
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Pharmacol. , 17 February 2022
Sec. Drugs Outcomes Research and Policies
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.843683
 Hazel Chloe Villalobos Barbon1
Hazel Chloe Villalobos Barbon1 Jamie Ledesma Fermin2†
Jamie Ledesma Fermin2† Shaira Limson Kee3†
Shaira Limson Kee3† Myles Joshua Toledo Tan3,4*†
Myles Joshua Toledo Tan3,4*† Nouar AlDahoul5
Nouar AlDahoul5 Hezerul Abdul Karim5*
Hezerul Abdul Karim5*Despite the many breakthroughs in the field of public health in the past century, the incidence of healthcare-associated infections (HCAI) remains to be at a high level in both low-middle-income- and high-income-countries across the globe as evidenced by the report from the World Health Organization (WHO) in 2011. Specifically, the Philippines, a low-middle-income country (LMIC), experiences this as well. Despite this, only a few local studies have demonstrated evidence regarding the prevalence of HCAIs, including Navoa-Ng et al. (2011) that reported the prevalence of device-associated infections (DAI), with ventilator-associated pneumonia (VAP) as the most common. The high statistics has also been attributed to a higher mortality rate, especially among adults confined in intensive care units (ICU) (Navoa-Ng et al., 2011).
A way to prevent transmission is through the practice of hand hygiene (HH). It is an integral part of healthcare and is one of the most effective and least expensive methods in preventing the spread of HCAIs (Saharman et al., 2019). Despite this, HH compliance remains to be low in many countries, both in LMICs and high-income countries (HICs) (WHO, 2013). In an effort to increase compliance, the WHO developed approaches seeking to improve HH behavior but is needing additional improvements. Optimization of these approaches may be applied through the use of electronic monitoring systems (EMS), a solution that may also be applied in the Philippines.
Healthcare-associated infection (HCAI), as defined by the WHO (2011), is an infection introduced to a patient during the process of treatment in healthcare facilities. This type of infection can appear during or after the patient receives treatment. Studies have shown that the prevalence of HCAIs has been consistently high in many countries, with much literature (Cai et al., 2017; Cassini et al., 2016; US CDC, 2019.1) focused on reporting about HICs (WHO, 2011).
Fewer studies give a depiction of the rates in LMICs, but findings report that the rate of HCAIs is significantly elevated as well (WHO, 2011). Results of the meta-analysis and systematic review conducted by Allegranzi et al. (2011) reports that one of the major burdens for patients and healthcare workers (HCWs) in LMICs, is the prevalence of HCAIs affecting as much as 15.5 per 100 population.
Limited studies investigate the rates of HCAIs in LMICs and even more so in the Philippines. The study of Navoa-Ng et al. (2011) conducted in the ICUs of only 3 hospitals in the country reported 183 DAIs in 2005–2009. Further reporting that ventilator-associated pneumonia (VAP), constituting 67.2% of the cases, as the most common DAI in adult ICUs. This was followed by catheter-associated urinary tract infections (CAUTI) and central line-associated bloodstream infections (CLABSI) at 22.4 and 10.4%, respectively.
HCAIs have been found to negatively impact many healthcare systems in LMICs, causing patients to increase their length of stay in the ICUs and have caused serious cases of morbidity and increased the rate of mortality (Navoa-Ng et al., 2007; Navoa-Ng et al., 2011). Such impacts can be mitigated by decreasing HCAI rates through behavioral change by HCWs, one of which can be done through increasing HH compliance (WHO, 2011).
One of the most common ways of transmitting HCAIs is through the hands of the HCWs (Pittet et al., 2006). As such, it is vital that proper HH is practiced among HCWs as a preventive measure. Hand hygiene has been proven to be effective at preventing transmission of all types of HCAIs. However, despite its simplicity and effectiveness, compliance to HH practices remains to be low in many countries, reportedly only 40% in HICs, with LMICs reported to have much lower statistics (Erasmus et al., 2010; Phan et al., 2018).
The WHO, seeking to standardize HH practices, developed “My 5 Moments of Hand Hygiene” (MFMHH). This method is based on the concept of finding optimal points during healthcare delivery to perform HH practices in order to disrupt the microbiological transmission of pathogens. The moments identified using this concept include: 1) before contact with patient; 2) before performing aseptic task; 3) after exposure to patient’s body fluids; 4) after contact with patient; and 5) after contact with patient’s surroundings (WHO, 2009b).
