- 1Division of Rheumatology, The Hospital for Sick Children, Toronto, ON, Canada
- 2Child Health Evaluative Sciences, SickKids Research Institute, Toronto, ON, Canada
- 3Division of Rheumatology, Allergy & Immunology, Department of Pediatrics, University of Minneapolis, Minneapolis, MN, United States
- 4Department of Rheumatology, Nationwide Children’s Hospital, Columbus, OH, United States
- 5Division of Pediatric Rheumatology, Department of Pediatrics, Stanford Medicine Children’s Health, Palo Alto, CA, United States
- 6Stanford School of Medicine, Stanford University, Palo Alto, CA, United States
- 7Division of Rheumatology, Department of Pediatrics, Children’s Mercy Kansas City, Kansas City, Missouri, United States
- 8School of Medicine, University of Missouri-Kansas City, Kansas City, MO, United States
- 9University of Minnesota Medical School, University of Minnesota, Minneapolis, MN, United States
- 10Department of Pediatric Rheumatology, M Health Fairview Masonic Children’s Hospital, Minneapolis, MN, United States
- 11Department of Pediatrics, Atrium Health Levine Children’s, Charlotte, NC, United States
- 12Wake Forest School of Medicine, Wake Forest University, Charlotte, NC, United States
- 13Department of Pediatrics, Faculty of Medicine, University of Toronto, Toronto, ON, Canada
Introduction: Juvenile idiopathic arthritis (JIA) is the most common childhood rheumatic disease which is commonly monitored by a combination of history, physical examination, bloodwork, and imaging. The COVID-19 pandemic prompted a rapid shift to telemedicine to ensure that patients continued to receive healthcare. The shift to telemedicine changed the methodology and ability of healthcare providers to monitor their patients' progress, as they were unable to perform direct hands-on assessments. The following survey sought to understand the impact of switching pediatric rheumatology healthcare delivery from in-person to telemedicine modality. Specifically, it sought to examine the rate of collection of critical data elements (CDE) for monitoring JIA disease activity and outcomes, barriers and facilitators to its collection, opinions on difficulty and importance of collecting CDE over telemedicine, tools and electronic medical record modifications that facilitated CDE collection, and other data elements that were important to collect during telemedicine visits.
Methods: A cross-sectional survey was sent to healthcare providers at all PR-COIN centers who saw patients using telemedicine. Qualitative data was analyzed using descriptive statistics and qualitative data was analyzed using an inductive approach.
Results: Survey respondents reported that they documented the CDE at least 75% of the time. Barriers to assessing and documenting critical data elements included (1) the inability to palpate or visualize all joints over telemedicine, (2) connectivity issues, and (3) forgetfulness with collecting all CDE. Respondents suggested using reminders within the electronic medical record to prompt documentation completeness and improve reliability. They also suggested including medication adherence, quality of life, and patient/caregiver satisfaction with their telemedicine experience as part of their documentation. A few centers reported that they had established processes to assist with data collection in advance of the telemedicine visit; however, the variation in responses reflects the need to standardize the process of providing care over telemedicine.
Discussion: Multiple barriers and facilitators to collecting CDE during telemedicine visits exist. Given that a proportion of the population will continue to be seen over telemedicine, teams need to adapt their practices to consistently provide high-quality care over virtual platforms, ensuring that patients at any institution receive a standardized level of service.
Introduction
Juvenile idiopathic arthritis (JIA) is a rare, childhood chronic condition which is estimated to affect between 2 and 8 million children worldwide (1, 2). Although JIA can be effectively managed with advanced anti-rheumatic therapies, ineffective treatment can result in pain, disability, and potential vision loss from uveitis (3, 4). Healthcare providers document various indicators to monitor JIA disease activity (5–10). These may include active joint count and provider global assessment (PGA) of disease activity. Patient reported indicators are also documented including pain scores and patient global assessment (PtGA) (11). Ultimately, reliable collection of these metrics influence disease monitoring and management, thereby impacting patients' long-term outcomes.
The Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN) learning network, currently comprised of 23 medical centers and parents across the United States and Canada, works collaboratively to identify and close gaps in healthcare for patients with JIA (12). They employ a “treat-to-target” strategy based on outcomes reported by both healthcare providers and patients or families is used to optimize care (13). PR-COIN previously established a set of quality measures to improve the care of children with JIA (10). Twenty measures including 10 outcome measures, 5 process measures, 4 data measures, and 1 balancing measure were included (10). Of the 20 measures identified, six were designated critical data elements (CDE): morning stiffness, joint pain, number of active joints, uveitis screening, PtGA, PGA of disease activity, which were deemed important for monitoring JIA disease activity and outcomes (10, 13). Consistent documentation and tracking of these CDE have enabled healthcare providers at PR-COIN sites to monitor their patient outcomes (10, 13). Monitoring of CDE has enabled healthcare providers to improve the outcomes of patients with JIA (14).
Access to care is essential for careful monitoring and timely management of JIA. Access to pediatric rheumatology care has long been a challenge due to the limited workforce in this field (15–17). The COVID-19 pandemic and its calls for physical distancing and quarantine further exacerbated the already limited access to healthcare providers and services (18, 19). During the pandemic, telemedicine use rose and became an alternative or complementary visit type to traditional in-person visits (20, 21). Coordinated design, evaluation, testing, adaptation, and sharing of best practices across rheumatology clinics is essential to optimize the care provided to patients with JIA in telemedicine settings (22–24).
Evidence supporting the provision of care using telemedicine in rheumatology in both the adult and pediatric populations has existed prior to the COVID-19 pandemic, but its adoption increased out of necessity for continued provision of care during the COVID crisis (25–30). An initial survey estimated that three-quarters of PR-COIN sites did not utilize telemedicine prior to the pandemic but were subsequently able to implement telemedicine by March 2020 (18). Providers felt that about half of their population could be safely and effectively seen over telemedicine (18). Although these centers were able to adapt to providing healthcare over telemedicine in the short-term, providers expressed concerns about the long-term effects of utilizing virtual care (18). This finding was not surprising given the hands-on examination is central to the examination process of pediatric rheumatology. During the pandemic, many PR-COIN site providers adopted the use of the Pediatric Gait, Arms, Legs, and Spine (PGALS) exam as an alternative to the hands-on exam (18, 31).
Recognizing the challenges of performing active joint count assessments over telemedicine, we wondered whether the shift of healthcare delivery to a virtual setting affected healthcare providers' ability to reliably collect all six CDE (10). We therefore sought to understand the healthcare providers' perspectives on the completion rates, barriers and facilitators to collecting CDE over telemedicine, which are important to successfully monitoring JIA disease activity and outcomes. The ultimate goal was to use these findings to design interventions to reduce these barriers, in turn, enabling more reliable collection of CDE via telemedicine, thereby improving the quality of healthcare provided over telemedicine to patients with JIA over telemedicine, resulting in better long-term outcomes.
Materials and methods
A cross-sectional electronic survey was created by the PR-COIN Digital-Health workgroup to characterize healthcare providers' experiences with the collection and documentation of CDE during telemedicine visits. The survey asked respondents to indicate which CDE they collected during telemedicine visits; their comfort level of collecting CDE over telemedicine; barriers to collecting CDE over telemedicine; tools that facilitated CDE collection; indicate which of the six CDE was most important to capture; which CDE was most difficult to capture, and what other data elements they thought was worth capturing during telemedicine visits. These responses were based on respondents' active recall and not an actual audit. Finally, respondents were asked to share changes which they instituted or had planned for their site's electronic medical record system as a result of delivering care over telemedicine.
