- 1Clinical Pharmacist, Al Galaa Military Medical Complex, Cairo, Egypt
- 2Clinical Pharmacy Department, Faculty of Pharmacy, Ain Shams University, Cairo, Egypt
- 3Assistant Director of the Military Medical Services, Cairo, Egypt
Background: Community-acquired pneumonia (CAP) is one of the most common infectious diseases affecting the respiratory tract and is responsible for a high mortality rate in children less than 5 years of age. The mortality rate due to CAP is much higher in low/middle-income countries than in high-income countries due to malnutrition and different micronutrient deficiencies that weaken the immune system.
Aim: The aim of this study was to compare the effects of zinc and vitamin A, as two elements of micronutrient agents, on the recovery rate of children suffering from CAP aged from 6 months to 5 years. The length of hospital stays was also investigated.
Method: A comparative, randomized, open-label, controlled, interventional study was carried out among children less than 5 years of age in the pediatric intensive care unit (PICU) diagnosed with CAP who were randomly divided into three groups. In addition to the standard therapy, group 1 was given zinc, group 2 was given vitamin A, and group 3 was the control group, given the standard therapy only. We compared the three groups in terms of recovery rate and hospital stay.
Result: The duration of hospitalization following zinc and vitamin A supplementation was reduced by an average of 3.21 days (95% CI: 5.01–1.41, p = 0.01) and 2.43 days (95% CI: 4.29–0.57, p = 0.01), respectively, compared to the control group. In addition, the two groups of vitamin A and zinc supplementation were associated with a shorter duration of pneumonic effusion (p < 0.001) in comparison to the control group. Additionally, there was no significant difference between the effects of zinc and vitamin A when compared to each other in terms of duration of hospital stay and pneumatic effusion.
Conclusion: The administration of zinc or vitamin A supplementation proved to be useful as an add-on therapy in community-acquired pneumonia, where it reduced the length of hospital stay and the duration of pneumonic effusion in pneumonic children less than 5 years of age.
Introduction
Pneumonia is one of the infectious diseases that affect the lower respiratory tract system (Katz and Williams, 2018). Pneumonia is an acute infection affecting the lung and alveoli that can be caused by many different micro-organisms (viruses, bacteria, or fungi) (Li et al., 2020). in which pathogens enter the lung, causing inflammation and weakening the gas exchange mechanism between alveoli and pulmonary capillaries (Jafarzadeh and Oscuii, 2019; Hamed et al., 2019).
Community-acquired pneumonia (CAP) is the most common type of pneumonia where individuals are affected by the pathogen away from hospitals or other healthcare facilities (Symington and Scott, 2017). In addition, it is considered a leading cause of morbidity and mortality around the world, especially in children under 5 years of age (Hamed et al., 2019; Harel-Sterling et al., 2019).
Additionally, community-acquired pneumonia is defined as an acute infection of the pulmonary parenchyma associated with at least some symptoms of acute infection, accompanied by the presence of an acute infiltrate on a chest radiograph or auscultatory finding consistent with pneumonia (such as altered breath sound and/or localized roles), in neither hospitalized patient nor residing in a long-term care facility for more than 14 days before the onset of symptoms (Basnet et al., 2012; Baek et al., 2018).
It is worthy to mention that around the world, CAP is considered the major cause of death in children (Mahalanabis et al., 2002; Srinivasan et al., 2012). Also, every year, millions of children younger than 5 years died; moreover, the annual incidence of pneumonia in children younger than 5 years of age is 34–40 cases per 1000 in high-income countries. On the other hand, the incidence approaches 2 to 10 times higher in low and middle-income countries (LMICs) than in the high-income countries. Regarding the severity of infection and mortality rate, they are higher in LMICs (Srinivasan et al., 2012; Sakulchit, 2017).
One of the most common responsible co-factors for the high incidence of death due to CAP and LMICs is micronutrient deficiencies which have an important role in the regulation of essential defense mechanisms of the human body against infectious diseases and are very essential as well for appropriate cellular and molecular functions, including the cell of immunity system (Schulz et al., 2010; Kuti et al., 2021).
It is well known that childhood malnutrition affects both innate and adaptive immune function in pediatrics as well as impair the ability of the immunity system to produce an appropriate immune response against infections (Basnet et al., 2012; Walker and Black, 2012; Kuti et al., 2021).
Essential micronutrients, including zinc and vitamin A, have an important role in many vital pathways affecting immunity and human health, where, their deficiency is considered one of the risk factors for respiratory infections (Reyes et al., 2002; Hoang and Han, 2021).
Zinc is essential for gene expression and has an important role in nucleic acid and protein synthesis, cell replication, tissue growth and repair, and is vital for the regulation of immune system function and defense mechanisms against infectious micro-organisms (Morse and High, 2018; Wang and Song, 2018; Mumtaz et al., 2019; Hoang and Han, 2021; Jegalakshmi et al., 2022).
Moreover, it could inhibit angiotensin-converting enzyme 2 (ACE2) activity, loading to impair the interaction between the spike proteins of many micro-organisms and the host cells (Skalny et al., 2020; Hunter et al., 2021; Ateya, A.M. et al., 2021).
In addition, it reduces the permeability of the cell membrane and inhibits the transcapillary movement of plasma protein, which results in a consecutive decrease in inflammation and local edema (Hunter et al., 2021). On the other hand, zinc deficiency causes thymus atrophy, decreases T-helper cell and B cell production, and increases the susceptibility of micro-organisms to produce toxins (Skalny et al., 2020; Jalal et al., 2021).
Concerning, vitamin A, it is one of the most important micronutrients, which is essential for many vital functions such as cell growth, epithelial integrity, and immune system response, and is considered an anti-infectious vitamin due to its essential role in immune function by controlling the discrimination of T-helper cells to Th2 and production of interleukin-4 and interleukin-5, regulating the humoral antibody response, and inhibition of bacteria growth (Abd El-Shaheed et al., 2018; Shahzad et al., 2018). Vitamin A also acts as an antioxidant agent, preventing oxidative stress and cell damage (Khadim and Al-Fartusie, 2021).