This method has been largely aimed at educating HCW, as well as in reporting their HH practices. Its application in LMICs, including the Philippines, may be hindered because it involves dividing the healthcare environment into two zones: the patient zone, which includes the patient and the space that surrounds them, and the healthcare zone, which includes all the other surfaces in the area not classified under the former. Many healthcare facilities in LMICs, including the Philippines, have overcrowding problems making the division of environment non-feasible (Loftus et al., 2019). Averaging at only 10.7 beds per 10,000 population, the Philippine health care facilities bed capacity is well below the WHO recommendation of 20 beds per 10,000 population (Alliance for Improving Health Outcomes Inc., 2017).2 In comparison, HICs average at around 53 hospital beds per 10,000 population (The World Bank Group, 2021).3
The patient zone includes the patient and the immediate space around them. Furthermore, anything that is frequently touched by the patient such as their bed railing, bed linen, etc., as well as anything frequently touched by HCWs when they are providing care to the patient are also classified as belonging to the patient zone. These are areas that are often contaminated by the patient but is cleaned after every patient admission. Healthcare zone, on the other hand, includes all other areas not included in the former, including other patients’ zone and other areas in the healthcare facility. These are areas where foreign microorganisms for a particular patient that can potentially infect them are present (Malik, 2008). Many healthcare facilities in LMICs, including the Philippines, have overcrowding problems making the division of environment non-feasible (Loftus et al., 2019; Lowe et al., 2021; Tyagi et al., 2018). Averaging at only 10.7 beds per 10,000 population, the Philippine health care facilities bed capacity is well below the WHO recommendation of 20 beds per 10,000 population (Alliance for Improving Health Outcomes Inc., 2017). In comparison, HICs average at around 53 hospital beds per 10,000 population (The World Bank Group, 2021).
Apart from MFMHH, the WHO also pushed for the use of a multi-modal approach in increasing compliance to HH practices. This approach involves five components: system change, training and education, evaluation and feedback, reminders in the workplace, and institutional safety climate (WHO, 2009a; Pfäfflin., 2017; Müller et al., 2021).
This involves the participation of the administration in crafting policies and guidelines and conducting educational and training campaigns to better encourage healthcare workers to engage in HH practices. Being multi-modal, this approach gives more room for tailoring interventions into the context of a healthcare facility.
These approaches can serve as an overarching intervention to increase HH compliance. To gauge progress, monitoring systems must be implemented.
Effective HH monitoring systems in healthcare facilities are needed to know HH compliance by HCWs. A traditionally used method and the gold standard is direct observation (WHO, 2009b). The WHO developed a way to quantify HH compliance based on MFMHH. This method involves a trained observer who is tasked to monitor the HH behavior of HCWs. Although proven to be effective and simple enough to be implemented in LMICs, this method presents some limitations. One of these includes being prone to biases, especially observer’s and selection biases. Besides this, the method can be time-consuming and need a number of employed observers to accurately describe the HH practice in a big healthcare facility (Masroor et al., 2017).
A way to remove these biases is to employ an EMS, a method in HH monitoring that has just recently been explored. EMS eliminates the need to employ a trained observer and is not prone to the aforementioned biases. Furthermore, EMS is more cost-effective in the long run as it can provide continuous real-time monitoring and feedback even in large facilities (Masroor et al., 2017). There are two types of EMS that will be explored in this paper.
There are a variety of EMS types that have been developed in recent years. This paper will focus on technologies utilizing real-time locating systems, namely, MediHandTrace and Biovigil. Both systems primarily utilize radio frequency identification (RFID) (Boudjema et al., 2013; McCalla et al., 2017).
For MediHandTrace, a specific RFID technology, “iCode RFID 15693” tag technology, is used together with an alcohol dispenser motor. In the pilot study conducted by Boudjema et al. (2013), four antennas were placed within the room, placed strategically to monitor HH based on MFMHH. The antennas were placed in the following locations: 1) outside the room under an alcohol dispenser; 2) door entrance; 3) inside the room under another alcohol dispenser; and 4) around the bed within a secured zone. A tag is inserted within the shoe of an HCW to determine their location within the room. Sensors were also placed near the two alcohol dispensers to measure the number of sprays as well as the volume used at a time. The placement of the antennae in the patient room is visualized in Figure 1. Data from the antenna, tag, and sensors were then read by another technology, which then transfers the data into the main server through an Ethernet connection. In the study, verification of whether the technology accomplished its purpose was verified through video cameras stationed within the room for the course of the study (Boudjema et al., 2013).
