- 1Department of Pharmaceutical Sciences, Faculty of Technology, Kumaun University, Nainital, India
- 2Department of Pharmaceutical Botany, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania
- 3ICHAT and Institute for Life Sciences, University of Agricultural Sciences and Veterinary Medicine of Cluj-Napoca, Cluj-Napoca, Romania
- 4Division BIOCEV, Institute of Molecular Genetics, Academy of Sciences of the Czech Republic, Prague, Czechia
- 5Applied Biotechnology Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
- 6Institute of Genetics and Animal Breeding of the Polish Academy of Sciences, Jastrzebiec, Poland
- 7School of Medical Sciences, Universiti Sains Malaysia, Kota Bharu, Malaysia
- 8Department of Public Health, Xi'an Jiaotong-Liverpool University, Suzhou, China
- 9Department of Pharmacognosy, University of Vienna, Vienna, Austria
- 10Department of Vascular Biology and Thrombosis Research, Centre for Physiology and Pharmacology, Medical University of Vienna, Vienna, Austria
Jaundice is a very common symptom especially in the developing countries. It is associated with several hepatic diseases which are still major causes of death. There are many different approaches to jaundice treatment and the growing number of ethnomedicinal studies shows the plant pharmacology as very promising direction. Many medicinal plants are used for the treatment of jaundice, however a comprehensive review on this subject has not been published. The use of medicinal plants in drug discovery is highly emphasized (based on their traditional and safe uses in different folk medicine systems from ancient times). Many sophisticated analytical techniques are emerging in the pharmaceutical field to validate and discover new biologically active chemical entities derived from plants. Here, we aim to classify and categorize medicinal plants relevant for the treatment of jaundice according to their origin, geographical location, and usage. Our search included various databases like Pubmed, ScienceDirect, Google Scholar. Keywords and phrases used for these searches included: “jaundice,” “hyperbilirubinemia,” “serum glutamate,” “bilirubin,” “Ayurveda.” The first part of the review focuses on the variety of medicinal plant used for the treatment of jaundice (a total of 207 medicinal plants). In the second part, possible mechanisms of action of biologically active secondary metabolites of plants from five families for jaundice treatment are discussed.
Jaundice: An Overview
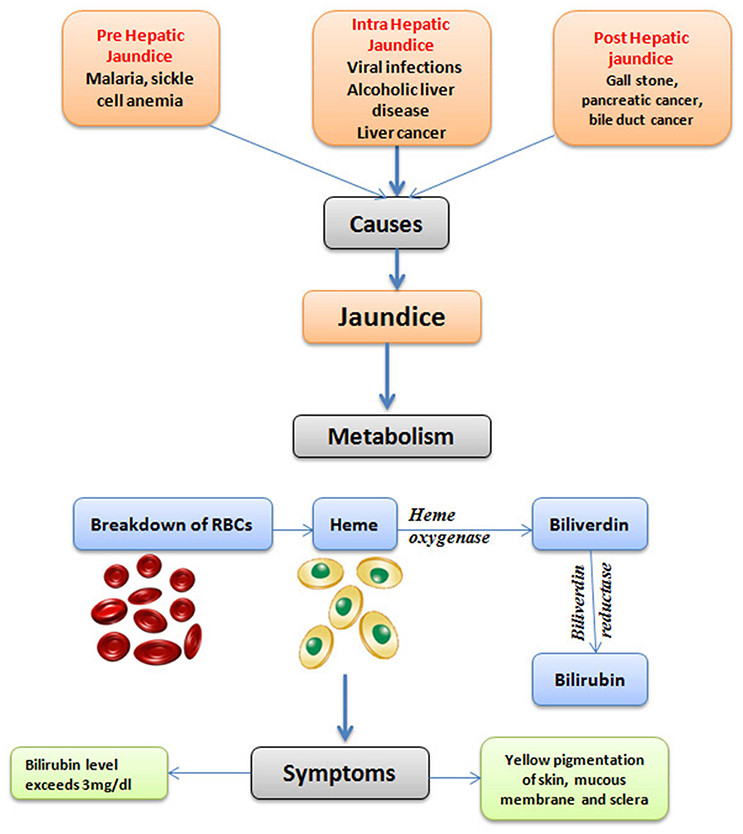
Jaundice is one of the most wide spread disease conditions occurring throughout the world. It is also a life-threatening condition, mostly in the underdeveloped countries. Jaundice is caused by elevated serum bilirubin concentration in the body (Ullah et al., 2016). The term “jaundice” is derived from the French word “jaune,” which literally means yellow (Constantin, 2011). The metabolism of bilirubin takes place through the hemolysis of red blood cells (RBCs), which leads to the release of hemoglobin. The heme oxygenase degrades heme into biliverdin and carbon monoxide within the reticuloendothelial system. Biliverdin is then converted to unconjugated bilirubin by biliverdin reductase (Figure 1). The unconjugated bilirubin binds to albumin and is transported to the liver. The unbound unconjugated bilirubin is toxic to the central nervous system as it can cross the blood-brain barrier (BBB) (Brites, 2012; Olds and Oghalai, 2015; Jasprova et al., 2016).
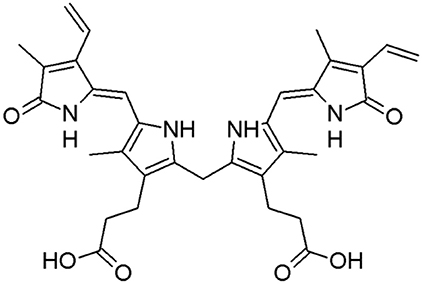
Jaundice is mainly observed in neonates and is not common in adults. However, when it is present in adults, it suggests a serious predicament. In developing countries in particular, jaundice is very prevalent and can be life-threatening. The pathophysiology of jaundice and the metabolism of bilirubin take place in three phases: viz. pre-hepatic phase, the intra-hepatic phase, and the post-hepatic phase. A problem in any of these phases can lead to jaundice. Bilirubin is the metabolic (or breakdown) product of hemoglobin in erythrocytes (Figure 2). The heme metabolism has a central role for bilirubin production (Memon et al., 2016). Heme is an iron-containing porphyrin that is present in hemoglobin, myoglobin, and numerous enzymes, such as hepatic cytochromes (de Visser and Stillman, 2016). It is estimated that 80% of bilirubin formation takes place through heme breakdown in reticuloendothelial cells, spleen, or liver.
The unconjugated bilirubin is largely insoluble in water, but can be reversibly conjugated to albumin. It is transported to the liver, escaping the filtration in kidneys. Generally 90–95% of the bilirubin circulating in the blood is unconjugated. In the case of hypoalbuminemia (a type of hypoproteinemia), bilirubin displacement from the albumin molecules may cause diffusion of bilirubin across the BBB. This is by means of an assortment of drugs and/or increase in the blood unconjugated bilirubin levels. If the higher amount of bilirubin crosses the BBB and the level of unconjugated bilirubin in the blood reaches 15–20 mg/dL, it causes bilirubin encephalopathy, or kernicterus (a bilirubin induced brain dysfunction; Kruger, 2011). The conjugation of bilirubin takes place across the sinusoidal membrane within the hepatocytes after the hepatic uptake, followed by the action of microsomal uridine diphosphoglucuronyl transferase (UDPGT), converting bilirubin to water-soluble form and facilitating its excretion into bile and by the urine (Kruger, 2011). The metabolism of heme results in about 4 mg/kg/day bilirubin production. Maximum amount (about 80%) of heme moiety is utilized by the catabolism of erythrocytes and the rest 20% resulting from the ineffective erythropoiesis and breakdown of muscle myoglobin and cytochromes (Pashankar and Schreiber, 2001).
The major manifestation of jaundice is the yellow color of skin and mucous membranes due to deposition/gathering of bile pigments in blood and body tissues by bilirubin. The color expression is the same in case of carotenemia, but in this condition the bilirubin levels are normal (Kruger, 2011; Schlosser et al., 2011). The pigment depositions are of little effect for most newborns, but in preterm infants even lower doses of bilirubin have the potential for causing kernicterus (Maisels, 2000; Santos et al., 2008). Adults usually have a normal range of serum total bilirubin concentration <1 mg/dL (Roy-Chowdhury and Roy-Chowdhury, 2011). There are several parameters by which the jaundice can be diagnosed once the bilirubin concentration reaches 2.0–2.5 mg/dL. However, even experienced clinicians may not observe the yellow skin coloration until the serum bilirubin levels reach 7–8 mg/dL. It is believed that this coloration is clinically detected once the serum bilirubin level increases above 3 mg/dL (51.3 μmol/L; Roche and Kobos, 2004).
