
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol., 17 May 2021
Sec. Neuropharmacology
Volume 12 - 2021 | https://doi.org/10.3389/fphar.2021.621856
Background: The efficacy and safety of fingolimod for relapsing-remitting multiple sclerosis (RRMS) had been well verified in several large randomized controlled trials (RCTs) during the past decade. However, there are fewer systematic comparisons of different doses of fingolimod and whether the dose of 0.5 mg/d is the optimal one still remains to be solved.
Objective: The objective of this systematic review was to evaluate the efficacy and safety of the four existing doses of fingolimod in the treatment of RRMS, especially the dose of 0.5 mg/d.
Methods: MEDLINE, EMBASE, Cochrane Library, and clinicaltrials.gov were searched for RCTs which were performed to evaluate different doses of fingolimod and the corresponding control (placebo or DMTs) up to October 2020. Review Manager 5.3 software was used to assess the data. The risk ratio (RR) and mean difference (MD) was analyzed and calculated with a random effect model.
Results: We pooled 7184 patients from 11 RCTs. Fingolimod 0.5 mg/d was superior to control group in all eight efficacy outcomes including annualized relapse rate (ARR) (MD −0.22, 95%CI −0.29 to −0.14, p < 0.00001) but surprisingly showed a higher risk of basal-cell carcinoma (RR 4.40, 95%CI 1.58 to 12.24, p = 0.004). Although 1.25 mg/d is more than twice the dose of 0.5 mg/d, the effect size was almost similar between them. Dose of 5 mg/d obtained an unsatisfactory efficacy while showing a greater risk of adverse events than other three doses (RR 1.17, 95%CI 1.05 to 1.30, p = 0.003). Additionally, fingolimod 0.25 mg/d not only showed a better performance in delaying the disease progress of magnetic resonance imaging (MRI), but also achieved a certain degree of patient treatment satisfaction.
Conclusion: At present, 0.5 mg/d remains to be the optimal dose of fingolimod for RRMS patients but trials of a lower dose are still of great clinical significance and should be paid more attentions.
Multiple sclerosis (MS) is a chronic inflammatory disease that can induce the immune system to produce autoimmune responses against the central nervous system (CNS), involved both white and grey matter region, thereby slowly losing the patient's physical activity (Owens, 2016). According to a recent report by the Multiple Sclerosis International Federation (The Multiple Sclerosis International Federation, 2020), the number of MS patients globally has increased to 2.8 million in 2020, which equates to 1 in 3000 people in the world living with MS. Relapsing-remitting multiple sclerosis (RRMS) is the most common phenotype of MS. The process of onset-remission-relapse can cause progressive disability in approximately 15–30% of MS patients, thus causing great damage to the quality of life (Thompson et al., 2018). There are several disease-modyfing treatments (DMTs) but still no cure for RRMS. Therefore, researches on the drugs that can effectively control the relapse and delay the progression of RRMS are still of great clinical significance.
Fingolimod (FTY720), as the first sphingosine 1-phosphate receptor (S1PR) modulator that routinely applied in the treatment of RRMS, has been proven to be effective in reducing the patients’ annualized relapse rate (ARR) and improving the magnetic resonance imaging (MRI) performance as earlier as 2006 (Kappos et al., 2006). The prevention of lymphocyte migration out of lymphoid tissues and the directly reduction of neurodegenerative process in the CNS might be the two underlying mechanisms that allow fingolimod to exert therapeutic effect in patients with RRMS (Chun and Hartung, 2010).
During the past decade, the efficacy and the safety of fingolimod had been well verified in several large randomized controlled trials (RCTs). At the same time, many systematic reviews based on these RCTs also made a good comparison between fingolimod and other DMTs or placebo on RRMS patients (Singer et al., 2011; Roskell et al., 2012; La Mantia et al., 2016; Yang et al., 2020). However, there are fewer systematic comparisons of different doses of fingolimod. Although the dose of 0.5 mg/d is currently approved worldwide for treatment of adult RRMS, whether a lower dose of fingolimod can maintain its effectiveness while reducing adverse events and costs still remain to be revealed. Doses of fingolimod lower than 0.5 mg per day were not evaluated in the fingolimod clinical development program. We thought that a further analysis of data may be of help for dose finding, particularly to explore whether different doses may be of help for clinicians to tailor treatment to RRMS persons in case of reduced tollerability/safety and/or not optimal efficacy. Thus, we pooled data from previous RCTs and conducted a meta-analysis to investigate the differences in efficacy and safety of different doses of fingolimod.
Before the project started, we drafted a research protocol following the Cochrane Collaboration format (Liberati et al., 2009).
We set the inclusion criteria as follows: a) study type: RCT; b) language restriction: only available in English; c) participants: patients 18–65 years of age diagnosed with RRMS; d) intervention: different doses of fingolimod and the corresponding control (placebo or DMTs); e) clinical outcomes: ARR, the number of patients free of relapse and the expanded disability status scale (EDSS); MRI outcomes: number of patients free of increased gadolinium-enhanced lesions in T1, number of patients with no new or newly enlarged lesions in T2 and the percentage brain volume change (PBVC); self-report outcomes: the beck depression inventory (BDI) score and the treatment satisfaction questionnaire for medication (TSQM) score; safety outcomes: adverse events (AEs) and serious adverse events (SAEs). Included RCTs were not requested to supply all the outcomes mentioned above.
