
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 10 January 2023
Sec. Pharmacoepidemiology
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.1092533
This article is part of the Research Topic Optimizing Medicines for Healthy Ageing View all 6 articles
Background: Residents in long-term care (LTC) facilities (LTCFs) may have multimorbidity and be unable to self-administer medication. Thus, due to the risk of potentially inappropriate medications (PIMs), epidemiological studies on PIM use and its associated factors should be conducted to ensure safe medication use for residents in LTCFs.
Objective: We evaluated PIM use among residents of LTCF and the associated factors in residents of LTCFs in Korea using a nationwide database.
Methods: This cross-sectional study used the Korea National Health Insurance Service Senior Cohort (KNHIS-SC) database 2.0 of the National Health Insurance Service (NHIS), a single public insurer in Korea. We analyzed older adults aged ≥65 years who were residents of LTCFs in 2018, using the KNHIS-SC database. The 2019 American Geriatrics Society (AGS) Beers criteria was used for PIM identification. The prevalence of PIM use was defined as the proportion of LTCF residents who received PIM prescriptions at least once. We evaluated the frequency of prescriptions, including PIMs, and determined the most frequently used PIMs. We also conducted a multivariable logistic regression analysis to identify the factors associated with PIM use.
Results: The prevalence of PIM among the LTCF residents was 81.6%. The prevalence of PIM was 74.9% for LTC grades 1 or 2 (high dependence) and 85.2% for LTC grades 3–5 (low dependence). Quetiapine was the most frequently prescribed PIM, followed by chlorpheniramine. The low dependence level was significantly associated with PIM use (odds ratio of LTC grades 3–5: 1.49, 95% confidence interval 1.32–1.68, reference: LTC grades 1 or 2); moreover, the number of medical institutions visited, and medications emerged as primary influencing factors.
Conclusion: Most LTCF residents were vulnerable to PIM exposure. Furthermore, exposure to PIMs is associated with LTC grade. This result highlights the need for comprehensive medication management of LTCF residents.
The life expectancy of humans at birth has been increasing, and population aging is a global situation (The World Bank, 2020). In Korea, as of 2020, the life expectancy of newborns is 83 years and the proportion of the aged population (≥65 years) is 15.7%. Aging in Korea is progressing rapidly, and Korea is expected to become a super-aged society, with more than 20% of the population aged 65 years or older by 2025 (20.6% of the total population) (The World Bank, 2020; KOrean Statistical Information Service (KOSIS), 2022). Aged people are susceptible to adverse drug reactions (ADRs), and these ADRs could progress to severe disease; the pharmacokinetic and pharmacodynamic response to medications is altered in ADRs, and polypharmacy is common in older adults (Mangoni and Jackson, 2004; Wastesson et al., 2018). ADR-related emergency department visits in aged patients were twice that of the general population, and the risk of the severe ADR was approximately 7 times higher (Budnitz et al., 2006).
Older patients are vulnerable to medication harm, and some potentially inappropriate medications (PIMs) may carry a greater risk to patient than the benefits provided by those medications. Therefore, guidelines for older adults have been announced for PIMs. The Beers Criteria, STOPP/START, NORGEP, and PRISCUS are representative guidelines (Rognstad et al., 2009; Holt et al., 2010; O’Mahony et al., 2015; By the American Geriatrics Society Beers Criteria Update Expert, 2019). The use of PIMs in older adults is associated with ADRs, falls and fractures, hospitalizations, and increased healthcare costs (Hyttinen et al., 2016; Damoiseaux-Volman et al., 2021; Yadesa et al., 2021). Thus, medication management to evaluate and prevent PIM use in older adults is important. The prevalence of PIM use in older adults varies according to study population and guidelines. A systematic review of PIM use in older inpatients reported a prevalence of 30.4%–97.1%, and the prevalence of PIM use in community-dwelling older patients in the US was 42.6% (Davidoff et al., 2015; Redston et al., 2018). Residents in long-term care facilities (LTCFs) are thought to be the frailest members of society because they lose independence in daily life beyond a certain level and have a short life expectancy.
