- Behavioral Studies, Graduate School, The Academic College at Wingate, Wingate, Israel
Major depression disorder is most commonly treated with antidepressants. However, due to their side effects clinicians seek non-pharmacologic options, and one of these is exercise. The literature on the benefits of exercise for depression is extensive. Nevertheless, two recent reviews focusing on antidepressants vs. other therapies as a basis for clinical practice guidelines recommended mainly antidepressants, excluding exercise as a viable choice for treatment of depression. The aim of this perspective is to analyze the literature exploring the reasons for this discrepancy. Two categories of publications were examined: randomized controlled trials (RCTs) and meta-analyses or systematic reviews. Based on this reassessment, RCTs comparing exercise to antidepressants reported that exercise and antidepressants were equally effective. RCTs comparing exercise combined with antidepressants to antidepressants only reported a significant improvement in depression following exercise as an adjunctive treatment. Almost all the reviews examining exercise vs. other treatments of depression, including antidepressants, support the use of exercise in the treatment of depression, at least as an adjunctive therapy. The two reviews examining pharmacologic vs. non-pharmacologic therapies as a basis for clinical practice guidelines examined limited evidence on exercise vs. antidepressants. In addition, it is possible that academics and health care practitioners are skeptical of viewing exercise as medicine. Maybe, there is a reluctance to accept that changes in lifestyle as opposed to pharmacological treatment can alter biological mechanisms. Longitudinal studies are needed for assessing the effectiveness of exercise in real clinical settings, as well as studies exploring dose-response relationship between exercise and depression.
Introduction
The perception of exercise as medicine has been discussed in relation to health conditions such as cognitive decline (e.g., Nagamatsu et al., 2014), cancer (e.g., Lin et al., 2016), cardiac rehabilitation (e.g., Almodhy et al., 2016), schizophrenia (e.g., Firth et al., 2015), alcohol use disorders (e.g., Hallgren et al., 2017), and all-cause mortality (e.g., Eklund et al., 2016). One meta-epidemiological study on mortality outcomes concluded that in a number of health conditions, such as heart failure, stroke, and diabetes, exercise and various pharmacological treatments are similar in their potential to extend longevity (Naci and Ioannidis, 2013). Thus, exercise interventions should be considered as a viable alternative to, or combination with, drug therapy (Naci and Ioannidis, 2013). It is therefore not surprising that comparative assessments of exercise and drug treatments were performed for some conditions, such as sleep disorders (Buman and King, 2010), chronic pain (Ambrose and Golightly, 2015), and mental health (Firth et al., 2016).
Probably more than for other health conditions, comparative benefits of exercise and pharmacologic treatments have been examined and discussed in relation to depression (e.g., Stubbs et al., 2015; Gartlehner et al., 2016). According to the WHO (World Health Organization), depression is the leading cause of disability worldwide (WHO, 2016 http://www.who.int/mediacentre/factsheets/fs369/en/).
Major depression disorder (MDD) is most commonly treated with antidepressant medication, where second-generation antidepressants are the most commonly prescribed drugs (Agency for Healthcare Research and Quality [AHRQ], 2016). However, many patients do not respond to antidepressant medications, or experience side effects (Gartlehner et al., 2016). In addition, increasing evidence indicated a large placebo response, making it more challenging for novel medications to demonstrate their effectiveness (Rutherford et al., 2012). Therefore, clinicians and patients seek non-pharmacologic options for treating depression – and one of them is physical exercise (e.g., Martiny et al., 2012).
The literature on the benefits of exercise for both minor and major depressive symptoms is extensive, with exceptionally numerous reviews perhaps outnumbering randomized controlled trials (RCTs) (e.g., Mead et al., 2009; Rethorst et al., 2009; Krogh et al., 2011; Rimer et al., 2012; Robertson et al., 2012; Cooney et al., 2013; Danielsson et al., 2013; Silveira et al., 2013; Josefsson et al., 2014; Mura et al., 2014; Knapen et al., 2015; Nyström et al., 2015; Stubbs et al., 2015; Kvam et al., 2016; Schuch et al., 2016b). In addition to exercise, additional studies (Adamson et al., 2016) and reviews (Zhai et al., 2015; Hallgren et al., 2016; Liu et al., 2016; Schuch et al., 2017) in recent years examined the relationship between sedentary behavior, physical activity, and depression. Interestingly, a recent study has shown that a 1-week of forced sedentary behavior may cause bad mood or depression in active individuals (Edwards and Loprinzi, 2016). Furthermore, it has been found that people with depression are at increased risk of sedentary behavior (Dugan et al., 2015; Schuch et al., 2017), which may cause cardiovascular diseases and metabolic syndromes (Gardner-Sood et al., 2015).
Along with RCTs and reviews examining exercise as a treatment for depression, there have been attempts to explore the mediating biological mechanisms explaining the reduction in depression in MDD as a result of exercise (Kandola et al., 2016; Schuch et al., 2016a). One explanation is hippocampus plasticity (Kandola et al., 2016). It has been shown that the hippocampus in depressed individuals may be affected by neuron atrophy (Mendez-David et al., 2013). Aerobic exercise has the potential to promote neuroplasticity and thus facilitate the function of the hippocampus (Erickson et al., 2011). Through increasing neuroplasticity in the hippocampus, it may be possible to generate structural changes that affect the region’s functioning and contribute to the alleviation of cognitive malfunction in MDD (Kandola et al., 2016). It has also been hypothesized that there is a relationship between the decline in neurogenesis and depressed mood (Duman et al., 1997). Based on the above, it was concluded that the anti-depressive effects of exercise are due to physiological changes that result in hippocampal neurogenesis (Ernst et al., 2006).
