
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 29 January 2025
Sec. Social Pediatrics
Volume 13 - 2025 | https://doi.org/10.3389/fped.2025.1479298
This article is part of the Research Topic Advances in Pediatric Rehabilitation Clinical Trials: Design, Methods, and Analysis View all 8 articles
Introduction: Children with medical complexity (CMC) are medically fragile with severe brain damage and chronic conditions, necessitating daily care. Their neurological impairments often limit participation in childhood activities, affecting quality of life. Current assessment tools fail to detect subtle abilities in CMC, hindering development of effective rehabilitation goals and interventions. The Pediatric Awareness and Sensory Motor Assessment (PASMA) was created to fill this gap, providing sensitive measurement of sensory awareness and motor response across five domains (i.e., olfactory, visual, auditory, gustatory, and tactile).
Methods: In this retrospective study, a Rasch analysis was conducted on PASMA data for CMC. The PASMA was administered five times over ten weekdays to each child, reflecting its intended clinical use to gain a reliable sense of each child's awareness.
Results: Analysis of data from 36 CMC revealed that the PASMA is sufficiently unidimensional, effectively measuring sensory awareness and motor response as a single construct. Its rating scale structure was validated without modifications, and the item hierarchy matched clinical expectations. High item reliability (0.97) was observed, with one item (V2 blink in response to light) slightly misfitting, but without affecting overall measures. Adequate person reliability was observed (0.81), with 15% person misfit. Person misfit did not degrade item measures or model statistics. Differential item functioning (DIF) was noted for the three easiest items on specific days. The PASMA successfully stratified participants into three distinct awareness levels (low, medium, and high awareness), without floor or ceiling effects.
Discussion: The PASMA is a valid unidimensional measure of sensory awareness and motor response in CMC. Rating scale characteristics, item hierarchy, and person separation measures all support the PASMA's measurement properties within this heterogeneous sample of CMC. DIF findings support a potential reduction in the recommended number of PASMA administrations per individual. Future research will focus on establishing rater reliability and external validity. Additional efforts will support health professionals to utilize the PASMA for baseline assessments, guiding personalized interventions, and tracking progress.
Conclusion: Clinical use of the PASMA could provide new opportunities to detect subtle abilities, preferences, and changes in CMC, to promote meaningful participation and improve quality of life.
Children with medical complexity are a medically fragile subset of children who have severe brain damage, chronic medical conditions, and persistent intensive daily care needs. Their origins of brain damage are varied and primary health conditions for these children include but are not limited to severe forms of cerebral palsy, traumatic brain injury, hypoxic encephalopathy, and genetic diseases (1, 2). Their needs commonly include complex medication regimens and dependence on medical equipment and technology including wheelchairs, ventilators, and feeding tubes.
Advances in medical technology have led to increased survival of children with medical complexity. Unfortunately, the neurological damage associated with medical complexity causes severe cognitive and motor disabilities. For this reason, children with medical complexity have intensive daily care needs and require special education programs, social services, and coordinated medical and rehabilitative care (3). Additional sequalae of medical complexity include unmet health care needs, family stress, limited participation in typical childhood occupations, and compromised quality of life (1, 4, 31).
Interprofessional health care teams including rehabilitation providers (i.e., physical therapists, occupational therapists, and speech language pathologists) can play an essential role in providing family support, and improving health, participation, and quality of life for children with medical complexity. However, the assessment tools currently used with this population do not offer adequate clinical information to guide long-term rehabilitation decision-making. For instance, imaging and electroencephalogram (EEG) are used to detect structural neurological impairment in children with brain damage, but they do not provide reliable information about functional capabilities or impairments for this population (5). Broad classifications of brain damage like the Glasgow Coma Scale (GCS) (6–8), the JFK Coma Recovery Scale-Revised (CRS-R) (9, 10), and The Rancho Levels of Cognitive Functioning Scale (LCFS) (11) provide important information in the acute phases of treatment. However, they do not have the sensitivity to identify subtle sensory awareness and motor behaviors.
Without appropriate assessment tools, interprofessional team members miss opportunities to develop appropriate goals and enhance participation and quality of life for this population. As a result, children with medical complexity commonly receive passive and custodial care instead of appropriate individualized care. Therefore, to improve care for children with medical complexity, there is an urgent need for an assessment that measures subtle abilities including nuanced signs of sensory awareness and purposeful motor behaviors. To meet this need, the Pediatric Awareness and Sensory Motor Assessment (PASMA) was developed by an interprofessional team of clinicians, therapists, and researchers who serve children with medical complexity. This is the first publication about this assessment.
The PASMA is an observation-based assessment designed to capture subtle signs of awareness of/response to sensory stimulation across multiple sensory domains, to help health professionals gain baseline knowledge of the child's awareness, guide individualized interventions, and monitor changes over time. The instrument was modeled after a similar tool for adults with severe brain damage, the Sensory Modality Assessment and Rehabilitation Technique (Adult SMART) (12). The Adult SMART is more effective at discriminating awareness and detecting higher levels of cognitive functioning in individuals with severe neuro-disability compared to other tools used with this population, including the Western Neuro Sensory Stimulation Profile (WNSSP) (13, 14), the JFK Coma Recovery Scale (15), and the Sensory Stimulation Assessment Measure (13, 16).