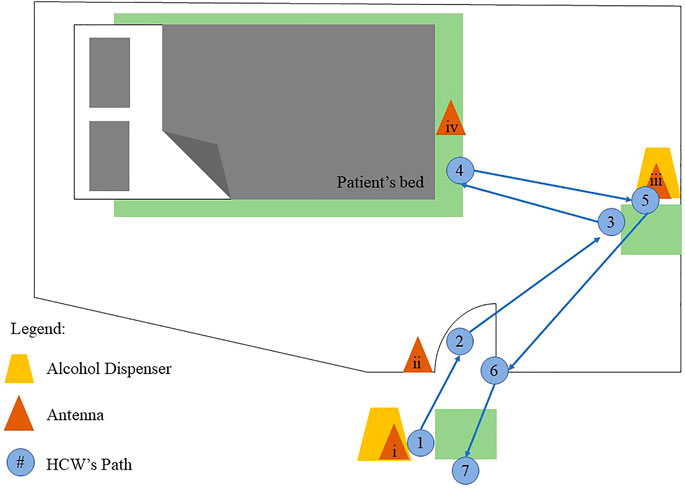
FIGURE 1. Antennae placement within patient room (adopted from Boudjema et al., 2013).
AADO modifies the traditional pen and paper method of recording observations by enabling observers to record their findings on mobile or tablet applications (Wiemken et al., 2018). These methods still employ direct observers but there is a marked reduction in the time spent on the transcription of data, as well as decrease the risk of introduction of errors in the analysis. (Cawthorne et al., 2021; Wang et al., 2021). Despite its potential, AADO technology is met with numerous challenge and limitations, the most prominent of which is its non-user-friendly nature and subsequent intensive training needed to be done for HCWs (Cawthorne et al., 2021).
CAO utilizes cameras either situated inside patient rooms or mounted in HCW’s chests that monitors HH practices that are then analyzed by either human observers or an algorithm (Brotfain et al., 2017; Wang et al., 2021). An example of this technology was used in the study by Awwad et al. (2018) which utilized positioned cameras in a patient’s room to capture images which were then analyzed using computer vision techniques to detect HH practices in accordance with the WHO’s MFMHH. However, this technique faces ethical issues as cameras can record not only HH practices but also patients during treatment (Gon et al., 2020a).
SAO employs the use of sensors, placed in either electronic dispensers, electronic dispensers combined with other sensors, and inertial measurement unit and microphone (IMU). In essence, electronic dispenser technology detects the usage frequency and dispense of HH products in patient’s rooms. IMU, on the other hand, detects and measures HCW’s movements which are then analyzed to determine their HH practices (Wang et al., 2021). This technology offers some advantages over direct observation including lesser expense as it no longer involves employing human observers, however it lacks the depth of analysis in the quality of HH practices performed by HCWs (Kato et al., 2021).
RLTS measures HH practice by sensing dispenser use and HCW movements inside a patient’s room by utilizing either of the following: radio frequency identification (RFID), infrared, Bluetooth, ultrasound, and Wi-Fi (Wang et al., 2021).
In this paper, the focus will be on technologies utilizing real-time locating systems, specifically those that primarily utilize RFID. RFID tags are commonly placed within a HCW’s clothing or are worn as bracelets or wristbands and are used in combination with sensors situated within the room to detect HCW compliance to HH practice. This information is then collected and communicated to a cloud server located in the hospital (Tarantini, 2019; Periyasamy et al., 2020; Huang et al., 2021; Wang et al., 2021).
Three systems utilizing RFID technology will be discussed in the following sections, MediHandTrace, and Biovigil (Boudjema et al., 2013; McCalla et al., 2017).
In contrast, Biovigil, although also utilizing RFID, functions with the use of a wristband that shows different colors indicating whether the HCW has performed a HH practice. These bands show a yellow-colored light which progresses to red to prompt the HCW to engage in HH practice. Once HH is done, the band will show a green-colored light, indicating that HH has been adequate. The band can also produce auditory prompts to signal HCWs to perform HH. Sensors within these bands can detect whether the HCW used soap and water or alcohol-based rub to sanitize their hand. After an HCW’s shift, data is gathered while the band is charging at a base station; this is then transmitted to cloud-based storage where it can be analyzed (McCalla et al., 2017).