A link to the voluntary, anonymous survey was sent to the lead principal investigators (PIs) of the 21 PR-COIN centers (number of existing center at the time of the study). The PIs were requested to share the survey link to their center's clinical staff who saw patients with JIA using telemedicine. The PIs were asked to confirm the number of recipients who they had sent the survey to in order to determine the denominator. This strategy was employed to avoid sending the survey to an outdated member mailing list. Participants provided implied consent to participate in the survey. The survey, which was conducted from August-September 2020.
The survey data was collected and managed using Research Electronic Data Capture (REDCap) (32, 33). REDCap is a workflow methodology and software solution designed for rapid development and deployment of electronic data capture tools to support clinical and translational research (32, 33).
Quantitative results were analyzed using descriptive statistics, and qualitative results were thematically analyzed using an inductive approach.
The PR-COIN registry and network-related collaborative quality improvement activities, including member surveys that are used as part of continuing quality improvement, were approved by Cincinnati Children's Medical Health Center's Institutional Review Board (IRB).
Results
Survey distribution and response rate
The survey was sent to the lead contact at 21 PR-COIN sites in the United States and Canada. Nineteen of 21 PR-COIN sites were represented in the survey response. Some sites were solely comprised of pediatric rheumatologists, while other sites were composed of a multidisciplinary team which included fellows and practitioners (medical professionals who are not physicians but have received additional training and are qualified to perform many similar functions as a physician, such as prescribing medications, diagnosing, treating, and managing patient care). Teams ranged from two staff pediatric rheumatologists at the smallest site to 14 staff pediatric rheumatologists, fellows, and practitioners. Fourteen (73.7%) sites reported having more than five pediatric rheumatologists at their sites.
The survey was sent to a total of 121 clinical staff who saw patients with JIA using telemedicine. A total of 119 (98.3%) completed the survey. Of the responses received, 103/119 (86.6%) surveys were fully completed, while 16 were partially completed.
Eighty-two (68.9%) respondents indicated they were staff pediatric rheumatologists, 24 (20.2%) were fellows, and the remainder (10.9%) were practitioners.
Collection and level of comfort collecting critical data elements during telemedicine visits
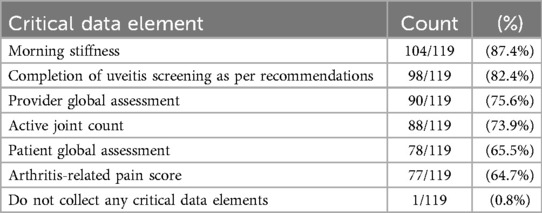
Respondents indicated that the six CDE data elements were collected more than half of the time (Table 1). The most documented CDE over telemedicine was morning stiffness 104/119 (87.4%), while the least commonly documented was arthritis-related pain score 77/119 (64.7%) (Table 1). Only one (0.8%) respondent indicated that they did not collect any of the 6 CDE identified by PR-COIN.
Of the 104 individuals indicating that they documented morning stiffness during telemedicine visits, 51 (49.0%) respondents indicated that they documented this parameter at every visit (Table 2). 89/104 (85.6%) respondents indicated that they were extremely comfortable documenting morning stiffness during telemedicine visits (Figure 1).
Of the 98 individuals indicating that they documented uveitis screening during telemedicine visits, 33 (33.7%) respondents indicated that they documented this parameter at every visit (Table 2). 75/98 (76.5%) respondents indicated that they were extremely comfortable documenting uveitis screening during telemedicine visits (Figure 1).
Of the 90 individuals indicating that they documented PGA during telemedicine visits, 25 (27.8%) respondents indicated that they documented this parameter at every visit (Table 2). 27/89 (30.3%) respondents indicated that they were extremely comfortable documenting PGA during telemedicine visits (Figure 1).
Of the 88 individuals indicating that they documented active joint count during telemedicine visits, 26 (29.5%) respondents indicated that they documented this parameter at every visit (Table 2). 15/88 (17.0%) respondents indicated that they were extremely comfortable documenting active joint count during telemedicine visits (Figure 1).
