
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Pharmacol. , 14 November 2016
Sec. Drugs Outcomes Research and Policies
Volume 7 - 2016 | https://doi.org/10.3389/fphar.2016.00429
This article is part of the Research Topic Patient Adherence to Medications: A Simple Concept but a Challenging Reality View all 18 articles
Introduction: Despite much research, interventions to improve medication adherence report disappointing and inconsistent results. Tailored approaches that match interventions and patient determinants of non-adherence were seldom used in clinical trials. The presence of a multitude of theoretical frameworks and models to categorize interventions and patient determinants complicated the development of common categories shared by interventions and determinants. We retrieved potential interventions and patient determinants from published literature on medication adherence, matched them like locks and keys, and categorized them according to the Theoretical Domains Framework (TDF).
Methods: We identified the most relevant literature reviews on interventions and determinants in a pragmatic literature search, extracted all interventions and determinants, grouped similar concepts to umbrella terms and assigned them to TDF categories. All steps were finalized in consensus discussion between the authors.
Results: Sixteen articles (5 with determinants, 11 with interventions) were included for analysis. We extracted 103 interventions and 42 determinants that we divided in 26 modifiable and 16 unmodifiable determinants. All interventions and modifiable determinants were matched within 11 categories (Knowledge; Skills; Social/professional role and identity; Beliefs about capabilities; Beliefs about consequences; Intentions; Memory, Attention and decision processes; Environmental context and resources; Social influences; Emotion; and Behavioral regulation).
Conclusion: In published trials on medication adherence, the congruence between interventions and determinants can be assessed with matching interventions to determinants. To be successful, interventions in medication adherence should target current modifiable determinants and be tailored to the unmodifiable determinants. Modifiable and unmodifiable determinants need to be assessed at inclusion of intervention studies to identify the patients most in need of an adherence intervention. Our matched categories may be useful to develop interventions in trials that investigate the effectiveness of adherence interventions.
After 4 decades of research on adherence to medication, the progress is disappointing and adherence remains a fragmented construct. Medication adherence is briefly defined as the behavioral response to an agreed medical recommendation (Sabaté, 2003) and is measured either dichotomously (either one is adherent, or one is not) or continuously. Recently, medication adherence has been defined to consist of three different phases: initiation, implementation, and persistence (Vrijens et al., 2012). Non-adherence is not simply the reverse of adherence. Two patients can be equally non-adherent with respect to measuring adherence, for example take only 60% of their pills. At the same time, the reasons for these patients to be non-adherent may vary widely.
The complexity of the characteristics of adherence was already known by the end of the 1970s (Becker and Maiman, 1975). Despite much research in the 1980s and 1990s, few new insights arose. Research in the 1990s emphasized the influence of patient beliefs about health in general and about illness/medication in particular (Horne and Weinman, 1999). Qualitative research on patients' perspectives started with the new millennium and identified new issues like the quality of the doctor-patient relationship and patient health beliefs (Vermeire et al., 2001). Grossly, five theoretical approaches could be identified that all view non-adherence from a different perspective (Leventhal and Cameron, 1987). The oldest approach is the biomedical model that focuses on dispositional characteristics of the patient such as demographic or personality traits. Operant behavior and social learning theories shifted the focus to the behaviors needed for adherence. In the communication model, the patient seeks expert advice and treatment from the healthcare professional; adherence results from persuasion through effective communication. The rational decision-health belief and reasoned action model generated the patient's perception of risk and motivation for action. Finally, the self-regulative systems theory sees the patients as an active problem solver. Extent and factors of non-adherence have been extensively investigated, and a plethora of strategies to improve adherence was developed, mostly without consistent success (Haynes et al., 2008).
A systematic review of reviews analyzed interventions with regard to theoretical models and found no clear correlation between the effectiveness of interventions that were theory-based and those without an explicit theoretical background (van Dulmen et al., 2007).
The most recent approach, the Theoretical Domains Framework (TDF), was developed to integrate the various behavior change theories. It aimed to simplify the investigation of behavioral problems such as adherence and to facilitate intervention design (Cane et al., 2012).
