
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 26 February 2025
Sec. Pediatric Urology
Volume 13 - 2025 | https://doi.org/10.3389/fped.2025.1555402
This article is part of the Research Topic Urinary Lithiasis In Children View all 5 articles
Objectives: The purpose of this study was to describe the prolene suture-assisted cystoscopic removal of double J ureteral stents in infants and summarize the safety, operability, and effectiveness of this approach.
Methods: The clinic data of patients who underwent double J ureteral stent removal by prolene suture-assisted cystoscopy were reviewed. The operation procedure was as follows: First, a folded 4-0 prolene suture was preset into the cystoscope sheath, and the telescope was placed. Second, the cystoscopy was performed by inserting the cystoscope into the urinary bladder and finding the end of the double J ureteral stent under cystoscopy. Subsequently, the folded suture was pushed out of the sheath to form a coil that was used to hook 1–2 cm of the end of the stent. Finally, the stent was caught by tightening the prolene coil while the cystoscope was retracted into the cystoscope sheath; the removal was accompanied by exiting the cystoscope. Cystoscopy was repeated to confirm no additional damage.
Results: Overall, 15 double J ureteral stents were retrieved in 15 infants, whose average age was 3.78 ± 1.2 months, average weight was 5,951 ± 797 g, average residence time of the stents in the ureter was 31.20 ± 2.14 days, and the average operation time was 3.5 ± 1.2 min. No complications, such as urethral injury, occurred during the operation.
Conclusions: Prolene suture-assisted cystoscopy is one of the simple, safe, and effective technique for the removal of double J ureteral stents, especially suitable for infants or patient in whom the grasping forceps cannot pass through the matching cystoscope sheath.
Double J ureteral stent (DJUS), a commonly used ureteral stent, is widely retained in infant patients after pyeloplasty and cystoureteroplasty, and is removed by using grasping forceps under cystoscopy at 4–6 weeks after the said operation. However, in some young infants with a small urethra, especially male infants, the grasping forceps cannot pass through the matching cystoscope sheath, or a suitable cystoscope is not available. Some advanced techniques attempted to remove a DJUS have been reported in the literature (1–3). Nevertheless, these techniques have been associated with adverse effects, such as additional damage, infection, discomfort, and failure of stent removal. Herein, we describe a hitherto unreported technique involving the use of prolene suture for the removal of a DJUS; we believe the technique affords the advantages of simplicity, effectiveness, and safety, and would be a good option for stent removal.
This study was approved by the ethics committee of the Affiliated Hospital of Southwest Medical University (KY2023002). Clinical data of infants who underwent surgery for DJUS removal from January 2019 to June 2022 were reviewed. The inclusion criteria: (1) The ureteral stents were confirmed to be in proper position by x-ray and ultrasound; (2) no indicator of infection was detected in the blood and urine routine examination; and (3) the infant's urethra was too small for the use of a cystoscope with an operating channel for grasping forceps. Written informed consent was obtained from all infants' parents.
The patient was placed in a lithotomy position after being administered a combination of intravenous and inhalation anesthesia (0.5–2 mg/kg ketamine) followed by routine disinfection and towel laying. During the procedure, a folded prolene suture was preset into the cystoscope sheath (Hawk 8Fr, N4009), with the coil facing forward, and retrograde cystoscopy (Hawk, T0193) was performed to find the end of the DJUS after injecting tetracaine hydrochloride mortar into the urethra for lubrication. The coil was pushed into the bladder by sliding the telescope and hooked to 1–2 cm of the end of DJUS under cystoscopy. The DJUS was caught by tightening the prolene coil while the cystoscope was retracted into the cystoscope sheath and removed completely accompanied by exiting the cystoscope sheath. A 6Fr catheter was placed into the bladder to drain urine after performing repeated cystoscopy to confirm no additional damage (Figure 1).
