
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Pediatr., 27 March 2025
Sec. Children and Health
Volume 13 - 2025 | https://doi.org/10.3389/fped.2025.1493780
This article is part of the Research TopicMaternal and Infant Nutrition: Impact on Breast Milk, Infant Gut Microbiota and Health DevelopmentView all 8 articles
 Wendy Sue Swanson1
Wendy Sue Swanson1 Erin Sundseth Ross2
Erin Sundseth Ross2 Luz Adriana Matiz3
Luz Adriana Matiz3 Laura Czerkies4
Laura Czerkies4 Lyndsey R. Huss5*
Lyndsey R. Huss5* Sarah Smith-Simpson6
Sarah Smith-Simpson6 Jodi Bettler7
Jodi Bettler7 Susan Pac5
Susan Pac5
Feeding infants and young children (IYC) is an emotional commitment for caregivers as they strive to achieve a sense of mastery, goodness, and accomplishment in providing nourishment for their children. Feeding practices are important during early childhood for lifelong health and well-being as behaviors related to healthy eating are established, and there is an interrelation between growth, gross/fine motor skills, and social-emotional behavior in shaping “learning to eat” for IYC. Mealtimes and feedings are opportunities for engagement with the family, formation of healthy habits, exposure to different foods, practicing eating skills, and learning to appreciate foods. The caregivers' role is pertinent as they influence and teach children “what” and “how” to eat and play a crucial role in supporting children's social, emotional, and cognitive development in relation to food and mealtimes. This mini review provides practical guidance for caregivers as their IYC “learn to eat.” Caregiver behaviors have changed, particularly in the choice of feeding methods, requiring an update on complementary feeding advice. Healthcare providers can encourage positive feeding practices. Family mealtimes provide opportunities for (1) bonding, (2) practicing and refining gross/fine motor, cognitive, language, and social-emotional skills, (3) offering a variety of nutrient-dense, appropriate textured foods, and (4) reinforcing the central role of the caregiver in establishing healthy eating patterns, a positive relationship with food, and joyful eating experiences. Healthcare providers play a pivotal role in raising awareness among caregivers about the importance of their role in feeding their child(ren).
The period of early childhood is crucial for development and lays the foundation for lifelong health and well-being (1–3). Nutrition plays a vital role in shaping developmental outcomes, and research suggests that there is a critical period when behaviors related to healthy eating are established (4, 5). The interrelation between growth, motor skills, and social-emotional behavior forms an axis where nutrition and feeding practices influence eating skills and shape “learning to eat” (Figure 1). Complementary feeding is defined as the period when pureed and solid foods are introduced around 6 months of age to support growth, development, and nutrition while promoting family engagement and form lifelong, healthy eating habits and practices (6, 7). While the focus of complementary feeding is often the immediate excitement, trepidation, and stepping stone of infants taking their first bite of food, the long-term goal of complementary feeding is to have enjoyable family mealtimes that support a healthy diet, support the social-emotional aspects of feeding, and follow hunger-satiety cues (7–13).
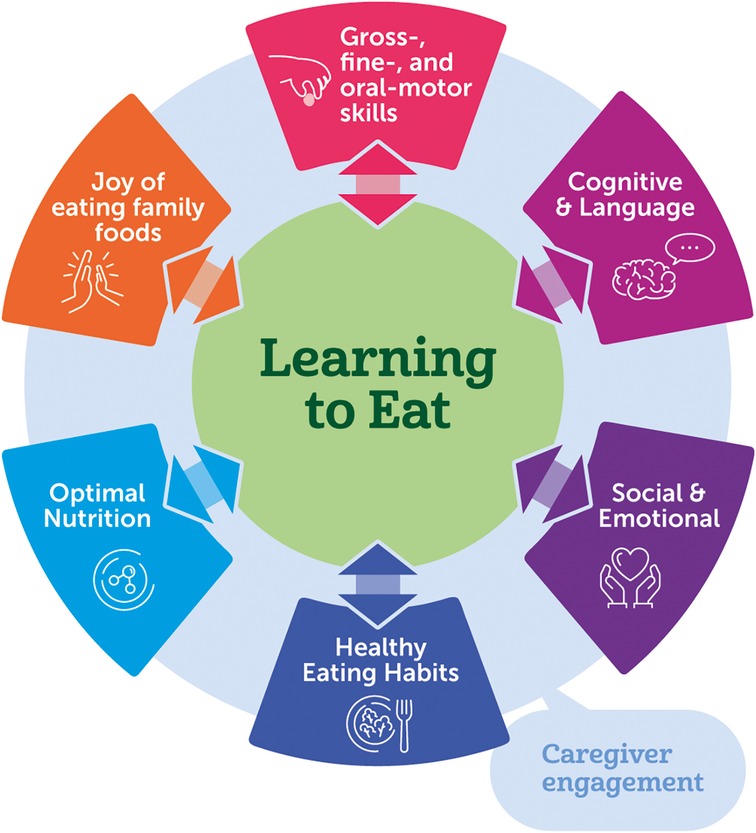
Figure 1. Learning to eat provides opportunities to build children's feeding skills and to nourish children's overall development through moments of family engagement and caregiver-child interactions.
Eating integrates multiple skill domains (gross/fine motor, social-emotional, cognitive). Recommendations for complementary feeding traditionally focus on the types and amounts of foods that infants eat (what) and address responsive feeding (how) (14, 15). Mealtimes and feedings are occasions for exposure to different foods (tastes, textures), practicing eating (chewing, use of utensils), learning to appreciate foods, and exploration. The caregivers' role to provide healthy food to their infant cannot be overlooked. Interactive learning (process involving mutual responsiveness), the caregiver-child relationship and the caregiver's and child's readiness should be considered (16). Families influence and teach their children to eat a variety of foods, and these practices can be encouraged by healthcare providers (HCPs) through supportive guidance and education (17).
This paper reviews and summarizes current research and guidance updating evidence and guidance for caregivers as their IYC “learn to eat.” Caregiver behaviors have changed over time, particularly in choice of feeding methods where infant-led approaches [introducing solid foods to infants which gives control of the feeding process to the infant (18–22)] are becoming increasingly popular. An updated look at complementary feeding advice is warranted. Multiple aspects of feeding the growing infant are addressed and practical strategies for HCPs to encourage positive, joyful feeding practices are provided.