The purpose of the present study was to examine item-level measurement properties of the PASMA using Rasch analysis. Unlike classical test theory which evaluates psychometric properties of an instrument as a whole, Rasch analysis examines measurement properties of each individual item within an assessment (17). Rasch analysis uses probabilistic mathematical modeling to examine a tool's ability to quantify abstract constructs in a meaningful way (18), which is especially useful for assessments that are based on clinician observation or patient report rather than physiological measurement (17, 32). Rasch analysis can be conducted when items within an assessment represent a single construct and a reasonable hierarchy of item difficulty can be presumed. When analyzing a dataset, the Rasch mathematical model assigns each assessment item a “difficulty” score and each person an “ability score”, and the probability that each person will be successful on each item is calculated based on these scores (17). The model produces multiple metrics of measurement properties for each assessment item and produces an ordered version of the assessment with item difficulty set on a linear scale (17).
We hypothesized that the PASMA's measurement characteristics would align with Rasch measurement theory as evidenced by measurement unidimensionality, an appropriate rating scale system, and an item hierarchy that aligns with clinical and theoretical expectations.
Study methodology was informed by the RULER statement (33). The present study is a retrospective secondary analysis of clinical data collected during a prospective descriptive cohort study of children with medical complexity. Informed consent was obtained for participation in the prospective study. Deidentified data were used in the present study and IRB approval of this secondary analysis was not required (19).
Medically stable children with medical complexity between the ages of 5 and 21 years old were eligible for inclusion in this study. Children with uncontrolled life-threatening diseases were excluded.
The PASMA consists of 30 scored items, and additional unscored components (e.g., a baseline observation period and documentation of observed side preferences for 17 items, described below) that provide important information about the child. Before beginning the scored portion of the PASMA, the child is seated in a quiet exam room for a five-minute baseline observation period. During this period, the assessor observes and documents the child's alertness and common motor behaviors (e.g., specific voluntary and involuntary movements). After the baseline observation period, the 30 scored items are administered. These items are structured across five sensory domains: Olfactory (four items), visual (10 items), auditory (two items), gustatory (six items), and tactile (eight items). Table 1 shows all PASMA items listed by sensory domain.
For 23 PASMA items, scoring is dichotomous (i.e., 0 = No response OR the child's commonly observed motor response, meaning no response beyond baseline motor patterns; 2 = a discrete response to the sensory information presented). The other seven PASMA items use a three-point rating scale (i.e., 0 = least possible response; 1 = medium response; 2 = best response). Table 2 shows examples of administration and scoring directions for select PASMA items.
Importantly, 17 PASMA items are administered on both the right and left side of the body (i.e., one olfactory item, six visual items, two auditory items, and eight tactile items) because a participant's responsiveness to unilateral stimuli will vary depending on their specific brain damage. Only the participant's best response for each item (i.e., response on the preferred side) is included in the PASMA score (see Table 3). Therefore, the item scores included in the Rasch analysis represent each participant's best sensory awareness and motor response (i.e., when all stimuli are presented on their preferred side). However, the participant's performance on both sides and any observed side preferences are recorded on the PASMA score sheet for use by clinicians and caregivers. Additionally, any other observed sensory preferences may be documented but are not scored (i.e., a preferred color on visual items, preferred scent on olfactory items, or preferred taste on gustatory items).
Like the Adult Smart, the PASMA was designed to be administered five times per participant, on five different days within 10 calendar weekdays. Multiple administrations are recommended because conditions that elicit each child's best performance (e.g., time of day and alertness) vary. This administration schedule allows the assessor to gain a thorough understanding of an individual's sensory awareness and motor functioning within a relatively short timeframe (12).
All but two participants in this sample completed testing on all five days; two completed less than five days of testing (completed 2 and 3 days) due to acute medical issues. Each participant who completed 5 days of testing was either seen in the morning for 3 days and the afternoon for 2 days, or vice versa. The time of day was recorded, but all scores from each PASMA administration were included in the Rasch analysis without controlling for time of day. This design was selected to examine the strength of item-level measurement properties irrespective of participant alertness level, to ensure a robust instrument. To examine whether dependent pairs of data impacted results, Differential Item Functioning was examined across the 5 assessment days.
Rasch analysis of the PASMA was completed with the Rating Scale Model in Winsteps version 3.93.1 (20).
The Rating Scale Model assumes unidimensionality of the instrument, meaning that all items on the instrument examine the same measurement construct. We hypothesized the PASMA captures a single comprehensive measurement of a child's sensory and motor awareness that consists of the five sensory domains. We tested this with a principal components analysis of residuals (21). The following criteria were used to determine whether unidimensionality was sufficient for measurement: (1) at least 50% variance in the data is explained by the Rasch dimension, (2) the first contrast in residuals explains <∼4% of data variance, and (3) the size (Eigenvalue) of the first contrast in the standardized residuals is ≤2 (22). If criteria were not met (i.e., suggesting multiple dimensions exist), we examined item clusters for additional dimensions and determined whether clusters made sense clinically and theoretically.
We also compared disattenuated correlations of additional dimensions with the Rasch dimension, to determine whether multiple dimensionality affected person measurement. Disattenuated correlations >0.82 were considered to represent dependent item clusters which were sufficiently unidimensional and not degrading measurement (22).
Additionally, we tested the Rasch model assumption that items on the instrument are locally independent. Items were considered locally independent if correlations between standardized residuals of items did not exceed 0.7 (33).
Linacre's three rating scale criteria were used to determine the appropriateness of rating scale categories: (1) Each rating scale category has a minimum of 10 observations; (2) The average measures of rating scale categories advance monotonically; and (3) Outfit mean square values are less than 2.0 (23).
