- 1Department of Pediatric Neurology, Children’s Hospital Affiliated to Capital Institute of Pediatrics, Beijing, China
- 2Department of Pediatrics, Beijing Friendship Hospital, Capital Medical University, Beijing, China
- 3Center of Children’s Healthcare, Children’s Hospital Affiliated to Capital Institute of Pediatrics, Beijing, China
- 4Medical Technology Department, Peking University Sixth Hospital, Beijing, China
- 5Guangzhou Rainjet Medical Equipment Co., Guangzhou, Guangdong, China
Objective: To study the characteristics of event related potential P300 in preschool children with attention deficit hyperactivity disorder (ADHD) aged 4–6 years (4≤ age <6), and to explore the differences in cognitive function compared with healthy children. To explore a new method for the study of cognitive function in preschool children with ADHD.
Methods: A total of 73 preschool children aged 4–6 years were selected from the outpatient clinic of Neurology Department, the ADHD-specialized Clinic and Health Care Department of the Children's Hospital Affiliated to the Capital Institute of Pediatrics from March 2021 to May 2024. They were divided into the ADHD group (45 cases) and healthy children group (28 cases). Event related potential P300 was measured in all children and the amplitude and latency of the wave were compared between the two groups separately.
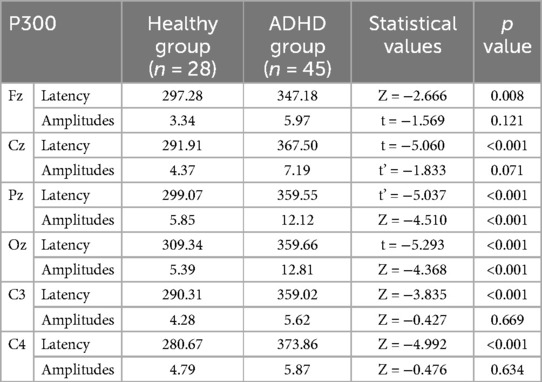
Results: The latency of P300 at all the recording electrodes (Fz, Cz, Pz, Oz, C3, C4) in the ADHD group was significantly longer than controls (p < 0.05). The wave amplitudes of children with ADHD were significantly higher than controls at Pz and Oz points.
Conclusion: The differences between two groups in P300 test show that preschool children with ADHD present longer latency at central line of the brain and bilateral central lobes compared with healthy children, and higher amplitude at the central parietal lobe and central occipital lobe. It may suggest that attention cognition has already impaired in preschool children with ADHD.
1 Introduction
Mental disorders are becoming one of the biggest global health problems in children and adolescents, which is also a major factor in their overall life expectancy (1). Attention deficit hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder in children and adolescents that manifests with symptoms of inattention, hyperactivity, and/or impulsivity in early childhood (2, 3). In recent years, a significant increasing number of preschool children with ADHD symptoms has been coming to clinical attention (4). It is reported that the prevalence of ADHD among school-age children is between 9 and 15 precent (5). However, many mental disorders are present during preschool years but most of them are not diagnosed until school age, including ADHD, the prevalence of which is estimated to be about 3% in preschool children (6). According to previous studies, nearly 90% of preschoolers with ADHD are not received a timely diagnosis, suggesting that they are less likely to receive effective and proper interventions that can lead to adverse outcomes (6, 7). In addition, the majority (more than 70%) of preschoolers with clinical issues about ADHD will persist throughout the school years and even into early adulthood, continuing to meet the diagnostic criteria for ADHD, which means children who show hyperactivity in the preschool years tend to develop impulsive behaviors, aggressive behaviors and social adjustment problems during the school years (8, 9). Consequently, it is very important to timely identify and assess the disorders in the preschool years of children with ADHD to improve their symptoms and the quality of life. Due to the instability of behavioral manifestations during preschool period, there is an imminent demand to find an objective predictor to assist clinicians in evaluating the condition of children.
Cognitive function refers to the advanced cognitive abilities necessary for the goal-directed behavior, which develops primarily during the preschool period (aged 3–5 years) (10). Current studies generally support that the cognitive function deficit is an essential contributor to the symptoms with ADHD, and this association is well-documented not only in school-age children but also in preschoolers (11–13). Therefore, timely identification of cognitive function deficit in children during their preschool years may contribute to early assessment and diagnosis of ADHD. Electrophysiological techniques, as a non-invasive measurement of brain state and neural activation, have been widely used in the studies to explore the cognitive functions due to their high temporal resolution and functional relevance (14).