Complementary feeding guidelines are generally consistent in recommending introducing complementary foods at about 6 months of age (3, 14, 23–25), not before 4 months of age nor delayed after 6 months of age (14, 23–25). As infants grow and become more active following the first 6 months of life, breastmilk alone no longer provides full nutritional requirements (3, 14, 26, 27); therefore, foods play a critical role in ensuring nutrient needs are met. Further, as infants advance in social-emotional development in concert with advancing fine motor skills, they exhibit curiosity and/or desire for flavors, textures, and foods they see their caregivers enjoy. Complementary feeding is a critical period in infant nutrition impacting outcomes later in life such as growth, non-communicable diseases, and food allergies (28).
All children develop at different rates; the ages outlined by the American Academy of Pediatrics (AAP) (29) and the US Centers for Disease Control (CDC) (30) at which certain skills are typically demonstrated are guides to use along with developmental readiness cues and determine when infants are ready to start solids. At 4–6 months, infants demonstrate emerging head control and loss of extrusor reflex (tongue thrust) (29). Sitting with support and wrapping fingers around objects placed in the hand like a spoon are gross/fine motor skills added to infants' repertoire at 4–6 months (4, 31). A spoon initially explored, with time, becomes a utensil for self-feeding. The oral cavity develops through 6 months where infants gain trunk stability and head control and sit independently (30, 32). Trunk stability is particularly important to support fine-motor and oral motor development and allow for self-feeding by infants. The prenatally developed feeding reflexes, including swallowing, sucking, gag, phasic bite, and rooting (33) gradually integrate with conscious actions until the development of mature eating. These reflexes integrate and disappear by the four-month period in the healthy infant (34). All these gross/fine motor milestones may indicate infants are ready to start complementary feeding. Acquisition of increasingly complex gross, fine, and oral motor skills is necessary for the developing child to progress through the journey of learning “how” to eat.
Providing appropriate foods and beverages is critical for IYC to establish healthy dietary patterns. As defined by the US Dietary Guidelines for Americans 2020–2025 (DGA), “a healthy dietary pattern includes a variety of nutrient-dense fruits, vegetables, grains, protein foods (including lean meats, poultry, eggs, seafood, nuts, and seeds), dairy (including milk, yogurt, and cheese), and oils” (14). Expert guidelines not only recommend nutrient-dense foods, but also foods that are developmentally appropriate and diverse to ensure nutritional adequacy and support healthy eating habits (14, 35, 36). Limited, but consistent, evidence indicates that maternal dietary flavors in amniotic fluid and breastmilk promote early food acceptance in infants which are shaped by maternal dietary variety and responsive breastfeeding (37–40), while innate taste preferences direct infants toward sweet tastes (41, 42), making learning to eat vegetables and some fruits more challenging. However, repeated exposure can positively influence acceptance of novel tastes and textures (43–45). IYC have a heightened receptiveness to new foods, offering an early window of opportunity to foster dietary variety and positively influence a child's lifelong relationship with food (41, 46, 47).
Nutrient-dense complementary foods are central to the diet once solid foods are started. A diverse diet including foods from all food groups of various tastes and textures can ensure adequate nutrition and increase acceptance of foods. IYC develop their complex oral-motor skills needed for chewing nutrient dense foods and thereby increasing diet diversity. Purposeful introduction of the major food allergens [e.g., milk, eggs, shellfish, tree nuts, peanuts, wheat, and soy (48) and inclusive of fish and sesame in the US] should be early in the first year of life when other complementary foods are introduced in the diet (14, 23, 49) and often, to reduce the risk of development of food allergies (14, 49, 50). A healthy dietary pattern should be followed at every life stage incorporating nutrient dense foods, leaving little remaining energy for added sugars. Establishing these patterns can set a solid foundation for healthy eating and adequate nutrient intake.
Texture is an important consideration in IYC feeding. Food textures should be tailored to the developmental needs of the IYC and should change as the child gets older (24). The WHO recommends pureed, mashed, and semi-solid foods beginning at six months of age, finger foods that can be eaten alone by 8-month-old infants, and that most children should be eating the same types of foods consumed by the rest of the family by 12 months. It is crucial to ensure foods are appropriate in size and texture to minimize choking hazards. Moreover, some organizations specifically recommend introducing lumpy textures by 8–10 months, to decrease the risk of feeding difficulties, such as pickiness and food refusal (27, 51, 52).
Modern feeding trends focus on challenging infants (providing food types and textures that may require effort and ability to gum, chew, or eat and/or test oral-motor and gross-motor skills) and having infants self-feed various food types and textures. This is based on applying child development and learning approaches for 3–6-year-olds where alternatives to conventional education culture are explored and applied (53) to the infant feeding experience. An approach to consider is balancing guaranteed success with opportunities for exploration at infants' own pace such as offering practice foods where infants can step up towards new foods in terms of food texture. The typical progression is from pureed and smooth foods to soft textures with gradually increasing lumps to more complex textures and coarsely chopped foods with noticeable pieces. Using the carrot as an example, at about 6 months of age, it could be assumed an infant who has attained the appropriate developmental milestones would successfully be able to eat pureed carrots; to support the development of feeding skills, infants can be presented with carrots cut into appropriate shapes (stick, coin, half-moon, mashed) starting around 6 months of age and prepared to various suitable textures (i.e., soft cooked). This approach encourages exposure to and acceptance of more complex textures, promoting infants' abilities to handle different food forms as they grow.
