- 1Department of Chinese Medicine, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 2School of Post-baccalaureate Chinese Medicine, Tzu Chi University, Hualien, Taiwan
- 3Sports Medicine Center, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 4Department of Medical Research, Buddhist Tzu Chi General Hospital, Hualien, Taiwan
- 5Department of Obstetrics and Gynecology, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan
- 6Department of Public Health, College of Medicine, Tzu Chi University, Hualien, Taiwan
- 7Department of Chinese Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan
Introduction: Tocolytic treatment is beneficial to pregnant women with a risk of premature labor or miscarriage. However, previous reports have shown that progestogen might not be effective and ritodrine may increase the risk of maternal vascular-related diseases. Chinese herbal products (CHP) are used as alternative therapies for pregnant women. The goal was to evaluate the efficacy of combined tocolytic therapy and CHP therapy in pregnancy outcomes for pregnant women in Taiwan.
Materials and Methods: We conducted a retrospective cohort study based on the National Health Insurance Research Database. A total of 47,153 pregnant women treated with tocolytics aged 18–50 years from 2001 to 2015 were selected from two million random samples. According to the medical use of tocolytics and CHP, we divided the users into two groups: western medicine (WM) only (n = 40,961) and WM/CHP (n = 6,192) groups. A propensity score (PS)-matched cohort (6,192 pairs) was established based on baseline confounders. All participants were followed up to perinatal outcomes. Conditional logistic regression analysis was used to examine the effects of CHP use on the odds of miscarriage and preterm birth.
Results: The adjusted odds ratio (OR) for premature birth in the WM/CHP group (n = 411, 6.64%) was significantly lower than in the WM group (n = 471, 7,61%) (0,86, 95% confidence interval [CI], 0.74–0.99). Further subgroup analysis based on the usage of formulae that activate blood and remove stasis or purgative formulae, the adjusted OR of preterm birth of those using these formulae was significantly lower in the WM/CHP group (n = 215, 6.32%) than that in the WM group (n = 265, 7.77%) (OR: 0.79, 95% CI: 0.65–0.96).
Conclusion: We found that the combination of CHP and tocolytics can be beneficial to pregnant women in the prevention of premature birth. Further research is required to investigate causal relationships.
1 Introduction
The use of tocolytics to prevent or eliminate uterine contractions occurring before 34 weeks of gestation has been the major strategy of obstetric management of threatened preterm labor for many years (Hubinont and Debieve, 2011). Preterm labor is the major cause of perinatal mortality and morbidity in high-income countries and constitutes a huge economic burden on the healthcare system (Blencowe et al., 2013). Administration of tocolytics can reduce the intensity and frequency of uterine contractions to prolong pregnancy, thereby providing time for further intrauterine maturation and interventions that may improve infant outcome (Dehaene et al., 2017).
A met-analysis of women with acute preterm labor found that these drugs were more effective than placebo/control in delaying delivery for 48 h and 7 days, but not for delaying delivery until 37 weeks (Haas et al., 2009). Many different agents have been used for tocolytic therapy to suppress uterine contractions, but a standard first-line drug has not emerged. Currently, drugs commonly used for tocolytic therapy include progesterone, β-agonists, calcium channel blockers, and oxytocin receptor antagonists (Younger et al., 2017; Hanley et al., 2019). In Taiwan, a perspective survey of tocolytic treatment for preterm birth prevention had revealed that nearly 60% of obstetric specialists prescribed ritodrine as the first-line medication, whether in oral or intravenous form. The second choice was nifedipine, and only 6% of. obstetrician gynecologists prescribed atosiban, a self-paid medication in Taiwan, as first-line tocolytics (Lee et al., 2022). However, the Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA) issued a warning in October 2013, stating that β-adrenergic receptor agonists (such as ritodrine) should only be used at gestational age 22–37 weeks and the duration of administration should not exceed 48 h. Long-term use of β-adrenergic receptor agonists has a high cardiovascular risk, which may outweigh its benefits (EMA, 2013). Therefore, the safety and efficacy of tocolytics for the treatment of spontaneous preterm labor or threatened miscarriage during pregnancy is of concern to pregnant women and physicians (Lamont and Jorgensen, 2019).
In addition to western medicine (WM), traditional Chinese medicine (TCM) treatment is another option. Chinese herbal medicine (CHM) has a long history of preventing miscarriage and premature birth. A review of relevant literature shows that compared with WM alone, the combined use of TCM and WM tocolytic treatments exhibits superior results and fewer side effects. The most frequently used formula is“Shou Tai Pill,” and it was thought to enhance the function of “Kidney” and regulate the “Qi” in the human body, thus improving the health condition of mothers and benefiting the fetus (Li et al., 2012; Li et al., 2014). The use of CHM during pregnancy or postpartum has been analyzed and reported in the literature (Chuang et al., 2009; Yeh et al., 2009). However, the safety and effectiveness of CHM use in pregnant women with signs of miscarriage or premature birth have not been further evaluated.
The National Health Insurance (NHI) research database (NHIRD) in Taiwan has long-term tracking data and an excellent drug registration process, which allows tracking of the efficacy and safety of Chinese herbal products (CHP) from retrospective cohort data. The purpose of this study was to use the NHIRD to explore the combined use of tocolytic drugs and CHP by pregnant women in Taiwan and evaluate their effects on birth outcome (including preterm delivery and miscarriage). The effectiveness of WM tocolytic drugs was also compared with that of their combined use with CHM preparations.
2 Materials and Methods
2.1 Data Resources
Taiwan launched a single-payer NHI Program in 1995 that covers almost the entire population. The NHI program database contains registration files and original claim data for reimbursement, while data in the NHIRD derived from the NHI program are released for research purposes. The data used in this study was a longitudinal health insurance database 2000 (LHID 2000) comprising medical claim data of 2,000,000 beneficiaries randomly sampled from the 2000 Registry for beneficiaries of the NHIRD.
The randomly sampled beneficiaries exhibited no significant differences in age, sex, birth year, and other basic characteristics from the general population. We used LHID 2000 data from 2001 to 2015, including inpatient and outpatient visits and medications, and the International Classification of Disease-Clinical Modification, ninth revision (ICD-9-CM) was used to define the disease in this study. The study was approved by the research ethics committee of Buddhist Tzu Chi General Hospital, Hualien.