Of the 78 individuals indicating that they documented PtGA during telemedicine visits, 14 (17.9%) respondents indicated that they documented this parameter at every visit (Table 2). 42/78 (53.8%) respondents indicated that they were extremely comfortable documenting PtGA during telemedicine visits (Figure 1).
Of the 77 individuals indicating that they documented arthritis-related pain scores during telemedicine visits, 22 (28.6%) respondents indicated that they documented this parameter at every visit (Table 2). 50/77 (64.9%) respondents indicated that they were extremely comfortable documenting arthritis-related pain scores during telemedicine visits (Figure 1).
Overall, respondents appeared to be more comfortable collecting data which were reported by patients than data based on their assessment over telemedicine.
Barriers to collection of critical data elements
Forgetfulness and not knowing which tool to use to collect data were barriers for the collection of all CDE. Barriers to collecting uveitis screening results included that patients did not have their last screening date readily available during their visit nor did they have their results. Other barriers to not collecting PGA and active joint CDE included the inability to see and palpate joints and being too distracted with technical issues of using telemedicine. Additional barriers for active joints collection included difficulty assessing small joints or detecting subtle swelling, difficulty assessing young patients, and being too distracted with technical issues. PtGA collection barriers included not having the proper resources to facilitate its collection over telemedicine and an element not typically collected by a specific site. Other barriers to collecting arthritis-related pain scores included lack of proper resources to facilitate its collection over telemedicine and patients lack clarity in knowing whether their pain was related to arthritis.
Tools used to assist with collection of critical data elements
When asked what tools clinicians were using to collect CDE, the respondents from 16/19 (84.2%) centers indicated that they were using the pGALS to support the evaluation of joints. 9/19 (47.4%) centers reported that they had developed or had an existing mechanism to collect patient reported outcomes prior to the telemedicine clinic visit. 13/19 (68.4%) sites reported that they had existing reminders (e.g., forms/templates/flowsheets) or had created reminders in their electronic medical record system to remind them to collect CDE.
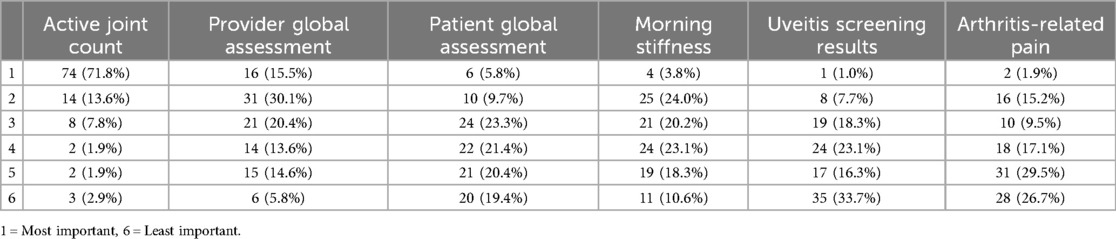
Ranking of critical data elements by importance and assessment difficulty
When respondents were asked to rank which CDE they thought was most important of the six, the majority indicated that was the active joint count 74/103 (71.8%) (Table 3).
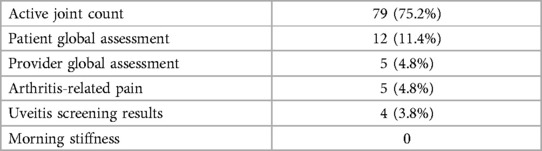
When respondents were asked to select which was the most difficult of CDE to collect during the telemedicine visit, the majority 79/109 (72.5%) indicated that it was the active joint count (Table 4).
Other elements to collect during telemedicine visits
When survey respondents were invited to suggest additional elements worth collecting during telemedicine visits, the majority suggested collecting a satisfaction survey regarding patient's telemedicine experience. Other suggestions included medication adherence, mood assessment, limitations in activities of daily living, quality of life, and the number of non-billable encounters that occurred over telemedicine.