Several feeding methods are implemented by caregivers, like spoon-feeding, baby-led weaning, and baby-led feeding (28, 54–57). Spoon-feeding is a method where spoon-fed purees are given first, gradually increasing to more complex textures like mash to lumpy with a shift towards family foods with infants feeding themselves (54, 58). Baby-led weaning is an approach to introducing solid food based on infants' developmental readiness that allows infants to decide when to begin eating foods, what to eat, how quickly to eat, and how much to consume (21). Baby-led feeding combines spoon-feeding and baby-led weaning where purees may or may not be introduced at 4–6 months of age, with table foods, finger foods, mashes, lumpy foods, and smooth purees offered from 6 months on (56). This combination method, as it is sometimes referred to, is what most caregivers practice (59), rather than strictly following just one method. Pediatric associations and the DGA (14) do not recommend a specific feeding method to use, citing further research is needed. Feeding methods are an individualized choice; caregivers can introduce foods in the way that is most appropriate for their child's development, parenting style, and needs of the family.
Regardless of the method, responsive feeding is the recommended evidence-based approach for all feeding methods for IYC (9–11, 60–65). Responsive feeding encourages the child to eat autonomously and is characterized by caregiver recognition and response to the child's hunger and satiety cues. This involves reciprocal nurturing feeding practices between caregiver and child (54, 55, 58) and stresses the importance of acknowledging the bidirectional aspect of the feeding relationship. Responsive feeding supports IYC social-emotional development by meeting hunger and fullness cues in a sensitive and timely manner. This builds trust, security, food enjoyment in children (62), and a positive emotional connection between the child and caregiver. The benefits of responsive feeding are numerous and well-documented (60, 63, 66–69).
A recently coined feeding term is “sensitive feeding” (70). Sensitive feeding broadens the concept of responsive feeding to incorporate understanding and anticipating the child's point of view by sensitively responding to the child's signals to foster a pleasant and safe atmosphere during mealtimes (71). In turn, this facilitates the child's association of eating with positive emotions and encourages the willingness to eat and try new foods (70, 71). Respecting a child's experience during eating and avoiding intrusiveness during mealtimes is an important pillar in supporting an IYC in learning to eat.
Without question, complementary feeding must provide optimal nutrition for the gross, fine, and oral motor development and growth of the IYC. Current evidence shows that the social-emotional, cognitive, and language-building aspects of feeding are also important and can be established and nurtured from the first bite (12, 72–74). Effective and stimulating communication exchange with caregivers and family members helps children express their preferences, ask for more food, or indicate when they are full. Fostering an engaging mealtime environment (positive affect of caregivers, conversing with those at the table, limiting distractions, honoring the role of both the child and the caregiver) can support better nutrition, better social-emotional outcomes, and promote the joy of eating among family members.
The AAP acknowledges the pivotal impact of early adult-child interactions in early brain development and recommends providing a rich and responsive language environment (75). One strategy that caregivers can implement is the 3Ts— “tune in, talk more, and take turns” (76). Family mealtimes provide a rich opportunity to practice this strategy; creating an environment with limited distractions encourages the caregiver to tune in to their child. During mealtime preparation, caregivers can talk to their IYC about what they're preparing, introducing numbers, colors (i.e., “I'm mashing up 3 pieces of a yellow banana”), increasing communication between the child and caregiver that can carry through mealtime. Taking turns inherently can occur during feeding, particularly as the IYC gets older. Early talk and interaction during specific periods in a child's early development where the brain is particularly receptive to learning certain skills, like language, and where experiences during that time can have a significant and lasting impact on future development can have positive effects on later language and cognitive development (77, 78). Feeding occasions provide caregivers with blocks where they can spend quality time with their IYC and simultaneously practice speaking and nurture communication.
Creating a positive and nurturing feeding environment to support social-emotional development is beneficial for a child's overall feeding and development. The connection between social-emotional development and responsive feeding demonstrates that feeding is not solely a physiological act, but a shared social-emotional experience. Self-regulation, attachment, social skills, food acceptance, autonomy, and emotional well-being all play a role in the development of feeding skills and the establishment of healthy eating habits (79, 80). In turn, a positive feeding environment offers opportunities for children to practice self-regulation, social skills, autonomy, and emotional well-being (12, 61). When caregivers respond sensitively to hunger, fullness, and other IYC cues, trust and a secure attachment between the IYC and caregiver are built, supporting social-emotional development (61, 81).
The role of the caregiver and family in learning to eat cannot be minimized. It is the responsibility of the caregiver to set the stage for sensitive feeding practices and responsive feeding. Maternal sensitive feeding behavior and positive affect, (smiling and complimenting rather than irritation or harshness) were positively associated with IYC vegetable intake and liking (70), demonstrating how the role of the caregiver can greatly influence the feeding experience of IYC. Eating, and role modeling how to eat, is associated with greater acceptance of novel foods (82). There is an interactive learning journey for accepting a variety of foods, and caregivers play a critical part in this journey. The dynamic between the caregiver and the IYC is bidirectional during the learning to eat journey; both caregiver and IYC need to be engaged and responsive to each other's cues. Creating an environment that is ideal for IYC feeding includes turning off screens and eating at the table where this dynamic can thrive (17, 83, 84).
Caregivers are inundated with well-intentioned feeding advice, whether from social media, friends, or family members. However, much of this advice centers on what foods to offer and glossing over the caregiver role and holistic feeding guidance to choose what works best for their family within a science-based framework. For example, historically it has been advised to introduce a single food at a time, waiting days before introducing another (85–87); this advice is not based on science and does not afford adequate time to encourage a diverse diet with various foods and textures in infancy (85). It is the role of the HCP to educate the caregiver on current advice regarding the importance of a diversified diet (in flavors, textures, types of foods) including foods that are common allergens, an appropriate feeding environment, repeated exposure, responsive and sensitive feeding practices, and food safety (17).
Dissemination of the message that caregivers are one of the most important “ingredients” in the feeding journey of their IYC can begin with the HCP. The 4-month well-child care visit (Figure 2) is an opportune time to discuss feeding goals and the caregiver's role. Some families mistakenly start complementary feeding prior to 4 months of age, so these conversations need to begin early, ideally at the 2 months visit as anticipatory guidance, and often, to reinforce the importance of starting solids around 6 months of age and not before 4 months of age. Open-ended questions can help assess the caregiver's understanding and aspiration for their IYC's feeding journey (Supplementary Figures S1–S6). This is a great way to set the stage for what the caregivers would like to accomplish (i.e., independent eaters) and their understanding of their role in the process. HCPs can educate families about “learning to eat”, focusing on developmental signs, the caregiver's readiness to move away from breast- or bottle-feeding, appropriate foods, the mealtime environment, and the caregiver's role through responsive and sensitive feeding, language, and engagement. Learning to eat is a journey that is greatly influenced by caregivers.