Event-related potentials (ERPs) is one of the most broadly utilized techniques in non-invasive neurological testing today. Through time-locked mechanism, ERPs can reveal the changes in neuronal signals in milliseconds, providing a temporal and load measure of changes in subject's brain activity while processing events occurring in real time (15). P300 is an endogenous component of ERPs with a peak of approximately 250–600 ms and reflects the cognitive function of participants (16). In ADHD, a wide range of deficits in cognitive domains have commonly been found, including attention, inhibitory control and working memory. P300 is widely used in the study of ADHD and cognitive deficits. A lot of researches focusing on adults and school-age children have showed that ADHD patients performed differently in P300 compared with the healthy, which well reflects their varies in cognitive functions (17–19). As a result, P300 has been consistently considered to be an indicator of cognitive processes and an objective criteria for cognitive function, as well as a promising endophenotype for ADHD (20–22). The diagnosis of ADHD in preschool children still remains controversial but P300 could provide uncontroversial evidence for the assessment of cognitive deficits. Therefore, it is particularly important to conduct studies on P300 in younger children, which may not only improve the current situation in ADHD assessment, but also have a chance to advance the time of clinical intervention, thereby improving the prognosis of the child.
The present study was conducted to investigate whether there are differences in cognitive function between preschool children with ADHD and healthy preschoolers aged 4–6 years, by analyzing and comparing the characteristics of their P300 waves, with the aim of exploring new approaches for the study of cognitive function in preschool children with ADHD.
2 Methods
2.1 Subjects
The study was approved by the Ethics Committee of the Children's Hospital Affiliated to the Capital Institute of Pediatrics. As all the participants were minors, written informed consents were collected from their guardians in accordance with the Declaration of Helsinki.
We recruited a total of 93 preschool children aged 4–6 years, who attended junior to senior kindergarten classes, from Neurology Department, the ADHD-specialized Clinic and Health Care Department of the Children's Hospital Affiliated to the Capital Institute of Pediatrics from March 2021 to May 2024. All the controls were healthy children, recruited from Health Care Department. The diagnosis of ADHD was made by more than two doctors, at least one of whom was the chief physician. Of the children whose caretakes complained of hyperactivity and/or attention deficit, 20 participants were excluded for not meeting the diagnostic criteria for ADHD according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition(DSM-5) (2). As for the children, who were diagnosed with ADHD, the situation of each child was explained with the parents honestly and efforts were made to find out individualize treatment options including both pharmacological and non-pharmacological treatments. ADHD children were categorized into three groups (2 predominantly attention deficit, ADHD-I; 20 predominantly hyperactive/impulsive disorder, ADHD-HI; and 23 combined type, ADHD-C) based on DSM-5. Eventually, 73 subjects participated in the study (28 controls and 45 ADHD), and all the participants exhibited DQ (Developmental quotient) ≥70 based on the Neuropsychological Development Assessment Scale for Children Aged 0–6 years(version 2016), which is widely used in China to assess the developmental level of children aged 0–6 years. All children with ADHD were diagnosed for the first time and were not taking psychostimulant medications prior to evaluation. None of the participants suffered from other types psychiatric disorders (such as autism spectrum disorder, anxiety disorder, obsessive-compulsive disorder) or neurological system diseases (such as epilepsy, tic disorder, cerebral palsy). Severe head injuries were also excluded. All subjects had normal or corrected-to-normal hearing and vision.
2.2 Procedure
The entire experimental procedure was conducted in a sound-shielded and dimly lit room, without interference and lasted for 20–30 min. The body temperature of the participants was below 37 degrees Celsius. Children were instructed to sit quietly and not to make any other movements while the electrodes were attached. Before the trial started, the physician would explain the processes of the task and launched into a practice to ensure the participants could adequately understand and perform the task. During the experiment, children were seated in front of a 17 inch screen with the seat was approximately 50 cm from the center of the screen. A repeated trial would be conducted for the children with a low level of cooperation in the first trial (23 children had to conduct repeated trials, occupied 24.73%), and the results with a higher superposition rate were included in the analysis.