We set the exclusion criteria as follows: a) study type: retrospective studies, cohort studies, case reviews and case reports; b) participants: patients with other forms of MS; c) control: active control (i.e. that a known, effective treatment as opposed to a placebo is compared to an experimental treatment).
Two independent investigators (XW and TX) systematically searched the Clinicaltrials.gov and three main databases including MEDLINE, EMBASE, and Cochrane Library to identify relevant studies published until October 2020. The following search strategy was used (fingolimod [Title/Abstract]) AND (multiple sclerosis [Title/Abstract]) for MEDLINE; ‘fingolimod’/exp AND ‘multiple sclerosis’/exp for EMBASE; “fingolimod” in Title Abstract Keyword AND “multiple sclerosis” in Title Abstract Keyword for Cochrane Library; “fingolimod | multiple sclerosis” for Clinicaltrials.gov. Additionally, the reference lists of RCTs, relevant systematic reviews and meta-analyses were also screened independently and manually to ensure a more comprehensive search.
According to the eligibility criteria listed above, two reviewers (XW and TX) independently evaluated all study records from the three electronic database and the reference lists of RCTs and relevant systematic reviews or meta-analyses. The duplicates and the research articles who only provided abstracts were excluded. A third reviewer (ZLW) who didn’t participate in the process of data collection would make the final decision of the disputed data when disagreements emerged among the two reviewers. After meticulous selection and evaluation, all data from the included RCTs were extracted as follows: basic information and outcome events included for each trail (Table 1), inclusion and exclusion criteria, study design, all efficacy and safety outcomes were showed in the online supplementary materials (Supplementary Table S1).
The risk of bias plot for individual studies was assessed with the Review Manager 5.3 software. The uniform criteria to assess the risk of bias for RCTs of the Cochrane Collaboration was applied, which included: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other potential biases. Each bias criterion was classified as “low”, “high”, or “unclear” after independently judged by the third reviewer.
Review Manager 5.3 software was used to assess the data. For the dichotomous outcomes, the risk ratio ([RR]; 95% confidence interval [CI]) was analyzed and calculated with a random effect model. Mean difference (MD) was used for the continuous outcomes such as ARR, EDSS score, PBVC, BDI score and TSQM score. Heterogeneity was estimated via the I2 statistic, which was as follows: I2 < 30% suggests “low heterogeneity”; I2 between 30 and 50% means “moderate heterogeneity”; I2 > 50% denotes “substantial heterogeneity”. Sensitivity analysis was used to explore the stability of the consolidated results. For all the analyses, two tailed tests were performed and a p value < 0.05 was considered to be statistical significant.
A total of 2508 titles and abstracts were returned from the search through MEDLINE, EMBASE, Cochrane Library and Clinicaltrials.gov. After quick screening the titles and abstracts, a total of 2257 articles were excluded due to duplication and irrelevance and 251 full text articles were assessed for eligibility. Among them, another 240 articles were excluded due to the limitation of publication types: 210 non-randomized clinical trials, 12 case reports, 11 meta-analyses and 7 reviews. The selection process was summarized in the flow diagram (Figure 1). All 11 elected RCTs (Kappos et al., 2006), (Kappos et al., 2010), (Cohen et al., 2010; Saida et al., 2012; Calabresi et al., 2014; Fox et al., 2014; ClinicalTrials.gov, 2014; ClinicalTrials.gov, 2015; Comi et al., 2017; Cree et al., 2018; Cree et al., 2020) enrolling 7184 patients were pooled for the analyses of efficacy and safety outcomes. The main characteristics of the included 11 studies were listed in Table 1.
The clinical outcomes included the ARR, the number of patients free of relapse and the EDSS score. Patients in fingolimod 0.5 mg/d and 1.25 mg/d group had significantly lower ARR and ΔEDSS (Δ means the changes from baseline to final) score than those in the control group (for the ARR: 0.5 mg/d: MD = −0.17 (−0.22 to −0.11), p < 0.00001; 1.25 mg/d: MD = −0.24 (−0.32 to −0.15), p < 0.00001; for the ΔEDSS: 0.5 mg/d: MD = −0.09 (−0.16 to −0.22), p = 0.01; 1.25 mg/d: MD = −0.14 (−0.21 to −0.06), p = 0.0003). Significant differences were also observed in the number of patients free of relapse between control group and three different doses of fingolimod group (0.5 mg/d: RR = 1.20 [1.09, 1.31], p = 0.0002; 1.25 mg/d: RR = 1.26 [1.14, 1.40], p < 0.0001; 5.0 mg/d: RR = 1.30 [1.13, 1.50], p = 0.0002). However, patients in fingolimod 0.25 mg/d group didn’t show significant differences in ARR and the number of patients free of relapse when compared with the patients in control group (p = 0.32 and 0.22, respectively). The detailed results of clinical outcomes analysis were showed in Table 2 and Supplementary Figures S1–S3.
