- 1Department of Orthopedics, Chongqing Key Laboratory of Pediatrics, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China
- 2Big Data Engineering Center (Medical Records Management Center), Chongqing Key Laboratory of Pediatrics, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China
- 3Department of Ultrasonography, Chongqing Key Laboratory of Pediatrics, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China
Introduction: Cannulated screws are widely used in pediatric orthopedic fixation. However, traditional screw removal requires preoperative x-ray positioning, leading to exposure to ionizing radiation. Sometimes, a larger incision is required, and trauma is a significant cause of x-ray positioning, which cannot be accurately marked on the skin. In this study, we aimed to evaluate the practicability of rapid removal of cannulated screws through a guide needle and small incision using ultrasound (US) guidance to locate the position of the screws accurately.
Methods: A retrospective analysis was performed on patients who underwent removal of internal fixation after proximal tibial fracture surgery at our hospital between January 2019 and March 2024. Patients were divided into Group A and Group B based on the different cannulated screw removal techniques. In Group A, the cannulated screws were removed under US guidance, while in Group B, they were removed under direct visualization using a traditional incision. The operative time, blood loss, success rate of removal, radiation frequency, and incision length were statistically analyzed. Knee function was evaluated using the Knee Society Score.
Results: 53 patients aged 15.3 ± 0.1 years were included in this study. Group A showed 50% shorter incision length (1.5 vs. 3.0 cm, p = 0.005) and average screw incisions (0.5 vs. 1.0 cm, p = 0.007), along with complete elimination of preoperative radiation exposure (0 vs. 2 times, p < 0.001) and dose (0 vs. 0.102 mGy, p < 0.001) compared to Group B. Participants in Group A had no postoperative complications, whereas one patient in Group B had an incision infection; however, no significant difference was observed between the groups.
Discussion: US-guided cannulated screw removal can be used in children with proximal tibial fractures, significantly reducing the preoperative radiation time and dose while minimizing the incisional length.
Level of evidence: III
Introduction
The cannulated screw can be easily placed percutaneously after closed reduction because it has a hollow structure that can be passed through the guide needle. It has been widely used in the fixation of pediatric fractures because it reduces patient trauma, such as femoral neck fracture (1, 2), tibial tuberosity fracture (3), epiphyseal fracture (4), and capitellum fracture (5). Metal implants can be selectively removed as they generally do not adversely affect the human body. However, experts recommend the removal of instrumentation because of concerns regarding the child's growth potential and life cycle (6). Additionally, internal fixation may cause pain, allergies, tissue irritation, and infection (7–10). The long-term presence of implants may result in stress concentration on the screw and stress shielding around the screw (11, 12). It may also lead to excessive trace metal content in the human body owing to the electrochemical interaction of metals (13, 14). Therefore, most surgeons prefer to remove internal fixations in children postoperatively.
With the development of ultrasound (US), its applications in orthopedics have increased (15), including screening for developmental dysplasia of the hip (DDH) (16, 17), tendon injury evaluation (18–20), fracture diagnosis (21), and intraoperative localization of foreign bodies in the body (22). A strong echo is observed when the ultrasonic waves hit the metal. Theoretically, the projection of the screw tail on the cortical bone surface onto the skin can be located using US. Chen et al. (22) successfully removed foreign bodies using US guidance combined with methylene blue labeling, thus reducing the radiation time, wound length, and operative time. Su et al. (23) performed a US-guided method for the closed reduction of radial neck fractures, reducing x-ray exposure and operative time. Chen et al. (24) diagnosed pain from excessive screw length in adults following total hip replacement using US. According to the literature reviewed, no studies have investigated US-assisted removal of cannulated screws in children.
In this study, we aimed to evaluate the advantages of US guidance in the postoperative removal of cannulated screws through a small incision compared to traditional surgery in children with tibial fractures.
Material and methods
Patients
A retrospective analysis was performed on children who underwent the removal of proximal tibial cannulated screw internal fixation at our hospital between January 2019 and March 2023. The cohort was stratified into group A and B according to the surgical approach for screw removal. Group A was treated with a small US-guided incision, whereas Group B was treated with a traditional incision.
