- 1Department of Child Health, Universitas Indonesia/Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 2Department of Child Health, Budhi Mulia Mother and Child Hospital, Pekanbaru, Indonesia
- 3Department of Neonatology, Khoo Teck Puat-National University Children’s Medical Institute, National University Hospital, Singapore, Singapore
- 4Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 5Department of Pediatrics, Ewha Womans University College of Medicine, Seoul, Republic of Korea
- 6Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 7Neonatal Research Network of Japan, Kyorin University, Tokyo, Japan
- 8Division of Neonatology, National Research Institute for Child Health and Development, Tokyo, Japan
Background: Optimum neonatal resuscitation practices are vital for improving neonatal survival and neurodevelopment outcomes, particularly in extremely preterm infants. However, such practices may vary between high-income countries (HICs) and low-middle-income countries (LMICs). This study aimed to evaluate the resuscitation practices of high-risk infants in a large multi-country sample of healthcare facilities among HICs and LMICs in Asia under the AsianNeo Network.
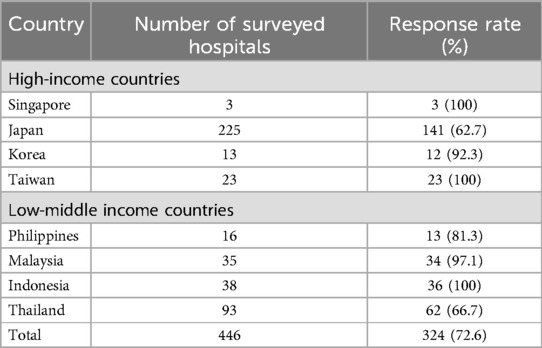
Methods: In 2021, a customized 6-item online survey on resuscitation practices of infants born at <29 weeks gestation (or birth weight <1,200 g) was sent by the representative of each country's neonatal network to all the Neonatal Intensive Care Units (NICUs) participating in AsianNeo network. At the time of the survey, there were 446 participating hospitals in eight countries: four high-income countries (Japan, Singapore, South Korea, and Taiwan) and four low-middle-income countries (Malaysia, Indonesia, Philippines, and Thailand).
Results: The study included 446 hospitals, with a response rate of 72.6% (ranging from 62.7% to 100%), with 179 (55.2%) in HICs and 145 (44.7%) in LMICs. Routine attendance of experienced NICU physicians during resuscitations is reported to be higher in HICs than LMICs, both during daytime (79% vs. 40%) and nighttime (62% vs. 23%). The NRP guidelines in each country were varied, with 4 out of 8 countries using indigenously developed guidelines. Equipment availability during resuscitation was also variable; saturation monitors, radiant warmers, and plastic wraps were available in almost all hospitals, whereas oxygen and air blenders, heated humidified gas, and end-tidal CO2 detectors were more available in HICs. The most common device for Positive Pressure Ventilation (PPV) was the T-piece resuscitator (52.3%).
Conclusion: The neonatal resuscitation practices for extremely preterm infants, encompassing staff, equipment, and guidelines, exhibited variance between HICs and LMICs in the AsianNeo region. Further enhancements are imperative to narrow this gap and optimize neonatal outcomes.
Background
Despite the significant progress achieved in recent decades and the notable improvement in survival rates, the care of very preterm and extremely preterm infants remains a complex endeavor, particularly from the moment of delivery (1–3). These infants are more prone to necessitate resuscitation and are at a heightened risk of experiencing complications during the resuscitative process (4). Multiple factors contribute to this, including susceptibility to hypothermia, underdeveloped pulmonary function, susceptibility to infection, and increased vulnerability to organ injury (5). Depending on the specific medical circumstances, resuscitative measures may encompass a range of increasingly intensive interventions, from ventilation and oxygenation to the administration of epinephrine and volume expanders (6).
Interventions to improve neonatal resuscitation are essential to any strategy to reduce neonatal mortality. Training neonatal healthcare providers in neonatal resuscitation should result in a 30% reduction in mortality among full-term babies and 5%–10% in preterm babies (7). Besides the personnel's skill and knowledge, adequate equipment in all delivery settings is crucial. Despite this fact, there has been a disparity between different countries regarding improving neonatal resuscitation, especially among LMICs (8). Neonatal mortality rates in HICs range from 0.8 to 2.4 per 1,000 live births, while in LMICs, the rates range from 4.6 to 12.6 per 1,000 live births (9).
Surveys on neonatal resuscitation have been conducted in high-resource countries (10–12) and more recently, in low and middle-income countries (7, 13, 14). However, a multicenter study that emphasizes the baseline characteristics leading to such discord between high-income and low—and middle-income countries has not yet been conducted. This survey aims to describe differences in resuscitation practices and equipment availability in a large representative sample between different Asian countries. We report data regarding the personnel, device, and guideline/program available for neonatal resuscitation, especially for infants born at <29 weeks gestation (or birth weight <1,200 g) in the AsianNeo regions.
Methods
Participants
The survey was conducted under the umbrella of the Asian Neonatal Network Collaboration (AsianNeo), which was established in 2019 to improve neonatal care in Asia. The AsianNeo currently consists of nine neonatal networks from Indonesia, Japan (network leader), Malaysia, Philippines, Singapore, South Korea, Taiwan, Thailand, and Sri Lanka (9, 15), but only eight countries participated in the survey (Table 1). The classification into HICs and LMICs is established using the Gross National Income (GNI) per capita, determined through the World Bank Atlas method. Countries with a GNI per capita above US$14,005 are considered high-income, while those below this threshold are classified as LMICs (16). Four high-income countries (Japan, Singapore, South Korea, and Taiwan) and four low-income countries (Malaysia, Indonesia, Philippines, and Thailand).