2.3 Stimuli and task
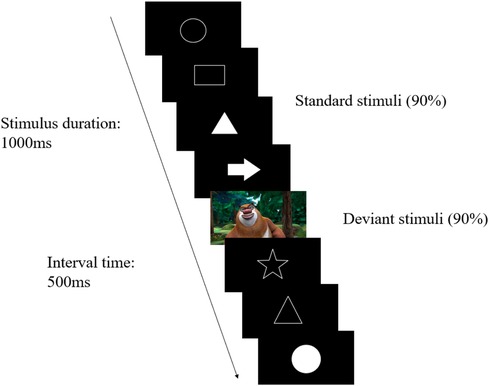
In our experiment, P300 was elicited by the visual Oddball paradigm (Figure 1), which was administered and displayed through the Innervate software. All the images appeared for 1,000 ms at the center of the screen on a black background, with a 500 ms interval. There were 40 images in total, of which 32 were different types of white patterns (standard stimuli) and 8 were colorful cartoon characters (deviant stimuli). The standard stimuli and deviant stimuli presented randomly with a ratio of 4:1. Participants were instructed to press the response button when the deviant-stimulus images occurred.
2.4 ERP recording and analysis
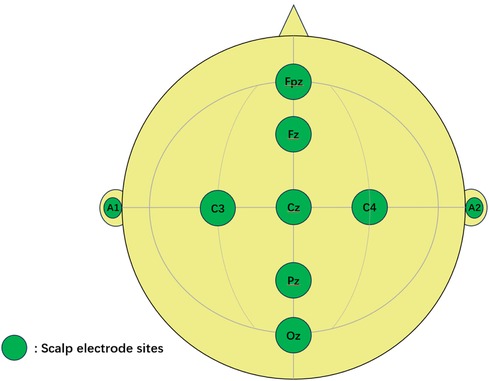
All measurements were performed in the Neurological Function Laboratory of the Children's Hospital Affiliated to the Capital Institute of Pediatrics. The original data of P300 were measured and recorded by a medical event-related potentiometer (WJ-1A) manufactured by Guangzhou Rainjet Medical Co., LTD. The electroencephalographic activity was recorded at the centerline (Fz, Cz, Pz and Oz) and bilateral central parietal area electrode sites (C3 and C4) according to the 10–20 system using a soft electrode cap suitable for preschool children. The ground electrode was positioned at the frontal midline electrode (Fpz), and all the electrodes were referenced to the right ear electrode(A2) (Figure 2) with a sampling frequency of 1,024 Hz. The impedance of all recording electrode sites was kept below 30Ω. The pre-filter range was set to 0.1–70 Hz and the post-filter was 3–70 Hz. The latency and amplitude of P300 were recorded in this study: the latency was defined as the interval time from the start of the task to the appearance of the spike, and the amplitude referred to the voltage level of the wave crest, expressed as the height of the spike. If two identical crests occurred in one P300 wave, the intersection of the ascending branch and descending branch was defined as the crest point, otherwise, the higher crest point prevailed. In the event of the latency/amplitude was out of the range of normal values, regarded as an outlier and not included in the calculation.
2.5 Statistical analysis
Statistical analysis was conducted through IBM SPSS version 26.0. (Armonk, NY: IBM Corp). Normality test was performed for all continuous variables. Data confirming to normal distribution were expressed as mean ± standard deviation (), and the skewed continuous variables were expressed as median with interquartile range [M (P25, P75)]. As in the case of demographic data and ERP data, independent t-test or Wilcoxon rank-sum test were performed for comparison between groups of measurement data. ANOVA was used to compare the measurement data of the three groups following normal distribution and homogeneity of variance. And categorical variables, such as gender, were compared using the chi-square test. All statistical tests were two-sided with a significance level of 0.05.
3 Results
3.1 Baseline characteristics
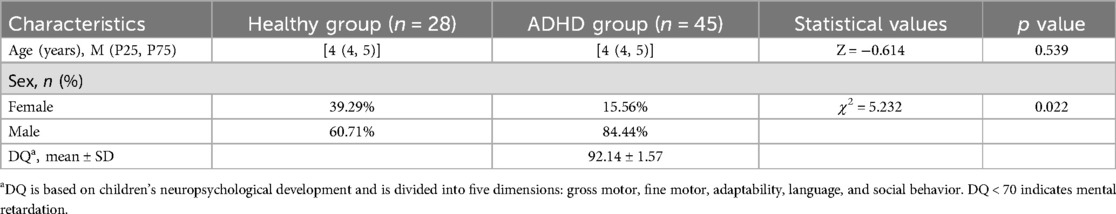
A total of 73 subjects were included in this study, and the baseline characteristics are shown in Table 1. The median age in both groups was [4 (4, 5)] years. There was no significant difference in ages between the two groups (p > 0.05). Both groups were dominated by boys (60.71% in healthy group and 84.44% in ADHD group), and compared with the healthy group, boys occurred more in the ADHD group (p < 0.05). The DQ scores of children in the ADHD group were (92.14 ± 1.57), which is in the normal range. In addition, there were no significant differences in the age, gender, and DQ scores among the different types of ADHD.