It is well known that vitamin A is not synthesized in the human body and thus should come from the diet (Erdfelder et al., 1996; Imdad et al., 2017). According to the WHO, there are about 250 million children in LMICs who are suffering from vitamin A deficiency, resulting in a high rate of morbidity and mortality in children less than 5 years old (Abd El-Shaheed et al., 2018).
Many studies have been conducted about the effect of micronutrients in the treatment of CAP and its role in the acceleration of recovery and the decrease of complications and mortality rates in children (Reyes et al., 2002; West, 2003; Shakur et al., 2009; Valavi et al., 2011; Shah et al., 2012; Imdad et al., 2017; Morse and High, 2018; Saleh and Abo El Fotoh, 2018; Wang and Song, 2018; Hoang and Han, 2021; R Prasad et al., 2019). According to our knowledge, there is no comparative study evaluating the effect of zinc versus vitamin A in pediatric pneumonia.
Thus, the aim of our study was to investigate the efficacy and safety of zinc supplementation compared to vitamin A as an adjuvant to the standard protocol of therapy used in the management of pneumonia in pediatric patients. This was performed through the evaluation of the role of each on the recovery rate in pediatric patients with pneumonia in terms of hospital stay and pneumonic effusion duration.
This study was made by collaboration between the physicians of the pediatric intensive care unit and a clinical pharmacist. Physicians diagnose the patient's clinical situation, prescribe the medication, and monitor the vital signs of the patient. While the clinical pharmacist's concern is the optimized use of medication, by making sure that every patient takes his right and optimal medication according to his clinical situation, check the dose and administration, and being aware of the side effect of each drug to decrease the medication error and achieve the optimize use of medication (Hepler, 2004; Alagha et al., 2011).
Patients and methods
Design
A comparative, randomized, open-label, controlled, pilot, and interventional study was carried out from January 2019 until February 2020. All cases included in the study were patients in the intensive care unit due to severe pneumonia. Patients included in the study were randomly divided into three groups with 25 cases in each one.
Setting
Pediatric intensive care unit (PICU) of the pediatric and gynecology specialized hospital at Al Galaa Military Complex and Ghamra military hospital, Cairo, Egypt.
Inclusion criteria
- Patients admitted to the pediatric intensive care unit were diagnosed with community-acquired pneumonia
- Age from 1 to 60 months
- Patient’s health status, which allowed oral medication
Exclusion criteria
Children with known heart disease, children on medication with zinc supplements or vitamin A, children with obstructive air-way disease or known case of asthma, children NPO (nothing by mouth) on a ventilator, children with active measles and known intolerance or allergy to zinc/vitamin A or zinc/vitamin A-containing products.
Method
Sample size calculation
The sample size was calculated by GPower v.3.1.9.4 (Erdfelder, E., Faul, F., and Bates, 1995). According to Lynne M. Connelly (2008), extant literature suggests that a pilot study sample should be around 10% of the sample project for the larger parent study.
Therefore, for a full-scale study, where the main dependent variables are hospital stay and post-treatment laboratory parameters. Using multiple linear regression with seven predictors (baseline value, age, gender, ABW, pneumonia grade, effusion presence, and treatment), expecting a modest effect on hospital stay and laboratory parameters a priori (effect size/Cohen’s f2 = 0.02), with the desired power of 95% to reject the null hypothesis (Ho: no increase in R2 by adding the grouping/treatment variable), and a type-I error probability not more than 0.05. For our pilot study, the required total sample size was decided to be 75 participants, equally allocated among the 3 groups (25 participants in each group).
A total of 75 eligible patients were divided into three groups (Supplementary Figure S1):
• Group (1) (zinc group): patients were administered zinc (Zinc Origin®, zinc sulfate syrup 10mg/5ml, manufacturing by Origin International Pharms, Egypt), in addition to the standard therapy, given for 7 days as follows; 10 mg once daily for children aged less than 1 year, or 20 mg once daily for children aged over 1 year to 5 years
• Group (2) (vitamin A group): in addition to the standard therapy for pneumonia, patients were given vitamin A (A-VITON®, vitamin A 50,000 IU soft gelatin capsule, manufactured by Kahera Pharma-Egypt) for 5 days on the dose of 50,000 international unit (IU) at day one and day five for children aged less than 1 year, or 100,000 international unit (IU) at day one and day five for children aged over 1 year to 5 years
• Group (3) (control group): patients were given the standard therapy and medication for the treatment of pneumonia
The standard therapy consisted of the following medications: empirical antibiotic treatment including vancomycin 15 mg/kg/8 h, meropenem 20 mg/kg/8 h, colistin 25000 IU/kg/8 h, and if suspected anaerobic infection they were given imipenem/cilastatin 20 mg/kg/6 h. The empirical antibiotics were exchanged after culture to sensitive antibiotics. Additionally, empirical antifungal treatment was given in case of suspected infection or for patients who stayed for more than 6 days in the ICU. Fluconazole 6 mg/kg/24h, antipyretic; paracetamol 15 mg/kg/dose up to 6 times daily, inhaler; ipratropium/salbutamol-albuterol, budesonide, saline, and anti-inflammatory agent; dexamethasone 0.15 mg/kg/6 h.
Clinical assessment and laboratory evaluation
1) Physical examination and vital sign assessment: the physician underwent physical investigations daily and nurses assessed body temperature, respiratory rate, and oxygen saturation was monitored daily through pulse oximetry
2) Laboratory data evaluation: on admission and every 3 days assessment of C-reactive protein, arterial blood gases [PCO2, PO2, and pH], kidney function [serum creatinine and blood urea nitrogen (BUN)], and liver function alanine aminotransferase (ALT), aspartate aminotransferase (AST) were performed
3) Monitoring of the expected side effects of the interventional medications: the side effects of zinc supplementation include nausea, vomiting, diarrhea, tarry stool, and stomach pain, while those of vitamin A include nausea, vomiting, diarrhea, liver damage, blurry vision, and skin irritation were monitored daily through a side effect monitoring form, where the appearance of any of the previously mentioned side effects were reported and the method of handling it as well was reported
Outcomes
• Primary outcome: the role of zinc supplementation and vitamin A on the recovery rate in the pediatric patient with pneumonia in terms of hospital stay and pneumonic effusion duration.
