
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 10 March 2022
Sec. Drugs Outcomes Research and Policies
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.744038
 Zia Ul Mustafa1,2*
Zia Ul Mustafa1,2* Shahzaib Haroon3
Shahzaib Haroon3 Naeem Aslam4
Naeem Aslam4 Ahsan Saeed5
Ahsan Saeed5 Muhammad Salman6*
Muhammad Salman6* Khezar Hayat7
Khezar Hayat7 Naureen Shehzadi8
Naureen Shehzadi8 Khalid Hussain8
Khalid Hussain8 Amer Hayat Khan1
Amer Hayat Khan1Introduction: While many low-middle income countries (LMICs), including Pakistan, try and ensure patient safety within available resources, there are considerable concerns with medication use. Unsafe and inappropriate medication use, especially high alert medications (HAMs), is one of the important factors compromising patient safety and quality of care. Besides economic loss, HAMs contribute to greater morbidity, hospitalization, and mortality. Physicians as key members of the provision of healthcare are expected to be well aware of the administration and regulations surrounding HAMs. However, the current status is unknown in Pakistan. Consequently, the objectives of this study were to evaluate the knowledge of Pakistani physicians about the administration, regulation, and practices related to HAMs. This builds on our recently published study with nurses.
Methods: An online cross-sectional study design was used, and data were gathered from the physicians throughout Pakistan using previously used self-administered questionnaires during a period of 5 months (January 1 to May 30, 2021). All data were entered and analyzed using SPSS 22 for Windows.
Results: Physicians (847) who provided consent were enrolled in the study. Most physicians (62.2%) were male, aged between 25 and 30 years (75.2%) and had 2- to 5-year work experience (50.9%). About 27% were working in the emergency departments. The median (IQR) knowledge score for HAMs administration and regulation was 5 (3) and 5 (2), respectively. About 46.4% of respondents were found to have moderate knowledge about HAMs; increasing age, work experience, and higher qualifications were significantly associated (p < 0.05) with better HAMs knowledge. Around 58% had good practices relating to HAMs during their routine work. Median practice scores increased significantly (p < 0.05) with age, work experience, and postgraduate qualification.
Conclusion: Most Pakistani physicians possess moderate knowledge about HAMs administration and regulations. However, their practices relating to the HAMs administration and regulations are typically sub-optimal. Consequently, HAMs awareness needs to be improved by including course content in the current curriculum, provision of hospital-based continuous training programs about patient safety and care, and establishment of multi-disciplinary health care teams, including board-certified pharmacists and specialized nurses, for the effective execution of medication use process in Pakistani hospitals in the future.
Medication is one of the frequently used modalities to treat illnesses throughout the world. However, improper medication use has a catastrophic impact on patients increasing adverse events (AEs), morbidity, prolonged hospital stays, costs, and mortality (Al Hamid et al., 2014; Aderemi-Williams et al., 2015; Watanabe et al., 2018; Formica et al., 2018; Giardina et al., 2018) Patient safety is one of the fundamental patient rights and should be ensured during the health care provision process.
According to the World Health Organization (WHO), AEs are included in the top 10 leading causes of death and disability worldwide (WHO, 2019a). Overall, 10% of hospital admissions are reported to be due to AEs following medication (WHO, 2015). More recently among countries in the Organization for Economic Co-operation and Development (OECD), it has been estimated that 15% of total hospital expenditure resulted from AEs (Slawomirski et al., 2017). In addition, in high-income countries, one out of every 10 hospitalized patients were harmed with AEs, with half of them considered preventable (WHO, 2019a). In the United States, more than 7 million hospitalized patients are affected by medication errors (MEs), and MEs are estimated overall to cost $40 billion annually (Tariq et al., 2020). In the United Kingdom, 2.37 million MEs are reported with an economic burden of £98.5 million per year (Hodkinson et al., 2020). The situation is even worse in low-middle income countries (LMICs) where more than 134 million AEs are reported due to unsafe medication, with more than 2.6 million deaths every year (WHO, 2019a). Patient safety is a key concern in the Eastern Mediterranean region where 18% of hospitalizations are associated with AEs; 3% lead to permanent disability or deaths with more than 80% AEs considered preventable (WHO, 2015).
Approximately two decades ago, the WHO instigated activities to enhance patient safety and proposed active debate in World Health Assembly (WHA). The subsequent resolution on patient safety urged Member States to take initiatives against patient harm. This campaign led to the development of safe medication programs across the world (WHO, 2019b). In 2021, again, a resolution presented in the 72nd WHA demonstrated the need to improve patient safety by implementing continuous training and skill development among health care professionals (WHO, 2021).
High alert medications (HAMs) are a special class of medicines bearing a greater risk of patient harm than other medicines when prescribed or administered inappropriately (Labib et al., 2018; Salman et al., 2020). HAMs include chemotherapeutic agents, cardiovascular medicines, anticoagulants, opioids and their derivatives, insulin, neuromuscular blocking agents, benzodiazepines, and certain electrolytes in high concentrations (Zyoud et al., 2019). Consequently, prescription, administration, storage, and handling of HAMs should require specific protocols and regulations to reduce or prevent harm related to their prescribing. The prevalence of MEs due to HAMs ranges from 3.8% to 100% in hospital settings with a pooled prevalence rate of 16.3% (Alves et al., 2021). The severity of these errors in this systematic review ranged from 0.1% to 19.2% for moderate errors and 0.2% to 15.4% for serious errors, and 1.9% lead to death (Alves et al., 2021). MEs related to HAMs can occur due to multiple factors including poor communications between health professionals and patients, the improper passage of medication information, organizational factors, interruption during the medication process, psychological impairment of staff, overburden on healthcare professionals (HCPs), lack of regulation and policies, and insufficient awareness among HCPs (Keers et al., 2013; Sessions et al., 2019).
