- 1Clinical Medical College, Yangzhou University, Yangzhou, China
- 2Department of Biostatistics and Epidemiology, University of Oklahoma Health Science Center, Oklahoma City, OK, United States
Background: Hematoma of the colon is a rare hemorrhagic complication that affects patients accepting low molecular weight heparin (LMWH) therapy. Only scarce cases of colon hematoma have been reported, usually in children or patients accepting warfarin therapy.
Case summary: A 76-year-old Chinese man was diagnosed with atrial fibrillation and heart failure, with cardiac function NYHA grade III on March 21, 2018. This patient was given LMWH for anticoagulation therapy and developed a colon hematoma on the third day of hospitalization. Abdominal computed tomography (CT) showed the thickening of areas of the colon up to 110 mm × 78 mm in thickness, which was a symptom of colon hematoma. The patient underwent conservative treatment successfully. On March 27, the patient’s abdominal pain was alleviated, and a CT scan showed that the intestinal hematoma was absorbed.
Conclusions: The most frequent minor bleeding events of LMWH anticoagulation are hemorrhage and subcutaneous hematoma. This case demonstrated that bowel hematoma despite its low incidence should be considered as an ADR of LMWH therapy, especially among patients who present with gastrointestinal symptoms.
Introduction
Low molecular weight heparin (LMWH) has become the preferred agent for the prophylaxis and treatment of thrombosis disease in patients as it has been shown to be safe and effective. It is also used as a bridging treatment of atrial fibrillation (AF) and then was switched to treatment with oral anticoagulants (Xia et al., 2018). As with any other anticoagulants, the main complication of LMWH therapy is bleeding. Most spontaneous gastrointestinal tract hematomas are caused by blunt abdominal trauma, which can also be secondary to anticoagulation therapy. Other risk factors for spontaneous gastrointestinal tract hematoma involve an endoscopic examination, coagulation disorder, and hemorrhagic disease (Zammit et al., 2013). Cases of spontaneous bowel hematoma associated with subcutaneous LMWH injection have been reported, while colon hematoma cases are very rare, usually in children or patients undergoing warfarin therapy (Chung, 2016; Choi et al., 2018). We herein present a novel case of spontaneous intramural hematoma of the colon associated with subcutaneous LMWH therapy.
Case Presentation
Chief Complaints
A 76-year-old Chinese man complained of acutely worsening abdominal pain after treatment with 4,000 anti-Xa U of LMWH, q12h (low molecular weight heparin calcium injection, 0.4 ml/4000IU) as an anticoagulant for 3 days.
History of Present Illness
The patient was admitted to our hospital because of palpitation and shortness of breath for three days, and diagnosed with atrial fibrillation and heart failure, with cardiac function NYHA grade III at Northern Jiangsu People’s Hospital on March 21, 2018. He had a CHA2DS2-VASc score of 4, which indicated a high risk of stroke. His body mass index was 21.66 kg/m2, and renal function was normal. Therefore, he was given furosemide and spironolactone for diuretic therapy, valsartan capsules for antihypertensive treatment, and LMWH for anticoagulation therapy.
History of Past Illness
The patient had a prior history of hypertension well controlled by treatment with angiotensin-converting enzyme inhibitors.
Personal and Family History
The patient had no specific underlying disease. He had no family history of other significant diseases.
Physical Examination Upon Admission
Physical examination showed abdomen tenderness and no signs of peritoneal irritation.