One mechanisms by which exercise could potentially facilitate this neurogenesis is the brain-derived neurotrophic factor (BDNF). A growing number of studies, performed both on animal models of depression and on depressed humans, have focused on the neurotrophic hypothesis of depression (Neto et al., 2011). According to this hypothesis, several alterations in the levels of neurotrophins, particularly of the BDNF, might produce the structural and neurochemical changes that underlie depression (Neto et al., 2011). Both pharmacological and non-pharmacological interventions for depression have been shown to produce changes in the levels of neurotrophins. BDNF increases have been reported to follow the administration of antidepressant drugs (Czubak et al., 2009), which suggests that BDNF expression may mediate the action of antidepressants. Furthermore, when exercise is combined with antidepressants, BDNF levels were found to increase in as little as two days, compared with two weeks with antidepressants alone (Russo-Neustadt et al., 2001).
Another mechanism for enhancing neurogenesis is serotonin. Adaptations in the serotonergic system may serve as potential facilitators of the antidepressant effects of exercise (Schuch et al., 2016a). As a result, antidepressant medications available today target the release and reuptake of serotonin. Exercise increases tryptophan hydroxylase (Chaouloff et al., 1989), which is necessary for serotonin synthesis. Results of animal studies point to a relationship between serotonin elevation and neurogenesis (Brezun and Daszuta, 2000).
According to Schuch et al. (2016a), it is possible that the antidepressant effect of exercise is caused by the interaction of several neurobiological mechanisms rather than by one mechanism exclusively. It is certain that exercise generates both acute and chronic responses, mainly in hormones, neurotrophines, and inflammation biomarkers (Schuch et al., 2016a).
It is, therefore, not surprising that quite a few attempts have been made to compare the effects of exercise to other treatments, including drug treatments, in various depressive disorders, specifically MDD. Four reviews on this topic were published in 2016. Two meta-analyses examining the efficacy of exercise as a treatment for major depression concluded that exercise as a treatment for depression can be recommended as a stand-alone treatment or as an adjunct to antidepressant medication (Kvam et al., 2016), and that exercise can be considered an evidence-based treatment for the management of depression (Schuch et al., 2016b). On the other hand, two systematic reviews comparing antidepressants to other therapies – including exercise – as a basis for clinical practice guidelines for depression, disregarded exercise in their recommendations. One concluded that “The American College of Physicians recommends that clinicians select between either cognitive behavioral therapy or second-generation antidepressants to treat patients with major depressive disorder…” (Qaseem et al., 2016, p. 355), and the other that “given comparable efficacy, cognitive behavioral therapy and antidepressants are both viable choices for initial MDD treatment” (Gartlehner et al., 2016, p. 338). The aim of this perspective is to analyze the available literature on the efficacy of exercise vs. antidepressants in the treatment of depression and to suggest a few explanations for this discrepancy.
Publications Examined
Two categories of publications were examined: RCTs (Table 1) and meta-analyses or systematic reviews (Table 2).
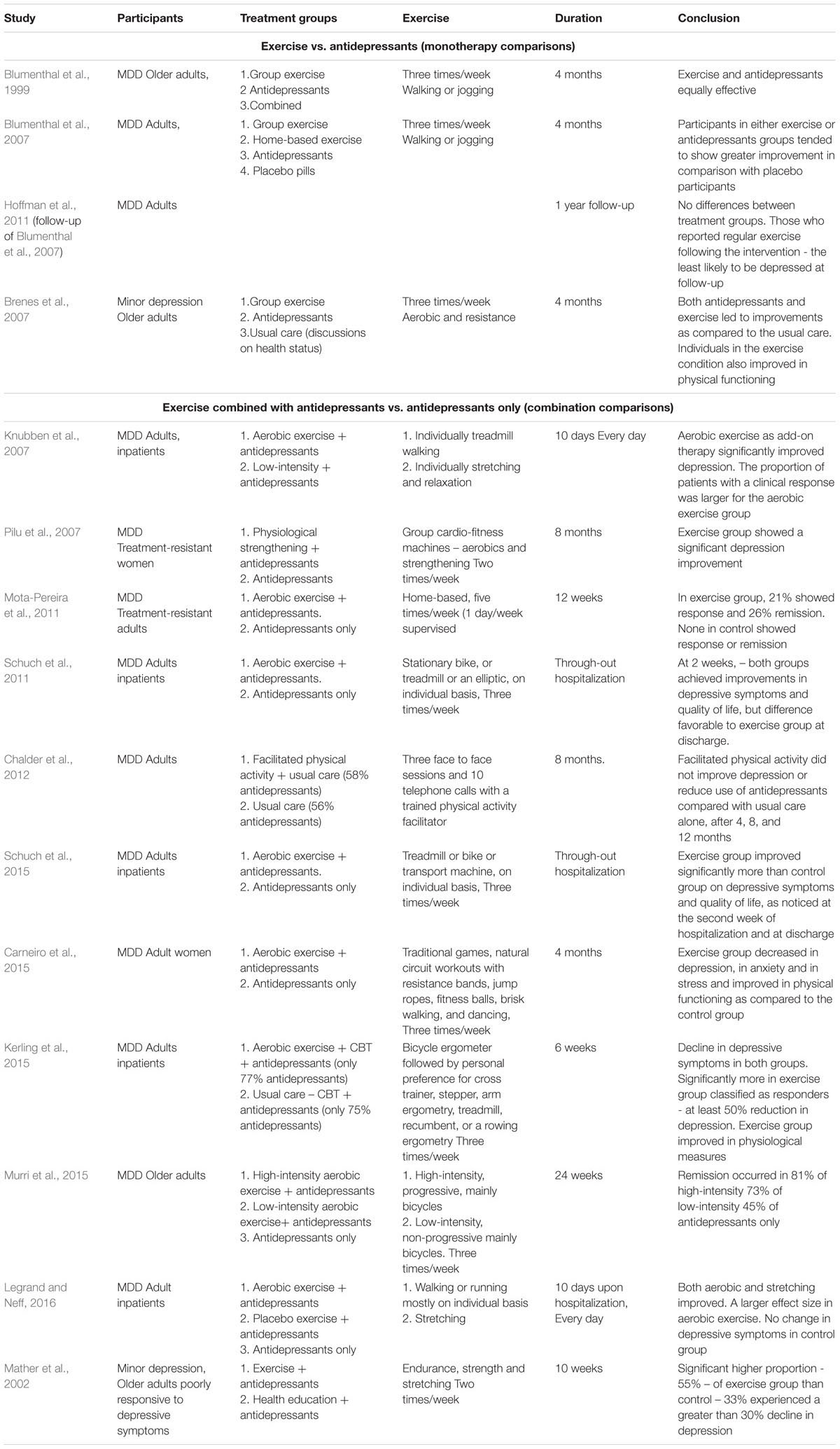
TABLE 1. Randomized controlled trials (RCTs) comparing exercise to antidepressants in the treatment of depression.