3.2 ERP results
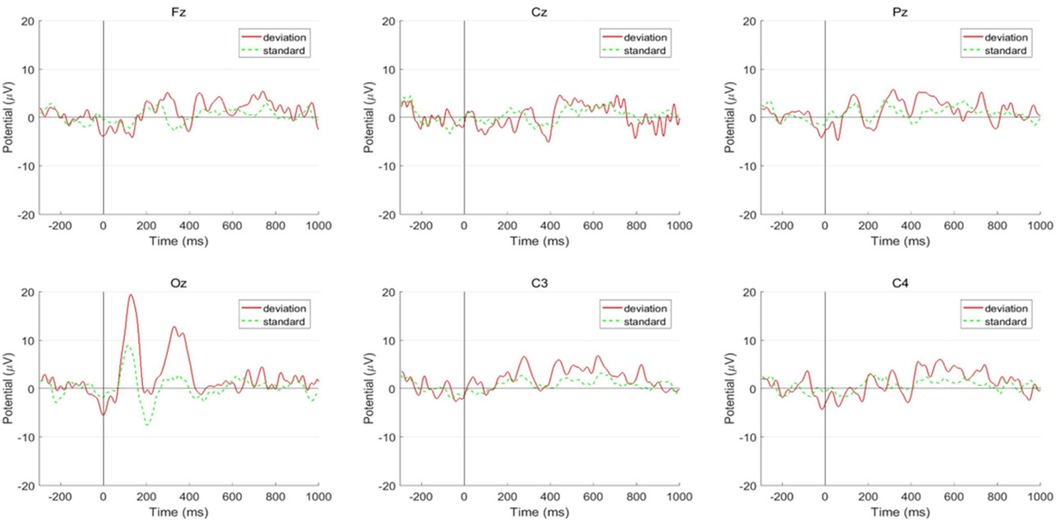
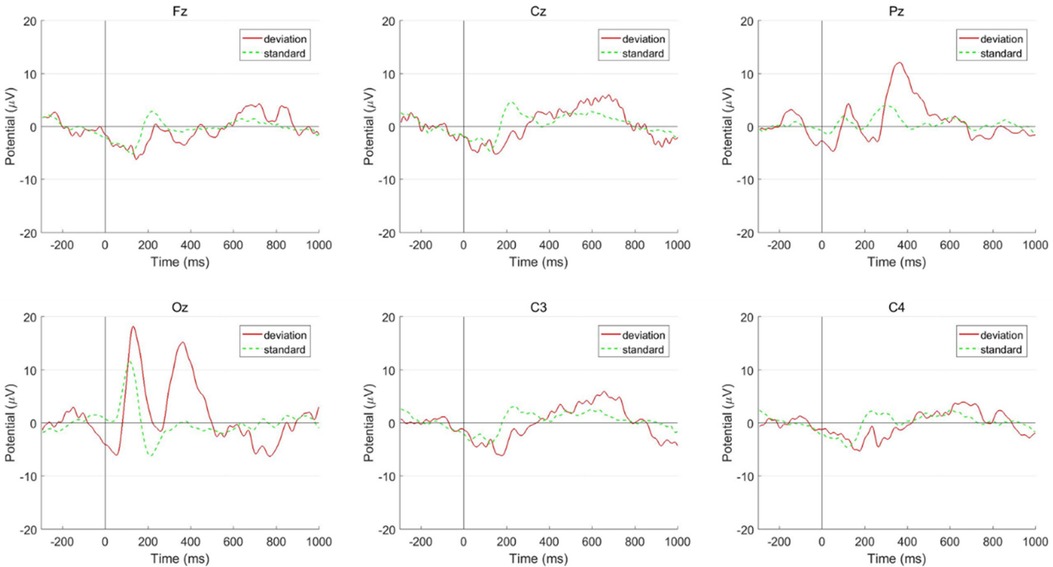
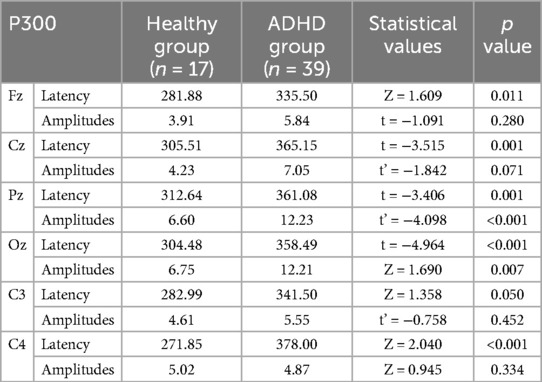
The latency of P300 at all the recording electrodes (Fz, Cz, Pz, Oz, C3, C4) in the ADHD group was significantly longer than it in the healthy children group (p < 0.05) (Table 2). The wave amplitudes of children with ADHD were significantly higher than in healthy children at Pz and Oz points, meanwhile, the amplitudes at other points (Fz, Cz, C3, C4) were not significantly different between the two groups (Figures 3, 4). In addition, there was no statistically significant difference in ERP results between the three types of ADHD in either latency or amplitude (Table 3), and for children with ADHD, their ERP outcomes did not differ by age or gender.
