- 1Yunnan Provincial Key Laboratory of Pharmacology, Kunming Medical University, Kunming, China
- 2Department of Pharmacy, Fuwai Yunnan Cardiovascular Hospital, Kunming, China
Background: Pulmonary arterial hypertension (PAH) associated with congenital heart disease (PAH-CHD) occurs predominantly among patients with uncorrected congenital heart disease (CHD). It is an intractable problem to control PAH continuously and stably after an operation.
Methods: 1) OPLS-DA combined with S-plot was used to retrospectively analyze the results of preoperative and postoperative PAH and 39 biochemical indicators of 235 patients admitted to Fuwai Yunnan Cardiovascular Hospital from January 2019 to December 2020. 2) Combined with Meta-analysis, the recurrence in postoperative PAH was analyzed in terms of operation factors, doses administered, and age factors.
Results: 1) 4 indicators (PAH, RBC, HGB, and CO2) that reflect the prognosis of patients had been found by OPLS-DA combined with S-plot. 2) The recurrence rate of postoperative PAH was 37.02%. The comprehensive therapeutic effect of interventional closure was better than that of surgical operation. PAH was not significantly higher again in patients who received either the instruction dose or the literature dose. Postoperative combination therapy (bosentan and sildenafil) was more effective than bosentan alone. Recovery after treatment was better in infants than in the other four age groups.
Conclusion: OPLS-DA combined with S-plot was used for the first time to analyze clinical examination data. In this study, this method proved to be a feasible method for analyzing clinical data We recommend interventional closure as the first choice for patients with PAH-CHD. For postoperative oral therapy, we recommend the combination therapy (bosentan with sildenafil). To prevent the recurrence, the dose should be strictly prescribed according to the instructions, literature, or body surface area converted. Moreover, we recommend treatment at a young age in these patients.
Introduction
Pulmonary arterial hypertension (PAH) associated with congenital heart disease (PAH-CHD) occurs predominantly among patients with uncorrected congenital heart disease (CHD). These patients have small cardiac defects (usually ventricular septal defects <1 cm and atrial septal defects <2 cm) (Nazzareno et al., 2016). A significant number of patients have persistent or recurrent PAH after congenital heart repair surgery or percutaneous closure (Xi et al., 2019). Some studies speculate that this phenomenon may be due to high surgical risk (Mclaughlin et al., 2009; Kiefer and Bashore, 2011; Melby et al., 2011). However, no studies had shown the cause of recurrence and no detailed analysis of the indicators that lead to PAH recurrence.
The orthogonal projections to latent structures discriminant analysis (OPLS-DA) is an extension of the principal component analysis (PCA) and currently used mainly for metabolomics data analysis (Zhao et al., 2017). In contrast to basal metabolomics studies, data collection in the clinic is limited, and patient data are only collected at the time of initial consultation and routine examinations. Doctors are accustomed to ignoring normal values in these examinations and interpret abnormal values based on anecdotal rather than scientific evidence. Studies had shown that PCA can save doctors’ time in analyzing clinical indicators (Li and Li, 2020). In this study, OPLS-DA was used for the first time to analyze the routine clinical examination to identify reliable indicators related to the prognosis of patients with PAH-CHD.
Currently, randomized controlled trials of bosentan and sildenafil have been conducted in children (More et al., 2016; Kelly et al., 2017). However, most studies have mostly reported short-term preoperative use of a single drug (bosentan or sildenafil), with no reports of long-term (>9 months) postoperative use (Gilbert et al., 2005; Ashraf and Midany, 2013). In the present long-term follow-up study, we retrospectively analyzed data from patients with PAH-CHD who underwent correction (interventional closure or surgery).
Materials and Methods
Patients’ Characteristics
The institutional review board approved this study and waived the requirement for individual consent because of its retrospective nature. From January 1, 2019 solstice to December 31, 2020, 235 patients with PAH-CHD were admitted and treated in Fuwai Yunnan Cardiovascular Hospital, Kunming, China. We collected the data (PAH, postoperative medications, and 39 other indications from routine examinations) on these patients who underwent correction. Clinical and baseline characteristics of the data were preliminarily analyzed.
Orthogonal Projections to Latent Structures Discriminant Analysis and S-Plot
OPLS-DA of SIMCA 14.1 (Umetrics, Kinnelon, New Jersey) was utilized to analyze and compare the indicators of the preoperative and follow-up groups, and S-plot was made. Forty indicators were including PAH by echocardiography and routine examinations (liver function examination item, kidney function examination item, blood lipid examination item, blood electrolyte, blood cell examination item). Then, we identified the indicators in S-plot where the difference was more than 0.5 and less than −0.5. The pre- and post-operative values of these different indicators were compared. The PAH indicators of the patients were analyzed over 2 years, including the preoperative group, the postoperative group, and the follow-up group.