The WHO has provided several guidelines to monitor HH in healthcare facilities. The first step in increasing HH compliance would be to create interventions that can make the environment in healthcare facilities more conducive to allow practice of MFMHH. This might be a lengthy process, especially in LMICs, and will require a sizable investment of resources and commitment from the hospital and government administration. Furthermore, the government must allocate more resources focused on the surveillance of HCAIs in the country since there is an evident lack of recent data reports and literature reporting on the prevalent types of HCAIs, at the national level. Once this is achieved, context-specific interventions and an optimized use of EMS will be possible and can aid in increasing HH compliance in healthcare facilities.
Given the problem of overcrowding in LMICs, making it harder to differentiate spaces to allow practice of MFMHH, incorporating an EMS that works similarly with MediHandTrace will be difficult. In the Philippines, where there is an insufficient number of beds for the population, EMS working similarly to MediHandTrace will most likely be unsustainable and difficult to implement. The study conducted by Dufour et al. (2017) utilizing this technology even had mixed results, concluding that HH compliance is still HCW-dependent. This study was conducted in France, a HIC, which has a better hospital bed to population ratio. Given its less than passable results coupled with its requirement of several system changes to work, applying it to a LMIC like the Philippines may not be a cost-effective decision.
In contrast, Biovigil, an EMS utilizing a wearable technology that can prompt a HCW to perform HH practice, may be more suitable in the Philippine context. Based on the information from study of McCalla et al. (2017), this EMS does not require many changes in the system. As such, EMS using a technology like Biovigil is a better recommendation since the Philippines has not yet been able to resolve the problems of patient overcrowding and does not appear to be able to solve it in the near future.
The application of a RFID system in a hospital setting as seen in Mitchell et al. (2017) is evidence that utilizing this type of technology is possible in the Philippines. With their study providing proof that such technology provides benefits in improving individual HCW HH practice, it is impartial to suggest that this technology will indeed be helpful in the improvement of HH practice. More studies in the future can follow and investigate which type of EMS is best to use given a certain hospital’s context. Perhaps, a large amount of research, as well as the overall improvement of public hospitals in the country is needed before this can be achieved. However, the point still stands that there is a great need to improve on the monitoring systems in the hospitals in the country and starting the application of EMS in hospitals is an excellent step towards that goal.
All in all, it is important that any technology used as EMS can be incorporated seamlessly into the healthcare system of the country. Based on the multi-modal approach of the WHO, to address HH compliance to lower HCAIs, the healthcare system must first be improved. To do this, incorporating these EMS will soon follow. Given the established fact that HH is an effective way to combat HCAIs like DAIs including VAP, CAUTI, and CLABSI, increasing HH compliance through EMS can greatly decrease the transmission rate of the aforementioned infections. As such, the impact of EMS lies in its ability to increase HH compliance in healthcare facilities. When this is done, the incidence of HCAIs will decrease.
Conceived the work: HB, JF, SK, MT, NA, and HK; Drafted the article: HB; Critically revised the manuscript: JF, SK, MT, NA, and HK; Acquired funding: HK. All authors contributed to the article and approved the submitted version.
The publication of this article was funded by Multimedia University, Malaysia.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1https://www.cdc.gov/hai/data/portal/progress-report.html
2https://www.aiho.org.ph/2017/05/08/philippine-health-system/
3https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?end=2019&start=1960&view=chart
Allegranzi, B., Bagheri Nejad, S., Combescure, C., Graafmans, W., Attar, H., Donaldson, L., et al. (2011). Burden of Endemic Health-Care-Associated Infection in Developing Countries: Systematic Review and Meta-Analysis. Lancet 377 (9761), 228–241. doi:10.1016/S0140-6736(10)61458-4