Item and person fit statistics were compared to previously established criteria to identify possible misfit (24). Items and individuals were classified as misfitting the Rasch model if outfit statistics had mean square standardized residuals ≥1.4 and standardized z-scores ≥2. Misfitting items were removed to examine the effect on remaining item fit and to determine whether their removal affected person ability measures. Items with misfit were retained if removing them caused additional items to misfit and/or if removing the item did not have a meaningful effect on person ability measures.
If >10% of persons in the sample were found to misfit the model's expectations for item response patterns, the effect of this misfit was explored by removing persons with the most unexpected patterns from the dataset to determine whether this affected item difficulty measures. Misfitting persons were retained if removal did not influence item difficulty measures.
The Rasch model produces item difficulty measures and person ability measures on the same interval scale using logits. Lower measures are assigned to easier items and persons with less ability. Higher measures are assigned to harder items and persons with more ability. Thus, conducting a Rasch analysis produces a hierarchy of item difficulty, based on the measure estimates of item difficulty. We examined this hierarchy to determine whether it was consistent with clinical and theoretical expectations (25).
We examined the distribution of person ability in our sample and assessed for floor effects and ceiling effects, defined as >15% of individuals in the sample having the minimum or maximum possible score, respectively (26).
Tests of differential item function (DIF) were used to test whether the test administration day had an effect on item difficulty measures. Items were considered to have DIF if item difficulty measures were different by a magnitude of 0.5 logits and had an associated t-statistic that was >2 or <−2 (27).
Person separation index was used to evaluate the assessment's ability to separate people into statistically distinct strata. The formula below was used to calculate the number of strata in our sample (28):
Thirty-six children with medical complexity participated in the original data collection study and all PASMA data collected from these participants was included in the present analysis. Participants were between 5 and 21 years old with a mean age of 11 years. The sample included 11 females (31%) and 25 males (69%), and multiple races and ethnicities were represented (see Table 4). All participants (100%) had severe brain damage, but the origins of brain damage varied; primary health conditions included cerebral palsy, traumatic brain injury, hypoxic encephalopathy, and genetic diseases. At the time of testing, all children were confirmed by their physician or nurse to be medically stable, defined as having life-threatening diseases under control. All 36 participants (100%) were wheelchair users and were dependent on caregivers for mobility, communication, and daily care needs (i.e., eating, bathing, grooming, dressing, toileting,). In addition to primary diagnoses, many participants had co-occurring medical conditions (e.g., 42% had a history of seizures) and many required specific medical support for survival (e.g., 75% used a gastrostomy tube for feeding and 11% used a tracheostomy tube for breathing).
The principal components analysis showed that the Rasch dimension explained 46.0% of the variance in our data, which did not meet the criterion of >50%. The first contrast in residuals explained 6.2% of the variance in our data, which did not meet the criterion of <4%. The corresponding eigenvalue was 3.4, which did not meet the criterion of <2.0.
Because criteria for unidimensionality were not met, we examined additional clusters to determine whether there was a clinical/theoretical explanation. We found that the secondary dimension consisted of visual items and was therefore explained by these items representing a specific sensory system. We examined the disattenuated correlations between the primary dimension (i.e., the Rasch dimension) and secondary dimensions, which was 1.0 (meeting the guideline of >0.82). This indicates that these two clusters of items are dependent and therefore, can be treated as representative of the same latent construct without degrading measurement quality (29). Therefore, the PASMA is sufficiently unidimensional for measuring sensory awareness/motor response, and all items can be considered a single construct.
Correlations between standardized residuals of items did not exceed 0.7 for any item pairs, meeting the assumption of local independence.
Rating scale structures for PASMA items met the three essential criteria. (1) Each rating scale category had >10 observations. (2) The rating scale categories advanced monotonically, and (3) Outfit mean square values are <than 2.0. The rating scale structure for the PASMA, observed averages for each score, and associated infit and outfit mean square values are shown in Table 5.
Item fit statistics are presented in Table 6. One of the 30 PASMA items (V2 blink in response to light) misfit the Rating Scale Model, with outfit mean square values and standardized z-scores above our pre-specified thresholds (≥1.4 and ≥2.0, respectively). Removing this item caused another item to misfit (G5 seeking taste lip gloss). Figure 1 shows results from the comparison of person ability measures with vs. without the misfitting item. The person ability measures from these scenarios were very highly correlated (R = 0.9926), indicating that removing this item does not cause a significant change in person ability measures. Therefore, we determined that keeping this item did not degrade PASMA measurement properties.