Analysis of the Causes of Pulmonary Arterial Hypertension Changes
Literature Search and Inclusion Criterion
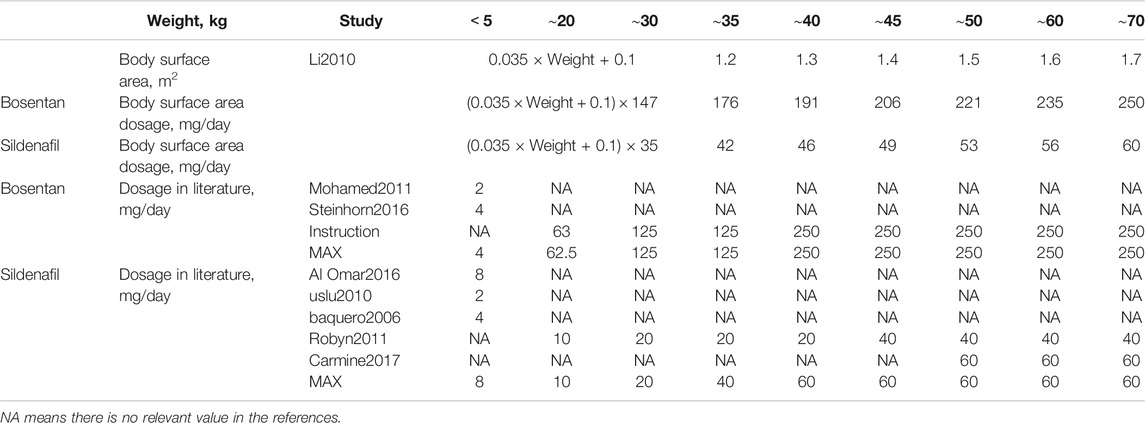
We conducted a comprehensive search for studies of patients with PAH-CHD who underwent correction. The literature was searched using MEDLINE, CNKI, WAN FANG, and Cochrane Library (up to December 2020). The screening methods of the three times are presented in Table 1.
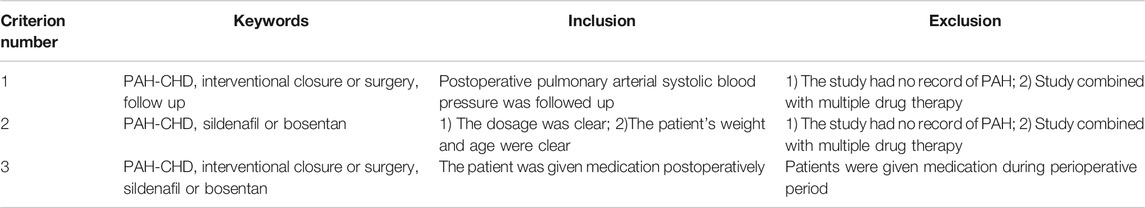
TABLE 1. Inclusion and exclusion criterion for three times literature retrievals in Chinese and English.
Interventional Closure and Surgery
We counted 235 cases of PAH recurrence between interventional closure and surgery. To further understand this difference, we performed the literature search by criterion 1. Firstly, the mean, sd, and n values of PAH in the study were formally adjusted and compared between preoperative, postoperative, and follow-up groups (Li and Li, 2020). Secondly, we performed a conventional meta-analysis to compare the therapeutic and prognostic outcomes of different operations. Differences were assessed by odds ratio (OR) with 95% confidence intervals (CIs). The possibility of publication bias was estimated using funnel plots. Heterogeneity among studies was evaluated by calculating p-value and the I2 measure of inconsistency, which was considered significant if p < 0.10 and I2 > 50%. All calculations were carried out using Review Manager 5.3 (The Nordic Cochrane Center, Copenhagen, Denmark).
Drug Factors
We reviewed the instructions for use of sildenafil and bosentan to ensure correct dosing. The literature was screened according to the criterion 2. At the same time, the dose of the two drugs was calculated according to the patient’s body surface area. The therapeutic and prognostic effects of three doses of sildenafil and bosentan were compared, including body surface dose (DBSA), literature dose (DL), and case review (DCR). Literature was screened according to the criterion 3 to compare the postoperative oral efficacy of the two drugs.
Age Factors
We divided 235 patients into five groups, namely infants (<1 year), toddlers (1–6 years), children (7–14 years), adolescents (15–17 years), and adults (≥18 years). Recurrence, preoperative PAH, and treatment outcomes were analyzed for each group.
Data Analysis
Statistical analysis was performed using t-test and ANOVA. The t-tests and graphs of each drug safety indicators were applied in GraphPad Prism 8 (GraphPad Software, San Diego, Canada). Results were considered statistically significant when the p-value was <0.05.
Result
Patients’ Characteristics
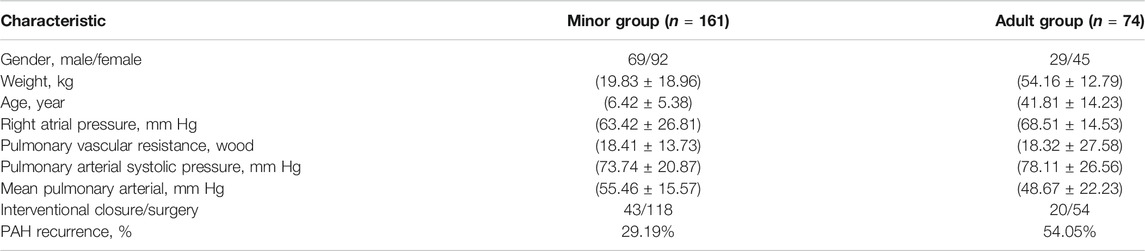
Among 235 patients, the number of juvenile patients was approximately two times that of adult patients, but the proportion of PAH recurrences in the juvenile group was half that of adult group (37.02%) (Table 2).
Orthogonal Projections to Latent Structures Discriminant Analysis and S-Plot
Using OPLS-DA with S-plot, we found four indicators: PAH, red blood cell (RBC), hemoglobin (HGB), and carbon dioxide levels in the blood (CO2) (Figure 1). By analyzing the data of 4 indicators, it was found that t-test result is consistent with the result of the S-plot results.