Survey instrument
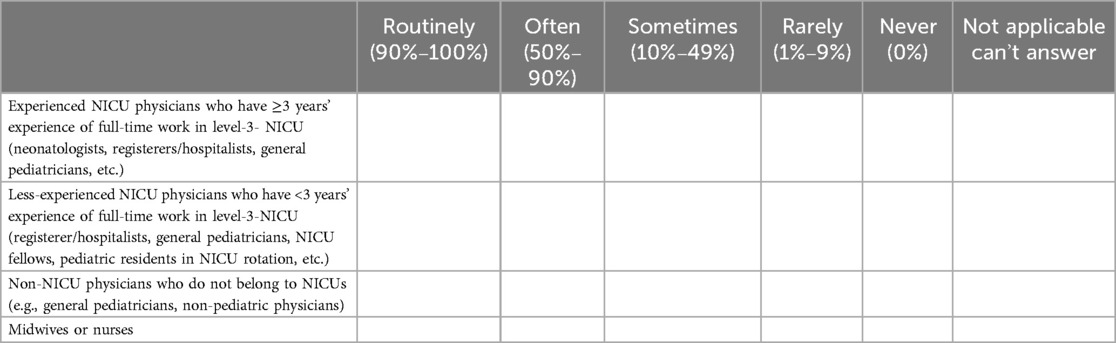
A survey on the resuscitation of high-risk infants (gestational age <29 weeks or birth weight <1,200 g) was conducted from February to March 2021 at level III neonatal medical centers across Asian countries, including both government and private hospitals. The decision to extend the gestational age and birth weight cutoff beyond extreme preterm and ELBW is due to a limited number of hospitals in certain countries that actively resuscitate infants in those categories. The survey consisted of 6 inquiries concerning the presence of the resuscitation team, the guidelines utilized, the standard device for positive pressure ventilation, the percentage of trained primary resuscitators, and other devices used during resuscitation (Appendix 1).
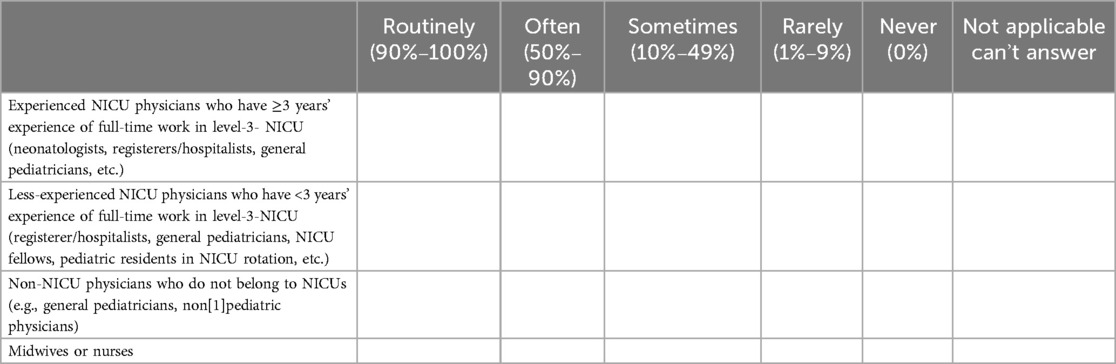
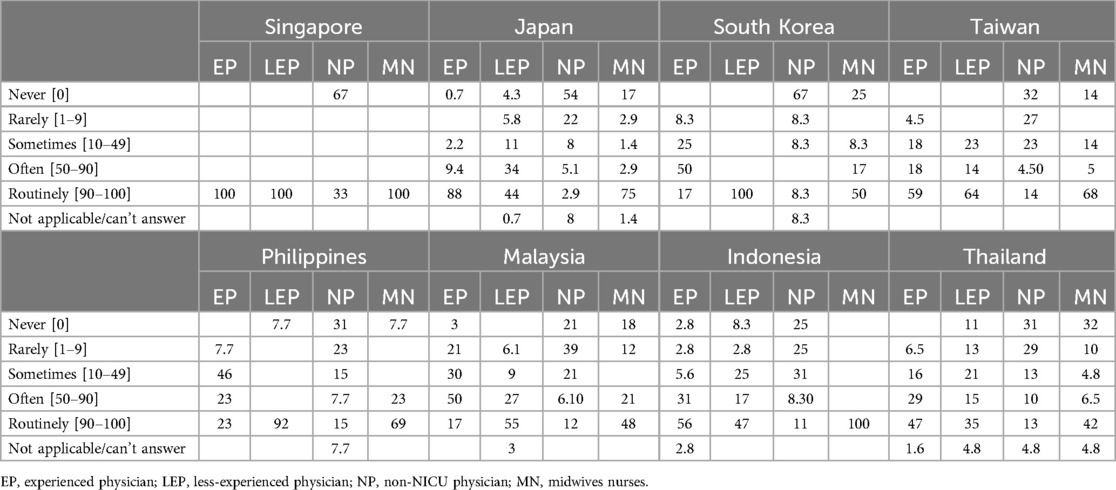
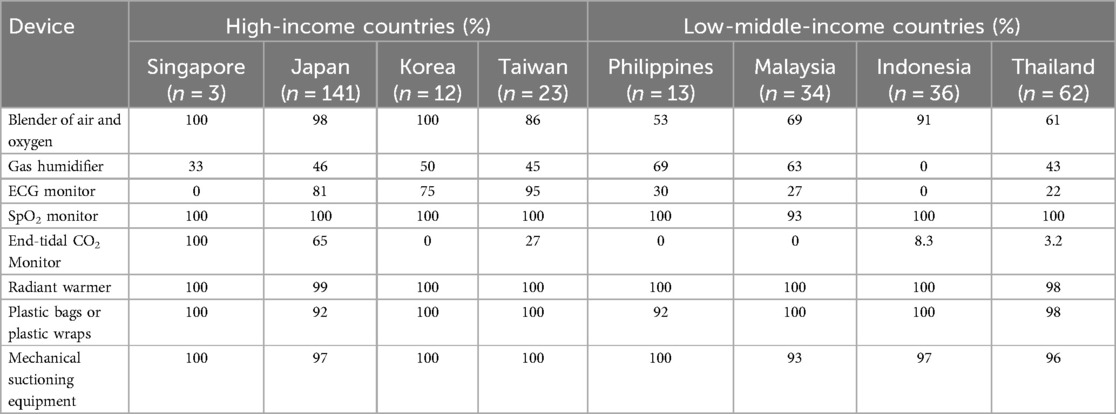
Primary resuscitators are categorized into four groups: experienced NICU physicians, less-experienced NICU physicians, non-NICU physicians, and midwives/nurses. Experienced NICU physicians are those who have at least 3 years’ experience of full-time work in level-3- NICU (neonatologists, registerers/hospitalists, general pediatricians, etc.), while less-experienced NICU physicians have less than 3 years' experience of full-time work in level-3-NICU (registerer/hospitalists, general pediatricians, NICU fellows, pediatric residents in NICU rotation, etc.). Non-NICU physicians who do not belong to NICUs (e.g., general pediatricians, non-pediatric physicians). Midwives and nurses are combined in one group because in some countries, including Indonesia, they receive similar training in neonatal resuscitation.