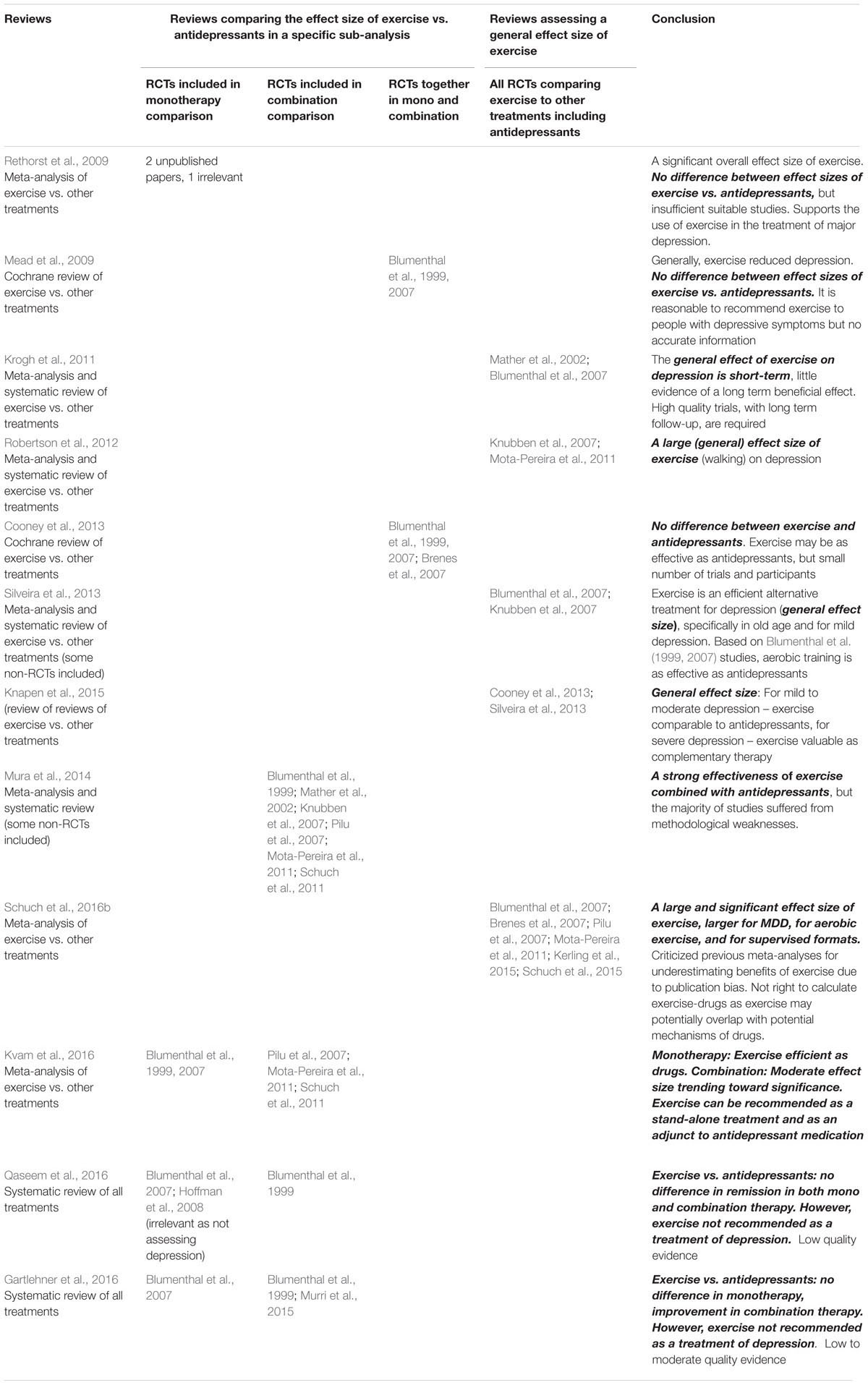
TABLE 2. A map of RCTs in reviews comparing exercise to antidepressants in the treatment of depression, and the conclusions regarding the effect size of exercise.
All RCTs published in 1999–2016 that are included in systematic and/or meta-analyses reviews published from 2009 to 2016 were examined, as well as two recent RCTs found in PubMed search. RCTs were excluded if they assessed participants with additional co-morbid diagnoses, such as cardiovascular diseases (e.g., Blumenthal et al., 2012), or if they assessed two kinds of interventions as add-on therapy – for example chronotherapy vs. exercise (Martiny et al., 2012). One group of RCTs compared exercise to antidepressants – monotherapy comparisons, and the other compared exercise combined with antidepressants to antidepressants only – combination comparisons (Table 1).