Modifications to electronic medical record system to delineate telemedicine visits
The majority [60/109 (55.0%)] of respondents indicated that their site had made changes to their electronic medical record system to indicate that visits were conducted over telemedicine. 22/109 (20.2%) respondents indicated that their electronic medical record system already had the capability of distinguishing which visits were conducted in-person and which visits were conducted over telemedicine. Eight (7.3%) respondents indicated that their site intended to make changes to their electronic medical record system in the future to enable them to distinguish which visits occurred in-person vs. over telemedicine.
Discussion
The COVID-19 pandemic has resulted in significant changes in healthcare delivery in both the inpatient and ambulatory settings (34–36). For pediatric rheumatologists, this change has been most apparent in the outpatient setting given that many patients with chronic disease, including JIA, require frequent outpatient follow-up visits. Although the availability of telemedicine increases access for our patients (26, 37), we must consider not only access and acceptability, but also the quality of healthcare delivered over this medium, which may ultimately affect safety and patient outcomes (38). Our initial work (18) indicated that there was a significant variability in the reliable collection of many data elements needed for clinical care at a PR-COIN site level. This study focused on individual provider practices. We observed that the majority of providers were collecting CDE at least 60% of the time when seeing patients over telemedicine. Certain CDE were collected more reliably than others. This may have been related to similarities in how the CDE is administered during in person visits. For example, morning stiffness is often verbally asked of the patient or proxy during their in-person clinic visits.
The inability to perform hands-on physical examinations mostly affected provider's ability to determine active joint count and, in turn, the PGA. This uncertainty, in turn, made them less comfortable in documenting their findings into the patient's electronic medical record.
Morning stiffness and uveitis screening were the most commonly collected CDE. However, when providers were asked to rank the importance of these elements, they considered these elements less important compared to arthritis-related pain score and PtGA. This indicates that although providers were collecting some data elements, not all elements were reliably collected.
Positive experiences and acceptability have been reported by the majority of patients/caregivers, especially when considering factors like the distance of patients' residence from the healthcare provider, patients' educational level and the perceived benefits for social distancing (39, 40). In addition to reduced travel time, decreased missed time from work/school and financial savings associated with in-person visits, patients reported ease of use, shorter waiting periods and possible continued use in the post- pandemic period (26, 27, 41–43). Healthcare providers also reported high satisfaction, especially when patients had reliable internet (44). Common barriers identified with practicing telemedicine include lack of physical examination, reduced diagnostic accuracy due to incomplete clinical information, difficulty reaching patients, missing nonverbal communication, and lack of or challenges using technology required for telemedicine visits (45, 46). Barriers unique to the pediatric rheumatology population include trying to keep very young patients focused during virtual physical exam, and difficulty assessing psychosocial factors in adolescents when caregivers are present (46–48). Unfortunately, lower socioeconomic status and lower educational background may affect access to and quality of telemedicine visits e.g., poor bandwidth, which has implications in continuity of care, medication adherence and disease control (49–51). The quality of virtual care may also depend on the specific disease and its activity level. A randomized controlled trial demonstrated that telemedicine visits were not inferior to in-person visits for adult patients with rheumatoid arthritis whose disease was in remission or had low disease activity (52).
Although barriers to data collection were in part due to the nature of telemedicine and limitations in exam, a large contributor was simply due to provider workflow issues. The inexperience and lack of training in using telemedicine platforms, completing virtual patient check-ins, performing physical exams in a virtual setting, and the lack of support collecting patient reported outcomes, impacted their ability to collect CDE and complete their documentation.
Further, survey results indicated that for specific elements there were two main barriers: (1) the inability to conduct a reliable joint assessment that includes direct palpation of joints (especially when patients were not present at the visit), and (2) providers forgetting to collect and document the pertinent data elements. This illustrates that although telemedicine has limitations for specific aspects to the musculoskeletal exam, there are opportunities to improve workflows to collect the non-exam dependent, patient-reported data elements such as the PtGA or pain scores. As providers continue to integrate telemedicine as part of their clinical practice, we will need to consider systematic approaches to address these barriers, such as allocating job responsibilities and establishing force functions to ensure the reliable collection of CDE.
