- 1Carver College of Medicine, University of Iowa, Iowa City, IA, United States
- 2Stead Family Department of Pediatrics-Cardiology, University of Iowa, Iowa City, IA, United States
- 3CHRISTUS Children’s Hospital, Baylor College of Medicine, San Antonio, TX, United States
Introduction: Congenital heart defects (CHDs) often involve complex anatomical structures that can be challenging for patients and their families to understand. While physicians utilize various imaging techniques such as cardiac echocardiograms, CT scans, and MRIs to comprehend these complexities, the information is typically conveyed to patients and families through two-dimensional (2D) images and drawings. Traditional methods often fail to fully capture the intricate nature of CHDs. This study compared the effectiveness of 2D imaging with three-dimensional (3D) virtual and 3D printed models in enhancing the understanding of CHDs among patients and their families.
Methods: Family members of patients with congenital heart disease, as well as patients aged 15 years or older, were recruited for the study. Participants were presented with an echocardiogram of their specific cardiac defect alongside an echocardiogram of a structurally normal heart for comparison. They were then randomly assigned to receive education using a 3D printed model or a 3D virtual model of their heart defect. Participants' knowledge of normal cardiac anatomy and the anatomy of their specific cardiac defect was assessed after viewing the echocardiogram (2D image) and again after reviewing the 3D models.
Results: One-hundred-nine subjects participated in the study, comprising 79 family members (72.5%) and 30 patients (27.5%). Subjects showed significant improvement in their understanding of normal cardiac anatomy with both 3D printed and 3D virtual models compared to the 2D image (p = 0.022 and p = 0.012, respectively). Among the subjects, 70% in the 3D printed group and 84% in the 3D virtual group indicated a preference for the 3D models over the 2D image. Both the 3D printed, and 3D virtual model groups rated themselves as having an increased understanding of normal cardiac anatomy compared to the 2D images (p = 0.009 and p < 0.001, respectively).
Discussion: These findings suggest that incorporating 3D models into the educational process for patients with congenital heart disease can lead to improved comprehension and greater satisfaction.
Introduction
Congenital heart diseases (CHDs) affect nearly 1% of births each year, with 25% of these patients having a critical defect needing surgery or other interventions (1, 2). There are various types of congenital heart defects (CHDs), which can be categorized based on the location and nature of the defects. One method of categorization includes: CHDs involving only the large blood vessels: These defects occur outside the heart chambers and primarily affect the major arteries and veins, CHDs involving only the heart chambers: These defects are confined to the atria or ventricles of the heart and CHDs involving multiple structural abnormalities: These defects affect both the large blood vessels and the heart chambers, leading to complex congenital heart conditions (3).
Given the prevalence and severity of CHDs, it is crucial to effectively communicate information about the defect to patients and their families. Currently, counseling happens using two-dimensional (2D) images, such as echocardiograms or pictures. While these 2D images can quickly review the anatomy of a patient's defect, they often provide a superficial view of the condition. In contrast, recent advancements in three-dimensional (3D) models offer a more detailed perspective, allowing observers to hold, rotate the model and appreciate the complex anatomy of CHDs.
These new models can be used in clinics to educate patients and families about their complex cardiac conditions. One study found that instruction in clinics with 3D printed models led to an increase in 5 min per visit, which was not perceived as a significant hindrance, especially given the increase in satisfaction gained from the use of these models (4). Biglino and colleagues used a focus group approach to gather information from patients, parents, clinicians and nurses about the usefulness and potential limitations of 3D models. All four groups believed that the 3D models would be beneficial for CHD education. Interestingly, parents indicated that they preferred a patient specific model as opposed to a more generic lesion specific model (5).
Previous studies have shown that using 3D printed models to counsel family members about CHDs can produce results equal to or better than current 2D drawings (6, 7). Additional studies have demonstrated the utility of 3D printed models in preoperative consultations (8), educating and training physicians (9–12) and planning for surgical intervention (13–16).
However, gaps in the literature exist regarding the comparative effectiveness of 3D printed and 3D virtual models, particularly when tested with patients and family members dealing with complex CHDs. One study in 2021 by Awori and colleagues compared 3D printed and 3D virtual models, but only tested these models in medical personnel and parents, patients were not included in the study (17). Additionally, the number of parents that were included was relatively small at 20 subjects. The authors found that the parents perceived understanding with 3D printed and 3D virtual models were significantly higher than traditional 2D images, and that 3D printed models were more useful than digital ones. While this study was instrumental in comparing the differences between 3D printed and 3D virtual models, it lacked a comparison of the two models in both patient and family education.