The occurrence of jaundice (icterus neonatorum) in newborns is observed for centuries. Juncker and Stahl (1724), in the Conspectus Medicinae Theoretico praticae distinguished “true jaundice” and “the icteric tinge which may be observed in infants, immediately after birth” (Lauer and Spector, 2011). A subcommittee on hyperbilirubinaemia estimated that apparent jaundice developed approximately in 60% of full term babies along with 85% of pre-term babies and about 10% of breast fed babies are still jaundiced at age of 1 month (Dennery et al., 2001; Zeitoun et al., 2013). The neonatal jaundice is apparent on day 3, peaking on day 5–7 and resolving by day 14 is called “physiological jaundice,” and it is considered as normal physiological condition. The “physiological” jaundice is usually benign, however brain injury and lifelong disability can occur if serum bilirubin (unconjugated), which is neurotoxic, is too high level and crosses the BBB causing damage of auditory nerve and basal ganglia (Subcommittee on Hyperbilirubinemia American Academy of Pediatrics, 2004). Such condition is rare (about seven new cases each year in the United Kingdom; Manning et al., 2007) and sequel include deafness, choreoathetoid cerebral palsy, and upgaze palsy. The signs and symptoms of jaundice are associated with serious liver disease, such as biliary atresia, whose treatment should be done at the age of 6 weeks (Hartley et al., 2009; Lauer and Spector, 2011). It should be noted that the disease imposes large social costs (Ebrahimimd et al., 2011). Most commonly accepted treatment of hyperbilirubinemia is phototherapy. However, there are several complications like dehydration, retinal injury, bronze baby syndrome and diarrhea, which can put the baby at risk (Stoll and Kliegman, 2004; Kliegman et al., 2007; Ebrahimimd et al., 2011).
History of Jaundice
The history of jaundice is very long and is described as a sign of “causeless hatred” in the Babylonian Talmud (Poduri, 2016). There are various ancient references related to jaundice which are presented in Babylonian Talmud, Sumerian Tablets, Ebers papyrus, and in Ancient Ayurveda (the Indian traditional system of medicine; Poduri, 2016).
Moreover, the work of Hippocrates (460–370 B.C.) also provided references to jaundice (Schmid, 2001; Bynum, 2008). The terms that are used in hepatology like “hepatic,” “liver,” and “jaundice” have been originated from Greek, Sanskrit and French languages, respectively (Riva et al., 2011; Definition, 2016)1. The most primitive Latin word used to indicate the liver was “iecur,” which is likely from Sanskrit “yakrt” (Riva et al., 2011). The word “jaundice” derives from an old French word “jalnice,” followed by “jaunice,” which means “yellowness.” In earlier times before 1800, there was limited notion about jaundice. Its relation to the alcohol uptake was described in 1836 by Addison (Gao and Bataller, 2011). In 1885 Lühraman recorded the occurrence of jaundice as an adverse effect of vaccination (Thomas et al., 2013; Trepo, 2014). In 1908 McDonald suggested that the probable cause of jaundice might be an agent, which was much smaller than bacterium (McDonald, 1908; Thomas et al., 2015). This idea was developed in 1923 by the hypothesis that virus was the cause for jaundice (Thomas et al., 2013; Poduri, 2016). A great number of death cases were observed during World War II (WWII) by hepatitis (1939–1945). During WWII, it was estimated that around 16 million people were killed as a consequence of hepatitis (Trepo, 2014). Therefore, different liver disease conditions like autoimmune hepatitis, liver cirrhosis, hepatitis A, B, C, D, E, hepatic carcinoma, or hemolytic anemia may lead to jaundice (Wahab et al., 2004; Amiri et al., 2014).
Discovery of Hepatitis Viruses
Most common hepatitis viruses are categorized as hepatitis-A (HAV), hepatitis-B (HBV), hepatitis-C (HCV), hepatitis-D (HDV), and hepatitis-E (HEV). Although, HBV, HCV, and HDV are spread mainly by blood exposure, HBV is transmitted mostly by unprotected sex. On the other hand HAV and HEV are spread predominantly by fecal-oral means (Singhal et al., 2009; Puri, 2014). A brief account on the discovery of these hepatitis viruses are presented here:
Hepatitis A Virus
HAV belongs to Picornaviridae family of the genus Hepatovirus. Seven genotypes of HAV in the feces may be seen and excretion of 106–1,011 viruses per gram of feces was recorded for HAV (Coudray-Meunier et al., 2014; Sánchez, 2015; Bennett et al., 2016). The origin of HAV may be traced back to epidemics of “campaign jaundice,” which afflicted the armies of Middle Ages and it has been a serious problem during the Korean and Vietnamese conflicts (Zuckerman, 1976; Beaumier et al., 2013). Every year around 1.4 million new cases of HAV infection are reported around the world [http://www.who.int/csr/disease/hepatitis/whocdscsredc2007/en/index4.html (Accessed on July 13, 2016) Kim et al., 2017].
Hepatitis B Virus
HBV belongs to the family Hepadnaviridae and genus Orthohepadnavirus (Tajiri and Shimizu, 2016). HBV isolates are categorized into 10 groups of genotypes with nucleotide sequence divergence of 7.5% or higher (Tong and Revill, 2016; Zhang et al., 2017). It is an enveloped DNA virus with presence of transcriptional template [3.2-kb covalently closed circular (ccc) DNA] in the infected hepatocytes nucleus (Seeger and Mason, 2015; Zhang et al., 2017). Lurman (1885) reported the occurrence of an epidemic of hepatitis in the Bremen's Shipyard workers, following vaccination against smallpox with glycerinated lymph of human origin in 1883. In 1970 transmission of hepatitis B was first carried out in chimpanzees. In 1981, the first vaccine against hepatitis B was licensed in the USA, which was prepared by purified hepatitis B surface antigen (HBsAg), a viral envelop protein from the plasma of chronically affected individuals (Geier et al., 2003).
Hepatitis C Virus
HCV belongs to the genus Hepacivirus which is a hepatotropic enveloped, positive-stranded RNA virus of Flaviviridae family (Elgharably et al., 2017). Seven major and more than 12 minor genotypes of HCV have been identified based on the genomic sequence heterogeneity (Petruzziello et al., 2016). Until 1975, hepatitis A and B were recognized since the diagnostic tests were available for both. However, hepatitis C was reported as a non-A non-B virus from stored samples of transfusion associated with hepatitis (Feinstone et al., 1975; Kim et al., 2016). The viral RNA was identified in 1989 by reversed-transcription PCR, and the subsequent cloning and sequencing led to the description of the whole genome (Kuo et al., 1989). Only few proteins out of the entire viral protein pool are serving as a base for different serologic tests and anti-HCV antibodies.
Hepatitis D Virus
Existence of HDV was found by immunofluorescence in liver biopsies from Italian patients with chronic HBV infection in 1978 as previously uncharacterized intranuclear antigen. The antigen is coupled with the capsid protein of previously unrecognized virus, afterwards termed as “hepatitis delta virus” (HDV; Rizzetto and Verme, 1985; Taylor, 2006). HDV was distinguished and did not share any homology to the other known animal viruses and resembled the plant virus satellites, which are also related to plant viroids (Sureau and Negro, 2016). The HDV genome consists of single-stranded RNA and eight genotypes have been identified from different geographical regions (Opaleye et al., 2016).
Hepatitis E Virus
HEV, an RNA-containing virus which is the only virus of genus Hepevirus belonging to family Hepeviridae. The virus is classified in four genotypes distributed all over the world (Fierro et al., 2016). Hepatitis E was recognized as a unique human disease in 1980 by examining stored clinical samples collected during water-borne epidemics of viral hepatitis A and B in Indians (Khuroo, 1980; Wong et al., 1980; Fierro et al., 2016). The massive epidemic of hepatitis, which occurred in Delhi, India during 1955–1956 by contamination of a major water treatment plant with raw sewage, was considered as a classical example of water borne hepatitis A (Kumar et al., 2013). The consequent studies revealed that the Indian population is highly endemic to hepatitis A, as HAV infected almost 100% of the population by the age of 5–10 years, which made it difficult to discriminate HAV from other causes before Delhi epidemic and other water born epidemics that occurred in young adults. In 1983 HEV was transmitted to a human volunteer and cynomolgus monkeys and visualized for a first time and its role in enteric transmitted NANB (ET-NANB) hepatitis was proved (Balayan et al., 1983).
Hepatitis G Virus
Hepatitis G virus is also described, however it is still not known if it causes any diseases in humans (Hall, 2007).
Apart from viral hepatitis, several other causes of jaundice are also reported. These include malignancy, sepsis, shock, cirrhosis, gall stones, drugs, and autoimmune hepatitis (Whitehead et al., 2001).
Ethnopharmacological Approaches for Management of Jaundice: History, Significance, and Diversity of the Used Medicinal Plants
According to the review by Hatfield (2004), several unusual practices have been employed to treat jaundice. In the British traditional medicine, there are some unusual home remedies for jaundice. A grotesque fallacy from Staffordshire is via the use of a bladder, which is filled by the patient's urine and placed close to the fire. It is believed that the patient recovers as it dries out. Another example of this kind is recorded from west Sussex, where an alive spider is rolled up in its own web and gulp down as a pill to cure jaundice. In Westmoreland alive head lice, and roasted powdered earthworms in Ireland, are ingested to cure jaundice (Hatfield, 2004). The use of snails was also found during seventeenth century as a cure for jaundice. Use of sheep's dung in water, giving the patient a violent fright (Hatfield, 2004) and a decoction of the common slater (woodlouse) in beer is also found to cure jaundice in Scotland. Urine was also used in various countries viz. in Ireland, urine mingled with milk like a drink against jaundice. In Yorkshire, baked rye cake with patient's urine under slow burning was believed to fade the illness away (Hatfield, 2004). In India such type of unusual practices were very common in the past. Certain people claimed to cure jaundice by spiritual practices and the use of Mantras (a sacred utterance, a spiritual sound, mainly are group of words in Sanskrit) along with some precautions, such as avoiding the fried and oily food, avoiding yellow color food especially use of turmeric in food. The practitioners used oil along with Durva [Cynodon dactylon (L.) Pers.], and used a bronze coin to treat the patients, for 3–4 weeks and within this time the patient gets rid from jaundice.