As a collection of RCTs does not reflect a general effect size, meta-analyses, Cochrane reviews and systematic reviews providing an effect size of exercise vs. antidepressants in the treatment of depression were examined. As a large number of meta-analyses and other reviews were conducted in the last decade, it was decided to screen only reviews from the last seven years (2009–2016). Interestingly, in spite of the large number of reviews, none of them focused solely on exercise vs. antidepressants. One group compared exercise to other treatments of depression, including antidepressants, and the other compared antidepressants to other therapies, including exercise. More specifically, the present review investigated: (1) whether comparisons were conducted specifically between exercise and antidepressants (as opposed to exercise vs. all other treatments together, or antidepressants vs. all other treatments together), (2) which RCTs comparing exercise to antidepressants were included in these reviews, (3) which conclusions were drawn from these comparisons, and (4) whether all published RCTs conducting such comparisons were included in the reviews.
Summary and Conclusions of the Findings
Randomized Controlled Trials
Exercise vs. antidepressants – monotherapy comparisons (Table 1)
Three RCTs compared 4 months of exercise to antidepressants– two for MDD (Blumenthal et al., 1999, 2007) and one for minor depression (Brenes et al., 2007). Two were conducted on older adults (Blumenthal et al., 1999; Brenes et al., 2007). One study (Hoffman et al., 2011) was a follow-up to a previous study (Blumenthal et al., 2007). The Blumenthal et al. (1999, 2007) studies included aerobic exercise, and the Brenes study a combination of aerobic and resistance exercises.
Conclusion: All these studies reported that exercise and standard antidepressant treatments were equally effective.
Exercise combined with antidepressants vs. antidepressants only – combination comparisons (Table 1)
Eleven RCTs compared exercise as an adjunctive treatment to antidepressants (combination comparisons) – 10 for MDD and one for minor depression (Table 1). The duration of the exercise period varied from 10 days (Knubben et al., 2007; Legrand and Neff, 2016), to 6 weeks (Kerling et al., 2015), 10 weeks (Mather et al., 2002), 3 months (Mota-Pereira et al., 2011), 4 months (Carneiro et al., 2015), 6 months (Murri et al. (2015), 8 months (Pilu et al., 2007), 12 months (Chalder et al., 2012), to throughout a hospitalization period (undefined time period) (Schuch et al., 2011, 2015). Control groups included antidepressants only (Mather et al., 2002; Pilu et al., 2007; Mota-Pereira et al., 2011; Schuch et al., 2011, 2015; Chalder et al., 2012; Carneiro et al., 2015; Kerling et al., 2015), light exercise with both exercise groups receiving antidepressants (Knubben et al., 2007; Legrand and Neff, 2016), and antidepressants only (Murri et al., 2015). The exercise mode included mostly aerobics (Knubben et al., 2007; Mota-Pereira et al., 2011; Schuch et al., 2011, 2015; Kerling et al., 2015; Murri et al., 2015; Legrand and Neff, 2016) or aerobic and strength (Pilu et al., 2007); aerobic, strength, and stretching exercises (Mather et al., 2002); aerobics and strength exercises, games and dancing (Carneiro et al., 2015), and facilitated physical activity chosen and performed individually by participants (Chalder et al., 2012). The studies using exercise in a control group used light stretching (Knubben et al., 2007; Legrand and Neff, 2016) and low-intensity aerobics (Murri et al., 2015). Most studies assessed adults in general; only two studies investigated older adults (Mather et al., 2002; Murri et al., 2015).
Of special interest are the studies using exercise placebo groups as a control group, in which improvements were observed in the aerobic exercise as compared to stretching (Knubben et al., 2007; Legrand and Neff, 2016), and the Murri et al. (2015) study that showed the greatest improvement in high-intensity aerobics, followed by low intensity aerobics, followed by antidepressants only. The Chalder et al. (2012) study only gave guidance about exercise but did not provide an exercise program.
Conclusion: All studies but one (Chalder et al., 2012) informed that patients using exercise as an adjunctive treatment for depression showed a significant depressive improvement after the exercise period, and/or that the proportion of patients with a clinical response was larger for the exercise group than the control.
Meta-Analyses or Systematic Reviews
Table 2 presents a map of RCTs comparing exercise to antidepressants in the meta-analyses or systematic reviews.
Almost all reviews examining exercise vs. other treatments of depression, including antidepressants, support the use of exercise in the treatment of depression, at least as an add-on therapy. Earlier reviews, which included only a few RCTs, were more careful in actually recommending exercise. For example, one review stated that “it is reasonable to recommend exercise…” (Mead et al., 2009, p. 14). Another review pointed out that “… exercise may be as effective as psychological or pharmacological treatments…” (Cooney et al., 2013, p. 35). Later reviews were more conclusive, claiming “a strong effectiveness of exercise combined with antidepressants” (Mura et al., 2014, p. 503); “Overall, our results provide robust evidence that exercise can be considered an evidence-based treatment for the management of depression.” (Schuch et al., 2016b, p. 47); and “Physical exercise is an effective intervention for depression. It also could be a viable adjunct treatment in combination with antidepressants” (Kvam et al., 2016, p. 67).
On the other hand, the two recent reviews from 2016 assessing antidepressants vs. other treatments of depression, including exercise, did not recommend exercise for the treatment of depression (Gartlehner et al., 2016; Qaseem et al., 2016). However, when comparing exercise to antidepressants, these reviews examined mainly the Blumenthal et al. (1999, 2007) studies, excluding other RCTs comparing exercise to antidepressants that were included in other recent reviews.