Both 3D printed and 3D virtual models can be used to educate patients and their families about CHDs, each with its own strengths and weaknesses. 3D printed models allow for physical manipulation, providing a tactile learning experience, whereas 3D virtual models are accessible through a computer or phone screen. However, 3D printing is expensive and time-consuming, and only one person can access the model at a time. In contrast, 3D virtual models are an easy-to-access and inexpensive alternative, allowing multiple people to view and interact with the model simultaneously. Importantly, these models can be accessed by patients and family members at any time via a QR code, enabling them to educate others, such as friends and relatives.
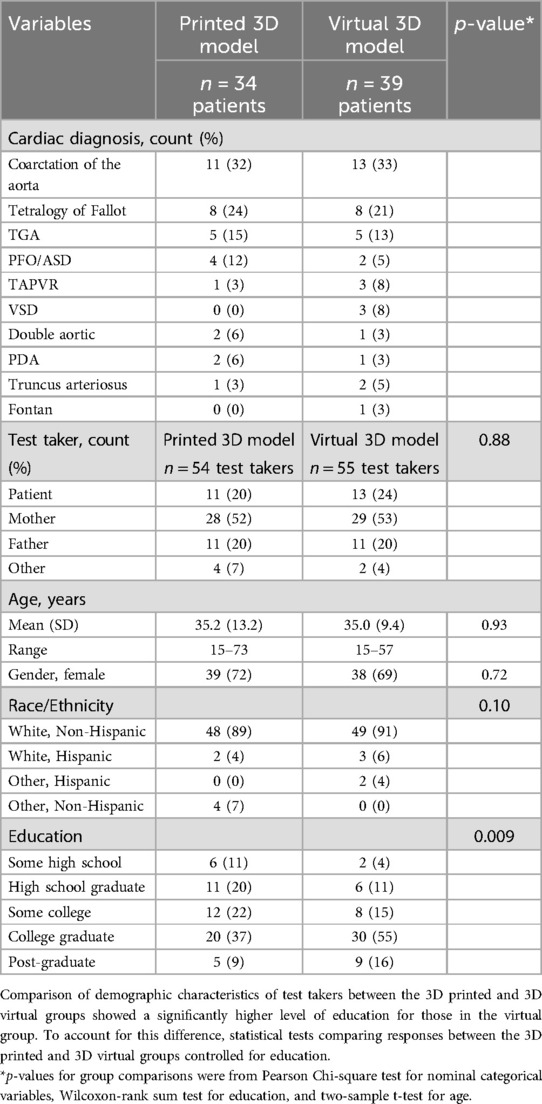
This study evaluated the differences between 3D printed and 3D virtual models in improving patient and family's knowledge of complex CHDs. We also compared the effectiveness of 2D cardiac models and 3D models on the same measures. The most common CHDs that subjects experienced were coarctation of the aorta, tetralogy of Fallot, and transposition of the great arteries (see Table 1 for the complete list). We hypothesized that 3D heart models would significantly improve participants' knowledge of CHD anatomy and normal heart anatomy compared to traditional 2D imaging. Additionally, we hypothesized that 3D virtual models would lead to significantly better performance compared to 3D printed models in terms of educating patients and family members.