2.2 Study Samples and Measured Variables
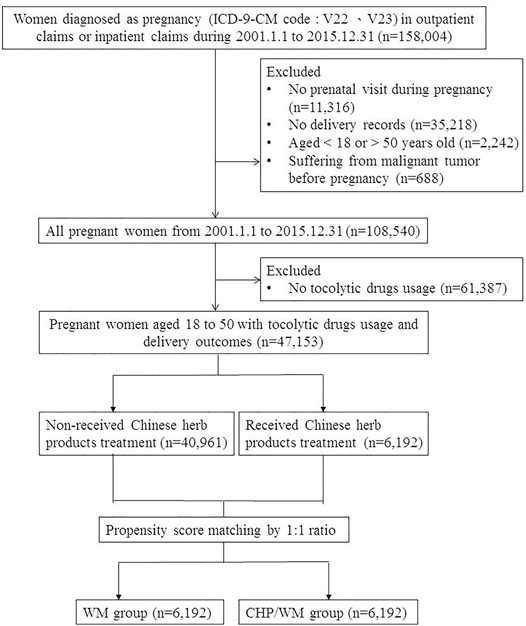
This was a retrospective cohort study based on data from the LHID 2000 collected between 1 Jan 2001 to 31 Dec 2015. There were 158,004 women with the diagnosis of pregnancy (ICD-9-CM codes:V22 and V23) during outpatient or inpatient visits. The exclusion criteria were as follows: 1) no prenatal visits (n = 11,316), 2) no birth outcome information including term birth (ICD-9-CM code: V27.0, V27.2, V27.3, V27.5, V27.6, V30-V37, V39, 650), preterm birth (ICD-9-CM code: 765.1), miscarriage (ICD-9-CM code: 632; ICD_OP_CODE:690, 695, 750), and stillbirth (ICD-9-CM code: V27.1, V27.4, V27.7, 656.4) (n = 35,218), 3) aged <18 or >50 years old (n = 2,242), 4) malignant tumor before pregnancy (n = 688), and 5) did not use any tocolytic drugs (n = 61,387). Based on the inclusion and exclusion criteria, we selected a total of 47,153 eligible pregnant women in our study cohort (Figure 1).
Pregnant women who had TCM outpatient visits along with CHP prescription records because of obstetrics-related disease (ICD-9-CM code: 610-677 or A code: A370-A394) in parallel to their tocolytic treatment were allocated to the WM/CHP group. Pregnant women who only received tocolytic treatment were assigned to the WM group. The index date of both groups was the estimated date of their last menstrual period and the end date was the date when labor ended. Before matching, there were 6,192 and 40,961 women in WM/CHP and WM groups, respectively.
2.3 Primary Outcome
The primary outcome was the labor results during the follow-up period including term birth, preterm birth, miscarriage, and stillbirth based on the ICD-9-CM code diagnosed by obstetrician-gynecologists. (ICD-9-CM code was described in the previous Section 2.2).
2.4 Characteristics, Comorbidities, and Drug
The following sociodemographic variables were collected: maternal age, year of pregnancy, first TCM outpatient visit (before or after pregnancy), frequency of prenatal visits, first prenatal visit, and pregnancy duration. The exact date of the last menstrual period was not available for the participants, so we indirectly deduced it from the date of the first prenatal visit. Pregnant women are offered 10 free prenatal visits during gestation in Taiwan. Each free prenatal visit with its corresponding sequence number from 41 to 50 represented specific gestational times, with number 41 representing the first free prenatal visit of the first trimester. The last menstrual period was determined by counting back 90 days from the sequence number 41. Duration of pregnancy was defined as the period between the estimated date of last menstrual period and the date of delivery.
Moreover, we included the comorbidities recommended by Bateman et al. (2013) such as severe preeclampsia/eclampsia (ICD-9-CM: 642.5, 642.6), mild preeclampsia (ICD-9-CM: 642.4), gestational hypertension (ICD-9-CM: 642.3), unspecified preeclampsia (ICD-9-CM: 642.7), chronic congestive heart failure (ICD-9-CM: 428.22, 428.23, 428.32, 428.33, 428.42, 428.43), congenital heart disease (ICD-9-CM: 745–747.4, 648.5), chronic ischemic heart disease (ICD-9-CM: 412-414), cardiac valvular disease (ICD-9-CM: 394-397, 424), pulmonary hypertension (ICD-9-CM: 416.0, 416.8, 416.9), preexisting hypertension (ICD-9-CM: 401-405, 642.0–642.2), sickle cell disease (ICD-9-CM: 282.4, 282.6), systemic lupus erythematosus (ICD-9-CM: 710.00), human immunodeficiency virus (ICD-9-CM: 042, V08), placenta previa (ICD-9-CM: 641.0, 641.1), chronic renal disease (ICD-9-CM: 581-583, 585, 587, 588, 646.2), asthma (ICD-9-CM: 493), preexisting diabetes mellitus (ICD-9-CM: 250, 648.0), multiple gestation (ICD-9-CM: V27.2-V27.8, 651), drug abuse (ICD-9-CM: 304, 305.2–3.05.9, 648.3), alcohol abuse (ICD-9-CM: 291, 303, 305.0), and previous cesarean delivery (ICD-9-CM: 654.2) (Bateman et al., 2013).
These diseases were determined by at least two outpatient visits or one inpatient visit at least 1 year before enrollment. We also considered the medication and cumulative usage days, including progestins (ATC code: G03DA04, G03DA03, G03DC01), ritodrine (ATC code: G02CA01), and nifedipine (ATC code: C08CA05). In addition, to fairly compare WM/CHP group and WM group, we adopted propensity score (PS) matching at a ratio of 1:1 of WM/CHP group to the matched WM group (Figure 1). PS was calculated using logistic regression with maternal age, pregnancy year, TCM outpatient visits before the half year of pregnancy, and comorbidity index at enrollment. The WM/CHP and WM groups were matched using the greedy matching algorithm of the log odds ratio (logit) of the PS within a caliper of 0.2 of the standard deviation of the logit of the PS.