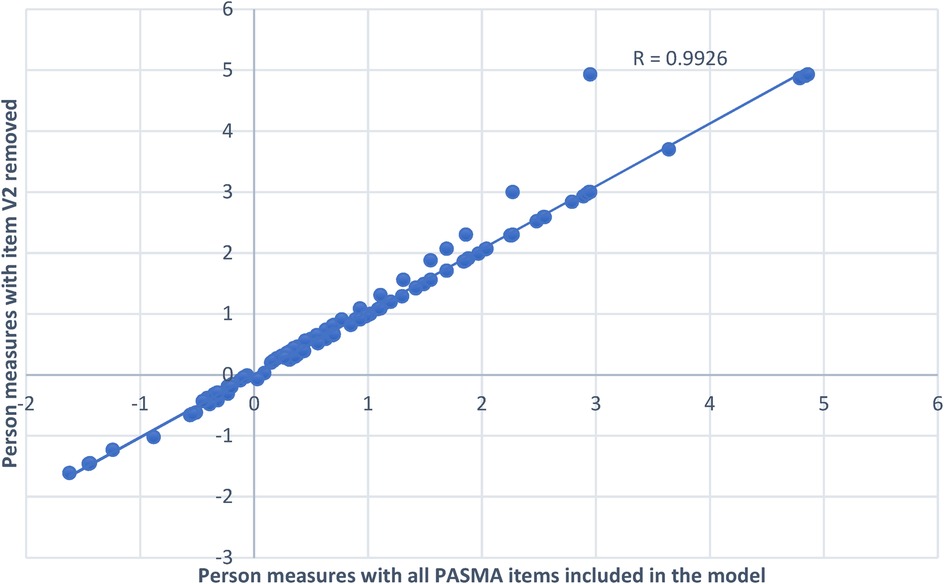
Figure 1. Comparing person ability measures with vs. without misfitting item (V2 blink in response to light) in the model. The x-axis of this figure displays person ability measure estimates with all PASMA items included in the model. The y-axis displays person ability measures estimates when the one misfitting item (V2 blink in response to light) was removed from the model. In spite of a few person measure outliers that occurred when item V2 was removed, person ability measures for both scenarios (with and without item V2) are very highly correlated (R = 0.9926). The line of best fit (the upward slanting dotted line) for both datasets is very close to person measure estimates with all items included in the model. Therefore, all items were left in the final analysis model.
Person fit scores from 26 of the 177 assessments (15%) in this sample misfit the Rasch model. Assessment scores for the nine (5%) most misfitting person response strings (i.e., tests for a single day) were removed from the model and item measures and item difficulty measures were compared with and without these persons. Figure 2 shows that item difficulty measure estimates with and without the nine most misfitting person response strings in the model were very highly correlated (R = 0.997). Therefore, misfitting persons did not affect item difficulty measures or the item hierarchy.

Figure 2. Comparing item difficulty measures with vs. without the 9 most misfitting person response strings in the model. The x-axis of this figure displays item difficulty measure estimates with all person response strings included in the model. The y-axis displays item difficulty measure estimates when the nine most misfitting person response strings were removed from the model. Item difficulty measures were very highly correlated (R = 0.997) for both scenarios (with vs. without the most misfitting person response strings). The line of best fit (the upward slanting dotted line) for both datasets is very close to the original item measure estimates (with all persons included in the model). Therefore, all person response strings were left in the final analysis model.
The person-item map (Figure 3) displays the distribution of all persons and items on the same linear scale. The range of distribution of person ability and item difficulty in our sample was six logits (−2–4). Average item difficulty is anchored at 0 logits by the Rating Scale Model, and average person ability level in our sample was 1.35 logits (SE = 0.46), which was >1 standard deviation higher than the average item difficulty. The easiest item on the PASMA was O1 mint scent (−1.54 logits, model SE = 0.25), and the most difficult item was V10 visually guided reach (1.97 logits, SE = 0.12).
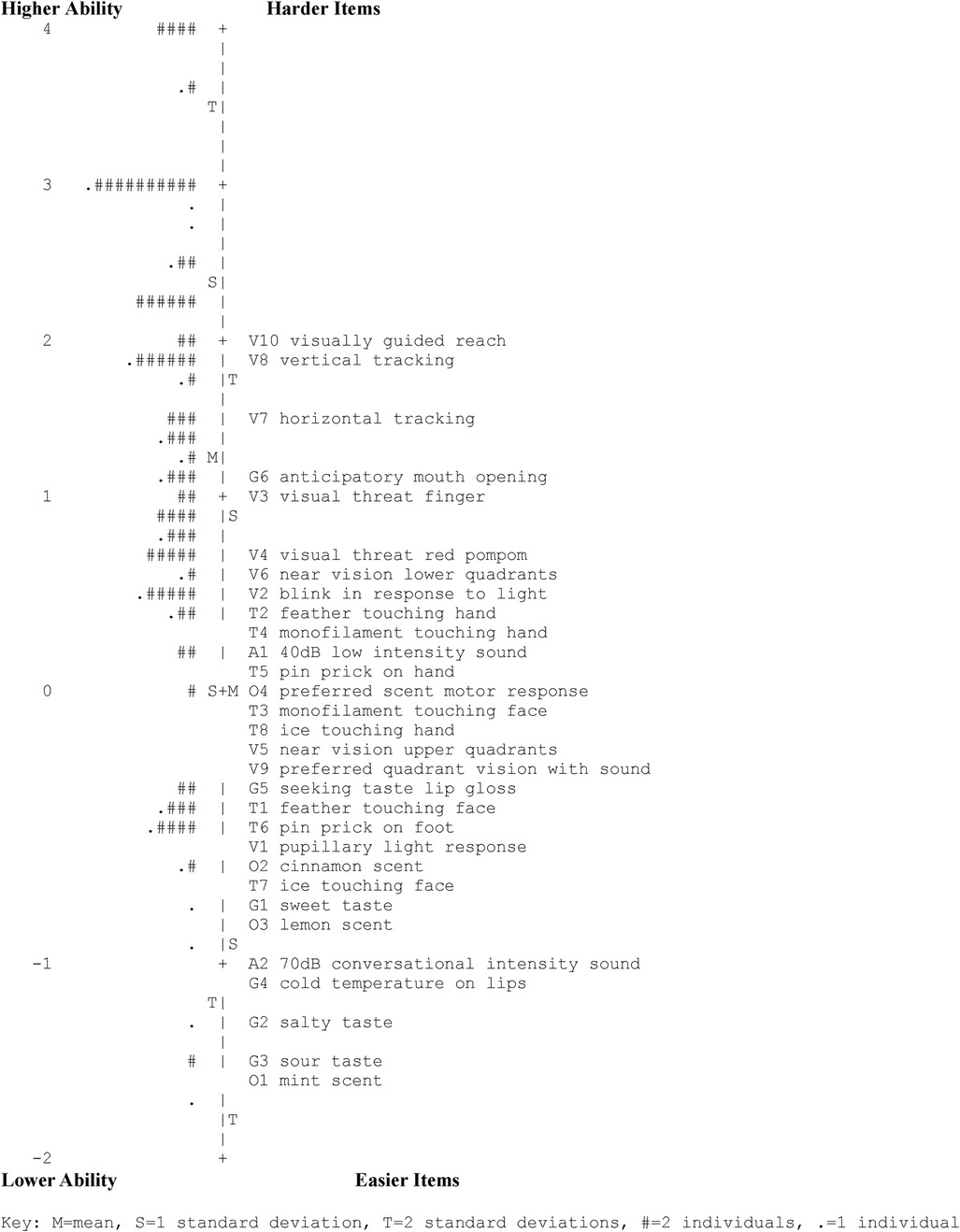