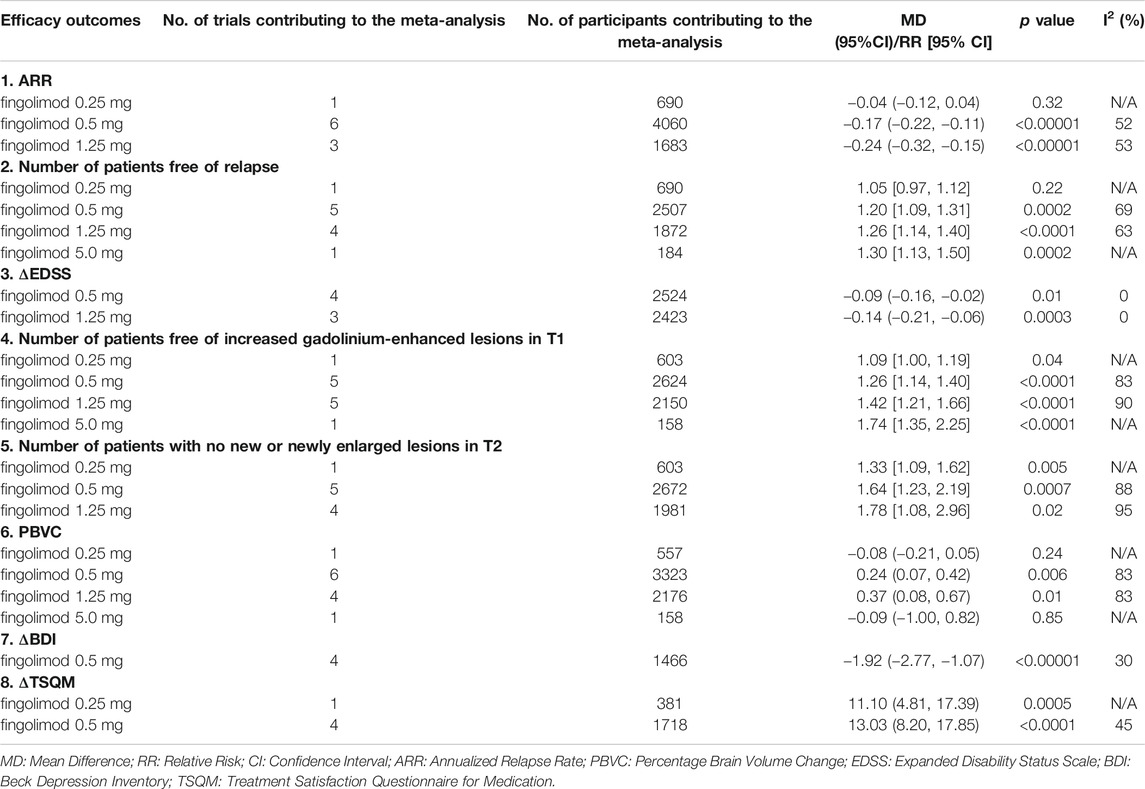
TABLE 2. Effects sizes from meta-analysis of efficacy outcomes; from all trials using random effects models.
The MRI outcomes included the number of patients free of increased gadolinium-enhanced lesions in T1, number of patients with no new or newly enlarged lesions in T2 and the PBVC. Compared with the control group, all fingolimod groups could both make more patients free of increased gadolinium-enhanced lesions in T1 (0.25 mg/d: RR = 1.09 [1.00, 1.19], p = 0.04; 0.5 mg/d: RR = 1.26 [1.14, 1.40], p < 0.0001; 1.25 mg/d: RR = 1.42 [1.21, 1.66], p < 0.0001; 5.0 mg/d: RR = 1.74 [1.35, 2.25], p = p < 0.0001), and the number of patients with no new or newly enlarged lesions in T2 was also significant smaller in those groups (0.25 mg/d: RR = 1.33 [1.09, 1.62], p = 0.005; 0.5 mg/d: RR = 1.64 [1.23, 2.19], p = 0.0007; 1.25 mg/d: RR = 1.78 [1.08, 2.96], p = 0.02). In addition, there was also a substantial significance in the PBVC of fingolimod 0.5 mg/d and 1.25 mg/d group when compared with the control group (0.5 mg/d: MD = 0.24 (0.07, 0.42), p = 0.006; 1.25 mg/d: MD = 0.37 (0.08, 0.67), p = 0.01). See Table 2 and Supplementary Figures S4–S6 to find the detailed results of MRI outcomes analysis.
