.06
Lian, J., Mcghee, S. M., So, C., Chau, J., Wong, C. K. H., Wong, W. C. W., et al. (2017). Five-year cost-effectiveness of the Patient Empowerment Programme (PEP) for type 2 diabetes mellitus in primary care. Diabetes Obes. Metab. 19, 1312–1316. doi:10.1111/dom.12919
Lian, J., Mcghee, S. M., So, C., Chau, J., Wong, C. K. H., Wong, W. C. W., et al. (2019). Long-term cost-effectiveness of a Patient Empowerment Programme for type 2 diabetes mellitus in primary care. Diabetes Obes. Metab. 21, 73–83. doi:10.1111/dom.13485
Loveman, E., Cave, C., Green, C., Royle, P., Dunn, N., Waugh, N., et al. (2003). The clinical and cost-effectiveness of patient education models for diabetes: A systematic review and economic evaluation. Health Technol. Assess. 7, 1–190. doi:10.3310/hta7220
Mash, R., Kroukamp, R., Gaziano, T., and Levitt, N. (2015). Cost-effectiveness of a diabetes group education program delivered by health promoters with a guiding style in underserved communities in Cape Town, South Africa. Patient Educ. Couns. 98, 622–626. doi:10.1016/j.pec.2015.01.005
Merakou, K., Knithaki, A., Karageorgos, G., Theodoridis, D., and Barbouni, A. (2015). Group patient education: Effectiveness of a brief intervention in people with type 2 diabetes mellitus in primary health care in Greece: A clinically controlled trial. Health Educ. Res. 30, 223–232. doi:10.1093/her/cyv001
Mohamed, A., Staite, E., Ismail, K., and Winkley, K. (2019). A systematic review of diabetes self-management education interventions for people with type 2 diabetes mellitus in the Asian Western Pacific (AWP) region. Nurs. Open 6, 1424–1437. doi:10.1002/nop2.340
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6, e1000097. doi:10.1371/journal.pmed.1000097
Molsted, S., Tribler, J., Poulsen, P., and Snorgaard, O. (2012). The effects and costs of a group-based education programme for self-management of patients with Type 2 diabetes. A community-based study. Health Educ. Res. 27, 804–813. doi:10.1093/her/cyr053
Odnoletkova, I., Goderis, G., Pil, L., Nobels, F., Aertgeerts, B., Annemans, L., et al. (2014). Cost-effectiveness of therapeutic education to prevent the development and progression of type 2 diabetes: Systematic review. Diabetes Metab. 5, 1–7. doi:10.4172/2155-6156.1000438
Odnoletkova, I., Ramaekers, D., Nobels, F., Goderis, G., Aertgeerts, B., Annemans, L., et al. (2016). Delivering diabetes education through nurse-led telecoaching. Cost-effectiveness analysis. PLoS One 11, e0163997. doi:10.1371/journal.pone.0163997
Oksman, E., Linna, M., Hörhammer, I., Lammintakanen, J., and Talja, M. (2017). Cost-effectiveness analysis for a tele-based health coaching program for chronic disease in primary care. BMC Health Serv. Res. 17, 138. doi:10.1186/s12913-017-2088-4
Prezio, E. A., Pagán, J. A., Shuval, K., and Culica, D. (2014). The community diabetes education (CoDE) program: Cost-effectiveness and health outcomes. Am. J. Prev. Med. 47, 771–779. doi:10.1016/j.amepre.2014.08.016
Schechter, C. B., Cohen, H. W., Shmukler, C., and Walker, E. A. (2012). Intervention costs and cost-effectiveness of a successful telephonic intervention to promote diabetes control. Diabetes Care 35, 2156–2160. doi:10.2337/dc12-0048
Schechter, C. B., Walker, E. A., Ortega, F. M., Chamany, S., and Silver, L. D. (2016). Costs and effects of a telephonic diabetes self-management support intervention using health educators. J. Diabetes Complicat. 30, 300–305. doi:10.1016/j.jdiacomp.2015.11.017