As previously indicated, fewer providers were comfortable performing physical examination to ascertain active joint count during telemedicine visit compared to acquiring other CDE due to the possibility of limited accuracy of the results. To address this concern, some providers may consider triaging patients to determine whether they should be seen virtually over telemedicine or if they should be seen in-person. To our knowledge, there is no universal established criteria on how to triage patients for telemedicine visits. One PR-COIN site utilized a pre-COVID developed triage tool that was developed prior to the pandemic which triaged based on referring symptoms to determine the urgency, time to be seen with the highest triaged levels 1 and 2 requiring in-person visit (53). Further research is also needed to identify which patients are most suitable to be seen for virtual visits and which might be better served by in-person assessment.
Alternatively, we may consider additional tools, models of care, and/or caregiver-specific education to facilitate the reliable reporting of physical examination results, including the active joint count. For example, there are already recommended modifications to the p-GALS, known as Virtual or Video-pGALS (V-pGALS), incorporating amended or additional maneuvers added to capture needed elements more accurately (47, 54). A pilot study has demonstrated the acceptability and reliability of this tool (31). Additional research needs to be performed to further validate the ability of the V-pGALS to perform joint assessment. This could be accomplished by performing a study where patients received a joint count over telemedicine followed by an in-person assessment shortly thereafter.
There is an opportunity to improve the collection of CDE that are not dependent on the clinical exam, such as patient-reported outcomes, over telemedicine. The introduction of new clinical workflows such as the incorporation of integrated electronic health record tools (for both providers and patients navigators), provider education with time sensitive scripting and checklists, medical staff virtual rooming protocols for medical staff, and pre-visit planning, may better support reliable collection of these metrics rather than forgetting. Enabling patients and proxies to take a proactive role in their healthcare by educating them on how to support their telemedicine visit and teaching them skill may empower them whilst improving the overall outcome of the telemedicine visit.
Despite being one of the ranked one of the most difficult CDE to collect via telemedicine, respondents indicated that active joint count was the most important CDE to collect over telemedicine. Given this opinion, additional efforts should be expended to improve the ability to accurately collect this variable. Recognizing that the varying levels of knowledge and technology literacy, educational curriculums should be carefully designed to ensure that healthcare providers possess the necessary knowledge and skillset to effectively provide care over telemedicine. Furthermore, the development of additional educational electronic tools i.e., phone applications, could improve timely access to providers.
It would be worth surveying patients to understand their opinion of healthcare delivery over telemedicine and their satisfaction with the process. Some studies have indicated that although being seen over telemedicine was preferred during the pandemic, it is not preferred after the pandemic (41, 42). Additional patient reported outcome measures/surveys could be introduced through patient portal builds in the electronic medical record.
Differentiating data that is collected by telemedicine to that from in-person visits will enable the comparison of patient outcomes to determine whether the delivery of care using telemedicine results in similar patient outcomes. This information will inform whether providing care over telemedicine is comparable to that in-person care or it may identify situations where telemedicine care is a satisfactory option.
Our study is limited by the fact that it surveyed the PR-COIN learning network. PR-COIN sites have previously collected CDE during in-person visits and they have already engrained this practice into their established workflows, practices, and culture. Therefore, these findings may be biased due to the active recall design of the survey, as well as the heightened awareness and prior collection of these data elements for clinical care. As such, these findings may not be representative of the broader pediatric rheumatology community. Broader surveys and studies involving the use of these data elements, both in in-person and virtual settings, amongst pediatric rheumatologists are required.
In addition, respondents answered questions based on their own practice. We did not inquire about the composition of their practice, such as the proportion of JIA subtypes seen in their clinic or the age range of their patient population. These factors may have influenced their responses. If their practice consisted primarily of adolescents with arthritis affecting larger joints, it may be easier to perform a virtual assessments may have been easier since because they can follow instructions, and the joint swelling would be more prominent, in contrast to a toddler with arthritis affecting small joints who is unable to follow instructions.