Pakistan is a LMIC located in South Asia with a struggling health care delivery system due to poor governance, inconsistent health policies, and insufficient resources (Kurji et al., 2016). Despite this, there have been a number of initiatives facilitated by the Government and others in Pakistan to enhance patient safety (Jafree et al., 2017); however, patient safety is challenging. It is recently reported that more than half a million deaths occur in Pakistan every year due to MEs, substantially higher than in the United States where the number of causalities due to MEs range between 7,000 and 9,000 per year (Dawn newspaper, 2017; Tariq et al., 2020). A previous study conducted by Mahmoud et al. among low-middle income Asian countries including Pakistan revealed that more than 95% of MEs were prescribing errors (Mahmoud et al., 2020).
A previous study undertaken in the United States indicated that most of the HCPs did not obtain sufficient training on HAMs during their education regarding medication use and HAMs. More specifically, the involvement of prescribers in the training on HAMs was reported to be lower among physicians compared with pharmacy and nursing personnel (Engels and Ciarkowski, 2015). Being an important member of multidisciplinary health care provision teams, physicians need to be informed about all aspects regarding medicines including their administration and potential harm.
Overall, physicians are a key player in addressing issues relating to patient safety as they are recognized as often initiators of the medication use process across sectors after examining the patients according to their needs. In addition, they often need to play the role of an expert in prescribing the right drug for the right patient with the right dose via the right route of administration (Maxwell, 2016). While there are multiple factors that contribute to MEs (Mutair et al., 2021), these are reduced in high-risk situations if they are properly educated, trained, and equipped to prevent such medicine-related harms (Wittich et al., 2014). Consequently, their knowledge regarding administration, regulations, and practices related to HAMs is of considerable importance to prevent HAMs-related errors among patients. Recently, the death of a 9-month-old baby girl due to abrupt administration of 15% potassium chloride (KCl) enhanced issues of HAMs errors in Pakistan (Salman et al., 2020). In view of this, the objectives of this study were to evaluate the awareness of Pakistani physicians about HAMs administration, regulations, and practices during their routine work. We have previously reported on HAM knowledge among nurses (Salman et al., 2020), and we are aware of previous publications regarding concerns with medication safety among physicians and pharmacists in Pakistan (Jafree et al., 2017; Mahmoud et al., 2020). We wanted to build on this to provide future guidance.
An online cross-sectional, questionnaire-based survey was undertaken among the registered medical practitioners of public sectors and primary, secondary, and tertiary hospitals of all provinces [Punjab, Sindh, Khyber Pakhtunkhwa (KPK), and Baluchistan] and the capital territory (Islamabad) of Pakistan.
All physicians registered with the Pakistan Medical Commission (PMC) (2020) currently serving in Pakistani public hospitals and voluntarily willing to participate in this survey were included in our study. Participants not registered with the PMC, medical students currently out of practice, and those not willing to participate due to any reason were excluded from the current survey.
According to the PMC, 281,072 physicians were registered throughout Pakistan (PMC, 2020). The sample size of the current study was calculated from an online sample size calculator, Rao soft, by considering 50% response distribution, 5% margin of error, and 95% confidence interval. A minimum of 384 physicians were required in the study. However, keeping in view the limitations of convenience sampling and web-based survey design, we empowered the sample by including a design effect. According to earlier studies (Wejnert and Heckathorn, 2008; Masoud et al., 2021), the minimal adequate design effect for convenience-sampled studies is 2. Hence, an adjusted minimum sample of 768 physicians was needed for this study.
A convenient sampling technique was subsequently employed by the investigators, and all potential participants were provided with a link to the e-questionnaire (Google Form) through WhatsApp, Gmail, and Facebook messenger groups of doctors, with a request to complete the survey. Online informed consents were taken from all the study participants prior to their enrolment in the current survey. The link was re-shared after a few days to remind non-participants to submit their responses.
The study tool used in this survey was adapted from a previous study (Hsaio et al., 2010) after permission from the concerned. As the original study questionnaire was in English and the curriculum taught to all physicians in Pakistan is also in English (Salman et al., 2020b), there was no need to translate the study tool into the native language (Urdu). The same data collection tool was employed in a previous study conducted among the registered nurses of Pakistan to extract information about their awareness to HAMs-related administration and regulations (Salman et al., 2020). Moreover, a pilot study was conducted among 20 physicians to improve the utility of study tool for the current study to enhance its robustness. During the pilot study, all the participants were asked about the clarity, understandability, and relevance of all the questions and response options of the study instrument. The original English questionnaire from Hsaio et al. had 20 items to evaluate knowledge about HAMs. However, the questionnaire used in the present study had 19 items because one item (Item # 10, related to Port-a-Cath) was excluded based on the findings of the pilot study to determine content validity. The content validity index after removing the aforementioned item reached 1. Alongside this, Cronbach's alpha of the questionnaire was found to be 0.814, showing adequate internal consistency. We also revised the instrument based on the suggestions of the participants (pilot study) to improve the clarity and understandability of questions. The final content of the study tool had the following four sections:
Section 1 contained six items about the demographic characteristics of the study participants like age (<25 years, 25–30 years, 31–35 years, and ≥36 years), gender (male or female), level of education (graduate or post-graduate), category of the hospital where they were currently serving (primary, secondary, or tertiary care hospital), years of experience (<1 year, 1–5 years, and >5 years), and working department [intensive care unit (ICU), critical care unit (CCU), emergency, surgery etc.].
Section 2 contained nine questions related to the knowledge about HAMs administration. Participants were requested to choose one response from three given options, i.e., yes, no, and do not know.
Section 3 comprised 10 questions about the HAMs-related regulations. This section also had three different options for the participants to select from.
