- 1Department of Radiology, Jiaxing Maternity and Children Health Care Hospital, Affiliated Women and Children Hospital Jiaxing University, Jiaxing, China
- 2Department of Fetal Medicine Center, Jiaxing Maternity and Children Health Care Hospital, Affiliated Women and Children Hospital Jiaxing University, Jiaxing, China
- 3Department of Ultrasound, Jiaxing Maternity and Children Health Care Hospital, Affiliated Women and Children Hospital Jiaxing University, Jiaxing, China
The article reports a case of fetal imperforate hymen diagnosed by prenatal MRI and confirmed by postnatal surgery. The pregnant woman underwent routine 37-week ultrasound examination, which revealed an enlarged fetal bladder and an abdominal cystic mass. Subsequent 37-week + 6 prenatal MRI showed fetal uterine and vaginal fluid accumulation, suggesting congenital vaginal atresia. At 39 weeks + 5, under ultrasound guidance, amniotic, fetal abdominal, and vaginal cyst fluid were aspirated through a maternal abdominal puncture, avoiding the bowel. The cysts were significantly reduced in size, and the patient delivered vaginally at 39 weeks + 6. On postpartum day 1, pelvic MRI of the neonate showed normal uterine and cervical anatomy, with a lengthened, thickened vaginal wall and no fluid collection. On postpartum day 2, the patient underwent surgical exploration, which confirmed the diagnosis of imperforate hymen. Partial hymenectomy was performed without complication.
Introduction
Congenital imperforate hymen is a common congenital malformation of the female reproductive tract. It typically results from incomplete canalization of the urogenital sinus during fetal development, leading to failure of the hymen to fully perforate (1). Imperforate hymen often presents with symptoms such as primary amenorrhea, gradually worsening cyclic lower abdominal pain, and an enlarging lower abdominal mass during puberty. Severe cases may also be accompanied by a feeling of rectal fullness, constipation, urinary frequency, or urinary retention (2, 3).
Ultrasound is the main diagnostic method for prenatal diagnosis of fetal hymenal atresia, but it is easily affected by factors such as maternal and fetal position. Application of MRI in this case can help guide treatment for prenatal and postnatal patients with Imperforate Hymen. The maternal was informed that her case would be submitted for publication and provided consent.
Case report
A 29-year-old gravida 0, para 0, female patient at 37 weeks + 3 days (October 23, 2024) gestation presented to the Jiaxing Maternal and Child Health Care Hospital for routine prenatal ultrasound examination. The prenatal ultrasound revealed that the fetal bladder measured 4 mm × 64 mm × 83 mm (Figure 1), with internal septations and echogenic debris. The posterior wall of the bladder showed a 40 mm × 11 mm heterogeneous, slightly hyperechoic area. Bilateral umbilical arteries were visualized, and a 47 mm × 37 mm × 44 mm anechoic area was noted anterior to the left side of the bladder. No dilatation of the renal pelves or ureters was observed.

Figure 1. Fetal ultrasound at 37 weeks + 3 days the image shows a large cystic mass, approximately 64 mm × 83 mm in size, within the fetal pelvis. The cyst contents exhibit heterogeneous echogenicity.
The ultrasound diagnosis was fetal bladder enlargement with an associated abdominal cystic mass. At 37 weeks + 6 days, a fetal MRI was performed, which showed a cystic structure measuring approximately 100 mm × 50 mm × 57 mm posterior to the fetal bladder. The cyst had low signal on T1-weighted images and high signal on T2-weighted images, with heterogeneous internal signal. The inferior margin of the cyst showed a “reverse rabbit ear” sign. A uterus-like structure was connected to the superior aspect of the cyst, with a small amount of fluid within its cavity, measuring approximately 10 mm × 6 mm. Compression of the adjacent bowel and bladder was noted (Figure 2). The fetal MRI diagnosis was a fetal abdominal cystic structure, most likely representing an imperforate hymen with associated voluminous vaginal and uterine fluid collection, as well as localized vaginal septation or adhesions in the superior and inferior aspects of the vagina.