The survey was performed using an English-language structured online questionnaire (SurveyMonkey®) and completed by the person or his/her designate in charge of neonatal care at each hospital. The questionnaire was translated into the native language of non-English-speaking countries. The country representative of each neonatal network sent the request for the survey to all the NICUs participating in the AsianNeo.
Statistical analysis
We performed statistical analyses using STATA 14.0 (STATA Corp, College Station, TX, USA). We conducted proper data coding and categorization and verified the data for completeness and accuracy. We performed descriptive statistics for personnel and program variables and obtained the means or medians for device variables. Categorical data were expressed as numbers and percentages.
Ethics
The ethical approval was obtained from the Ethics Committee of the Faculty of Medicine, University of Indonesia, Cipto Mengunkusumo Hospital, Jakarta, Indonesia. All participants provided informed consent to participate in this study.
Results
The study involved 446 hospitals, with a response rate of 72.6%, varying from 62.7% to 100% across different countries. The distribution of participating hospitals was equal between HICs and LMICs, with 179 (55.2%) located in HICs and 145 (44.7%) in LMICs (Table 1). Data for neonatal resuscitation personnel, equipment, and trained staff were missing from 5 hospitals in Japan (3), Malaysia (1), and Taiwan (1).
Resuscitation team during daytime and nighttime
The personnel attending neonatal resuscitation varies during the daytime in different countries (Appendix 2) and among the HICs vs. LMICs (Figure 1). HICs have a higher presence of experienced and midwives or nurses during the daytime than those in LMICs (Figures 1A,D). However, similarities in resuscitation team components between the two groups are observed in the routine attendance of less experienced NICU physicians and non-NICU physicians (Figures 1B,C).
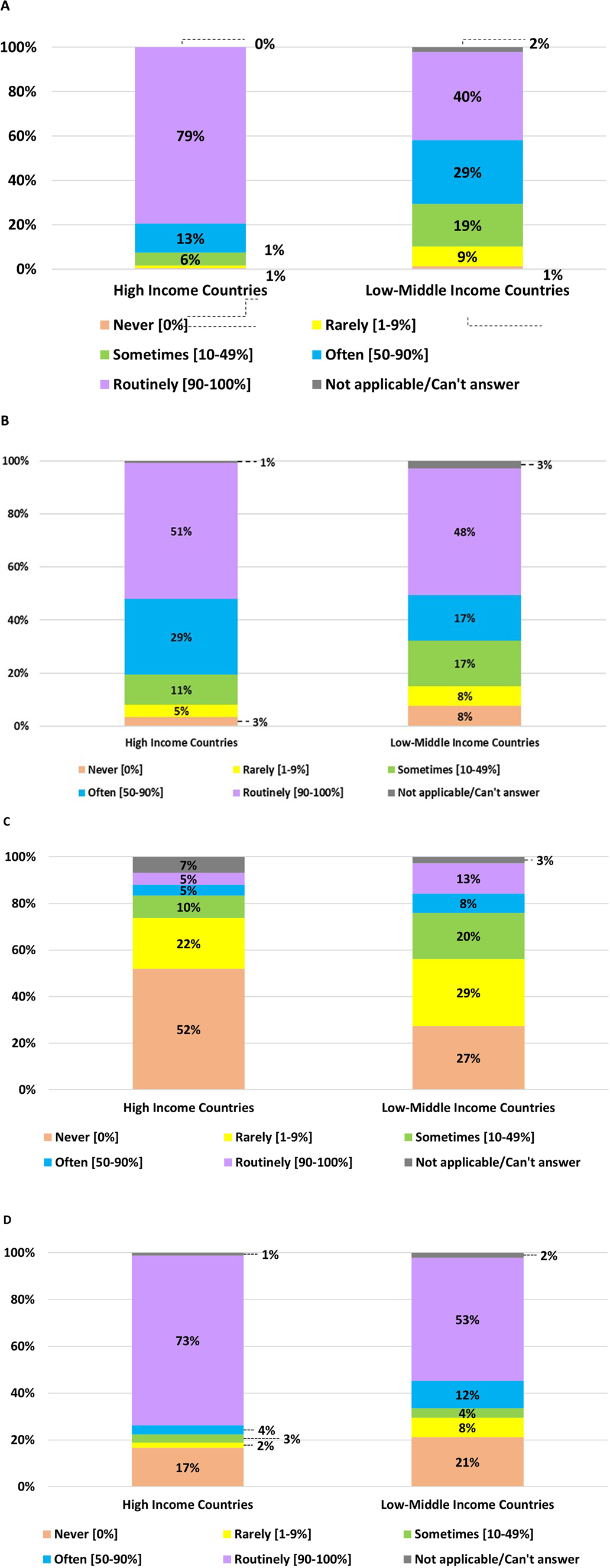
Figure 1. Personnel attending the resuscitation of infants born at <29 weeks gestation (or birth weight <1,200 g) during daytime in HICs vs. LMICs. (A) Experienced NICU physicians with ≥3 years of work experience. (B) Less-experienced NICU physicians with <3 years of work experience. (C) Non-NICU physicians. (D) Midwives or nurses.