Section 4 had five questions related to the practices regarding HAMs including one question reverse coded to avoid cognitive bias. Participants were allowed to select one option from the five-item Likert scale including always, often, sometimes, rarely, and never.
The scoring system employed in the current study built on the previous study among registered nurses (Salman et al., 2020). Each right response from Sections 2 and 3 was given a score of 1, while a wrong or do not know response was scored 0. Consequently, the total knowledge score on HAMs administration and regulation were 9 and 10, respectively. To calculate the overall knowledge score, each correct answer in Sections 2 and 3 (total of 19 questions) was given 5 points, with a total score of 95; incorrect or do not know answers were scored 0. Knowledge scores were classified as good knowledge ≥70%, moderate knowledge 50–69%, and poor knowledge <50%. The total score related to HAMs practices ranged 5–25; with ≥70% scores indicating good practices, 50–69% as moderate, and <50% scores as poor practices.
Ethical approval of the current study was obtained from the Ethics Committee, Department of Pharmacy Practice, the University of Lahore (UOL) vide approval number REC/DPP/FOP/29 before initiation of study (December 28, 2020). Moreover, online informed consent was obtained from all survey participants before their enrolment in the study. Any queries related to the execution and purpose of this research were sorted out by the investigators. Participants who decided to leave this survey during response filling could do it without any restriction.
The categorical data were presented as frequency and percentages. Median and interquartile ranges (IQRs) were expressed for continuous variables. For inferential analysis, Kruskal–Wallis and Mann–Whitney tests were performed for continuous data. All data analyses were carried out using the Statistical Package for the Social Sciences (SPSS Inc., version 22, IBM, Chicago, IL, United States). A p < 0.05 was set as statistical significance.
As shown in Figure 1, a total of 847 physicians [Punjab 46.4%, Sindh 22.3%, KPK 14.5%, Baluchistan 11.3%, and Islamabad (Capital territory) 5.4%] from across Pakistan completed the questionnaire (participation rate 82.9%). Demographic characteristics of the study participants are presented in Table 1. The majority of the participants were men (62.2%) belonging to 25–30 years age group (75.2%) followed by the 31–35 years age group (13.7%). Nearly half of the study participants had 2–5 years working experience, while 7.9% had more than 5 years working experience. As far as the education of the study participants is concerned, 80% were Bachelor of Medicine, Bachelor of Surgery (MBBS), while 20% of the physicians were Doctor of Medicine (MD)-Master of Surgery (MS)/Fellow of College of Physicians and Surgeons (FCPS). The majority of the study population (58.6%) were working in tertiary care/teaching hospitals, followed by 30.2% from secondary care hospitals. With regard to the working departments, the majority of participants (25.6%) were currently serving in emergency departments followed by surgery and allied departments (19.1%).
As documented in Table 2, the majority of the physicians (74.3%) provided correct responses concerning the administration of epinephrine in mild allergic reactions. About 66.7% of the physicians gave correct response about the administration of calcium chloride (CaCl2), and 71.3% knew that calcium gluconate and CaCl2 were not the same medicines and, therefore, not interchangeable. Surprisingly, only 57.3% gave correct response about the dose expression of insulin. Furthermore, only 63.8% and 55.3% of physicians correctly answered the questions related to administration of 15% KCl and 3% sodium chloride (NaCl). The median (IQR) score related to HAMs administration was 5 (3). As shown in Table 3, there was a significant difference of knowledge score related to HAMs administration (p < 0.05) between age, education (FCPS/MD > MBBS), experience, hospital, and province categories. Inter-group comparison of knowledge scores related to HAMs administration are shown in Table 4. The higher age group was found to be associated with better HAMs administration knowledge scores. Furthermore, physicians having >5 years work experience had significantly better knowledge scores compared with those with 1–5 and <1 year work experience.
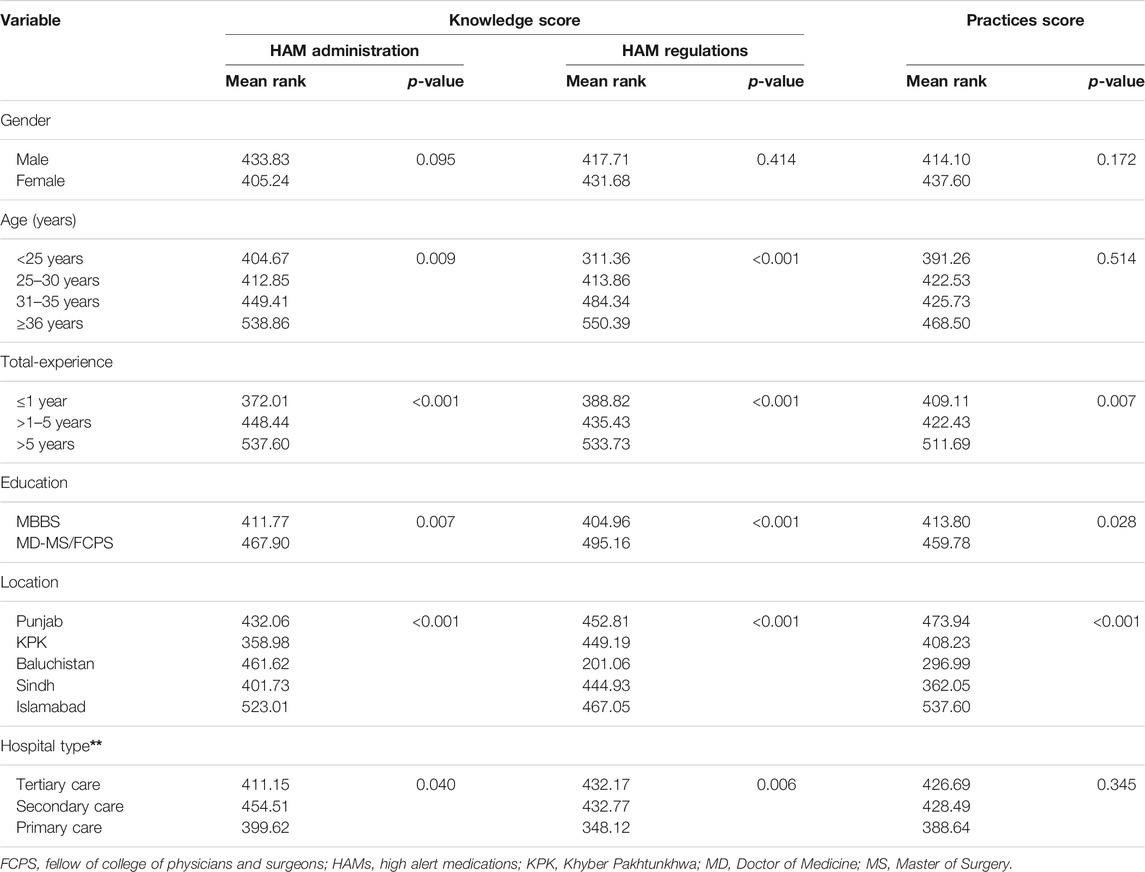
TABLE 3. Comparison of high alert medications knowledge and practices among demographics using Mann–Whitney U and Kruskal–Wallis H tests.