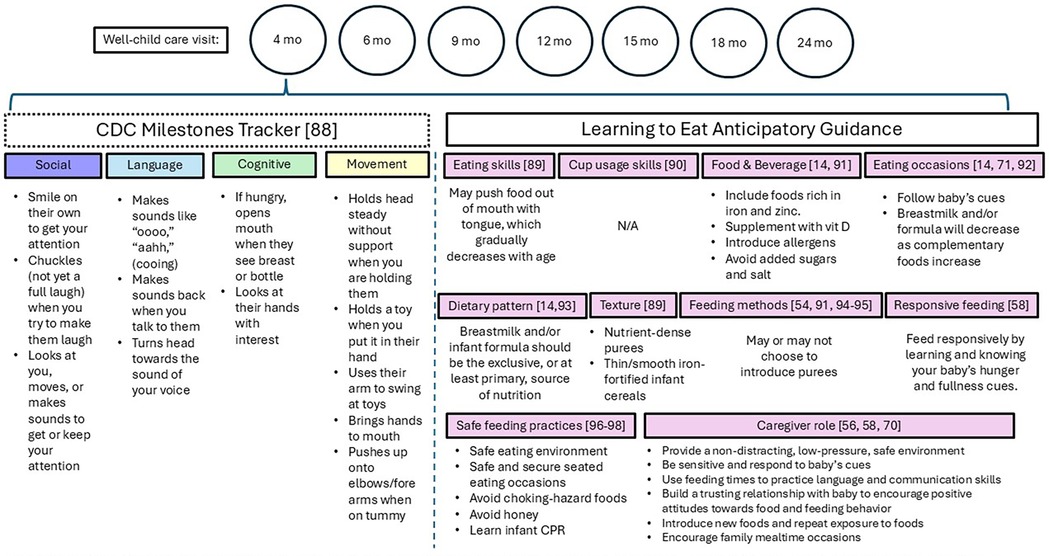
Figure 2. Overview of anticipatory developmental feeding guidance aligned with the 4-month well-child care visit. The above are not isolated events but build upon each other over time in an additive manner. As children grow and progress in age, they continue to develop and refine their skills, creating a foundation for further learning and development.
Research gaps in early feeding practices of IYC need to be addressed to refine advice for caregivers. Feeding methods have received attention, but it remains unclear if one method has scientifically validated advantages. Studies with appropriate outcomes, follow-up, and comparison groups are needed to inform HCPs and caregivers. Effective feeding methods and strategies must be identified to ensure children receive proper nutrition. This includes understanding the impact on growth and development, including social/emotional, as well as barriers caregivers may face. Understanding cultural beliefs and practices related to feeding is crucial for effective caregiver education. Dietary practices vary across cultures, but a generalized knowledge base that can be tailored to each family is ideal. This knowledge is essential for developing caregiver-education programs that support children's healthy development. Overall, addressing research gaps is vital for evidence-based guidance and support to caregivers in feeding their children and promoting their development.
Family mealtimes provide opportunities for bonding between the IYC and caregivers and for practicing and refining not only gross, fine, and oral motor skills, but cognitive, language, and social-emotional skills. Nutrient-dense foods and those that commonly cause allergies should be offered in textures, shapes, and sizes appropriate for the developmental stage of the IYC. The caregiver-child dynamic relationship is central to establishing healthy dietary patterns and joyful associations from the start. Regardless of feeding method used, responsive and sensitive feeding practices where the caregiver is attuned to the IYC feeding cues and an active role model for exploring foods are of utmost importance. The HCP is pivotal in bringing awareness to caregivers of just how crucial their role is in the feeding journey for their child that sets the tone for a life of healthy eating.
WS: Conceptualization, Validation, Writing – review & editing. ESR: Conceptualization, Validation, Writing – review & editing. LAM: Conceptualization, Validation, Writing – review & editing. LC: Conceptualization, Visualization, Writing – original draft. LH: Conceptualization, Project administration, Visualization, Writing – original draft. SS: Conceptualization, Visualization, Writing – review & editing. JB: Conceptualization, Funding acquisition, Supervision, Visualization, Writing – review & editing. SP: Conceptualization, Supervision, Visualization, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by Nestlé.
The authors would like to thank the following colleagues for their expert guidance: Liz Greenstreet, Diandra Brkic, and Marine Devezeaux de Lavergne. All individuals have consented to the acknowledgement.
Nestlé funded the work discussed in this paper. WSS, LAM, ESR, and LC received consultant fees from Nestlé for their input on this paper. LRH, SSS, JB, and SP are employees of Nestlé. LC was employed by LC Consulting LLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1493780/full#supplementary-material
1. American Academy of Pediatrics Committee on Nutrition. Complementary feeding. In: Kleinman RE, Greer FR, editors. Pediatric Nutrition. 8th ed. Itasca, IL: American Academy of Pediatrics (2020) p. 163–86.
2. World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices: Definitions and Measurement Methods. Geneva: World Health Organization and the United Nations Children's Fund (UNICEF) (2021).
3. World Health Organization. Infant and Young Child Feeding Fact Sheet (December 20, 2023). Infant and Young Child Feeding (who.int). (Accessed March 25, 2024).
4. Butte N, Cobb K, Dwyer J, Graney L, Heird W, Rickard K. The start healthy feeding guidelines for infants and toddlers. J Am Diet Assoc. (2004) 104(3):442–54. doi: 10.1016/j.jada.2004.01.027
5. Nicklaus S. The role of food experiences during early childhood in food pleasure learning. Appetite. (2016) 104:3–9. doi: 10.1016/j.appet.2015.08.022
6. Lutter CK, Grummer-Strawn L, Rogers L. Complementary feeding of infants and young children 6 to 23 months of age. Nutr Rev. (2021) 79(8):825–46. doi: 10.1093/nutrit/nuaa143
7. World Health Organization. WHO Guideline for Complementary Feeding of Infants and Young Children 6–23 Months of Age. Geneva: World Health Organization (2023).