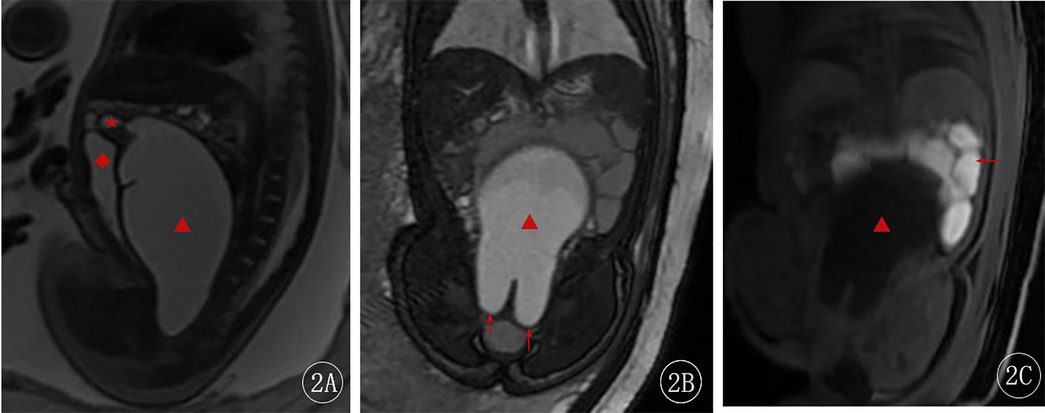
Figure 2. Fetal MRI at 37 weeks + 6 days. (A) Sagittal 2D FIESTA image—the red star (★) indicates the uterine cavity, and the red diamond (◆) shows the compressed bladder. (B) Coronal 2D FIESTA image—the red arrow points to the distal vaginal obstruction, showing the “reverse rabbit ear” sign. (C) Coronal LAVA-Flex image—the red arrow indicates the compressed bowel.
At 39 weeks + 5 days, under ultrasound guidance, a 20G spinal needle was inserted through the maternal abdominal wall, into the amniotic cavity, and then into the fetal abdominal cavity and vaginal cyst (avoiding the bowel). Turbid fluid was aspirated. Post-aspiration ultrasound showed significant reduction in the size of the cyst. The needle was removed, and the puncture site was covered with a dressing. Fetal heart rate remained stable at 138 bpm.
The cyst fluid cytology revealed numerous mature squamous epithelial cells. At 39 weeks + 6 days, the patient had a spontaneous vaginal delivery of a female neonate weighing 3,400 g, with an Apgar score of 10. The placenta was delivered spontaneously and intact. The patient had a first-degree perineal laceration that was repaired.
On postpartum day 1, pelvic MRI of the neonate showed normal uterine and cervical morphology, with an elongated and thickened vaginal wall, and no fluid collection (Figure 3). On postpartum day 2, the neonate underwent surgical exploration, which revealed a septum between the urethra and the vagina, with a completely covered vaginal orifice (imperforate hymen; Figure 4). A successful partial hymenectomy was performed.
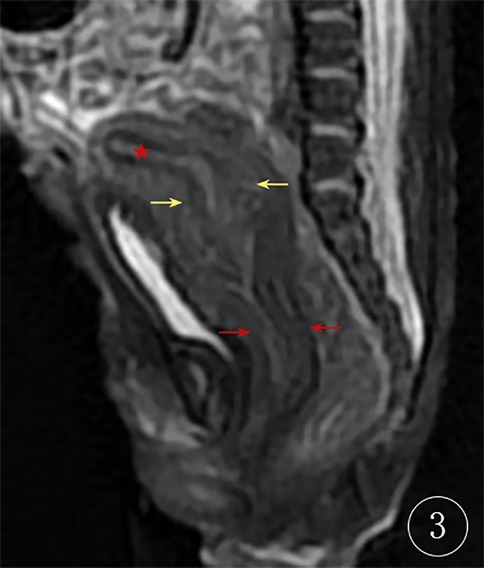
Figure 3. Neonatal MRI at 1 day postpartum the red star (★) represents the uterine cavity, the yellow arrow indicates the cervix, and the red arrow points to the thickened vaginal wall.

Figure 4. Intraoperative findings the image clearly demonstrates the diagnosis of imperforate hymen.
On postpartum day 7, the surgical site was healing well without erythema or swelling. Subsequent ultrasound showed no fluid collection in the uterus or vagina.
Discussion
Congenital imperforate hymen is a rare Müllerian duct anomaly resulting from the failure of the hymenal membrane to perforate during fetal development. It is one of the most common obstructive anomalies of the female reproductive tract, with an estimated incidence of 0.1%–0.5% in newborn females (4, 5). The condition often remains asymptomatic until adolescence, when patients typically present with primary amenorrhea, cyclic abdominal pain, and occasionally a palpable lower abdominal mass due to hematocolpos (accumulation of menstrual blood in the vagina) (5). In rare cases, it may be diagnosed prenatally or in infancy if associated with hydrocolpos (fluid accumulation in the vagina) due to maternal estrogen stimulation (4).