Discussion
Exercise vs. pharmacologic treatment of depression in the clinical practice guideline of the American College of Physicians – is it evidence-based?
It appears that the reviews examining pharmacologic vs. non-pharmacologic treatments of depression as a basis for clinical practice guidelines examined limited evidence on exercise vs. antidepressants, and thus disregarded exercise as a viable choice for treating depression as a stand-alone treatment or as an add-on therapy. This position is contrary to the reviews examining exercise vs. other treatments for depression, including antidepressants, which generally recommend exercise as a stand-alone and/or as adjunctive treatment for depression. The evidence is even greater when considering two additional recent well-designed RCTs not included in any of the reviews (possibly because they were published later than the RCTs mentioned in the reviews) which pointed out the effect of exercise as a complement to antidepressant medication (Carneiro et al., 2015; Legrand and Neff, 2016) (Table 1). Furthermore, while the underlying biological mechanisms mediating between exercise and reduced depressive symptoms are not entirely clear, it is apparent that exercise induces both acute and chronic responses, particularly in hormones, neurotrophines, and inflammation biomarkers, and that there is an association between hippocampus neurogenesis as a result of exercise and depressive symptoms’ improvement (Schuch et al., 2016a).
Is exercise medicine for the treatment of depression?
Based on the present review, which examined most or all RCTs published in 1999–2016, and most or all meta-analyses/systematic reviews published in 2009–2016, it can be stated that exercise is an evidenced-based medicine for depression – at least as an add-on to antidepressants. Furthermore, people with depression are at increased risk of sedentary behavior (Dugan et al., 2015; Schuch et al., 2017), which may cause cardiovascular diseases and metabolic syndrome (Gardner-Sood et al., 2015). Thus, exercise contributes to the physical health in addition to mental health. It is also worth mentioning the adverse effects commonly associated with drugs, including constipation, diarrhea, dizziness, headache, insomnia, nausea, adverse sexual events, and somnolence (Qaseem et al., 2016), which may further support the use of exercise as a viable alternative or adjunctive pharmacotherapy.
It is unclear why exercise was disregarded as a viable choice for treating depression in the clinical practice guidelines recommended in the two recent reviews (Gartlehner et al., 2016; Qaseem et al., 2016). Is there a reluctance among academics and health care practitioners to view exercise as medicine? Do they caution that there is no strong evidence to suggest that modifiable lifestyle factors as opposed to pharmacological treatment can alter biological mechanisms in similar pathways or similar dynamics to biochemical interventions?
Interestingly, this argument was raised by Nagamatsu et al. (2014) regarding the effect of exercise on the brain and cognition in old age. These authors made the case that despite the large and consistent pool of evidence generated over the past five decades linking exercise to improved cognitive functions in older adults, skepticism remains and health practitioners continue to hinder the adoption of exercise as a legitimate medical strategy for the prevention of cognitive decline.
Future directions of research should include dose-response interventions to determine the precise dose of exercise required to maximize the benefits for depression. In addition, more studies are needed to inquire the underlying molecular and cellular mechanisms mediating between exercise and depression. Furthermore, another important issue for assessing the benefits of exercise for depression is its effectiveness as opposed to efficacy (Beedie et al., 2016). While efficacy refers to the ability of exercise to achieve the desired effect under well controlled circumstances, effectiveness refers to the ability of exercise to affect depression in real life situations. Therefore, longitudinal observational studies exploring the benefits of exercise in depression are needed, which assess adherence issues as well as economic and professional matters.
Author Contributions
The author confirms being the sole contributor of this work and approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Adamson, B. C., Yang, Y., and Motl, R. W. (2016). Association between compliance with physical activity guidelines, sedentary behavior and depressive symptoms. Prev. Med. 91, 152–157. doi: 10.1016/j.ypmed.2016.08.020
Agency for Healthcare Research and Quality [AHRQ] (2016). Effective Health Care Program. Rockville, MD: Agency for Healthcare Research and Quality.
Almodhy, M., Ingle, L., and Sandercock, G. R. (2016). Effects of exercise-based cardiac rehabilitation on cardiorespiratory fitness: a meta-analysis of UK studies. Int. J. Cardiol. 221, 644–651. doi: 10.1016/j.ijcard.2016.06.101
Ambrose, K. R., and Golightly, Y. M. (2015). Physical exercise as non-pharmacological treatment of chronic pain: why and when. Best Pract. Res. Clin. Rheumatol. 29, 120–130. doi: 10.1016/j.berh.2015.04.022
Beedie, C., Mann, S., Jimenez, A., Kennedy, L., Lane, A. M., Domone, S., et al. (2016). Death by effectiveness: exercise as medicine caught in the efficacy trap! Br. J. Sports Med. 50, 323–324. doi: 10.1136/bjsports-2014-094389
Blumenthal, J. A., Babyak, M. A., Doraiswamy, P. M., Watkins, L., Hoffman, B. M., Barbour, K. A., et al. (2007). Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom. Med. 69, 587–596. doi: 10.1097/PSY.0b013e318148c19a