8. D'Auria E, Borsani B, Pendezza E, Bosetti A, Paradiso L, Zuccotti GV, et al. Complementary feeding: pitfalls for health outcomes. Int J Environ Res Public Health. (2020) 17(21):7931. doi: 10.3390/ijerph17217931
9. Di Prete A, Del Grosso D, Focaroli V, Paoletti M, Pecora G, Hodges EA, et al. Complementary feeding approach and maternal responsiveness in 8- and 12-month-old Italian infants: a longitudinal study. Appetite. (2023) 190:107028. doi: 10.1016/j.appet.2023.107028
10. Fernandes C, Martins F, Santos AF, Fernandes M, Veríssimo M. Complementary feeding methods: associations with feeding and emotional responsiveness. Children (Basel). (2023) 10(3):464. doi: 10.3390/children10030464
11. Pérez-Escamilla R, Segura-Pérez S, Lott M, on behalf of the RWJF HER Expert Panel on Best Practices for Promoting Healthy Nutrition, Feeding Patterns, and Weight Status for Infants and Toddlers from Birth to 24 Months. Feeding Guidelines for Infants and Young Toddlers: A Responsive Parenting Approach. Durham, NC: Healthy Eating Research (2017) p. 8–57. Available at: http://healthyeatingresearch.org (Accessed March 25, 2024).
12. Wood AC, Blissett JM, Brunstrom JM, Carnell S, Faith MS, Fisher JO, et al. Caregiver influences on eating behaviors in young children: a scientific statement from the American heart association. J Am Heart Assoc. (2020) 9(10):e014520. doi: 10.1161/JAHA.119.014520
13. World Health Organization. Complementary Feeding. Complementary feeding (who.int). (2024a). (Accessed March 12, 2024).
14. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. 9 Edition. December 2020. Available online at: https://www.dietaryguidelines.gov/ (Accessed March 25, 2024).
15. American Academy of Pediatrics. Ages & Stages (2024). Available online at: https://www.healthychildren.org/english/ages-stages/baby/Pages/default.aspx (Accessed March 12, 2024).
16. Institute of Medicine and National Research Council. Transforming the Workforce for Children Birth Through Age 8: A Unifying Foundation. Washington, DC: The National Academies Press (2015). doi: 10.17226/19401
17. Muth ND, Bolling C, Hannon T, Sharifi M. Section on obesity; committee on nutrition. The role of the pediatrician in the promotion of healthy, active living. Pediatrics. (2024) 153(3):e2023065480. doi: 10.1542/peds.2023-065480
18. Arden MA, Abbott RL. Experiences of baby-led weaning: trust, control and renegotiation. Matern Child Nutr. (2015) 11(4):829–44. doi: 10.1111/mcn.12106
19. Rapley G. Baby-led weaning: transitioning to solid foods at the baby’s own pace. Community Pract. (2011) 84(6):20–3.21739856
20. Rapley G. Baby-Led Weaning: A Developmental Approach to the Introduction of Complementary Foods In: Maternal and Infant Nutrition and Nurture: Controversies and Challenges.
21. Rapley G, Forste R, Cameron S, Brown A, Wright C. Baby-Led weaning: a new frontier? ICAN: Infant Child Adolesc Nutr. (2015) 7(2):77–85. doi: 10.1177/1941406415575931
22. Rapley G, Murkett T. Baby-led Weaning: Helping Your Baby to Love Good Food. London: Vermilion Random House UK (2008).
23. Castenmiller J, de Henauw S, Hirsch-Ernst KI, Kearney J, Maciuk A, Mangelsdorf I, et al. Appropriate age range for introduction of complementary feeding into an infant’s diet. EFSA J. (2019) 17(9):e05780. doi: 10.2903/j.efsa.2019.5780
24. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee on Scoping Existing Guidelines for Feeding Recommendations for Infants and Young Children Under Age 2. In: Harrison M, Dewey K, editors. Feeding Infants and Children from Birth to 24 Months: Summarizing Existing Guidance. Washington (DC): National Academies Press (US) (2020) p. 23–85.
25. World Health Organization. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students. Geneva: World Health Organization (2009).
26. Abeshu MA, Lelisa A, Geleta B. Complementary feeding: review of recommendations, feeding practices, and adequacy of homemade complementary food preparations in developing countries—lessons from Ethiopia. Front Nutr. (2016) 3:41. doi: 10.3389/fnut.2016.00041
27. Fewtrell M, Bronsky J, Campoy C, Domellöf M, Embleton N, Fidler Mis N, et al. Complementary feeding: a position paper by the European society for paediatric gastroenterology, hepatology, and nutrition (ESPGHAN) committee on nutrition. J Pediatr Gastroenterol Nutr. (2017) 64(1):119–32. doi: 10.1097/MPG.0000000000001454
28. Capra ME, Decarolis NM, Monopoli D, Laudisio SR, Giudice A, Stanyevic B, et al. Complementary feeding: tradition, innovation and pitfalls. Nutrients. (2024) 16(5):737. doi: 10.3390/nu16050737
29. Zubler JM, Wiggins LD, Macias MM, Whitaker TM, Shaw JS, Squires JK, et al. Evidence-informed milestones for developmental surveillance tools. Pediatrics. (2022) 149(3):e2021052138. doi: 10.1542/peds.2021-052138
30. Centers for Disease Control and Prevention. CDC’s Developmental Milestones (2024). Available online at: https://www.cdc.gov/ncbddd/actearly/milestones/index.html (Accessed March 12, 2024).