Methods
Model creation
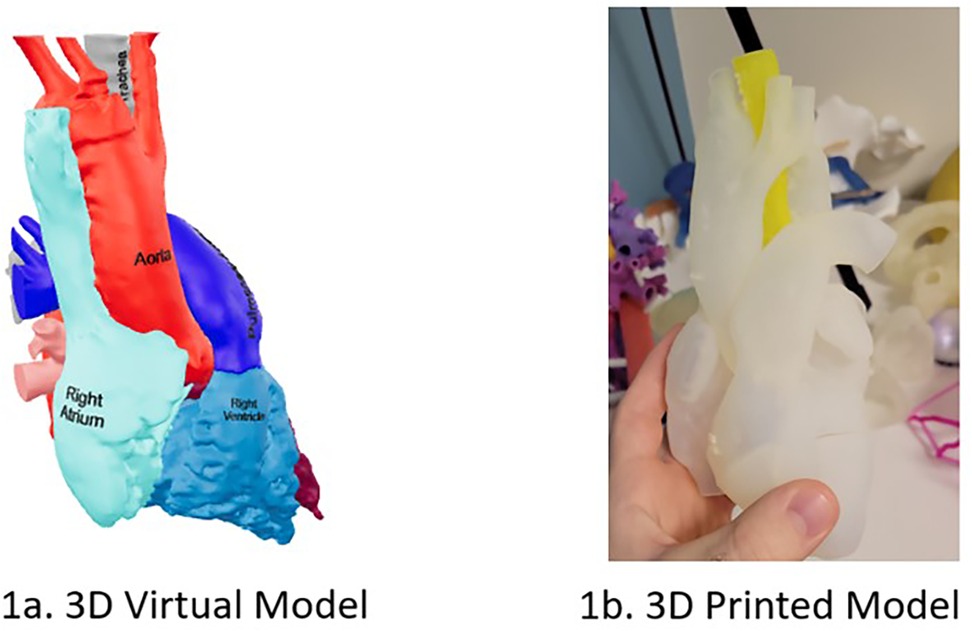
We created 3D printed and 3D virtual models (Figure 1) of various congenital heart defects (CHDs) representing patients seen in outpatient setting, including tetralogy of Fallot and coarctation of the aorta (Table 1). For each model, CT scan data was imported into Materialize Mimics software (version 25.0, Materialize, Leuven, Belgium). A threshold function was used to create the initial 3D model from the heart's blood pool. The heart model was segmented using this blood pool, allowing for the coloring of different components. The segmented model was then imported into Materialize 3-Matic, where we performed global and local smoothing operations. We labeled the structures in 3D based on the model's defect and performed a hollowing function for 3D printing to better visualize internal heart defects such as ventricular septal defects (VSDs) or an overriding aorta. The finished models were printed on a Stratasys J750 using Agilus 30 plastic. The same file used to create the 3D printed model was also used to make the 3D virtual model. Instead of hollowing the model, we exported the file to Blender, allowing us to color each cardiac segment and upload the file as a QR code that subjects could access by scanning with their smartphone.
Study cohort and design
This study was approved by the Institutional Review Board. Family members of patients with CHD, as well as patients aged 15 years or older, were recruited. Most subjects were recruited from an outpatient pediatric cardiology clinic, with a few recruited from a neonatal intensive care unit. Subjects' demographic information was recorded, including age, race, ethnicity, gender, and education level.
Subjects were shown a normal echocardiogram and an echocardiogram image of a heart corresponding to the patient's cardiac defect. They completed a questionnaire to assess their knowledge of the cardiac defect, normal cardiac anatomy, and perceived understanding of their family member's CHD. First, subjects were asked to select the 2D diagram of the heart that represented the cardiac defect from four hearts with different CHDs. Second, they were asked to identify the right ventricle, aorta, left atrium, and tricuspid valve. Subjects then rated their understanding of normal heart anatomy and their understanding of the patient's heart condition on a five-point scale from “poor” to “excellent.” Finally, subjects rated the helpfulness of the model in aiding their understanding of the cardiac defect on a five-point scale from “not at all helpful” to “extremely helpful”.
Subjects were then randomly assigned to one of two groups: 3D printed model or 3D virtual model. The 3D printed model group received education using a 3D printed model of a normal heart and a 3D printed model representing the patient's cardiac defect. The 3D virtual model group received education using a 3D virtual model of a normal heart and a 3D virtual model representing the patient's cardiac defect. After the education session with the 3D model, subjects completed the same questionnaire. Additionally, subjects were asked to compare the helpfulness of the 3D model to the 2D image and respond to two questions about how likely they would be to use the 3D model to explain the cardiac defect to friends/family and to other medical professionals (e.g., emergency department physicians). One researcher (LZ) conducted all education sessions.
Statistical analysis
The Cochran-Mantel-Haenzel test statistic based on rank scores, and controlling for education, was used to compare score/rating between the virtual and 3D printed groups. Additionally, the Wilcoxon signed-rank test was used to test for change within each group before and after introduction to the respective 3D model. Logistic regression fitted by the GEE method was utilized to account for correlation of response of test takers representing the same patient.