• Secondary outcome: evaluation of the safety of zinc supplementation and vitamin A in pediatric patients with pneumonia in terms of proportion of adverse drug events and complications.
Ethical consideration
The study protocol was revised and approved (under no; 228) by the institutional review board of the ethics committee of faculty of pharmacy, Ain Shams University which is registered at the Egyptian Ministry of Health (MOH).
The current study was conducted according to the code of ethics of declaration (Hunter et al., 2021a; Hunter et al., 2021) (Review et al., 2014), communication and principles, and followed the CONSORT guidelines (Schulz et al., 2010; Ateya et al., 2021).
The caregivers of the eligible children were informed about the study and asked to sign a written informed consent before starting the study without any obligation on them to continue if they did not want to.
Statistical analysis
The statistical analysis was performed using R software version 3.6.1. Two-sided p-values less than 0.05 were considered statistically significant. The normality assumption was tested by Shapiro–Wilk’s test; normally distributed continuous data were represented by mean and standard deviation and were compared using Student’s t-test or one-way analysis of variance (ANOVA); skewed data were represented by median and range and were compared using the Mann–Whitney’s test or Kruskal–Wallis test. Tukey’s HSD (honestly significant difference) test was performed after significant ANOVA.
Age was categorized as infants (birth to ≤12 months), toddlers (>12 months to ≤36 months), and preschools (>36 months). Subjects were categorized according to their weight-for-age or weight-for-height to underweight, healthy, overweight, and obese using the CDC and WHO growth charts.
Multiple linear regression analysis was performed to quantify the marginal effect of treatment with vitamin A or zinc (vs. control) on the duration of hospitalization while controlling for age, gender, bodyweight category, pneumonia grade, and presence of effusion. Two-way repeated-measures ANOVAs were also performed to quantify the effect of treatment with vitamin A or zinc on post-treatment vital signs and sepsis-related lab parameters, including temperature, respiratory rate, O2 saturation, hemoglobin level, total leukocyte count, platelet count, CRP, ALT, and serum creatinine.
Results
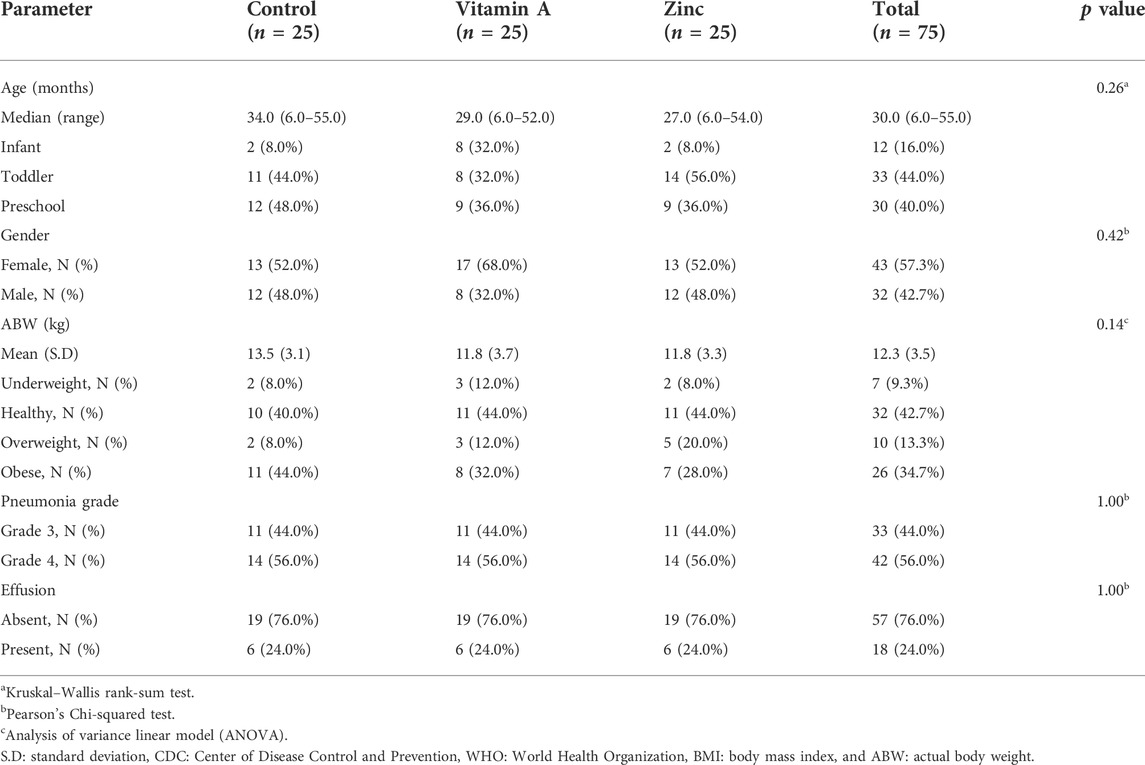
Patients’ demographics
A total of 75 patients completed the study without dropouts. The median age of subjects was 30 months (range: 6–55 months). At baseline, the values of age, gender, actual body weight, and the weight/BMI-to-age or BMI-to-height CDC/WHO weight category, pneumonia grade, and presence/absence of pneumonic effusion were all comparable. Subjects’ baseline demographic characteristics are shown in Table 1.
Laboratory evaluation and physical examinations
At baseline, there was no significant difference in the patients’ clinical laboratory parameters and vital signs among the studied groups; additionally, no participant was presented with markers of organ damage (Table 2).