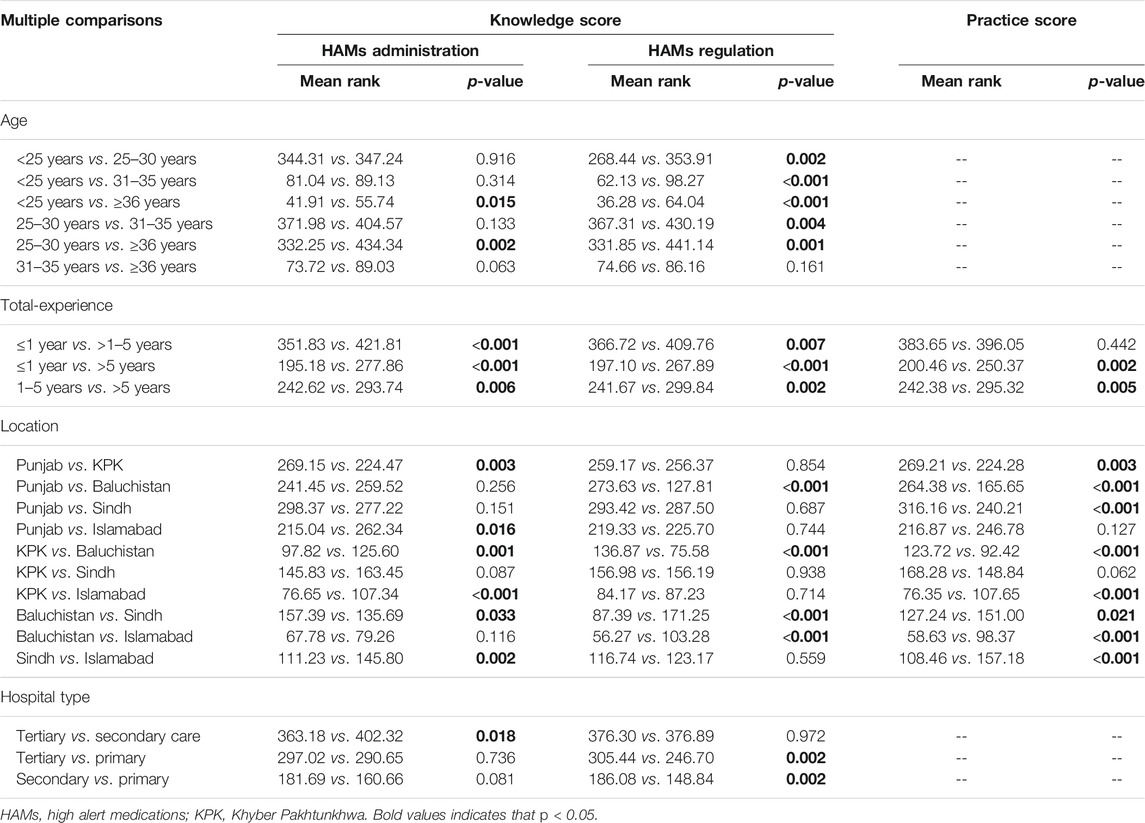
TABLE 4. Inter-group comparisons of high alert medications knowledge and practices score among selected demographic variables
As shown in Table 5, approximately two-thirds of our study participants knew “mg” and “gram” should not be replaced with “ampule” or “vial” for dose expression. Moreover, approximately half of the participants knew not to use inconsistent abbreviations (“U” or “IU” instead of “units”) for the dose expression of HAMs. Only 48.3% of study participants knew insulin and heparin should not be stored together. Additionally, 53.5% provided correct answers regarding the storage of atracurium. The median (IQR) knowledge score related to HAMs regulation was 5 (2). As shown in Table 3, there was a significant difference of knowledge score related to HAMs regulation between age, experience, education (FCPS/MD > MBBS), and province/location categories of physicians. Inter-group comparisons (post hoc analysis) of knowledge score related to HAMs regulations are shown in Table 4. Increasing age was significantly associated with better HAMs regulation knowledge scores. Physicians having >5 years work experience had significantly better knowledge about HAMs regulations than those with 1–5 and <1 year work experience. Furthermore, physicians working in tertiary and secondary care settings had better scores than those from primary care settings.