31. Scharf RJ, Scharf GJ, Stroustrup A. Developmental milestones. Pediatr Rev. (2016) 37(1):25–37. doi: 10.1542/pir.2014-0103
32. Carruth BR, Ziegler PJ, Gordon A, Hendricks K. Developmental milestones and self-feeding behaviors in infants and toddlers. J Am Diet Assoc. (2004) 104(1 Suppl 1):s51–6. doi: 10.1016/j.jada.2003.10.019
33. Naylor AJ, Ardythe LM. Developmental Readiness of Normal Full Term Infants To Progress from Exclusive Breastfeeding to the Introduction of Complementary Foods: Reviews of the Relevant Literature Concerning Infant Immunologic, Gastrointestinal, Oral Motor and Maternal Reproductive and Lactational Development (2001).
34. Törölä H, Lehtihalmes M, Yliherva A, Olsén P. Feeding skill milestones of preterm infants born with extremely low birth weight (ELBW). Infant Behav Dev. (2012) 35(2):187–94. doi: 10.1016/j.infbeh.2012.01.005
35. Venter C, Greenhawt M, Meyer RW, Agostoni C, Reese I, du Toit G, et al. EAACI position paper on diet diversity in pregnancy, infancy and childhood: novel concepts and implications for studies in allergy and asthma. Allergy. (2020) 75(3):497–523. doi: 10.1111/all.14051
36. World Health Organization. Infant and Young Child Feeding. Infant and Young Child Feeding (who.int) (2024b). (Accessed March 24, 2024).
37. De Cosmi V, Scaglioni S, Agostoni C. Early taste experiences and later food choices. Nutrients. (2017) 9(2):107. doi: 10.3390/nu9020107
38. Mennella JA, Jagnow CP, Beauchamp GK. Prenatal and postnatal flavor learning by human infants. Pediatrics. (2001) 107(6):E88. doi: 10.1542/peds.107.6.e88
39. Spahn JM, Callahan EH, Spill MK, Wong YP, Benjamin-Neelon SE, Birch L, et al. Influence of maternal diet on flavor transfer to amniotic fluid and breast milk and children’s responses: a systematic review. Am J Clin Nutr. (2019) 109(Suppl_7):1003S–26. doi: 10.1093/ajcn/nqy240
40. Ventura AK, Worobey J. Early influences on the development of food preferences. Curr Biol. (2013) 23(9):R401–8. doi: 10.1016/j.cub.2013.02.037
41. Birch LL. Development of food acceptance patterns in the first years of life. Proc Nutr Soc. (1998) 57(4):617–24. doi: 10.1079/pns19980090
42. Fidler Mis N, Braegger C, Bronsky J, Campoy C, Domellöf M, Embleton ND, et al. Sugar in infants, children and adolescents: a position paper of the European society for paediatric gastroenterology, hepatology and nutrition committee on nutrition. J Pediatr Gastroenterol Nutr. (2017) 65(6):681–96. doi: 10.1097/MPG.0000000000001733
43. Nekitsing C, Hetherington MM, Blundell-Birtill P. Developing healthy food preferences in preschool children through taste exposure, sensory learning, and nutrition education. Curr Obes Rep. (2018) 7(1):60–7. doi: 10.1007/s13679-018-0297-8
44. Forestell CA. You are what your parents eat: parental influences on early flavor preference development. Nestle Nutr Inst Workshop Ser. (2020) 95:78–87. doi: 10.1159/000511516
45. Murray RD. Savoring sweet: sugars in infant and toddler feeding. Ann Nutr Metab. (2017) 70(Suppl 3):38–46. doi: 10.1159/000479246
46. Mazzocchi A, De Cosmi V, Scaglioni S, Agostoni C. Towards a more sustainable nutrition: complementary feeding and early taste experiences as a basis for future food choices. Nutrients. (2021) 13(8):2695. doi: 10.3390/nu13082695
47. Nicklaus S. The role of dietary experience in the development of eating behavior during the first years of life. Ann Nutr Metab. (2017) 70(3):241–5. doi: 10.1159/000465532
48. Soriano VX, Ciciulla D, Gell G, Wang Y, Peters RL, McWilliam V, et al. Complementary and allergenic food introduction in infants: an umbrella review. Pediatrics. (2023) 151(2):e2022058380. doi: 10.1542/peds.2022-058380
49. Greer FR, Sicherer SH, Burks AW, COMMITTEE ON NUTRITION; SECTION ON ALLERGY AND IMMUNOLOGY. The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, hydrolyzed formulas, and timing of introduction of allergenic complementary foods. Pediatrics. (2019) 143(4):e20190281. doi: 10.1542/peds.2019-0281
50. Abrams EM, Ben-Shoshan M, Protudjer JLP, Lavine E, Chan ES. Early introduction is not enough: CSACI statement on the importance of ongoing regular ingestion as a means of food allergy prevention. Allergy Asthma Clin Immunol. (2023) 19(1):63. doi: 10.1186/s13223-023-00814-2
51. Sdravou K, Printza A, Emmanouilidou-Fotoulaki E, Michou E, Sotiriadou F, Fotoulaki M. Developmental feeding stages and their impact on child feeding behavior. J Pediatr Gastroenterol Nutr. (2023) 77(6):769–78. doi: 10.1097/MPG.0000000000003892
52. Health Canada. Nutrition for Healthy Term Infants: Recommendations from Six to 24 Months (July 12, 2023). Nutrition for Healthy Term Infants: Recommendations from Six to 24 Months—Canada.ca (Accessed March 27, 2024).