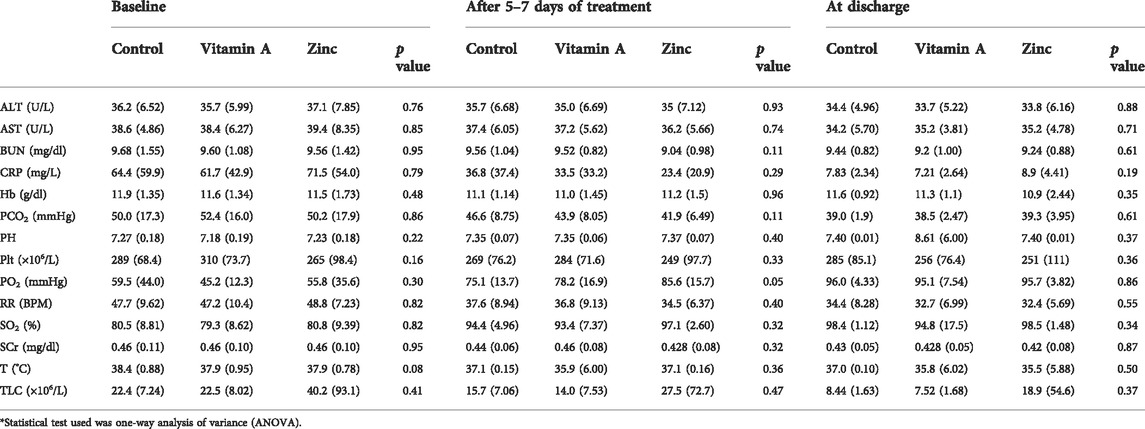
TABLE 2. Values of the patients’ laboratory parameters and vitals at baseline and at the end of the study.
After intervention and at discharge, there was no significant difference among the studied groups concerning the clinical laboratory parameters and vital signs (Table 2). Moreover, no side effects were reported during the study due to the administration of zinc and vitamin A supplementation.
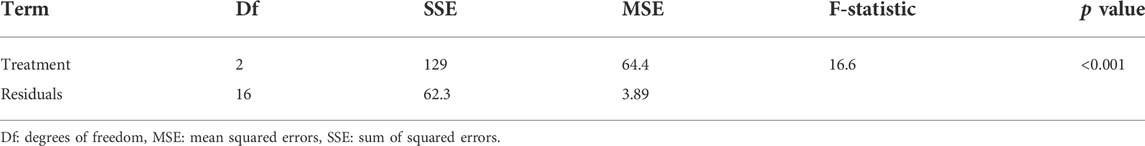
Effect of zinc and vitamin A supplementation on the effusion’s days
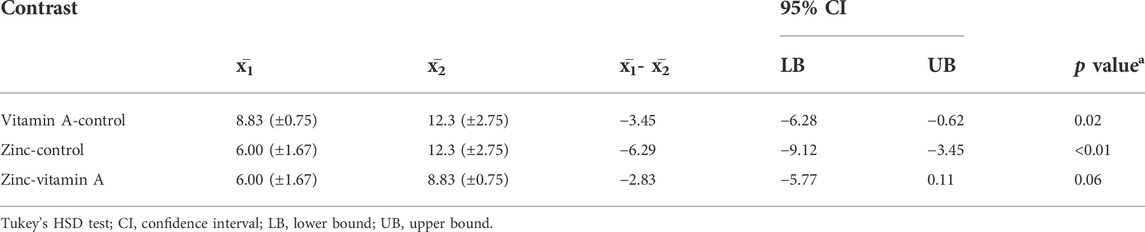
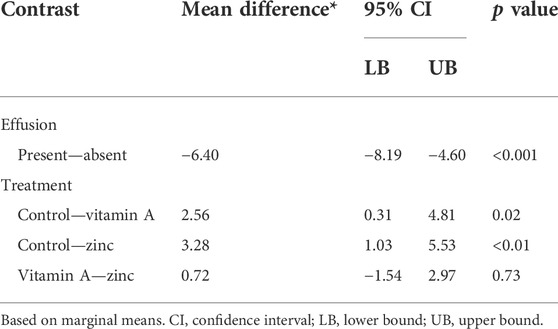
Statistical analysis of the obtained results showed that both groups of vitamin A and zinc were associated with a significantly shorter duration of pneumonic effusion (p-value < 0.001) compared to the control group (Table 3).
Post hoc contrasts showed that the both vitamin A and zinc groups were superior to the control one (Table 4). Duration of effusion was 3 days lower with zinc therapy compared to vitamin A. However, the difference between the effect of zinc and vitamin A was statistically insignificant (p value = 0.06).
Duration of hospitalization
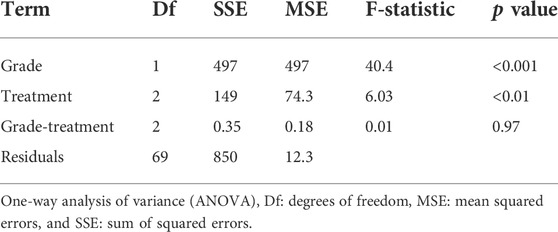
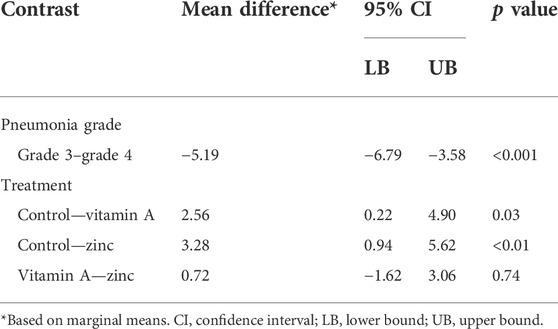
A follow-up two-way ANOVA (Tables 5, 6) showed a non-significant interaction between either pneumonia grade, presence/absence of effusion, and vitamin A/zinc (indicating independence of response to supplementation to pneumonia grade or effusion) (Supplementary Figures S2, S3).
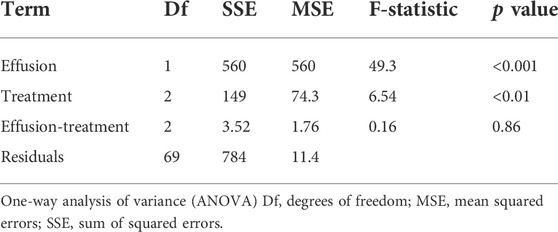
TABLE 5. The duration of hospitalization regarding effusion presence or absence among the studied groups.
Post hoc contrasts (Tables 7, 8) showed that both vitamin A and zinc supplementation were correlated with a significantly shorter duration of hospitalization in days compared to the control group.