The inclusion criteria were: (1) proximal tibial fractures fixed using cannulated screws, (2) age <18 years, (3) fresh fractures, and (4) complete fracture union. The exclusion criteria were: (1) simultaneous use of other types of internal fixation materials, (2) incomplete follow-up data, (3) pathological fractures, and (4) poor fracture healing. Written informed consent was obtained from all participants or their legal guardians for the publication of any potentially identifiable images or data included in this article. This study was approved by the our hospital's Ethics Committee (approval number: 2024−152) and was conducted in accordance with relevant guidelines and regulations.
Surgical procedures
All operations were performed by four attending doctors and one US localization doctor in our hospital. The US equipment used was produced by Mindray (TE9S; Shenzhen, China), with a probe model of L14-6 s and a frequency of 10 MHz.
Patients in Group A were scanned using a US probe near the incision at screw penetration before disinfection. The position of the screw tail was determined using a strong echo (Figure 1b), and its projected position on the skin surface was marked with a marker pen. After disinfection, a screw-guide needle with an appropriate diameter was inserted into the skin at the surface positioning center of the screw tail. The tail of the screw (metal friction) was detected. The tunnel of the cannulated screw was fully penetrated by shaking the needle from side to side and slightly adjusting the direction. Third, a small incision was made at the skin entry needle. The skin and subcutaneous tissues were separated using hemostatic forceps up to the tail of the screw. Finally, a cannulated screwdriver was inserted along the guide needle, the screw was removed by rotation, and the incision was stitched (Figure 1).
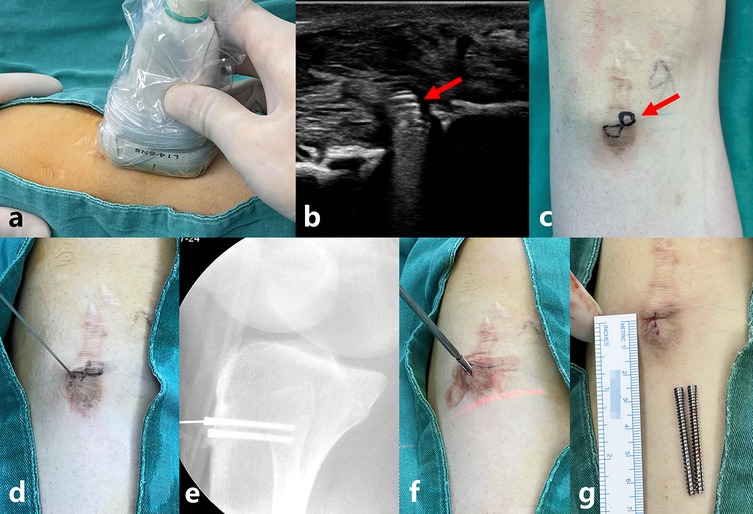
Figure 1. Shows a typical patient. A 13-year-old boy who came to remove the cannulated screws 14 months after right tibial tuberosity fracture surgery. He was injured because he tripped while running. (a) shows the position of the probe on the body surface. (b) shows the ultrasound image of the screw. The red arrow shows the screw tail. (c) shows the surface position of the screws. The red arrow shows the mark of the screw tail on the skin. (d) shows the penetration of the guide needle into the cannulated screw. (e) shows a radiograph confirming that the guide needle is inside the cannulated screw. Radiographs are not required after becoming proficient in surgical operations. (f) shows the placement of the screwdriver along the guide needle and the removal of the screw. (g) shows the incision being only 0.5 cm, and the screws were successfully removed.
In Group B, the protrusion of the screw tail was marked by palpation before disinfection. If the position of the screw tail could not be determined by palpation, posterior marking was confirmed using x-ray fluoroscopy. After disinfection and coverage with a sterile towel, the skin and subcutaneous tissue were cut along the original incision, screws were removed, and the incision was sutured. In patients in whom the screw deviated far from the incision, it was removed after a skin incision at the surface.
Postoperative evaluation: The operative time, average screw removal time, incision length, average screw incision length, number of internal fixations, blood loss, radiation time and dose before screw removal, hospital stay, and cost were recorded using the medical data of each group. The operative time encompassed both the US imaging and screw removal procedures. The mean screw removal time was calculated by dividing the operative time by the number of screws. The average screw incision length was calculated by dividing the incision length by the number of screws used. The wound condition was monitored within 5 days after surgery. The Knee Society Score was used to evaluate knee function 1 month after surgery. According to the score, they were divided into two groups: excellent (≥85 points) and poor (<85 points) (25).