Laboratory Examinations
On March 21, laboratory results showed that N-terminal pro–B-type natriuretic peptide was 1590 pg/ml, international normalized ratio was 1.14, activated partial thromboplastin time (APTT) was 38.20 s, fibrinogen was 1.67 g/L, hemoglobin was 113 g/L, red blood cell count was 3.34 × 1012/L, creatinine was 83 μmol/L, alanine transferase was (ALT) 39.0 U/L, aspartate aminotransferase (AST) was 36.0 U/L, gamma-glutamyltransferase (GGT) was 115.0 U/L, and platelet cell count was 183 × 109/L. After anticoagulation therapy for 3 days, an emergency laboratory test showed that the red blood cell count was 2.56 × 1012/L, and hemoglobin and platelet counts decreased to 82 g/L and 102 × 109/L, respectively. Furthermore, the coagulation function test demonstrated a prolonged APTT of 49.50 s. There was no bleeding per rectum, and his fecal occult blood test was negative. Considering the patient’s symptoms of abdominal pain and the rapid drop in hemoglobin and red blood cell count, there was clinical suspicion for retroperitoneal or gastrointestinal hemorrhage.
Imaging Examinations
Abdominal computed tomography (CT) showed the thickening areas of the colon up to 110 mm × 78 mm in thickness, which was a symptom of hematoma of the colon (Figures 1A,B).
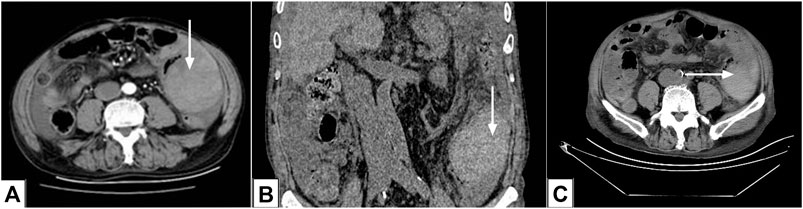
FIGURE1. Abdominal computed tomography images. (A, B) Contrast-enhanced computed tomography (CT) images showing a hematoma of the colon (arrows) on March 23, 2018; C: CT image revealed that the colon hematoma had been absorbed (arrow) on March 27, 2018.
Final Diagnosis
Hematoma of the colon took place after a subcutaneous LMWH injection. The patient had no medical history of hemorrhagic diseases, trauma, and any other anticoagulation therapy; we suspected that it was an adverse drug reaction (ADR) of LMWH. The assessment of ADR was evaluated via the Naranjo probability scale (Naranjo et al., 1981), which helps to identify the causal relation between an ADR and a drug based on the validated clinical questionnaire set by domain experts. The Naranjo scale consists of 10 questions which are administered for each patient’s clinical record. The Naranjo scale assigns a causality score, which is the sum of the scores of all Naranjo questions, that classifies the case into one of four causality types: doubtful (≤0), possible (1–4), probable (5–8), and definite (≥9). This patient had a Naranjo probability score of 8, which indicated that LMWH was a probable cause of this bleeding event. All the above examinations revealed a final diagnosis of hematoma of the colon, a rare ADR caused by LMWH therapy.
Treatment
The patient accepted conservative management with bowel rest and intravenous fluids. His anticoagulation therapy of subcutaneous LMWH injection was discontinued immediately. Phloroglucinol injection (40 mg) as a musculotropic antispasmodic drug was prescribed to relieve abdominal pain. Tranexamic acid as a procoagulant was used to reduce the risk of bleeding, and omeprazole was prescribed to prevent gastrointestinal mucosal injury.
Outcome and Follow-Up
On March 27th, the patient’s abdominal pain was relieved, and a CT scan showed that intestinal hematoma was absorbed (Figure 1C). The patient was discharged from hospital 2 weeks later.
Discussion
Spontaneous bowel intramural hematoma is a rare complication under anticoagulant therapy. Warfarin is the most common cause of spontaneous intramural small-bowel hematoma in adults. The incidence of bowel hematoma was reported to be 1/2500 per year in patients receiving warfarin, and the incidence is relatively higher in males (Bettler et al., 1983). Limmer and Clement (2017) reported a case of successful conservative treatment of bowel hematoma caused by overdose anticoagulation with warfarin in a 71-year-old man. Shaw et al. (2005) reported one case of small-bowel hematoma in a child who received therapeutic doses of LMWH because of deep venous thrombosis. Approximately 85% of spontaneous intestinal intramural hematomas in patients with anticoagulant therapy occur in the small bowel (Xiao et al., 2015); however, the incidence of spontaneous hematoma is extremely rare in the colon. Thus, we herein present a novel case of spontaneous intramural hematoma of the colon associated with subcutaneous LMWH therapy.