BDI and TSQM are two patients self-evaluated scales that can reflect depression and treatment satisfaction, respectively (Arnau et al., 2001), (Atkinson et al., 2004). The results showed that, compared with control group, fingolimod 0.5 mg/d could significantly reduce the depression scores (MD = −1.92 (−2.77, −1.07), p < 0.00001) while improving patient treatment satisfaction (MD = 13.03 (8.20, 17.85), p < 0.0001). In the meanwhile, patients in fingolimod 0.25 mg/d group were also more willing to give a higher score in the TSQM scale (MD = 11.10 (4.81, 17.39), p = 0.0005). The detailed results of patients evaluated outcomes analysis were also showed in Table 2 and Supplementary Figures S7,S8.
The safety outcomes were assessed by adverse events and serious adverse events. We combined the data collected from the 11 trials and found that fingolimod 5.0 mg/d showed a significant high risk of the adverse events (RR = 1.17 [1.05, 1.30], p = 0.003, Table 3 and Supplementary Figure S9). In addition, for the serious adverse events, fingolimod 0.5 mg/d also showed a significant high risk compared with the control group (RR = 1.25 [1.01, 1.54], p = 0.04, Table 3 and Supplementary Figure S10). Thus, we further sub-analyzed the specific serious adverse event that at least two trials provided data in the fingolimod 0.5 mg/d group. The results showed that compared with placebo or DMTs group, the patients in fingolimod 0.5 mg/d group were more likely to have basal-cell carcinoma, which made major contribution to the high risk of serious adverse events (RR = 4.40 [1.58, 12.24], p = 0.004, Table 4 and Supplementary Figures S11–S14).
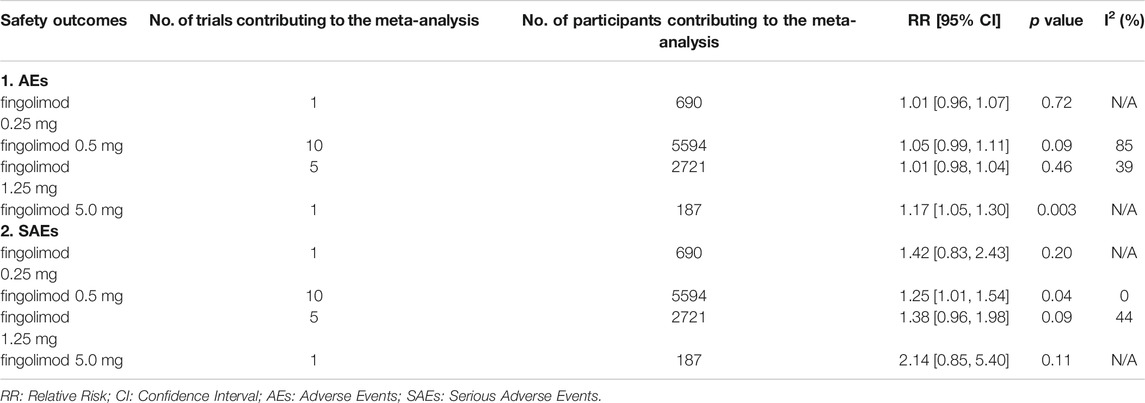
TABLE 3. Effects sizes from meta-analysis of safety outcomes; from all trials using random effects models.
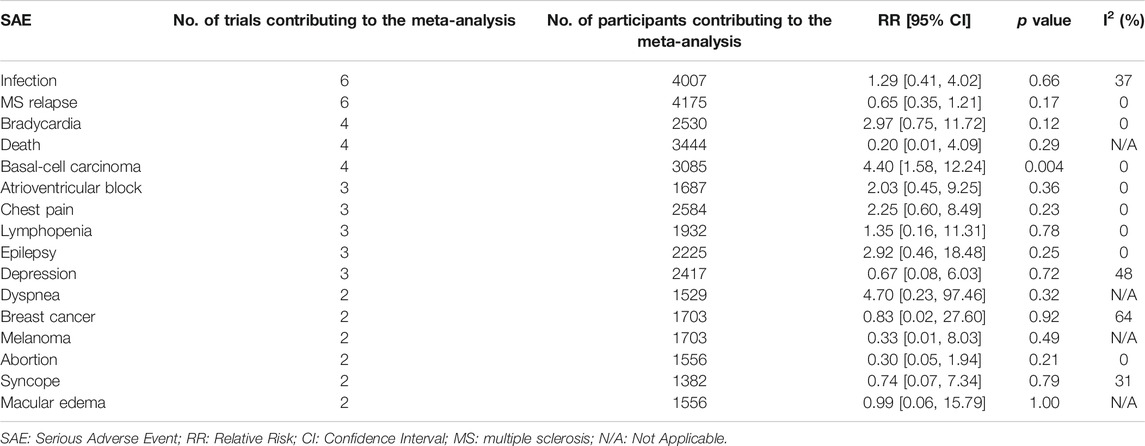
TABLE 4. Meta-analysis of SAEs between fingolimod 0.5 mg/d and placebo or DMTs groups; from all trials using random effects models, where at least two trials provided data that could be included.
