- Department of Pediatric Surgery, University Medicine Greifswald, Greifswald, Germany
Acute glans ischemia is a severe complication that can occur after penile surgery, such as circumcision, hypospadias repair, or disassembly of the corpora in epispadias. This rare condition is described in the current literature, especially after circumcision, although it is the less invasive procedure among those previously mentioned. We present a case of 7-month-old boy who developed glans ischemia after correction of megaprepuce. The condition was treated by intravenous unfractionated heparin. In our case, the complication of ischemia was complete dehiscence of the suture line at the coronal sulcus. Glans penis recovered completely and secondary intention wound healing occurred within 4 weeks. We reviewed the literature over the past 43 years (1981–2023) to describe the current options of surveillance, treatment, and outcome of glans ischemia after penile surgery in boys.
Introduction
Several techniques have been described for the correction. At our institution, the surgical technique is performed according to Hirsch et al. or Shalaby and Cascio, with few modifications, with complete degloving of the penile shaft combined with a VY-plasty at the penoscrotal junction (1, 2). The inner prepuce is resected subtotally and not used for penile shaft coverage. Although it is an invasive operation, glans ischemia was not previously described in this procedure. The current literature discusses that ischemic complications in penile surgery may result from local anesthetics with or without vasoconstrictor agents such as epinephrine, vasospasm induced by dorsal penile nerve block (DNPB) and their techniques (e.g., ringblock vs. bilateral injections), microtrauma caused by cautery, circular bandages, increased local pressure due to edema and local hematoma, or the use of tourniquets to achieve blood-free surgical fields (3–15). All these conditions temporarily reduce blood flow and can lead to transient ischemia or, if long-lasting, to gangrene.
In the present case, renewing of dressing at day 3 postoperatively potentially led to glans ischemia. Unfractionated heparin (UFH) was used for treatment according to the current reviewed literature.
Case report
A 7-month-old boy (at 5 months of adjusted age) was referred to our department for the correction of megaprepuce. He was born preterm at 28 weeks and 4 days of gestation with a birth weight of 980 g. Urinary tract infections (UTIs) occurred due to urinary retention under the foreskin and his parents expressed the foreskin from time to time to empty residual urine completely. The child exhibited postponement of micturition, which raised the parents’ concerns due to a history of infections and the inconspicuous appearance of the penis. Surgery was performed to prevent further UTIs and to treat voiding postponements. A preoperative ultrasound examination revealed a normal upper and lower urinary tract and intraoperative cystoscopy showed no signs of urethral valves. The ureteric orifices were cone-shaped and located at the trigone.
The correction of megaprepuce was performed under general anesthesia and caudal epidural block with 2% ropivacaine. First, a small ventral slit of the foreskin was made, extended only to the point where the foreskin could be fully retracted. After inspecting the glans, a circumferential incision was made parallel to the coronal sulcus, leaving a 4 mm mucosal collar intact. The penile skin was incised ventrally along the penile raphe, degloved to the penopubic level dorsally and to the level of penoscrotal junction ventrally, leading to penile straightening. The inner prepuce was partially resected. The skin was mobilized by VY-plasty at the ventral base of the penis to gain length of the ventral skin to cover the penile shaft at this site and to remodel the penoscrotal junction. No temporary tourniquet was applied. At the end of the surgical procedure, a transurethral catheter and loose padding bandage were placed. On the third postoperative day, the bandage was removed, revealing well-healing tissue with smooth, rosy skin. The boy’s discharge was scheduled for the following day. However, as the boy passed soft to fluid stools several times in the afternoon, the pediatric surgeon on the night shift applied a circular bandage. The patient developed a subfebrile temperature of 38.8°C approximately 3 h after the bandage was renewed. The boy experienced interrupted and fitful sleep. The next day, the circular dressing was removed, revealing a black-colored glans and inner preputial rim with a dry surface.
Within 2 h of the bandage being removed, no visual improvement of the glans was observed.