Blumenthal, J. A., Babyak, M. A., Moore, K. A., Craighead, W. E., Herman, S., Khatri, P., et al. (1999). Effects of exercise training on older patients with major depression. Arch. Intern. Med. 159, 2349–2356. doi: 10.1001/archinte.159.19.2349
Blumenthal, J. A., Babyak, M. A., O’Connor, C., Keteyian, S., Landzberg, J., Howlett, J., et al. (2012). Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA 308, 465–474. doi: 10.1001/jama.2012.8720
Brenes, G. A., Williamson, J. D., Messier, S. P., Rejeski, W. J., Pahor, M., Ip, E., et al. (2007). Treatment of minor depression in older adults: a pilot study comparing sertraline and exercise. Aging Ment. Health 11, 61–68. doi: 10.1080/13607860600736372
Brezun, J., and Daszuta, A. (2000). Serotonin may stimulate granule cell proliferation in adult hippocampus, as observed in rats grafted with foetal raphe neurons. Eur. J. Neurosci. 12, 391–396. doi: 10.1046/j.1460-9568.2000.00932.x
Buman, M. P., and King, A. C. (2010). Exercise as a treatment to enhance sleep. Am. J. Lifestyle Med. 4, 500–514. doi: 10.1177/1559827610375532
Carneiro, L. S., Fonseca, A. M., Vieira-Coelho, M. A., Mota, M. P., and Vasconcelos-Raposo, J. (2015). Effects of structured exercise and pharmacotherapy vs. pharmacotherapy for adults with depressive symptoms: a randomized clinical trial. J. Psychiatr. Res. 71, 48–55. doi: 10.1016/j.jpsychires.2015.09.007
Chalder, M., Wiles, N. J., Campbell, J., Hollinghurst, S. P., Haase, A. M., Taylor, A., et al. (2012). Facilitated physical activity as a treatment for depressed adults: randomised controlled trial. BMJ 344:e2758. doi: 10.1136/bmj.e2758
Chaouloff, F., Laude, D., and Elghozi, J. (1989). Physical exercise: evidence for differential consequences of tryptophan on 5-HT synthesis and metabolism in central serotonergic cell bodies and terminals. J. Neural Transm. 78, 1435–1463. doi: 10.1007/BF01252498
Cooney, G. M., Dwan, K., Greig, C. A., Lawlor, D. A., Rimer, J., Waugh, F. R., et al. (2013). Exercise for depression. Cochrane Database Syst. Rev. CD004366. doi: 10.1111/jebm.12076
Czubak, A., Nowakowska, E., Kus, K., Burda, K., Metelska, J., Baer-Dubowska, W., et al. (2009). Influences of chronic venlafaxine, olanzapine and nicotine on the hippocampal and cortical concentrations of brain-derived neurotrophic factor (BDNF). Pharmacol. Rep. 61, 1017–1023. doi: 10.1016/S1734-1140(09)70163-X
Danielsson, L., Noras, A. M., Waern, M., and Carlsson, J. (2013). Exercise in the treatment of major depression: a systematic review grading the quality of evidence. Physiother. Theory Pract. 29, 573–585. doi: 10.3109/09593985.2013.774452
Dugan, S. A., Bromberger, J. T., Segawa, E., Avery, E., and Sternfeld, B. (2015). Association between physical activity and depressive symptoms: midlife women in SWAN. Med. Sci. Sports Exerc. 47, 335–342. doi: 10.1249/MSS.0000000000000407
Duman, R., Heninger, G., and Nestler, E. A. (1997). Molecular and cellular theory of depression. Arch. Gen. Psychiatry 54, 597–606. doi: 10.1001/archpsyc.1997.01830190015002
Edwards, M. K., and Loprinzi, P. D. (2016). Effects of a sedentary behavior-inducing randomized controlled intervention on depression and mood profile in active young adults. Mayo Clin. Proc. 91, 984–998. doi: 10.1016/j.mayocp.2016.03.021
Eklund, U., Steene-Johannessen, J., Brown, W. J., Fagerland, M. W., Owen, N., Powell, K. E., et al. (2016). Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388, 1302–1310. doi: 10.1016/S0140-6736(16)30370-1
Erickson, K. I., Voss, M. W., Prakash, R. S., Basak, C., Szabo, A., Chaddock, L., et al. (2011). Exercise training increases size of hippocampus and improves memory. Proc. Natl. Acad. Sci. U.S.A. 108, 3017–3022. doi: 10.1073/pnas.1015950108
Ernst, C., Olson, A. K., Pinel, J. P., Lam, R. W., and Christie, B. R. (2006). Antidepressant effects of exercise: evidence for an adult-neurogenesis hypothesis? J. Psychiatry Neurosci. 31, 84–92.
Firth, J., Carney, R., Elliott, R., French, P., Parker, S., McIntyre, R., et al. (2016). Exercise as an intervention for first-episode psychosis: a feasibility study. Early Interv. Psychiatry doi: 10.1111/eip.12329 [Epub ahead of print].
Firth, J., Cotter, J., Elliott, R., French, P., and Yung, A. (2015). A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol. Med. 45, 1343–1361. doi: 10.1017/S0033291714003110
Gardner-Sood, P., Lally, J., Smith, S., Atakan, Z., Ismail, K., Greenwood, K. E., et al. (2015). Cardiovascular risk factors and metabolic syndrome in people with established psychotic illnesses: baseline data from the IMPaCT randomized controlled trial. Psychol. Med. 45, 2619–2629. doi: 10.1017/S0033291715000562
Gartlehner, G., Gaynes, B. N., Forneris, C., Amick, H. R., Asher, G. N., Morgan, L. C., et al. (2016). Comparative benefits and harms of antidepressant, psychological, complementary, and exercise treatments for major depression: an evidence report for a Clinical Practice Guideline from the American College of Physicians. Ann. Intern. Med. 164, 331–341. doi: 10.7326/M15-1813
Hallgren, M., Herring, M. P., Owen, N., Dunstan, D., Ekblom,Ö, Helgadottir, B., et al. (2016). Exercise, physical activity, and sedentary behavior in the treatment of depression: broadening the scientific perspectives and clinical opportunities. Front. Psychiatry 7:36. doi: 10.3389/fpsyt.2016.00036
Hallgren, M., Vancampfort, D., Giesen, E. S., Lundin, A., and Stubbs, B. (2017). Exercise as treatment for alcohol use disorders: systematic review and meta-analysis. Br. J. Sports Med. doi: 10.1136/bjsports-2016-096814 [Epub ahead of print].