2.5 Statistical Analyses
Continuous variables are reported as means and standard deviation, whereas categorical variables are reported as frequencies and percentage. We used an independent sample t-test or Chi-square test to compare the means or proportions of sample characteristics of the two groups. Furthermore, we used a conditional logistic regression analysis to examine the effect of CHP use on the outcome of pregnant women, controlling for potential confounding factors including maternal age at delivery, categories of tocolytic drugs used, and cumulative days of tocolytic drug use. In addition, to examine the safety of the different types of CHP used, we stratified pregnant women into two groups: those who used 1) products for activating blood and removing stasis or purgatives and 2) products that did not have these properties. The mechanisms of activating blood and removing stasis formulae or purgatives formulae were dilating blood vessels and inhibiting platelet aggregation. The most commonly used formula, Gui-Zhi-Fu-Ling-Wan, possesses significant spasmolytic effects on uterine tetanic contractions (Sun et al., 2016). Accordingly, activating blood and removing stasis formulae or purgatives formulae were believed to have the potential to prevent miscarriage or preterm birth. The p value <0.05 was considered statistically significant. Data were analyzed using SAS version 9.3 (SAS Institute, Inc., Cary, NC, Unite States).
3 Results
There were 108,540 pregnant women in our study period, and we enrolled 47,153 pregnant women in the cohort according to the inclusion and exclusion criteria, consisting of 6,192 who received CHP because of obstetrics-related diseases with a CHP utilization rate of 13.1%. The mean age was 29.75 years old and >99% of the sample population had their first prenatal visit in the first trimester. The estimated mean duration of pregnancy was 284 days. Before PS matching, the WM/CHP group tended to be older and a higher proportion experienced threatened abortion, so we conducted PS-matched to balance the baseline characteristics between the two groups. After PS matching, there were still differences in the usage of medications. In terms of progestins, compared to pregnant women in the WM group, more pregnant women in the WM/CHP group received progestins treatment (68.44% vs 72.06%, respectively). Among them, more than 95% women treated with progestins in the first trimester. Regarding tocolytic drugs, less than 3% pregnant women were prescribed Ritodrine or Nifedipine in their first trimester. Among women using Ritodrine or Nifedipine, over 90% pregnant women were prescribed Ritodrine or Nifedipine in their second or third trimester both in WM group and WM/CHP group. In addition, a higher percentage of women in the WM/CHP group received more than one tocolytic drug than those in the WM group (28.37% vs 25.89%, respectively). As to CHP, nearly 78% of pregnant women in the WM/CHP group received TCM treatment in the first trimester and the mean cumulative usage days of CHP was 23.72 days (Table1).
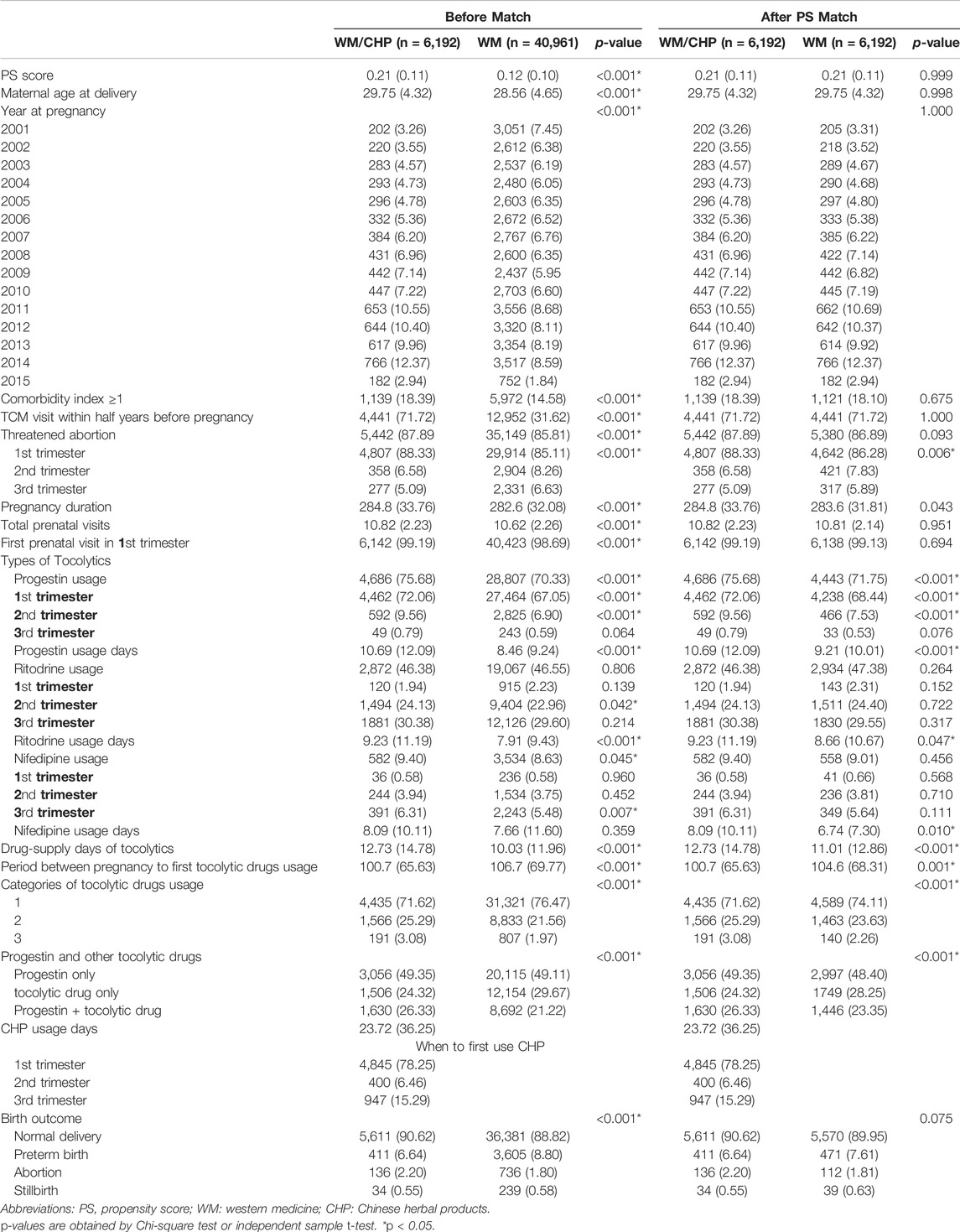
TABLE 1. Characteristics of pregnant women classified according to the use of Chinese herbal products.