Several household remedies are used for jaundice treatment including eggs, cider, tea made from oats (Avena sp.) and vinegar. Some less distasteful propositions were, to use pearls dissolved in vinegar (De Lys, 1948) and a mixture of horn scraping and honey (Allen, 1963). Eating shellfish is a suggestion of Japanese origin (UCLA Folk Archives, record number 23_5423). Similarly to the Yorkshire method, baking of cornmeal cake with the patient's urine and its burning was used to cure jaundice (Hyatt, 1965; Hatfield, 2004). Various amulets are also used in North American folk medicine against jaundice. Some of these were made up of metals such as a copper necklace, or coin worn around the neck (UCLA Folklore Archives, record number 11_6404; Hatfield, 2004); gold piece of $ 5 strapped to the chest, or red beets worn round the neck (Puckett, 1981). Dressing of the patient in yellow clothes is a common practice in Pennsylvania to cure jaundice, which is in fact a custom of Russian origin (Crosby, 1927; Hatfield, 2004). Transference is also a typical example of jaundice cure, in which hard-boiled eggs strung over a necklace or placed under the armpits overnight (Hyatt, 1965; Hatfield, 2004). The next morning the egg white would be yellow, and the patient becomes white (Rogers, 1941). Some other sundry remedies for children suffering from jaundice are to place baby between two pillows, which would “bleach” out the jaundice (UCLA Folklore Archives, record number 23_58900, Hatfield, 2004). Although, these are based on typical practices used in older times, presumably these “treatments” do not work.
In Ayurveda, a variety of pathological conditions associated with jaundice are described under the generalized title referred as “Pandu-roga” (generally considered as anemia) which is a Sanskrit term meaning yellowish pale, or white disease. One of the important unique texts of Ayurveda, the Charak Samhita, or Carak Samhita (Before second Century A.D.) described in detail the eight categories of Pandu-roga (wherein another term “Udarroga” is mentioned for gastroenterological disorder) including “Kamala,” which seems to be the most relevant for jaundice condition. It was further described that Kamala (jaundice) is not developed during the initial stage of the condition. The occurrence of jaundice may develop if the initial Pandu-roga is not cured properly, and if the patient consumes bile-producing food. There are several important symptoms attributed to Kamala, which seem to be clearly associated with jaundice. They include: yellowish to greenish-yellow coloration of urine, sclera, nails and skin, reduction in the power of the senses, weakness, anorexia, indigestion, burning sensation and sometimes red urine (Durkin, 1988). Charaka (Caraka) described the treatment of various Pandu-roga including Kamala by different methods like emesis, evacuation of bowels, ingestion of medicated ghee, diet rich in rice, wheat, barley, and broth of Mung leaves (Vigna radiata L. R. Wilczek), as well as the use of different medications, which could restore humoral balance. All categories of Pandu-roga were mainly described as caused by the eating habits, and that the excess of hot, sour, salty, lentils, sesame oil, and seed pulp may cause various gastrointestinal problems. As the Ayurveda also tells about the life style, it was further depicted that overindulgence in sexual intercourse, suppression and negligence of bodily urges, emotional attributes (anger, sorrow, worry etc.) and day time sleeping may also cause an imbalance among the three humors (Vata, Pitta, Kapha, which are the basis of Ayurveda) by provoking bile in excess amount. Such types of imbalance showed different symptoms of jaundice and mainly the yellow pigmentation of skin. Some of the frequently used plants described include Phyllanthus emblica L., Operculina turpethum (L.) Silva Manso, Azadirachta indica A. Juss., Zingiber officinale Roscoe, Piper longum L., P. nigrum L., Curcuma spp. Swertia chirayita (Roxb.) Buch.-Ham. ex C.B.Clarke, Picrorhiza kurroa Royle ex Benth., Terminalia bellirica (Gaertn.) Roxb., and T. chebula. Most of these plants are already listed in Table 1, which indicates the significance of the Ayurvedic plants for the treatment of this condition. In Nepal it was described that some of the Vaidyas are being practicing Ayurved (Indian System of medicine). The Vaidyas of Kathmandu used to treat several ailments, although they are renowned for their ability to treat jaundice. Jaundice is considered as one of the most common disease conditions in Nepal and its association with viral hepatitis. An interesting fact reported by Durkin in 1988 is that, even though the people who generally do not rely on Ayurvedic treatment are also consulting to Vaidya, if jaundice occurs to them or their family members. It is also believed that effective treatment for jaundice is present in Ayurveda. The use of numerous plants in jaundice supports the above statement as Ayurveda utilizes a large number of medicinal plants and the major portion of Ayurvedic treatment relies on medicinal plant based formulations. The term Kamala and Kamala pitta are generally used by Vaidya in Nepal for jaundice. The cause of jaundice may include bile promoting food, dirty water intake from which the microbes could transmit and seasonal fluctuations (it was also observed that occurrence of jaundice is more frequent in autumn; Durkin, 1988).
Various herbal medicines for treatment of jaundice are being used from ancient times. Combination of Bogbean (Menyanthes trifoliate L.), raspberry (Rubus sp.) and wild mint (Mentha spp.) was used to treat jaundice (Beith, 1995; Hatfield, 2004). In Shetland, Bogbean is known as gulsa girse, which literally means “yellow sickness plant” (Vickery, 1995). The bark decoction of another important plant, Barberry (Berberis vulgaris L.) also known as the “jaundice tree” in Cornwall; has been widely used for the treatment of jaundice in England and Ireland (Vickery, 1995). Some other important plants used for jaundice treatment are: dandelion (Taraxacum campylodes G.E. Haglund), Ulex europaeus L. (Vickery, 1995; Hatfield, 2004), and nettle roots (probably Urtica dioca; Hatfield, 2004). Greater celandine (Chelidonium majus L.) is used for the treatment of infantile jaundice. Other plants used mainly in European countries for the treatment of jaundice are Primarose (Primula vulgaris Huds.) in Ireland, cowslip (Primula veris L.), in England, leaves of the savage tree (Juniperus sp.) in Wales, (EFS record number 221), chickweed (Tragopogon porrifolius L.), salsify [Stellaria media (L.) Vill.] in East England, Ulmus spp. boiled in milk in Herefordshire and Ireland (Vickery, 1995; Hatfield, 2004).
In Britain other herbal remedies are used like dandelion (Taraxacum sp.), greater celandine, which is either worn in the shoes (Lick and Brendle, 1923) or ingested (Meyer, 1985). Various botanical remedies like walnut bark (Juglans sp.), boneset (Eupatorium perfoliatum L.), hops (Humulus lupulus L.), wild cherry bark (Prunus serotina Ehrh.), black alder [Ilex verticillata (L.) A. Gray], leaves or bark of peach [Prunus persica (L.) Batsch], cinquefoil (Potentilla Canadensis L.) (Meyer, 1985), strawberry leaves (Fragaria spp.) (Lick and Brendle, 1923), a tea made from catnip (Nepeta cataria L.) (Puckett, 1981) or from mullein (Verbascum sp.) (Parler, 1962) are used to treat jaundice. Some other important herbal infusion which are used to treat jaundice are yarrow (Achillea millefolium L.) (Hendricks, 1959), crossvine (Bignonia capreolata L.) (Rogers, 1941), calamus root (Acorus calamus L.) (Puckett, 1981), mayapple root (Podophyllum peltatum L.) (Clark, 1970), yellow dock root (Rumex crispus L.) (Lick and Brendle, 1923), rosemary leaves (Rosmarinus officinalis L.) (UCLA Folklore Archives, record number 4_2092), ironwood bark (Carpinus caroliniana Walter), and St. John's wort (Hypericum perforatum L.) (Hatfield, 2004). In Carolina, tea brewed from wild oranges and basil (Ocimum basilicum L.) (Brown, 1952-1964) was used for treating jaundice. In the Midwest, bruised lobelia and red pepper pods in whisky were used (Pickard and Buley, 1945). In Indiana a mixture containing bitter root (Lewisia sp.), red sumac (Rhus sp.), wild cherry bark (Prunus sp.), sarsaparilla root, and wild poplar root (Populus sp.) was used (Halpert, 1950; Hatfield, 2004). Haematoxylon spp. (longwood) has been used to treat jaundice in Mexico. The Haematoxylon spp. extract is utilized by two ways drinking the liquid extract, or by placing the glassful of extract on the window still for patient to gawk; further it was hoped to transfer the yellow color from the patient to the liquid (Curtin, 1907; Hatfield, 2004). Vegetables viz. collards (Brassica oleracea L.) (Browne, 1958), artichokes (Helianthus tuberosus L.) were also found useful in jaundice treatment, (UCLA Folklore Achieves, record number 6_7607). The use of tobacco (Nicotiana spp.) alleviate jaundice (Smith, 1929) and daisies (Bellis perennis L.) is recommended for the re-coloration after jaundice treatment (Clark, 1970). Native American practices are also rich in terms of plants for hepatic disorder. For example the use of Juglans cinerea L. is recommended from Iroquois (Herrick, 1977; Hatfield, 2004).