Hoffman, B. M., Babyak, M. A., Craighead, W. E., Sherwood, A., Doraiswamy, P. M., Coons, M. J., et al. (2011). Exercise and pharmacotherapy in patients with major depression: one-year follow-up of the SMILE study. Psychosom. Med. 73, 127–133. doi: 10.1097/PSY.0b013e31820433a5
Hoffman, B. M., Blumenthal, J. A., Babyak, M. A., Smith, P. J., Rogers, S. D., Doraiswamy, P. M., et al. (2008). Exercise fails to improve neurocognition in depressed middle-aged and older adults. Med. Sci. Sports Exerc. 40, 1344–1352. doi: 10.1249/MSS.0b013e31816b877c
Josefsson, T., Lindwall, M., and Archer, T. (2014). Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand. J. Med. Sci. Sport 24, 259–272. doi: 10.1111/sms.12050
Kandola, A., Hendrikse, J., Lucassen, P. J., and Yücel, M. (2016). Aerobic exercise as a tool to improve hippocampal plasticity and function in humans: practical implications for mental health treatment. Front. Hum. Neurosci. 10:373. doi: 10.3389/fnhum.2016.00373
Kerling, A., Tegtbur, U., Gützlaff, E., Kück, M., Borchert, L., Ates, Z., et al. (2015). Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J. Affect. Disord. 177, 1–6. doi: 10.1016/j.jad.2015.01.006
Knapen, J., Vancampfort, D., Moriën, Y., and Marchal, Y. (2015). Exercise therapy improves both mental and physical health in patients with major depression. Disabil. Rehabil. 37, 1490–1495. doi: 10.3109/09638288.2014.972579
Knubben, K., Reischies, F. M., Adli, M., Schlattmann, P., Bauer, M., and Dimeo, F. (2007). A randomized controlled study on the effects of a short-term endurance training programme in patients, with major depression. Br. J. Sports Med. 41, 29–33. doi: 10.1136/bjsm.2006.030130
Krogh, J., Nordentoft, M., Sterne, J. A., and Lawlor, D. A. (2011). The effect of exercise in clinically depressed adults: systematic review and meta-analysis of randomized controlled trials. J. Clin. Psychiatry 72, 529–538. doi: 10.4088/JCP.08r04913blu
Kvam, S., Kleppe, C. L., Nordhus, I. H., and Hovland, A. (2016). Exercise as a treatment for depression: a meta-analysis. J. Affect. Disord. 15, 67–86. doi: 10.1016/j.jad.2016.03.063
Legrand, F. D., and Neff, E. M. (2016). Efficacy of exercise as an adjunct treatment for clinically depressed inpatients during the initial stages of antidepressant pharmacotherapy: an open randomized controlled trial. J. Affect. Disord. 191, 139–144. doi: 10.1016/j.jad.2015.11.047
Lin, K. Y., Frawley, H. C., Denehy, L., Feil, D., and Granger, C. L. (2016). Exercise interventions for patients with gynaecological cancer: a systematic review and meta-analysis. Physiotherapy 102, 309–319. doi: 10.1016/j.physio.2016.02.006
Liu, M., Wu, L., and Yao, S. (2016). Dose-response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br. J. Sports Med. 50, 1252–1258. doi: 10.1136/bjsports-2015-095084
Martiny, K., Refsgaard, E., Lund, V., Lunde, M., Sorensen, L., Thougaard, B., et al. (2012). A 9-week randomized trial comparing a chronotherapeutic intervention (wake and light therapy) to exercise in major depressive disorder patients treated with duloxetine. J. Clin. Psychiatry 73, 1234–1242. doi: 10.4088/JCP.11m07625
Mather, A. S., Rodriguez, C., Guthrie, M. F., McHARG, A. M., Reid, I. C., and McMurdo, M. E. (2002). Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder. Randomised controlled trial. Br. J. Psychiatry 180, 411–415. doi: 10.1192/bjp.180.5.41
Mead, G. E., Morley, W., Campbell, P., Greig, C. A., McMurdo, M., and Lawlor, D. A. (2009). Exercise for depression. Cochrane Database Syst. Rev. CD004366. doi: 10.1002/14651858.CD004366.pub4
Mendez-David, I., Hen, R., Gardier, A. M., and David, D. J. (2013). Adult hippocampal neurogenesis: an actor in the antidepressant-like action. Ann. Pharm. Fr. 71, 143–149. doi: 10.1016/j.pharma.2013.02.006
Mota-Pereira, J., Silverio, J., Carvalho, S., Ribeiro, J. C., Fonte, D., and Ramos, J. (2011). Moderate exercise improves depression parameters in treatment-resistant patients with major depressive disorder. J. Psychiatr. Res. 45, 1005–1011. doi: 10.1016/j.jpsychires.2011.02.005
Mura, G., Moro, M. F., Patten, S. B., and Carta, M. G. (2014). Exercise as an add-on strategy for the treatment of major depressive disorder: a systematic review. CNS Spectr. 19, 496–508. doi: 10.1017/S1092852913000953
Murri, M. B., Amore, M., Menchetti, M., Toni, G., Neviani, F., Cerri, M., et al. (2015). Physical exercise for late-life major depression. Br. J. Psychiatry 207, 235–242. doi: 10.1192/bjp.bp.114.150516
Naci, H., and Ioannidis, J. P. A. (2013). Comparative effectiveness of exercise and drug interventions on mortality outcomes: meta-epidemiological study. Br. J. Sports Med. 49, 1414–1422. doi: 10.1136/bmj.f5577