Full details of the risk bias for all enrolled studies were showed in Figure 2. One clinical trials showed unclear risk of bias both in random sequence generation and allocation concealment. For the blinding of participants and personnel, the risk of bias was high in five studies. For the blinding of outcome assessment, the risk of bias was high in four trials. For the incomplete outcome data, the risk of bias was low in all eleven trials. For selective reporting, the risk of bias was unclear in four study. Apart from these items, unclear risk of bias was also observed in three RCTs.
Nowadays, oral fingolimod is widely used in the treatment of RRMS and has achieved good therapeutic effects. Several large clinical trials have shown that fingolimod with once-daily doses of 0.5, 1.25 and 5 mg could both significantly lower the ARR compared with the placebo group (Kappos et al., 2006), (Kappos et al., 2010). Moreover, in response to the recommendation of US Food and Drug Administration, study that evaluated fingolimod with once-daily dose of 0.25 mg has recently appeared (Cree et al., 2020). For a more comprehensive comparison in the efficacy of different doses of fingolimod, a total of eight outcomes were included in this meta-analysis and were divided into three major parts: clinical outcomes, MRI outcomes and self-report outcomes. We conducted this meta-analysis for the purpose of evaluating the efficacy and safety of the four existing doses. On the basis of our data pooled from the eleven published RCTs, we found fingolimod with once-daily dose of 0.5 mg was superior to placebo or DMTs in all efficacy terms that included in this study but showed a higher risk of serious adverse events. At the same time, although 1.25 mg is more than twice the dose of 0.5 mg, the effect size in the reduction of clinical relapse and the amelioration of MRI performance was almost similar between them. As the largest dosage, fingolimod 5 mg/d certainly showed the highest MD in the number of patients free of clinical relapse and increased gadolinium-enhanced lesions in T1 compared with placebo or DMTs. Nevertheless, this dose also means a greater financial burden for the patients or public health system, and a higher risk of adverse events than other doses according to our analysis. In comparison with placebo or DMTs, fingolimod 0.25 mg/d not only showed a better performance in MRI parameters, but also achieved a certain degree of patient treatment satisfaction. Therefore, it is necessary to conduct more studies in the future to evaluate the efficacy and safety of fingolimod 0.25 mg/d.
As the most commonly reported clinical outcome in RRMS trials, ARR was widely selected in systematic reviews (Rae-Grant et al., 2018), (Fogarty et al., 2016). Combined with the number of patients free of relapse, investigators could intuitively evaluate the relapse level of patients. In this study, patients treated with fingolimod 0.5 mg/d and 1.25 mg/d showed a significant lower relapse level compared with placebo or DMTs. In addition, the inclusion criteria of almost all RRMS trials both included the EDSS scores, which ranged from 0 to 10 and was positively related to the degree of disability (Kurtzke, 1983). An increase greater or equal to one point in the EDSS score after three months was considered as disability progression if the most inclusive definition was acceptable (Lorscheider et al., 2016). The MD in ΔEDSS of fingolimod 0.5 mg/d and 1.25 mg/d were both negative in this study, which indicated that fingolimod 0.5 and 1.25 mg/d could effectively prevent or retard the progression of disability when compared with placebo or DMTs.
For MRI outcomes, we included number of patients free of increased gadolinium-enhanced lesions in T1, number of patients with no new or newly enlarged lesions in T2 and the PBVC. Gadolinium-enhanced T1 lesions and new or newly enlarged T2 lesions in MRI are considered as a measure of the focal inflammatory activity (Simon, 2014). Because of the higher sensitivity than clinical assessment in detecting MS disease activity, they sometimes can surrogate ARR and serve as the primary outcomes in RRMS trials (Filippi et al., 2014). All doses even 0.25 mg/d of fingolimod both performed better than placebo or DMTs, as fingolimod induced more patients free of MS disease activity in T1 and T2. Brain volume change is another recognized MRI marker that can reflect both focal and diffuse pathology in MS(De Stefano et al., 2014), (Filippi et al., 2019). A post hoc analysis of FREEDOMS trail (Kappos et al., 2010) found that brain volume loss was associated to the disability progression and could further worsen disability over a longer period of time (Jeffery et al., 2016). Among the four doses of fingolimod, only 0.5 mg/d and 1.25 mg/d had a significant decreased brain volume loss than the placebo or DMTs group. Thereby, although the dose of 0.25 mg/d might be able to maintain the stability of the disease for a certain duration, its effectiveness in long-term brain volume loss and accompanying disability progression was still worse than 0.5 and 1.25 mg/d.