As depicted in Figure 2, majority (46.4%) of physicians had moderate/average knowledge about HAMs. Only 13.5% of the respondents were found to possess excellent knowledge (score ≥70%) about HAMs.
As shown in Table 6, only 14.4% of the physicians reported of never delivering verbal orders about HAMs to the nursing staff, hence following good practices related to the HAMs. Moreover, 55.3% and 55.8% reported of following standard operating procedures on HAMs in their hospitals and prescribing these drugs in a designated place in the patients' medical record, respectively. About 65% of the physicians reported they prescribe HAMs with complete information to nursing staff to avoid errors. Furthermore, 53% always instructed nursing staff to “double-check” prior to administration. The median HAMs practice score was 20 (4), with the majority (57.9%) of study participants following adequate practices (score >70%) related to HAMs. Total experience, location, and hospital type of the study participants had significant associations (p < 0.05) with median score towards HAM practices (Table 3). Those having a FCPS or MD qualification had significantly better practices than those having only a MBBS qualification. Moreover, as shown in Table 4, physicians having >5 years work experience had significantly better practices than those with 1–5 and <1 year work experience. In addition, physicians from the hospitals in Islamabad and Punjab had better practices than in the others (Table 4).
We believe this is the first study of its kind in Pakistan to evaluate the knowledge and practices on HAMs-related administration and regulations among physicians throughout Pakistan, building on our previous study among nurses (Salman et al., 2020). There were areas of encouragement. However, we identified a number of areas of concern that need to be addressed. Epinephrine is recommended as first-line therapy in anaphylaxis, and it should be administered at a dose of 0.1 mg in the diluted form via slow infusion (in 5–15 min). However, one-fourth of the Pakistani physicians in our study were unable to administer this HAM according to these guidelines. Our previous study conducted among registered nurses revealed similar findings about the administration of epinephrine (Salman et al., 2020). Our findings though are in line with a recent study reported by Wijekoon et al. (2021) from Sri Lanka who revealed that majority of the study population knew that epinephrine is the first-line drug to treat anaphylaxis along with correct dose in children and adults (Wijekoon et al., 2021). Encouragingly, our findings are better than previous studies reported from the United Kingdom, where 15% of physicians were familiar with the recommended way of epinephrine administration in anaphylaxis (Droste and Narayan, 2010; Droste and Narayan, 2012; Tyree et al., 2012).
Similarly, CaCl2, another HAM, indicated for electrolytes abnormalities to advance cardiac life support (Chakraborty and Can, 2021), carries the potential of cutaneous burning sensation and peripheral vasodilation when administered via intravenous (IV) push. Consequently, it is recommended to administer CaCl2 slowly (in 5–10 min) and repeat the same if necessary (Lindner et al., 2020). The concentration of calcium in CaCl2 is three times than that present in calcium gluconate, and hence they cannot be replaced by each other. However, one-third of physicians in our study were not aware of the right way of CaCl2 administration and even considered that CaCl2 can be replaced with calcium gluconate. These findings though are in line with the previous study from the United Kingdom (Powell et al., 2013) that reported poor knowledge among doctors about the IV administration of different IV fluids including CaCl2.
Abrupt administration of concentrated KCl carries the risk of arrhythmias, cardiac arrest, and even deaths reported throughout the world (Grissinger, 2011; Bertol, et al., 2012). Consequently, physicians must prescribe KCl in a diluted form and administer it slowly to avoid complications. However, one-third of our study population were not aware of the right way of KCl administration, and less than half of the participants agreed to add KCl in Ringer's solution despite the chances of metabolic alkalosis. These findings though are similar to the results of a previous study from Japan that reported inadequate physicians' knowledge about the KCl administration necessitating interventions for improvement (Nakatani et al., 2019). Another HAM, insulin, needs to be administered carefully with the right dose usually calculated in international units. Moreover, it should be administered using a dedicated insulin syringe. However, of concern is that nearly half of the physicians in our study were unaware that dose expression for insulin is in international units and not in “ml.” Our findings are contrary though to those of Bain et al. (2019) who reported a better understanding of insulin-related factors among junior doctors, pharmacists, and nurses from the United Kingdom where more than two-thirds of consultant physicians possessed good knowledge about insulin and its administration (Bain et al., 2019).
Incorrect dose calculation, especially among children, is one of the major contributing factors in the emergence of adverse drug events (ADEs). Consequently, physicians are expected to be precise while prescribing to them. However, only one-third of physicians in our study gave correct responses to the question about dose calculation in children and adults. These findings are contrary to the result of a previous study from Australia that reported a high percentage of medical students were well aware of the dose calculation methods (Harries and Botha, 2013). Our survey revealed that the age, level of education, working experience, and hospital type are related to better HAMs administration scores among physicians. These findings are in line with a recent study reported from KPK Province, Pakistan, where age and working experience of the medical doctors are associated with better drug safety knowledge (Sharif et al., 2021). In our previous study conducted among nurses, no associations though were observed between HAMs administration awareness with age, experience, and level of education (Salman et al., 2020). We are not sure of the reasons why; however, this may relate to greater learning curves among physicians as they gain experience. We also found that physicians currently serving in tertiary care/teaching hospitals possessed better HAMs awareness compared with primary and secondary hospital physicians, similar to the previous study conducted among nurses from tertiary care hospitals that found they also had better HAMs knowledge (Salman et al., 2020). This may reflect a greater complexity of cases in tertiary hospitals and the need to be more vigilant regarding HAMs.