Table 2 demonstrated the OR of birth outcomes of the two groups, compared with the WM group before PS matching the proportion and the adjusted OR of preterm birth in the WM/CHP group was significantly lower (OR: 0.80, 95% CI: 0.71–0.89). After PS matching and adjusting for maternal age, the categories of tocolytic drugs used, and cumulative tocolytic drug use days, the adjusted OR of the WM/CHP group (n = 411, 6.64%) remained significantly lower than that in the WM group (n = 471, 7.61%) (OR: 0.86, 95% CI: 0.74–0.99). However, there were 136 (2.20%) pregnant women in WM/CHP and 112 (1.81%) pregnant women in WM group suffered from miscarriage, respectively. There was no significant difference in the incidence of miscarriage between the two groups (OR: 1.38, 95% CI: 0.93–2.05).
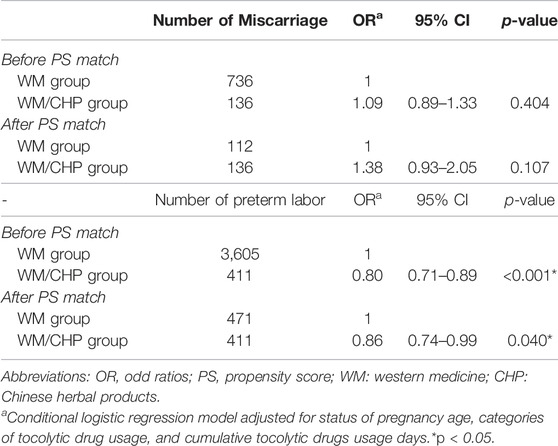
TABLE 2. Odd ratio estimates for birth outcome (preterm labor or miscarriage) of pregnant women between WM and WM/CHP groups.
Table 3 presented the subgroup analysis based on the use of activating blood and removing stasis formulae or purgative formulae, the adjusted OR of preterm birth of those using these formulae was significantly lower in the WM/CHP group (n = 215) than that in the WM group (n = 265) (OR: 0.79, 95% CI: 0.65–0.96). In contrast, there was no significant difference between the WM/CHP and WM groups in the incidence of miscarriage or preterm birth among pregnant women not receiving blood activating and stasis removing formula or purgative formula. Furthermore, we also listed the top five single herb and herbal formulae in Supplementary Table S1, S2. (The composition and indications are derived from the classical herbal pharmacopeia).
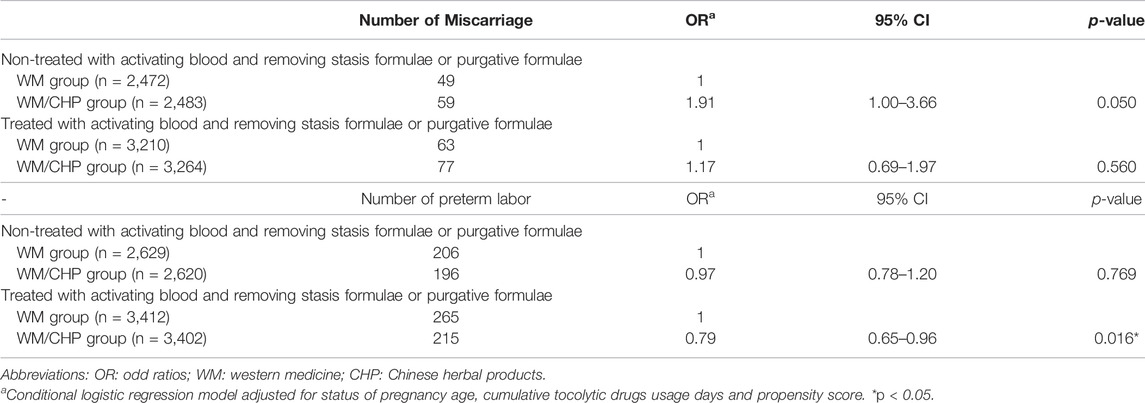
TABLE 3. Subgroup analysis for odd ratios of birth outcome (preterm labor or miscarriage) based on treated with activating blood and removing stasis formulae or purgative formulae between WM and WM/CHP groups.
4 Discussion
To the best of our knowledge, this was the first study to conduct a correlation assessment of perinatal outcomes between the use of tocolytic drugs and CHPs in a retrospective cohort of pregnant women who experienced threatened abortion in Taiwan, using the NHIRD. Although the cause of most miscarriages is unclear, they are presumably due to complex interactions between parental age, genetic, hormonal, immunological, comorbidities, and environmental factors (Garrido-Gimenez and Alijotas-Reig, 2015). Therefore, we included maternal age at delivery, comorbidities of major pregnancy-related diseases, and the use of CHP before pregnancy as variables in the statistical analysis and matched these to reduce the risk assessment that might affect outcome results. We found that the adjusted OR of preterm birth in the WM/CHP group was significantly lower than that in the WM group. Some women with symptoms of threatened abortion or preterm labor in Taiwan also use CHM for tocolytic treatment or to alleviate the side effects of treatment with WM tocolytic drugs. Therefore, co-treatment with CHM products may also reduce the side effects of tocolytic drugs and achieve better effects. Previous systemic reviews have reported that the proportions of patients in the WM/TCM and WM groups who experienced an extension of gestational age to 28 weeks (7 months) were 94.4% and 73.6%, respectively (Li et al., 2012). The meta-analysis results showed that the combination of TCM preparations and WM was more effective than either treatment strategy was alone (Li et al., 2014).