As for the patients evaluated outcomes, TSQM score and BDI score were selected for analysis. TSQM score was both evaluated as primary study subject in the three included EPOC trails that were separately conducted in USA, Russian and Italy (Fox et al., 2014; ClinicalTrials.gov, 2014; ClinicalTrials.gov, 2015). A higher TSQM score indicated a greater treatment satisfaction. Patients treated with fingolimod 0.25 and 0.5 mg/d showed a significant greater extent of improvement in ΔTSQM than the patients treated with placebo or DMTs. The better effectiveness as we mentioned earlier, the fewer side effects and a more convenient way of administration may be the reasons why fingolimod was superior to other injectable DMTs in terms of patient satisfaction. Depression is common psychiatric comorbidities in patients with MS and MS-related immune-inflammatory, and brain structural alterations might play a role of its pathogenesis (Solaro et al., 2018), (Rossi et al., 2017). The incidence of depression would increase shortly after or during the disease exacerbations in RRMS(Moore et al., 2012). The current study used the BDI score to investigate the efficacy of fingolimod 0.5 mg/d in MS-related depression compared with placebo or DMTs. With a MD of −1.92, fingolimod 0.5 mg/d demonstrated a numerically larger scores reduction from baseline to the final.
Regarding safety, fingolimod 0.5 and 5 mg/d were found a significant higher risk of SAEs and AEs when compared with placebo or DMTs, respectively. After sub-analyzing the specific SAE in fingolimod 0.5 mg/d group, we found that the risk of basal-cell carcinoma was much higher than other SAEs. As with many immunodulatory agent, the effect of fingolimod on the immune system might confer a greater risk of malignancy including the basal-cell carcinoma (Cohen et al., 2019). Furthermore, the current findings were also consistent with a long-term extension study that the basal-cell carcinoma was the most common SAEs, in which all patients were treated with oral fingolimod 0.5 mg once daily (Cohen et al., 2019). Despite this, 0.5 mg/d still seems to be the best dose choice of fingolimod for RRMS patients at present.
Several limitations of the present meta-analysis should not be ignored. Firstly, the analysis of the dose of 0.25 and 5 mg/d were performed based on limited data. Only one published RCT with 370 and 92 patients were pooled to test the efficacy and safety of 0.25 and 5 mg/d, respectively. Secondly, this meta-analysis was not registered prior to the data collection. Thirdly, high level of heterogeneity was found in several data. As we showed in Table 1 and Supplementary Table S1, the variation in the study designs, the inclusion and exclusion criteria, the baseline characteristics of mean age and the region of study, and especially the duration of the trials might make the explanation. For the data with heterogeneity greater than 50%, sensitivity analysis was performed. After we excluded the trial by Cohen et al.12, the heterogeneity of the ARR in the 1.25 mg/d group changed from 64 to 53% (Supplementary Figure S15). Other sensitivity analyses demonstrated that all the statistics were robust (Supplementary Figures S16,S17).
In conclusion, the present study indicated that combined safety and the efficacy comprehensively obtained from clinical outcomes, MRI outcomes and patients evaluated outcomes, 0.5 mg/d remains to be the optimal dose of fingolimod for RRMS patients so far. Besides, trials of the dose lower than 0.5 mg/d are still of great clinical significance and should be paid more attentions.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
ZhW and WZ was the principal investigator. XW and TX designed the study and developed the analysis plan. XW and TX analyzed the data and performed meta-analysis. XW and TX contributed in writing of the article. ZiW, ZC, and XZ revised the manuscript and polish the language. All authors read and approved the final submitted paper.
This work was supported by the Suzhou Health Talents Training Project (GSWS2019002).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.621856/full#supplementary-material
Arnau, R. C., Meagher, M. W., Norris, M. P., and Bramson, R. (2001). Psychometric Evaluation of the Beck Depression Inventory-II with Primary Care Medical Patients. Health Psychol. 20 (2), 112–119. doi:10.1037/0278-6133.20.2.112
Atkinson, M. J., Sinha, A., Hass, S. L., Colman, S. S., Kumar, R. N., Brod, M., et al. (2004). Validation of a General Measure of Treatment Satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), Using a National Panel Study of Chronic Disease. Health Qual. Life Outcomes 2, 12. doi:10.1186/1477-7525-2-12
Calabresi, P. A., Radue, E.-W., Goodin, D., Jeffery, D., Rammohan, K. W., Reder, A. T., et al. (2014). Safety and Efficacy of Fingolimod in Patients with Relapsing-Remitting Multiple Sclerosis (FREEDOMS II): A Double-Blind, Randomised, Placebo-Controlled, Phase 3 Trial. Lancet Neurol. 13 (6), 545–556. doi:10.1016/s1474-4422(14)70049-3
Chun, J., and Hartung, H.-P. (2010). Mechanism of Action of Oral Fingolimod (FTY720) in Multiple Sclerosis. Clin. neuropharmacol. 33 (2), 91–101. doi:10.1097/wnf.0b013e3181cbf825
ClinicalTrials.gov (2014). A 6 month, Randomized, Active Comparator, Open-Label, Multi-Center Study to Evaluate Patient Outcomes, Safety and Tolerability of (Fingolimod) 0.5 Mg/day in Patients with Relapsing Remitting Multiple Sclerosis Who Are Candidates for Multiple Sclerosis (MS) Therapy Change from Previous Disease Modifying Therapy (DMT). ClinicalTrials website. Available at: https://clinicaltrials.gov/ct2/show/NCT01534182?term_NCT01534182&draw_2&rank_1 (Accessed September 10, 2020).