HAMs typically require special precautions during their prescription, administration, and storage in the wards. Consequently, special regulations are typically needed to avoid any harm due to their inappropriate use. Using inconsistent abbreviations while prescribing HAMs carries an even greater risk of MEs, so prescribers need to be careful while prescribing them. The use of only “U” instead of “units” needs to be avoided as an appropriate strategy for the prescriber, as discussed in the previous study (Zyoud et al., 2019). Insulin is a refrigerated medicine (2–8°C), whereas heparin should be stored at room temperature under lock and key (Riley and Meyers, 2016). Regarding atracurium regulation, it should be refrigerated at 2–8°C to preserve potency, and it should be used within 14 days, even if re-refrigerated. This is a concern as an earlier study by Engels et al. revealed that 6% of HAMs-related errors were associated with their inappropriate storage (Engels and Ciarkowski, 2015). Again, some physicians in our study were not familiar with these regulations on HAMs. This is different from our findings among registered nurses where the majority of study participants were familiar with HAM related regulations (Salman et al., 2020). This may be because nurses typically administer heparin and consequently are expected to know more about storage requirements.
Verbal orders about medication are associated with MEs due to poor audition, understanding, and wrong word heard; thus, verbal orders about HAMs should not be delivered by the physicians (Moghaddasi et al., 2017). For the safety of patients, there is a recommended place in the patient's medical record for the prescription of HAMs in order that all members of the health care provision team can easily identify it and be attentive while dealing with that drug. After prescribing, physicians must instruct the nursing staff to use a “double-check policy” (Hewitt et al., 2016) to confirm the patient's name, drug name, dose, frequency, and route of administration before initiation of medication administration. Encouragingly, most of our study physicians followed good practices including prescribing HAMs with complete instructions, stressing double-check policies, and following standard operating procedures developed to reduce HAM-related errors as all these strategies have been devised to reduce errors related to HAMs.
This was the first study of its kind to evaluate the knowledge and practices on HAMs-related administration and regulations among physicians throughout Pakistan. We believe our comprehensive study including an appreciably higher number of physicians than the sample size calculations provides policy makers in Pakistan with specific guidance on future measures to enhance patient safety in hospitals. However, we are aware of limitations that were inherent in our study. Firstly, due to COVID-19 restrictions, investigators were unable to approach working physicians directly. Consequently, an online cross-sectional study was conducted using convenient sampling. We are aware though that this sampling method is associated with some shortcomings, e.g., sampling bias, over-representation, and non-generalizability. Secondly, most of the study participants recruited in our survey were MBBS degree holders with comparatively less working experience which may limit the generalizability of the study. Furthermore, as the physicians working in private sector hospitals were not included in our study, our findings may not be representative of the entire Pakistani physicians' population. However, we believe that despite these limitations, this study provides much needed baseline information related to HAMs knowledge among Pakistani physicians to provide future direction to key policy makers and others in Pakistan.
The current survey showed that most of the Pakistani physicians possessed average knowledge about the administration and regulation of HAMs. Similar trends were observed about their practices related to HAM during their routine work. Consequently, policy makers and others need to instigate future measures to enhance patient safety during routine health care provision. All concerned authorities should take appropriate steps to revise the current curriculum in medical institutions to ensure key subjects about patient's safety, in particular, HAMs, are included. All hospital settings should also ensure continuous trainings/workshops for the physicians with a special focus on HAMs and patient safety. Standard operating procedures related to HAMS administration and regulations should also be introduced and monitored at the institutional level. Moreover, hospitals should seek to establish multidisciplinary health care provision teams, if not already implemented, through engaging board-certified clinical pharmacists and specialized nurses to develop guidelines and standard operating procedures to minimize future harms related to the medication use process, and continually monitor activities.
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding authors.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We acknowledge the help of Professor Brian Godman in the development and refinement of this manuscript.
Aderemi-Williams, R. I., Awodele, O., and Boyle, C. A. (2015). Adverse Drug Reactions Amongst Adult Patients Admitted in Lagos State University Teaching Hospital Lagos, Nigeria. Curr. Drug Saf. 10 (2), 136–144. doi:10.2174/1574886309666140601211211
Al Hamid, A., Ghaleb, M., Aljadhey, H., and Aslanpour, Z. (2014). Reply to the Letter Regarding 'A Systematic Review of Hospitalization Resulting from Medicine Related Problems in Adult Patients'. Br. J. Clin. Pharmacol. 78 (2), 1467–1468. doi:10.1111/bcp.12460
Alves, B. M. C. S., de Andrade, T. N. G., Cerqueira Santos, S., Goes, A. S., Santos, A. D. S., Lyra Júnior, D. P., et al. (2021). Harm Prevalence Due to Medication Errors Involving High-Alert Medications: A Systematic Review. J. Patient Saf. 17 (1), e1–e9. doi:10.1097/PTS.0000000000000649
Bain, A., Kavanagh, S., McCarthy, S., and Babar, Z. (2019). Assessment of Insulin-Related Knowledge Among Healthcare Professionals in a Large Teaching Hospital in the United Kingdom. Pharmacy (Basel) 7 (1), 16. doi:10.3390/pharmacy7010016
Bertol, E., Politi, L., and Mari, F. (2012). Death by Potassium Chloride Intravenous Injection: Evaluation of Analytical Detectability. J. Forensic Sci. 57 (1), 273–275. doi:10.1111/j.1556-4029.2011.01907.x
Dawn newspaper (2017). Medication Errors Cause Half a Million Deaths in Pakistan, Say Pharmacists. Available at: https://www.dawn.com/news/1362951#:∼:text=%E2%80%9CAs%20many%20as%20500%2C000%20people,(PSHP)%2C%20at%20a%20press.
Droste, J., and Narayan, N. (2012). Anaphylaxis: Lack of Hospital Doctors' Knowledge of Adrenaline (Epinephrine) Administration in Adults Could Endanger Patients' Safety. Eur. Ann. Allergy Clin. Immunol. 44 (3), 122–127.