Statistical analysis
All data were analyzed using SPSS 26.0 (IBM Corp., Armonk, NY, USA). Non-normally distributed data were expressed as median and quartile. Continuous variables were tested using the non-parametric Mann–Whitney U-test, while categorical variables were tested using the chi-square test. P < 0.05 was considered statistically significant.
Results
Patient characteristics
The study included 53 patients with a mean age of 15.3 ± 0.1 years, 10 in Group A, aged 15.1 (14.6–16.2) years, and 43 in Group B, aged 15.3 (14.5–15.9) years. Age did not significantly differ between the two groups.
Radiation exposure analysis
Group A had a preoperative radiation time of 0 min, which was significantly lower than that of Group B (P < 0.001). The preoperative radiation dose in group A was 0 mGy, which was significantly lower than that in group B (P < 0.001).
Surgical outcomes
The average incision length of Group A was 1.5 (1–2.25) cm, which was shorter than that in Group B (P = 0.005). The average screw incision length in Group A was 0.5 (0.46–1) cm, which was shorter than that in Group B (P = 0.007). All incisions in Group A healed well, and one patient in Group B showed redness and swelling. No statistically significant differences were observed between the two groups in terms of operative time, mean screw removal time, blood loss, hospitalization days, and hospitalization cost (Table 1). Despite the higher localization costs in Group A compared with Group B, the total hospitalization costs for patients showed no significant difference between the two groups.
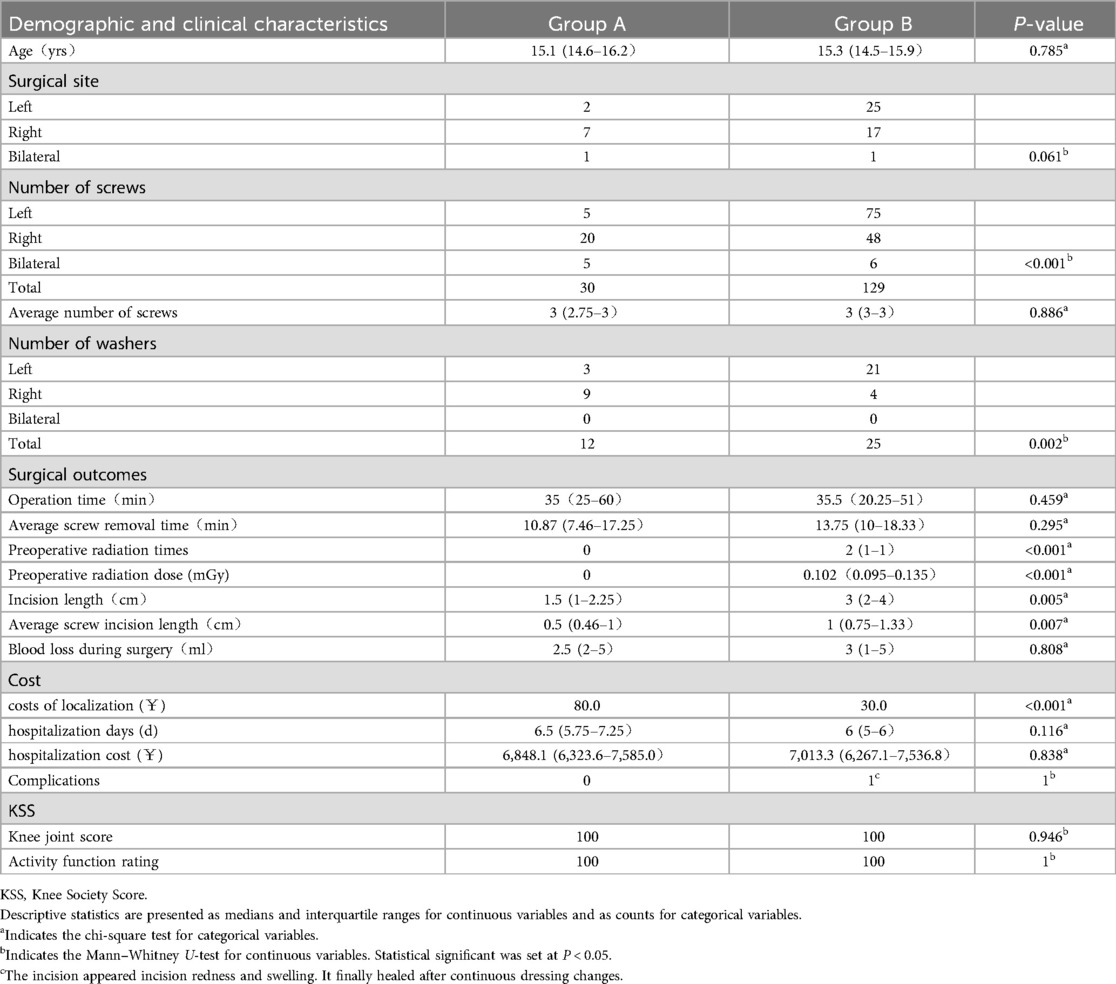
Table 1. Patients’ demographic characteristics, surgery evaluation, hospitalization costs, complications and KSS.