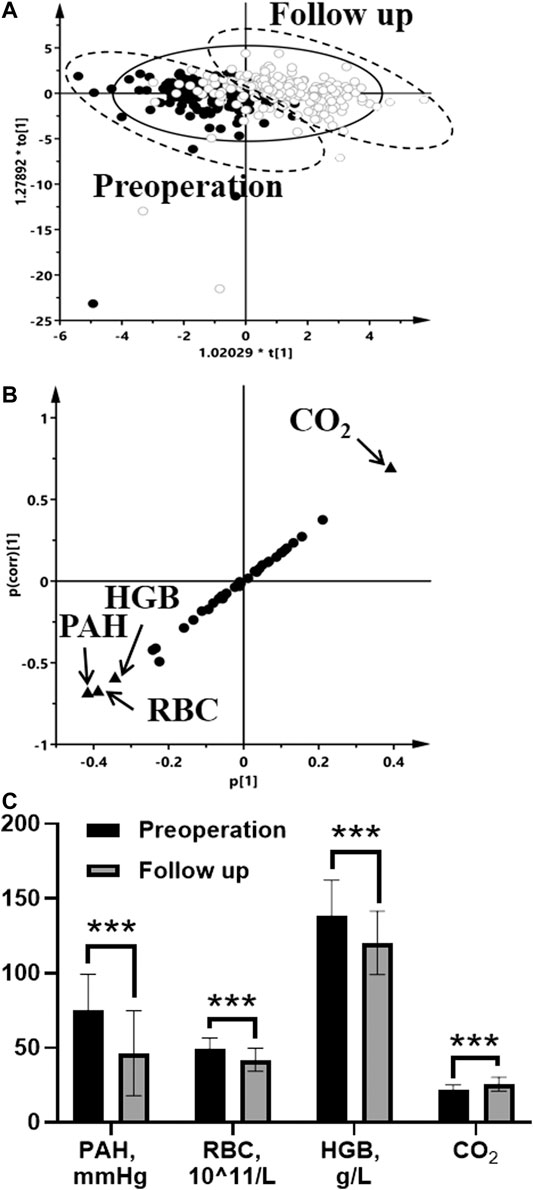
FIGURE 1. Indicators analysis in the preoperative group and the follow-up group by OPLS-DA score plots (A), S-plot (B), and comparison of four difference indicators (C) (●, the preoperative group in score plots; ○, the follow-up group in score plots; four differential indicators are labeled in S-plots). Statistical analysis was performed using t test. *p < 0.05; **p < 0.01; ***p < 0.001.
We performed a statistical analysis of PAH, including preoperative, postoperative, and follow-up periods (Figure 2). After treatment (interventional closure or surgery), PAH improved significantly, with a mean decrease of 28.85 mmHg. However, it increased in the postoperative follow-up group 60–90 days (p < 0.05). There were no subnormal values of pulmonary artery systolic pressure (36 mmHg) in the preoperative, postoperative, and follow-up groups, so we used PAH to represent pulmonary artery systolic pressure.
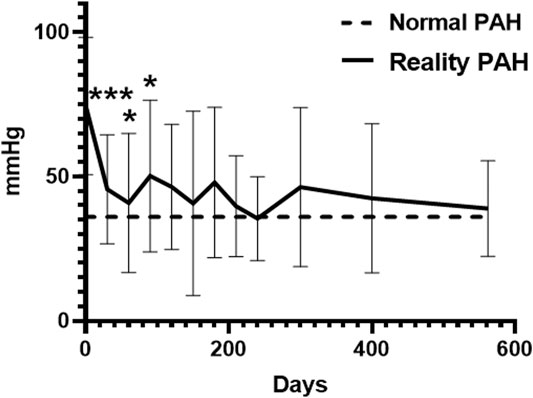
FIGURE 2. PAH changes in 2 years including preoperation, postoperation, and follow up.*p < 0.05; **p < 0.01; ***p < 0.001.
Cause Analysis of Pulmonary Arterial Hypertension Changes
Interventional Closure and Surgery
Echocardiography of pre-treatment PAH was performed in 10 patients only and was not included in the analysis of PAH results. From a review of 224 cases, the recurrence rate of PAH of surgery (50.83%, n = 172) was higher than that of interventional closure (41.26%, n = 52). We selected nine Chinese literature about patients with PAH-CHD who underwent correction according to criterion 1 (Table 3) (Zhang et al., 2012; Jing, 2013; Zhao, 2013; Cao et al., 2016; Jing et al., 2016; Sun et al., 2016; Zhang et al., 2016; Chao and Zhao, 2017; Wang et al., 2020). In Table 3, we also recorded the PAH of both groups in this case review.
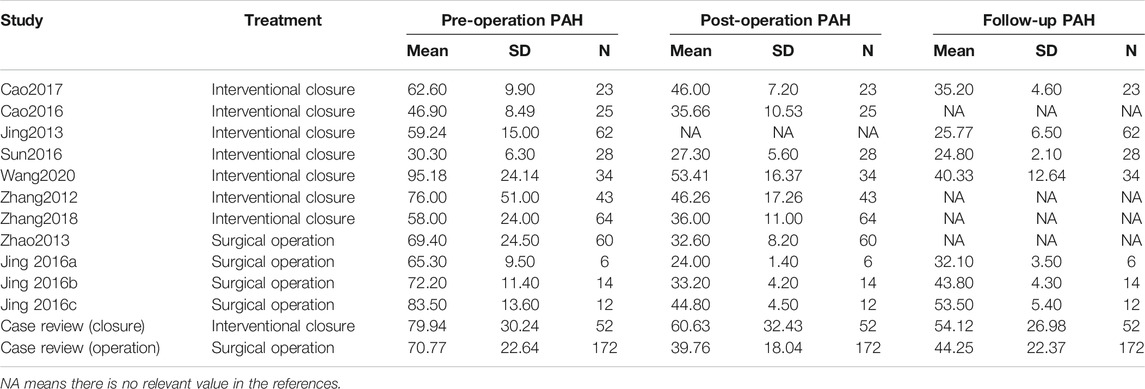
TABLE 3. PAH in nine studies including preoperative group, postoperative group, and follow-up group.