In the multiple linear regression analysis (Table 9), vitamin A supplementation marginally reduced the duration of hospitalization by an average of 2.43 days (95% CI: 4.29–−0.57, p-value = 0.01). Similarly, zinc supplementation reduced the duration of hospitalization by an average of 3.21 days (95% CI: 5.01–−1.41, p-value < 0.01). Age, gender, and weight had no significant impact on the duration of hospitalization.
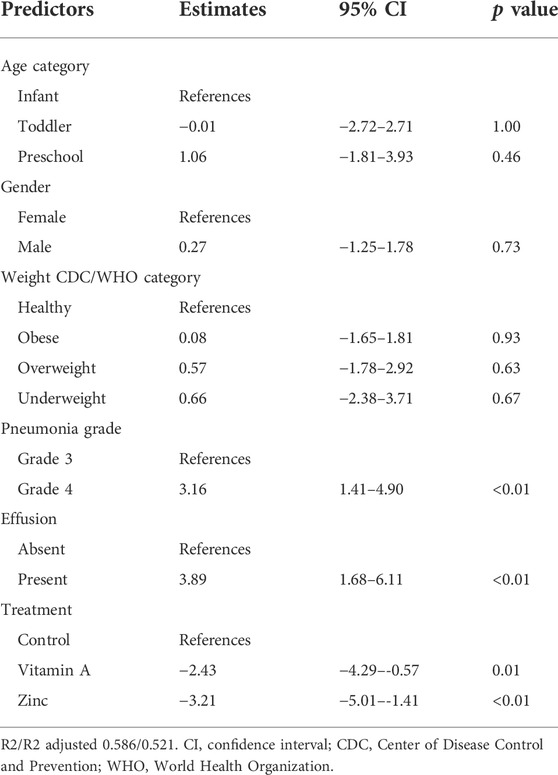
TABLE 9. Impact of vitamin A/zinc supplementation while controlling for demographics and patients’ factors.
Discussion
Zinc and vitamin A are micronutrients that have biological activities related to the immune system and recovery after lower respiratory tract infections, and their concentration is usually reported as lower than required in children of LMICs (Gupta et al., 2020; Afolami, 2021).
Zinc has an essential role in the metabolisms of cells and immunity. Its deficiency causes a defect in the integration of epithelial cells of the lung (Shakur et al., 2009). It is well known that zinc is effective in the treatment of respiratory tract infection (RTI) as it reduces the duration of symptoms as well as decreases the severity of the disease, (Hunter et al., 2021), through its ability to inhibit an angiotensin-converting enzyme 2 (ACE2) and consequently impairs the ability of infection (McPherson et al., 2020). In addition, zinc was found to reduce the percentage of developing mild to moderate symptoms consistent with RTI as it decreases the respiratory rate, body temperature, and influenza-like illnesses (Hunter et al., 2021).
On the other hand, vitamin A is considered one of the broadly studied micronutrients regarding its effect on the immune system (Karter et al., 1995) and is named anti-infectious vitamin owing to its effect on the regulation of human immune function (Bates et al., 1995). It was reported by Zhang et al., and West et al., that vitamin A deficiency causes recurrent respiratory tract infection as it is one of the fat-soluble vitamins which have a great effect on the health of the immunity system while its deficiency for a long time increases the morbidity and mortality level, especially in the pediatric population (Zhang et al., 2019).
In a cross-sectional study performed by Abd El-Shaheed et al. (2018) reported that there was a positive association between vitamin A and both CD4 and Tβ4, thus, vitamin A deficiency reduced the efficacy of the immunity system against infectious diseases. In another clinical trial, it was reported that vitamin A intervention caused a decrease in the duration of fever and hospital stay (Li et al., 2020a). In terms of hospital stay, we found that the interventions with zinc or vitamin A reduced days of hospitalization by an average of 3.21 days (95% CI: 5.01–−1.41, p < 0.01) and 2.43 days (95% CI: 4.29–−0.57, p = 0.01), respectively. This result is similar to those found in the study by Valavi et al. (2011), where they used zinc at 2 mg/kg/day (max. daily dose: 20 mg) for 5 days for children from 3 to 60 months old, and those reported in the study by Reyes et al. (2002), who used zinc at 15 mg twice daily until discharge from hospital or up to maximum 7 days for children from 2 to 60 months old.
Concerning the significance of the reduction in length of hospital stay in the current study, it is important to mention that reduction in the length of hospital stay is an indicator of good medical practice and the efficacy of the treatment protocol (Baek H. et al., 2018). Moreover, there is a criterion for hospital discharge depending on the hospitalized case, according to Marrie et al., a patient with pneumonia is considered ready for discharge when his vital signs have been normalized, lung function and oxygenation have returned to the baseline status, results of blood culture is negative, and the blood cell count is lower than 12×109/L (Marrie et al., 2000; Moeller et al., 2006).
On the other hand, Nacul et al. (1998) reported that the results obtained in their study required more evidence to recognize the effect of vitamin A on the recovery of pneumonia by using two different doses of vitamin A (100000–200000 IU per dose) for children from 1 to 48 months old. However, Shah et al. (2012) found that zinc had no significant reduction effect on hospital stay in pneumonia patients upon the administration of 10 mg twice daily for 7 days for children from 2 to 60 months old.
In the present study, although the zinc group showed a much lower length of stay than vitamin A, on comparing the effects of zinc and vitamin A on hospitalization length of stay, the difference was not statistically significant which might be attributed to the short period of the study due to the short total period of patients’ hospital residence either in the ICU or the inpatient ward, according to the physicians’ decisions, not the researchers, where, this obtained difference might be significant in case of a longer period of supplementation administration time.
Pleural effusion is a pathological condition where excess fluid accumulates between the visceral and parietal pleural membranes that surround the lungs. This condition causes impaired lung function due to the fluid between the tissues in the pleural cavity (Arad et al., 2009; Bai et al., 2019). In the present work, the duration of effusion in the groups of zinc and vitamin A was found to be significantly lower compared to the control group. On comparing the zinc group to the vitamin A group, it was found that zinc causes a 3 days non-significant reduction in the duration of effusion compared to vitamin A.