The patient’s body temperature returned to normal 4 h after the dressing was removed. A urine probe showed no signs of UTI. We removed the transurethral catheter to avoid any pressure on the corpus spongiosum whose distal end is the glans penis. Further treatment opportunities were discussed with pediatricians.
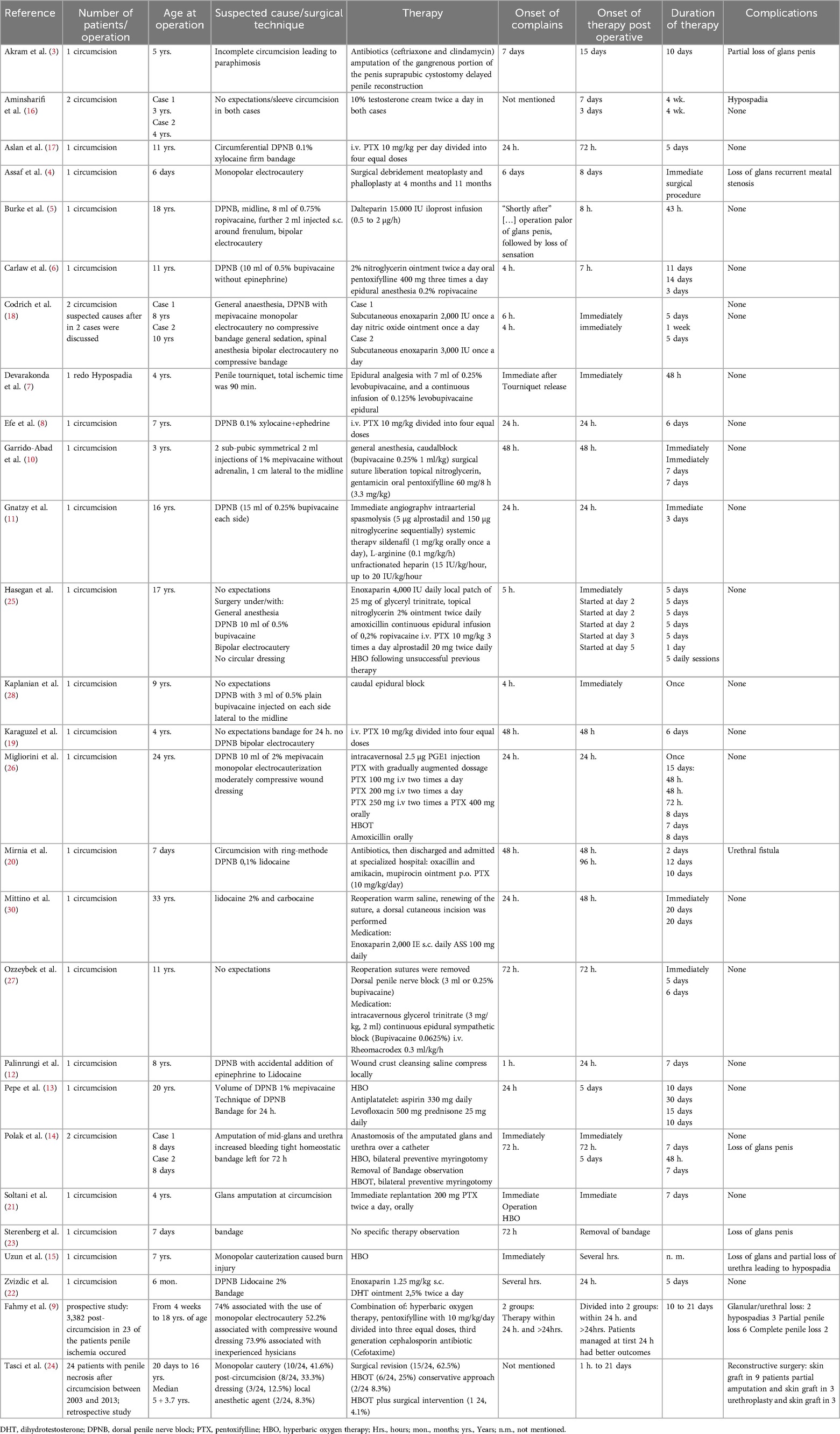
Even if no uniform treatment guidelines exist, the literature reports different options for medical treatment in children (Table 1), such as therapy with pentoxifylline (PTX) or heparin (5, 6, 8, 17–22).