As shown in Figure 3, similar trends in PAH in the case review and literature: 1) PAH decreases significantly after treatment, which was statistically significance (p < 0.05). The decrease in PAH after surgery was more significant than in the interventional closure group. 2) PAH decreased during follow-up in the interventional closure group, but was not statistically significant in the case review, whereas it was statistically significant in the literature (p < 0.05). 3) PAH increased during follow-up in all surgical groups (p < 0.05). According to the meta-analysis (Figure 4), closure and surgery are feasible to reduce PAH in patients with PAH-CHD (p < 0.10, I2 > 50%). Pulmonary artery pressure control was poor in the postoperative group (I2 < 50%), whereas it was good in the closed group (p < 0.10, I2 > 50%).
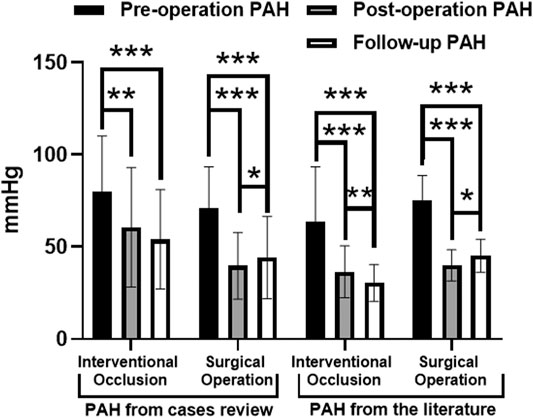
FIGURE 3. PAH in case review and nine studies between interventional occlusion and surgical operation including preoperation, postoperation, and follow up.*p < 0.05; **p < 0.01; ***p < 0.001.
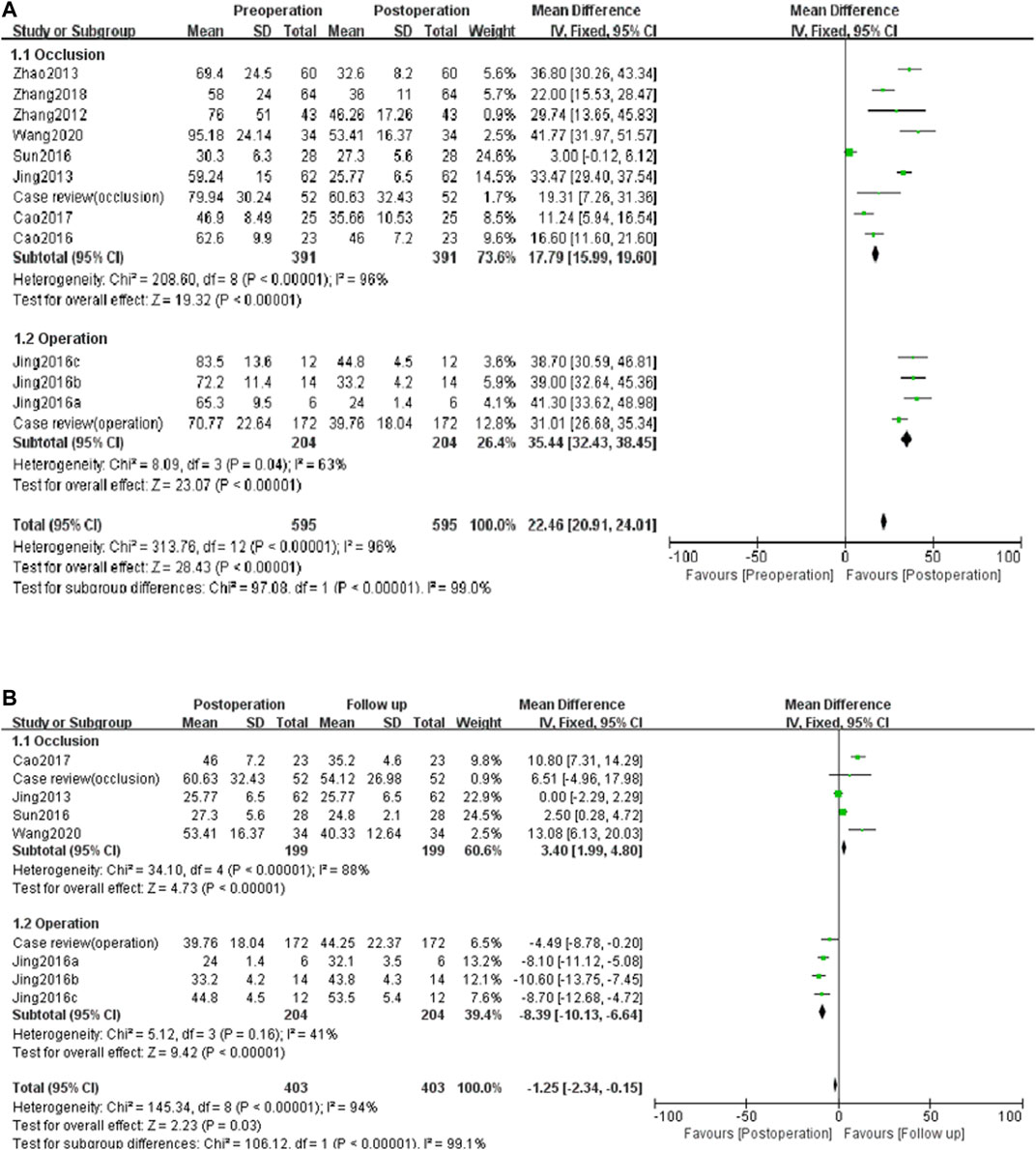
FIGURE 4. Meta-analysis to compare the therapeutic effects (A) and prognostic effects (B) of different operation.