Nagamatsu, L. S., Flicker, L., Kramer, A. F., Voss, M. W., Erickson, K. I., Hsu, C. L., et al. (2014). Exercise is medicine, for the body and the brain. Br. J. Sports Med. 48, 943–944. doi: 10.1136/bjsports-2013-093224
Neto, F. L., Borges, G., Torres-Sanchez, S., Mico, J. A., and Berrocoso, E. (2011). Neurotrophins role in depression neurobiology: a review of basic and clinical evidence. Curr. Neuropharmacol. 9, 530–552. doi: 10.2174/157015911798376262
Nyström, M. B., Neely, G., Hassmén, P., and Carlbring, P. (2015). Treating major depression with physical activity: a systematic overview with recommendations. Cogn. Behav. Ther. 44, 341–352. doi: 10.1080/16506073.2015.1015440
Pilu, A., Sorba, M., Hardoy, M. C., Floris, A. L., Mannu, F., Seruis, M. L., et al. (2007). Efficacy of physical activity in the adjunctive treatment of major depressive disorders: preliminary results. Clin. Pract. Epidemiol. Ment. Health 3:8. doi: 10.1186/1745-0179-3-8
Qaseem, A., Barry, M. J., Kansagara, D., and Clinical Guidelines Committee of the American College of Physicians (2016). Non-pharmacologic vs pharmacologic treatment of adult patients with major depressive disorder: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 164, 350–359. doi: 10.7326/M15-2570
Rethorst, C. D., Wipfli, B. M., and Landers, D. M. (2009). The antidepressive effects of exercise: a meta-analysis of randomized trials. Sports Med. 39, 491–511. doi: 10.2165/00007256-200939060-00004
Rimer, J., Dwan, K., Lawlor, D. A., Greig, C. A., McMurdo, M., Morley, W., et al. (2012). Exercise for depression. Cochrane Database Syst. Rev. CD004366. doi: 10.1002/14651858.CD004366.pub5
Robertson, R., Robertson, A., Jepson, R., and Maxwell, M. (2012). Walking for depression or depressive symptoms: a systematic review and meta-analysis. Ment. Health Phys. Act. 5, 66–75. doi: 10.1016/j.mhpa.2012.03.002
Russo-Neustadt, A., Ha, R., and Ramirez, R. (2001). Physical activity antidepressant treatment combination: impact on brain derived neurotrophic factor and behavior in an animal model. Behav. Brain Res. 120, 87–95. doi: 10.1016/S0166-4328(00)00364-8
Rutherford, B. R., Mori, S., Sneed, J. R., Pimontel, M. A., and Roose, S. P. (2012). Contribution of spontaneous improvement to placebo response in depression: a meta-analytic review. J. Psychiatr. Res. 46, 697–702. doi: 10.1016/j.jpsychires.2012.02.008
Schuch, F., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P., Reichert, T., et al. (2017). Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J. Affect. Disord. 210, 139–150. doi: 10.1016/j.jad.2016.10.050
Schuch, F. B., Deslandesc, A. C., Stubbs, B., Gosmannb, N. P., Silva, C. T., and Fleck, M. P. (2016a). Neurobiological effects of exercise on major depressive disorder: a systematic review. Neurosci. Biobehav. Rev. 61, 1–11. doi: 10.1016/j.neubiorev.2015.11.012
Schuch, F. B., Vancampfort, D., Richards, J., Rosenbaum, S., Ward, P. B., and Stubbs, B. (2016b). Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J. Psychiatr. Res. 77, 42–51. doi: 10.1016/j.jpsychires.2016.02.023
Schuch, F. B., Vasconcelos-Moreno, M. P., Borowsky, C., and Fleck, M. P. (2011). Exercise and severe depression: preliminary results of an add-on study. J. Affect. Disord. 133, 615–618. doi: 10.1016/j.jad.2011.04.030
Schuch, F. B., Vasconcelos-Moreno, M. P., Borowsky, C., Zimmermann, A. B., Rocha, N. S., and Fleck, M. P. (2015). Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J. Psychiatr. Res. 61, 25–32. doi: 10.1016/j.jpsychires.2014.11.005
Silveira, H., Moraes, H., Oliveira, N., Coutinho, E. S., Laks, J., and Deslandes, A. (2013). Physical exercise and clinically depressed patients: a systematic review and meta-analysis. Neuropsychobiology 67, 61–68. doi: 10.1159/000345160
Stubbs, B., Vancampfort, D., Rosenbaum, S., Ward, P. B., Richards, J., Ussher, M., et al. (2015). Challenges establishing the efficacy of exercise as an antidepressant treatment: a systematic review and meta-analysis of control group responses in exercise randomised controlled trials. Sports Med. 46, 699–713. doi: 10.1007/s40279-015-0441-5
WHO (2016). Available at: http://www.who.int/mediacentre/factsheets/fs369/en/
Keywords: antidepressants, exercise therapy, monotherapy, combination therapy, adjunctive therapy
Citation: Netz Y (2017) Is the Comparison between Exercise and Pharmacologic Treatment of Depression in the Clinical Practice Guideline of the American College of Physicians Evidence-Based? Front. Pharmacol. 8:257. doi: 10.3389/fphar.2017.00257
Received: 12 March 2017; Accepted: 25 April 2017;
Published: 15 May 2017.
Edited by:
Mihajlo Jakovljevic, University of Kragujevac, SerbiaReviewed by:
Dejan Stevanovic, General Hospital Sombor, SerbiaGeorgi Iskrov, Plovdiv Medical University, Bulgaria
Copyright © 2017 Netz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yael Netz, bmV5YWVsQHdpbmNvbC5hYy5pbA==
 Yael Netz
Yael Netz