Droste, J., and Narayan, N. (2010). Hospital Doctors' Knowledge of Adrenaline (Epinephrine) Administration in Anaphylaxis in Adults Is Deficient. Resuscitation 81 (8), 1057–1058. doi:10.1016/j.resuscitation.2010.04.020
Engels, M. J., and Ciarkowski, S. L. (2015). Nursing, Pharmacy, and Prescriber Knowledge and Perceptions of High-Alert Medications in a Large, Academic Medical Hospital. Hosp. Pharm. 50 (4), 287–295. doi:10.1310/hpj5004-287
Formica, D., Sultana, J., Cutroneo, P. M., Lucchesi, S., Angelica, R., Crisafulli, S., et al. (2018). The Economic burden of Preventable Adverse Drug Reactions: a Systematic Review of Observational Studies. Expert Opin. Drug Saf. 17 (7), 681–695. doi:10.1080/14740338.2018.1491547
Giardina, C., Cutroneo, P. M., Mocciaro, E., Russo, G. T., Mandraffino, G., Basile, G., et al. (2018). Adverse Drug Reactions in Hospitalized Patients: Results of the FORWARD (Facilitation of Reporting in Hospital ward) Study. Front. Pharmacol. 9, 350. doi:10.3389/fphar.2018.00350
Grissinger, M. (2011). Potassium Chloride Injection Still Poses Threats to Patients. P T 36 (5), 241–302.
Harries, C., and Botha, J. (2013). Can Medical Students Calculate Drug Doses? South. Afr. J. Anaesth. Analgesia 19 (5), 248–251. doi:10.1080/22201173.2013.10872934
Hewitt, T., Chreim, S., and Forster, A. (2016). Double Checking: a Second Look. J. Eval. Clin. Pract. 22 (2), 267–274. doi:10.1111/jep.12468
Hodkinson, A., Tyler, N., Ashcroft, D. M., Keers, R. N., Khan, K., Phipps, D., et al. (2020). Preventable Medication Harm across Health Care Settings: a Systematic Review and Meta-Analysis. BMC Med. 18 (1), 313. doi:10.1186/s12916-020-01774-9
Hsaio, G. Y., Chen, I. J., Yu, S., Wei, I. L., Fang, Y. Y., and Tang, F. I. (2010). Nurses' Knowledge of High-Alert Medications: Instrument Development and Validation. J. Adv. Nurs. 66 (1), 177–190. doi:10.1111/j.1365-2648.2009.05164.x
Jafree, S. R., Zakar, R., Zakar, M. Z., and Fischer, F. (2017). Assessing the Patient Safety Culture and ward Error Reporting in Public Sector Hospitals of Pakistan. Saf. Health 3 (1), 1–8. doi:10.1186/s40886-017-0061-x
Keers, R. N., Williams, S. D., Cooke, J., and Ashcroft, D. M. (2013). Causes of Medication Administration Errors in Hospitals: a Systematic Review of Quantitative and Qualitative Evidence. Drug Saf. 36 (11), 1045–1067. doi:10.1007/s40264-013-0090-2
Kurji, Z., Premani, Z. S., and Mithani, Y. (2016). Analysis of the Health Care System of Pakistan: Lessons Learnt and Way Forward. J. Ayub Med. Coll. Abbottabad 28 (3), 601–604.
Labib, J. R., Labib-Youssef, M. R., and Fatah, S. (2018). High Alert Medications Administration Errors in Neonatal Intensive Care Unit: A Pediatric Tertiary Hospital Experience. Turk J. Pediatr. 60 (3), 277–285. doi:10.24953/turkjped.2018.03.007
Lindner, G., Burdmann, E. A., Clase, C. M., Hemmelgarn, B. R., Herzog, C. A., Małyszko, J., et al. (2020). Acute Hyperkalemia in the Emergency Department: a Summary from a Kidney Disease: Improving Global Outcomes Conference. Eur. J. Emerg. Med. 27 (5), 329–337. doi:10.1097/MEJ.0000000000000691
Mahmoud, M. A., Ibrahim, A. A. M., and Alolayan, S. O. (2020). Medication-Related Challenges in Lower Middle-Income Countries of Asia: A Review of Four Countries and Recommendations for Improvement. Syst. Rev. Pharm. 11 (11), 355–359. doi:10.31838/srp.2020.11.52
Masoud, A. T., Zaazouee, M. S., Elsayed, S. M., Ragab, K. M., Kamal, E. M., Alnasser, Y. T., et al. (2021). KAP-COVIDGLOBAL: a Multinational Survey of the Levels and Determinants of Public Knowledge, Attitudes and Practices towards COVID-19. BMJ open 11 (2), e043971. doi:10.1136/bmjopen-2020-043971
Maxwell, S. R. (2016). Rational Prescribing: the Principles of Drug Selection. Clin. Med. (Lond) 16 (5), 459–464. doi:10.7861/clinmedicine.16-5-459
Moghaddasi, H., Farahbaksh, M., and Zehtab, H. (2017). Verbal Orders in Medicine: Challenges; Problems and Solutions. JOJ Nurs. Health Care 1 (5). doi:10.19080/jojnhc.2017.01.555575
Mutair, A. A., Alhumaid, S., Shamsan, A., Zaidi, A. R. Z., Mohaini, M. A., Al Mutairi, A., et al. (2021). The Effective Strategies to Avoid Medication Errors and Improving Reporting Systems. Medicines (Basel) 8 (9), 46. doi:10.3390/medicines8090046
Nakatani, K., Nakagami-Yamaguchi, E., Shinoda, Y., Tomita, S., and Nakatani, T. (2019). Improving the Safety of High-Concentration Potassium Chloride Injection. BMJ Open Qual. 8 (2), e000666. doi:10.1136/bmjoq-2019-000666
Pakistan Medical Commission (2020). Key Statistics. Available at: https://pmc.gov.pk/.