Drug Factors
In order to study the appropriate dose, we selected seven literature through criterion 2 (Table 4) (Mohamed and Ismail, 2012; Steinhorn et al., 2016; Omar et al., 2016; Hernando and Amed, 2006; Sinan et al., 2011; Robyn et al., 2011; Carmine et al., 2017). According to the literature, we listed the corresponding body surface area with different body weights and the calculated dose of two drugs based on the body surface area (Li, 2010). As shown in Figure 5, the actual doses of bosentan and sildenafil were insufficient when compared with the dosage in the literature and surface area calculated. The dosage in consistent with the literature and the dosage in inconsistent with the literature were divided into two groups. It was found that the literature group still had a statistically significant reduction in PAH after 30 to 60 days of follow-up (p < 0.05). On the other hand, the group that did not follow the literature dosage showed a sustained increase in PAH after 30 days of follow-up.
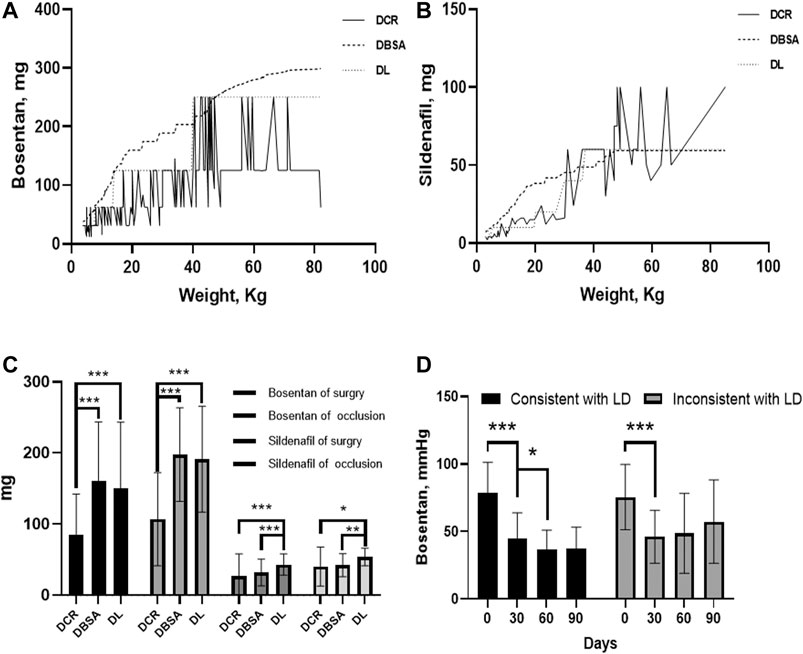
FIGURE 5. The comparision of the therapeutic and prognostic effects of drug factors. Three doses were including dose based on body surface area (DBSA), dose based on literature (DL), and based on case review (DCR). (A) Curves of 3 doses of bosentan with body weight. (B) Curves of 3 doses of sildenafil with body weight. (C) Dose comparison of 3 doses of bosentan and sildenafil administered in different operations. (D) The variation of pulmonary artery pressure concerning the consistency or inconsistency of bosentan literature dosage. *p < 0.05; **p < 0.01; ***p < 0.001.
In order to study the postoperative treatment effect of these two drugs, two literature were screened out by criterion 3. Since no literature was found on postoperative combination therapy (sildenafil and bosentan), this study focused only on the effect of postoperative sildenafil monotherapy (Cheng et al., 2014; Yang, 2014). We found a statistically significant reduction in PAH in both the literature group of sildenafil and the case review group with combination therapy (p < 0.05). Bosentan reduced PAH only in the literature group, which was statistical difference in Figure 6 (p < 0.05).
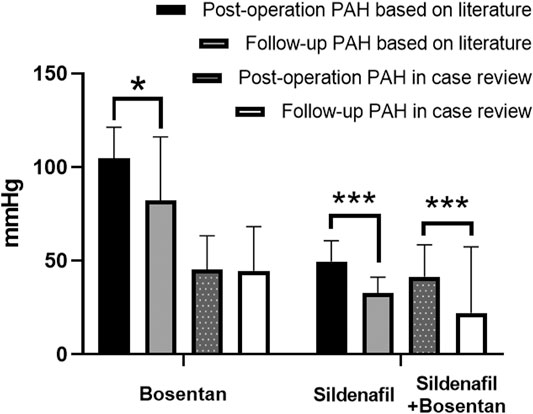
FIGURE 6. Comparison of postoperative pulmonary pressure reduction effects between bosentan and sildenafil in case review and literature. *p < 0.05; **p < 0.01; ***p < 0.001.
Age Factors
We divided 235 patients into five groups (48 infants, 46 toddlers, 47 children, 22 adolescents, and 72 adults) (Table 5). The number of minors hospitalized for PAH-CHD was twice as many as adults (163:72). The best treatment outcome (36.14 mmHg) and the lowest recurrence rate (0.15%) were observed mainly in infants.