Results
109 subjects participated in the study over a 2-month period, representing 73 individual patients (Table 1). Patients were only allowed to participate in the study if they were 15 years or older, therefore most subjects were the patient's parents (72.5%). Fifty-four subjects were randomized to receive education using a 3D printed model and 55 were randomized to receive education using a 3D virtual model. We found no initial significant differences between the two groups except for education level. Subjects that were randomized to receive education using a 3D virtual model had significantly higher levels of education. We controlled for this difference during analysis.
Knowledge of CHD and normal anatomy
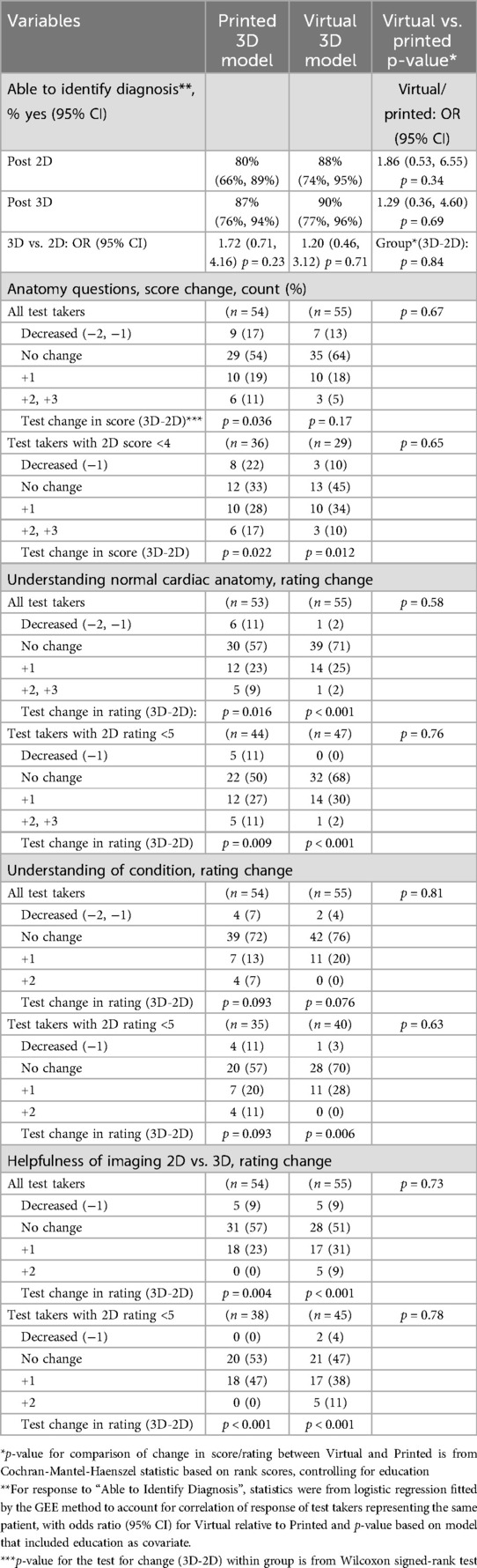
We analyzed subjects' performance on the anatomy portion of the questionnaire, comparing the subjects' knowledge after viewing the 2D image (Table 2). In analyzing, we found no statistically significant difference between the 3D printed and 3D virtual model groups. After viewing the 2D image, most subjects (n = 91, 83%) were able to identify the cardiac diagnosis when asked to select the one heart that corresponded with their CHD out of four hearts, and there was no significant increase in subject's ability to identify their cardiac diagnosis after viewing either 3D printed or 3D virtual model (p = 0.23, n = 47, 87% and p = 0.71, n = 49, 89% respectively) (Table 3). The subject's anatomy knowledge was assessed by asking them four questions to identify structures of normal heart anatomy. Subjects who initially obtained a perfect anatomy knowledge score (n = 44) were excluded from this portion of the analysis. Subjects in both 3D printed and 3D virtual model groups had a significant increase in their anatomy knowledge score between the first questionnaire (after the 2D image) and second questionnaire (after the 3D model) (p = 0.022 and p = 0.012 respectively) (Table 3).