Although the majority of video platforms used in telemedicine have matured over time, they may vary in terms of available features and ease of use. These differences can influence the technical system requirements needed to operate the software or the user's learning curve.
It is also possible that self-reported collection of data elements may not accurately reflect actual practices, potentially over or underestimating actual practices. Collecting objective data on the frequency that these metrics are captured during visits would more definitively identify gaps. Additionally, while this survey primarily captures largely the provider experience with collecting data elements via telemedicine, future next steps may want to examine patient acceptability regarding the ways in which patient-reported outcomes are collected and utilized in telemedicine care. Ultimately, a deeper understanding of how collection of these data elements are collected and utilized, and how they affect patient clinical outcomes in JIA is needed and is currently being investigated currently underway.
It is important to remember that although it may be easy for some healthcare institutions to offer telemedicine to patients, health inequities still exist. These disparities can affect some individuals' ability to access care using this medium (21, 55). Additional steps must be taken to ensure equitable healthcare delivery using telemedicine in the future (25, 29, 56).
Conclusion
Multiple barriers and facilitators exist in the delivery of pediatric rheumatology care over telemedicine. Our findings suggest that telemedicine processes and practices vary both across different centers, as well as within individual centers. This highlights the need to standardize telemedicine visit procedures to ensure that CDE are reliably and consistently collected, irrespective of visit type. Given that a portion of patients with JIA will likely continue to be serviced over telemedicine post-pandemic, teams need to adapt and refine their existing clinical practices to continue providing high-quality care using this platform.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Cincinnati Children's Hospital Medical Center. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because implied consent was used as the mechanism for consent for the healthcare providers who chose to complete the survey.
Author contributions
YG: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MR: Conceptualization, Data curation, Formal Analysis, Methodology, Resources, Visualization, Writing – original draft, Writing – review & editing. SA: Writing – original draft, Writing – review & editing. RP: Conceptualization, Writing – original draft, Writing – review & editing. JH: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. DB: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. SV: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. TL: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. ST: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. FB-S: Conceptualization, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
This project was conducted with the cooperation and assistance of the Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN) and the physicians, providers and families participating in this multicenter learning health network www.pr-coin.org.
Conflict of interest
The authors declare that when the research was conducted, there was an absence of any commercial or financial relationships that could be construed as a potential conflict of interest. This research was conducted using data obtained through the Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN), collected by the physicians and providers participating in this multicenter Quality Improvement Collaborative. https://pr-coin.org/. Since the completion of this research, YG has received educational grant from Pfizer to improve the delivery of telemedicine visits for patients with JIA. Since the completion of the research, FB-S has departed her academic position at Nationwide Children's Hospital and secured employment at Amgen.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dave M, Rankin J, Pearce M, Foster HE. Global prevalence estimates of three chronic musculoskeletal conditions: club foot, juvenile idiopathic arthritis and juvenile systemic lupus erythematosus. Pediatr Rheumatol Online J. (2020) 18(1):49. doi: 10.1186/s12969-020-00443-8
2. Petty RE, Laxer RM, Lindsley CB, Wedderburn L. Textbook of Pediatric Rheumatology. 7th ed. Elsevier Health Sciences: Philadelphia, PA (2015). p. 736.