There is an emerging interest in the use of medicinal plants that have been used traditionally for treating various diseases. This is because medicinal plants have the lesser adverse effects and fewer complications compared to synthetic drugs. This is an important advantage of plant derived drugs, which is also advised by the World Health Organization (WHO). The search of bilirubin reducing substances of herbal origin has gained particular interest in recent times (Dennery, 2002; Wong et al., 2005). A number of plant derived products are used either alone, or in combination with various other modern treatment such as exchange transfusion or the phototherapy of infants with high bilirubin concentration (Ebrahimimd et al., 2011). Systematic scientific studies are required to evaluate the safety, efficacy and toxicity profile of various herbal drugs (Kunwar et al., 2009). The utilization of the medicinal plants in the treatment of jaundice is also evident from the number of case series, which exhibited faster reduction of jaundice than western medicine treatment (Ebrahimimd et al., 2011).
The induction of glutathione S-transferase and UDP-glucouronyl transferase (UGT) and the effect on bilirubin metabolism in rats was reported upon treatment with Scutellaria, Rheum officinale L., Artemesia, and Gardenia. The combination of extracts from the above mentioned plants is known as “Yin Zhi Huang” in the Chinese traditional medicine and is used in Asia for the management and treatment of neonatal jaundice via enhancement of bilirubin clearance (Yang and Lu, 1984; Chen and Guan, 1985; Dong et al., 1992; Elferink, 2004). Various medicinal plants have also been used from an ancient time in different countries, including Iran, China, Ethiopia, Mexico, West Africa, Turkey, Peru, Nepal etc., but there are still more studies required to prove their efficacy. Clinical studies have also been carried out in Iran to evaluate the effect of aqueous extract of Zizyphus jujuba Mill. on the neonatal jaundice. The results showed a straight effect of the plant extract on the neonates. The use of medicinal plants in the treatment of jaundice showed in some studies more potent stimulatory effect on bilirubin clearance when compared to phenobarbital (Yin et al., 1993; Zhao et al., 2006). Some of the plants such as Z. jujuba are used in the reinforcement of liver function during jaundice (Chan, 1994; Huang, 1998; Ebrahimimd et al., 2011). However there are some limitations present in the study carried out with Z. jujuba as it was shown effective in the treatment against neonatal jaundice during the first 12 h, but it was not found effective in the consecutive days (Ebrahimimd et al., 2011). The use of herbal medicines to heal the jaundice was also reported from Mashhad city in Iran, where the disease was found to be major health problem (Amiri et al., 2014).
There are two widely accepted methods of neonatal jaundice treatment, phototherapy and blood exchange (Amiri et al., 2014; Chen et al., 2017). In addition, herbal remedies are also very popular in the treatment of jaundice, especially in the Iranian tradition (Rajaei and Mohamadi, 2012; Amiri et al., 2014). A number of plant species have been utilized in Iran (Table 1 and Figure 3). There are very limited pharmacological interventions, which are used for the treatment of neonatal jaundice. The available pharmacological approaches for treatment of neonatal jaundice are based on different mechanisms of action. Metalloporphyrins, for example act via inhibition of heme oxygenase—the rate limiting enzyme in bilirubin production. The metalloporphyrin consists of a biocompatible metal ion, which does not degrade in tissues and is not photochemically active. Some of the important tissue heme oxygenase inhibitors are chromium mesoporphyrin (CrMP) and tin mesoporphyrin (SnMP) (Vreman et al., 1993; Dennery, 2002). Although, the metalloporphyrin are used frequently and are highly effective, some of those compounds are photochemically active (Dennery, 2002; Lee et al., 2017). Some of the studies revealed a dosage dependent mortality associated with SnMP application in neonatal Wistar rats (Hintz et al., 1990), moreover lipid peroxidation and heamolysis of RBCs was also reported (Keino et al., 1990). Some other adverse effect such as arrhythmia, tachyphylaxis (which is due to the induction of HO-1 protein and mRNA) etc. were also reported upon metalloporphyrins use. Though CrMP does not possess phototoxicity, it cannot be considered as safe because of the carcinogenic effect of Cr metal (De Flora et al., 1980; Voitkun et al., 1998; Dillon et al., 2000). Another important therapeutic regimen for neonatal jaundice is D-Penicillamine. The drug is used to cure neonatal jaundice mainly in Europe but not in the USA (Dennery, 2002). Its main mechanism of action is by the inhibition of HO activity (Juckett et al., 1998). Still there are risks of fatalities associated with this drug, along with the onset of aplastic anemia, thrombocytopenia, myasthenia gravis and Goodpasture syndrome (Louie et al., 1986; Peces et al., 1987; Fishel et al., 1989; Kaufman et al., 1996; Narayanan and Behari, 1999; Teive et al., 2017).
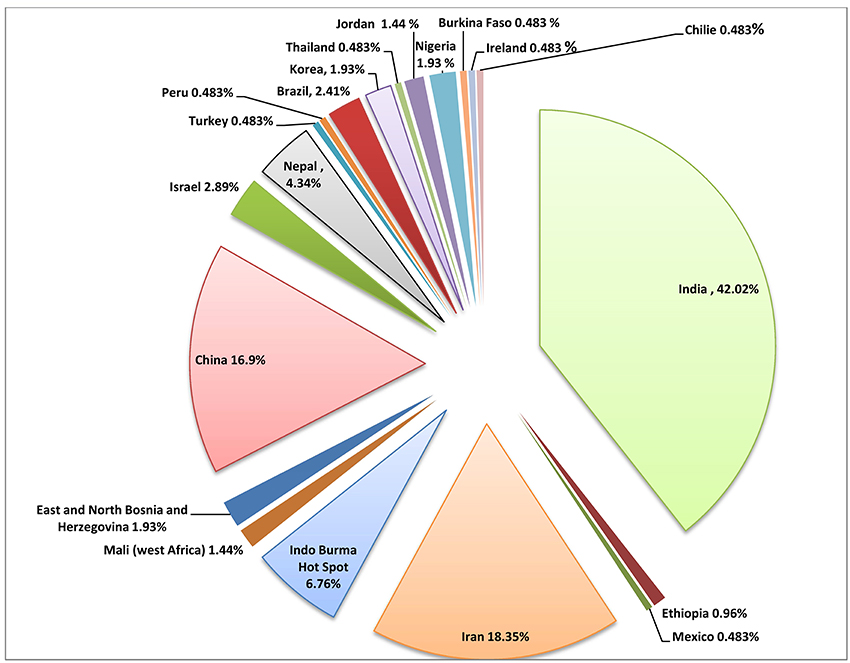
Figure 3. Pie chart showing the distribution of the ethnopharmacologically important plants for the treatment of jaundice worldwide.
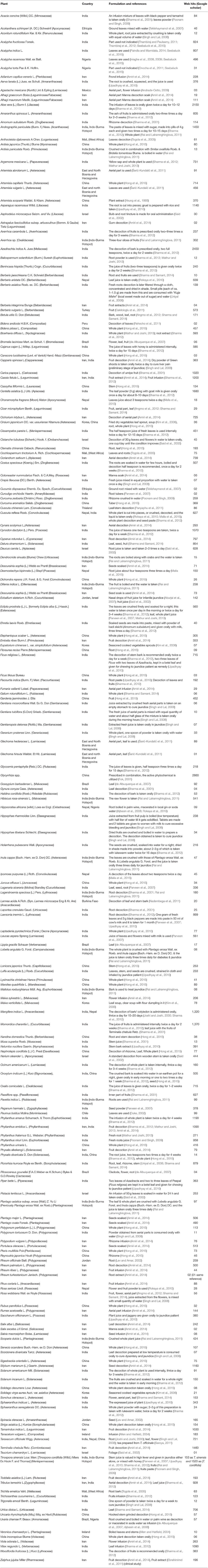
An extensive review has been carried out to explore the use of medicinal plants for jaundice treatment. A total of 207 plant species have been documented and presented in Table 1. The botanical name of the plant, family with the country name from where the plant is reported followed by formulation used for jaundice are summarized and web hits from Google scholar were gathered through Boolean information retrieval method using plant name with “AND” operator (Pohl et al., 2010).
Our work is the first review, which presents comprehensive documentation of the ethnomedicinal uses of the plants for the prevention and treatment of jaundice. Large number of medicinal plants has been shown to have potential in the development of approaches to obtain therapeutic regimen for the treatment of jaundice, although some of the molecules like sylimarin and andrographolide are already well established and widely used for the management of hepatic disorders worldwide. Many medicinal plants are being used from a long back in several countries. Graphical representation at Figure 3 shows the number of medicinal plants used for jaundice in 20 different countries/region, which have been documented in the review.
Conclusion
Various new chemical entities have been developed from natural products, which have been filed in last few decades. Ethnopharmacological information is of prime importance for discovery and usage of significant therapeutically important molecules either obtained from natural sources, or inspired by nature. In this first part of our review, we discussed the history, metabolism process; some unusual practices used in older times and a comprehensive detail about 207 plants, which are used in the treatment or management of jaundice. The substantiation presented is an indicative of the utilization of the plants in the prevention and/or treatment of jaundice. Though there is tremendous ethnopharmacological information about the plants involved in jaundice treatment, only some of them were used in clinical trials and have been explored for their mechanism of action. These studies will be covered in the next part of the review.