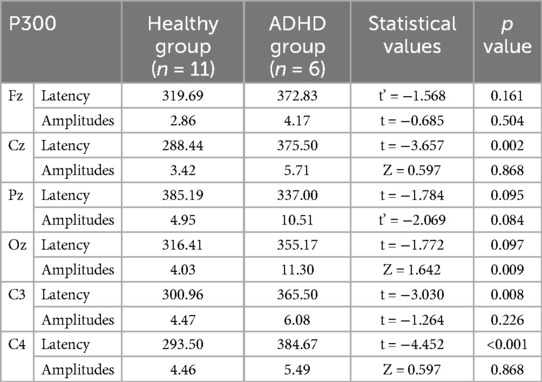
Since there was a significant difference in the ratio of boys to girls between the ADHD and healthy groups, we analyzed P300 results in the boys and girls separately (Tables 4, 5). In boys, there were significant differences in latency between two groups at Fz, Cz, Pz, Oz, C4 electrodes, and significant differences in amplitudes at both Pz and Oz electrodes (p < 0.05). For girls’ group, the latency at Cz, C3, C4 are significantly different between ADHD children and healthy children, and the amplitudes at Oz point differ between two groups (p < 0.05).
4 Discussion
In recent years, there have been many studies focusing on cognitive function in children with ADHD, however, the application of ERPs in the diagnosis of ADHD is seriously lagging behind. The brain dysfunction of children with ADHD often precedes the diagnosis, so it is essential to identify the clinical symptoms, cognitive functions, and related brain abnormalities in early childhood, which might be the most predictive period for later development of ADHD. Long latency potentials such as the P300 are of use in the study of cognitive and attentional functions, and abnormalities in latency or wave amplitude can indicate the alteration in cognitive processing function of the subject. To the best of our knowledge, the current research is the first to use event-related potential P300 in preschool children with ADHD. Using a cross-sectional study, our study compared and analyzed the characteristics of ERPs in preschool children with ADHD and healthy children to explore the value of P300 for assessment of ADHD in preschool children.