Preference for 3d model
Subjects were asked to rate their understanding of normal anatomy. Both the 3D printed and 3D virtual model groups reported significantly higher self-rated understanding of normal cardiac anatomy compared to their ratings after viewing the 2D image (p = 0.009 and p < 0.001, respectively) (Table 3).
Next, subjects were asked to rate their understanding of their own or their family member's cardiac condition. Those in the 3D virtual model group who initially rated their understanding as less than 5/5 after viewing the 2D image later reported a significantly increased understanding (p = 0.006). However, there was no significant difference in the 3D printed model group on this measure (Table 3).
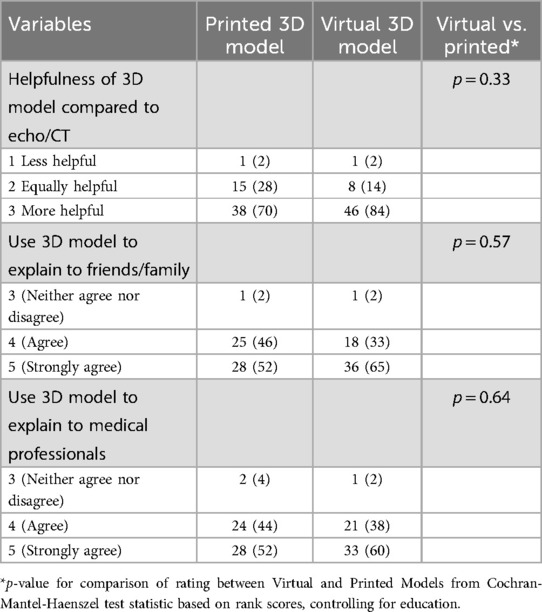
Finally, subjects in both the 3D printed and 3D virtual model groups found the 3D models more helpful (70% and 84%, respectively) compared to the 2D image (Table 4). Most subjects in both groups selected “agree” or “strongly agree” when asked if they would use the 3D model to explain their cardiac diagnosis to friends and family (98.1% and 98.2%, respectively). Similarly, most subjects in both groups selected “agree” or “strongly agree” when asked if they would use the 3D model to explain their cardiac diagnosis to other medical professionals (96.3% and 98.2%, respectively).
Discussion
This study is the first to compare the effectiveness of 3D printed models vs. 3D virtual models of congenital heart disease (CHD) in enhancing patient and family understanding. Existing literature predominantly focuses on the educational benefits of 3D printed models (4–8). By incorporating 3D virtual models, our research demonstrates that both types of models significantly improve patient and family comprehension and self-reported helpfulness.
While 3D printing is notably more time-consuming and costly, 3D virtual models offer a quicker, customizable alternative. These virtual models can be tailored to an individual's CT scan and shared via QR codes, allowing patients and families to easily explain the diagnosis to friends, relatives, and medical professionals.
The 3D printer used in this study was a high-end commercial printer and required expertise and time, however, given the advances in the availability of this technology, it may be more viable for individuals to print heart models on more consumer-accessible desktop printers. Additionally, these models can be customized to the printer's preferred design. Various resins can be used to depict the models along with the addition of color to highlight areas of the defect.
Our findings corroborate previous research on the educational impact of 3D models (4–8). Participants in both 3D model groups exhibited significant improvements in their knowledge of cardiac anatomy after viewing the 3D models compared to the 2D images. Additionally, subjects reported that the 3D models were more effective in aiding their understanding of their own or their family member's condition.
Interestingly, this study does not replicate the findings of Awori and colleagues in their 2021 study in which they concluded that printed models were of greater benefit to parents of children with CHDs (17). However, this study only included subjective measures of parent's preferences for the models, and did not include tests to assess their objective understanding of the CHD. Additionally, they stratified their analysis to differentiate between parents who perceived themselves to be more comfortable with modern technology and found that those who were more comfortable with modern technology rated 3D virtual models more highly than printed models. In future work, replicating our study with an added component of perceived comfort with modern technology could provide more insight into patient and family preferences.
Each model has its strengths and weaknesses. Based on our experiences 3D printed models are easier to manipulate but more costly to produce while 3D virtual models are easier to access while being cost effective. Additionally, some CHDs can be easily portrayed with the use of one model, however, other CHDs have substantial variety within one condition, such as TAPVR. This would require multiple models to accurately portray one condition, something that can be more easily done in a virtual environment specifically tailored to an individual patient's condition. Advanced 3D virtual models can be developed to enable patients and families to virtually dissect the heart, providing a clearer visualization of intracardiac defects. This level of customization is not feasible with 3D printed models. Other ways to visualize CHDs, such as virtual reality, could be used in future studies for educating patients and family members (18, 19).