Figure 3. PASMA person-item Map. Numbers on the left side of the map (ranging from −2 to 4) are logits that represent measurement of person ability (left of the vertical dotted line) and item difficulty (right of the vertical dotted line). The lowest person ability and easiest items are shown at the bottom, and the highest person ability and hardest items are shown at the top. The Rating Scale Model anchors the mean item difficulty estimate for a sample to a logit value of 0. Therefore, items with a logit of 0 (i.e., O4 preferred scent motor response) represent the average item difficulty. This map shows that the easiest PASMA item is O1 mint scent and the hardest item is V10 visually guided reach. Left of the vertical dotted line, the lowest symbol (.) represents the participant with the least ability; the highest symbol (####) represents the participants with the most ability. Within this sample, the mean person ability was 1.35 logits higher than the mean PASMA item difficulty (anchored at 0 logits).
The PASMA had high person reliability (0.81) and high item reliability (0.97). Zero of 177 assessment score totals (0%) received the minimum possible score, and eight of 177 (4.5%) received the maximum possible score on the PASMA. Thus, floor and ceiling effects were not observed.
Twenty-seven PASMA items (90%) functioned consistently when examined across five assessment days, but three items (i.e., O1 mint scent, G2 salty taste, and G3 sour taste) showed differential item function on specific days, as shown in Figure 4. These are the three easiest items on the assessment, meaning that participants were most likely to notice/respond to these olfactory and gustatory sensory stimuli. On some test days, participants responded less than expected to these three items, but even then, the items were among the easiest on the PASMA.
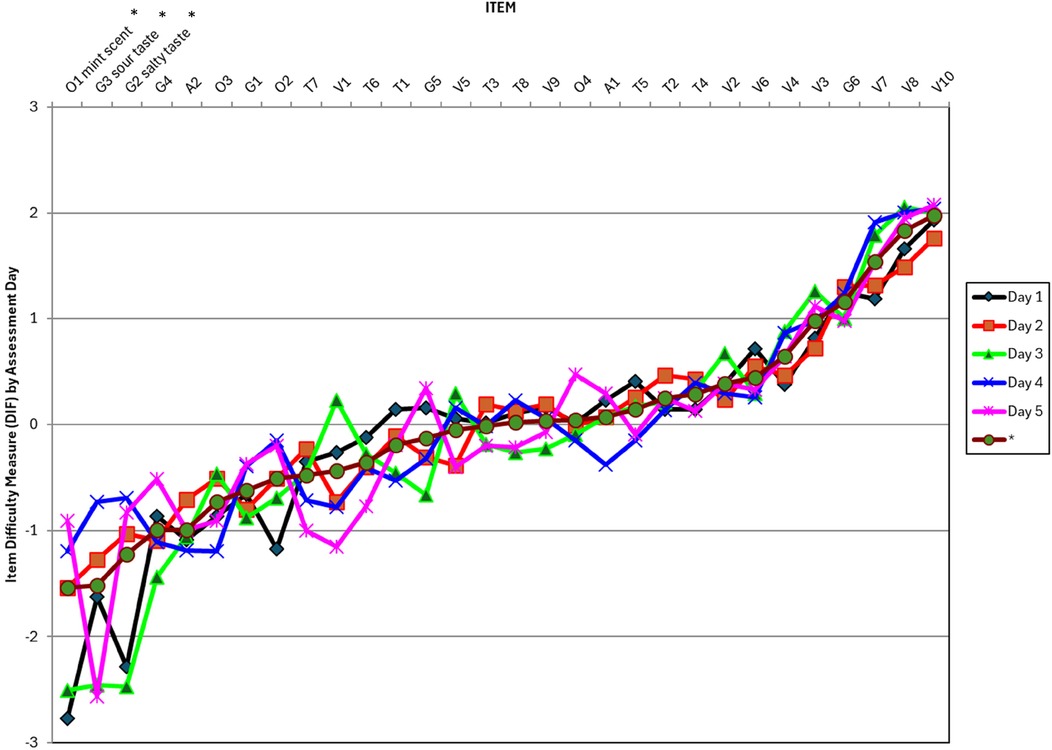
Figure 4. Differential item functioning across PASMA assessment days. PASMA items are listed in difficulty order from the easiest (on the left) to the hardest (on the right). Item difficulty estimates for each assessment day (1 through 5) are shown on the plot in the color/shape that corresponds with the key on the right side of the figure. The maroon line with a circle on the plot (shown below Day 5 on the figure legend) represents the item difficulty measure estimate from all assessment days combined. *Full items names are shown for the three items with differential item functioning across assessment days (O1 mint scent, G3 sour taste, and G2 salty taste). These items are the easiest on the PASMA (based on measure estimates for all assessment days combined) and their item difficulty was significantly lower on the days with differential item functioning (represented by the lowest points on the y-axis between −2 and −3).