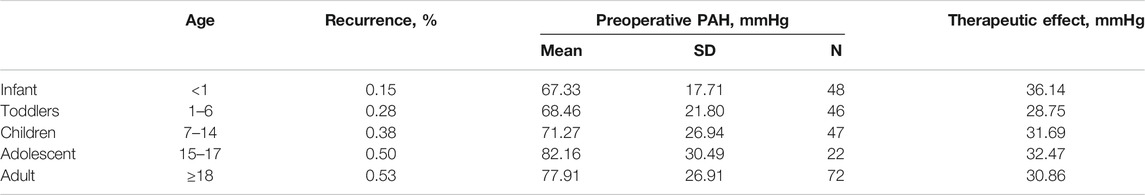
TABLE 5. Comparison of recurrence and therapeutic effect in 5 age groups (Infant, toddlers, children, adolescent, and adult).
Discussion
Orthogonal Projections to Latent Structures-Discriminant Analysis and S-Plot
OPLS-DA could be applicable to the analysis from routine clinical examination data, and S-plot could be helpful to screen out the indicators. We believe that simple methods such as OPLS-DA and S-plot are extremely important for screening prognostic indicators, in terms of saving doctors’ time to read the checklist and saving patients’ medical examination costs than PCA. Although four indicators (PAH, RBC, HGB, and CO2) were screened out in this paper, few studies have used RBC, HGB, and CO2 as prognostic indicators.
Cause Analysis of Elevated Pulmonary Arterial Hypertension
Reasons for the Operation
Combined with the literature and the case review in this study, surgery is inferior to closure. This phenomenon is widespread. The reason for this phenomenon might due to surgery requiring open chest and extracorporeal blood circulation. In contrast, the closure is less invasive and reduces the risk of infection. In this study, although the inclusion criterion for three times literature retrievals were consulted English and Chinese, almost most of the included literature was in Chinese (Suzuki et al., 2017; Akagi et al., 2018; Zwijnenburg et al., 2018). This might be because Chinese researchers might be more concerned with the follow-up of postoperative PAH, while researchers in other countries might pay more attention to the outcome of the operation itself. To improve patient survival, we believe that the postoperative follow-up of patients with PAH-CHD (detection of adverse factors and timely intervention) is very important. We hope that more researchers studying PAH will focus on the long-term postoperative follow-up to optimize the treatment and even provide a basis for treatment recommendations for patients with PAH-CHD.
Reasons for the Drug
The effect of combination therapy (bosentan and sildenafil) was more effective than that of bosentan. This result is consistent with the results of meta-analysis (Li et al., 2020). We propose that the main reason for poor postoperative control might be caused by insufficient dose and inappropriate medication. Most of the patients with PAH-CHD in our hospital were pediatric patients. Unfortunately, The drug dosage of these patients was not indicated on the packaging of bosentan and sildenafil. The commonly used method to determine the dosage of pediatric medicine is to convert it according to body weight, body surface area, or adult dosage. One study argued that doses should be calculated according to the 2/3 power of body weight (West, 2018). For example, Bosentan 60 kg adult dose is 250 mg/day, then the daily dose for a 10 kg toddler is 250/(60/10)2/3 ≈ 75 mg. However, no matter which method is used to calculate, the dosage of drugs in some patients was far from adequate. We also consider the efficacy of controlling postoperative pulmonary arterial pressure by standardizing patient dosing, which requires further study.
Reasons for the Age
The younger the patient’s age, the more effective the reduction in PAH. As the patient ages, the CHD might lead to cardiac remodeling and pulmonary artery function. Also, Also, damage to multiple organs may occur in the body due to chronic hypoxia, and a sudden increase in oxygen saturation does not reverse the damage. Therefore, we strongly recommend early operation (closure or surgery) for patients with CHD to improve the recovery outcome.
Conclusion
For the first time, OPLS-DA combined with S-plot was used to analyze clinical examination data, and four indicators (PAH, RBC, HGB, and CO2) reflecting patients’ prognosis were found. We suggest that occlision therapy would be preferred in patients with PAH-CHD. To prevent recurrence, the dose should be formally prescribed according to the instructions or literature for use. The effect of combination therapy (bosentan and sildenafil) is more effective than that of bosentan. The younger the patient is, the more effective the treatment is.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Yunnan Fuwai Cardiovascular Disease Hospital. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
XL: Data analysis, discussion, the meta-analysis methods and results, data extraction and quality control was performed. TL: Quality control.
Funding
This research was funded by Yunnan Clinical Medical Center of Fuwai Yunnan Cardiovascular Hospital, Project No. 2020YFKT-13, and Scientific Research Fund of Yunnan Provincial Education Department, Project No. 2021J0292.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We wish to thank the colleagues from Fuwai Yunnan Cardiovascular Hospital for their support. We also wish to thank the professors and schoolmates from Kunming Medical University.