As the aging population increases, the number of residents in LTCF also increases. In Korea, the number of residents in LTCF has increased to 169,405 in 2018 after the adoption of social long-term care insurance (LTCI) in 2008. LTCI is mandatory social insurance and operates by the National Health Insurance Service (NHIS) in Korea. Older adults, as well as younger adults who require long-term care (LTC), are eligible for LTCI. Care needs were assessed by the NHIS based on the care need certification (CNC) system, which is a standardized 52-item functional assessment tool and procedure (Kim et al., 2013). LTCI assesses older adults for their LTC grade based on activities of daily living, cognition, behavioral problems, and need for nursing care and rehabilitation. The LTC grade was classified into six categories according to the degree of need for LTC services identified in the comprehensive evaluation results: Level 1 (older adults with complete dependence), Level 2 (severe dependence), Level 3 (moderate dependence), Level 4 (mild dependence), Level 5 (dementia patients with lighter physical dependence), and Level 6 (dementia patients using services for day-care centers or home-dwellings) (Kim and Kwon, 2021; National Health Insurance Service, 2021).
The prevalence of PIM use in LTCF was reported to be 18.5%–82.6% based on the Beers criteria (Storms et al., 2017) and the factors associated with PIM use in LTCF were age, duration of institutionalization, geriatric score, physician’s role, dementia, and polypharmacy (Anrys et al., 2018; Moreira et al., 2020). In Korea, 58.2% of residents of LTCFs used PIMs, and the number of co-medications and the LTCI grade were associated with PIM use, when data regarding 20 LTCFs were evaluated (Hwang et al., 2015). There is a need to develop strategies for safe medication use among residents in LTCFs. However, to the best of our knowledge, no study has comprehensively evaluated PIM use among LTCF residents in Korea. Considering that the impact of medication could be greater in frail older adults, PIM use should be evaluated according to the LTC level.
Therefore, we aimed to evaluate PIM use and its associated factors in residents of LTCFs in Korea using a nationwide database.
This cross-sectional study used data from the Korea National Health Insurance Service Senior Cohort (KNHIS-SC) database (DB) 2.0 of the National Health Insurance Service (NHIS), a single public insurer in Korea. This database included de-identified information for approximately 8% of the aged population (aged 60 years and older) from 2002 to 2019: sociodemographic data including age, sex, decile of insurance contribution of each subject and death event, healthcare utilization, such as hospitalization, outpatient visits, and medication prescription; results of national health screening services; and information on LTCI, such as LTC grade and type of service used.
This study included older adults who were admitted to LTCF for the first time in 2018 and defined the date of the first claim for LTCF use in 2018 for each patient as the index date. We used the LTCI grade as an indicator of the level of LTC needs. We excluded residents with LTC grade 6 (dementia patients using services for day-care centers or home-dwellings) because they could not use LTCF. We then classified them as LTCF residents based on their LTC grade: LTC grade 1 or 2 for patients with high dependence, and LTC grade 3–5 for patients with low dependence.
We applied the criteria of “potentially inappropriate medication use in older adults” from the 2019 Beers criteria to identify PIM use in the study population; however, the PIM criteria for medications not approved in Korea were not considered (The 2019 American Geriatrics Society Beers Criteria® Update Expert Panel, 2019). PIM use was identified by applying the guideline based on the diagnosis code or medication to evaluate PIM use accurately. The International Classification of Diseases 10th revision (ICD-10) codes are listed in Supplementary Table S1.
PIM use was identified for each outpatient prescription 1 year after the index date, excluding topical agents. The prevalence of PIM use in LTCF residents was calculated using the number of residents who were prescribed PIMs at least once a year and the total number of residents included as the numerator and denominator, respectively. In addition, we evaluated the frequency and duration of PIMs in each patient. The top ten ingredients were identified based on the number of prescriptions.
The characteristics of the included residents and LTCF were considered covariates in this study: 1) for residents, healthcare utilization, socio-demographic characteristics (age, sex, and insurance types), comorbidities using the Charlson Comorbidity Index (CCI) and other chronic diseases, number of medications prescribed, LTC grade, duration of LTCI beneficiaries (from the initial date of LTC grade evaluation to index date), and duration of residence in a LTCF (from the initial claim date of LTCF to index date); 2) for LTCF, the bed capacity, ownership type (private or other, local government, corporate), and number of contracted doctors of LTCF. Healthcare utilization, number of medications prescribed, CCI, and other chronic diseases were identified a year before the index date. Chronic diseases were defined as hospitalization (≥2 days) or two or more outpatient visits according to the main diagnosis code. The ICD-10 codes or ICD-10 of reference medications used are listed in Supplementary Table S1. Other variables, such as age, sex, insurance type, and LTC grade, were identified at the index date.
The mean, standard deviation (SD), and percentage were used for descriptive statistics, and t-tests and chi-squared tests were used to identify differences between the groups. Multiple logistic regression was used to identify factors associated with PIM use among LTCF residents. SAS 9.4 (SAS Institute, Inc., Cary, NC, United States) was used for data management and statistical analyses. The statistical significance was analyzed at a p-value ≤ .05.