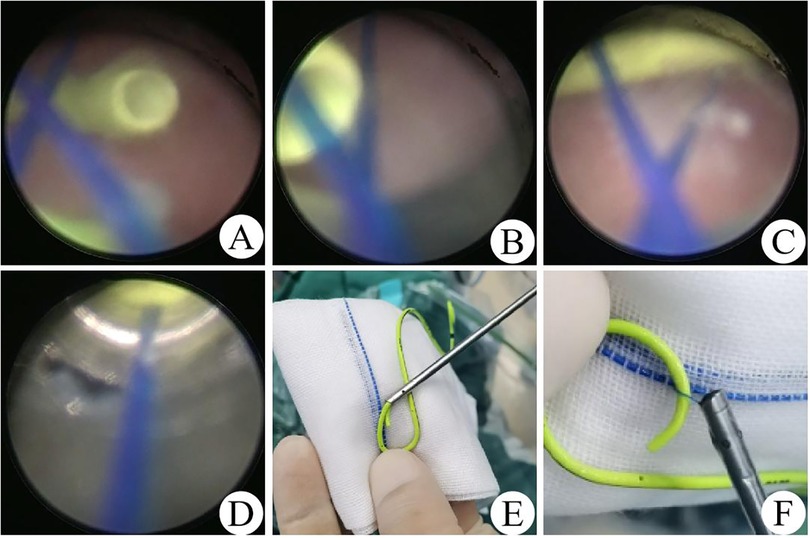
Figure 1. The process of prolene suture-assisted cystoscopic removal DJUS. (A) Find the end of the DJUS under cystoscopy. (B,C) Hook the end of the DJUS. (D) Tighten the prolene coil to the cystoscope sheath. (E) DJUS removal. (F) Grasp the DJUS.
All patients were sent to the postanesthesia care unit after the procedure. The operation time was calculated from the folding of the prolene suture until the removal of the DJUS. All patients were discharged and sent home after the removal of the urinary catheter on the second day of the operation.
A total of 15 patients, i.e., 15 boys, with an average age of 3.78 ± 1.2 months and an average weight of 5,951 ± 797 g were enrolled were enrolled, and they were underwent Laparoscopic Anderson-Hynes operation for the treatment of ureteropelvic junction obstruction (UPJO) due to grade 3 or higher hydronephrosis, meanwhile the DJUSs were implanted to prevent anastomotic stenosis and drain urine. After an average of 31.20 ± 2.14 days, 15 DJUSs were removed by prolene suture-assisted cystoscopy. The mean operation time was 3.5 ± 1.2 min (Table 1). There were no complications such as a urethral laceration or bladder perforation in any case.
Ureteral stents have been widely used in upper urinary tract surgery since the first report by Hepperlen et al. in 1978 (4). The DJUS is the most commonly used stent, and it is mainly used in surgeries for managing congenital ureteral malformations in children, such as ureteropelvic junction obstruction, ureterovesical junction obstruction and vesicoureteral reflux. When the hydroneurosis grade reached Ⅲ or above, and gradual thinning of the renal cortex was detected by serial ultrasound, especially a finding of <40% was obtained on diuretic renal scintigraphy, even infants needed active surgical treatment to prevent irreversible damage to renal function. Percutaneous nephrostomy and insertion of a DJUS into the renal pelvis through retrograde cystoscopy had been reported in the literature. However, there were some disadvantages such as secondary operation, easy infection, and recurrence after DJUS removal.