53. Lillard AS. Shunned and admired: montessori, self-determination, and case for radical school reform. Educ Psychol Rev. (2019) 31:939–65. doi: 10.1007/s10648-019-09483-3
54. Brown A. Differences in eating behaviour, well-being and personality between mothers following baby-led vs. Traditional weaning styles. Matern Child Nutr. (2016) 12(4):826–37. doi: 10.1111/mcn.12172
55. D'Auria E, Bergamini M, Staiano A, Banderali G, Pendezza E, Penagini F, et al. Italian society of pediatrics. baby-led weaning: what a systematic review of the literature adds on. Ital J Pediatr. (2018) 44(1):49. doi: 10.1186/s13052-018-0487-8
56. Morison BJ, Heath AM, Haszard JJ, Hein K, Fleming EA, Daniels L, et al. Impact of a modified version of baby-led weaning on dietary variety and food preferences in infants. Nutrients. (2018) 10(8):1092. doi: 10.3390/nu10081092
57. Boswell N. Complementary feeding methods-A review of the benefits and risks. Int J Environ Res Public Health. (2021) 18(13):7165. doi: 10.3390/ijerph18137165
58. Cameron SL, Taylor RW, Heath AL. Parent-led or baby-led? Associations between complementary feeding practices and health-related behaviours in a survey of New Zealand families. BMJ Open. (2013) 3(12):e003946. doi: 10.1136/bmjopen-2013-003946
59. Moreira PR, Nunes LM, Neves RO, Belin CHS, Fuhr J, Gomes E, et al. Adherence to different methods for introducing complementary food to 7-month-old babies: a randomized clinical trial. Rev Paul Pediatr. (2022) 41:e2021235. doi: 10.1590/1984-0462/2023/41/2021235
60. Bergamini M, Simeone G, Verga MC, Doria M, Cuomo B, D'Antonio G, et al. Complementary feeding caregivers’ practices and growth, risk of overweight/obesity, and other non-communicable diseases: a systematic review and meta-analysis. Nutrients. (2022) 14(13):2646. doi: 10.3390/nu14132646
61. Black MM, Aboud FE. Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr. (2011) 141(3):490–4. doi: 10.3945/jn.110.129973
62. Finnane JM, Jansen E, Mallan KM, Daniels LA. Mealtime structure and responsive feeding practices are associated with less food fussiness and more food enjoyment in children. J Nutr Educ Behav. (2017) 49(1):11–18.e1. doi: 10.1016/j.jneb.2016.08.007
63. Komninou S, Halford JCG, Harrold JA. Differences in parental feeding styles and practices and toddler eating behaviour across complementary feeding methods: managing expectations through consideration of effect size. Appetite. (2019) 137:198–206. doi: 10.1016/j.appet.2019.03.001
64. Pérez-Escamilla R, Jimenez EY, Dewey KG. Responsive feeding recommendations: harmonizing integration into dietary guidelines for infants and young children. Curr Dev Nutr. (2021) 5(6):nzab076. doi: 10.1093/cdn/nzab076
65. Schwendler TR, Na M, Keller KL, Jensen L, Kodish SR. Observational methods in studies of infant and young child feeding practices in low- and middle-income countries: a twenty-year retrospective review. Nutrients. (2024) 16(2):288. doi: 10.3390/nu16020288
66. Bąbik K, Patro-Gołąb B, Zalewski BM, Wojtyniak K, Ostaszewski P, Horvath A. Infant feeding practices and later parent-reported feeding difficulties: a systematic review. Nutr Rev. (2021) 79(11):1236–58. doi: 10.1093/nutrit/nuaa135
67. Bocquet A, Brancato S, Turck D, Chalumeau M, Darmaun D, De Luca A, et al. “Baby-led weaning”—progress in infant feeding or risky trend? Arch Pediatr. (2022) 29(7):516–25. doi: 10.1016/j.arcped.2022.08.012
68. Fernandes C, Martins F, Santos AF, Fernandes M, Veríssimo M. Complementary feeding methods: associations with feeding and emotional responsiveness. Children (Basel). (2023) 10(3):464. doi: 10.3390/children10030464
69. Pang WW, McCrickerd K. The impact of feeding experiences during infancy on later child eating behaviours. Curr Opin Clin Nutr Metab Care. (2021) 24(3):246–51. doi: 10.1097/MCO.0000000000000744
70. van Vliet MS, Schultink JM, Jager G, de Vries JHM, Mesman J, de Graaf C, et al. The baby’s first bites RCT: evaluating a vegetable-exposure and a sensitive-feeding intervention in terms of child health outcomes and maternal feeding behavior during toddlerhood. J Nutr. (2022) 152(2):386–98. doi: 10.1093/jn/nxab387
71. van der Veek SMC, de Graaf C, de Vries JHM, Jager G, Vereijken CMJL, Weenen H, et al. Baby’s first bites: a randomized controlled trial to assess the effects of vegetable-exposure and sensitive feeding on vegetable acceptance, eating behavior and weight gain in infants and toddlers. BMC Pediatr. (2019) 19(1):266. doi: 10.1186/s12887-019-1627-z
72. Fisher J, Lumeng J, Miller L, Smethers A, Lott M. EvidenceBased Recommendations and Best Practices for Promoting Healthy Eating Behaviors in Children 2 to 8 Years. Durham, NC: Healthy Eating Research (2021. Available at: https://healthyeatingresearch.org
73. Jeong J, Bliznashka L, Sullivan E, Hentschel E, Jeon Y, Strong KL, et al. Measurement tools and indicators for assessing nurturing care for early childhood development: a scoping review. PLOS Glob Public Health. (2022) 2(4):e0000373. doi: 10.1371/journal.pgph.0000373 Erratum in: PLOS Glob Public Health. 2023 May 2;3(5):e0001906. doi: 10.1371/journal.pgph.000190636962242
74. Levin O, McIsaac JD, Campbell J, Dickson E, Rossiter MD. ‘For me it’s just the conversation:’ responsive feeding influences among early childhood educators. Public Health Nutr. (2024) 27(1):e200. doi: 10.1017/S1368980024001885
75. Council on early childhood; Council on school health. The pediatrician’s role in optimizing school readiness. Pediatrics. (2016) 138(3):e20162293. doi: 10.1542/peds.2016-2293
76. LoRe D, Ladner P, Suskind D. Talk, read, sing: early language exposure as an overlooked social determinant of health. Pediatrics. (2018) 142(3):e20182007. doi: 10.1542/peds.2018-2007
77. Gilkerson J, Richards JA, Warren SF, Oller DK, Russo R, Vohr B. Language experience in the second year of life and language outcomes in late childhood. Pediatrics. (2018) 142(4):e20174276. doi: 10.1542/peds.2017-4276