In 2018, 51,632 out of 599,513 older adults were LTCI beneficiaries, and 8,835 were LTCF residents (Figure 1). Women accounted for 77.8%, and the mean age was 82.1 years (SD 5.8). Approximately, half of the residents presented with dementia (57.6%) and hypertension (48.9%) as comorbidities, and 39.4% were hospitalized. The LTC grade of most residents was Level 3 (39.2%), the average LTCI beneficiary period was 52.1 months, and the average LTCF residence period was 36.4 months. Among the LTCF residents, 81.6% (n = 7,207) had at least one PIM prescription per year. The number of outpatient visits (23.4 vs. 14.0, p < .001), number of medical institutions used (3.0 vs. 1.9, p < .001), and number of medications (7.7 vs. 5.6, p < .001) were significantly higher for PIM users than for PIM non-users. A proportion of residents (32% and 47.5%) who were PIM users and non-users, respectively, had LTC grades 1–2 (with high dependence) (p < .001) (Table 1).
Healthcare utilization and PIM use according to the LTC grade are shown in Table 2. Residents with LTC grades 3–5 had more outpatient visits, number of medical institutions visited, and prescriptions, compared to residents with LTC grade 1–2 (no. of outpatient visits 20.5 vs. 22.3, p < .001; no. of medical institutions visited 2.4 vs. 3.0, p < .001; and no. of outpatient visits 19.5 vs. 22.5, p < .001, respectively). Nevertheless, 74.9% and 85.2% of residents with LTC grade 1–2 and LTC grade 3–5 were PIM users, respectively (p < .001). The number of prescriptions with PIM and the prescription period for PIM use in LTC grade 3–5 resident PIM users were significantly higher than those in LTC grade 1–2 resident PIM users (no. of prescriptions 12.4 vs. 10.5, p < .001 and prescription period of PIM 250.5 vs. 215.8, p < .001, respectively).
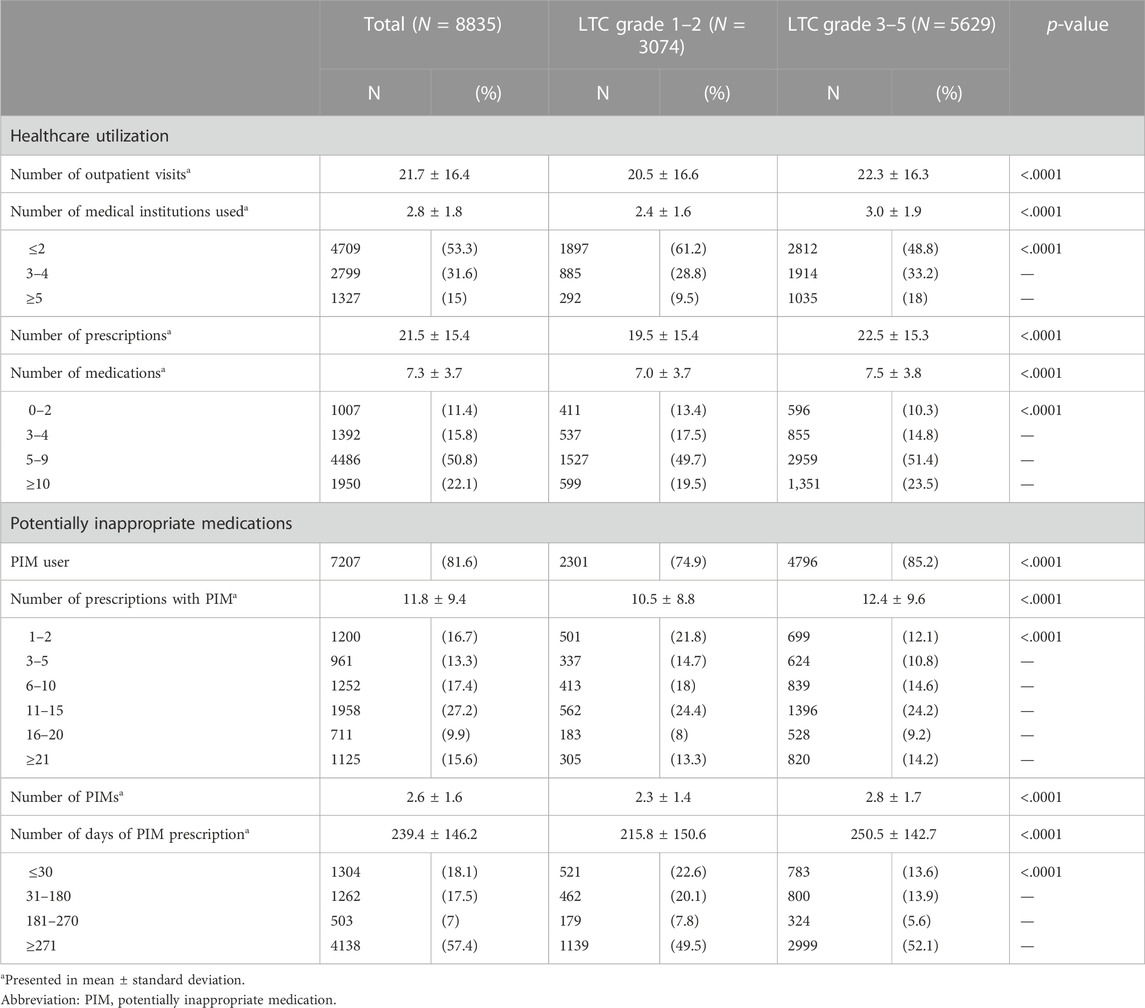
TABLE 2. Healthcare utilization and potentially inappropriate medication use according to the LTC grade.