The incidence of threatened abortion is approximately 10%–25% and over half of these pregnant women will eventually experience miscarriage (Everett, 1997; Hossain et al., 2007). Most threatened miscarriages occur in the first trimester, and when threatened abortion occurs before gestation week 6, the incidence of miscarriage is as high as 29% (Basama and Crosfill, 2004; Mulik et al., 2004). Our results also showed that the first time tocolytic drugs were used was in the first trimester (nearly 60%–70%), and nearly 85% of the users were diagnosed with threatened abortion, including approximately 50% who used progesterone with other tocolytic drugs. Tocolytic therapy is generally used for the suppression of preterm labor or threatened abortion. Progesterone supplementation is the most commonly used treatment for preventing miscarriage. The results of systematic reviews suggest that progesterone-based derivatives are probably effective in the treatment of threatened miscarriage but may have little or no effect on the rate of preterm birth (Coomarasamy et al., 2011; Lee et al., 2017; Wahabi et al., 2018). However, some studies have reported that the use of progesterone therapy in the first trimester of pregnancy does not show tocolytic effects against miscarriages in women with a history of unexplained recurrent miscarriages (Coomarasamy et al., 2015). However, this recent clinical evidence of the efficacy of progesterone and progesterone-based derivatives remains controversial.
Progesterone is one of the earliest known mediators of embryo implantation and uterine quiescence. Additionally, progesterone has anti-inflammatory properties, which prevent prostaglandin production and inhibit human oxytocin receptor signaling (Younger et al., 2017). A wide variety of tocolytic drugs have been used to suppress uterine contractions as acute tocolytic therapy and maintenance, but these drugs usually have some unwanted reactions or adverse side effects in pregnant women. Calcium channel blockers (such as nifedipine) are antagonists that interfere with calcium ion transfer through the myometrial cell membrane to decrease intracellular free calcium concentration and promote myometrial relaxation.
A Cochrane Database review meta-analysis published in 2014 reported that calcium channel blockers showed benefits over betamimetics in prolongation of pregnancy and preventing serious neonatal morbidity and maternal adverse effects (Flenady et al., 2014). Selective β2 agonists (such as ritodrine) have been used in clinical practice for preterm labor since the 1980s, and are the only US Food and Drug Administration (FDA) approved drug for acute treatment of preterm labor, which is currently unavailable in the US. These drugs decrease intracellular cyclic AMP concentration and facilitate myometrial relaxation.
Randomized controlled trials comparing betamimetics with placebo have shown that betamimetics decreased the number of women in preterm labor who gave birth within 48 h (Neilson et al., 2014). However, the lack of benefit for long-term tocolysis and perinatal mortality is compounded by reports of an enhanced maternal morbidity rate (Li et al., 2005; EMA, 2013; Neilson et al., 2014). Because the effects of WM tocolysis are uncertain and divergent and few side effects will occur, it is necessary to regularly monitor the mother and fetus.
The five most prescribed single herbs identified in the present study were Scutellaria baicalensis Georgi (Huang Qin), Eucommia ulmoides Oliv. (Du Zhong), Cuscuta chinensis Lam. (Tu Si Zi), Cyperus rotundus L. (Xiang Fu), and Atractylodes macrocephala Koidz. (Bai Zhu) (Supplementary Table S1). The main ingredient in Scutellaria baicalensis Georgi is baicalein, and its effects may be mediated by the reduction of interferon (IFN)-γ and the increase of progesterone levels. These changes have a protective effect on injured decidual cells and increase blood supply to the placenta, thereby exerting anti-abortifacient effects (Ma et al., 2009; Wang et al., 2014).
Atractylodes macrocephala Koidz. (Bai Zhu) is used in combination with Scutellaria baicalensis Georgi (Huang Qin) to prevent miscarriage by suppressing maternal-fetal interface immunity (Zhong et al., 2002), while Atractylodes macrocephala Koidz. (Bai Zhu) also increases the availability of free radical scavengers and antioxidants and inhibits uterine contractions (Han et al., 2016; Wang et al., 2016). Previous study has shown that Eucommia ulmoides Oliv. (Du Zhong) contains isoflavonoids, which have been reported to exhibit phytoestrogenic and androgenic properties that may be related to the optimization of sex hormone activity in the maternal body (Hussain et al., 2016).
The main active ingredients of Cuscuta chinensis Lam. (Tu Si Zi) are flavonoids, which can increase estrogen receptor expression in the hippocampus, hypothalamus, and pituitary as well as luteinizing hormone receptor expression in the ovaries (Ke and Duan, 2013). Recent studies have reported that these flavonoids can promote the migration and invasion of extravillous trophoblast cells by increasing matrix metalloproteinase 9 (MMP9) expression and prevent miscarriage by activating Notch, AKT, and mitogen-activated protein kinase (MAPK) signaling pathways (Gao et al., 2018). Previous research has shown that these herbs also nourish the kidneys and have similar effects to those of endocrine hormones by acting directly on the ovaries and regulating the hypothalamic-pituitary-ovarian axis to prevent miscarriage (Zhu et al., 2014).
The top three herbal formulae used by pregnant women in the present study were Dang-Gui-Shao-Yao-San, Jia-Wei-Xiao-Yao-San, and Wen-Jing-Tang. Dang-Gui-Shao-Yao San is used to treat pregnancy-induced abdominal pain and blood deficiency syndrome. Recent clinical trials and animal experiments have found that it corrects luteal phase insufficiency via an antioxidant mechanism and antagonism of both prostaglandin F2-α and acetylcholine-induced uterine contractions (Usuki et al., 2002; Shen et al., 2005). Jia-Wei-Xiao-Yao-San can be used to treat premenstrual tension, climacteric syndrome, and infertility in women (Washio, 2003).
In particular, the anxiolytic effects of Jia-Wei-Xiao-Yao-San are considered mediated by neurosteroid synthesis, followed by stimulation of central gamma-amino-butyric acid A/benzodiazepine receptors via attenuation of stress-induced upregulation of α-synuclein and corticosterone and downregulation of protein phosphatase 2A in the hippocampus (Cao et al., 2016). Wen-Jing-Tang is effective in improving endocrine-related conditions in the treatment of disturbances of ovulation and may suppress contractions of the uterine smooth muscle (Hsu et al., 2003; Ushiroyama et al., 2006). Wen-Jing-Tang plus Dang-Gui-Sha-Yao-San was the most prescribed dual-herbal formula used to treat female infertility in Taiwan (Hung et al., 2016).