Prenatal ultrasound is an important tool for diagnosing fetal imperforate hymen. Ultrasound examination can reveal an anechoic area in the uterine cavity, as well as dilatation of the cervical canal extending to the vaginal orifice, with an anechoic area within (6). However, ultrasound findings can be influenced by factors such as fetal position and gestational age.
Fetal MRI, with its high resolution and ability to image in multiple planes and angles, is not affected by maternal or fetal positioning, and provides superior delineation of the detailed anatomy of the vagina and uterus for the diagnosis of imperforate hymen (7). In the present case, the fetal ultrasound was unable to clearly differentiate the bladder from the lesion, but the fetal abdominal MRI clearly visualized the dilated vagina and uterus, the distal vaginal obstruction (“reverse rabbit ear” sign), and the detailed anatomy of the uterus and vagina, providing a definitive diagnosis and guiding the treatment strategy.
The differential diagnosis of fetal imperforate hymen primarily includes transverse vaginal septum, vaginal atresia, and uterovaginal fluid accumulation (due to other causes) (8). On imaging, a transverse vaginal septum typically presents as fluid distension in the upper vaginal segment, with the septum located at a higher position, often near the cervix, distinguishing it from the distal obstruction seen in imperforate hymen (9). Vaginal atresia, on the other hand, is characterized by partial or complete absence of the vaginal canal, potentially associated with uterine developmental anomalies. Imaging reveals fluid accumulation in the upper vagina and uterus, with complete obstruction of the lower vaginal segment (10). Uterovaginal fluid accumulation due to other causes, such as cervical atresia or distal vaginal stenosis, requires precise localization of the obstruction via ultrasound or MRI (11). Imaging plays a pivotal role in differentiating these conditions, with imperforate hymen typically demonstrating obstruction at the distal vaginal level.
We described a case of a fetus with prenatal ultrasound-detected fetal pelvic cystic mass, which was further confirmed by MRI and underwent prenatal ultrasound-guided aspiration and drainage, followed by postnatal surgical treatment for hymenal atresia. In utero aspiration offers several potential benefits. Early decompression via drainage can alleviate pressure on fetal organs, potentially improving organ development and function (12). In cases of excessive fluid accumulation, which may lead to preterm labor, aspiration can help prolong gestation (13). Furthermore, early intervention may improve fetal survival rates and long-term prognosis in select cases. Finally, fluid obtained through aspiration allows for cytogenetic or biochemical analysis, aiding in the diagnosis of underlying conditions. It improves both fetal development and maternal well-being, making it a valuable intervention when performed by an experienced multidisciplinary team (14). In the present case, the patient had a strong desire for a vaginal delivery, but the enlarged fetal abdominal circumference could have complicated the delivery. Therefore, ultrasound-guided intrauterine aspiration was performed, which relieved the compression on the bladder and bowel, improving the patient's quality of life.
The postnatal management of imperforate hymen involves the prompt performance of a hymenotomy to establish an effective drainage pathway, prevent re-accumulation of fluid, alleviate pressure on surrounding organs, and avert long-term complications such as endometriosis, pelvic adhesions, or infertility (15, 16).