Author Contributions
DT, AM, EP, ZM, YL, and AA have written the first draft of the manuscript. AS, SN, LH, and JH revised and improved the first draft. All authors have seen and agreed on the finally submitted version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
AA acknowledges the support by the Polish KNOW (Leading National Research Centre) Scientific Consortium “Healthy Animal—Safe Food,” decision of Ministry of Science and Higher Education No. 05-1/KNOW2/2015 and by the Austrian Science Fund (FWF) project P25971-B23. AM acknowledges the support by UEFISCDI, Romania, project no. PNII-RU-TE-2014-4-1247 and ZM was supported by a postdoctoral research fellowship from the Universiti Sains Malaysia Research University Individual (RUI) grant (ref. no. 1001/PPSP/812151).
Footnotes
1. ^Definition of Icterus (2016). Available online at: http://www.medicinenet.com/script/main/art.asp?articlekey=3890 (Accessed on September 18 2016).
References
Aburjai, T., Hudaib, M., Tayyem, R., Yousef, M., and Qishawi, M. (2007). Ethnopharmacological survey of medicinal herbs in Jordan, the Ajloun Heights region. J. Ethnopharmacol. 110, 294–304. doi: 10.1016/j.jep.2006.09.031
Ajibesin, K. K., Ekpo, B. A., Bala, D. N., Essien, E. E., and Adesanya, S. A. (2008). Ethnobotanical survey of Akwa Ibom State of Nigeria. J. Ethnopharmacol. 115, 387–408. doi: 10.1016/j.jep.2007.10.021
Allen, D. E., and Hatfield, G. (2004). Medicinal Plants in Folk Tradition: an Ethnobotany of Britain & Ireland. Portland, OR: Timber Press.
Allen, J. W. (1963). Legends and Lore of Southern Illinois. Carbondale, IL: Southern Illinois University.
Amiri, M. S., Joharchi, M. R., and TaghavizadehYazdi, M. E. (2014). Ethno-medicinal plants used to cure jaundice by traditional healers of Mashhad, Iran. Iran. J. Pharm. Res 13, 157–162.
Andrade-Cetto, A. (2009). Ethnobotanical study of the medicinal plants from Tlanchinol, Hidalgo, Mexico. J. Ethnopharm. 122, 163–171. doi: 10.1016/j.jep.2008.12.008
Angmo, K., Adhikari, B. S., and Rawat, G. S. (2012). Changing aspects of Traditional Healthcare System in Western Ladakh, India. J. Ethnopharm. 143, 621–630. doi: 10.1016/j.jep.2012.07.017
Balayan, M. S., Andjaparidze, A. G., Savinskaya, S. S., Ketiladze, E. S., Braginsky, D. M., Savinov, A. P., et al. (1983). Evidence for a virus in non-A, non-B hepatitis transmitted via the fecal-oral route. Intervirology 20, 23–31. doi: 10.1159/000149370
Beaumier, C. M., Gomez-Rubio, A. M., Hotez, P. J., and Weina, P. J. (2013). United states military tropical medicine: extraordinary legacy, uncertain future. PLoS Negl. Trop. Dis. 7:e2448. doi: 10.1371/journal.pntd.0002448
Beith, M. (1995). Healing Threads. Traditional Medicines of the Highlands and Islands. Edinburgh: Polygon.
Bennett, A. J., Sibley, S. D., Lauck, M., Weny, G., Hyeroba, D., Tumukunde, A., et al. (2016). Naturally circulating hepatitis a virus in olive baboons, Uganda. Emerg. Infect. Dis. 22, 1308–1310. doi: 10.3201/eid2207.151837
Brites, D. (2012). The evolving landscape of neurotoxicity by unconjugated bilirubin: role of glial cells and inflammation. Front. Pharmacol. 3:88. doi: 10.3389/fphar.2012.00088
Brown, F. C. (1952-1964). Collection of North Carolina Folklore, Vol. 7. Durham, NC: Duke University Press.
Browne, R. B. (1958). Popular Beliefs and Practices from Alabama. Folklore Studies 9. Berkeley, CA; Los Angeles, CA: University of California Publications.
Bynum, W. (2008). The History of Medicine: A Very Short Introduction, Vol. 191. Oxford: Oxford University Press.
Cakilcioglu, U., Khatun, S., Turkoglu, I., and Hayta, S. (2011). Ethnopharmacological survey of medicinal plants in Maden (Elazig-Turkey). J. Ethnopharmacol. 137, 469–486. doi: 10.1016/j.jep.2011.05.046
Chan, K. (1994). The Pharmacology of Chinese Herbs. Kee Chang Huang Published 1993. Boca Raton, FL: CRC Press, Inc.
Chen, Z. L., and Guan, W. H. (1985). Approach to the effect and indication of Yin Zhi Huang to treat neonatal jaundice. J. Clin. Pediatr. Dentistry 3, 302–303.
Chen, Z., Zhang, L., Zeng, L., Yang, X., Jiang, L., Gui, G., et al. (2017). Probiotics supplementation therapy for pathological neonatal jaundice: a systematic review and meta-analysis. Front. Pharmacol. 8:432. doi: 10.3389/fphar.2017.00432
Constantin, T. (2011). Jaundice obstructive syndrome. Curr. Health Sci. J. 37, 96–100. Available online at: http://chsjournal.org/files/PDF_CHSJ/2011/2/CHSJ_2011.2.08.pdf
Coudray-Meunier, C., Fraisse, A., Mokhtari, C., Martin-Latil, S., Roque-Afonso, A.-M., and Perelle, S. (2014). Hepatitis A virus subgenotyping based on RT-qPCR assays. BMC Microbiol. 14:296. doi: 10.1186/s12866-014-0296-1
Crosby, R. J. R. (1927). Modern witches of Pennsylvania. J. Am. Folklor. 40, 304–309. doi: 10.2307/534989
Curtin, R. G. (1907). The medical superstitions of precious stones, including notes on the therapeutics of other stones. Bull. Am. Acad. Med. 8, 444–494.
de Albuquerque, U. P., Muniz de Medeiros, P., de Almeida, A. L., Monteiro, J. M., de Freitas Lins Neto, E., de Melo, J. G., et al. (2007). Medicinal plants of the caatinga (semi-arid) vegetation of NE Brazil: a quantitative approach. J. Ethnopharmacol. 114, 325–354. doi: 10.1016/j.jep.2007.08.017
De Flora, S., Coppola, R., Camoirano, A., Battaglia, M. A., and Bennicelli, C. (1980). Mutagenicity and toxicity of chromyl chloride and its vapours. Carcinogenesis 1, 583–587. doi: 10.1093/carcin/1.7.583
de Visser, S. P., and Stillman, M. J. (2016). Challenging density functional theory calculations with hemes and porphyrins. Int. J. Mol. Sci. 17:519. doi: 10.3390/ijms17040519
Dennery, P. A. (2002). Pharmacological interventions for the treatment of neonatal jaundice. Semin. Neonatol. 7, 111–119. doi: 10.1053/siny.2002.0098
Dennery, P. A., Seidman, D. S., and Stevenson, D. K. (2001). Neonatal hyperbilirubinemia. N. Engl. J. Med. 344, 581–590. doi: 10.1056/NEJM200102223440807
Dillon, C. T., Lay, P. A., Bonin, A. M., Cholewa, M., and Legge, G. J. (2000). Permeability, cytotoxicity, and genotoxicity of Cr(III) complexes and some Cr(V) analogues in V79 Chinese hamster lung cells. Chem. Res. Toxicol. 13, 742–748. doi: 10.1021/tx0000116
Dong, Y. S., Huang, Z. H., and Wu, L. F. (1992). Treatment of infantile hepatitis syndrome with injection of yin zhi huang. Zhongguo Zhong Xi Yi Jie He Za Zhi 12, 26–7, 5–6.
Durkin, M. (1988). Ayurvedic treatment for jaundice in Nepal. Soc. Sci. Med. 27, 491–495. doi: 10.1016/0277-9536(88)90372-3
Ebrahimimd, S., Ashkani-Esfahani, S., and Poormahmudibs, A. (2011). Investigating the efficacy of zizyphus jujuba on neonatal jaundice. Iran. J. Pediatr. 21, 320–324.
Elferink, R. O. (2004). Yin Zhi Huang and other plant-derived preparations: where herbal and molecular medicine meet. J. Hepatol. 41, 691–693. doi: 10.1016/j.jhep.2004.08.001
Elgharably, A., Gomaa, A. I., Crossey, M. M. E., Norsworthy, P. J., Waked, I., and Taylor-Robinson, S. D. (2017). Hepatitis C in Egypt–past, present, and future. Int. J. Gen. Med. 10:1. doi: 10.2147/IJGM.S119301
Feinstone, S. M., Kapikian, A. Z., Purcell, R. H., Alter, H. J., and Holland, P. V. (1975). Transfusion-associated hepatitis not due to viral hepatitis type A or B. N. Engl. J. Med. 292, 767–770. doi: 10.1056/NEJM197504102921502
Fierro, N. A., Realpe, M., Meraz-Medina, T., Roman, S., and Panduro, A. (2016). Hepatitis E virus: an ancient hidden enemy in Latin America. World J. Gastroenterol. 22, 2271–2283. doi: 10.3748/wjg.v22.i7.2271
Fishel, B., Tishler, M., Caspi, D., and Yaron, M. (1989). Fatal aplastic anaemia and liver toxicity caused by D-penicillamine treatment of rheumatoid arthritis. Ann. Rheum. Dis. 48, 609–610. doi: 10.1136/ard.48.7.609
Fok, T. F. (2001). Neonatal jaundice-traditional Chinese medicine approach. J. Perinatol. 21(Suppl. 1), S98–S100; discussion: S104–S107. doi: 10.1038/sj.jp.7210643
Gao, B., and Bataller, R. (2011). Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology 141, 1572–1585. doi: 10.1053/j.gastro.2011.09.002
Geier, M. R., Geier, D. A., and Zahalsky, A. C. (2003). A review of hepatitis B vaccination. Expert Opin. Drug Safety 2, 113–122. doi: 10.1517/14740338.2.2.113
Hartley, J. L., Davenport, M., and Kelly, D. A. (2009). Biliary atresia. Lancet 374, 1704–1713. doi: 10.1016/S0140-6736(09)60946-6
Hatfield, G. (2004). Encyclopedia of Folk Medicine: Old World and New World Traditions. Santa Barbara, CA: ABC-CLIO.