In contrast to PTX, UFH is a widely used and safe therapy for many conditions in infants. In contrast to subcutaneous low-molecular-weight heparin (LMWH), UFH is well adjustable. We therefore decided to begin a continuous intravenous infusion of UFH with 10 IE/kg/h as low-dose therapy. Anticoagulant therapy was adjusted based on partial thromboplastin time (PTT), with values set above the baseline normal range. The first PTT control was made 6 h after the low-dose heparin infusion was started.
Doppler ultrasound was performed before heparin therapy and 24 h after. In each examination, neither abnormal flow pattern in the dorsal penile artery nor thrombosis of the corpora cavernosa was seen. Approximately 4 h after heparin therapy was started, reddish spots appeared on the dark-colored glans. Within 24 h, the glans became responsive, with the initial livid discoloration that gradually becoming increasingly rosy. No modifications or additions to previous therapy were implemented due to the continuous visible improvement. The glans had an almost pink appearance in all areas on day 4 of the continuous intravenous heparin administration. At this point, the therapy was ended, and the boy remained under surveillance as an inpatient for another 24 h. The patient was discharged without any medication.
In our case, as a complication of ischemic conditions, complete dehiscence of the suture line at the coronal sulcus occurred; however, the wound healed completely secondarily within another 4 weeks. Despite this complication, there were no signs of gangrene, such as blistering or shedding, at the surface of the glans. In the patient’s outpatient visits at 4 weeks and 6 months postoperatively, no further deterioration was noticed. We observed good cosmesis with a completely recovered glans penis and no signs of meatal stenosis, hypospadias, or concealed penis.
Methods and review of the literature
According to the Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA), a systematic search of English-language full-text articles was made on the PubMed Database. The keywords were “glans ischemia” (73 results), “glans necrosis” (208 results), and “glans ischemia after circumcision” (26 results). Duplicates and articles that were not concerned with glans ischemia after penile surgery in children or adolescents were removed. We then checked all the reference lists of the included articles. In total, 27 articles were analyzed (25 case reports, 1 retrospective study, and 1 prospective study), due to surgical procedure, onset of perfusion disturbances, patients’ age, therapeutic measures and duration, monitoring of therapy, and outcome (Table 1).
Results
No guidelines exist for the treatment of glans ischemia. As shown in Table 1, the reviewed literature reports on the duration of therapy and outcome as well as different therapeutic strategies. Such strategies are systemic or local vasodilatation, local spasmolysis, anticoagulation, or rheological changes. Hyperbaric oxygen therapy (HBOT) for better oxygen administration is also described in detail. Treatment with heparin (LMWH and UFH) or PTX for systemic vasodilatation, anticoagulation, and rheological changes was described in nine reviewed articles (5, 6, 8, 17–22).
The authors reported surgical procedures alone in five cases or only surveillance in one case (3, 4, 12, 14, 15, 23).
HBOT alone was described in detail and within the retrospective study of 24 cases from Tasci et al. (24, 25). Antibiotics were administered in seven of the reported cases (3, 9, 10, 13, 20, 25, 26). In three cases, epidural anesthesia was used for sympathicolysis to treat glans ischemia (7, 27, 28).