Our study found that preschool children with ADHD had longer latency for P300 at all the electrode sites than healthy controls, which was consistent with the results of other studies in school-age children (23–25). The latency of P300 is considered to reflect the time for the subjects to complete stimulus categorization, with good stability and consistency (26). Generators of the P300 is associated with attentional function-related structures, including the reticular formation, prefrontal cortex, temporal cortex, parietal cortex, limbic system, part of the thalamus and the projection systems between frontal lobes (25, 27). The prolonged latency in ADHD group can be explained by the slower processing of attentional cognitive functions in ADHD children than in normal children. This result indicates that preschoolers with ADHD take longer to process the same stimuli during active attention, which is clinically characterized by attention deficits and extended time required for voluntary attention. Meanwhile, we also found that children in the ADHD group had higher wave amplitudes in the central parietal lobe and central occipital lobe than healthy preschoolers, which contrasts with the findings in school-age children (28, 29). It is generally considered that the amplitude of ERPs reflects the intensity of cognitive resource utilization by the brain: the more resources invested, the higher amplitudes evoked, and there is a positive correlation between the two magnitudes (30, 31). In this study, the reason for the increased amplitude of waves in ADHD children may be that during voluntary-attention progress, more attentional resources were required to be allocated to accomplish the task. Considering the differences in the gender distribution between two groups, an attempt was made to correct for possible bias by statistical methods: we described and compared boys and girls in both groups separately. Almost the same results were found in boys, that is, children with ADHD showed the prolonged latency generally and the higher amplitude in the parietal and occipital lobes. Only the result of latency at C3 differed. Further studies with wider distribution of electrode sites and a larger sample size are required to confirm whether this discrepancy was caused by the lateralization effect. In the case of the girls’ group, the number of subjects was not sufficient enough, but the results still did not appear conflict apparently. We believe that, in future studies, balancing the baseline characteristics properly would make the finding more convincing. Many related studies have obtained prolonged latencies of P300 in ADHD patients, which can be well interpreted as more time required for the brain to process same tasks for children with ADHD. However, studies in the amplitude have yielded different results, including the present research. This may be related to the development of children's own cognitive ability, in addition, the difficulty of each paradigm is different and the “ceiling effect” cannot be ignored. Furthermore, anxiety, obsessive-compulsive, and some other emotional or psychiatric disorders should also be considered. Consequently, how to set up a suitable paradigm for different subjects, or even making individualized programs with adaptive difficulty individually, may be one of the most important directions for future researches. Setting up a queue of regular visits for the appropriate groups is also likely to offer more information.
The results of this study could also provide some information for the clinic: these differences found in younger ADHD patients may suggest that earlier assessment and intervention, such as early cognitive training or medication, may be able to improve the child's condition and prognosis. In conclusion, the results of this study suggest that cognitive impairment has already existed in preschool children with ADHD, which would persist throughout the school age. And the changes in P300 component may provide objective indicators for clinical assessment in preschool children with ADHD.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee, Capital Institute of Pediatrics. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MT: Writing – review & editing, Writing – original draft, Methodology, Investigation, Data curation. JS: Writing – original draft, Resources, Methodology, Investigation, Data curation. SL: Writing – original draft, Validation, Methodology, Investigation, Formal Analysis, Data curation. YZ: Writing – original draft, Validation, Methodology, Investigation, Data curation, Conceptualization. YR: Writing – original draft, Validation, Methodology, Investigation, Formal Analysis, Data curation, Conceptualization. ZL: Writing – original draft, Methodology, Investigation, Formal Analysis, Data curation. XiaW: Writing – original draft, Resources, Methodology, Investigation, Formal Analysis, Data curation. WY: Writing – review & editing, Visualization, Software, Project administration, Methodology, Investigation, Formal Analysis, Data curation. GL: Writing – original draft, Validation, Project administration, Methodology, Investigation, Data curation, Conceptualization. XinW: Writing – review & editing, Supervision, Resources, Methodology, Data curation. WZ: Writing – review & editing, Data curation, Visualization, Software. JZ: Writing – review & editing, Validation, Supervision, Project administration, Methodology, Formal Analysis. JY: Funding acquisition, Formal Analysis, Data curation, Conceptualization, Writing – review & editing, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (No. 82271579); the Research Foundation of Capital Institute of Pediatrics (LCPY-2021-26); the Research Foundation of Capital Institute of Pediatrics (Commercial Research Funds 202344).
Conflict of interest
WZ was employed by Guangzhou Rainjet Medical Equipment Co.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Younger DS. Epidemiology of childhood mental illness: a review of U.S. surveillance data and the literature. World J Neurosci. (2017) 07(01):48–54. doi: 10.4236/wjns.2017.71005
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™. 5th ed Arlington, VA: American Psychiatric Publishing, Inc (2013). p. 68.