Powell, A. G. M. T., Walker, V. C., Paterson-Brown, L., Clark, G., Drummond, G. B., and Paterson-Brown, S. (2013). Intravenous Fluid Prescribing Knowledge and Confidence in F1 Doctors. Bull. R. Coll. Surgeons Engl. 95 (6). doi:10.1308/147363513x13588739440979
Riley, M., and Meyers, R. (2016). & Advocacy Committee for the Pediatric Pharmacy Advocacy GroupPosition Statement on Heparin Safety Concerns. J. Pediatr. Pharmacol. Ther. 21 (6), 530–532. doi:10.5863/1551-6776-21.6.530
Salman, M., Mustafa, Z. U., Asif, N., Zaidi, H. A., Hussain, K., Shehzadi, N., et al. (2020). Knowledge, Attitude and Preventive Practices Related to COVID-19: a Cross-Sectional Study in Two Pakistani university Populations. Drugs Ther. Perspect. 36, 1–7. doi:10.1007/s40267-020-00737-7
Salman, M., Mustafa, Z. U., Rao, A. Z., Khan, Q. U., Asif, N., Hussain, K., et al. (2020). Serious Inadequacies in High Alert Medication-Related Knowledge Among Pakistani Nurses: Findings of a Large, Multicenter, Cross-Sectional Survey. Front. Pharmacol. 11, 1026. doi:10.3389/fphar.2020.01026
Sessions, L. C., Nemeth, L. S., Catchpole, K., and Kelechi, T. J. (2019). Nurses' Perceptions of High-Alert Medication Administration Safety: A Qualitative Descriptive Study. J. Adv. Nurs. 75 (12), 3654–3667. doi:10.1111/jan.14173
Sharif, M. J. H., Murtaza, G., Kharaba, Z., Ibrahim, N. A., Ismail, M., Mannan, A., et al. (2021). An Exploration of Knowledge, Attitude, and Practices of Physicians toward Pharmacovigilance at Tertiary Care Hospitals in Khyber-Pakhtunkhwa Province, Pakistan. Am. J. Trop. Med. Hyg. 105, 1624–1630. doi:10.4269/ajtmh.21-0336
Slawomirski, L., Auraaen, A., and Klazinga, N. (2017). The Economics of Patient Safety: Strengthening a Value-Based Approach to Reducing Patient Harm at National Level. OECD Health Working Papers, No. 96. Paris: OECD Publishing. doi:10.1787/5a9858cd-en
Tariq, R. A., Vashisht, R., Sinha, A., and Scherbak, Y. (2020). Medication Dispensing Errors and Prevention. Treasure Island, FL, USA: StatPearls.
Tyree, H. K., Gerard, R. B., and Aubrey, R. (2012). Managing the Intravenous Calcium Shortage: Evaluation of Calcium Chloride Stability in 0.9% Sodium Chloride and Dextrose 5% Water Polyvinyl Chloride Bags. Hosp. Pharm. 47 (1), 27–30. doi:10.1310/hpj4701-27
Watanabe, J. H., McInnis, T., and Hirsch, J. D. (2018). Cost of Prescription Drug-Related Morbidity and Mortality. Ann. Pharmacother. 52 (9), 829–837. doi:10.1177/1060028018765159
Wejnert, C., and Heckathorn, D. D. (2008). Web-based Network Sampling: Efficiency and Efficacy of Respondent-Driven Sampling for Online Research. Sociological Methods Res. 37 (1), 105–134. doi:10.1177/0049124108318333
WHO (2015). Patient Safety. Available at: http://www.emro.who.int/entity/patient-safety/index.html.
WHO (2019a). Patient Safety. Available at: https://www.who.int/news-room/fact-sheets/detail/patient-safety (Accessed May 18, 2021).
WHO (2021). Patient Safety. WHA 72.6 Global Action on Patient. Available at: https://extranet.who.int/dataformv3/index.php/166776?lang=en.
WHO (2019b). Patient Safety. Policies and Strategies. Available at: https://www.who.int/patientsafety/policies/en/.
Wijekoon, C. N., Wettasinghe, I., Fernando, D., Dissanayake, A. S., Gunawardana, M., Minuwanpitiya, G., et al. (2021). Preparedness of Pre-intern Medical Graduates of Three Universities in Sri Lanka to Diagnose and Manage Anaphylaxis. BMC Med. Educ. 21 (1), 1–10. doi:10.1186/s12909-021-02588-w
Wittich, C. M., Burkle, C. M., and Lanier, W. L. (2014). Medication Errors: an Overview for Clinicians. Mayo Clin. Proc. 89 (8), 1116–1125. doi:10.1016/j.mayocp.2014.05.007
Keywords: medication, physicians, errors, awareness, administration, regulation
Citation: Mustafa ZU, Haroon S, Aslam N, Saeed A, Salman M, Hayat K, Shehzadi N, Hussain K and Khan AH (2022) Exploring Pakistani Physicians' Knowledge and Practices Regarding High Alert Medications: Findings and Implications. Front. Pharmacol. 13:744038. doi: 10.3389/fphar.2022.744038
Received: 19 July 2021; Accepted: 24 January 2022;
Published: 10 March 2022.
Edited by:
Alvaro Francisco Lopes Sousa, University of São Paulo, BrazilReviewed by:
Mainul Haque, National Defence University of Malaysia, MalaysiaCopyright © 2022 Mustafa, Haroon, Aslam, Saeed, Salman, Hayat, Shehzadi, Hussain and Khan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zia Ul Mustafa, emlhLnVjcEBnbWFpbC5jb20mI3gwMjAwYTs=; Muhammad Salman, bXNrNTAxMkBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.