Herrick, J. W. (1977). Iroquois Medical Botany. Ph.D. thesis, State University of New York, NY; Albany.
Hintz, S. R., Vreman, H. J., and Stevenson, D. K. (1990). Mortality of metalloporphyrin-treated neonatal rats after light exposure. Dev. Pharmacol. Ther. 14, 187–192.
Hong, L., Guo, Z., Huang, K., Wei, S., Liu, B., Meng, S., et al. (2015). Ethnobotanical study on medicinal plants used by Maonan people in China. J. Ethnobiol. Ethnomed. 11, 32. doi: 10.1186/s13002-015-0019-1
Hyatt, H. M. (1965). Folklore from Adams County Illinois, 2nd Edn. New York, NY: Memories of the Alma Egan Hyatt Foundation.
Iniaghe, O. M., Malomo, S. O., Adebayo, J. O., and Arise, R. O. (2008). Evaluation of the antioxidant and hepatoprotective properties of the methanolic extract of Acalypha racemosa leaf in carbon tetrachloride-treated rats. Afr. J. Biotechnol. 7, 1716–1720. doi: 10.5897/AJB08.229
Iniaghe, O. M., Malomo, S. O., and Adebayo, J. O. (2009). Proximate composition and phytochemical constituents of leaves of some Acalypha species. Pakistan J. Nutr. 8, 256–258. doi: 10.3923/pjn.2009.256.258
Jasprova, J., Dal Ben, M., Vianello, E., Goncharova, I., Urbanova, M., Vyroubalova, K., et al. (2016). The biological effects of bilirubin photoisomers. PLoS ONE 11:e0148126. doi: 10.1371/journal.pone.0148126
Joshi, A. R., and Joshi, K. (2000). Indigenous knowledge and uses of medicinal plants by local communities of the Kali Gandaki Watershed Area, Nepal. J. Ethnopharmacol. 73, 175–183. doi: 10.1016/S0378-8741(00)00301-9
Juckett, M., Zheng, Y., Yuan, H., Pastor, T., Antholine, W., Weber, M., et al. (1998). Heme and the Endothelium: effects of nitric oxide on catalytic iron and heme degradation by heme oxygenase. J. Biol. Chem. 273, 23388–23397. doi: 10.1074/jbc.273.36.23388
Juncker, J., and Stahl, G. E. (1724). Conspectus Medicinæ Theoretico-Practicæ, Tabulis 137 Omnes Primarios Morbos Methodo Stahliana Tractandos Exhibens: Secunda Vice Editus et Auctus Cum…Præfatione…Stahlii, etc. MS. Notes. Germany: Impensis Orphanotrophei Waisenhaus; Halle an der Saale.
Kaufman, D. W., Kelly, J. P., Jurgelon, J. M., Anderson, T., Issaragrisil, S., Wiholm, B. E., et al. (1996). Drugs in the aetiology of agranulocytosis and aplastic anaemia. Eur. J. Haematol. Suppl. 60, 23–30. doi: 10.1111/j.1600-0609.1996.tb01641.x
Keino, H., Nagae, H., Mimura, S., Watanabe, K., and Kashiwamata, S. (1990). Dangerous effects of tin-protoporphyrin plus photoirradiation on neonatal rats. Eur. J. Pediatr. 149, 278–279. doi: 10.1007/BF02106294
Khuroo, M. S. (1980). Study of an epidemic of non-A, non-B hepatitis: possibility of another human hepatitis virus distinct from post-transfusion non-A, non-B type. Am. J. Med. 68, 818–824. doi: 10.1016/0002-9343(80)90200-4
Kim, H., Song, M. J., and Potter, D. (2006). Medicinal efficacy of plants utilized as temple food in traditional Korean Buddhism. J. Ethnopharmacol. 104, 32–46. doi: 10.1016/j.jep.2005.08.041
Kim, K.-A., Lee, A., Ki, M., and Jeong, S.-H. (2017). Nationwide seropositivity of hepatitis A in Republic of Korea from 2005 to 2014, before and after the Outbreak Peak in 2009. PLoS ONE 12:e0170432. doi: 10.1371/journal.pone.0170432
Kim, S., Han, K.-H., and Ahn, S. H. (2016). Hepatitis C virus and antiviral drug resistance. Gut Liver 10, 890. doi: 10.5009/gnl15573
Kliegman, R. M., Behrman, R. E., Jenson, H. B., and Stanton, B. M. D. (2007). Nelson Textbook of Pediatrics. Philadelphia, PA: Elsevier Health Sciences.
Kruger, D. (2011). The assessment of jaundice in adults: tests, imaging, differential diagnosis. JAAPA 24, 44–49. doi: 10.1097/01720610-201106000-00009
Kumar, S., Subhadra, S., Singh, B., and Panda, B. K. (2013). Hepatitis E virus: the current scenario. Int. J. Infect. Dis. 17, e228–e233. doi: 10.1016/j.ijid.2012.11.026
Kunwar, R. M., Uprety, Y., Burlakoti, C., Chowdhary, C. L., and Bussmann, R. W. (2009). Indigenous use and ethnopharmacology of medicinal plants in far-west Nepal. Ethnobot. Res. Appl. 7, 5–28. doi: 10.17348/era.7.0.5-28
Kuo, G., Choo, Q. L., Alter, H. J., Gitnick, G. L., Redeker, A. G., Purcell, R. H., et al. (1989). An assay for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitis. Science 244, 362–364. doi: 10.1126/science.2496467
Lauer, B. J., and Spector, N. D. (2011). Hyperbilirubinemia in the newborn. Pediatr. Rev. 32, 341–349. doi: 10.1542/pir.32-8-341
Lee, H. H., Choi, M.-G., and Hasan, T. (2017). Application of photodynamic therapy in gastrointestinal disorders: an outdated or re-emerging technique? Korean J. Intern. Med. 32, 1. doi: 10.3904/kjim.2016.200
Lev, E., and Amar, Z. (2002). Ethnopharmacological survey of traditional drugs sold in the Kingdom of Jordan. J. Ethnopharmacol. 82, 131–145. doi: 10.1016/S0378-8741(02)00182-4
Lick, D. E., and Brendle, T. R. (1923). “Plant names and plant lore among the Pennsylvania Germans,” in Proceedings and Address of the Pennsylvania German Society, Vol. 33 (Lancaster, PA: The Society), 280.
Louie, S., Gamble, C. N., and Cross, C. E. (1986). Penicillamine associated pulmonary hemorrhage. J. Rheumatol. 13, 963–966.
Maisels, M. J. (2000). The Clinical Approach to the Jaundiced Newborn. Neonatal Jaundice. Amsterdam: Harwood Academic Publishers.
Malla, B., Gauchan, D. P., and Chhetri, R. B. (2015). An ethnobotanical study of medicinal plants used by ethnic people in Parbat district of western Nepal. J. Ethnopharmacol. 165, 103–117. doi: 10.1016/j.jep.2014.12.057
Manning, D., Todd, P., Maxwell, M., and Platt, M. J. (2007). Prospective surveillance study of severe hyperbilirubinaemia in the newborn in the UK and Ireland. Arch. Dis. Child. Fetal Neonatal Ed. 92, F342–F346. doi: 10.1136/adc.2006.105361
Mathur, A., and Joshi, H. (2013). Ethnobotanical studies of the Tarai Region of Kumaun, Uttarakhand, India. Ethnobot. Res. Appl. 11, 175–203. doi: 10.17348/era.11.0.174-203
Memon, N., Weinberger, B. I., Hegyi, T., and Aleksunes, L. M. (2016). Inherited disorders of bilirubin clearance. Pediatr. Res. 79, 378–386. doi: 10.1038/pr.2015.247
Nadembega, P., Boussim, J. I., Nikiema, J. B., Poli, F., and Antognoni, F. (2011). Medicinal plants in Baskoure, Kourittenga Province, Burkina Faso: an ethnobotanical study. J. Ethnopharm. 133, 378–395. doi: 10.1016/j.jep.2010.10.010
Narayanan, C. S., and Behari, M. (1999). Generalized myasthenia gravis following use of D-pencillamine in Wilson's disease. J. Assoc. Phys. India 47, 648.