Conclusion
The definitive diagnosis provided by the fetal MRI in this case was crucial for guiding the subsequent treatment plan. The ultrasound-guided intrauterine aspiration facilitated a successful vaginal delivery and the patient's postpartum recovery. The postnatal hymenectomy prevented the risk of future complications. Although the postoperative recovery was smooth, the short follow-up period limits the assessment of long-term prognosis, which will require closer long-term monitoring.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical Committee of Maternity and Child Health Care Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
WB: Data curation, Funding acquisition, Project administration, Writing – original draft, Writing – review & editing. JG: Data curation, Writing – review & editing. JY: Data curation, Writing – review & editing. YW: Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Science and Technology Program of Jiaxing, Grant/Award Number: 2024AD30125.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hamouie A, Dietrich JE. Imperforate hymen: clinical pearls and implications of management. Clin Obstet Gynecol. (2022) 65:699–707. doi: 10.1097/GRF.0000000000000703
2. Ibishi VA, Latifi H, Ibishi L. Ultrasonographic examination and resolution of a pronounced hematocolpometra linked to an imperforate hymen: a detailed case study. Radiol Case Rep. (2023) 18:4119–22. doi: 10.1016/j.radcr.2023.08.098
3. Chubanovova N, Chmel R Jr, Kelcik R, Novakova J, Novackova M. Hymenal atresia - a rare congenital anomaly with the risk of late diagnosis. Ceska Gynekol. (2022) 87:118–23. doi: 10.48095/cccg2022118
4. Garcia Rodriguez R, Pérez González J, Garcia Delgado R, Rodriguez Guedes A, de Luis Alvarado M, Medina Castellano M, et al. Fetal hydrometrocolpos and congenital imperforate hymen: prenatal and postnatal imaging features. J Clin Ultrasound. (2018) 46:549–52. doi: 10.1002/jcu.22588
5. Tedyanto CP, Dewi S, Santoso FI, Ere MAP, Oeylex KR. A rare case report of a congenital imperforate hymen causing obstructive uropathy and constipation in an 11-year-old girl. Int Med Case Rep J. (2024) 17:985–9. doi: 10.2147/IMCRJ.S494697
6. Wang L, Chen L, Li D, Wang B, Yang Z. Characteristics of fetal physiological and pathological uterine effusion observed on prenatal ultrasonography: a case report. BMC Pregnancy Childbirth. (2022) 22:405. doi: 10.1186/s12884-022-04715-x
7. Berger-Chen SW, Amies Oelschlager AME. Diagnosis and management of hymenal variants: ACOG committee opinion, number 780. Obstet Gynecol. (2019) 133:e372–6. doi: 10.1097/AOG.0000000000003283
8. Berger-Chen SW, Amies Oelschlager AME. Management of acute obstructive uterovaginal anomalies: ACOG committee opinion, number 779. Obstet Gynecol. (2019) 133:e363–71. doi: 10.1097/AOG.0000000000003281
9. Shetty J, Pandey D, Reddy D. High imperforate transverse vaginal septum with vaginal cicatrisation: a surgical tribulation. BMJ Case Rep. (2024) 17:e257180. doi: 10.1136/bcr-2023-257180
10. Xu S, Zhang J, Wang S, Yang L, Qian J, Yue S, et al. MRI features and differential diagnoses of congenital vaginal atresia. Gynecol Endocrinol. (2019) 35:777–81. doi: 10.1080/09513590.2019.1588875
11. He H, Guo H, Han J, Wu Y, Zhu F. An atresia cervix removal, lower uterine segment substitute for cervix and uterovaginal anastomosis: a case report and literature review. Arch Gynecol Obstet. (2015) 291:93–7. doi: 10.1007/s00404-014-3361-y
12. Pellegrinelli JM, Kohler A, Kohler M, Weingertner AS, Favre R. Prenatal management and thoracoamniotic shunting in primary fetal pleural effusions: a single centre experience. Prenat Diagn. (2012) 32:467–71. doi: 10.1002/pd.3840
13. Duncombe GJ, Dickinson JE, Kikiros CS. Prenatal diagnosis and management of congenital cystic adenomatoid malformation of the lung. Am J Obstet Gynecol. (2002) 187:950–4. doi: 10.1067/mob.2002.127460
14. Benachi A, Vivanti AJ. Ethical issues in fetal therapies of life-threatening malformations. Eur J Pediatr. (2024) 184:110. doi: 10.1007/s00431-024-05922-8
15. Casey SR, Fang ME, Goytia K, Monestime G, Dietrich JE. Diagnostic accuracy of imperforate hymen at a single referral center. J Pediatr Adolesc Gynecol. (2025) 13:1–11. doi: 10.1016/j.jpag.2025.01.004
Keywords: imperforate hymen, fetus, ultrasonography, magnetic resonance imaging, prenatal
Citation: Bian W, Gu J, Yang J and Wang Y (2025) Intra- and extra-uterine diagnosis and treatment of peripartum imperforate hymen: a case report. Front. Pediatr. 13:1546721. doi: 10.3389/fped.2025.1546721
Received: 14 January 2025; Accepted: 17 March 2025;
Published: 31 March 2025.
Edited by:
Margherita Neri, University of Ferrara, ItalyReviewed by:
Kun Liu, Second Affiliated Hospital and Yuying Children's Hospital of Wenzhou Medical University, ChinaMazen Kurdi, King AbdulAziz University, Saudi Arabia
Copyright: © 2025 Bian, Gu, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Wang, d2FuZ3l1QG1haWwuemp4dS5lZHUuY24=
 Wei Bian
Wei Bian Jianmei Gu2
Jianmei Gu2