The person separation index was 2.06, indicating that the PASMA differentiated individuals in our sample into 3.08 statistically distinct strata.
Findings from this study demonstrate that the PASMA is a unidimensional measure that can be used to quantify sensory and motor awareness in children with medical complexity.
A secondary dimension consisting of visual items of the PASMA was identified, and these items could be explored as an independent measurement scale in future study. However, the Rasch analysis findings show that keeping visual items in the PASMA and treating all sensory sections as a single construct does not degrade the assessment's measurement characteristics. Clinically, keeping all PASMA items together enables the examiner to have one unified measurement value for a child's overall sensory and motor functioning which can guide holistic participation-based interventions. Therefore, we do not recommend removing any items at this time. This decision is supported by Andrich's metaphor of measuring student achievement in mathematics: Achievement can be subdivided into areas such as addition, subtraction, multiplication, and division and tested separately; or they can be grouped together on a single test to provide a broader measurement of mathematical achievement (30).
The item hierarchy (shown on the right side of the person-item map in Figure 3) shows that the easiest PASMA items examine participants' responses to intense discreet sensory inputs (e.g., demonstrating awareness of smells such as mint, lemon, and cinnamon; concentrated sour, salty, and sweet flavors; oral tactile sensations such as cold temperatures; hearing their name spoken by a familiar person; and pupils reflexively constricting in response to light shining into eyes).
More challenging items included more subtle sensory inputs (e.g., whispering the child's name or touching the child's hand or face with a feather or pipe cleaner). Consistent hierarchies emerged within sensory sections. For example, demonstrating awareness of touch sensations on the face was relatively easy (i.e., a feather, a pipe cleaner, and ice), but demonstrating awareness of touch sensations on the hands was found to be more challenging. Patterns of tactile awareness were also identified: Noticing a pin prick stimulus on the hand was the easiest, whereas noticing a pipe cleaner or a feather touching the hand was more difficult.
The most difficult PASMA items were those that required participants to demonstrate a higher level motor response to sensory stimuli (e.g., moving away from approaching visual threats; opening mouth in response to a preferred flavor being offered; purposeful visual pursuits such as horizontal and vertical tracking to follow an engaging toy; and purposeful reaching toward the toy).
Overall, the item hierarchy derived from this analysis is consistent with clinical and theoretical expectations of sensory awareness and motor responses. Collectively, findings from this analysis suggest that this measurement scale is a conceptually valid representation of the construct of sensory and motor awareness among children with medical complexity.
As shown in Table 6, Rasch analysis of the PASMA revealed that one item (V2 blink in response to light) misfit criteria for outfit. However, since this misfitting item does not degrade the measurement properties of the PASMA, we recommend keeping all items in the assessment to preserve fidelity to the original construct validity of this assessment. Item V2 takes less than ten seconds to administer, and it provides important information about whether the blink reflex is intact. This information can inform safe and comfortable participation in activities where noxious visual stimuli may be present. For instance, for children who do not reflexively blink in response to light, protective measures (e.g., protective eyewear, reduced bright lights/glare, and/or lubricating eye drops) could promote enjoyable participation in meaningful activities in their home, school, and community settings.
The average person ability in this sample (1.35 logits) was higher than the average item difficulty (anchored at 0 logits by the Rasch model), but person-item match was adequate. The range of difficulty of PASMA items was sufficient to cover the spread of person ability in this sample, which was a heterogeneous group of children with medical complexity that was representative of the range of abilities observed among this population in clinical practice. Therefore, the item difficulty spread is believed to be sufficient to measure the wide range of sensory and motor awareness in the intended population of children.
The person separation index showed that the PASMA divided this sample into 3.08 statistically distinct person strata, meaning participants were separated into three groups based on sensory awareness and motor responsiveness: a group with low responsiveness, medium responsiveness, and the highest responsiveness (17). This distribution will be useful for identifying and understanding subgroups of sensory and motor awareness and may help to quantify changes (increases or decreases) in awareness which may occur in response to health status, medication, or rehabilitation.
Further exploration is needed to understand the cause of differential item function and determine whether this finding supports using fewer than five PASMA administrations per individual. For instance, if participants responded less to these items on later assessment days due to learning/habituation to the sensory stimuli, then fewer test administrations could reduce habituation, and thereby, reduce differential item functioning across days. Fewer PASMA administrations per individual could make using the assessment in clinical practice more feasible by decreasing the burden of testing on patients and therapists. However, because children with medical complexity commonly have variable alertness and responsiveness day to day, more research will be needed to demonstrate that the final recommended number of administrations (e.g., three) is sufficient to understand individuals' sensory and motor awareness and unique sensory and side preferences.
First, this study is a secondary analysis of data that was collected for purposes other than examining item-level measurement properties. As such, some dataset factors were not optimal for this analysis. For example, in the analysis we used only the best score for items that are tested on both sides of the body. This represents the individual's sensory and motor awareness in the most ideal conditions (i.e., when stimuli are presented on their preferred side). We believe this scoring system provides maximum opportunity for therapists and caregivers to recognize each individual's rehabilitative potential. However, for children with medical complexity, sensory and motor awareness may be lower when conditions are not ideal (e.g., when stimuli are presented on the non-preferred side). Although this discrepancy is represented qualitatively on the PASMA score sheet (i.e., by showing point values for each side and noting observed side preference), it is not represented in the PASMA scores used in this Rating Scale Analysis.