ClinicalTrials.gov (2015). A 6-month, Randomized, Active Comparator, Open-Label, Multi-Center Study to Evaluate Patient Outcomes, Safety and Tolerability of Fingolimod (FTY720) 0.5 Mg/day in Patients with Relapsing Remitting Multiple Sclerosis Who Are Candidates for Ms Therapy Change from Previous Disease Modifying therapy (EPOC). ClinicalTrials website. Available at: https://clinicaltrials.gov/ct2/show/NCT01317004?term_NCT01317004&draw_2&rank_1 (Accessed September 10, 2020).
Cohen, J. A., Barkhof, F., Comi, G., Hartung, H.-P., Khatri, B. O., Montalban, X., et al. (2010). Oral Fingolimod or Intramuscular Interferon for Relapsing Multiple Sclerosis. N. Engl. J. Med. 362 (5), 402–415. doi:10.1056/nejmoa0907839
Cohen, J. A., Tenenbaum, N., Bhatt, A., Zhang, Y., and Kappos, L. (2019). Extended Treatment with Fingolimod for Relapsing Multiple Sclerosis: the 14-year LONGTERMS Study Results. Ther. Adv. Neurol. Disord. 12, 1756286419878324. doi:10.1177/1756286419878324
Comi, G., Patti, F., Patti, F., Rocca, M. A., Mattioli, F. C., Amato, M. P., et al. (2017). Efficacy of Fingolimod and Interferon Beta-1b on Cognitive, MRI, and Clinical Outcomes in Relapsing-Remitting Multiple Sclerosis: an 18-month, Open-Label, Rater-Blinded, Randomised, Multicentre Study (The GOLDEN Study). J. Neurol. 264 (12), 2436–2449. doi:10.1007/s00415-017-8642-5
Cree, B. A. C., Arnold, D. L., Cascione, M., Fox, E. J., Williams, I. M., Meng, X., et al. (2018). Phase IV Study of Retention on Fingolimod versus Injectable Multiple Sclerosis Therapies: A Randomized Clinical Trial. Ther. Adv. Neurol. Disord. 11, 1756286418774338. doi:10.1177/1756286418774338
Cree, B. A. C., Goldman, M. D., Corboy, J. R., Singer, B. A., Fox, E. J., Arnold, D. L., et al. (2020). Efficacy and Safety of 2 Fingolimod Doses vs Glatiramer Acetate for the Treatment of Patients with Relapsing-Remitting Multiple Sclerosis: A Randomized Clinical Trial. JAMA Neurol. 78, 1-13. doi:10.1001/jamaneurol.2020.2950
De Stefano, N., Airas, L., Grigoriadis, N., Mattle, H. P., O’Riordan, J., Oreja-Guevara, C., et al. (2014). Clinical Relevance of Brain Volume Measures in Multiple Sclerosis. CNS drugs. 28 (2), 147–156. doi:10.1007/s40263-014-0140-z
Filippi, M., Brück, W., Chard, D., Fazekas, F., Geurts, J. J. G., Enzinger, C., et al. (2019). Association between Pathological and MRI Findings in Multiple Sclerosis. Lancet Neurol. 18 (2), 198–210. doi:10.1016/s1474-4422(18)30451-4
Filippi, M., Preziosa, P., and Rocca, M. A. (2014). Magnetic Resonance Outcome Measures in Multiple Sclerosis Trials. Curr. Opin. Neurol. 27 (3), 290–299. doi:10.1097/wco.0000000000000095
Fogarty, E., Schmitz, S., Tubridy, N., Walsh, C., and Barry, M. (2016). Comparative Efficacy of Disease-Modifying Therapies for Patients with Relapsing Remitting Multiple Sclerosis: Systematic Review and Network Meta-Analysis. Mult. Scler. Relat. Disord. 9, 23–30. doi:10.1016/j.msard.2016.06.001
Fox, E., Edwards, K., Burch, G., Wynn, D. R., LaGanke, C., Crayton, H., et al. (2014). Outcomes of Switching Directly to Oral Fingolimod from Injectable Therapies: Results of the Randomized, Open-Label, Multicenter, Evaluate Patient OutComes (EPOC) Study in Relapsing Multiple Sclerosis. Mult. Scler. Relat. Disord. 3 (5), 607–619. doi:10.1016/j.msard.2014.06.005
Jeffery, D. R., Di Cantogno, E. V., Ritter, S., Meier, D. P., Radue, E.-W., and Camu, W. (2016). The Relationship between the Rate of Brain Volume Loss during First 24 Months and Disability Progression over 24 and 48 Months in Relapsing MS. J. Neurol. 263 (2), 299–305. doi:10.1007/s00415-015-7959-1
Kappos, L., Antel, J., Comi, G., Montalban, X., O'Connor, P., Polman, C. H., et al. (2006). Oral Fingolimod (FTY720) for Relapsing Multiple Sclerosis. N. Engl. J. Med. 355 (11), 1124–1140. doi:10.1056/nejmoa052643