Awwad, S., Tarvade, S., Piccardi, M., and Gattas, D. J. (2019). The Use of Privacy-Protected Computer Vision to Measure the Quality of Healthcare Worker Hand hygiene. Int. J. Qual. Health Care 31 (1), 36–42. doi:10.1093/intqhc/mzy099
Blomgren, P.-O., Lytsy, B., Hjelm, K., and Swenne, C. L. (2021). Healthcare Workers' Perceptions and Acceptance of an Electronic Reminder System for Hand hygiene. J. Hosp. Infect. 108, 197–204. doi:10.1016/j.jhin.2020.12.005
Boudjema, S., Dufour, J. C., Aladro, A. S., Desquerres, I., and Brouqui, P. (2013). MediHandTrace ®: a Tool for Measuring and Understanding Hand hygiene Adherence. Clin. Microbiol. Infect. 20 (1), 22–28. doi:10.1111/1469-0691.12471
Boyce, J. M. (2017). Electronic Monitoring in Combination with Direct Observation as a Means to Significantly Improve Hand hygiene Compliance. Am. J. Infect. Control. 45 (5), 528–535. doi:10.1016/j.ajic.2016.11.029
Brotfain, E., Livshiz-Riven, I., Gushansky, A., Erblat, A., Koyfman, L., Ziv, T., et al. (2017). Monitoring the Hand hygiene Compliance of Health Care Workers in a General Intensive Care Unit: Use of Continuous Closed circle Television versus Overt Observation. Am. J. Infect. Control. 45 (8), 849–854. doi:10.1016/j.ajic.2017.03.015
Brouqui, P., Boudjema, S., Soto Aladro, A., Chabrière, E., Florea, O., Nguyen, H., et al. (2017). New Approaches to Prevent Healthcare-Associated Infection. Clin. Infect. Dis. 65 (Suppl. l_1), S50–S54. doi:10.1093/cid/cix433
Cai, Y., Venkatachalam, I., Tee, N. W., Tan, T. Y., Kurup, A., Wong, S. Y., et al. (2017). Prevalence of Healthcare-Associated Infections and Antimicrobial Use Among Adult Inpatients in Singapore Acute-Care Hospitals: Results from the First National point Prevalence Survey. Clin. Infect. Dis. 64 (Suppl. l_2), S61–S67. doi:10.1093/cid/cix103
Caris, M. G., Labuschagne, H. A., Dekker, M., Kramer, M. H. H., van Agtmael, M. A., and Vandenbroucke-Grauls, C. M. J. E. (2018). Nudging to Improve Hand hygiene. J. Hosp. Infect. 98 (4), 352–358. doi:10.1016/j.jhin.2017.09.023
Cassini, A., Plachouras, D., Eckmanns, T., Abu Sin, M., Blank, H. P., Ducomble, T., et al. (2016). Burden of Six Healthcare-Associated Infections on European Population Health: Estimating Incidence-Based Disability-Adjusted Life Years through a Population Prevalence-Based Modelling Study. Plos Med. 13 (10), e1002150. doi:10.1371/journal.pmed.1002150
Cawthorne, K.-R., Oliver, C., and Cooke, R. P. D. (2021). A User's View of Commercial mobile Applications Designed to Measure Hand hygiene Compliance by Direct Observation. J. Hosp. Infect. 117, 4–8. doi:10.1016/j.jhin.2021.08.008
Doll, M. E., Masroor, N., Cooper, K., Trimmer, T., Pryor, R., Auricchio, J., et al. (2019). A Comparison of the Accuracy of Two Electronic Hand hygiene Monitoring Systems. Infect. Control. Hosp. Epidemiol. 40 (10), 1194–1197. doi:10.1017/ice.2019.209
Dufour, J. C., Reynier, P., Boudjema, S., Soto Aladro, A., Giorgi, R., and Brouqui, P. (2017). Evaluation of Hand hygiene Compliance and Associated Factors with a Radio-Frequency-Identification-Based Real-Time Continuous Automated Monitoring System. J. Hosp. Infect. 95 (4), 344–351. doi:10.1016/j.jhin.2017.02.002
Erasmus, V., Daha, T. J., Brug, H., Richardus, J. H., Behrendt, M. D., Vos, M. C., et al. (2010). Systematic Review of Studies on Compliance with Hand hygiene Guidelines in Hospital Care. Infect. Control. Hosp. Epidemiol. 31 (3), 283–294. doi:10.1086/650451
Gon, G., de Barra, M., Dansero, L., Nash, S., and Campbell, O. M. R. (2020b). Birth Attendants' Hand hygiene Compliance in Healthcare Facilities in Low and Middle-Income Countries: a Systematic Review. BMC Health Serv. Res. 20 (1), 1116–16. doi:10.1186/s12913-020-05925-9
Gon, G., Ali, S. M., Aunger, R., Campbell, O. M., de Barra, M., de Bruin, M., et al. (2020a). A Practical Guide to Using Time-And-Motion Methods to Monitor Compliance with Hand Hygiene Guidelines: Experience from Tanzanian Labor Wards. Glob. Health Sci. Pract. 8 (4), 827–837. doi:10.9745/ghsp-d-20-00221
Gould, D. J., Creedon, S., Jeanes, A., Drey, N. S., Chudleigh, J., and Moralejo, D. (2017a). Impact of Observing Hand hygiene in Practice and Research: a Methodological Reconsideration. J. Hosp. Infect. 95 (2), 169–174. doi:10.1016/j.jhin.2016.08.008
Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., and Taljaard, M. (2017b). Interventions to Improve Hand hygiene Compliance in Patient Care. Cochrane Database Syst. Rev. 9 (9), CD005186. doi:10.1002/14651858.CD005186.pub4
Granqvist, K., Ahlstrom, L., Karlsson, J., Lytsy, B., and Andersson, A. E. (2021). Learning to Interact with New Technology: Health Care Workers’ Experiences of Using a Monitoring System for Assessing Hand hygiene–a Grounded Theory Study. Am. J. Infect. Control.