The mechanisms by which zinc and vitamin A cause the reduction in the duration of hospital stay or pleural effusion are unknown, but it could be due to their antibacterial and anti-inflammatory properties, as well as their role in tissue growth regulation (Shahzad et al., 2018; Skalny et al., 2020; Khadim and Al-Fartusie, 2021). Zinc could be more effective than vitamin A due to zinc’s activities in reducing the susceptibility of micro-organisms to producing toxins and its role in regulating the cell membrane permeability of water and minerals (Skalny et al., 2020; Hunter et al., 2021).
At the end of the present study period, a significant difference regarding the clinical assessment and laboratory values found among the studied groups similar to that reported in the study by Srinivasan et al. (2012), Valentiner- Branth et al. (2010) regarding zinc supplementation, and Nacul et al. (1998) for vitamin A supplementation.
In the study by Shah et al. (2012) and Valentiner- Branth et al. (2010); it was found that the female patients had lower susceptibility to pneumonia infection than the male patients, where the recorded percentages were 35.35% and 42%, respectively, but in our study, we found that the female patients had higher susceptibility (57.3%) which may be related to a general condition where the mean of hemoglobin and total leukocyte count of female participated in our study at admission were 11.5 g/dl and 33.01 × 109/L, respectively, which was lower than the mean in male participants, 11.7 g/dl and 22.1 × 109/L, respectively.
Conclusion
Administration of either zinc or vitamin A supplementation in community-acquired pneumonia in children aged less than 5 years significantly reduces the hospitalization stay and duration of effusion compared to the control group with a non-significant difference between the effect of zinc and/or vitamin A supplementation.
Based on our knowledge, this is the first clinical study that assesses and compares the effect of zinc and vitamin A as supplement treatment in community-acquired pneumonia in children less than 5 years old in terms of hospital stay and pleural effusion. So, we hope that our funding could be helpful for more clinical trials that may use our results to test the significance between the effect of zinc and vitamin A by using different duration of administration or assessing other parameters.
Limitations
This is a preliminary study to investigate the effect of zinc versus vitamin A in pediatric patients with community-acquired pneumonia performed on a limited number of patients being a preliminary (pilot) study; the relatively small sample size of our study may reduce the ability to determine the statistical significance of the variables. It is recommended that further large-scale studies be performed on a large number of patients. A second limitation was the measurement of micronutrient concentration, as both zinc and vitamin A levels, which were not detected at baseline.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Medical Research Ethics Committee, Al Galaa Military Medical Complex. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
All authors contributed to the study conception and design. Material presentation, data collection, and analysis were performed by AS, RE, and NS. Practical part of clinical trials was carried out under the supervision of MR. The first draft of the manuscript was written by AS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Acknowledgments
The authors would like to thank the pediatrics department in Al Galaa Military hospital and Ghamra Military hospital for their help and collaboration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.933998/full#supplementary-material
References
Abd El-Shaheed, A., Abd El-Shaheed, A., El-Zayat, S., Sibaii, H., Mahfouz, N., and Moustafa, R. (2018). A new insight into the immune regulatory functions of vitamin A in children and adolescents. J. Arab. Soc. Med. Res. 13 (1), 1. doi:10.4103/jasmr.jasmr_30_17
Afolami, I. (2021). Efficacy of biofortified ( yellow ) cassava on Serum Retinol in nigerian pre-school Children. Wageningen: Staff Publications.
Alagha, H. Z., Badary, O. A., Ibrahim, H. M., and Sabri, N. A. (2011). Reducing prescribing errors in the paediatric intensive care unit: An experience from Egypt. Acta Paediatr. 100 (10), e169–e174. doi:10.1111/j.1651-2227.2011.02270.x
Arad, M., Zlochiver, S., Davidson, T., Shoenfeld, Y., Adunsky, A., and Abboud, S. (2009). The detection of pleural effusion using a parametric EIT technique. Physiol. Meas. 30 (4), 421–428. doi:10.1088/0967-3334/30/4/006
Ateya, A. M., and Sabri, N. A. (2021). Zinc supplementation for males during COVID-19: Is it beneficial? Med. Hypotheses 146, 110403. doi:10.1016/j.mehy.2020.110403
Baek, H., Cho, M., Kim, S., Hwang, H., Song, M., and Yoo, S. (2018). Analysis of length of hospital stay using electronic health records: A statistical and data mining approach. PloS one 13 (4), e0195901. doi:10.1371/journal.pone.0195901
Bai, K. J., Chuang, K. J., Chen, J. K., Tsai, C. Y., Yang, Y. L., Chang, C. C., et al. (2019). Alterations by air pollution in inflammation and metals in pleural effusion of pneumonia patients. Int. J. Environ. Res. Public Health 16 (5), E705–E710. doi:10.3390/ijerph16050705
Basnet, S., Shrestha, P. S., Sharma, A., Mathisen, M., Prasai, R., Bhandari, N., et al. (2012). A randomized controlled trial of zinc as adjuvant therapy for severe pneumonia in young children. Pediatrics 129 (4), 701–708. doi:10.1542/peds.2010-3091
Connelly, L. M. (2008). Pilot studies. Medsurg Nurs. 17 (6), 411–412. https://www.proquest.com/openview/553d762f3224a627486acfbf1a7320e0/1?pqorigsite=gscholar&cbl=30764