Second, while the heterogeneous sample promotes generalizability of findings to a wide range of children with medical complexity between five and 21 years old, our findings are not generalizable to individuals with medical complexity outside of this age range. Additionally, factors that caused individuals to misfit the model expectations are not well understood, but our findings may be less generalizable to this misfitting subset of children with medical complexity.
The PASMA enables detection of subtle motor responses to sensory input. This information will help therapists and caregivers to set appropriate goals, design individualized interventions, and detect changes in the child's awareness and responses over time.
Perhaps most importantly, the PASMA provides information about a child's unique sensory strengths and preferences. This information can readily be applied to choose activities that suit the individual, to promote meaningful and enjoyable participation in daily activities. For example, a child who responds positively to olfactory and gustatory stimuli may enjoy being involved in cooking activities. A child who responds positively to tactile stimuli may enjoy water-based activities or hippotherapy.
Further, information from the PASMA can be applied to set up activities and environments to promote optimal participation. For instance, for a child participating in hippotherapy, knowledge of whether they respond more to stimuli on one side of the body will inform the therapist's position and how the horse's movements are directed. Auditory and visual environments of the activity can also be modified to meet the child's unique needs to make participation as immersive and enjoyable as possible (e.g., using an ideal voice volume and the best color for the horse's reigns and saddle). Importantly, knowledge of a child's sensory preferences can also be applied to everyday environments to help the child feel more regulated, comfortable, and safe.
This study has established conceptual and structural validity of the PASMA using methodology informed by the RULER statement (33). Additionally, a degree of item measure reliability was established by examining differential item functioning across the five days that the PASMA was administered, but more research is needed to assess the reproducibility of these results and to address items that have differential function across assessment days. Future research is also needed to establish rater reliability and external validity of the PASMA. Future research will also examine consequential validity and will be geared toward optimizing use of PASMA results to guide rehabilitation decision-making for children with medical complexity.
Although opportunities for future study have been described and will further enhance measurement properties of the PASMA, overall, this Rasch analysis provides support for this assessment's item-level measurement properties. The PASMA is a unified measurement tool which captures subtle signs of awareness of and response to sensory stimulation across domains in children with medical complexity. Future work will examine reliability and validity of the PASMA and will examine how baseline knowledge from this instrument can be used to guide individualized interventions, promote meaningful and enjoyable participation, and monitor changes over time for children with medical complexity.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Medical University of South Carolina Institution Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
BM: Conceptualization, Data curation, Formal Analysis, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. BS: Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. CC: Conceptualization, Data curation, Investigation, Resources, Writing – original draft. KK: Conceptualization, Data curation, Investigation, Resources, Writing – original draft. CD: Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition, Investigation, Resources, Supervision, Visualization.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. American Physical Therapy Association's Academy of Pediatric Physical Therapy, Foundation for Physical Therapy Research Institutional Development Award from the National Institute of General Medical Sciences of the National Institutes of Health under grant number 4–GM104941 (PI: Binder–Macleod).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. (2012) 130(6):e1463–70. doi: 10.1542/peds.2012-0175
2. Millar K, Rodd C, Rempel G, Cohen E, Sibley KM, Garland A. The clinical definition of children with medical complexity: a modified Delphi study. Pediatrics. (2024) 153(6):1–10. doi: 10.1542/peds.2023-064556
3. Cardenas A, Esser K, Wright E, Netten K, Edwards A, Rose J, et al. Caring for the caregiver (C4C): an integrated stepped care model for caregivers of children with medical complexity. Acad Pediatr. (2023) 23(2):236–43. doi: 10.1016/j.acap.2022.06.001
4. Pordes E, Goodpasture M, Bordini BJ. Overmedicalization in children with medical complexity. Pediatr Ann. (2020) 49(11):e478–85. doi: 10.3928/19382359-20201019-01
5. Glader L, Plews-Ogan J, Agrawal R. Children with medical complexity: creating a framework for care based on the international classification of functioning, disability and health. Dev Med Child Neurol. (2016) 58(11):1116–23. doi: 10.1111/dmcn.13201
6. Van de Voorde P, Sabbe M, Rizopoulos D, Tsonaka R, De Jaeger A, Lesaffre E, et al. Assessing the level of consciousness in children: a plea for the Glasgow coma motor subscore. Resuscitation. (2008) 76(2):175–9. doi: 10.1016/j.resuscitation.2007.07.007
7. Holmes JF, Palchak MJ, MacFarlane T, Kuppermann N. Performance of the pediatric Glasgow coma scale in children with blunt head trauma. Acad Emerg Med. (2005) 12(9):814–9. doi: 10.1197/j.aem.2005.04.019