Neither a method for surveillance of therapy nor for the initial assessment of glans ischemia was described in the reviewed literature. Initial and follow-up grayscale, color Doppler ultrasound, and D-dimer levels were reported (8, 11, 19, 29). However, only Efe et al. described pathologic findings in grayscale ultrasound, including thickening of the epithelial layer with normal penile and glanular blood flow (8, 30). In contrast to those findings, Barnes et al. revealed a lack of vascularity in the glans on color Doppler imaging and hypoechoic glans tissues in high frequency grayscale ultrasound in a 2-week-old male infant who developed glans ischemia after circumcision. In the same study, an ultrasound scan in a patient of the same age showed no such pathologies after an uneventful circumcision (29).
Gnatzy et al. reported a case of glans ischemia in a 16-year-old boy treated by angiography with local spasmolysis. However, neither vasospasm nor blood flow abnormities were found on angiography (11). No evidence was found correlating glans ischemia with detectable changes in blood flow abnormalities on color Doppler ultrasound or angiography.
Efe et al. also describe elevated D-dimer levels of 2.57 mg/L in a 7-year-old boy with severe ischemia of the glans penis (8), whereas Gnatzy et al. and Karaguzel et al. found normal D-Dimer levels in their patients (11, 19).
There are inconsistent findings in the assessment of glans ischemia and its probable causes. Post-circumcision findings suggest that ischemia may result from specific surgical factors, such as local anesthesia in DPNB, the volume used, with or without vasoconstrictive agents, tight bandages, hemorrhage, a tight suture line, or monopolar cauterization, which may cause thermal injury or vasospasm due to the electric current passing through the small penile diameter. However, a review of the current literature does not provide clear evidence correlating glans ischemia with specific steps in the surgical procedure. For example, Codrich et al. compared two cases from their institution where glans ischemia occurred after circumcision in boys aged 8 and 10 years (18). One operation was performed under general anesthesia with a dorsal penile nerve block, using monopolar cauterization, while the other was under general anesthesia with an additional caudal block and bipolar cauterization. Both surgeries involved the same suturing technique, with no dressing applied. In both cases, transient glans ischemia occurred.
However, within the reviewed literature, severe complications including partial penile loss are consistently reported, especially after a delay in the beginning of treatment (3, 4, 9, 14–16, 20, 23, 24).
Conclusion
At our institution, only bipolar cautery is used during penile operations such as hypospadias surgery, correction of buried penis, and megaprepuce. Surgery is performed under general anesthesia with an additional caudal block with 0.2% ropivacaine or dorsal penile nerve block. Dressings are placed with care only in the operating room using the sandwich technique or as padding bandages. It is mandatory that the glans is visible despite the bandage for postoperative evaluation. After the dressing is removed, a new bandage should be avoided. First, children get scared bandages are changed. Furthermore, there is no proven benefit of changing the dressing. In the present case, placing a circular dressing potentially led to glans ischemia. After treatment with intravenous UFH, the glans recovered completely. The question of whether reperfusion would occur spontaneously without intervention remains uncertain. In our case, early therapy was initiated based on findings in the literature, which highlight that complications are common after treatment is delayed.