Success in a complex process like adherence can only be achieved with the integration of many ingredients, and a single obstruction causes failure. This concept is sometimes referred to as the “Anna Karenina principle,” referring to the first sentence in Tolstoy's novel Anna Karenina: “Happy families are all alike. Every unhappy family is unhappy in its own way.” In this regard, it takes one deficient factor to cause non-adherence. Therefore, the purpose of any intervention strategy should be to compensate for each reason causing non-adherence. As acknowledged by others (Hugtenburg et al., 2013; Linn et al., 2013; Müller et al., 2015), it seems thus obvious that a tailored approach is required, i.e., an approach that adapts the keys (interventions) to the locks (patient determinants).
Various attempts to categorize interventions ended up with coarse sections like educational, behavioral, social, and mixed forms (Kripalani et al., 2007) or simple groupings (Haynes et al., 2005). In the field of behavior change research, a recent international consensus developed a framework (the Behavior Change Technique Taxonomy) with 93 behavior change techniques clustered in 16 groups (Michie et al., 2013). Although not specific for medication adherence, the new taxonomy has been used to classify interventions in the field of adherence research (Joost et al., 2014). As behavior change is only one aspect of medication adherence, this unilateral framework appears limited to categorize the sum of all adherence interventions. A broader view on adherence was captured by a Cochrane Review on interventions to improve safe and effective medicines use (Ryan et al., 2014). Interventions were grouped in eight categories: Providing information or education; Facilitating communication and/or decision making; Acquiring skills and competencies; Supporting behavior change; Support; Minimizing risks or harms; Improving quality, and Consumer system participation.
Patient determinants of non-adherence were often categorized according to the five dimensions of non-adherence proposed by WHO (Sabaté, 2003) or variations of these concepts (Baudrant-Boga et al., 2012): Social- and economic-related factors; Health system/health care team-related factors; Therapy-related factors; Condition-related factors, and Patient-related factors.
Matching possible targets for medication adherence to the types of interventions will yield more insight in effective strategies able to overcome the different barriers for medication adherence. To our knowledge, common categories shared by interventions and patient determinants of non-adherence have never been proposed. As a result, interventions for improving adherence and patient determinants were seldom matched in clinical trials. As an example, from 109 studies aimed at improving patient adherence, only 13% reported the assessment of patient determinants at baseline (Haynes et al., 2015). Even though some studies reported tailoring of interventions to patient characteristics, the specific procedure remains often unclear and thus, the results are almost impossible to replicate (Haynes et al., 2015).
In this article, we retrieved potential interventions and patient determinants from published literature on medication adherence and aimed at matching them like locks and keys.
• To extract from literature salient (a) interventions intended to improve adherence and (b) related patient determinants of non-adherence.
• To categorize the retrieved (a) interventions and (b) determinants.
• To match (a) and (b).
Several recent systematic literature reviews exist on interventions and patient determinants of non-adherence. It seemed superfluous to repeat this process and thus, we abstained from a systematic literature search with broad major/MeSH terms such as “patient compliance.” Rather and in order to identify literature with the highest relevance to our aims, we pursued a pragmatic search strategy to identify existing reviews with the terms “intervention” and “determinant” or “factor” which are widely used in conjunction with medication adherence. We combined these specific terms with the established terms “adherence” or “compliance.”
We searched Medline via Pubmed on March 10, 2015 (without time limits) with the following terms and a limit set to reviews:
a) intervention*[title] AND (improv*[title] OR enhanc*[title]) AND medication[title] AND (adherence[title] OR compliance[title]).
b) (determinant*[title] OR factor*[title]) AND medication[title] AND (adherence[title] OR compliance[title]).
Titles and abstracts of the search results were screened for relevance by two investigators (SA, IA). To assure a generic view on medication adherence (not restricted to specific diseases, medications or settings), we excluded full-text articles when they investigated:
• single conditions
• single medication groups
• specific providers
• specific target groups
• single intervention
• economic evaluations
• specific adherence measurement methods.
All extractions were performed in MAXQDA 11 (VERBI GmbH, Berlin, Germany). All steps were performed separately for interventions and determinants.
In the first step, IA and SA reviewed full-texts from the included articles. Both investigators independently extracted items of (a) interventions and (b) determinants for non-adherence and scanned the reference list for additional articles. Investigators were not blinded with regard to authors or journal. The lists were reviewed by both investigators in a consensus discussion and umbrella terms were introduced for items with similar connotations.
In the second step, IA and SA independently matched each intervention to individual determinants. Items that did not match were listed separately.
In the third step, IA and SA assigned the matched interventions and determinants to the 14 domains of the TDF. We chose the TDF because it offers the most recent framework, combines various theoretical models, and has a strong empirical base. We determined consistency among raters performing an interrater reliability analysis using the Kappa statistic.