Discussion
This study proved that US-guided removal of cannulated screws in the proximal tibia effectively reduces radiation time, radiation dose, and surgical incision compared to traditional surgery.
US, as a non-invasive and radiation-free imaging modality with rapid scanning capability, is unlikely to induce thermal tissue damage (26, 27). To the best of our knowledge, no previous studies have investigated the adverse effects of US. US can dynamically observe the morphology of bone and muscle tissues. Numerous studies have reported its wide application in orthopedics. For example, Dong et al. (16) and Xiao et al. (17) identified the risk factors for DDH while using US in DDH diagnosis. They believed that US played an important role in the early diagnosis, treatment, and follow-up of DDH. Snelling et al. (21) confirmed that US had high accuracy in diagnosing fractures in 135 children with distal forearm injuries. A previous study (28) reported that US is a highly sensitive and accurate tool for detecting radiolucent foreign bodies. Jia et al. (29) reported using US-guided closed reduction and internal fixation for ulnar and radial fractures in children, which could reduce radiation dose and operative time. Su et al. (23) reported US-guided treatment of pediatric radial neck fractures. US can help avoid injury to the posterior interosseous nerve of the radius by providing a precise location. When ultrasonic waves hit metal, they produce a strong echo with accompanying acoustic shadows (Figure 2). Chen et al. (24) reported two patients experiencing pain after total hip replacement. They found an acetabular screw protruding from the ischium on US examination, and the pain significantly improved after screw removal. Therefore, US localization of screws in vivo is feasible. To date, we have not found any studies related to the minimally invasive removal of cannulated screws after US positioning.
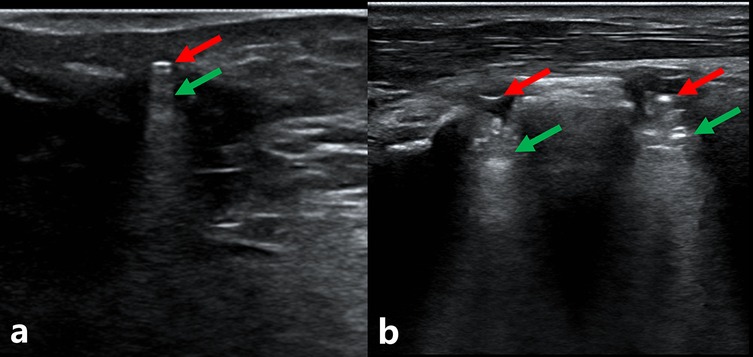
Figure 2. Displays the ultrasound images of a 15-year-old boy with three cannulated screws in his right tibia. (a) shows one of the screws. (b) shows the other two screws in one scan. The red arrow shows that the strong echo produced by the ultrasonic hits the screw tail. The green arrow refers to the acoustic shadow below the screw tail.