We further analyzed whether TCM herbs used for activating blood and removing stasis or as purgatives, which are contraindicated in pregnancy in TCM because they may cause adverse reactions leading to miscarriage, may actually be beneficial. The results showed that the odds of premature labor in the WM/CHP group were significantly lower than those in the WM group. Modern research has confirmed that some habitual miscarriage cases are associated with increased blood viscosity and possibly antiphospholipid antibodies (APA; i.e., anti-cardiolipin antibodies) that induce thrombosis in placental blood vessels with uterine spiral arterials and atherosclerosis (Pritchard et al., 2016; Santos et al., 2017). A recent systemic review indicated that some Chinese herbal medicines such as mild blood moving herbs used alone or in combination with progesterone-based western therapies may in fact help preserve pregnancy (Yang et al., 2013). This is particularly applicable to women with APA syndrome who have an increased risk of thromboembolic events during pregnancy (Zeng and Yao, 2010). Recent studies indicate that Gui-Zhi-Fu-Ling-Wan possesses significant spasmolytic effects on uterine tetanic contractions (Sun et al., 2016). Furthermore, some blood activating and stasis removing herbs can dilate blood vessels and inhibit platelet aggregation, thereby preventing the formation of thrombosis or blood coagulation and modulating T-cell function (Liu et al., 2013). Additional research is required in this area of reproductive medicine in the future.
This study has the following limitations. First, not all tocolytic drugs are covered by health insurance. Medication information such as whether pregnant women are required to use self-funded tocolytic drugs or TCM herbs at hospitals or the use of other herbs or health foods obtained from herbal clinics or pharmacies is not available. This lack of information leads to an underestimation of drug exposure. Access to information on interfering factors affecting outcome results such as being bedridden, smoking, living habits, occupation, and multiple births is limited by the database and cannot be obtained or controlled. Second, the dosing days provided in the database are the number of days the doctor prescribed the drug, which does not reflect actual use by the patient. In future studies, the definition of drug use in the WM/CHP group should be more protracted, the timing of drug use should be further considered, and this information should be used simultaneously or sequentially.
5 Conclusion
In conclusion, 13.1% of pregnant women use CHP and tocolytic drugs in combination during pregnancy and the OR of preterm birth in the WM/CHP group was significantly lower than that in the WM group. In the future, rigorous research is needed to investigate the causal relationships of our findings and the safety of the CHP used by pregnant women with threaten miscarriage.
Data Availability Statement
The datasets presented in this article are not readily available because datasets are restricted and not publicly available due to confidentiality agreements. Requests to access the datasets should be directed to H-CW, eHVhbmdAbXM2NS5oaW5ldC5uZXQ=.
Author Contributions
W-CC and D-LW helped to use statistical techniques to analyse study data. H-CW and H-SS carried out the research and wrote the first draft of the manuscript. S-HW and Y-LC revised the manuscript. H-CW guided the research project and submitted the manuscript. All authors read and approved the final manuscript.
Funding
We would like to express our sincere gratitude for the support provided for this project in the form of grants from the Taipei Tzu Chi General Hospital [TCRD-TPE-106-22 and TCRD-TPE-111-RT-4(1/3)]. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are grateful to Professor Yu Ru Kou for his valuable suggestions for the preparation of this manuscript. The data of this study is obtained from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health, and managed by the Health and Welfare Statistics Application Center, Ministry of Health and Welfare. The interpretations and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health, or Ministry of Health and Welfare.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.831690/full#supplementary-material
References
Basama, F. M., and Crosfill, F. (2004). The Outcome of Pregnancies in 182 Women with Threatened Miscarriage. Arch. Gynecol. Obstet. 270, 86–90. doi:10.1007/s00404-003-0475-z
Bateman, B. T., Mhyre, J. M., Hernandez-Diaz, S., Huybrechts, K. F., Fischer, M. A., Creanga, A. A., et al. (2013). Development of a Comorbidity Index for Use in Obstetric Patients. Obstet. Gynecol. 122, 957–965. doi:10.1097/AOG.0b013e3182a603bb
Blencowe, H., Cousens, S., Chou, D., Oestergaard, M., Say, L., Moller, A. B., et al. (2013). Born Too Soon: the Global Epidemiology of 15 Million Preterm Births. Reprod. Health 10 (Suppl. 1), S2. doi:10.1186/1742-4755-10-S1-S2
Cao, G. P., Gui, D., Fu, L. D., Guo, Z. K., and Fu, W. J. (2016). Anxiolytic and Neuroprotective Effects of the Traditional Chinese Medicinal Formulation Dan-Zhi-Xiao-Yao-San in a Rat Model of Chronic Stress. Mol. Med. Rep. 14 (2), 1247–1254. doi:10.3892/mmr.2016.5382
Chuang, C. H., Chang, P. J., Hsieh, W. S., Tsai, Y. J., Lin, S. J., and Chen, P. C. (2009). Chinese Herbal Medicine Use in Taiwan during Pregnancy and the Postpartum Period: a Population-Based Cohort Study. Int. J. Nurs. Stud. 46 (2), 787–795. doi:10.1016/j.ijnurstu.2008.12.015
Coomarasamy, A., Truchanowicz, E. G., and Rai, R. (2011). Does First Trimester Progesterone Prophylaxis Increase the Live Birth Rate in Women with Unexplained Recurrent Miscarriages? BMJ 342, d1914. doi:10.1136/bmj.d1914
Coomarasamy, A., Williams, H., Truchanowicz, E., Seed, P. T., Small, R., Quenby, S., et al. (2015). A Randomized Trial of Progesterone in Women with Recurrent Miscarriages. N. Engl. J. Med. 373 (22), 2141–2148. doi:10.1056/NEJMoa1504927
Dehaene, I., Bergman, L., Turtiainen, P., Ridout, A., Mol, B. W., and Lorthe, E. (2017). Maintaining and Repeating Tocolysis: A Reflection on Evidence. Semin. Perinatol. 41 (8), 468–476. doi:10.1053/j.semperi.2017.08.005
EMA (2013). Assessment Report for Short Acting Beta Agonists (SABAs) Containing Medicinal Products Authorised in Obstetric Indications. Available at: https://www.ema.europa.eu/en/documents/referral/short-acting-beta-agonists-article-31-referral-prac-assessment-report_en.pdf (Accessed 10 23, 2013).