Haque, M., Sartelli, M., McKimm, J., and Abu Bakar, M. (2018). Health Care-Associated Infections - an Overview. Infect. Drug Resist. 11, 2321–2333. doi:10.2147/IDR.S177247
Huang, F., Boudjema, S., and Brouqui, P. (2021). Three-year Hand hygiene Monitoring and Impact of Real-Time Reminders on Compliance. J. Hosp. Infect. 117, 111–116. doi:10.1016/j.jhin.2021.08.015
Jeanes, A., Coen, P. G., Gould, D. J., and Drey, N. S. (2019). Validity of Hand hygiene Compliance Measurement by Observation: a Systematic Review. Am. J. Infect. Control. 47 (3), 313–322. doi:10.1016/j.ajic.2018.08.004
Kato, H., Takeda, R., Ideno, Y., Suzuki, T., Sano, K., and Nakamura, K. (2021). Physicians' Compliance for Hand hygiene in Medical Outpatient Clinics: Automated Hand-hygiene Monitoring with Touch Sensor and Wireless Internet. Am. J. Infect. Control. 49 (1), 50–54. doi:10.1016/j.ajic.2020.05.037
Lambe, K. A., Lydon, S., Madden, C., Vellinga, A., Hehir, A., Walsh, M., et al. (2019). Hand hygiene Compliance in the ICU: a Systematic Review. Crit. Care Med. 47 (9), 1251–1257. doi:10.1097/CCM.0000000000003868
Livorsi, D. J., Goedken, C. C., Sauder, M., Vander Weg, M. W., Perencevich, E. N., and Reisinger, H. S. (2018). Evaluation of Barriers to Audit-And-Feedback Programs that Used Direct Observation of Hand hygiene Compliance: a Qualitative Study. JAMA Netw. Open 1 (6), e183344. doi:10.1001/jamanetworkopen.2018.3344
Loftus, M. J., Guitart, C., Tartari, E., Stewardson, A. J., Amer, F., Bellissimo-Rodrigues, F., et al. (2019). Hand hygiene in Low- and Middle-Income Countries. Int. J. Infect. Dis. 86, 25–30. doi:10.1016/j.ijid.2019.06.002
Lowe, H., Woodd, S., Lange, I. L., Janjanin, S., Barnet, J., and Graham, W. (2021). Challenges and Opportunities for Infection Prevention and Control in Hospitals in Conflict-Affected Settings: a Qualitative Study. Confl Health 15 (1), 94–10. doi:10.1186/s13031-021-00428-8
Makhni, S., Umscheid, C. A., Soo, J., Chu, V., Bartlett, A., Landon, E., et al. (2021). Hand Hygiene Compliance Rate during the COVID-19 Pandemic. JAMA Intern. Med. doi:10.1001/jamainternmed.2021.1429
Maki, G., and Zervos, M. (2021). Health Care-Acquired Infections in Low- and Middle-Income Countries and the Role of Infection Prevention and Control. Infect. Dis. Clin. North. Am. 35 (3), 827–839. doi:10.1016/j.idc.2021.04.014
Malik, R. (2008). A Manual for WHO “My Five Moments of Hand Hygiene” Concept. Multan, Pakistan: WHO.Int.. Available at: http://who.int/gpsc/tools/Ma nual_5_moments_Pakistan.pdf?ua=1.