Radiation exposure and damage in children cannot be ignored (30–34). We concur with the principle that radiation exposure should be minimized during pediatric surgery (35), even though the dose of radiation that causes cancer is currently controversial. According to Su et al. (23), the fracture site of the radial neck and Kirschner wire can be dynamically observed using US guidance. Using US guidance for the closed reduction of radial neck fractures in children can significantly reduce the time and dose of radiation compared to reduction under x-ray fluoroscopy. Shen et al. (36) reported a method for closed reduction of lateral humeral condyle fractures in children assisted by US without intraoperative x-ray fluoroscopy and achieved satisfactory results in fracture reduction and elbow joint function. Various methods exist to locate the screw tail during cannulated screw removal; for example, the screw tail can be palpated on the body surface. However, most tibial tubercles are in athletic adolescents with thick subcutaneous fat, and it is difficult to touch the screw tail accurately by palpation. Sometimes, misjudgment may occur because of blocking of the periosteum or scarring, rendering the method inaccurate. Multi-angle fluoroscopy, often required 1–3 times, facilitates accurate positioning because fluoroscopy produces a planar image. In this study, the US positioning method was used to dynamically scan the cortical bone of the surgical area, and the screw tail could be accurately located according to the “strong echo” and reduced radiation exposure.
Accurate localization of the surgical site can shorten the surgical incision. Chen et al. (22) documented US-guided removal of foreign bodies on the body surface. Using US to locate the foreign body, methylene blue was injected around the foreign body for labeling under dynamic US monitoring. The incision length in 11 patients was 1.21 ± 0.13 cm, significantly shorter than that of the control group. Li et al. (37) reported on 85 patients who underwent long tubular bone internal fixation removal, with 40 patients undergoing minimally invasive methods resulting in an average incision length of 5.07 ± 1.18 cm, significantly shorter than that of the traditional group. However, x-ray fluoroscopy is required during surgery, and metal plates are used for internal fixation material. As mentioned previously, locating screws at superficial sites during cannulated screw removal can be challenging. Traditional screw removal methods involve cutting the original scar and removing the screw under direct visualization. The surgery is simple; however, the incision is long. Sometimes, repeated exploration is necessary to locate the screw, or the incision may need to be extended if the screw placement point is far from the incision. Traditional surgery may require a larger incision than previous surgery, which undoubtedly increases surgical trauma. The method used in this study reduced surgical trauma. The screw was removed under US guidance, and the average screw incision length was only 0.5 cm, equivalent to the diameter of the cannulated screw tail and significantly shorter than that of the control group. This reduction is attributed to precise incision placement after determining the position of the screw tail using US, thus avoiding prolongation of the incision owing to inaccurate positioning to reduce trauma.
A guide needle was used to probe the screw to determine its position. The specific method is to use a guide needle to “scan” the puncture near the screw. When metal friction was felt, the direction was adjusted by slight shaking, and the central tunnel of the screw was inserted. A small incision was made at the skin puncture site, and the screw was removed using a matching cannulated screwdriver under the guidance of a guide needle. This method involves a small incision and can accurately locate the position of the screw; multiple punctures are sometimes required to locate the tail of the screw, which requires more time and increases acupuncture trauma.
Less tissue dissection results in less bleeding. No significant difference was observed in the amount of bleeding between the two groups in this study. Since the study population included patients with proximal tibial fractures, we used a tourniquet during surgery. The only bleeding event that occurred during the operation involved oozing blood from the nail tract, and the amount of bleeding was low. According to Li et al. (37), the internal fixation of the metal plate was removed through a minimally invasive incision. The intraoperative and postoperative blood loss were 103.10 ± 24.44 ml and 44.30 ± 10.93 ml, respectively, significantly less than that of traditional incision removal of internal fixation. This reduction is because a minimally invasive approach reduces the incision length and exposes less tissue. We believe that in patients in whom a tourniquet is missing or cannot be used, such as those with cannulated screws at the femoral neck, bleeding will be reduced owing to smaller wounds relative to traditional open removal.
This method is considered feasible for the removal of deep cannulated screws, including those after femoral neck fracture. US techniques can guide the insertion of a guide needle into the interior of the cannulated screw and remove the internal fixation through a small incision. This approach avoids excessive exposure of the fascia lata and deep tissues. Theoretically, it can reduce the incision, amount of bleeding, and suture time.