Sigurdardottir, A. K., Jonsdottir, H., and Benediktsson, R. (2007). Outcomes of educational interventions in type 2 diabetes: WEKA data-mining analysis. Patient Educ. Couns. 67, 21–31. doi:10.1016/j.pec.2007.03.007
Simon, J., Gray, A., Clarke, P., Wade, A., Neil, A., and Farmer, A. (2008). Cost effectiveness of self monitoring of blood glucose in patients with non-insulin treated type 2 diabetes: Economic evaluation of data from the DiGEM trial. BMJ 336, 1177–1180. doi:10.1136/bmj.39526.674873.BE
Tao, L., Wilson, E. C., Wareham, N. J., Sandbaek, A., Rutten, G. E., Lauritzen, T., et al. (2015). Cost-effectiveness of intensive multifactorial treatment compared with routine care for individuals with screen-detected type 2 diabetes: Analysis of the ADDITION-UK cluster-randomized controlled trial. Diabet. Med. 32, 907–919. doi:10.1111/dme.12711
Trento, M., Passera, P., Bajardi, M., Tomalino, M., Grassi, G., Borgo, E., et al. (2002). Lifestyle intervention by group care prevents deterioration of type II diabetes: A 4-year randomized controlled clinical trial. Diabetologia 45, 1231–1239. doi:10.1007/s00125-002-0904-8
Varney, J. E., Liew, D., Weiland, T. J., Inder, W. J., and Jelinek, G. A. (2016). The cost-effectiveness of hospital-based telephone coaching for people with type 2 diabetes: A 10 year modelling analysis. BMC Health Serv. Res. 16, 521. doi:10.1186/s12913-016-1645-6
Weise, A., Büchter, R. B., Pieper, D., and Mathes, T. (2022). Assessing transferability in systematic reviews of health economic evaluations – A review of methodological guidance. BMC Med. Res. Methodol. 22, 52. doi:10.1186/s12874-022-01536-6
WHO (2021). Diabetes [online]. Available: http://www.who.int/diabetes/en/(Accessed February 11, 2021).
Wild, S., Roglic, G., Green, A., Sicree, R., and King, H. (2004). Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 27, 1047–1053. doi:10.2337/diacare.27.5.1047
Wu, W. C., Taveira, T. H., Jeffery, S., Jiang, L., Tokuda, L., Musial, J., et al. (2018). Costs and effectiveness of pharmacist-led group medical visits for type-2 diabetes: A multi-center randomized controlled trial. PLoS One 13, e0195898. doi:10.1371/journal.pone.0195898
Zhang, Y., and Chu, L. (2018). Effectiveness of systematic health education model for type 2 diabetes patients. Int. J. Endocrinol. 2018, 6530607. doi:10.1155/2018/6530607
Zhou, C., and Byard, R. W. (2018). An analysis of the morbidity and mortality of diabetes mellitus in a forensic context. J. Forensic Sci. 63, 1149–1154. doi:10.1111/1556-4029.13674
Keywords: pharmacoeconomic, systematic review, diabetes mellitus, educational intervention, cost-effectiveness
Citation: Wan Rohimi WNLH and Mohd Tahir NA (2022) The cost-effectiveness of different types of educational interventions in type II diabetes mellitus: A systematic review. Front. Pharmacol. 13:953341. doi: 10.3389/fphar.2022.953341
Received: 26 May 2022; Accepted: 04 July 2022;
Published: 22 July 2022.
Edited by:
Ileana Mardare, Carol Davila University of Medicine and Pharmacy, RomaniaReviewed by:
Yen-Ming Huang, National Taiwan University, TaiwanCopyright © 2022 Wan Rohimi and Mohd Tahir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nurul Ain Mohd Tahir, bnVydWxhaW5tdEB1a20uZWR1Lm15
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.