The PIM prescribed most frequently to LTCF residents was quetiapine (22.8%), followed by chlorpheniramine (13.8%), and zolpidem (7.1%; Table 3). The top three PIM medications were the same regardless of LTC grade. No difference was found between the two groups in terms of the composition of the top ten PIMs within the different rankings.
Table 4 shows the risk factors associated with the use of PIM. The older age group had a lower likelihood of PIM use than the group with individuals aged 65–74 years (Additional information of the model was reported in Supplementary Table S2). Medical aid beneficiaries and residents with mental disorders, including dementia, were associated with a higher likelihood of PIM use. LTC grade 3–5 was significantly associated with PIM use (odds ratio: 1.49, 95% CI: 1.32–1.68). As the number of medical institutions visited and medications increased, the likelihood of PIM prescriptions increased. The characteristics related to LTC, such as length of stay in LTCF, duration of LTCI, ownership type of LTCF, number of contracted physicians in LTCF, and bed capacity of LTCF, were not significantly affected by PIM use.

TABLE 4. Risk factors of potentially inappropriate medication use in long-term care facility residents.
Most LTCF residents were vulnerable to PIM exposure. PIM users visited physicians more, visited various medical institutions, received more prescriptions, and took more medications than PIM non-users. Our results show that PIM use by LTCF residents in Korea (81.6%) was high. The high prevalence of PIM could be explained by differences in PIM criteria and population characteristics. The PIMs of the Beers criteria have been expanded as the criteria were revised (American Geriatrics Society Beers Criteria Update Expert Panel, 2012; American Geriatrics Society Beers Criteria Update Expert Panel et al., 2015). According to a systematic review (SR) reporting the range of PIM prevalence in LTCF, the PIM prevalence in the study using Beers 2012 criteria (58.2%–82.6%) was higher than that reported in studies using Beers pre-2012 criteria (18.5%–50.3%) (Storms et al., 2017). In addition, a recent study using Beers 2019 reported a 90.8% prevalence of PIM in nursing home residents (Díez et al., 2022). The prevalence of PIM use among older adults in Asian countries is relatively high. The prevalence of PIM was reported to be 66.7%–72.5% among older Chinese adults (Yang et al., 2015; Li et al., 2017), 77.2%–78.4% among older Japanese adults (Komagamine and Hagane, 2017; Komagamine et al., 2018), and 70.3%–81.0% among older Korean adults (Kim et al., 2016; Nam et al., 2016; Jang et al., 2021). One possible reason for the high prevalence of PIM was polypharmacy, which was associated with PIM according to the SR of PIM predictors (Tommelein et al., 2015). Asian countries have a cultural preference for medicines (Lo et al., 1994; Bates et al., 1995).
Furthermore, the risk of exposure to PIM is associated with the LTC grade, which indicates the degree of dependence in daily life. Residents with LTC grades 3–5 (low dependence) visited various medical centers and had more frequent outpatient visits and prescriptions than those with LTC grades 1 or 2 (high dependence). One possible explanation is that residents with low dependence could voluntarily use medical services more than those with high dependence. For LTCF residents in Korea, outpatient care can be received by a physician contracted with an LTCF; however, visiting an external medical institution, depending on the residents’ choices, is also possible. A previous study on LTCI beneficiaries in Korea reported similar results: those with low dependence (i.e., higher grades in social LTCI) had more outpatient visits, medications, and prescription days (Kang et al., 2021). The deprescribing effort for patients with limited life expectancy could also be an explanation. Deprescribing is an effort to reduce and manage inappropriate polypharmacy in older patients, which is more emphasized in frail older patients (Thompson and Farrell, 2013). According to a study that reported the cause of deprescribing according to physician specialties, the first reason for deprescribing by geriatricians was the limited benefit given the limited lifespan. This was different from the most common cause of deprescribing in other specialties such as ADRs (Goyal et al., 2020). Also, most patients and caregivers (77.6% and 76.4%, respectively) in Korea wanted to reduce the number of medications (Lee et al., 2022).