Figure 2 shows the team present for nighttime neonatal resuscitation in HICs and LMICs. The details of the nighttime team across countries are presented in Appendix 2. Compared to daytime resuscitation, the presence of experienced NICU physicians during nighttime has decreased overall in all participants, from 61.9% to 44%. However, it is still more common in HICs than LMICs. Attendance among less-experienced NICU physicians is lower during night shifts compared to LMICs. During nighttime resuscitation, the proportion of less experienced NICU and non-NICU physicians, midwives, or nurses is comparable to daytime resuscitation.
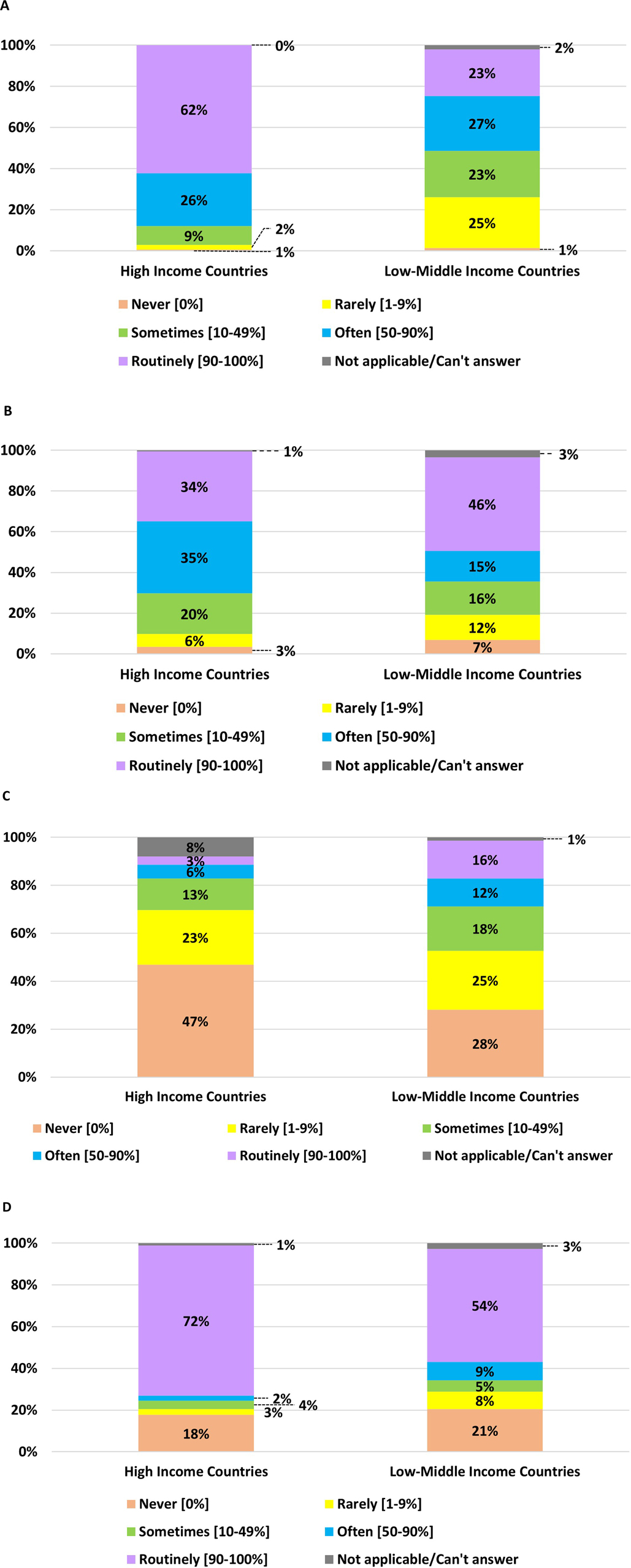
Figure 2. Personnel attend the resuscitation of infants born at <29 weeks gestation (or birth weight <1,200 g) during nighttime in HICs vs. LMICs. (A) Experienced NICU physicians with ≥3 years of work experience. (B) Less-experienced NICU physicians with <3 years of work experience. (C) Non-NICU physicians. (D) Midwives or nurses.