Pyeloplasty has become the gold standard in the treatment of ureteropelvic junction obstruction, since it was first described by Anderson and Hynes in 1949. With innovations in surgical instruments and suture materials, open, laparoscopic, and robot-assisted pyeloplasties have become more popular and safe for infants (5, 6). Hydronephrosis was significantly relieved after the operation, and maximum renal function was retained. Chandrasekharam et al. (7) showed that the improvement in renal function after laparoscopic pyeloplasty was better among infants than in older children. Regardless of the surgical method chosen, the DJUS is placed in the ureter to avoid anastomotic stricture, decrease postoperative leakage, maintain reliable urinary drainage, and facilitate anastomosis. The DJUS was removed by a forcep under cystoscopy 4–6 weeks after the operation, which has the advantages of direct vision and a 100% success ratec. However, some patients, especially male infants, were still too young and their urethra was too small for cystoscopy with the operating channel. Therefore, DJUS removal was tricky in such cases, and some investigators attempted to remove DJUS without cystoscope. Kajbafzadeh et al. (8) inserted the DJUS in the feeding tube and fixed it using a proline suture during the open pyeloureteroplasty, then, they secured the feeding tube to the external skin via an additional incision. Hadley et al. (9) inserted a kidney internal splint stent catheter into the ureter and one end was left on the back of the patient through a renal puncture during laparoscopic pyeloureteroplasty. Both of the aforementioned articles indicated that the ureteral stent could be removed in the clinic without cystoscopy by removing the exposed tube, because it was connected to the ureteral stent. However, there were some disadvantages of this approach, such as additional trauma, unintended stent removal, inconvenient nursing, and urinary tract infection would be increased due to the stents wad exposed outside the body. Lin et al. (2) and Shao et al. (3) used a simple self-made device comprising a monofilament suture was tied to the end of a 5Fr feeding tube to form an open loop, and removal the stent by noncystoscopic just received minimal nitrous oxide inhalational anesthesia or administered orally chloral hydrate of 0.5 ml/kg. However, two to three attempts were required for stent removal in approximately 13% of the patients treated thusly, and failure in some cases eventually necessitated cystoscopy or other methods. Further, attention needs to be paid to the potential risks associated with this approach, in that the feeding tube may become tangled to form a knot when it is in the bladder and multiple attempts might be required to untangle it, which in turn might injure the urethra, especially in infants with a small urethra. Kajbafzadeh et al. (1) used an extraction string, which was fixed on the DJUS, sutured to the subcoronal skin in male children or the inner surface of the labia majora in girls through the urethra. The stent was removed by pulling the string. However, the DJUS slipped unexpectedly in some cases, moving the suture inadvertently causes pain, and the suture in the urethra causes discomfort. The use of magnetic DJUS in children has also been reported (10). However, it is difficult to push the magnet through the ureterovesical junction, and the approach is only suitable for retrograde catheterization cases, such as vesico-ureteral reimplantation, which limits its application. Furthermore, magnetic DJUSs are more expensive (11).
Consequently, safe and easy removal of DJUS among patients in whom cystoscopy can be used without a forceps channel is an urgent problem due to some cystoscopes without matching sheaths. We drew inspiration from the process of roping horses with horse poles. Thus, we folded a 4-0 prolene suture to form a coil, which was achieved easily because of suture hardness. Then the coil was placed into the cystoscope sheath to make a device similar to the horse pole. Due to the smooth nature of the prolene suture, cystoscopy was not affected, and the prolene suture could be tightened freely. We immediately made a training device with a 3-mm trocar, a balloon filled with water, and a DJUS to simulate the urethra and bladder. After several training sessions, the DJUS could be removed smoothly with this approach. Therefore, we communicated this idea and related risks to the patients' parents. The parents agreed to go through with the procedure and provided signed informed consent. Then, we used the technique to remove the 15 DJUS (average procedure time: 3.5 ± 1.2 min) in 15 children, whose average age was 3.78 ± 1.2 months, without causing bladder or urethra injury.
Although we used additional cystoscopy to remove the DJUS compare with the other methods reported in the literature, the whole operation process was performed using the sheath and under cystoscopy. We believe that with this technique, there will be no damage to the bladder and urethra if the cystoscope is used correctly. Since infant tissue is too delicate to allow repeated procedures, minimizing blind operation is the safest approach. Our technology precisely follows such principles.
In summary, the key point of the new technique is to push the folded prolene coil into the bladder approximately 1 cm after the end of the DJUS. If there is a large amount of floc in the bladder, which leads to unclear visualization, it is necessary to rinse the bladder with normal saline until it can be clearly visualized. When the coil traps the end of the DJUS, it is not urgent to tighten the prolene coil. It is necessary to adjust the cystoscope angle along the radian of the stent, so that the coil can cover the stent for at least 1 cm. Then, the prolene suture is tightened; meanwhile, the cystoscope is pushed forward to prevent slippage between the prolene coil and DJUS, until the coil fixes the stent into the sheath. To accurately and rapidly grasp the DJUS, complete training in the laboratory in advance is a must. Fortunately, physicians with cystoscope operation experience can master the technique with two to three training sessions.