The factors associated with PIM use were sex; age; the beneficiaries of Medical Aid; number of medical institutions used; number of medications (or polypharmacy); and presence of dementia, mental disorders, or osteoarthritis, in line with previous studies (Vieira de Lima et al., 2013; Chang et al., 2014; Almeida et al., 2019; Moreira et al., 2020; Roux et al., 2020). Furthermore, we confirmed that residents with low dependence had a higher likelihood of PIM use. Hwang et al. showed that patients with low dependence (i.e., higher LTCI grade) had a higher likelihood of PIM use among older adults living in LTCF; however, this study was conducted for only 20 LTCFs (Hwang et al., 2015). Among overall senior patients, frail senior citizens (such as LTCF residents) are more likely to receive PIM prescriptions than normal senior citizens (Arnoldo et al., 2016; Maclagan et al., 2017); however, our results indicate that PIM use could be low in the frailer senior citizens among LTCF residents. Contrary to the private LTCFs, which exhibited a pattern of more PIM use than public LTCFs in a previous study (Liew et al., 2019), the characteristics of LTCF, such as ownership type, bed capacity, and the number of contracted physicians, were not associated with PIM use. As most LTCFs in Korea are for-profit facilities operated by corporations and private companies (95.3%), the insignificant effect of LTCF setting could be partially explained.
This study has several limitations. First, owing to the characteristics of the claims data, actual medication use could not be confirmed. However, given that the study participants inhabited LTCF, the difference between prescription information and actual medication intake may be minimal. Second, due to the lack of clinical data and absence of medical charts, the reasons for prescribing were not available. Therefore, we could not determine whether the physician decided that the benefits outweighed the risks of PIM use. Third, because the longitudinal cohort (KNHIS-SC DB) was constructed with patients in 2008, the included patients might have been older than the general aged population in Korea as LTCF residents in 2018. Considering the change in criteria for the LTC needs level in 2018 and the latest data on medication use, 2018 was selected as the study year, instead of the year when the cohort was constructed (2008).
The effective and safe use of medicine, particularly for frail older adults, such as LTCF residents, is crucial. We found most LTCF residents to be vulnerable to PIM exposure. Furthermore, exposure to PIMs is associated with LTC needs (i.e., LTC grade). Among the residents of LTCF, those with low LTC needs had more outpatient visits, medications, and PIM use. We should consider LTC and medical needs to optimize medications for senior LTCF residents. This result highlights the need for comprehensive medication management in LTCF residents.
The data analyzed in this study is subject to the following licenses/restrictions: This study used data from the Korea National Health Insurance Service—Senior Cohort (KNHIS–SC) database 2.0 (NHIS–2022–2–073). Third-party data were obtained from the Korean National Health Insurance Service (KNHIS). The authors had no special access privileges to the data. Interested, qualified researchers can apply for access to the data by contacting the KNHIS. Requests to access these datasets should be directed to https://nhiss.nhis.or.kr/bd/ab/bdaba001cv.do.
The studies involving human participants were reviewed and approved by Institutional Review Board of Gachon University (IBN No. 1044396-202111-HR-236-01). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
SJa, Y-MA, and SJn conceived and designed the study. SJa and YK collected and analyzed the data. SJa and Y-MA contributed equally to the interpretation of results and writing of the manuscript. SJn, J-YL, and J-HK participated in drafting the manuscript and critically revised it for content. All the authors have read and approved the manuscript.
This research was supported by a grant of Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health and Welfare, Republic of Korea (Grant No. HC21C0069).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.1092533/full#supplementary-material
ADR, Adverse drug reaction; CCI, Charlson Comorbidity Index; ICD-10, The International Classification of Diseases 10th revision; KNHIS-SC DB, Korea National Health Insurance Service Senior Cohort database; LTCF, Long-term care facility; LTCI, Long-term care insurance; NHIS, National Health Insurance Service; NSAID, non-steroidal anti-inflammatory inhibitor; OR, odds ratio; PIM, Potentially inappropriate medication; SD, standard deviation.