Clinical presentation of bowel hematoma can vary from mild abdominal pain to intestinal obstruction or an acute abdomen. Nausea and vomiting are found in half of the cases and are related to intestinal obstruction. The average time from the occurrence of symptoms until medical attendance is 2.5 days (Sorbello et al., 2007). The diagnosis of bowel hematoma requires imaging data. Abdominal CT is currently the preferred imaging method for intestinal hematoma. Some people suggested that non-contrast CT should be performed for oral and intravenous contrast medium application, as contrast-enhanced CT alone may mask the presence of intramural hemorrhage. Most bowel hematomas can be treated conservatively, including discontinuing or reversing the anticoagulation and alleviating abdominal pain caused by intestinal obstruction. Surgery is indicated for complications or persistence of bowel hematoma (Zammit et al., 2013). Our patient was 76 years old, with a body mass index of 21.66. He had normal coagulation, liver, and kidney function at admission, and had no medical history of hemorrhagic diseases. Abdominal pain occurred 3 days after subcutaneous injection of LMWH, and abdominal CT scan indicated an intramural hematoma of the colon. This colon hematoma ADR is not mentioned in the official product information of LMWH.
LMWH has become the preferred agent for the prophylaxis and treatment of thrombosis disease. Compared with heparin, it has been shown to be safe and effective, with reduced incidence of heparin-induced thrombocytopenia (HIT) complication. LMWH molecular weight around 5000 Da is considerably variable in the chemical structure and has anti-factor Xa and anti-factor IIa activities (Hao et al., 2019). LMWH has a lower anti-factor IIa activity and a relatively higher anti-factor Xa activity. Subcutaneous LMWH injection is absorbed completely, with a half-life period of 3–5 h. While routine monitoring of coagulation parameters is not usually necessary for LMWH, certain populations (including pregnant patients, children, obese patients, and patients with renal impairment) may benefit from the monitoring of anti-factor Xa activity to help guide drug therapy (Levine et al., 2004; Sunseri et al., 2018). The main risk of LMWH, as with any anticoagulation agent, is bleeding. Hemorrhagic events that are reported usually include subcutaneous hematoma, hematuria, hemorrhinia, and gastrointestinal and retroperitoneal hemorrhage, while bowel hematoma rarely occurs. One of the mechanisms leading to bowel intramural hematoma might be the rapid decompression of splanchnic circulation due to decreased abdominal pressure, causing the bowel to rupture and bleed while he was on therapeutic anticoagulation therapy. There were limitations in our case; it was unclear whether LMWH dosage was a factor in the hemorrhage as the anti-Xa level was not monitored, and some other features such as genetic factors were also not been measured.
Conclusion
The most frequent minor bleeding events of LMWH anticoagulation are hemorrhage and subcutaneous hematoma. This case demonstrated that bowel hematoma despite its low incidence should be considered as an ADR of LMWH therapy, especially among patients who present with gastrointestinal symptoms.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
YZ was the patient’s doctor, reviewed the literature, and contributed to revision of the manuscript; CW collected the clinical data; CX was responsible for English language revision; JL designed and wrote the article.
Funding
Supported by the National Natural Science Foundation of China (No. 81800250) and Yangzhou Science and Technology bureau for social development (YZ2020074).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Bettler, S., Montani, S., and Bachmann, F. (1983). [Incidence of Intramural Digestive System Hematoma in Anticoagulation. Epidemiologic Study and Clinical Aspects of 59 Cases Observed in Switzerland (1970–1975)]. Schweiz Med. Wochenschr 113 (17), 630–636.