Everett, C. (1997). Incidence and Outcome of Bleeding before the 20th Week of Pregnancy: Prospective Study from General Practice. BMJ 315 (7099), 32–34. doi:10.1136/bmj.315.7099.32
Flenady, V., Wojcieszek, A. M., Papatsonis, D. N., Stock, O. M., Murray, L., Jardine, L. A., et al. (2014). Calcium Channel Blockers for Inhibiting Preterm Labour and Birth. Cochrane Database Syst. Rev. 2014 (6), Cd002255. doi:10.1002/14651858.CD002255.pub2
Gao, F., Zhou, C., Qiu, W., Wu, H., Li, J., Peng, J., et al. (2018). Total Flavonoids from Semen Cuscutae Target MMP9 and Promote Invasion of EVT Cells via Notch/AKT/MAPK Signaling Pathways. Sci. Rep. 8 (1), 17342. doi:10.1038/s41598-018-35732-6
Garrido-Gimenez, C., and Alijotas-Reig, J. (2015). Recurrent Miscarriage: Causes, Evaluation and Management. Postgrad. Med. J. 91 (1073), 151–162. doi:10.1136/postgradmedj-2014-132672
Haas, D. M., Imperiale, T. F., Kirkpatrick, P. R., Klein, R. W., Zollinger, T. W., and Golichowski, A. M. (2009). Tocolytic Therapy: a Meta-Analysis and Decision Analysis. Obstet. Gynecol. 113 (3), 585–594. doi:10.1097/AOG.0b013e318199924a
Han, B., Gao, Y., Wang, Y., Wang, L., Shang, Z., Wang, S., et al. (2016). Protective Effect of a Polysaccharide from Rhizoma Atractylodis Macrocephalae on Acute Liver Injury in Mice. Int. J. Biol. Macromol. 87, 85–91. doi:10.1016/j.ijbiomac.2016.01.086
Hanley, M., Sayres, L., Reiff, E. S., Wood, A., Grotegut, C. A., and Kuller, J. A. (2019). Tocolysis: A Review of the Literature. Obstet. Gynecol. Surv. 74 (1), 50–55. doi:10.1097/OGX.0000000000000635
Hossain, R., Harris, T., Lohsoonthorn, V., and Williams, M. A. (2007). Risk of Preterm Delivery in Relation to Vaginal Bleeding in Early Pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 135 (20), 158–163. doi:10.1016/j.ejogrb.2006.12.003
Hsu, C. S., Yang, J. K., and Yang, L. L. (2003). Effect of a Dysmenorrhea Chinese Medicinal Prescription on Uterus Contractility In Vitro. Phytother. Res. 17 (7), 778–783. doi:10.1002/ptr.1235
Hubinont, C., and Debieve, F. (2011). Prevention of Preterm Labour: 2011 Update on Tocolysis. J. Pregnancy 2011, 941057. doi:10.1155/2011/941057
Hung, Y. C., Kao, C. W., Lin, C. C., Liao, Y. N., Wu, B. Y., Hung, I. L., et al. (2016). Chinese Herbal Products for Female Infertility in Taiwan: A Population-Based Cohort Study. Medicine 95 (11), e3075. doi:10.1097/MD.0000000000003075
Hussain, T., Tan, B., Liu, G., Oladele, O. A., Rahu, N., Tossou, M. C., et al. (2016). Health-Promoting Properties of Eucommia Ulmoides: A Review. Evid. Based Complement. Altern. Med. 2016, 5202908. doi:10.1155/2016/5202908
Ke, J., and Duan, R. (2013). Effects of Flavonoids from Semen Cuscutae on the Hippocampal-Hypothalamic-Pituitary-Ovarian Sex Hormone Receptors in Female Rats Exposed to Psychological Stress. Clin. Exp. Obstet. Gynecol. 40 (2), 271–274.
Lamont, R. F., and Jørgensen, J. S. (2019). Safety and Efficacy of Tocolytics for the Treatment of Spontaneous Preterm Labour. Curr. Pharm. Des. 25 (5), 577–592. doi:10.2174/1381612825666190329124214
Lee, H. H., Yeh, C. C., Yang, S. T., Liu, C. H., Chen, Y. J., and Wang, P. H. (2022). Tocolytic Treatment for the Prevention of Preterm Birth from a Taiwanese Perspective: A Survey of Taiwanese Obstetric Specialists. Int. J. Environ. Res. public health 19 (7), 4222. doi:10.3390/ijerph19074222
Lee, H. J., Park, T. C., Kim, J. H., Norwitz, E., and Lee, B. (2017). The Influence of Oral Dydrogesterone and Vaginal Progesterone on Threatened Abortion: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2017, 3616875. doi:10.1155/2017/3616875
Li, L., Dou, L., Leung, P. C., and Wang, C. C. (2012). Chinese Herbal Medicines for Threatened Miscarriage. Cochrane Database Syst. Rev. 5, Cd008510. doi:10.1002/14651858.CD008510.pub2
Li, L., Leung, P. C., Chung, T. K., and Wang, C. C. (2014). Systematic Review of Chinese Medicine for Miscarriage during Early Pregnancy. Evid. Based Complement. Altern. Med. 2014, 753856. doi:10.1155/2014/753856
Li, X., Zhang, Y., and Shi, Z. (2005). Ritodrine in the Treatment of Preterm Labour: a Meta-Analysis. Indian J. Med. Res. 121 (2), 120–127.