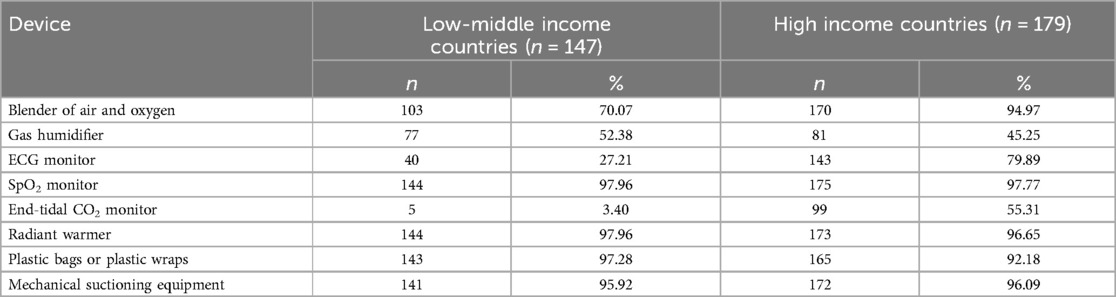
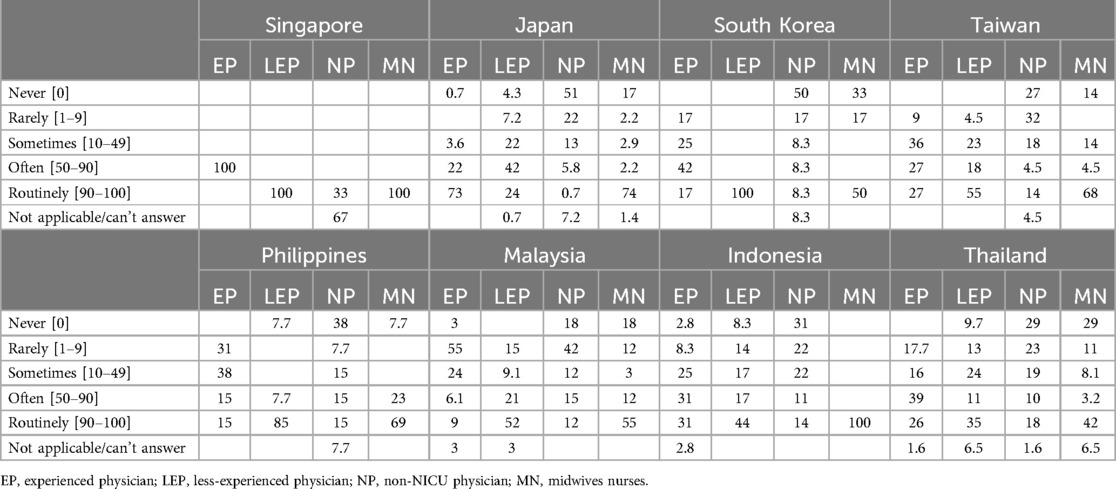
Most participants in MICs and LMICs had a SpO2 monitor, radiant warmers, plastic bags or wraps, and mechanical suctioning equipment. Nevertheless, there was a substantial discrepancy between HICs and LMICs regarding the availability of some essential equipment, including blenders of air and oxygen, ECG monitors, and end-tidal CO2 monitors. Interestingly, gas humidifiers were slightly more prevalent in LMICs than in HICs (Table 2). Details of equipment availability in each country is presented in Appendix 3.
The equipment used for providing respiratory support during resuscitation varied. However, the T-piece resuscitator was the most used for very preterm infants (Figure 3). Interestingly, the T-piece resuscitator is more widely used in low- and middle-income countries (LMICs) than in high-income countries (HICs) (Table 3). Japan is the country with the lowest utilization of the T-piece resuscitator and instead prefers the use of the flow-inflating bag (Appendix 4).
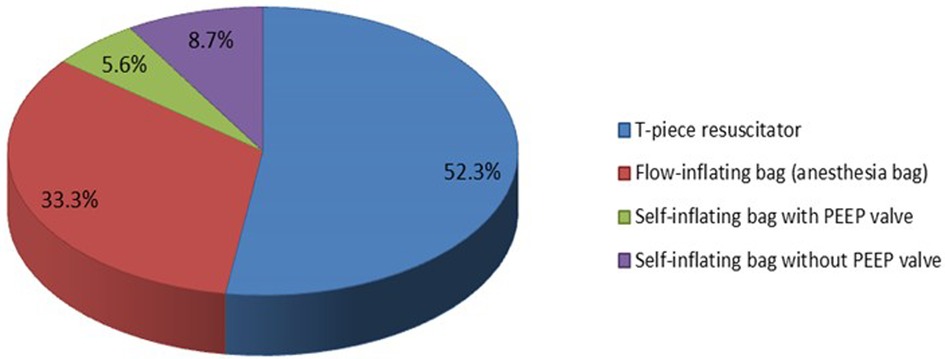
Figure 3. The most common device for positive pressure ventilation (PPV) used in neonatal resuscitation of very preterm infants born at <29 weeks gestation (or birth weight <1,200 g) immediately after birth.
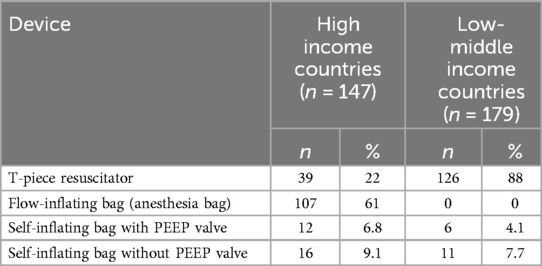
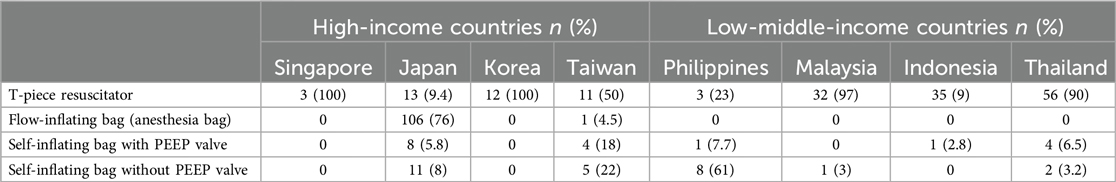
Table 3. The most common device for positive pressure ventilation (PPV) used in neonatal resuscitation of very preterm infants born at <29 weeks gestation (or birth weight <1,200 g) just after birth.
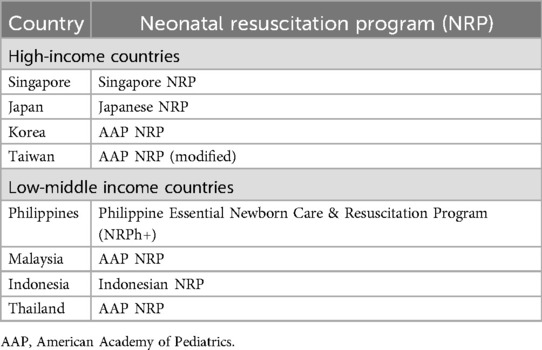
Table 4 presents the variations in resuscitation guidelines in Asian-Neo countries. However, American Academy of Pediatrics (AAP) guidelines are used in half of the participating countries, both in HICs and LMICs. Most primary resuscitators already have either certification or training in neonatal resuscitation programs, both in HICs and LMICs (Figure 4).