Choi, B. H., Koeckert, M., and Tomita, S. (2018). Intramural Bowel Hematoma Presenting as Small Bowel Obstruction in a Patient on Low-Molecular-Weight Heparin. Case Rep. Pediatr. 2018, 1–3. doi:10.1155/2018/8780121
Chung, K. T. (2016). Intra-Abdominal Hematoma Following Enoxaparin Injection. Clin. Med. Insights Case Rep. 9, 1–38. doi:10.4137/CCRep.S17881
Hao, C., Sun, M., Wang, H., Zhang, L., and Wang, W. (2019). Low Molecular Weight Heparins and Their Clinical Applications. Prog. Mol. Biol. Transl. Sci. 163, 21–39. doi:10.1016/bs.pmbts.2019.02.003
Levine, M. N., Raskob, G., Beyth, R. J., Kearon, C., and Schulman, S. (2004). Hemorrhagic Complications of Anticoagulant Treatment. Chest 126 (3 Suppl. l), 287s–310s. doi:10.1378/chest.126.3_suppl.287S
Limmer, A. M., and Clement, Z. (2017). Extensive Small Bowel Intramural Haematoma Secondary to Warfarin. J. Surg. Case Rep. 2017 (3), rjx044. doi:10.1093/jscr/rjx044
Naranjo, C. A., Busto, U., Sellers, E. M., Sandor, P., Ruiz, I., Roberts, E. A., et al. (1981). A Method for Estimating the Probability of Adverse Drug Reactions. Clin. Pharmacol. Ther. 30 (2), 239–245. doi:10.1038/clpt.1981.154
Shaw, P. H., Ranganathan, S., and Gaines, B. (2005). A Spontaneous Intramural Hematoma of the Bowel Presenting as Obstruction in a Child Receiving Low-Molecular-Weight Heparin. J. Pediatr. Hematol. Oncol. 27 (10), 558–560. doi:10.1097/01.mph.0000183865.56533.9b
Sorbello, M. P., Utiyama, E. M., Parreira, J. G., Birolini, D., and Rasslan, S. (2007). Spontaneous Intramural Small Bowel Hematoma Induced by Anticoagulant Therapy: Review and Case Report. Clinics 62 (6), 785–790. doi:10.1590/s1807-59322007000600020
Sunseri, M., Ahuja, T., Wilcox, T., and Green, D. (2018). Acquired Coagulopathy and Hemorrhage Secondary to Subcutaneous Heparin Prophylaxis. Case Rep. Hematol. 2018, 1–5. doi:10.1155/2018/9501863
Xia, Z.-N., Zhou, Q., Zhu, W., and Weng, X.-S. (2018). Low Molecular Weight Heparin for the Prevention of Deep Venous Thrombosis after Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Int. J. Surg. 54 (Pt A), 265–275. doi:10.1016/j.ijsu.2018.04.059
Xiao, L., Ling, F., Tan, L., Li, H., Hu, C., Luo, Y., et al. (2015). Spontaneous Calf Hematoma in a Patient with Diabetic Nephropathy Receiving Maintenance Hemodialysis: A Case Report and Review of the Literature. Hemodial Int. 19 (4), E49–E53. doi:10.1111/hdi.12246
Keywords: anticoagulation, bowel, hematoma, low molecular weight heparin, case report
Citation: Zhu Y, Wang C, Xu C and Liu J (2021) Case Report: Spontaneous Intramural Hematoma of the Colon Secondary to Low Molecular Weight Heparin Therapy. Front. Pharmacol. 12:598661. doi: 10.3389/fphar.2021.598661
Received: 25 August 2020; Accepted: 21 April 2021;
Published: 14 May 2021.
Edited by:
Marleen Van Der Kaaij, Amstelland Hospital, NetherlandsReviewed by:
Raymond Noordam, Leiden University Medical Center, NetherlandsLoes Visser, Erasmus Medical Center, Netherlands
Marijke Trappenburg, Amstelland Hospital, Netherlands
Copyright © 2021 Zhu, Wang, Xu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Liu, bGl1amlhODU5MTJAMTYzLmNvbQ==
 Ye Zhu
Ye Zhu Chao Wang1
Chao Wang1 Chao Xu
Chao Xu Jia Liu
Jia Liu