3. Miao S, Han J, Gu Y, Wang X, Song W, Li D, et al. Reduced prefrontal cortex activation in children with attention-deficit/hyperactivity disorder during GO/No-Go task: a functional near-infrared spectroscopy study. Front Neurosci. (2017) 11:367. doi: 10.3389/fnins.2017.00367
4. Souissi S, Chamari K, Bellaj T. Assessment of executive functions in school-aged children: a narrative review. Front Psychol. (2022) 13:991699. doi: 10.3389/fpsyg.2022.991699
5. Rowland AS, Skipper BJ, Umbach DM, Rabiner DL, Campbell RA, Naftel AJ, et al. The prevalence of ADHD in a population-based sample. J Atten Disord. (2015) 19(9):741–54. doi: 10.1177/1087054713513799
6. Canals Sans J, Morales Hidalgo P, Roige Castellvi J, Voltas Moreso N, Hernandez Martinez C. Prevalence and epidemiological characteristics of ADHD in pre-school and school age children in the province of Tarragona, Spain. J Atten Disord. (2021) 25(13):1818–33. doi: 10.1177/1087054720938866
7. Wichstrøm L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E, Sveen TH. Prevalence of psychiatric disorders in preschoolers. J Child Psychol Psychiatry. (2012) 53(6):695–705. doi: 10.1111/j.1469-7610.2011.02514.x
8. Law EC, Sideridis GD, Prock LA, Sheridan MA. Attention-deficit/hyperactivity disorder in young children: predictors of diagnostic stability. Pediatrics. (2014) 133(4):659–67. doi: 10.1542/peds.2013-3433
9. Lahey BB, Lee SS, Sibley MH, Applegate B, Molina BSG, Pelham WE. Predictors of adolescent outcomes among 4–6-year-old children with attention-deficit/hyperactivity disorder. J Abnorm Psychol. (2016) 125(2):168–81. doi: 10.1037/abn0000086
10. Skogan AH, Zeiner P, Egeland J, Urnes AG, Reichborn-Kjennerud T, Aase H. Parent ratings of executive function in young preschool children with symptoms of attention-deficit/-hyperactivity disorder. Behav Brain Funct. (2015) 11:16. doi: 10.1186/s12993-015-0060-1
11. Schoemaker K, Bunte T, Wiebe SA, Espy KA, Dekovic M, Matthys W. Executive function deficits in preschool children with ADHD and DBD. J Child Psychol Psychiatry. (2012) 53(2):111–9. doi: 10.1111/j.1469-7610.2011.02468.x
12. Shuai L, Wang Y, Li W, Wilson A, Wang S, Chen R, et al. Executive function training for preschool children with ADHD: a randomized controlled trial. J Atten Disord. (2021) 25(14):2037–47. doi: 10.1177/1087054720956723
13. Zhu Y, Liu S, Zhang F, Ren Y, Zhang T, Sun J, et al. Response inhibition in children with different subtypes/presentations of attention deficit hyperactivity disorder: a near-infrared spectroscopy study. Front Neurosci. (2023) 17:1119289. doi: 10.3389/fnins.2023.1119289
14. Yakubov B, Das S, Zomorrodi R, Blumberger DM, Enticott PG, Kirkovski M, et al. Cross-frequency coupling in psychiatric disorders: a systematic review. Neurosci Biobehav Rev. (2022) 138:104690. doi: 10.1016/j.neubiorev.2022.104690
15. Cao J, Wang S, Ren Y, Zhang Y, Cai J, Tu W, Shen H, et al. Interference control in 6–11 year-old children with and without ADHD: behavioral and ERP study. Int J Dev Neurosci. (2013) 31(5):342–9. doi: 10.1016/j.ijdevneu.2013.04.005
16. Chen C, Yang H, Du Y, Zhai G, Xiong H, Yao D, et al. Altered functional connectivity in children with ADHD revealed by scalp EEG: an ERP study. Neural Plast. (2021) 2021:6615384. doi: 10.1155/2021/6615384
17. Karakaş S, Erzengin OU, Başar E. A new strategy involving multiple cognitive paradigms demonstrates that ERP components are determined by the superposition of oscillatory responses. Clin Neurophysiol. (2000) 111(10):1719–32. doi: 10.1016/S1388-2457(00)00418-1
18. Gamma A, Kara O. Event-Related potentials for diagnosing children and adults with ADHD. J Atten Disord. (2020) 24(11):1581–7. doi: 10.1177/1087054716631821
19. Spronk M, Jonkman LM, Kemner C. Response inhibition and attention processing in 5- to 7-year-old children with and without symptoms of ADHD: an ERP study. Clin Neurophysiol. (2008) 119(12):2738–52. doi: 10.1016/j.clinph.2008.09.010