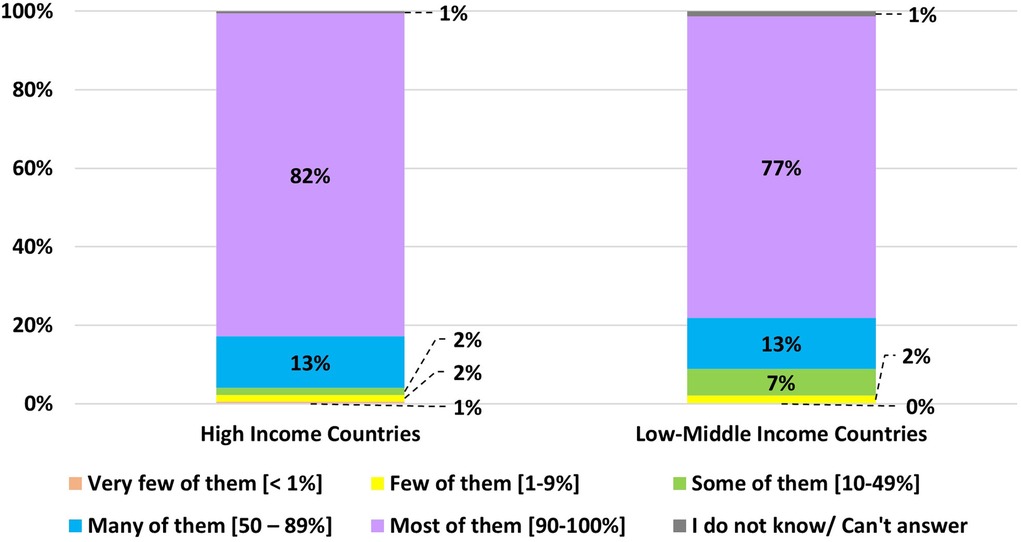
Figure 4. The proportion of the main resuscitators of very preterm infants (gestational age <29 weeks or birth weight <1,200 g) trained or certified for neonatal resuscitation programs regardless of the type of the program.
Discussion
This survey provides the first comprehensive analysis of neonatal resuscitation preparedness and resources in Asian countries. It highlights disparities in resuscitation practices for infants born before 29 weeks of gestational age and weighing less than 1,200 g, comparing HICs to LMICs within the AsianNeo network. Although we do not examine the differences in neonatal mortality rates between these two groups in this survey, a previously published AsianNeo report indicated that neonatal mortality rates in HICs range from 0.8 to 2.4 per 1,000 live births. In contrast, in LMICs, the rates range from 4.6 to 12.6 per 1,000 live births (9). These disparities may stem from differences in personnel and medical equipment availability between the two groups.
The key factor affecting neonatal outcomes in both groups is the availability of experienced NICU physicians, which is more common in high-income countries (HICs) than in low- and middle-income countries (LMICs), both during the day and at night. Although expected, this matter warrants attention as per the recommendation of the American Academy of Pediatrics, which stipulates the presence of a proficient neonatal resuscitation team. In the event of an anticipated high-risk birth, such as that of an extremely preterm infant, it is imperative to assemble a well-staffed team capable of providing positive pressure ventilation, tracheal intubation, chest compressions, emergency vascular access, medication preparation, and event documentation before the birth (5). Based on the meta-analysis conducted by Patel et al. (8), implementation of neonatal resuscitation training resulted in a significant reduction in early neonatal mortality.
The second most significant factor impacting outcomes is the equipment used in delivery or resuscitation rooms for extremely preterm infants. It was noted that LMICs lacked oxygen and air blenders, ECG monitors, and end-tidal CO2 (EtCO2) monitors. The American Heart Association's current recommendations advise adjusting the delivery of oxygen to newborns to achieve specific target oxygen levels rather than simply administering 100% oxygen (17). Without consistent access to oxygen blending, newborns in low-resource environments are often treated with pure oxygen and are placed at significant risk of hyperoxia-induced injury (18). For example, in India, the incidence of ROP is markedly higher than in high-income countries, and ROP has become the leading cause of avoidable blindness in children (19). A cardiac monitor with 3 chest leads or limb leads provides a rapid and reliable method of continuously displaying the baby's heart rate if the pulse oximeter has difficulty acquiring a signal (5). The International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations (CoSTR) also echoed this (20). Detecting exhaled CO2 and an increasing heart rate are the primary methods of confirming endotracheal tube insertion (5). EtCO2 monitoring may be an early indication of lung expansion and may help to guide successful respiratory support in the delivery room—an observational study conducted by Hawkes et al. (21) reported that EtCO2 monitoring in the delivery room is feasible and safe. EtCO2 values obtained after birth reflect the establishment of functional residual capacity and effective ventilation. Other clinical practices to confirm correct endotracheal tube placement include condensation in the endotracheal tube, chest movement, and the existence of equal breath sounds bilaterally. However, these practices have not been systematically evaluated in newborns (22).
There is room for improvement in resuscitation equipment across all participants. The gas humidifier was not universally available in most resuscitation rooms in LMICs and HICs. Oxygen given to newborns for a prolonged period of time should be heated and humidified to prevent heat loss (5). A meta-analysis conducted by Meyer et al. (23). The use of heated humidified gases showed that the number of infants with severe hypothermia (<35.5°C) was significantly reduced. It showed that a gas humidifier improved admission temperature in preterm infants.