Almeida, T. A., Reis, E. A., Pinto, I. V. L., Ceccato, M., Silveira, M. R., Lima, M. G., et al. (2019). Factors associated with the use of potentially inappropriate medications by older adults in primary health care: An analysis comparing AGS Beers, EU(7)-PIM List, and Brazilian Consensus PIM criteria. Res. Soc. Adm. Pharm. 15, 370–377. doi:10.1016/j.sapharm.2018.06.002
American Geriatrics Society Beers Criteria Update Expert Panel (2012). A merican G eriatrics S ociety updated B eers C riteria for potentially inappropriate medication use in older adults. J. Am. Geriatrics Soc. 60, 616–631. doi:10.1111/j.1532-5415.2012.03923.x
Anrys, P. M. S., Strauven, G. C., Foulon, V., Degryse, J. M., Henrard, S., and Spinewine, A. (2018). Potentially inappropriate prescribing in Belgian nursing homes: Prevalence and associated factors. J. Am. Med. Dir. Assoc. 19, 884–890. doi:10.1016/j.jamda.2018.06.010
Arnoldo, L., Cattani, G., Cojutti, P., Pea, F., and Brusaferro, S. (2016). Monitoring polypharmacy in healthcare systems through a multi-setting survey: Should we put more attention on long term care facilities? J. Public Health Res. 5, 745. doi:10.4081/jphr.2016.745
Bates, D. W., Boyle, D. L., Vander Vliet, M. B., Schneider, J., and Leape, L. (1995). Relationship between medication errors and adverse drug events. J. Gen. Intern. Med. 10, 199–205. doi:10.1007/BF02600255
Budnitz, D. S., Pollock, D. A., Weidenbach, K. N., Mendelsohn, A. B., Schroeder, T. J., and Annest, J. L. (2006). National surveillance of emergency department visits for outpatient adverse drug events. Jama 296, 1858–1866. doi:10.1001/jama.296.15.1858
By the American Geriatrics Society Beers Criteria Update Expert (2019). American geriatrics society 2019 updated AGS beers Criteria® for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 67, 674–694. doi:10.1111/jgs.15767
Chang, C. B., Lai, H. Y., Yang, S. Y., Wu, R. S., Liu, H. C., Hsu, H. Y., et al. (2014). Patient- and clinic visit-related factors associated with potentially inappropriate medication use among older home healthcare service recipients. PLoS One 9, e94350. doi:10.1371/journal.pone.0094350
Damoiseaux-Volman, B. A., Raven, K., Sent, D., Medlock, S., Romijn, J. A., Abu-Hanna, A., et al. (2021). Potentially inappropriate medications and their effect on falls during hospital admission. Age Ageing 51. doi:10.1093/ageing/afab205
Davidoff, A. J., Miller, G. E., Sarpong, E. M., Yang, E., Brandt, N., and Fick, D. M. (2015). Prevalence of potentially inappropriate medication use in older adults using the 2012 Beers criteria. J. Am. Geriatr. Soc. 63, 486–500. doi:10.1111/jgs.13320
Díez, R., Cadenas, R., Susperregui, J., Sahagún, A. M., Fernández, N., García, J. J., et al. (2022). Potentially inappropriate medication and polypharmacy in nursing home residents: A cross-sectional study. J. Clin. Med. 11, 3808. doi:10.3390/jcm11133808
Goyal, P., Anderson, T. S., Bernacki, G. M., Marcum, Z. A., Orkaby, A. R., Kim, D., et al. (2020). Physician perspectives on deprescribing cardiovascular medications for older adults. J. Am. Geriatr. Soc. 68, 78–86. doi:10.1111/jgs.16157
Holt, S., Schmiedl, S., and Thürmann, P. A. (2010). Potentially inappropriate medications in the elderly: The PRISCUS list. Dtsch. Arztebl Int. 107, 543–551. doi:10.3238/arztebl.2010.0543
Hwang, H.-J., Kim, S.-H., and Lee, K. S. (2015). Potentially inappropriate medications in the elderly in Korean long-term care facilities. Drugs-real world outcomes 2, 355–361. doi:10.1007/s40801-015-0046-1
Hyttinen, V., Jyrkkä, J., and Valtonen, H. (2016). A systematic review of the impact of potentially inappropriate medication on health care utilization and costs among older adults. Med. Care 54, 950–964. doi:10.1097/MLR.0000000000000587
Jang, S., Jeong, S., and Jang, S. (2021). Patient-and prescriber-related factors associated with potentially inappropriate medications and drug–drug interactions in older adults. J. Clin. Med. 10, 2305. doi:10.3390/jcm10112305