Manoukian, S., Stewart, S., Graves, N., Mason, H., Robertson, C., Kennedy, S., et al. (2021). Bed-days and Costs Associated with the Inpatient burden of Healthcare-Associated Infection in the UK. J. Hosp. Infect. 114, 43–50. doi:10.1016/j.jhin.2020.12.027
Masroor, N., Doll, M., Stevens, M., and Bearman, G. (2017). Approaches to Hand hygiene Monitoring: from Low to High Technology Approaches. Int. J. Infect. Dis. 65, 101–104. doi:10.1016/j.ijid.2017.09.031
McCalla, S., Reilly, M., Thomas, R., and McSpedon-Rai, D. (2017). An Automated Hand hygiene Compliance System Is Associated with Improved Monitoring of Hand hygiene. Am. J. Infect. Control. 45 (5), 492–497. doi:10.1016/j.ajic.2016.12.015
Mitchell, K. F., Barker, A. K., Abad, C. L., and Safdar, N. (2017). Infection Control at an Urban Hospital in Manila, Philippines: a Systems Engineering Assessment of Barriers and Facilitators. Antimicrob. Resist. Infect. Control. 6 (1), 90–99. doi:10.1186/s13756-017-0248-2
Müller, S. A., Diallo, A. O. K., Rocha, C., Wood, R., Landsmann, L., Camara, B. S., et al. (2021). Mixed Methods Study Evaluating the Implementation of the WHO Hand hygiene Strategy Focusing on Alcohol Based Handrub and Training Among Health Care Workers in Faranah, Guinea. PloS one 16 (8), e0256760. doi:10.1371/journal.pone.0256760
Navoa-Ng, J. A., Berba, R., Galapia, Y. A., Rosenthal, V. D., Villanueva, V. D., Tolentino, M. C., Genuino, G. A., Consunji, R. J., and Mantaring, J. B. (2011). Device-associated Infections Rates in Adult, Pediatric, and Neonatal Intensive Care Units of Hospitals in the Philippines: International Nosocomial Infection Control Consortium (INICC) Findings. Am. J. Infect. Control. 39 (7), 548–554. doi:10.1016/j.ajic.2010.10.018
Navoa-Ng, J. A., Rosenthal, V. D., Asetre-Luna, I., and Yu, C. (2007). Healthcare-Associated Infection Rates, Extra Length of Stay and Mortality in a Hospital of the Philippines. Findings of the INICC. Am. J. Infect. Control. 35 (5), E55–E56. doi:10.1016/j.ajic.2007.04.055
Periyasamy, M., Karthikeyan, S., and Mahendran, G. (2020). Electromagnetic Immunity Testing of Radio Frequency Identification Devices (RFID) in Healthcare Environment–A Selected Review. Mater. Today Proc.
Pfäfflin, F., Tufa, T. B., Getachew, M., Nigussie, T., Schönfeld, A., Häussinger, D., et al. (2017). Implementation of the WHO Multimodal Hand hygiene Improvement Strategy in a University Hospital in Central Ethiopia. Antimicrob. Resist. Infect. Control. 6 (1), 3–10. doi:10.1186/s13756-016-0165-9
Phan, H. T., Tran, H. T. T., Tran, H. T. M., Dinh, A. P. P., Ngo, H. T., Theorell-Haglow, J., et al. (2018). An Educational Intervention to Improve Hand hygiene Compliance in Vietnam. BMC Infect. Dis. 18 (1), 116–6. doi:10.1186/s12879-018-3029-5
Pittet, D., Allegranzi, B., Sax, H., Dharan, S., Pessoa-Silva, C. L., Donaldson, L., et al. (2006). Evidence-based Model for Hand Transmission during Patient Care and the Role of Improved Practices. Lancet Infect. Dis. 6 (10), 641–652. doi:10.1016/S1473-3099(06)70600-4
Purssell, E., Drey, N., Chudleigh, J., Creedon, S., and Gould, D. J. (2020). The Hawthorne Effect on Adherence to Hand hygiene in Patient Care: a Systematic Review. J. Hosp. Infect.