From the survey, it was noteworthy that various resuscitation guidelines/programs were used in the participating countries, with 4 out of 8 countries using indigenously developed guidelines and other countries using the AAP guidelines. There are some differences among the national guidelines. For example, oxygen administration is divided into ≥35 weeks (21%) and <35 weeks (21%–30%) gestational age in both Indonesia and Japan guidelines, while Singapore guideline uses different categories such as ≥33 weeks (21%) and <33 weeks (21%–30%) gestational age. The room temperature is set into 23°C–25°C in both Singapore and Japan guidelines, while Indonesia guideline uses 24°C–26°C (16–18).
The strength of this study is representative data from both low-middle income countries and high-resource countries, comprehensive coverage of the survey's participants across the countries with high response rates even in the pandemic era with otherwise limited access to conduct direct surveys. However, this study has some limitations, such as the different number of participants in each country and reliance on self-reporting by a person contacted through the survey without inspection of the sites. This would cause room for a degree of bias; however, with the limitation of direct surveys, this is a viable alternative and room for possible future improvement of multicenter surveys. Another limitation we can improve in future studies is the details of each participant's hospital, resuscitation team size, and area background regarding the socio-economic and geographical conditions. These details could aid in a more specific strategy to improve neonatal resuscitation practice to the potential of each hospital.
Conclusion
We identified significant variations in neonatal resuscitation practices among Asian countries among the AsianNeo collaborators. This survey identifies the resources available, such as personnel, equipment, and program/guidelines, for neonatal resuscitation in low-income to high-resource countries with various socio-economic backgrounds. Our study provides the possibility for improvements through the AsianNeo network in neonatal care with specific strategies, using background data of each hospital as a basis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The ethical approval was obtained from the Ethics Committee of the Faculty of Medicine, University of Indonesia, Cipto Mengunkusumo Hospital, Jakarta, Indonesia. All participants provided informed consent to participate in this study.
Author contributions
RR: Conceptualization, Resources, Writing – original draft. RD: Investigation, Writing – review & editing. JS: Formal Analysis, Project administration, Writing – original draft. ZA: Data curation, Investigation, Writing – review & editing. YY: Data curation, Investigation, Writing – review & editing. SYK: Data curation, Investigation, Writing – review & editing. SC: Data curation, Investigation, Writing – review & editing. YC: Data curation, Investigation, Writing – review & editing. SK: Data curation, Resources, Writing – review & editing. FM: Data curation, Investigation, Software, Validation, Writing – review & editing. TI: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Higgins BV, Baer RJ, Steurer MA, Karvonen KL, Oltman SP, Jelliffe-Pawlowski LL, et al. Resuscitation, survival and morbidity of extremely preterm infants in California 2011–2019. J Perinatol. (2024) 44:209–16. doi: 10.1038/s41372-023-01774-6
2. Wall SN, Lee AC, Niermeyer S, English M, Keenan WJ, Carlo W, et al. Neonatal resuscitation in low-resource settings: what, who, and how to overcome challenges to scale up? Int J Gynaecol Obstet. (2009) 107:S47–64. doi: 10.1016/j.ijgo.2009.07.013
3. Zhu Z, Yuan L, Wang J, Li Q, Yang C, Gao X, et al. Mortality and morbidity of infants born extremely preterm at tertiary medical centers in China from 2010 to 2019. JAMA Netw Open. (2021) 4:e219382. doi: 10.1001/jamanetworkopen.2021.9382
4. Soraisham AS, Lodha AK, Singhal N, Aziz K, Yang J, Lee SK, et al. Neonatal outcomes following extensive cardiopulmonary resuscitation in the delivery room for infants born at less than 33 weeks gestational age. Resuscitation. (2014) 85:238–43. doi: 10.1016/j.resuscitation.2013.10.016
5. American Academy of Pediatrics. Textbook of neonatal resuscitation. In: Weiner GM, Zaichkin J, editors. Washington, DC: American Academy of Pediatrics (2021). 361.
6. Cavolo A, de Casterlé BD, Naulaers G, Gastmans C. Neonatologists’ decision-making for resuscitation and non-resuscitation of extremely preterm infants: ethical principles, challenges, and strategies—a qualitative study. BMC Med Ethics. (2021) 22:129. doi: 10.1186/s12910-021-00702-7
7. Trevisanuto D, Cavallin F, Arnolda G, Chien TD, Lincetto O, Xuan NM, et al. Equipment for neonatal resuscitation in a middle-income country: a national survey in Vietnam. BMC Pediatr. (2016) 16:1–8. doi: 10.1186/s12887-016-0664-0
8. Patel A, Khatib MN, Kurhe K, Bhargava S, Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatr Open. (2017) 1:e000183. doi: 10.1136/bmjpo-2017-000183
9. Isayama T, Miyake F, Rohsiswatmo R, Dewi R, Ozawa Y, Tomotaki S, et al. Asian neonatal network collaboration (AsianNeo): a study protocol for international collaborative comparisons of health services and outcomes to improve quality of care for sick newborn infants in Asia—survey, cohort and quality improvement studies. BMJ Open. (2024) 14:e082712. doi: 10.1136/bmjopen-2023-082712
10. Charles E, Hunt K, Murthy V, Harris C, Greenough A. UK neonatal resuscitation survey. Arch Dis Child Fetal Neonatal. (2018) 0:F1–2. doi: 10.1136/archdischild-2018-315526
11. Izquierdo M, Iriondo M, Ruiz C, Zeballos G, Sánchez M, Gonzalez E, et al. Survey of neonatal resuscitation practices showed post training improvements but need to reinforce preterm management, monitoring and adrenaline use. Acta Paediatr. (2017) 106(6):897–903. doi: 10.1111/apa.13791