Kang, H.-J., Jang, S., and Jang, S. (2021). Comparison of medical utilization and drug prescription patterns of long-term care insurance beneficiaries and non-beneficiaries. Yakhak Hoeji 65, 453–459. doi:10.17480/psk.2021.65.6.453
Kim, D. S., Jeon, H. L., Park, J., and Bae, S. (2016). Factors associated with potentially inappropriate medication use in elderly Koreans in an outpatient setting: A population-based study. J. Am. Geriatrics Soc. 64, e21–e23. doi:10.1111/jgs.14267
Kim, H., and Kwon, S. (2021). A decade of public long-term care insurance in South Korea: Policy lessons for aging countries. Health Policy 125, 22–26. doi:10.1016/j.healthpol.2020.11.003
Kim, H., Kwon, S., Yoon, N. H., and Hyun, K. R. (2013). Utilization of long-term care services under the public long-term care insurance program in Korea: Implications of a subsidy policy. Health Policy 111, 166–174. doi:10.1016/j.healthpol.2013.04.009
Komagamine, J., and Hagane, K. (2017). Intervention to improve the appropriate use of polypharmacy for older patients with hip fractures: An observational study. BMC Geriatr. 17, 288. doi:10.1186/s12877-017-0681-3
Komagamine, J., Sugawara, K., and Hagane, K. (2018). Characteristics of elderly patients with polypharmacy who refuse to participate in an in-hospital deprescribing intervention: A retrospective cross-sectional study. BMC Geriatr. 18, 96. doi:10.1186/s12877-018-0788-1
KOrean Statistical Information Service (KOSIS) (2022). Kosis Estimated population by major age group. Available: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA003&vw_cd=MT_ZTITLE&list_id=A41_10&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=MT_ZTITLE&path=%252FstatisticsList%252FstatisticsListIndex.do (Accessed Aug 10, 2022).
Lee, H.-G., Kwon, S., Jang, B.-H., Jeon, J. P., Lee, Y.-S., Jung, W.-S., et al. (2022). A study on the perceptions of Korean older adult patients and caregivers about polypharmacy and deprescribing. Int. J. Environ. Res. Public Health 19, 11446. doi:10.3390/ijerph191811446
Liew, N. Y., Chong, Y. Y., Yeow, S. H., Kua, K. P., Saw, P. S., and Lee, S. W. H. (2019). Prevalence of potentially inappropriate medications among geriatric residents in nursing care homes in Malaysia: A cross-sectional study. Int. J. Clin. Pharm. 41, 895–902. doi:10.1007/s11096-019-00843-1
Li, H., Pu, S., Liu, Q., Huang, X., Kuang, J., Chen, L., et al. (2017). Potentially inappropriate medications in Chinese older adults: The beers criteria compared with the screening tool of older persons' prescriptions criteria. Geriatr. Gerontol. Int. 17, 1951–1958. doi:10.1111/ggi.12999
Lo, A. Y., Hedley, A. J., Pei, G. K., Ong, S. G., Ho, L. M., Fielding, R., et al. (1994). Doctor-shopping in Hong Kong: Implications for quality of care. Int. J. Qual. Health Care 6, 371–381. doi:10.1093/intqhc/6.4.371
Maclagan, L. C., Maxwell, C. J., Gandhi, S., Guan, J., Bell, C. M., Hogan, D. B., et al. (2017). Frailty and potentially inappropriate medication use at nursing home transition. J. Am. Geriatr. Soc. 65, 2205–2212. doi:10.1111/jgs.15016
Mangoni, A. A., and Jackson, S. H. (2004). Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. Br. J. Clin. Pharmacol. 57, 6–14. doi:10.1046/j.1365-2125.2003.02007.x
Moreira, F. S. M., Jerez-Roig, J., Ferreira, L., Dantas, A., Lima, K. C., and Ferreira, M. a. F. (2020). Use of potentially inappropriate medications in institutionalized elderly: Prevalence and associated factors. Cien Saude Colet. 25, 2073–2082. doi:10.1590/1413-81232020256.26752018
Nam, Y. S., Han, J. S., Kim, J. Y., Bae, W. K., and Lee, K. (2016). Prescription of potentially inappropriate medication in Korean older adults based on 2012 beers criteria: A cross-sectional population based study. BMC Geriatr. 16, 118. doi:10.1186/s12877-016-0285-3
National Health Insurance Service (2021). Long term care insurance statistical yearbook. Korea: National Health Insurance Service, 2020.