References
Akagi, S., Kasahara, S., Sarashina, T., Nakamura, K., and Ito, H. (2018). Treat-and-repair Strategy is a Feasible Therapeutic Choice in Adult Patients with Severe Pulmonary Arterial Hypertension Associated with a Ventricular Septal Defect: Case Series. Eur. Heart J. Case Rep. 2 (2), yty033. doi:10.1093/ehjcr/yty033
Ashraf, A. H. E., and Midany, E. A. (2013). Etc. Perioperative Sildenafil Therapy for Pulmonary Hypertension in Infants Undergoing Congenital Cardiac Defect Closure[J]. Interact Cardiovasc. Thorac. Surg. 17 (6), 963–968. doi:10.1093/icvts/ivt353
Cao, L. M., Jin, B., Wang, F. M., et al. (2016). Clinical Analysis of Unclosed Ductus Arteriosus in Children with Severe Pulmonary Hypertension [J]. J. Nanjing Med. Univ. (Natural Science). 36 (12), 1534–1537. doi:10.7655/NYDXBNS20161236
Carmine, D., Sastry, B., and Zeenat, S. (2017). etc.Efficacy of 1, 5, and 20 Mg Oral Sildenafil in the Treatment of Adults with Pulmonary Arterial Hypertension: a Randomized, Double-Blind Study with Open-Label Extension[J]. BMC Pulm. Med. 17, 44–56. doi:10.1186/s12890-017-0374-x
Chao, J., and Zhao, L. L. (2017). Changes in Pulmonary Artery Pressure after Atrial Septal Defect Closure in Adults [J]. Chin. J. Contemp. Med. 24 (028), 36–38. doi:10.3969/j.issn.1674-4721.2017.28.012
Cheng, G. H., Zhang, Y. S., and Du, Y. J. (2014). etc.Targeted-drug Combined with Interventional Therapy in the Treatment of Congenital Heart Disease Complicated with Severe Pulmonary Hypertension [J]. J. Cardiovasc. Surg. 3 (01), 19–22. CNKI: XXGW. 0.2014-01-005
Gilbert, N., Luther, Y.-C., Miera, O., Nagdyman, N., Ewert, P., Berger, F., et al. (2005). Initial Experience with Bosentan (Tracleer) as Treatment for Pulmonary Arterial Hypertension (PAH) Due to Congenital Heart Disease in Infants and Young Children. ZS Kardiologie. 94 (9), 570–574. doi:10.1007/s00392-005-0266-6
Hernando, B., and Amed, etc. (2006). Oral Sildenafil in Infants with Persistent Pulmonary Hypertension of the Newborn: a Pilot Randomized Blinded study.[J]. Pediatrics. 117 (4), 1077–1083. doi:10.1542/peds.2005-0523
Jing, W. R. (2013). Interventional Therapy for Patients with Atrial Septal Defect and Moderate to Severe Pulmonary Hypertension: A Follow-Up Study [D]. Kunming: Kunming Medical University
Jing, X. Y., Yang, X. Y., Su, J. W., et al. (2016). Clinical Study on Diagnostic Treatment of Congenital Heart Disease Complicated with Severe Pulmonary Hypertension [J]. J. Cardiopulmonary Vasc. Dis. 35 (04), 293–296. doi:10.3969/j.issn.1007-5062.2016.04.011
Kelly, L. E., Ohlsson, A., and Shah, P. S. (2017). Sildenafil for Pulmonary Hypertension in Neonates. Cochrane Database Syst. Rev. 8 (8), CD005494. doi:10.1002/14651858.CD005494.pub4
Kiefer, T. L., and Bashore, T. M. (2011). Pulmonary Hypertension Related to Left-Sided Cardiac Pathology[J]. Pulm. Med. 2011 (2090-1836), 381787. doi:10.1155/2011/381787
Li, H. Z., Gong, Y. Y., and Xu, W. X. (2020). Meta-analysis of Bosentan Combined with Sildenafil in the Treatment of Pulmonary Hypertension [J]. J. Clin. Ther. 18 (01), 63–68. doi:10.3969/j.issn.1672-3384.2020.01.015
Li, X., and Li, T. (2020). Combined Methods (Formal Adjusted Indirect Comparison, Meta-Analysis and Principal Component Analysis) Comparisons of the Safety and Efficacy of Ambrisentan, Bosentan, and Sildenafil in the Patients with Pulmonary Arterial Hypertension. Front. Pharmacol. 11, 400. doi:10.3389/fphar.2020.00400
Li, Z. F. (2010). Practical Pediatric Drug Dose Survey Manual [M]. Beijing: China Medical Science and Technology Press, 4–5.
Mclaughlin, V. V., Archer, S. L., Badesch, D. B., Barst, R. J., Farber, H. W., Lindner, J. R., et al. (2009). ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension. J. Am. Coll. Cardiol. 53 (17), 1573–1619. doi:10.1016/j.jacc.2009.01.004
Melby, S. J., Moon, M. R., Lindman, B. R., Bailey, M. S., Hill, L. L., and Damiano, R. J. (2011). Impact of Pulmonary Hypertension on Outcomes after Aortic Valve Replacement for Aortic Valve Stenosis. J. Thorac. Cardiovasc. Surg. 141 (6), 1424–1430. doi:10.1016/j.jtcvs.2011.02.028
Mohamed, W. A., and Ismail, M. (2012). A Randomized, Double-Blind, Placebo-Controlled, Prospective Study of Bosentan for the Treatment of Persistent Pulmonary Hypertension of the Newborn. J. Perinatol. 32 (8), 608–613. doi:10.1038/jp.2011.157
More, K., Athalye-Jape, G. K., Rao, S. C., and Patole, S. K. (2016). Endothelin Receptor Antagonists for Persistent Pulmonary Hypertension in Term and Late Preterm Infants. Cochrane Database Syst. Rev. (8), CD010531. doi:10.1002/14651858.CD010531.pub2