8. Caruana M, Hackenbruch SN, Grech V, Farrugia R. Inconsistency in the application of Glasgow coma scale in pediatric patients. Med Princ Pract. (2024) 33(1):41–6. doi: 10.1159/000534797
9. Giacino JT, Kalmar K, Whyte J. The JFK coma recovery scale-revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. (2004) 85(12):2020–9. doi: 10.1016/j.apmr.2004.02.033
10. Lovstad M, Froslie KF, Giacino JT, Skandsen T, Anke A, Schanke AK. Reliability and diagnostic characteristics of the JFK coma recovery scale-revised: exploring the influence of rater’s level of experience. J Head Trauma Rehabil. (2010) 25(5):349–56. doi: 10.1097/HTR.0b013e3181cec841
11. Gouvier W, Blanton P, LaPorte K, Nepomuceno C. Reliability and validity of the disability rating scale and the levels of cognitive functioning scale in monitoring recovery from severe head injury. Arch Phys Med Rehabil. (1987) 68(2):94–7.3813863
12. Gill-Thwaites H, Munday R. The sensory modality assessment and rehabilitation technique (SMART): a valid and reliable assessment for vegetative state and minimally conscious state patients. Evaluation studies research support, non-U.S. Gov't. Brain Inj. (2004) 18(12):1255–69. doi: 10.1080/02699050410001719952
13. Gill-Thwaites H. The sensory modality assessment rehabilitation technique—a tool for assessment and treatment of patients with severe brain injury in a vegetative state. Brain Inj. (1997) 11(10):723–34. doi: 10.1080/026990597123098
14. Wilson SL, Gill-Thwaites H. Early indication of emergence from vegetative state derived from assessments with the SMART–a preliminary report [research support, non-U.S. Gov't]. Brain Inj. (2000) 14(4):319–31. doi: 10.1080/026990500120619
15. Kalmar K, Giacino JT. The JFK coma recovery scale–revised. Neuropsychol Rehabil. (Sep 2005) 15(3-4):454–60. doi: 10.1080/09602010443000425
16. Rader MA, Ellis DW. The sensory stimulation assessment measure (SSAM): a tool for early evaluation of severely brain injured patients. Brain Inj. (1994) 8:309–21. doi: 10.3109/02699059409150982
17. Bond TG, Fox CM. Applying the Rasch Model: Fundamental Measurement in the Human Sciences. 2nd ed. New York: Routledge Taylor & Francis Group (2007).
18. Wright BD, Linacre JM. Observations are always ordinal; measurements, however, must be interval. Arch Phys Med Rehabil. (1989) 70(12):857–60. Available online at: https://www.scopus.com/inward/record.uri?eid=2-s2.0-0024759059&partnerID=40&md5=1736796b47ba7dffed56f669049a38272818162
19. HHS.gov. Revised Common Rule. (2024). Available online at: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/common-rule/index.html (Accessed July 29, 2024).
20. Linacre JM. Winsteps Rasch Measurement [Computer Software] (2015). Chicago, IL. Available online at: Winsteps.com
21. Linacre JM. Detecting multidimensionality: which residual data-type works best? J Outcome Meas. (1998) 2:266–83.9711024
22. Linacre JM. A user’s guide to Winsteps® Ministeps Rasch model computer programs. (2022). Winsteps Program Manual. Available online at: https://www.winsteps.com/winman/copyright.htm (Accessed June 03, 2024).
23. Linacre JM. Optimizing rating scale category effectiveness. J Appl Meas. (2002) 3(1):85–106. Available online at: https://www.scopus.com/inward/record.uri?eid=2-s2.0-0036373007&partnerID=40&md5=e28018aae216ddbb6e14af4ae34366de11997586
24. Wright BD, Linacre J M. Reasonable mean-square fit values. Rasch Measurement Transactions. (1994). Available online at: Available online at: https://www.rasch.org/rmt/rmt83b.htm (Accessed July 29, 2024).
25. Tennant A, Pallant JF. DIF matters: a practical approach to test if differential item functioning makes a difference. Rasch Meas Trans. (2007) 20:1082–4.
26. McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. (1995) 4(4):293–307. doi: 10.1007/BF01593882
27. DIF - DPF - bias - interactions concepts. (n.d.). Available online at: https://winsteps.com/winman/difconcepts.htm (Accessed June 03, 2024).
28. Wright BD, Masters GN. Number of person or item strata. Rasch Measurement Transactions. (2006). Available online at: https://www.rasch.org/rmt/rmt264g.htm (Accessed June 17, 2024).
29. Baghaei P. Local dependency and Rasch measures. Rasch Meas Trans. (2008) 21(3):1105–6. Available online at: https://www.rasch.org/rmt/rmt213b.htm
30. Andrich D. Implications and applications of modern test theory in the context of outcomes based education. Stud Educ Eval. (2002) 28:103–21. doi: 10.1016/S0191-491X(02)00015-9
31. Seltzer RR, Thompson BS. Pediatrician as advocate and protector: an approach to medical neglect for children with medical complexity. Pediatr Clin N Am. (2024) 71(1):59–70. doi: 10.1016/j.pcl.2023.08.006
32. Velozo CA. Using measurement to highlight occupational therapy’s distinct value. Am J Occup Ther. (2021) 75(6):1–12. doi: 10.5014/ajot.2021.746001
Keywords: children with medical complexity (CMC), Pediatric Awareness and Sensory Motor Assessment (PASMA), Rasch analysis, item response theory (IRT), pediatric assessment, assessment validation
Citation: Mulrenin B, Seamon BA, Cormack C, Kascak KL and Dodds C (2025) Item-level measurement properties of the pediatric awareness and sensory motor assessment in children with medical complexity. Front. Pediatr. 13:1479298. doi: 10.3389/fped.2025.1479298
Received: 11 August 2024; Accepted: 16 January 2025;
Published: 29 January 2025.
Edited by:
Stephanie C. DeLuca, Virginia Tech, United StatesReviewed by:
Harshvardhan Singh, University of Alabama at Birmingham, United StatesCopyright: © 2025 Mulrenin, Seamon, Cormack, Kascak and Dodds. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cynthia Dodds, ZG9kZHNjYkBtdXNjLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.