Disagreements were resolved by discussion until consensus was reached (first and second steps) or by an adjudicator (third step).
A total of 65 articles were obtained (Figure 1). Two articles were updated versions of previous Cochrane analyses (Haynes et al., 2008; Schedlbauer et al., 2010). Screening of the reference lists yielded two additional articles that were included in the review (Vermeire et al., 2001; Ryan et al., 2014). Five articles were excluded after screening of titles and abstracts because they were not relevant to our aims. After full-text screening, 44 articles were excluded because they investigated (a) single conditions (18; schizophrenia, psychiatric disorder, transplantation, diabetes, hypertension, Parkinson, inflammatory bowel, rosacea); (b) single medication groups (14; antidepressant, cardiovascular, heart failure, antipsychotic, osteoporosis, hypoglycemic and lipid lowering agents); (c) specific providers (4; pharmacist, physician, nurse); (d) specific target groups (1; children); (e) single intervention (4; HIT, technology-mediated, cultural responsive, electronic reminders); (f) economic evaluations (2); (g) adherence measurement methods (1; electronically compiled drug dosing history).
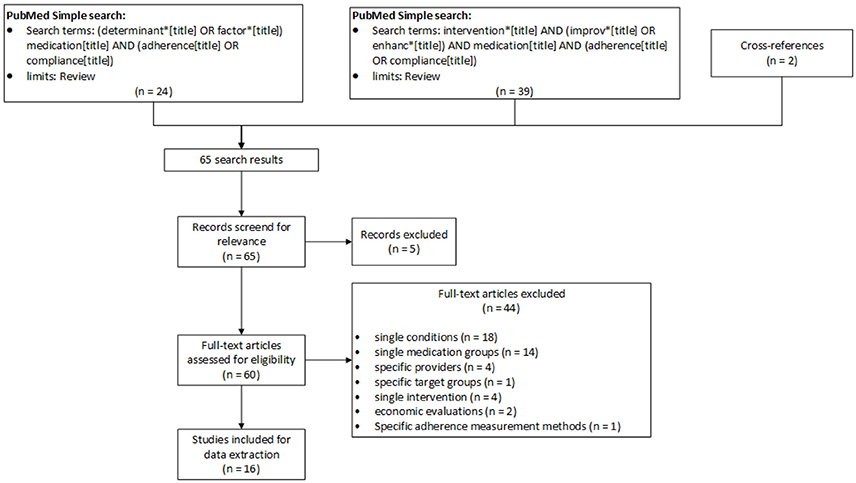
Figure 1. PRISMA flow diagram (Moher et al., 2009) for study selection process.
The final set included 16 articles (11 with interventions, 5 with determinants, Table 1).
We extracted 103 different interventions, including variations of the same concept such as different forms of reminders. We extracted 42 determinants that we divided into 26 modifiable and 16 unmodifiable determinants. We defined modifiable determinants as factors that may be changed by interventions (such as knowledge or behaviors) and unmodifiable determinants as those that are unchangeable (such as age). Some unmodifiable determinants may appear modifiable at first sight, such as level of education or employment situation. However, those determinants are not targeted by the adherence interventions, albeit they may influence the choice of an appropriate intervention. Thus, unmodifiable determinants (Box 1) were not included in the matching procedure.
Unmodifiable determinants of non-adherence
• Age (Vlasnik et al., 2005; Ingersoll and Cohen, 2008; Schäfer-Keller et al., 2010; Baudrant-Boga et al., 2012)
• Gender (Vlasnik et al., 2005)
• Level of education (Vlasnik et al., 2005; Ingersoll and Cohen, 2008) (literacy)
• Employment situation (Vlasnik et al., 2005)
• Financial situation (Vlasnik et al., 2005; Baudrant-Boga et al., 2012) (socioeconomic status, lack of insurance, income, material resources)
• Insurance type/coverage (Zeber et al., 2013)
• Ethnicity and culture (Vlasnik et al., 2005; Schäfer-Keller et al., 2010; Baudrant-Boga et al., 2012; Zeber et al., 2013) (language difficulties, race, immigration status)
• Housing situation/living situation (Vlasnik et al., 2005; Baudrant-Boga et al., 2012; Zeber et al., 2013) (lack of fixed address, living alone, marital status)
• Cognitive impairment (Vlasnik et al., 2005; Ingersoll and Cohen, 2008; Baudrant-Boga et al., 2012)
• Illness chronicity (Zeber et al., 2013)
• Illness severity (Vlasnik et al., 2005; Schäfer-Keller et al., 2010; Baudrant-Boga et al., 2012; Zeber et al., 2013) (absence, reduction, disappearance or fluctuation of symptoms)
• Polymorbidity (Zeber et al., 2013)
• Change of therapy (Vlasnik et al., 2005; Schäfer-Keller et al., 2010)
• History of non-adherence (Vlasnik et al., 2005)
• Past treatment response (Zeber et al., 2013)
• Duration of treatment (Schäfer-Keller et al., 2010; Baudrant-Boga et al., 2012).