Erdfelder, E., Faul, F., and Buchner, A. (1996). Gpower: A general power analysis program. Behav. Res. Methods, Instrum. Comput. 28 (1), 1–11. doi:10.3758/BF03203630
Gupta, S., Brazier, A. K. M., and Lowe, N. M. (2020). Zinc deficiency in low- and middle-income countries: Prevalence and approaches for mitigation. J. Hum. Nutr. Diet. 33 (5), 624–643. doi:10.1111/jhn.12791
Hamed, A. M. M., Kassem, Y. T., Fayed, H. K., and Solaiman, A. M. (2019). Serum zinc levels in hospitalized children with pneumonia: A hospital-based case–control study. Egypt. J. Bronchol. 13 (5), 730–737. doi:10.4103/ejb.ejb_30_19
Harel-Sterling, M., Diallo, M., Santhirakumaran, S., Maxim, T., and Tessaro, M. (2019). Emergency department resource use in pediatric pneumonia: Point-of-Care lung ultrasonography versus chest radiography. J. Ultrasound Med. 38 (2), 407–414. doi:10.1002/jum.14703
Hepler, C. D. (2004). Clinical pharmacy, pharmaceutical care, and the quality of drug therapy. Pharmacotherapy 24 (11), 1491–1498. doi:10.1592/phco.24.16.1491.50950
Hoang, B. X., and Han, B. (2021). Micronutrient zinc roles in adjunctive therapy for COVID-19 by enhancing patients immunoregulation and tolerance to the pathogen. Rev. Med. Microbiol. 32 (3), 149–157. doi:10.1097/mrm.0000000000000263
Hunter, J., Arentz, S., Goldenberg, J., Yang, G., Beardsley, J., Mertz, D., et al. (2021). Corrigendum to "rapid review protocol: Zinc for the prevention or treatment of COVID-19 and other coronavirus-related respiratory tract infections" [integr med res 9 (2020): 100457]. Integr. Med. Res. 9, 100689. doi:10.1016/j.imr.2020.100689
Hunter, J., Arentz, S., Goldenberg, J., Yang, G., Beardsley, J., Myers, S. P., et al. (2021a). Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: A rapid systematic review and meta-analysis of randomised controlled trials. BMJ Open 11 (11), e047474. doi:10.1136/bmjopen-2020-047474
Imdad, A., Mayo-Wilson, E., Herzer, K., and Bhutta, Z. A. (2017). Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst. Rev. 3 (3), CD008524. doi:10.1002/14651858.CD008524.pub3
Jafarzadeh, N., and Oscuii, H. N. (2019). Numerical simulation of mucous layer formation effects on oxygen transfer phenomena from the respiratory membrane in pulmonary diseases. Biomed. Phys. Eng. Express 5 (6), 065012. doi:10.1088/2057-1976/ab4694
Jalal, Z., Bakour, M., and Lyoussi, B. (2021). Medicinal plants and zinc: Impact on COVID-19 pandemic. Sci. World J. 2021, 9632034. doi:10.1155/2021/9632034
Jegalakshmi, E., Rameshbabu, M., Razia, M., Florence, S. S., Bakri, M., Muthupandi, S., et al. (2022). Structural, optical and antimicrobial activity of Ferric doped zinc sulphide (ZnS) nanoparticles. Mater. Today Proc. 49, 2611–2614. doi:10.1016/j.matpr.2021.07.274
Karter, D. L., Karter, A. J., Yarrish, R., Patterson, C., Kass, P. H., Nord, J., et al. (1995). Vitamin A deficiency in nonvitamin-supplemented patients with AIDS: A cross − sectional study. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 8, 199–203. doi:10.1097/00042560-199502000-00012
Katz, S. E., and Williams, D. J. (2018). Pediatric community-acquired pneumonia in the United States: Changing epidemiology, diagnostic and therapeutic challenges, and areas for future research. Infect. Dis. Clin. North Am. 32 (1), 47–63. doi:10.1016/j.idc.2017.11.002
Khadim, R. M., and Al-Fartusie, F. S. (2021). Antioxidant vitamins and their effect on immune system. J. Phys. Conf. Ser. 1853 (1), 012065. doi:10.1088/1742-6596/1853/1/012065
Kuti, B. P., Adetola, H. H., and Oyelami, O. A. (2021). Serum micronutrients as related to childhood pneumonia severity and outcome in a Nigerian health facility. J. Infect. Dev. Ctries. 15 (7), 953–961. doi:10.3855/jidc.13792
Li, D., Wang, Q., Su, M., Wang, L. L., Zhang, Q., Wang, C. Y., et al. (2020). Molecular epidemiology and clinical features of Haemophilus influenzae among hospitalized children with community-acquired pneumonia in chengde, China. Biomed. Environ. Sci. 33 (8), 623–627. doi:10.3967/bes2020.082
Li, Y., Guo, Z., Zhang, G., Tian, X., Li, Q., Chen, D., et al. (2020a). The correlation between vitamin a status and refractory Mycoplasma Pneumoniae pneumonia (RMPP) incidence in children. BMC Pediatr. 20 (1), 1–9.
Mahalanabis, D., Chowdhury, A., Jana, S., Bhattacharya, M. K., Chakrabarti, M. K., Wahed, M. A., et al. (2002). Zinc supplementation as adjunct therapy in children with measles accompanied by pneumonia: A double-blind, randomized controlled trial. Am. J. Clin. Nutr. 76 (3), 604–607. doi:10.1093/ajcn/76.3.604
Marrie, T. J., Lau, C. Y., Wheeler, S. L., Wong, C. J., Vandervoort, M. K., and Feagan, B. G. (2000). A controlled trial of a critical pathway for treatment of community-acquired pneumonia. CAPITAL Study Investigators. Community-Acquired Pneumonia Intervention Trial Assessing Levofloxacin. Jama 283 (6), 749–755. doi:10.1001/jama.283.6.749
McPherson, S. W., Keunen, J. E., Bird, A. C., Chew, E. Y., and Van Kuijk, F. J. (2020). Investigate oral zinc as a prophylactic treatment for those at risk for COVID-19. Am. J. Ophthalmol. 216, A5–A6. doi:10.1016/j.ajo.2020.04.028
Moeller, J. J., Ma, M., Hernandez, P., Marrie, T., Touchie, C., and Patrick, W. (2006). Discharge delay in patients with community-acquired pneumonia managed on a critical pathway. Can. J. Infect. Dis. Med. Microbiol. 17 (2), 109–113. doi:10.1155/2006/375645
Morse, C. G., and High, K. P. (2018). 11 - Nutrition, immunity, and infection. Eighth edi, mandell, douglas, and bennett’s Principles and practice of infectious diseases. Eighth Edi. Amsterdam, Netherlands: Elsevier.