12. Trevisanuto D, Gizzi C, Gagliardi L, Ghirardello S, Fabio SD, Beke A, et al. Neonatal resuscitation practices in Europe: a survey of the union of European neonatal and perinatal societies. Neonatology. (2022) 119(2):184–92. doi: 10.1159/000520617
13. Patel P, Nimbalkar S, Shinde M. Insights from a cross-sectional survey of neonatal resuscitation instructors from India. Sci Rep. (2023) 13(1):15255. doi: 10.1038/s41598-023-42382-w
14. Aso ME, Sharma A, Iloh K. Resuscitation of preterm infants in Nigeria—a national survey on practice. Niger J Clin Pract. (2022) 25(5):612–20. doi: 10.4103/njcp.njcp_1560_21
15. AsianNeo. About Us. Asian Neonatal Network Collaboration (AsianNeo) (2021). Available online at: https://asian-neo.org/about-us.html (Accessed July 30, 2024)
16. Bank W. World Bank Country and Lending Groups. Washington, DC: World Bank (2023). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (Accessed August 16, 2024)
17. Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, et al. Part 5: neonatal resuscitation: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2020) 142:S524–50. doi: 10.1161/CIR.0000000000000902
18. Mantena S, Burke TF. Oxygen blending is urgently needed in resource-limited settings. J Pediatr. (2021) 237:288–91. doi: 10.1016/j.jpeds.2021.04.060
19. Vinekar A, Dogra M, Azad RV, Gilbert C, Gopal L, Trese M. The changing scenario of retinopathy of prematurity in middle and low income countries: unique solutions for unique problems. Indian J Ophthalmol. (2019) 67:717–9. doi: 10.4103/ijo.IJO_496_19
20. Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres JW, Fawke J, et al. Neonatal life support 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. (2020) 156:A156–87. doi: 10.1016/j.resuscitation.2020.09.015
21. Hawkes GA, Kenosi M, Finn D, O’Toole JM, O’Halloran KD, Boylan GB, et al. Delivery room end tidal CO2 monitoring in preterm infants <32 weeks. Arch Dis Child Fetal Neonatal. (2016) 101:F62–5. doi: 10.1136/archdischild-2015-308315
22. Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, Gallagher J, et al. Part 15: neonatal resuscitation: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2010) 122:S909–19. doi: 10.1161/CIRCULATIONAHA.110.971119
23. Meyer MP, Owen LS, Te Pas AB. Use of heated humidified gases for early stabilization of preterm infants: a meta-analysis. Front Pediatr. (2018) 6:319. doi: 10.3389/fped.2018.00319
Appendix 1
AsianNeo survey: delivery and resuscitation.
1. During daytime, how often the following personnel attend the resuscitation of infants born at <29 weeks gestation (or birth weight <1,200 g) in your hospitals? (The attendance at resuscitation includes not only those as a main resuscitator but also those as a support person for neonatal resuscitation).
2. During nighttime, how often the following personnel attend the resuscitation of infants born at <29 weeks gestation (or birth weight <1,200 g) in your hospitals? (The attendance at resuscitation includes not only those as a main resuscitator but also those as a support person for neonatal resuscitation).
3. What is the most common device for positive pressure ventilation used in neonatal resuscitation of very preterm infants born at <29 weeks gestation (or birth weight <1,200 g) just after birth in your hospital?
a. T-piece resuscitator
b. Flow-inflating bag (anesthesia bag)
c. Self-inflating bag with PEEP valve
d. Self-inflating bag without PEEP valve
e. Other (please specify)
4. What is the most common device for positive pressure ventilation used in neonatal resuscitation of very preterm infants born at <29 weeks gestation (or birth weight <1,200 g) just after birth in your hospital?
a. T-piece resuscitator
b. Flow-inflating bag (anesthesia bag)
c. Self-inflating bag with PEEP valve
d. Self-inflating bag without PEEP valve
e. Other (please specify)
5. How much proportion of the main resuscitators* of very preterm infants (gestational age <29 weeks or birth weight <1,200 g) are trained or certified for neonatal resuscitation program regardless of the type of the program? Main resuscitators are the persons who manage respiratory support in resuscitation such as bag-mask ventilation.
a. Most of them [90%–100%]
b. Many of them [50%–89%]
c. Some of them [10%–49%]
d. Few of them [1%–9%]
e. Very few of them [<1%]
f. I do not know can't answer
6. Does your NICU generally use the following device or equipment for neonatal resuscitation of very preterm infants born at <29 weeks gestation (or birth weight <1,200 g) in delivery or resuscitation rooms when needed? Please select YES or NO for each device or equipment.
Appendix 2
Personnel attending the resuscitation during daytime and nighttime across countries.Daytime attendance
Nighttime attendanceAppendix 3
Equipment for neonatal resuscitation across countries.
Appendix 4
Most common device for positive pressure ventilation (PPV) across countries.
Keywords: neonatal resuscitation, gap practice, low-middle income countries, high-income countries, multicenter survey, preterm (birth)
Citation: Rohsiswatmo R, Dewi R, Sutantio J, Amin Z, Youn Y-A, Kim SY, Cho SJ, Chang YS, Kusuda S, Miyake F and Isayama T (2025) Addressing the gap in preterm resuscitation practices in high-income and low-middle income countries: a multicenter survey of the Asian neonatal network collaboration. Front. Pediatr. 12:1517843. doi: 10.3389/fped.2024.1517843
Received: 27 October 2024; Accepted: 31 December 2024;
Published: 30 January 2025.
Edited by:
Naveed Hussain, University of Connecticut Health Center, United StatesReviewed by:
Wannasiri Lapcharoensap, Oregon Health and Science University, United StatesMonika Patil, Baylor College of Medicine, United States
Copyright: © 2025 Rohsiswatmo, Dewi, Sutantio, Amin, Youn, Kim, Cho, Chang, Kusuda, Miyake and Isayama. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rinawati Rohsiswatmo, cmluYXJvaHNpc0BnbWFpbC5jb20=
 Rinawati Rohsiswatmo
Rinawati Rohsiswatmo Rizalya Dewi2
Rizalya Dewi2 Jennie Sutantio
Jennie Sutantio Zubair Amin
Zubair Amin Young-Ah Youn
Young-Ah Youn Satoshi Kusuda
Satoshi Kusuda Tetsuya Isayama
Tetsuya Isayama