From the original 14 domains of the TDF, 11 suffice to categorize our 103 interventions and 26 modifiable determinants (Table 2). No intervention or determinant could be assigned to the three original domains “Optimism,” “Reinforcement,” and “Goals.” Because heterogeneous interventions and determinants were included in the domain “Environmental context and resources,” we created the subdomains “Regimen,” “Adverse events,” “Integration and coordination of care,” and “Financial aspects” (Table 3).
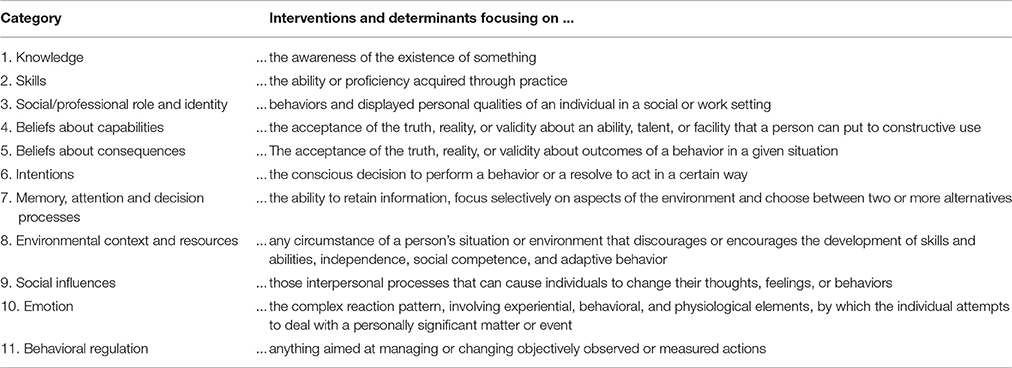
Table 2. Final 11 categories of the TDF with corresponding definitions sufficient to categorize interventions and patient determinants.
The interrater reliability was substantial with a Cohen's Kappa of 0.7 (95% CI 0.5–0.9, p <0.001).
Based on a literature review, we were able to match 103 adherence interventions and 26 patient determinants within 11 common categories. The fact that interventions were more diverse than patient determinants is not surprising, as there is usually more than one way to target a single determinant. In a previous review on patient determinants, the authors grouped similar contents together and ended up with 40 heterogeneous umbrella terms (Kardas et al., 2013). What appears nearly identical to our 42 patient determinants is slightly different, since no overlap existed with our determinants for 6 of the 40 umbrella terms (“Social stigma of disease”; “Prescription coverage”; “Prescription by a specialist”; “Certain diagnoses/indications”; “Drug type,” and “Well organized treatment”). A subset of patient determinants must be considered unmodifiable, such as age, gender, or culture. In our view, this distinction is essential for the choice of adherence interventions. In order to be effective, we postulate that interventions have on one hand to target current modifiable patient determinants and on the other hand to be tailored to the unmodifiable patient determinants. This lack of distinction among the patient determinants in previous literature may explain partly why no meta-analysis could demonstrate an overall benefit of interventions aimed at enhancing adherence (Nieuwlaat et al., 2014). Further research is needed to investigate if adherence is improved when the intervention is matched to the patient determinants for non-adherence according to our matching list.