Certain difficulties may be encountered during the operation. First, the screw tail is covered by soft tissue, which causes the driver to fail to engage smoothly. However, under the guidance of a guide needle, the screwdriver was gently rotated to the left and right when it reached the screw. Simultaneously, pressure was applied to extrude the soft tissue and engage the screwdriver with the nut. Second, removing screws using washers is more difficult; it requires a detailed preoperative review of the medical records of the previous operation and a careful examination of the radiographs to determine the presence of the washer. In patients with washers, we probed the washer deep along the screw using a vascular clamp or stripper before completely removing the screw. Subsequently, the washer and the screw was removed.
Our study had some limitations. First, the learning curve is long, requiring surgeons to have imaging knowledge and the ability to recognize US images. Young residents may not be able to fully grasp the direction of the guide needle, resulting in a situation in which the guide needle cannot locate the screw tail or becomes bent. Based on our experience, it took approximately 5–10 cases for the surgical team to achieve proficiency, making the screw removal time using US equivalent to that using fluoroscopy. Second, the sample size was small; hence, more patients from multiple centers are required for verification. Third, this study was retrospective; thus, further prospective double-blind controlled studies are required. Lastly, the participants were inconsistent, resulting in differences in the timing of the surgical procedure.
Conclusion
US-guided cannulated screw removal can significantly reduce the amount of preoperative radiation, radiation dose, and length of incision. It is an optional surgical method.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Children's Hospital of Chongqing Medical University (IRB approval number: 2024-152). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. All human images included in the study were obtained with the informed consent of the participants or their legal guardians.
Author contributions
KG: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. JQ: Methodology, Writing – review & editing. MG: Methodology, Writing – original draft. RC: Methodology, Writing – original draft. JC: Data curation, Writing – original draft. FQ: Data curation, Writing – original draft. YZ: Methodology, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank the anesthesiology department for providing ultrasound equipment.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pavone V, Testa G, Riccioli M, Di Stefano A, Condorelli G, Sessa G. Surgical treatment with cannulated screws for pediatric femoral neck fractures: a case series. Injury. (2019) 50(Suppl 2):S40–s4. doi: 10.1016/j.injury.2019.01.043
2. Kumar I, Ahmed W, Roshan R, Kumar S, Bhadani JS. Traumatic bilateral neck of femur fracture in paediatric age: a case report and review of literature. Med J Armed Forces India. (2023) 79(Suppl 1):S307–s10. doi: 10.1016/j.mjafi.2022.01.006
3. Pace JL, McCulloch PC, Momoh EO, Nasreddine AY, Kocher MS. Operatively treated type IV tibial tubercle apophyseal fractures. J Pediatr Orthop. (2013) 33(8):791–6. doi: 10.1097/BPO.0b013e3182968984
4. Seidenstein AH, Torrez TW, Garcia JA, Awad SK, Debell H, Gilbert SR, et al. Delayed presentation of popliteal artery injury after salter-harris III proximal tibia fracture. Case Rep Orthop. (2023) 2023:4104127. doi: 10.1155/2023/4104127
5. Ong KL, Mahadev A. Cannulated cancellous screw fixation for capitellum fractures in adolescents. J Orthop Surg (Hong Kong). (2011) 19(3):346–9. doi: 10.1177/230949901101900317