Conclusions
Given the lack of statistically significant differences between the two 3D groups, we propose that 3D virtual models are a more sophisticated option for the reasons outlined above. Furthermore, both 3D printed and virtual models are superior to 2D images for patient education and can be routinely implemented in clinical practice. Future research should focus on developing more advanced 3D virtual models and evaluating their effectiveness in clinical settings for patient and family education.
Limitations
This study has several limitations. Subjects completed the questionnaire after viewing the 2D image and again after viewing the 3D models. While score increases may reflect a learning effect, subjects were not informed of the correct answers between the two tests. Additionally, a single heart model was used to represent each condition, which may not accurately reflect each patient's specific CHD. Future studies could improve upon this by creating heart models from each patient's CT scan, similar to the approach used by Biglino et al. in their 2017 study (7), and the Sun et al. study (20).
The subjects were aware that the study was comparing 2D models to 3D models. It is possible that preference for the 3D models could be impacted by social desirability bias. The increase in subjects’ knowledge was not likely impacted by social desirability, although it is possible that preference for the 3D model over the 2D model could have been influenced. This could be mitigated by randomly assigning the 2-D and 3- D models in future studies.
Although the recent census indicates that over 90% of individuals have broadband internet access at home and 90% have at least one computer (21), there are a small number of patients and families who would not be able to access the 3D virtual model at their home residence. In other countries with more limited access to the internet and 3D printers, fewer patients and clinicians may be able to utilize 3D models for education.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Iowa Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
LZ: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing, Formal Analysis, Project administration, Visualization. AM: Data curation, Software, Visualization, Writing – review & editing. ER: Conceptualization, Investigation, Methodology, Writing – review & editing. CB: Software, Visualization, Writing – review & editing. RA: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
2D, two-dimensional; 3D, three-dimensional; CHDs, congenital heart diseases.
References
1. Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. (2013) 131(5):e1502–8. doi: 10.1542/peds.2012-3435
2. Hoffman JIE, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. (2002) 39(12):1890–900. doi: 10.1016/S0735-1097(02)01886-7
3. Ahmad Azahari AFA, Wan Ab Naim WN, Md Sari NA, Lim E, Mohamed Mokhtarudin MJ. Advancement in computational simulation and validation of congenital heart disease: a review. Comput Methods Biomech Biomed Engin. (2024):1–14. doi: 10.1080/10255842.2024.2377338
4. Biglino G, Capelli C, Wray J, Schievano S, Leaver LK, Khambadkone S, et al. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: feasibility and acceptability. BMJ Open. (2015) 5(4):e007165. doi: 10.1136/bmjopen-2014-007165
5. Biglino G, Capelli C, Leaver LK, Schievano S, Taylor AM, Wray J. Involving patients, families and medical staff in the evaluation of 3D printing models of congenital heart disease. Commun Med. (2016) 12(2-3):157–69. doi: 10.1558/cam.28455
6. Marella NT, Gil AM, Fan W, Aristizabal CA, Asrani P, Harrington J, et al. 3D-printed cardiac models for fetal counseling: a pilot study and novel approach to improve communication. Pediatr Cardiol. (2023) 44(8):1800–7. doi: 10.1007/s00246-023-03177-y
7. Biglino G, Koniordou D, Gasparini M, Capelli C, Leaver LK, Khambadkone S, et al. Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during clinical consultations. Pediatr Cardiol. (2017) 38(4):813–8. doi: 10.1007/s00246-017-1586-9