Long term follow-up after transient glans ischemia is necessary to monitor for late complications, such as meatal stenosis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
SK: Conceptualization, Writing – original draft, Writing – review & editing, Supervision, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization. FM: Writing – review & editing. VS: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hirsch K, Schwaiger B, Kraske S, Wullich B. Megaprepuce: presentation of a modified surgical technique with excellent cosmetic and functional results. J Jpurol. (2019) 15:4. doi: 10.1016/2019.05.018
2. Shalaby M, Cascio S. Megaprepuce: a systematic review of a rare condition with a controversial surgical management. Pediatr Surg Int. (2021) 37:6. doi: 10.1007/s00383-021-04883-5
3. Akram A, Ansari Z, Akram S. Delayed gangrene and amputation of penile glans after a religious circumcision in male child—a case report. Trop Doct. (2021) 51:4. doi: 10.1177/0049475521998834
4. Assaf R, Albahhah T, Ayoub K, Al-Janzir Z, Tarzi M, Rahmeh AR, et al. Penile reconstruction using scrotal flap after usage of monopolar electrocautery in a 2-month-old Syrian child: a case report. J Surg Case Rep. (2019) 2019:12. doi: 10.1093/jscr/rjz351
5. Burke D, Joypaul V, Thomson MF. Circumcision supplemented by dorsal penile nerve block with 0.75% ropivacaine: a complication. Reg Anesth Pain Med. (2000) 25:4. doi: 10.1053/rapm.2000.7594
6. Carlaw K, Chia D, Allaway M, Harvey J. Acute ischaemia of the glans penis post-circumcision managed with pentoxifylline, topical nitroglycerin and epidural. BMJ Case Rep. (2023) 16:1. doi: 10.1136/bcr-2022-249049
7. Devarakonda K, Aghavendra TR. A case of ischemia of the glans penis. Paediatr Anaesth. (2010) 20:574–83. doi: 10.1111/j.1460-9592.2010.03312.x
8. Efe E, Resim S, Bulut BB, Eren M, Garipardic M, Ozkan F, et al. Successful treatment with enoxaparin of glans ischemia due to local anesthesia after circumcision. Pediatrics. (2013) 131:2. doi: 10.1542/peds.2012-1400
9. Fahmy MAB, Sabra TA, Abdelmohsen SM. Management of penile postcircumcision ischemia by pentoxifylline infusion and hyperbaric oxygen therapy. BMC Urol. (2023) 23:117. doi: 10.1186/s12894-023-01284-9
10. Garrido-Abad P, Suárez-Fonseca C. Glans ischemia after circumcision and dorsal penile nerve block: case report and review of the literature. Urol Ann. (2015) 7:4. doi: 10.4103/0974-7796.164862
11. Gnatzy R, Fuchs J, Siekmeyer M, Beeskow AB, Gosemann JH, Lacher M. Glans ischemia after circumcision in a 16-year-old boy: full recovery after angiography with local spasmolysis, systemic vasodilatation, and anticoagulation. European J Pediatr Surg Rep. (2018) 13:e66–9. doi: 10.1055/s-0038-1667330
12. Palinrungi MA, Palinrungi ALR, Christeven R, Faruk M. Penile ischemia as a complication of epinephrine use in penile nerve block: truth or myth? Res Rep Urol. (2021) 2021:13. doi: 10.2147/RRU.S308428
13. Pepe P, Pietropaolo F, Candiano G, Pennisi M. Ischemia of the glans penis following circumcision: case report and revision of the literature. Arch Ital Urol Androl. (2015) 31:87. doi: 10.4081/aiua.2015.1.93
14. Polak N, Fishelev G, Lang E, Wang Z, Neheman A, Ben Haim Y, et al. Hyperbaric oxygen as salvage therapy for neonates suffering from critical ischemia of the glans penis after circumcision. Urology. (2021) 2021:149. doi: 10.1016/j.urology.2020.09.006
15. Uzun G, Ozdemir Y, Eroglu M, Mutluoglu M. Electrocautery induced gangrene of the glans penis in a child following circumcision. BMJ Case Rep. (2012) 2012:1–2 doi: 10.1136/bcr-2012-007096
16. Aminsharifi A, Afsar F, Tourchi A. Delayed glans necrosis after circumcision: role of testosterone in salvaging glans. Indian J Pediatr. (2013) 80:9. doi: 10.1007/s12098-012-0820-y