Olds, C., and Oghalai, J. S. (2015). Audiologic impairment associated with bilirubin-induced neurologic damage. Semin. Fetal Neonatal Med. 20, 42–46. doi: 10.1016/j.siny.2014.12.006
Onocha, P. A., Oloyede, G. K., and Afolabi, Q. O. (2011). Phytochemical investigation, cytotoxicity and free radical scavenging activities of non-polar fractions of Acalypha hispida (leaves and twigs). EXCLI J. 10, 1–8. Available online at: http://pubmedcentralcanada.ca/pmcc/articles/PMC5109007/
Opaleye, O. O., Japhet, O. M., Adewumi, O. M., Omoruyi, E. C., Akanbi, O. A., Oluremi, A. S., et al. (2016). Molecular epidemiology of hepatitis D virus circulating in Southwestern Nigeria. Virol. J. 13, 61. doi: 10.1186/s12985-016-0514-6
Paindla, P., and Mamidala, E. (2014). Phytochemical and chromatographic studies in the leaves extract of Acalypha indica. Online Int. Interdisc. Res. J. 4, 175–182. Available online at: https://scholar.google.co.in/scholar?q=Phytochemical+and+chromatographic+studies+in+the+leaves+extract+of+Acalypha+indica&btnG=&hl=en&as_sdt=0%2C5
Panyaphu, K., Van On, T., Sirisa-Ard, P., Srisa-Nga, P., Chansakaow, S., and Nathakarnkitkul, S. (2011). Medicinal plants of the Mien (Yao) in Northern Thailand and their potential value in the primary healthcare of postpartum women. J. Ethnopharm. 135, 226–237. doi: 10.1016/j.jep.2011.03.050
Parler, M. C. (1962). Folk Beliefs from Arkansas, Vol. 15. Fayetteville, AR: University of Arkansas.
Parveen Upadhyay, B., Roy, S., and Kumar, A. (2007). Traditional uses of medicinal plants among the rural communities of Churu district in the Thar Desert, India. J. Ethnopharm. 113, 387–399. doi: 10.1016/j.jep.2007.06.010
Pashankar, D., and Schreiber, R. A. (2001). Jaundice in older children and adolescents. Pediatr. Rev. 22, 219–226. doi: 10.1542/pir.22-7-219
Peces, R., Riera, J. R., Arboleya, L. R., Lopez-Larrea, C., and Alvarez, J. (1987). Goodpasture's syndrome in a patient receiving penicillamine and carbimazole. Nephron 45, 316–320. doi: 10.1159/000184171
Petruzziello, A., Marigliano, S., Loquercio, G., and Cacciapuoti, C. (2016). Hepatitis C virus (HCV) genotypes distribution: an epidemiological up-date in Europe. Infect. Agents Cancer 11:53. doi: 10.1186/s13027-016-0099-0
Pickard, M. E., and Buley, R. C. (1945). The Midwest Pioneer, Hills Ills, Cures and Doctors. Crawfordsville, IN: R. E. Bantham.
Poduri, C. D. (2016). Jaundice: a brief historical perspective. Apollo Med. 13, 76–79. doi: 10.1016/j.apme.2014.05.014
Pohl, S., Zobel, J., and Moffat, A. (2010). “Extended boolean retrieval for systematic biomedical reviews,” in Proceedings of the Thirty-Third Australasian Conferenc on Computer Science – Vol. 102 (Darlinghurst: Australian Computer Society, Inc.), 117–126. Available online at: http://dl.acm.org/citation.cfm?id=1862199.1862212
Poonam, K., and Singh, G. S. (2009). Ethnobotanical study of medicinal plants used by the Taungya community in Terai Arc Landscape, India. J. Ethnopharm. 123, 167–176. doi: 10.1016/j.jep.2009.02.037
Puckett, N. N., Hand, W. D., Casetta, A., and Thiederman, S. D. (1981). Popular Beliefs and Superstitions: A Compendium of American Folklore from the Ohio Collection of Newbell Niles Puckett. Boston, MA: G. K. Hall.
Puri, P. (2014). Tackling the hepatitis B disease burden in India. J. Clin. Exp. Hepatol. 4, 312–319. doi: 10.1016/j.jceh.2014.12.004
Rai, P. K., and Lalramnghinglova, H. (2011). Ethnomedicinal plants of India with special reference to an Indo-Burma Hotspot Region: an overview. Ethnobot. Res. Appl. 9, 379–420. doi: 10.17348/era.9.0.379-420
Rajaei, P., and Mohamadi, N. (2012). Ethnobotanical study of medicinal plants of hezar mountain allocated in south east of Iran. Iran. J. Pharm. Res. 11, 1153–1167.
Rehecho, S., Uriarte-Pueyo, I., Calvo, J., Vivas, L. A., and Calvo, M. I. (2011). Ethnopharmacological survey of medicinal plants in Nor-Yauyos, a part of the Landscape Reserve Nor-Yauyos-Cochas, Peru. J. Ethnopharmacol. 133, 75–85. doi: 10.1016/j.jep.2010.09.006
Riva, M. A., Riva, E., Spicci, M., Strazzabosco, M., Giovannini, M., and Cesana, G. (2011). “The city of Hepar”: rituals, gastronomy, and politics at the origins of the modern names for the liver. J. Hepatol. 55, 1132–1136. doi: 10.1016/j.jhep.2011.05.011
Rizzetto, M., and Verme, G. (1985). Delta hepatitis—present status. J. Hepatol. 1, 187–193. doi: 10.1016/S0168-8278(85)80766-2
Roche, S. P., and Kobos, R. (2004). Jaundice in the adult patient. Am. Fam. Phys. 69, 299–304. doi: 10.1016/B978-0-323-05611-3/00019-7
Rokaya, M. B., Munzbergova, Z., and Timsina, B. (2010). Ethnobotanical study of medicinal plants from the Humla district of western Nepal. J. Ethnopharmacol. 130, 485–504. doi: 10.1016/j.jep.2010.05.036
Roy-Chowdhury, N., and Roy-Chowdhury, J. (2011). Classification and causes of jaundice or asymptomatic hyperbilirubinemia. UpToDate 1–11. Available online at: https://scholar.google.co.in/scholar?hl=en&q=Classification+and+causes+of++jaundice+or+asymptomatic+hyperbilirubinemia.&btnG=
Said, O., Khalil, K., Fulder, S., and Azaizeh, H. (2002). Ethnopharmacological survey of medicinal herbs in Israel, the Golan Heights and the West Bank region. J. Ethnopharmacol. 83, 251–265. doi: 10.1016/S0378-8741(02)00253-2
Sánchez, G. (2015). Processing strategies to inactivate hepatitis A virus in food products: a critical review. Compr. Rev. Food Sci. Food Saf. 14, 771–784. doi: 10.1111/1541-4337.12154
Santos, J. S. D., Kemp, R., Sankarankutty, A. K., Salgado Júnior, W., Souza, F. F., Teixeira, A. C., et al. (2008). Clinical and regulatory protocol for the treatment of jaundice in adults and elderly subjects: a support for the health care network and regulatory system. Acta Cirúrgica Brasileira 23, 133–142. doi: 10.1590/S0102-86502008000700022
Šarić-Kundalić, B., Dobeš, C., Klatte-Asselmeyer, V., and Saukel, J. (2011). Ethnobotanical survey of traditionally used plants in human therapy of east, north and north-east Bosnia and Herzegovina. J. Ethnopharmacol. 133, 1051–1076. doi: 10.1016/j.jep.2010.11.033
Schlosser, B. J., Pirigyi, M., and Mirowski, G. W. (2011). Oral manifestations of hematologic and nutritional diseases. Otolaryngol. Clin. North Am. 44, 183–203. doi: 10.1016/j.otc.2010.09.007
Schmid, R. (2001). History of viral hepatitis: a tale of dogmas and misinterpretations. J. Gastroenterol. Hepatol. 16, 718–722. doi: 10.1046/j.1440-1746.2001.02509.x
Seebaluck, R., Gurib-Fakim, A., and Mahomoodally, F. (2015). Medicinal plants from the genus Acalypha (Euphorbiaceae)-A review of their ethnopharmacology and phytochemistry. J. Ethnopharmacol. 159, 137–157. doi: 10.1016/j.jep.2014.10.040
Seeger, C., and Mason, W. S. (2015). Molecular biology of hepatitis B virus infection. Virology 479, 672–686. doi: 10.1016/j.virol.2015.02.031
Sharma, H. K., Chhangte, L., and Dolui, A. K. (2001). Traditional medicinal plants in Mizoram, India. Fitoterapia 72, 146–161. doi: 10.1016/S0367-326X(00)00278-1
Sharma, J., Gairola, S., Gaur, R. D., and Painuli, R. M. (2012). The treatment of jaundice with medicinal plants in indigenous communities of the Sub-Himalayan region of Uttarakhand, India. J. Ethnopharmacol. 143, 262–291. doi: 10.1016/j.jep.2012.06.034
Sharma, P., and Samant, S. S. (2014). Diversity, distribution and indigenous uses of medicinal plants in Parbati Valley of Kullu district in Himachal Pradesh, Northwestern Himalaya. Asian J. Adv. Basic Sci. 2, 77–98. doi: 10.4172/2332-2543.1000177
Singh, K. N., and Lal, B. (2008). Ethnomedicines used against four common ailments by the tribal communities of Lahaul-Spiti in western Himalaya. J. Ethnopharmacol. 115, 147–159. doi: 10.1016/j.jep.2007.09.017
Singhal, V., Bora, D., and Singh, S. (2009). Hepatitis B in health care workers: Indian scenario. J. Lab. Phys. 1, 41–48. doi: 10.4103/0974-2727.59697
Smith, W. R. (1929). “Animals and plants in Oklahoma folk cures,” in Folk Say- A Regional Miscellany, ed B. A. Botkin (Norman, OK: Folklore Society), 74.