We described a safe, simple, and reliable procedure for removing ureteral stents, DJUSs, in small infants by using prolene suture-assisted cystoscopy. This technique is also suitable for patients in whom the grasping forceps cannot pass through the matching cystoscope sheath.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Clinical Research Management Committee of Affiliated Hospital of Southwest Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
XZ: Conceptualization, Methodology, Visualization, Supervision, Writing – original draft. NL: Funding acquisition, Project administration, Validation, Writing – review & editing. TL: Formal analysis, Investigation, Writing – review & editing. XW: Formal analysis, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Natural Science Project of Southwest Medical University (2020ZRQNB005).
The authors are grateful to the enrolled patients, their families and the referring physician.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kajbafzadeh AM, Nabavizadeh B, Keihani S, Hosseini Sharifi SH. Revisiting the tethered ureteral stents in children: a novel modification. Int Urol Nephrol. (2015) 47(6):881–5. doi: 10.1007/s11255-015-0963-7
2. Lin H, Xu M, Jiang D, Xu G, Fang X, Jia J, et al. Non-cystoscopic removal of retained ureteral stents with mild sedation in children. Urology. (2016) 94:255–8. doi: 10.1016/j.urology.2016.03.026
3. Shao H, Liu P, Zhang H, Chen C, Lin X. Noncystoscopic removal of retained ureteral stents in children: a retrospective study from a single-center. Medicine (Baltimore). (2018) 97(1):e9540. doi: 10.1097/MD.0000000000009540
4. Hepperlen TW, Mardis HK, Kammandel H. Self-retained internal ureteral stents: a new approach. J Urol. (1978) 119(6):731–4. doi: 10.1016/S0022-5347(17)57613-2
5. Chandrasekharam VVS, Babu R. A systematic review and meta-analysis of conventional laparoscopic versus robot-assisted laparoscopic pyeloplasty in infants. J Pediatr Urol. (2021) 17(4):502–10. doi: 10.1016/j.jpurol.2021.03.009
6. Polok M, Borselle D, Toczewski K, Apoznanski W, Jedrzejuk D, Patkowski D. Laparoscopic versus open pyeloplasty in children: experience of 226 cases at one centre. Arch Med Sci. (2020) 16(4):858–62. doi: 10.5114/aoms.2019.84496
7. Chandrasekharam VVS, Babu R, Arlikar J, Satyanarayana R, Murali Krishna N. Functional outcomes of pediatric laparoscopic pyeloplasty: post-operative functional recovery is superior in infants compared to older children. Pediatr Surg Int. (2021) 37(8):1135–9. doi: 10.1007/s00383-021-04914-1
8. Kajbafzadeh AM, Zeinoddini A, Ebadi M, Heidari R, Tajalli A. External extension of double-J ureteral stent during pyeloplasty: inexpensive stent and non-cystoscopic removal. Int Urol Nephrol. (2014) 46(4):671–6. doi: 10.1007/s11255-013-0594-9
9. Hadley DA, Wicher C, Wallis MC. Retrograde percutaneous access for kidney internal splint stent catheter placement in pediatric laparoscopic pyeloplasty: avoiding stent removal in the operating room. J Endourol. (2009) 23(12):1991–4. doi: 10.1089/end.2009.0170
10. Chalhoub M, Kohaut J, Vinit N, Botto N, Aigrain Y, Héloury Y, Lottman H, et al. Feasibility and safety of magnetic-end double-J ureteral stent insertion and removal in children. World J Urol. (2021) 39(5):1649–55. doi: 10.1007/s00345-020-03339-0
Keywords: cystoscopy, double J stent, infant, prolene suture, hydronephrosis
Citation: Zeng X, Lian N, Liu T and Wang X (2025) Prolene suture-assisted cystoscopic removal of double J ureteral stents in infants. Front. Pediatr. 13:1555402. doi: 10.3389/fped.2025.1555402
Received: 4 January 2025; Accepted: 30 January 2025;
Published: 26 February 2025.
Edited by:
Alberto Parente, Reina Sofia University Hospital, SpainReviewed by:
Javier Ordóñez Pereira, Gregorio Marañón Hospital, SpainCopyright: © 2025 Zeng, Lian, Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinhao Zeng, emVuZ3hpbmhhbzE5OTBAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.