Liu, Y., Yin, H., and Chen, K. (2013). Platelet Proteomics and its Advanced Application for Research of Blood Stasis Syndrome and Activated Blood Circulation Herbs of Chinese Medicine. Sci. China Life Sci. 56 (11), 1000–1006. doi:10.1007/s11427-013-4551-8
Ma, A. T., Zhong, X. H., Liu, Z. M., Shi, W. Y., Du, J., Zhai, X. H., et al. (2009). Protective Effects of Baicalin against Bromocriptine Induced Abortion in Mice. Am. J. Chin. Med. 37 (1), 85–95. doi:10.1142/S0192415X09006709
Mulik, V., Bethel, J., and Bhal, K. (2004). A Retrospective Population-Based Study of Primigravid Women on the Potential Effect of Threatened Miscarriage on Obstetric Outcome. J. Obstet. Gynaecol. 24 (3), 249–253. doi:10.1080/01443610410001660724
Neilson, J. P., West, H. M., and Dowswell, T. (2014). Betamimetics for Inhibiting Preterm Labour. Cochrane Database Syst. Rev. 2, Cd004352. doi:10.1002/14651858.CD004352.pub2
Pritchard, A. M., Hendrix, P. W., and Paidas, M. J. (2016). Hereditary Thrombophilia and Recurrent Pregnancy Loss. Clin. Obstet. Gynecol. 59 (3), 487–497. doi:10.1097/GRF.0000000000000226
Santos, T. D. S., Ieque, A. L., de Carvalho, H. C., Sell, A. M., Lonardoni, M. V. C., Demarchi, I. G., et al. (2017). Antiphospholipid Syndrome and Recurrent Miscarriage: A Systematic Review and Meta-Analysis. J. Reprod. Immunol. 123, 78–87. doi:10.1016/j.jri.2017.09.007
Shen, A. Y., Wang, T. S., Huang, M. H., Liao, C. H., Chen, S. J., and Lin, C. C. (2005). Antioxidant and Antiplatelet Effects of Dang-Gui-Shao-Yao-San on Human Blood Cells. Am. J. Chin. Med. 33 (5), 747–758. doi:10.1142/S0192415X05003351
Sun, L., Liu, L., Zong, S., Wang, Z., Zhou, J., Xu, Z., et al. (2016). Traditional Chinese Medicine Guizhi Fuling Capsule Used for Therapy of Dysmenorrhea via Attenuating Uterus Contraction. J. Ethnopharmacol. 191, 273–279. doi:10.1016/j.jep.2016.06.042
Ushiroyama, T., Hosotani, T., Mori, K., Yamashita, Y., Ikeda, A., and Ueki, M. (2006). Effects of Switching to Wen-Jing-Tang (Unkei-to) from Preceding Herbal Preparations Selected by Eight-Principle Pattern Identification on Endocrinological Status and Ovulatory Induction in Women with Polycystic Ovary Syndrome. Am. J. Chin. Med. 34 (2), 177–187. doi:10.1142/S0192415X06003746
Usuki, S., Higa, T. N., and Soreya, K. (2002). The Improvement of Luteal Insufficiency in Fecund Women by Tokishakuyakusan Treatment. Am. J. Chin. Med. 30 (2-3), 327–338. doi:10.1142/S0192415X02000247
Wahabi, H. A., Fayed, A. A., Esmaeil, S. A., and Bahkali, K. H. (2018). Progestogen for Treating Threatened Miscarriage. Cochrane Database Syst. Rev. 8, Cd005943. doi:10.1002/14651858.CD005943.pub5
Wang, X., Li, L., Ran, X., Dou, D., Li, B., Yang, B., et al. (2016). What Caused the Changes in the Usage of Atractylodis Macrocephalae Rhizoma from Ancient to Current Times? J. Nat. Med. 70 (1), 36–44. doi:10.1007/s11418-015-0934-4
Wang, X., Zhao, Y., and Zhong, X. (2014). Protective Effects of Baicalin on Decidua Cells of LPS-Induced Mice Abortion. J. Immunol. Res. 2014, 859812. doi:10.1155/2014/859812
Washio, M. (2003). Kami-shoyo-san Is Usually Used for Women. Psychiatry Clin. Neurosci. 57 (3), 345. doi:10.1046/j.1440-1819.2003.01129.x
Yang, G. Y., Luo, H., Liao, X., and Liu, J. P. (2013). Chinese Herbal Medicine for the Treatment of Recurrent Miscarriage: a Systematic Review of Randomized Clinical Trials. BMC Complement. Altern. Med. 13, 320. doi:10.1186/1472-6882-13-320
Yeh, H. Y., Chen, Y. C., Chen, F. P., Chou, L. F., Chen, T. J., and Hwang, S. J. (2009). Use of Traditional Chinese Medicine Among Pregnant Women in Taiwan. Int. J. Gynaecol. Obstet. 107 (2), 147–150. doi:10.1016/j.ijgo.2009.07.024
Younger, J. D., Reitman, E., and Gallos, G. (2017). Tocolysis: Present and Future Treatment Options. Semin. Perinatol. 41 (8), 493–504. doi:10.1053/j.semperi.2017.08.008
Zeng, Q. L., and Yao, M. Y. (2010). Progress of Integrative Medical Treatment of Recurrent Natural Abortion Induced by Immune Factor. Zhongguo Zhong Xi Yi Jie He Za Zhi 30 (6), 669–671.
Zhong, X. H., Zhou, Z. X., Li, T. S., Wang, E. Q., Shi, W. Y., and Chu, S. M. (2002). Anti-abortive Effect of Radix Scutellariae and Rhizoma Atractylodis in Mice. Am. J. Chin. Med. 30 (1), 109–117. doi:10.1142/S0192415X02000120
Keywords: preterm labor, threatened miscarriage, tocolytic treatment, Chinese herbal products, National health insurance research database
Citation: Shen H-S, Chang W-C, Chen Y-L, Wu D-L, Wen S-H and Wu H-C (2022) Chinese Herbal Medicines Have Potentially Beneficial Effects on the Perinatal Outcomes of Pregnant Women. Front. Pharmacol. 13:831690. doi: 10.3389/fphar.2022.831690
Received: 08 December 2021; Accepted: 16 May 2022;
Published: 06 June 2022.
Edited by:
Thomas Efferth, Johannes Gutenberg University Mainz, GermanyReviewed by:
Marjon Alina De Boer, VU Medical Center, NetherlandsFerdinando Antonio Gulino, Azienda di Rilievo Nazionale e di Alta Specializzazione (ARNAS) Garibaldi, Italy
Copyright © 2022 Shen, Chang, Chen, Wu, Wen and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hsien-Chang Wu, eHVhbmdAbXM2NS5oaW5ldC5uZXQ=
 Hsuan-Shu Shen
Hsuan-Shu Shen Wei-Chuan Chang4
Wei-Chuan Chang4 Shu-Hui Wen
Shu-Hui Wen Hsien-Chang Wu
Hsien-Chang Wu