O'mahony, D., O'sullivan, D., Byrne, S., O'connor, M. N., Ryan, C., and Gallagher, P. (2015). STOPP/START criteria for potentially inappropriate prescribing in older people: Version 2. Age Ageing 44, 213–218. doi:10.1093/ageing/afu145
Redston, M. R., Hilmer, S. N., Mclachlan, A. J., Clough, A. J., and Gnjidic, D. (2018). Prevalence of potentially inappropriate medication use in older inpatients with and without cognitive impairment: A systematic review. J. Alzheimers Dis. 61, 1639–1652. doi:10.3233/JAD-170842
Rognstad, S., Brekke, M., Fetveit, A., Spigset, O., Wyller, T. B., and Straand, J. (2009). The Norwegian General Practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients. A modified Delphi study. Scand. J. Prim. Health Care 27, 153–159. doi:10.1080/02813430902992215
Roux, B., Sirois, C., Simard, M., Gagnon, M. E., and Laroche, M. L. (2020). Potentially inappropriate medications in older adults: A population-based cohort study. Fam. Pract. 37, 173–179. doi:10.1093/fampra/cmz060
American Geriatrics Society Beers Criteria Update Expert Panel, Fick, D.M. Semla, T. P., Beizer, J., Brandt, N., Dombrowski, R., Dubeau, C. E., Eisenberg, W., et al. (2015). American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J. Am. Geriatrics Soc. 63, 2227–2246. doi:10.1111/jgs.13702
Storms, H., Marquet, K., Aertgeerts, B., and Claes, N. (2017). Prevalence of inappropriate medication use in residential long-term care facilities for the elderly: A systematic review. Eur. J. Gen. Pract. 23, 69–77. doi:10.1080/13814788.2017.1288211
The World Bank (2020). Life expectancy at birth, total (years) [Online]. Available: https://data.worldbank.org/indicator/SP.DYN.LE00 (Accessed Aug 09, 2022).
Thompson, W., and Farrell, B. (2013). Deprescribing: What is it and what does the evidence tell us? Can. J. Hosp. Pharm. 66, 201–202. doi:10.4212/cjhp.v66i3.1261
Tommelein, E., Mehuys, E., Petrovic, M., Somers, A., Colin, P., and Boussery, K. (2015). Potentially inappropriate prescribing in community-dwelling older people across Europe: A systematic literature review Eur. J. Clin. Pharmacol. 71, 1415–1427. doi:10.1007/s00228-015-1954-4
Vieira De Lima, T. J., Garbin, C. A., Garbin, A. J., Sumida, D. H., and Saliba, O. (2013). Potentially inappropriate medications used by the elderly: Prevalence and risk factors in Brazilian care homes. BMC Geriatr. 13, 52. doi:10.1186/1471-2318-13-52
Wastesson, J. W., Morin, L., Tan, E. C. K., and Johnell, K. (2018). An update on the clinical consequences of polypharmacy in older adults: A narrative review. Expert Opin. Drug Saf. 17, 1185–1196. doi:10.1080/14740338.2018.1546841
Yadesa, T. M., Kitutu, F. E., Deyno, S., Ogwang, P. E., Tamukong, R., and Alele, P. E. (2021). Prevalence, characteristics and predicting risk factors of adverse drug reactions among hospitalized older adults: A systematic review and meta-analysis. SAGE Open Med. 9, 20503121211039099. doi:10.1177/20503121211039099
Yang, P. J., Lee, Y. T., Tzeng, S. L., Lee, H. C., Tsai, C. F., Chen, C. C., et al. (2015). Potentially inappropriate prescribing in disabled older patients with chronic diseases: A screening tool of older persons' potentially inappropriate prescriptions versus beers 2012 criteria. Med. Princ. Pract. 24, 565–570. doi:10.1159/000435955
Keywords: potentially inappropriate medications, long-term care facilities, long-term care grade, determinants, comprehensive medication management, adverse drug reaction
Citation: Jang S, Ah Y-M, Jang S, Kim Y, Lee J-Y and Kim J-H (2023) Potentially inappropriate medication use and associated factors in residents of long-term care facilities: A nationwide cohort study. Front. Pharmacol. 13:1092533. doi: 10.3389/fphar.2022.1092533
Received: 08 November 2022; Accepted: 23 December 2022;
Published: 10 January 2023.
Edited by:
Amy Page, University of Western Australia, AustraliaCopyright © 2023 Jang, Ah, Jang, Kim, Lee and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sunmee Jang, c21qYW5nQGdhY2hvbi5hYy5rcg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.