6. Hanson B, van der Werken C, Stengel D. Surgeons’ beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord. (2008) 9:73. doi: 10.1186/1471-2474-9-73
7. VanPelt MD, Athey A, Yao J, Ennin K, Kassem L, Mulligan E, et al. Is routine hardware removal following open reduction internal fixation of tarsometatarsal joint fracture/dislocation necessary? J Foot Ankle Surg. (2019) 58(2):226–30. doi: 10.1053/j.jfas.2018.08.016
8. Davison BL. Refracture following plate removal in supracondylar-intercondylar femur fractures. Orthopedics. (2003) 26(2):157–9. doi: 10.3928/0147-7447-20030201-17
9. Gamble JG, Ziino C, Imrie MN, Young JL. Trans-metaphyseal screws placed in children: an argument for monitoring and potentially removing the implants. J Pediatr Orthop. (2019) 39(1):e28–31. doi: 10.1097/BPO.0000000000001280
10. Montgomery BK, Gamble JG, Kha ST, Hecht GG, Vorhies JS, Lucas JF. Indications for and risks associated with implant removal after pediatric trauma. J Am Acad Orthop Surg Glob Res Rev. (2022) 6(4):e22.00050. doi: 10.5435/JAAOSGlobal-D-22-00050
11. Wu L, Sun J, Fang N, Peng Q, Gao S, Liu L. Should cannulated screws be removed after a femoral neck fracture has healed, and how? A finite element analysis of the femur before and after cannulated screw removal. Int Orthop. (2022) 46(10):2393–403. doi: 10.1007/s00264-022-05516-9
12. Kelly B, Heyworth B, Yen YM, Hedequist D. Adverse sequelae due to plate retention following submuscular plating for pediatric femur fractures. J Orthop Trauma. (2013) 27(12):726–9. doi: 10.1097/BOT.0b013e31829089e1
13. Kasai Y, Iida R, Uchida A. Metal concentrations in the serum and hair of patients with titanium alloy spinal implants. Spine (Phila Pa 1976). (2003) 28(12):1320–6. doi: 10.1097/01.BRS.0000065482.41115.B4
14. Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. (1998) 80(2):268–82. doi: 10.2106/00004623-199802000-00015
15. Matasović T. Dijagnosticki ultrazvuk u ortopediji [Diagnostic ultrasound in orthopedics]. Lijec Vjesn. (1991) 113(5-6):172–8.
16. Dong TT, Nie F, Yang LL, Wang T. Ultrasonography in the evaluation of various factors of developmental dysplasia of the hip in infants: results from a retrospective study in a large hospital of northwest China. J Orthop Sci. (2024) 29(4):976–82. doi: 10.1016/j.jos.2023.05.009
17. Xiao H, Tang Y, Su Y. Risk factors of developmental dysplasia of the hip in a single clinical center. Sci Rep. (2022) 12(1):19461. doi: 10.1038/s41598-022-24025-8
18. Obeidat N, Al-Mnayyis A, Essa SB, Alkhatatba M, Al Qudah H, Aljarrah MM, et al. Early career accuracy of shoulder ultrasound in evaluating rotator cuff tendon tears. Med Glas (Zenica). (2024) 21(1):190–5. doi: 10.17392/1702-23
19. Horvat U, Kozinc Ž. The use of shear-wave ultrasound elastography in the diagnosis and monitoring of musculoskeletal injuries. Crit Rev Biomed Eng. (2024) 52(2):15–26. doi: 10.1615/CritRevBiomedEng.2023049807
20. Hallgren HB, Nicolescu D, Törnqvist L, Casselgren M, Adolfsson L. Ultrasound examination of acute soft tissue lesions in the elbow has good intra rater reliability and acceptable agreement with MRI. J Shoulder Elbow Surg. (2024) 33(7):1615–23. doi: 10.1016/j.jse.2024.01.050
21. Snelling PJ, Jones P, Bade D, Gillespie A, Keijzers G, Ware RS. Ultrasound secondary signs for the diagnosis of pediatric distal forearm fractures: a diagnostic study. Ultrasound Med Biol. (2024) 50(6):898–907. doi: 10.1016/j.ultrasmedbio.2024.02.015
22. Chen K, Wang M, Su Y. Foreign body removal with the assistance of ultrasound guidance and methylene blue staining in children-a cohort study. Int Orthop. (2022) 46(8):1831–8. doi: 10.1007/s00264-022-05427-9
23. Su Y, Jin C, Duan X, Wang J, Li K. Treatment of displaced radial neck fractures under ultrasonographic guidance in children. Int Orthop. (2020) 44(11):2337–42. doi: 10.1007/s00264-020-04630-w