Kappos, L., Radue, E.-W., O'Connor, P., Polman, C., Hohlfeld, R., Calabresi, P., et al. (2010). A Placebo-Controlled Trial of Oral Fingolimod in Relapsing Multiple Sclerosis. N. Engl. J. Med. 362 (5), 387–401. doi:10.1056/nejmoa0909494
Kurtzke, J. F. (1983). Rating Neurologic Impairment in Multiple Sclerosis: an Expanded Disability Status Scale (EDSS). Neurology. 33 (11), 1444. doi:10.1212/wnl.33.11.1444
La Mantia, L., Tramacere, I., Firwana, B., Pacchetti, I., Palumbo, R., and Filippini, G. (2016). Fingolimod for Relapsing-Remitting Multiple Sclerosis. Cochrane Database Syst. Rev. 4, Cd009371. doi:10.1002/14651858.CD009371.pub2
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gotzsche, P. C., Ioannidis, J. P. A., et al. (2009). The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies that Evaluate Healthcare Interventions: Explanation and Elaboration. J. Clin. Epidemiol. 339, b2700. doi:10.1136/bmj.b2700
Lorscheider, J., Buzzard, K., Jokubaitis, V., Spelman, T., Havrdova, E., Horakova, D., et al. (2016). Defining Secondary Progressive Multiple Sclerosis. Brain 139 (Pt 9), 2395–2405. doi:10.1093/brain/aww173
Moore, P., Hirst, C., Harding, K. E., Clarkson, H., Pickersgill, T. P., and Robertson, N. P. (2012). Multiple Sclerosis Relapses and Depression. J. Psychosomatic Res. 73 (4), 272–276. doi:10.1016/j.jpsychores.2012.08.004
Rae-Grant, A., Day, G. S., Marrie, R. A., Rabinstein, A., Cree, B. A. C., Gronseth, G. S., et al. (2018). Comprehensive Systematic Review Summary: Disease-Modifying Therapies for Adults with Multiple Sclerosis. Neurology. 90 (17), 789–800. doi:10.1212/wnl.0000000000005345
Roskell, N. S., Zimovetz, E. A., Rycroft, C. E., Eckert, B. J., and Tyas, D. A. (2012). Annualized Relapse Rate of First-Line Treatments for Multiple Sclerosis: a Meta-Analysis, Including Indirect Comparisons versus Fingolimod. Curr. Med. Res. Opin. 28 (5), 767–780. doi:10.1185/03007995.2012.681637
Rossi, S., Studer, V., Motta, C., Polidoro, S., Perugini, J., Macchiarulo, G., et al. (2017). Neuroinflammation Drives Anxiety and Depression in Relapsing-Remitting Multiple Sclerosis. Neurology. 89 (13), 1338–1347. doi:10.1212/wnl.0000000000004411
Saida, T., Kikuchi, S., Itoyama, Y., Hao, Q., Kurosawa, T., Nagato, K., et al. (2012). A Randomized, Controlled Trial of Fingolimod (FTY720) in Japanese Patients with Multiple Sclerosis. Mult. Scler. 18 (9), 1269–1277. doi:10.1177/1352458511435984
Simon, J. H. (2014). MRI Outcomes in the Diagnosis and Disease Course of Multiple Sclerosis. Handbook Clin. Neurol. 122, 405–425. doi:10.1016/b978-0-444-52001-2.00017-0
Singer, B., Ross, A. P., and Tobias, K. (2011). Oral Fingolimod for the Treatment of Patients with Relapsing Forms of Multiple Sclerosis. Int. J. Clin. Pract. 65 (8), 887–895. doi:10.1111/j.1742-1241.2011.02721.x
Solaro, C., Gamberini, G., and Masuccio, F. G. (2018). Depression in Multiple Sclerosis: Epidemiology, Aetiology, Diagnosis and Treatment. CNS drugs. 32 (2), 117–133. doi:10.1007/s40263-018-0489-5
The Multiple Sclerosis International Federation (2020). Atlas of MS, 3rd Edn. Available at: https://www.atlasofms.org
Thompson, A. J., Baranzini, S. E., Geurts, J., Hemmer, B., and Ciccarelli, O. (2018). Multiple Sclerosis. Lancet. 391 (10130), 1622–1636. doi:10.1016/s0140-6736(18)30481-1
Keywords: fingolimod, multiple sclerosis, relapsing-remitting, different doses, systematic review
Citation: Wu X, Xue T, Wang Z, Chen Z, Zhang X, Zhang W and Wang Z (2021) Different Doses of Fingolimod in Relapsing-Remitting Multiple Sclerosis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 12:621856. doi: 10.3389/fphar.2021.621856
Received: 27 October 2020; Accepted: 26 April 2021;
Published: 17 May 2021.
Edited by:
Heike Wulff, University of California, United StatesCopyright © 2021 Wu, Xue, Wang, Chen, Zhang, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhong Wang, d2FuZ3pob25nNzYxQDE2My5jb20=; Wei Zhang, bXJ6aGFuZ3dlaXNoQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.