78. Webber C, Blissett J, Addessi E, Galloway AT, Shapiro L, Farrow C. An infant-led approach to complementary feeding is positively associated with language development. Matern Child Nutr. (2021) 17(4):e13206. doi: 10.1111/mcn.13206
79. Santos AF, Fernandes C, Fernandes M, Santos AJ, Veríssimo M. Associations between emotion regulation, feeding practices, and preschoolers’ food consumption. Nutrients. (2022) 14(19):4184. doi: 10.3390/nu14194184
80. Scaglioni S, Arrizza C, Vecchi F, Tedeschi S. Determinants of children’s eating behavior. Am J Clin Nutr. (2011) 94(6 Suppl):2006S–11. doi: 10.3945/ajcn.110.001685
81. Scaglioni S, De Cosmi V, Ciappolino V, Parazzini F, Brambilla P, Agostoni C. Factors influencing children’s eating behaviours. Nutrients. (2018) 10(6):706. doi: 10.3390/nu10060706
82. Addessi E, Galloway AT, Visalberghi E, Birch LL. Specific social influences on the acceptance of novel foods in 2–5-year-old children. Appetite. (2005) 45(3):264–71. doi: 10.1016/j.appet.2005.07.007
83. Jusienė R, Urbonas V, Laurinaitytė I, Rakickienė L, Breidokienė R, Kuzminskaitė M, et al. Screen use during meals among young children: exploration of associated variables. Medicina (Kaunas). (2019) 55(10):688. doi: 10.3390/medicina55100688
84. Litterbach EK, Laws R, Zheng M, Campbell KJ, Spence AC. Mothers’ experiences of reducing family mealtime screen use in Australian households with young children. Public Health Nutr. (2023) 27(1):e21. doi: 10.1017/S1368980023002847
85. Fleischer DM, Chan ES, Venter C, Spergel JM, Abrams EM, Stukus D, et al. A consensus approach to the primary prevention of food allergy through nutrition: guidance from the American academy of allergy, asthma, and immunology; American college of allergy, asthma, and immunology; and the Canadian society for allergy and clinical immunology. J Allergy Clin Immunol Pract. (2021) 9(1):22–43.e4. doi: 10.1016/j.jaip.2020.11.002
86. Centers for Disease Control and Prevention. When, What, and How to Introduce Solid Foods (2018). Available online at: https://www.cdc.gov/infant-toddler-nutrition/?CDC_AAref_Val=https://www.cdc.gov/nutrition/infantandtoddlernutrition/foods-and-drinks/how-much-and-how-often.html (Accessed February 10, 2025).
87. Hagan JF, Shaw JS, Duncan PM, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 4th ed. Elk Grove Village, IL: American Academy of Pediatrics (2017). p. 177.
88. Centers for Disease Control and Prevention. CDC’s Milestone Tracker App (2023). Available at: https://www.cdc.gov/ncbddd/actearly/milestones-app.html (Accessed June 3, 2024).
89. Ross E. Eating development in young children: understanding the complex interplay of developmental domains. In: Saavedra JM, Dattilo AM, editors. Early Nutrition and Long-Term Health : Mechanisms, Consequences, and Opportunities. Amsterdam: Elsevier (2017). p. 229–62. doi: 10.1016/B978-0-08-100168-4.00009-4
90. Pridham KF. Feeding behavior of 6- to 12-month-old infants: assessment and sources of parental information. J Pediatr. (1990) 117(2 Pt 2):S174–80. doi: 10.1016/s0022-3476(05)80016-2
91. Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services. Table D7.5, Page 445 for 6–12 m (2020). U.S. Department of Agriculture, Agricultural Research Service, Washington, DC.
92. American Academy of Pediatrics. Responsive Feeding (April 28, 2023). AAP-Responsive-Feeding_Print-Fact-Sheet.pdf. (Accessed March 12, 2024).
93. American Academy of Pediatrics. How Often and How Much Should Your Baby Eat? How Often and How Much Should Your Baby Eat?—HealthyChildren.org (April 2, 2024). (Accessed June 27, 2024).
94. Centers for Disease Control and Prevention. How much and How Often to Feed (April 11, 2022). Available online at: https://www.cdc.gov/infant-toddler-nutrition/?CDC_AAref_Val=https://www.cdc.gov/nutrition/infantandtoddlernutrition/foods-and-drinks/how-much-and-how-often.html (Accessed February 10, 2025).
95. U.S. Department of Agriculture, Food and Nutrition Service, WIC Works Resource System. Infant Feeding: Tips for Food Safety (October 2016). Infant Feeding Food Safety (usda.gov). (Accessed March 12, 2024).
96. Centers for Disease Control and Prevention. Choking Hazards (February 25, 2022). Available at: https://www.cdc.gov/infant-toddler-nutrition/foods-and-drinks/choking-hazards.html?CDC_AAref_Val=https://www.cdc.gov/nutrition/infantandtoddlernutrition/foods-and-drinks/choking-hazards.html (Accessed February 10, 2025).
97. American Academy of Pediatrics. Food Safety and Children (January 10, 2024). Available at: https://www.aap.org/en/patient-care/environmental-health/promoting-healthy-environments-for-children/food-safety/ (Accessed July 24, 2024).
98. Centers for Disease Control and Prevention. (June 28, 2022). Solid Foods in Early Care and Education (ECE): Tips for ECE Providers. Available online at: https://www.cdc.gov/obesity/strategies/early-care-education/pdf/solid-foods-ece-062022.pdf (Accessed July 24, 2024).
Keywords: guidance, families, nutrition, feeding practices, early childhood, lifelong health, healthy eating, infants and young children
Citation: Swanson WS, Ross ES, Matiz LA, Czerkies L, Huss LR, Smith-Simpson S, Bettler J and Pac S (2025) Essential elements for learning to eat: guidance to support families with infants and young children. Front. Pediatr. 13:1493780. doi: 10.3389/fped.2025.1493780
Received: 9 September 2024; Accepted: 12 March 2025;
Published: 27 March 2025.
Edited by:
Valeria Calcaterra, University of Pavia, ItalyReviewed by:
Virginia Rossi, University of Milan, ItalyCopyright: © 2025 Swanson, Ross, Matiz, Czerkies, Huss, Smith-Simpson, Bettler and Pac. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lyndsey R. Huss, bHluZHNleS5odXNzQHVzLm5lc3RsZS5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.