Mumtaz, A., Munir, H., Zubair, M. T., and Arif, M. H. (2019). Mimosa pudica gum based nanoparticles development, characterization, and evaluation for their mutagenicity, cytotoxicity and antimicrobial activity. Mat. Res. Express 6 (10), 105308. doi:10.1088/2053-1591/ab34ab
Nacul, L. C., Arthur, P., Kirkwood, B. R., Morris, S. S., Cameiro, A. C., and Benjamin, A. F. (1998). The impact of vitamin A supplementation given during a pneumonia episode on the subsequent morbidity of children. Trop. Med. Int. Health 3 (8), 661–666. doi:10.1046/j.1365-3156.1998.00259.x
Prasad, R., Sharma, A., Das, B. K., Mishra, S. P., and Singh, U. K. (2019). Serum retinol, vitamin D and zinc levels in under five children with acute lower respiratory tract infections. Indian J. Pediatr. 86 (2), 196–197. doi:10.1007/s12098-018-2805-y
Review, C., Communication, S., and Principles, G. (2014). World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 81 (3), 428–432. doi:10.1093/acprof:oso/9780199241323.003.0025
Reyes, H., Villalpando, S., Perez-Cuevas, R., Rodriguez, L., Perez-Cuevas, M., Montalvo, I., et al. (2002). Frequency and determinants of vitamin A deficiency in children under 5 years of age with pneumonia. Arch. Med. Res. 33 (2), 180–185. doi:10.1016/S0188-4409(01)00361-7
Sakulchit, T. (2017). Child health update zinc supplementation for pediatric pneumonia. Can. Fam. Physician 63, 763–765. https://www.cfp.ca/content/cfp/63/10/763.full.pdf
Saleh, N. Y., and Abo El Fotoh, W. M. M. (2018). Low serum zinc level: The relationship with severe pneumonia and survival in critically ill children. Int. J. Clin. Pract. 72 (6), e13211–9. doi:10.1111/ijcp.13211
Schulz, K. F., Altman, D. G., and Moher, D.CONSORT Group (2010). CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 152 (11), 726–732.
Shah, G. S., Dutta, A. K., Shah, D., and Mishra, O. P. (2012). Role of zinc in severe pneumonia: A randomized double bind placebo controlled study. Ital. J. Pediatr. 38 (1), 36–6. doi:10.1186/1824-7288-38-36
Shahzad, S., Ashraf, M. A., Sajid, M., Shahzad, A., Rafique, A., and Mahmood, M. S. (2018). Evaluation of synergistic antimicrobial effect of vitamins (A, B1, B2, B6, B12, C, D, E and K) with antibiotics against resistant bacterial strains. J. Glob. Antimicrob. Resist. 13, 231–236. doi:10.1016/j.jgar.2018.01.005
Shakur, S., Malek, M. A., Bano, N., Rahman, M., and Ahmed, M. (2009). Serum and hair zinc in severely malnourished Bangladeshi children associated with or without acute lower respiratory infection. Indian J. Pediatr. 76 (6), 609–614. doi:10.1007/s12098-009-0109-y
Skalny, A. V., Rink, L., Ajsuvakova, O. P., Aschner, M., Gritsenko, V. A., Alekseenko, S. I., et al. (2020). Zinc and respiratory tract infections: Perspectives for Covid’19 (review). Int. J. Mol. Med. 46 (1), 17–26. doi:10.3892/ijmm.2020.4575
Srinivasan, M. G., Ndeezi, G., Mboijana, C. K., Kiguli, S., Bimenya, G. S., Nankabirwa, V., et al. (2012). Zinc adjunct therapy reduces case fatality in severe childhood pneumonia: A randomized double blind placebo-controlled trial. BMC Med. 10, 14–10. doi:10.1186/1741-7015-10-14
Symington, S., and Scott, T. (2017). Community-acquired pneumonia: Making use of the guidelines from pediatrics to adults. Physician Assist. Clin. 2 (2), 155–163. doi:10.1016/j.cpha.2016.12.001
Valavi, E., Hakimzadeh, M., Shamsizadeh, A., Aminzadeh, M., and Alghasi, A. (2011). The efficacy of zinc supplementation on outcome of children with severe pneumonia. A randomized double-blind placebo-controlled clinical trial. Indian J. Pediatr. 78 (9), 1079–1084. doi:10.1007/s12098-011-0458-1
Walker, C. L. F., and Black, R. E. (2012). Zinc treatment for serious infections in young infants. Lancet 379 (9831), 2031–2033. doi:10.1016/S0140-6736(12)60695-3
Wang, L., and Song, Y. (2018). Efficacy of zinc given as an adjunct to the treatment of severe pneumonia: A meta-analysis of randomized, double-blind and placebo-controlled trials. Clin. Respir. J. 12 (3), 857–864. doi:10.1111/crj.12646
West, K. P. (2003). Vitamin A deficiency disorders in children and women. Food Nutr. Bull. 24 (4), 78–90. doi:10.1177/15648265030244S204
Keywords: pneumonia, micronutrient, zinc, vitamin A, effusion, hospital stay, intensive care, pediatric
Citation: Saied A, El Borolossy RM, Ramzy MA and Sabri NA (2022) Effect of zinc versus vitamin A supplementation on pediatric patients with community-acquired pneumonia. Front. Pharmacol. 13:933998. doi: 10.3389/fphar.2022.933998
Received: 01 May 2022; Accepted: 20 July 2022;
Published: 30 August 2022.
Edited by:
Swaran J. S. Flora, National Institute of Pharmaceutical Education and Research, IndiaReviewed by:
Gregory Thomas Knipp, Purdue University, United StatesAshok K. Shakya, Al-Ahliyya Amman University, Jordan
Prakash Ghosh, International Centre for Diarrhoeal Disease Research (ICDDR), Bangladesh
Copyright © 2022 Saied, El Borolossy, Ramzy and Sabri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aya Saied, YXlhc2FpZWQ3M0BnbWFpbC5jb20=
 Aya Saied
Aya Saied Radwa Maher El Borolossy
Radwa Maher El Borolossy Mourad Alfy Ramzy3
Mourad Alfy Ramzy3 Nagwa A. Sabri
Nagwa A. Sabri