The importance of tailoring interventions to patient characteristics has been acknowledged previously (Hugtenburg et al., 2013; Linn et al., 2013; Müller et al., 2015). To our knowledge, no published framework aimed to match interventions and patient determinants of non-adherence. Specific toolboxes for tailored interventions cover a restricted number of interventions or patient determinants (Staring et al., 2006; Herborg et al., 2008). Their intended use is the application in daily practice where a workable toolbox trumps a comprehensive framework. The 5 WHO dimensions that could be used to classify both interventions and patient determinants are too coarse to provide meaningful guidance (Sabaté, 2003). The TDF has been the most recent and complete effort to develop theory-informed behavior change interventions (French et al., 2012) or assess the underlying theoretical constructs of interventions (Little et al., 2015). Because it was not specifically developed for interventions and patient determinants of non-adherence, some adaption was warranted. While we were able to assign all interventions and patient determinants to one of the domains, we did not use 3 of the original 14 domains: “Optimism,” “Reinforcement,” and “Goals”. “Optimism” (i.e., the confidence that things will happen for the best or that desired goals will be attained) may theoretically differ from beliefs, but we chose not to differentiate between the two concepts for practical reasons. By definition, “Reinforcement” (i.e., increasing the probability of a response by arranging a dependent relationship, or contingency, between the response and a given stimulus) can only apply to interventions. Hence, we were not able to use this domain for shared interventions and determinants. Instead, we assigned interventions belonging to the “Reinforcement” domain to “Intentions”. “Goals” (i.e., mental representations of outcomes or end states that an individual wants to achieve) also overlaps with “Intentions” and we chose not to differ between the two concepts.
Some of the extracted interventions did not target patient determinants. They represent much more unspecific interventions such as general education to improve knowledge. In contrast, one extracted determinant (Prescribing errors) could not be matched to a specific intervention. Although, it is obvious that studies to reduce prescribing errors were performed, they may not have been aimed at enhancing adherence to treatment.
Our matching list allows for the assessment of congruency between interventions and patient determinants in published trials. Under the prerequisite that a causal relationship exists between our interventions and corresponding patient determinants, our list may help to assess the quality of published studies and their results (Nieuwlaat et al., 2014). Furthermore, our matching list may be useful to develop interventions and to plan trials to assess the effectiveness of interventions with respect to modifiable and unmodifiable patient determinants.
We acknowledge some limitations. First, we applied a very specific search strategy to identify the most relevant literature. A systematic approach with broader search terms and additional databases might have yielded more articles, however, may not have yielded additional items of interventions or patient determinants. The 85% overlapping between our determinants and those retrieved from a systematic review of reviews (Kardas et al., 2013) reinforces this assumption. Second, we did not consider the effectiveness of the interventions, the frequency of the patient determinants, nor the impact size of the patient determinants on adherence. Consequently, matching interventions to patient determinants based on our results does not guarantee for a successful adherence intervention. Other concepts may be important to consider: determinants may be different for each phase of medication adherence: initiation, implementation, and persistence (Vrijens et al., 2012; Kardas et al., 2013). The current literature lacks the information about which determinant is associated to each of the three phases. Third, our final matching list was not externally validated. However and in line with others, the existence of ~40 different determinants seems plausible.
Our study has some strengths. First, we based our selection on published models and theories, and previously proposed categories. Consequently, our matching list represents a robust framework in line with underlying theories. Second, reliability was given from two independent investigators for extraction and categorization reaching substantial agreement. Third, the exclusion of reviews with focus on specific diseases, populations or other criteria guarantees a broad applicability of the matching list.
Matched interventions and patient determinants in common categories are needed to assess the congruency between interventions and patient determinants in published trials on medication adherence. Our matching list may be useful to develop interventions in trials that investigate the effectiveness of adherence interventions. Application of this list will show its practicability and may initiate its refinement and further development into a practical tool. To be successful, interventions in medication adherence should target current modifiable patient determinants and be tailored to the unmodifiable patient determinants. Modifiable and unmodifiable determinants need to be assessed at inclusion of intervention studies to identify the patients most in need of an adherence intervention.
All authors contributed to the design of the study. SA and IA performed the analysis and drafted the manuscript. RN, BV, and KH critically revised the work prior to submission. All authors approved the manuscript in its final version for submission and agreed to be accountable for the work presented.
This study was funded by the University of Basel, Switzerland.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would like to thank Dr. Liset van Dijk for her critical review and valuable inputs to the manuscript and Corina Metaxas, MSc for serving as adjudicator to resolve disagreements between investigators.
Banning, M. (2009). A review of interventions used to improve adherence to medication in older people. Int. J. Nurs. Stud. 46, 1505–1515. doi: 10.1016/j.ijnurstu.2009.03.011
Baudrant-Boga, M., Lehmann, A., and Allenet, B. (2012). “Penser autrement l'observance médicamenteuse: d'une posture injonctive à une alliance thérapeutique entre le patient et le soignant–Concepts et déterminants,” in Annales Pharmaceutiques Francaises, ed A. Astier (Paris: Elsevier), 15–25.