Nazzareno, G., Humber, M., and Ronald, J. (2016). Etc. 2015 ESC/ERS Guidelines Fro the Diagnosis and Treatment of Pulmonary Hypertension[J]. Eur. Heart J. 37, 69–119. doi:10.1183/13993003.01032-2015
Omar, S. A., Salama, H., and Hail, M. A. (2016). Etc. Effect of Early Adjunctive Use of Oral Sildenafil and Inhaled Nitric Oxide on the Outcome of Pulmonary Hypertension in Newborn Infants. A Feasibility Study[J]. J. Neonatal-Perinatal Med. 9 (3) ,251–259. doi:10.3233/NPM-16161
Robyn, J., Dunbar, I., and Guillermo, G. (2011). etc.A Randomized, Double-Blind, Placebo-Controlled, Dose-Ranging Study of Oral Sildenafil Citrate in Treatment-Naive Children with Pulmonary Arterial Hypertension[J]. Pediatr. Cardiol. 7, 324–334. doi:10.1161/CIRCULATIONAHA.110.016667
Sinan, U., Soner, K., and Ali, B. (2011). Etc. A Comparison of Magnesium Sulphate and Sildenafil in the Treatment of the Newborns with Persistent Pulmonary Hypertension: A Randomized Controlled Trial[J]. J. Trop. Pediatr. 57 (4), 245. doi:10.1093/tropej/fmq091
Steinhorn, R. H., Fineman, J., Kusic-Pajic, A., Cornelisse, P., Gehin, M., Nowbakht, P., et al. (2016). Bosentan as Adjunctive Therapy for Persistent Pulmonary Hypertension of the Newborn: Results of the Randomized Multicenter Placebo-Controlled Exploratory Trial. J. Pediatr. 177, 90–96.e3. doi:10.1016/j.jpeds.2016.06.078
Sun, W. F., Zhu, M. X., and Cui, T. (2016). A Follow-Up Study of Left Heart Function after Patent Ductus Arteriosus Closure by Transthoracic Echocardiography [J]. Chin. J. Interv. Cardiol. 24 (02), 74–78. doi:10.3969/j.issn.1004-8812.2016.02.003
Suzuki, H., Hanawa, H., Torigoe, T., and Sato, S. (2017). Improvement of Pulmonary Arterial Hypertension Following Medication and Shunt Closure in a BMPR2 Mutation Carrier with Atrial Septal Defect. J. Cardiol. Cases. 16 (1), 11–13. doi:10.1016/j.jccase.2017.03.005
Wang, Z. Y., Jin, M., and Wang, X. F. (2020). Interventional Treatment and Follow-Up Study of Adults with Unclosed Ductus Arteriosus and Severe Pulmonary Hypertension [J]. J. Cardiopulmonary Vasc. Dis. 39 (01), 27–35. doi:10.3969/j.issn.1007-5062.2020.01.005
West, G. (2018). Scale: The Universal Laws of Growth, Innovation, Sustainability, and the Pace of Life in Organisms,cities, Economies, and companies[M]. New York: Penguin Books
Xi, S.-B., Wang, S.-S., Qian, M.-Y., Xie, Y.-M., Li, J.-J., and Zhang, Z.-W. (2019). Predictors of Operability in Children with Severe Pulmonary Hypertension Associated with Congenital Heart Disease. Chin. Med. J. 132 (7), 811–818. doi:10.1097/CM9.0000000000000145
Yang, S. Q. (2014). Clinical Observation of Sildenafil in Treatment of Pulmonary Hypertension after Surgery for Congenital Heart Disease [J]. J. Clin. Med. 34 (03), 43–45. CNKI:SUN:EBED.0.2014-03-029
Zhang, C. H., Wang, J. P., and Tian, Y. (2016). etc.Comparison of Pulmonary Arterial Pressure and Blood Pressure before and after Patent Ductus Arteriosus Interventional Closure [J]. Guizhou Med. Sci. 40 (01), 16–18. doi:10.3969/j.issn.1000-744X.2016.01.006
Zhang, K. C., Yuan, J., and Yu, B. (2012). Etc. Study on Changes of Pulmonary Artery Pressure after Interventional Treatment of Patent Ductus Arteriosus [J]. J. Cardiovasc. Rehabil. Med. 021 (004), 409–412. doi:10.3969/j.issn.1008-0074.2012.04.23
Zhao, Q., Li, X.-M., Liu, H.-N., Gonzalez, F. J., and Li, F. (2017). Metabolic Map of Osthole and its Effect on Lipids, Xenobiotica. 48, 285–299. doi:10.1080/00498254.2017.1306660
Zhao, X. B. (2013). Follow-up Study after Unclosed Ductus Arteriosus and Pulmonary Hypertension Closure [D]. Shandong: Shandong University. doi:10.7666/d.y2433747
Zwijnenburg, R. D., Baggen, V. J. M., Geenen, L. W., Voigt, K. R., Roos-Hesselink, J. W., and van den Bosch, A. E. (2018). The Prevalence of Pulmonary Arterial Hypertension before and after Atrial Septal Defect Closure at Adult Age: A Systematic Review. Am. Heart J. 201, 63–71. doi:10.1016/j.ahj.2018.03.020
Keywords: pulmonary artery hypertension, interventional closure, surgery, doses administered, sildenafil
Citation: Li X and Li T (2021) Inadequate Dosage May Lead to the Recurrence of Postoperative Pulmonary Hypertension in Patients With Congenital Heart Disease. Front. Pharmacol. 12:660405. doi: 10.3389/fphar.2021.660405
Received: 29 January 2021; Accepted: 21 April 2021;
Published: 29 April 2021.
Edited by:
Jean Paul Deslypere, Aesculape CRO, BelgiumReviewed by:
Rao Fu, Sichuan University, ChinaXiaonan Yang, Guangxi Medicinal Botanical Garden, China
Copyright © 2021 Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Te Li, YXQxMDI5QDE2My5jb20=
 Xinmei Li
Xinmei Li Te Li
Te Li