20. Lenartowicz A, Loo SK. Use of EEG to diagnose ADHD. Curr Psychiatry Rep. (2014) 16(11):498. doi: 10.1007/s11920-014-0498-0
21. Santopetro NJ, Barch D, Luby JL, Hennefield L, Gilbert KE, Whalen DJ, et al. Deficits in doors P300 amplitude during adolescence associated with preschool-onset depression. Psychophysiology. (2023) 60(10):e14331. doi: 10.1111/psyp.14331
22. Hajcak G, Foti D. Significance?… Significance! Empirical, methodological, and theoretical connections between the late positive potential and P300 as neural responses to stimulus significance: an integrative review. Psychophysiology. (2020) 57(7):e13570. doi: 10.1111/psyp.13570
23. Buchmann J, Gierow W, Reis O, Haessler F. Intelligence moderates impulsivity and attention in ADHD children: an ERP study using a go/nogo paradigm. World J Biol Psychiatry. (2011) 12(sup1):35–9. doi: 10.3109/15622975.2011.600354
24. Jahanshahloo HR, Shamsi M, Ghasemi E, Kouhi A. Automated and ERP-based diagnosis of attention-deficit hyperactivity disorder in children. J Med Signals Sens. (2017) 7(1):26–32. doi: 10.4103/2228-7477.199152
25. Yamamuro K, Ota T, Iida J, Nakanishi Y, Matsuura H, Uratani M, et al. Event-related potentials reflect the efficacy of pharmaceutical treatments in children and adolescents with attention deficit/hyperactivity disorder. Psychiatry Res. (2016) 242:288–94. doi: 10.1016/j.psychres.2016.05.061
26. Yoon HH, Iacono WG, Malone SM, Bernat EM, McGue M. The effects of childhood disruptive disorder comorbidity on P3 event-related brain potentials in preadolescents with ADHD. Biol Psychol. (2008) 79(3):329–36. doi: 10.1016/j.biopsycho.2008.08.001
27. Mudrik L, Deouell LY. Neuroscientific evidence for processing without awareness. Annu Rev Neurosci. (2022) 45:403–23. doi: 10.1146/annurev-neuro-110920-033151
28. Janssen TWP, Geladé K, van Mourik R, Maras A, Oosterlaan J. An ERP source imaging study of the oddball task in children with attention deficit/hyperactivity disorder. Clin Neurophysiol. (2016) 127(2):1351–7. doi: 10.1016/j.clinph.2015.10.051
29. Zarka D, Cebolla AM, Cevallos C, Palmero-Soler E, Dan B, Cheron G. Caudate and cerebellar involvement in altered P2 and P3 components of GO/NoGO evoked potentials in children with attention-deficit/hyperactivity disorder. Eur J Neurosci. (2021) 53(10):3447–62. doi: 10.1111/ejn.15198
30. Barry RJ, Clarke AR, McCarthy R, Selikowitz M, Brown CR, Heaven PC. Event-related potentials in adults with attention-deficit/hyperactivity disorder: an investigation using an inter-modal auditory/visual oddball task. Int J Psychophysiol. (2009) 71(2):124–31. doi: 10.1016/j.ijpsycho.2008.09.009
31. Horowitz-Kraus T, Fotang J, Niv L, Apter A, Hutton J, Farah R. Executive functions abilities in preschool-age children are negatively related to parental EF, screen-time and positively related to home literacy environment: an EEG study. Child Neuropsychol. (2024) 30(5):738–59. doi: 10.1080/09297049.2023.2272339
Keywords: attention deficit hyperactivity disorder, event related potential, P300, children, ERP, ADHD
Citation: Tao M, Sun J, Liu S, Zhu Y, Ren Y, Liu Z, Wang X, Yang W, Li G, Wang X, Zheng W, Zhang J and Yang J (2024) An event-related potential study of P300 in preschool children with attention deficit hyperactivity disorder. Front. Pediatr. 12:1461921. doi: 10.3389/fped.2024.1461921
Received: 9 July 2024; Accepted: 29 October 2024;
Published: 13 November 2024.
Edited by:
R. Grant Steen, Louisiana State University, United StatesReviewed by:
Samson Nivins, Karolinska Institutet (KI), SwedenAntonio Narzisi, Stella Maris Foundation (IRCCS), Italy
Copyright: © 2024 Tao, Sun, Liu, Zhu, Ren, Liu, Wang, Yang, Li, Wang, Zheng, Zhang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianzhao Zhang, emp6MTg1MTgzODc2MThAdmlwLjE2My5jb20=; Jian Yang, eWFuZ2ppYW4xMzA2QHNpbmEuY29t
†These authors have contributed equally to this work
 Mengjiao Tao
Mengjiao Tao Jing Sun1,†
Jing Sun1,† Yike Zhu
Yike Zhu Ziqi Liu
Ziqi Liu Jianzhao Zhang
Jianzhao Zhang