Becker, M. H., and Maiman, L. A. (1975). Sociobehavioral determinants of compliance with health and medical care recommendations. Med. Care 13, 10–24. doi: 10.1097/00005650-197501000-00002
Cane, J., O'connor, D., and Michie, S. (2012). Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 7:37. doi: 10.1186/1748-5908-7-37
French, S. D., Green, S. E., O'connor, D. A., McKenzie, J. E., Francis, J. J., Michie, S., et al. (2012). Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement. Sci. 7:38. doi: 10.1186/1748-5908-7-38
Haynes, R. B., Jeffery, R. A., Keepanasseril, A., Wilczynski, N. L., Navarro-Ruan, Mustafa R. A., et al. (2015). Methods for trials of interventions to enhance patient adherence to medication prescriptions, based on a systematic review of recent randomized trials. Clin. Res. Trials 1, 20–25. doi: 10.15761/CRT.1000106
Haynes, R., Yao, X., Degani, A., Kripalani, S., Garg, A., and McDonald, H. (2005). Interventions for enhancing medication adherence. Cochrane Library. 2005:CD000011. doi: 10.1002/14651858.cd000011.pub2
Haynes, R. B., Ackloo, E., Sahota, N., McDonald, H. P., and Yao, X. (2008). Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2008:CD000011. doi: 10.1002/14651858.CD000011.pub3
Herborg, H., Haugbølle, L. S., Sørensen, L., Rossing, C., and Dam, P. (2008). Developing a generic, individualised adherence programme for chronic medication users. Pharm. Pract. (Internet) 6, 148–157. doi: 10.4321/S1886-36552008000300006
Horne, R., and Weinman, J. (1999). Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J. Psychosom. Res. 47, 555–567. doi: 10.1016/S0022-3999(99)00057-4
Hugtenburg, J. G., Timmers, L., Elders, P. J., Vervloet, M., and Van Dijk, L. (2013). Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Patient Prefer. Adherence 7, 675–682. doi: 10.2147/PPA.S29549
Ingersoll, K. S., and Cohen, J. (2008). The impact of medication regimen factors on adherence to chronic treatment: a review of literature. J. Behav. Med. 31, 213–224. doi: 10.1007/s10865-007-9147-y
Joost, R., Dörje, F., Schwitulla, J., Eckardt, K.-U., and Hugo, C. (2014). Intensified pharmaceutical care is improving immunosuppressive medication adherence in kidney transplant recipients during the first post-transplant year: a quasi-experimental study. Nephrol. Dial. Transplant. 29, 1597–1607. doi: 10.1093/ndt/gfu207
Kardas, P., Lewek, P., and Matyjaszczyk, M. (2013). Determinants of patient adherence: a review of systematic reviews. Front. Pharmacol. 4:91. doi: 10.3389/fphar.2013.00091
Kripalani, S., Yao, X., and Haynes, R. B. (2007). Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch. Intern. Med. 167, 540–549. doi: 10.1001/archinte.167.6.540
Leventhal, H., and Cameron, L. (1987). Behavioral theories and the problem of compliance. Patient Educ. Couns. 10, 117–138. doi: 10.1016/0738-3991(87)90093-0
Linn, A. J., van Weert, J. C., Smit, E. G., Perry, K., and van Dijk, L. (2013). 1 + 1 = 3? The systematic development of a theoretical and evidence-based tailored multimedia intervention to improve medication adherence. Patient Educ. Couns. 93, 381–388. doi: 10.1016/j.pec.2013.03.009
Little, E. A., Presseau, J., and Eccles, M. P. (2015). Understanding effects in reviews of implementation interventions using the Theoretical Domains Framework. Implement. Sci. 10, 1. doi: 10.1186/s13012-015-0280-7
McDonald, H. P., Garg, A. X., and Haynes, R. B. (2002). Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA 288, 2868–2879. doi: 10.1001/jama.288.22.2868
Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., et al. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 46, 81–95. doi: 10.1007/s12160-013-9486-6
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 151, 264–269. doi: 10.7326/0003-4819-151-4-200908180-00135
Müller, S., Kohlmann, T., and Wilke, T. (2015). Validation of the adherence barriers questionnaire–an instrument for identifying potential risk factors associated with medication-related non-adherence. BMC Health Serv. Res. 15:153. doi: 10.1186/s12913-015-0809-0
Nieuwlaat, R., Wilczynski, N., Navarro, T., Hobson, N., Jeffery, R., Keepanasseril, A., et al. (2014). Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2014:CD000011. doi: 10.1002/14651858.CD000011.pub4
Ryan, R., Santesso, N., Lowe, D., Hill, S., Grimshaw, J., Prictor, M., et al. (2014). Interventions to improve safe and effective medicines use by consumers: an overview of systematic reviews. Cochrane Database Syst. Rev. 2014:CD007768. doi: 10.1002/14651858.CD007768.pub3
Sabaté, E. (2003). Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization.