17. Aslan A, Karagüzel G, Melikoglu M. Severe ischemia of the glans penis following circumcision: a successful treatment via pentoxifylline. Int J Urol. (2005) 12:7. doi: 10.1111/j.1442-2042.2005.01129.x
18. Codrich D, Boscarelli A, Cerrina A, Scarpa MG, Iaquinto M, Olenik D, et al. Glans ischemia after circumcision in children: two case reports. World J Clin Pediatr. (2012) 10:4. doi: 10.5409/wjcp.v10.i4.79
19. Karaguzel E, Tok DS, Kazaz IO, Gur M, Colak F, Kutlu O, et al. Postcircumcisional ischemia of the glans penis treated with pentoxifylline. Case Rep Urol. (2013) 2013:1–3. doi: 10.1155/2013/278523
20. Mirnia K, Safari A, Saeedi M, Sangsari R. Glans ischemia treatment with pentoxifylline following circumcision in a neonate. J Compr Pediatr. (2021) 12:2. doi: 10.5812/compreped.99559
21. Soltani S, Mottaghi M, Jafarpisheh A, Tavakkoli M. Penile glans amputation following circumcision: a case report of a rare complication. Case Rep Urol. (2020) 2020:1–3. doi: 10.1155/2020/5806987
22. Zvizdic Z, Anic D, Popovic N, Vranic S. Acute glans ischemia after circumcision successfully treated with low-molecular-weight heparin and topical dihydrotestosterone: a case report. Medicine (Baltimore). (2020) 99:29. doi: 10.1097/MD
23. Sterenberg N, Golan J, Ben-Hur N. Necrosis of the glans penis following neonatal circumcision. Plast Reconstr Surg. (1981) 68:237–9. doi: 10.1097/00006534-198108000-00022
24. Tasci AI, Danacioglu YO, Arikan Y, Colakoglu Y, Yapar B, Buyuk Y. Management of post-circumcision necrosis of the penis: the medicolegal aspect. Pediatr Surg Int. (2020) 36:4. doi: 10.1007/s00383-020-04630-2
25. Hașegan A, Mihai I, Bratu D, Bacilă C, Roman MD, Mohor CI, et al. Severe acute ischemia of glans penis after achieving treatment with only hyperbaric oxygen therapy: a rare case report and systematic literature review. J Pers Med. (2023) 12:13. doi: 10.3390/jpm13091370
26. Migliorini F, Bianconi F, Bizzotto L, Porcaro AB, Artibani W. Acute ischemia of the glans penis after circumcision treated with hyperbaric therapy and pentoxifylline: case report and revision of the literature. Urol Int. (2018) 100:3. doi: 10.1159/000444399
27. Ozzeybek D, Koca U, Elar Z, Olguner M, Hakgüder G. Glycerol trinitrate plus epidural sympathetic block in the ischemia of glans penis. Anesth Analg. (1999) 89(4):1066. doi: 10.1213/00000539-199910000-00057
28. Kaplanian S, Chambers NA, Forsyth I. Caudal anaesthesia as a treatment for penile ischaemia following circumcision. Anaesthesia. (2007) 62:7. doi: 10.1111/j.1365-2044.2007.05060.x
29. Barnes S, Ben Chaim J, Kessler A. Postcircumcision necrosis of the Glans penis: gray-scale and color Doppler sonographic findings. J Clin Ultrasound. (2007) 35:2. doi: 10.1002/jcu.20271
Keywords: glans ischemia, megaprepuce, dorsal penile nerve block, electrocautery, dressings, pentoxifylline, heparin
Citation: Kraske S, Müller F and Schellerer V (2025) Glans ischemia in a 7-month-old boy who underwent correction of megaprepuce: case report and review of the literature. Front. Pediatr. 12:1460717. doi: 10.3389/fped.2024.1460717
Received: 6 July 2024; Accepted: 26 December 2024;
Published: 27 February 2025.
Edited by:
Lisandro Ariel Piaggio, Universidad Nacional del Sur, ArgentinaReviewed by:
Marleen van den Heijkant, Groene Hart Ziekenhuis, NetherlandsSantiago Vallasciani, Sidra Medicine, Qatar
Juan Ignacio Bortagaray, Royal Children’s Hospital, Australia
Copyright: © 2025 Kraske, Müller and Schellerer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanne Kraske, c3VzYW5uZS5rcmFza2VAbWVkLnVuaS1ncmVpZnN3YWxkLmRl
 Susanne Kraske
Susanne Kraske Fanny Müller
Fanny Müller Vera Schellerer
Vera Schellerer