24. Chen CC, Cheng HY, Shih KS, Hou SM. Ultrasound-diagnosed screw protrusion in total hip arthroplasty: a case report and literature review. Asian J Surg. (2024) 47(3):1403–5. doi: 10.1016/j.asjsur.2023.11.101
25. Ryd L, Kärrholm J, Ahlvin P. Knee scoring systems in gonarthrosis. Evaluation of interobserver variability and the envelope of bias. Score assessment group. Acta Orthop Scand. (1997) 68(1):41–5. doi: 10.3109/17453679709003973
26. O'Brien WD Jr, Deng CX, Harris GR, Herman BA, Merritt CR, Sanghvi N, et al. The risk of exposure to diagnostic ultrasound in postnatal subjects: thermal effects. J Ultrasound Med. (2008) 27(4):517–35. quiz 37-40. doi: 10.7863/jum.2008.27.4.517
27. Rowlands R, Rippey J, Tie S, Flynn J. Bedside ultrasound vs x-ray for the diagnosis of forearm fractures in children. J Emerg Med. (2017) 52(2):208–15. doi: 10.1016/j.jemermed.2016.10.013
28. Tahmasebi M, Zareizadeh H, Motamedfar A. Accuracy of ultrasonography in detecting radiolucent soft-tissue foreign bodies. Indian J Radiol Imaging. (2014) 24(2):196–200. doi: 10.1055/s-0041-1734408
29. Jia S, Wang J, Yu B, Xu C, Li K. Ultrasound assistance in treatment with elastic stable intramedullary nail fixation in radial and ulnar fractures in children. Int Orthop. (2023) 47(3):773–9. doi: 10.1007/s00264-022-05683-9
30. Kaçar Güveli T, Özkan S, Öner Tamam M, Uyanık E, Ediz N, Mülazımoğlu M, et al. The effect of high dose radioiodine therapy on formation of radiation retinopathy during thyroid cancer treatment. Mol Imaging Radionucl Ther. (2014) 23(3):84–8. doi: 10.4274/mirt.33042
31. Dorman T, Drever B, Plumridge S, Gregory K, Cooper M, Roderick A, et al. Radiation dose to staff from medical x-ray scatter in the orthopaedic theatre. Eur J Orthop Surg Traumatol. (2023) 33(7):3059–65. doi: 10.1007/s00590-023-03538-6
32. Bratschitsch G, Leitner L, Stücklschweiger G, Guss H, Sadoghi P, Puchwein P, et al. Radiation exposure of patient and operating room personnel by fluoroscopy and navigation during spinal surgery. Sci Rep. (2019) 9(1):17652. doi: 10.1038/s41598-019-53472-z
33. Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond). (2005) 55(6):498–500. doi: 10.1093/occmed/kqi048
34. Foucault A, Ancelet S, Dreuil S, Caër-Lorho S, Ducou Le Pointe H, Brisse H, et al. Childhood cancer risks estimates following CT scans: an update of the French CT cohort study. Eur Radiol. (2022) 32(8):5491–8. doi: 10.1007/s00330-022-08602-z
35. Connolly B, Racadio J, Towbin R. Practice of ALARA in the pediatric interventional suite. Pediatr Radiol. (2006) 36 Suppl 2(Suppl 2):163–7. doi: 10.1007/s00247-006-0192-4
36. Li XT, Shen XT, Wu X, Wang S. Ultrasound-assisted closed reduction and percutaneous pinning for displaced and rotated lateral condylar humeral fractures in children. J Shoulder Elbow Surg. (2021) 30(9):2113–9. doi: 10.1016/j.jse.2021.01.031
Keywords: bone screws, ultrasound, child, minimally invasive surgery, cannulated bone screw
Citation: Gu K, Qin J, Guo M, Chu R, Chen J, Qian F and Zhong Y (2025) The application of ultrasound-guided cannulated screw removal after proximal tibial fracture surgery: a retrospective study. Front. Pediatr. 13:1535675. doi: 10.3389/fped.2025.1535675
Received: 3 December 2024; Accepted: 31 March 2025;
Published: 15 April 2025.
Edited by:
Stefano Marco Paolo Rossi, Fondazione Poliambulanza Istituto Ospedaliero, ItalyReviewed by:
Oussama Abousamra, Children's Hospital of Los Angeles, United StatesFrancesco Pelillo, San Matteo Hospital Foundation (IRCCS), Italy
Copyright: © 2025 Gu, Qin, Guo, Chu, Chen, Qian and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Zhong, MzU3Njc3NTg0QHFxLmNvbQ==
 Kai Gu1
Kai Gu1 Yi Zhong
Yi Zhong