Schäfer-Keller, P., Garzoni, D., Dickenmann, M., and De Geest, S. (2010). Medikamentöse Nicht-Adhärenz–Prädiktive Faktoren und Diagnostik. Therapeutische Umschau 67, 283–288. doi: 10.1024/0040-5930/a000051
Schedlbauer, A., Davies, P., and Fahey, T. (2010). Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst. Rev. 2010:CD004371. doi: 10.1002/14651858.CD004371.pub3
Schlenk, E. A., Dunbar-Jacob, J., and Engberg, S. (2004). Medication non-adherence among older adults: a review of strategies and interventions for improvement. J. Gerontol. Nurs. 30, 33–43. doi: 10.3928/0098-9134-20040701-08
Staring, A. B., Mulder, C. L., Van Der Gaag, M., Selten, J.-P., Loonen, A. J., and Hengeveld, M. W. (2006). Understanding and improving treatment adherence in patients with psychotic disorders: a review and a proposed intervention. Curr. Psychiatry Rev. 2, 487–494. doi: 10.2174/157340006778699738
van Dulmen, S., Sluijs, E., van Dijk, L., de Ridder, D., Heerdink, R., and Bensing, J. (2007). Patient adherence to medical treatment: a review of reviews. BMC Health Serv. Res. 7:55. doi: 10.1186/1472-6963-7-55
van Eijken, M., Tsang, S., Wensing, M., de Smet, P. A., and Grol, R. P. (2003). Interventions to improve medication compliance in older patients living in the community. Drugs Aging 20, 229–240. doi: 10.2165/00002512-200320030-00006
Vermeire, E., Hearnshaw, H., Van Royen, P., and Denekens, J. (2001). Patient adherence to treatment: three decades of research. A comprehensive review. J. Clin. Pharm. Ther. 26, 331–342. doi: 10.1046/j.1365-2710.2001.00363.x
Vlasnik, J. J., Aliotta, S. L., and Delor, B. (2005). Medication adherence: factors influencing compliance with prescribed medication plans. Case Manager 16, 47–51. doi: 10.1016/j.casemgr.2005.01.009
Vrijens, B., De Geest, S., Hughes, D. A., Przemyslaw, K., Demonceau, J., Ruppar, T., et al. (2012). A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 73, 691–705. doi: 10.1111/j.1365-2125.2012.04167.x
Williams, A., Manias, E., and Walker, R. (2008). Interventions to improve medication adherence in people with multiple chronic conditions: a systematic review. J. Adv. Nurs. 63, 132–143. doi: 10.1111/j.1365-2648.2008.04656.x
Zeber, J. E., Manias, E., Williams, A. F., Hutchins, D., Udezi, W. A., Roberts, C. S., et al. (2013). A systematic literature review of psychosocial and behavioral factors associated with initial medication adherence: a report of the ISPOR medication adherence & persistence special interest group. Value Health 16, 891–900. doi: 10.1016/j.jval.2013.04.014
Keywords: medication adherence, intervention, patient determinants, theoretical domains framework, theory
Citation: Allemann SS, Nieuwlaat R, van den Bemt BJF, Hersberger KE and Arnet I (2016) Matching Adherence Interventions to Patient Determinants Using the Theoretical Domains Framework. Front. Pharmacol. 7:429. doi: 10.3389/fphar.2016.00429
Received: 18 August 2016; Accepted: 27 October 2016;
Published: 14 November 2016.
Edited by:
Bernard Vrijens, AARDEX Group, BelgiumReviewed by:
Nora Ibargoyen, Basque Office for Health Technology Assessment (Osteba), SpainCopyright © 2016 Allemann, Nieuwlaat, van den Bemt, Hersberger and Arnet. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samuel S. Allemann, cy5hbGxlbWFubkB1bmliYXMuY2g=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.