Saharman, Y. R., Aoulad Fares, D., El-Atmani, S., Sedono, R., Aditianingsih, D., Karuniawati, A., et al. (2019). A Multifaceted Hand hygiene Improvement Program on the Intensive Care Units of the National Referral Hospital of Indonesia in Jakarta. Antimicrob. Resist. Infect. Control. 8 (1), 93–10. doi:10.1186/s13756-019-0540-4
Seyed Nematian, S. S., Palenik, C. J., Mirmasoudi, S. K., Hatam, N., and Askarian, M. (2017). Comparing Knowledge and Self-Reported Hand hygiene Practices with Direct Observation Among Iranian Hospital Nurses. Am. J. Infect. Control. 45 (6), e65–e67. doi:10.1016/j.ajic.2017.03.007
Stahmeyer, J. T., Lutze, B., Von Lengerke, T., Chaberny, I. F., and Krauth, C. (2017). Hand hygiene in Intensive Care Units: a Matter of Time? J. Hosp. Infect. 95 (4), 338–343. doi:10.1016/j.jhin.2017.01.011
Stewart, S., Robertson, C., Pan, J., Kennedy, S., Dancer, S., Haahr, L., et al. (2021). Epidemiology of Healthcare-Associated Infection Reported from a Hospital-wide Incidence Study: Considerations for Infection Prevention and Control Planning. J. Hosp. Infect. 114, 10–22. doi:10.1016/j.jhin.2021.03.031
Tarantini, C., Brouqui, P., Wilson, R., Griffiths, K., Patouraux, P., and Peretti-Watel, P. (2019). Healthcare Workers' Attitudes towards Hand-hygiene Monitoring Technology. J. Hosp. Infect. 102 (4), 413–418. doi:10.1016/j.jhin.2019.02.017
The World Bank Group (2021). Hospital Beds (Per 1,000 People). Washington, DC: World Bank Open Data | Data. Available at: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?end=2017&name_desc=false&start=1960 (Retrieved, 2021).
Tyagi, M., Hanson, C., Schellenberg, J., Chamarty, S., and Singh, S. (2018). Hand hygiene in Hospitals: an Observational Study in Hospitals from Two Southern States of India. BMC public health 18 (1), 1299–9. doi:10.1186/s12889-018-6219-6
Wang, C., Jiang, W., Yang, K., Yu, D., Newn, J., Sarsenbayeva, Z., et al. (2021). Electronic Monitoring Systems for Hand Hygiene: Systematic Review of Technology. J. Med. Internet Res. 23 (11), e27880. doi:10.2196/27880
Wiemken, T. L., Furmanek, S. P., Mattingly, W. A., Haas, J., Ramirez, J. A., and Carrico, R. M. (2018). Googling Your Hand hygiene Data: Using Google Forms, Google Sheets, and R to Collect and Automate Analysis of Hand hygiene Compliance Monitoring. Am. J. Infect. Control. 46 (6), 617–619. doi:10.1016/j.ajic.2018.01.010
World Health Organization (2011). Report on the burden of Endemic Health Care-Associated Infection Worldwide. Available at: https://apps.who.int/iris/bitstream/handle/10665/80135/9789241501507_eng.pdf;sequence=1 (Retrieved August 17, 2021).
World Health Organization (2013). Systematic Literature Review of Automated/electronic Systems for Hand hygiene Monitoring. Available at:http://www. who. int/gpsc/5ma y/automated-hand-hygiene-monitoring. pdf (Retrieved August 17, 2021).
World Health Organization (2009b). WHO Guidelines on Hand hygiene in Health Care. Geneva. Available at: http://apps.who.int/iris/bitstream/10665/44102/1/9789241597906_eng.pdf (Retrieved August 17, 2021).
World Health Organization (2009a). A Guide to the Implementation of the WHO Multimodal Hand hygiene Improvement Strategy. Geneva: World Health Organization. Available at: https://apps.who.int/iris/handle/10665/70030.
Keywords: healthcare-acquired infections, Philippines, hand hygiene compliance, electronic monitoring systems, low-middle-income countries, hand hygiene, monitoring system, infection
Citation: Barbon HCV, Fermin JL, Kee SL, Tan MJT, AlDahoul N and Karim HA (2022) Going Electronic: Venturing Into Electronic Monitoring Systems to Increase Hand Hygiene Compliance in Philippine Healthcare. Front. Pharmacol. 13:843683. doi: 10.3389/fphar.2022.843683
Received: 26 December 2021; Accepted: 01 February 2022;
Published: 17 February 2022.
Edited by:
Domenico Criscuolo, Italian Society of Pharmaceutical Medicine, ItalyReviewed by:
Maria Angélica Peterlini, Federal University of São Paulo, BrazilCopyright © 2022 Barbon, Fermin, Kee, Tan, AlDahoul and Karim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Myles Joshua Toledo Tan, bWoudGFuQHVzbHMuZWR1LnBo; Hezerul Abdul Karim, aGV6ZXJ1bEBtbXUuZWR1Lm15
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.