8. Guo HC, Wang Y, Dai J, Ren CW, Li JH, Lai YQ. Application of 3D printing in the surgical planning of hypertrophic obstructive cardiomyopathy and physician-patient communication: a preliminary study. J Thorac Dis. (2018) 10(2):867–73. doi: 10.21037/jtd.2018.01.55
9. Brunner BS, Thierij A, Jakob A, Tengler A, Grab M, Thierfelder N, et al. 3D-printed heart models for hands-on training in pediatric cardiology—the future of modern learning and teaching? GMS J Med Educ. (2022) 39(2):1–21. doi: 10.3205/ZMA001544
10. White SC, Sedler J, Jones TW, Seckeler M. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects: 3D printing in pediatric resident education. Congenit Heart Dis. (2018) 13(6):1045–9. doi: 10.1111/chd.12673
11. Loke YH, Harahsheh AS, Krieger A, Olivieri LJ. Usage of 3D models of tetralogy of Fallot for medical education: impact on learning congenital heart disease. BMC Med Educ. (2017) 17(1):54. doi: 10.1186/s12909-017-0889-0
12. Asif A, Lee E, Caputo M, Biglino G, Shearn AIU. Role of 3D printing technology in paediatric teaching and training: a systematic review. BMJPO. (2021);5(1):e001050. doi: 10.1136/bmjpo-2021-001050
13. Riggs KW, Dsouza G, Broderick JT, Moore RA, Morales DLS. 3D-printed models optimize preoperative planning for pediatric cardiac tumor debulking. Transl Pediatr. (2018) 7(3):196–202. doi: 10.21037/tp.2018.06.01
14. Xu JJ, Luo YJ, Wang JH, Xu WZ, Shi Z, Fu JZ, et al. Patient-specific three-dimensional printed heart models benefit preoperative planning for complex congenital heart disease. World J Pediatr. (2019) 15(3):246–54. doi: 10.1007/s12519-019-00228-4
15. Salavitabar A, Figueroa CA, Lu JC, Owens ST, Axelrod DM, Zampi JD. Emerging 3D technologies and applications within congenital heart disease: teach, predict, plan and guide. Future Cardiol. (2020) 16(6):695–709. doi: 10.2217/fca-2020-0004
16. Illmann CF, Ghadiry-Tavi R, Hosking M, Harris KC. Utility of 3D printed cardiac models in congenital heart disease: a scoping review. Heart. (2020) 106(21):1631–7. doi: 10.1136/heartjnl-2020-316943
17. Awori J, Friedman SD, Chan T, Howard C, Seslar S, Soriano BD, et al. 3D models improve understanding of congenital heart disease. 3D Print Med. (2021) 7(1):26. doi: 10.1186/s41205-021-00115-7
18. O'Sullivan DM, Foley R, Proctor K, Gallagher S, Deery A, Eidem BW, et al. The use of virtual reality echocardiography in medical education. Pediatr Cardiol. (2021) 42(4):723–6. doi: 10.1007/s00246-021-02596-z
19. Lim TR, Wilson HC, Axelrod DM, Werho DK, Handler SS, Yu S, et al. Virtual reality curriculum increases paediatric residents’ knowledge of CHDs. Cardiol Young. (2023) 33(3):410–4. doi: 10.1017/S1047951122000890
20. Sun Z. Patient-specific 3D-printed models in pediatric congenital heart disease. Children. (2023) 10(2):319. doi: 10.3390/children10020319
21. Mejía D. Computer and Internet Use in the United States: 2021. Washington, DC: U.S. Census Bureau (2024). Available online at: https://www2.census.gov/library/publications/2024/demo/acs-56.pdf
Keywords: congenital heart disease, patient education, 3D printing, cardiac models, digital models
Citation: Zerwic L, Mohan A, Riley E, Byeman C and Ashwath R (2025) The impact of 3D printed vs. 3D virtual congenital heart models on patient and family knowledge. Front. Pediatr. 13:1525549. doi: 10.3389/fped.2025.1525549
Received: 9 November 2024; Accepted: 17 February 2025;
Published: 14 March 2025.
Edited by:
Xicheng Deng, Hunan Children's Hospital, ChinaReviewed by:
Martin L. Tomov, Emory University, United StatesMohd Jamil Mohamed Mokhtarudin, Universiti Malaysia Pahang, Malaysia
Copyright: © 2025 Zerwic, Mohan, Riley, Byeman and Ashwath. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ravi Ashwath, cmF2aS5hc2h3YXRoQGNocmlzdHVzaGVhbHRoLm9yZw==
†Present Address: Connor Byeman, Pediatrics Department, Boston Children's Hospital, Boston MA, United States
 Luke Zerwic
Luke Zerwic Ashray Mohan
Ashray Mohan Emily Riley
Emily Riley Connor Byeman
Connor Byeman Ravi Ashwath
Ravi Ashwath