Stoll, B. J., and Kliegman, R. M. (2004). “Jaundice and hyperbilirubinemia in the newborn,” in Nelson Textbook of Pediatrics, eds R. E. Behrman and R. M. Kliegman (Philadelphia, PA: WB Saunders), 592–596.
Subcommittee on Hyperbilirubinemia American Academy of Pediatrics (2004). Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114:297. doi: 10.1542/peds.114.1.297
Sureau, C., and Negro, F. (2016). The hepatitis delta virus: replication and pathogenesis. J. Hepatol. 64, S102–S116. doi: 10.1016/j.jhep.2016.02.013
Tajiri, K., and Shimizu, Y. (2016). New horizon for radical cure of chronic hepatitis B virus infection. World J. Hepatol. 8:863. doi: 10.4254/wjh.v8.i21.863
Teive, H. A. G., Barbosa, E. R., and Lees, A. J. (2017). Wilson's disease: the 60th anniversary of Walshe's article on treatment with penicillamine. Arq. Neuropsiquiatr. 75, 69–71. doi: 10.1590/0004-282x20160166
Teklehaymanot, T., Giday, M., Medhin, G., and Mekonnen, Y. (2007). Knowledge and use of medicinal plants by people around Debre Libanos monastery in Ethiopia. J. Ethnopharmacol. 111, 271–283. doi: 10.1016/j.jep.2006.11.019
Thambiraj, J., and Paulsamy, S. (2011). Antimicrobial screening of stem extract of the folklore medicinal plant, Acalypha fruticosa Forssk. Int. J. Pharm. Pharm. Sci. 3, 285–287. Available online at: https://scholar.google.co.in/scholar?hl=en&q=Antimicrobial+screening+of+stem+extract+of+the+folklore+medicinal+plant%2C+Acalypha+fruticosa+Forssk&btnG=
Thambiraj, J., Paulsamy, S., and Sevukaperumal, R. (2012). Evaluation of in vitro antioxidant activity in the traditional medicinal shrub of western districts of Tamilnadu, India, Acalypha fruticosa Forssk. (Euphorbiaceae). Asian Pac. J. Trop. Biomed. 2, S127–S130. doi: 10.1016/S2221-1691(12)60142-7
Thomas, E., Yoneda, M., and Schiff, E. R. (2015). Viral hepatitis: past and future of HBV and HDV. Cold Spring Harb. Perspect. Med. 5:a021345. doi: 10.1101/cshperspect.a021345
Thomas, R. E., Lorenzetti, D. L., and Spragins, W. (2013). Mortality and morbidity among military personnel and civilians during the 1930s and World war II from transmission of hepatitis during yellow fever vaccination: systematic review. Am. J. Public Health 103, e16–e29. doi: 10.2105/AJPH.2012.301158
Togola, A., Diallo, D., Dembélé, S., Barsett, H., and Paulsen, B. S. (2005). Ethnopharmacological survey of different uses of seven medicinal plants from Mali, (West Africa) in the regions Doila, Kolokani and Siby. J. Ethnobiol. Ethnomed. 1:7. doi: 10.1186/1746-4269-1-7
Tong, S., and Revill, P. (2016). Overview of hepatitis B viral replication and genetic variability. J. Hepatol. 64, S4–S16. doi: 10.1016/j.jhep.2016.01.027
Trepo, C. (2014). A brief history of hepatitis milestones. Liver Int. 34(Suppl. 1), 29–37. doi: 10.1111/liv.12409
Ullah, S., Rahman, K., and Hedayati, M. (2016). Hyperbilirubinemia in neonates: types, causes, clinical examinations, preventive measures and treatments: a narrative review article. Iran. J. Public Health 45, 558.
Uniyal, S. K., Singh, K. N., Jamwal, P., and Lal, B. (2006). Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. J. Ethnobiol. Ethnomed. 2:14. doi: 10.1186/1746-4269-2-14
Upadhyay, B., Parveen Dhaker, A. K., and Kumar, A. (2010). Ethnomedicinal and ethnopharmaco-statistical studies of Eastern Rajasthan, India. J. Ethnopharmacol. 129, 64–86. doi: 10.1016/j.jep.2010.02.026
Voitkun, V., Zhitkovich, A., and Costa, M. (1998). Cr(III)-mediated crosslinks of glutathione or amino acids to the DNA phosphate backbone are mutagenic in human cells. Nucleic Acids Res. 26, 2024–2030. doi: 10.1093/nar/26.8.2024
Vreman, H. J., Ekstrand, B. C., and Stevenson, D. K. (1993). Selection of metalloporphyrin heme oxygenase inhibitors based on potency and photoreactivity. Pediatr. Res. 33, 195–200. doi: 10.1203/00006450-199302000-00021
Wahab, M. A., Yousaf, M., and Hossain, M. E. (2004). Some indigenous medicinal knowledge for treating jaundice in Chittagong hill tracts Bangladesh. Hamdard Med. 47, 55–58. Available online at: https://scholar.google.co.in/scholar?q=Some+indigenous+medicinal++knowledge+for+treating+jaundice+in+Chittagong+hill+tracts+Bangladesh&btnG=&hl=en&as_sdt=0%2C5
Whitehead, M. W., Hainsworth, I., and Kingham, J. G. C. (2001). The causes of obvious jaundice in South West Wales: perceptions versus reality. Gut 48, 409–413. doi: 10.1136/gut.48.3.409
Wong, D., Purcell, R., Sreenivasan, M. A., Prasad, S. R., and Pavri, K. (1980). Epidemic and endemic hepatitis in India: evidence for a non-A, non-B hepatitis virus aetiology. Lancet 316, 876–879. doi: 10.1016/S0140-6736(80)92045-0
Wong, V. W.-S., Law, M.-Y., Hui, A. Y., Lo, A. O.-S., Li, C.-Y., Soo, M.-T., et al. (2005). A hospital clinic-based survey on traditional Chinese medicine usage among chronic hepatitis B patients. Complem. Ther. Med. 13, 175–182. doi: 10.1016/j.ctim.2005.04.006
Yang, S. H., and Lu, C. F. (1984). Effects of decoction of Artemisia, Rheum, Gardenia, Coptidis and Rhizoma on neonatal jaundice in Chinese newborn infants. J. Chin. Child Med. 25, 144–148.
Yeung, C. Y., Leung, C. S., and Chen, Y. Z. (1993). An old traditional herbal remedy for neonatal jaundice with a newly identified risk. J. Paediatr. Child Health 29, 292–294. doi: 10.1111/j.1440-1754.1993.tb00514.x
Yin, J., Wennberg, R. P., and Miller, M. (1993). Induction of hepatic bilirubin and drug metabolizing enzymes by individual herbs present in the traditional Chinese medicine, yin zhi huang. Dev. Pharmacol. Therap. 20, 186–194.
Zeitoun, A. A., Elhagrasy, H. F., and Abdelsatar, D. M. (2013). Predictive value of umbilical cord blood bilirubin in neonatal hyperbilirubinemia. Egypt. Pediatr. Assoc. Gaz. 61, 23–30. doi: 10.1016/j.epag.2013.04.006
Zhang, F., Tang, X., Garcia, T., Lok, A. S., Wang, Y., Jia, H., et al. (2017). Characterization of contrasting features between hepatitis B virus genotype A and genotype D in small envelope protein expression and surface antigen secretion. Virology 503, 52–61. doi: 10.1016/j.virol.2017.01.009
Keywords: jaundice, bilirubin, medicinal plants, ethnopharmacology, traditional use, metalloporphyrin
Citation: Tewari D, Mocan A, Parvanov ED, Sah AN, Nabavi SM, Huminiecki L, Ma ZF, Lee YY, Horbańczuk JO and Atanasov AG (2017) Ethnopharmacological Approaches for Therapy of Jaundice: Part I. Front. Pharmacol. 8:518. doi: 10.3389/fphar.2017.00518
Received: 17 February 2017; Accepted: 24 July 2017;
Published: 15 August 2017.
Edited by:
Kalin Yanbo Zhang, University of Hong Kong, Hong KongReviewed by:
Gokhan Zengin, Selçuk University, TurkeyArmando Caceres, University of San Carlos of Guatemala, Guatemala
Copyright © 2017 Tewari, Mocan, Parvanov, Sah, Nabavi, Huminiecki, Ma, Lee, Horbańczuk and Atanasov. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atanas G. Atanasov, YS5hdGFuYXNvdi5tYWlsYm94QGdtYWlsLmNvbQ==
†These authors have contributed equally to this work.
 Devesh Tewari
Devesh Tewari Andrei Mocan
Andrei Mocan Emil D. Parvanov4
Emil D. Parvanov4 Archana N. Sah
Archana N. Sah Seyed M. Nabavi
Seyed M. Nabavi Zheng Feei Ma
Zheng Feei Ma Yeong Yeh Lee
Yeong Yeh Lee Jarosław O. Horbańczuk
Jarosław O. Horbańczuk Atanas G. Atanasov
Atanas G. Atanasov