3. Murray KJ, Lovell DJ. Advanced therapy for juvenile arthritis. Best Pract Res Clin Rheumatol. (2002) 16(3):361–78. doi: 10.1053/berh.2002.0234
4. Len CA, Miotto e Silva VB, Terreri MTRA. Importance of adherence in the outcome of juvenile idiopathic arthritis. Curr Rheumatol Rep. (2014) 16(4):410. doi: 10.1007/s11926-014-0410-2
5. McErlane F, Beresford MW, Baildam EM, Thomson W, Hyrich KL. Recent developments in disease activity indices and outcome measures for juvenile idiopathic arthritis. Rheumatology (Oxford). (2013) 52(11):1941–51. doi: 10.1093/rheumatology/ket150
6. Consolaro A, Giancane G, Schiappapietra B, Davì S, Calandra S, Lanni S, et al. Clinical outcome measures in juvenile idiopathic arthritis. Pediatr Rheumatol Online J. (2016) 14(1):23. doi: 10.1186/s12969-016-0085-5
7. Wallace CA, Ruperto N, Giannini E; Childhood Arthritis and Rheumatology Research Alliance; Pediatric Rheumatology International Trials Organization; Pediatric Rheumatology Collaborative Study Group. Preliminary criteria for clinical remission for select categories of juvenile idiopathic arthritis. J Rheumatol. (2004) 31(11):2290–4.15517647
8. Wallace CA, Huang B, Bandeira M, Ravelli A, Giannini EH. Patterns of clinical remission in select categories of juvenile idiopathic arthritis. Arthritis Rheum. (2005) 52(11):3554–62. doi: 10.1002/art.21389
9. Magni-Manzoni S, Ruperto N, Pistorio A, Sala E, Solari N, Palmisani E, et al. Development and validation of a preliminary definition of minimal disease activity in patients with juvenile idiopathic arthritis. Arthritis Rheum. (2008) 59(8):1120–7. doi: 10.1002/art.23916
10. Bingham CA, Harris JG, Qiu T, Gilbert M, Vora SS, Yildirim-Toruner C, et al. Pediatric rheumatology care and outcomes improvement network’s quality measure set to improve care of children with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). (2023) 75(12):2442–52. doi: 10.1002/acr.25168
11. Trachtman R, Wang CM, Murray E, Szymonifka J, Pan N, Adams AB, et al. PROMIS computer adaptive tests and their correlation with disease activity in juvenile idiopathic arthritis. J Clin Rheumatol. (2021) 27(4):131–5. doi: 10.1097/RHU.0000000000001171
12. Harris JG, Bingham CA, Morgan EM. Improving care delivery and outcomes in pediatric rheumatic diseases. Curr Opin Rheumatol. (2016) 28(2):110–6. doi: 10.1097/BOR.0000000000000257
13. El Tal T, Ryan ME, Feldman BM, Bingham CA, Burnham JM, Batthish M, et al. Consensus approach to a treat-to-target strategy in juvenile idiopathic arthritis care: report from the 2020 PR-COIN consensus conference. J Rheumatol. (2022) 49(5):497–503. doi: 10.3899/jrheum.210709
14. Harris JG, Bingham CA, Vora SS, Yildirim-Toruner C, Batthish M, Bullock DR, et al. Using a collaborative learning health system approach to improve disease activity outcomes in children with juvenile idiopathic arthritis in the pediatric rheumatology care and outcomes improvement network. Front Pediatr. (2024) 12:1434074. doi: 10.3389/fped.2024.1434074
15. Correll CK, Klein-Gitelman MS, Henrickson M, Battafarano DF, Orr CJ, Leonard MB, et al. Child health needs and the pediatric rheumatology workforce: 2020–2040. Pediatrics. (2024) 153(Suppl 2):e2023063678R. doi: 10.1542/peds.2023-063678R
16. Lee JJY, Laxer RM, Feldman BM, Barber CEH, Batthish M, Berard R, et al. Variations in pediatric rheumatology workforce and care processes across Canada. J Rheumatol. (2022) 49(2):197–204. doi: 10.3899/jrheum.201611
17. Cox A, Piper S, Singh-Grewal D. Pediatric rheumatology consultant workforce in Australia and New Zealand: the current state of play and challenges for the future. Int J Rheum Dis. (2017) 20(5):647–53. doi: 10.1111/1756-185X.12802
18. Goh YI, Bullock DR, Taylor J, Pooni R, Lee TC, Vora SS, et al. exploring pediatric tele-rheumatology practices during COVID-19: a survey of the PRCOIN network. Front Pediatr. (2021) 9:642460. doi: 10.3389/fped.2021.642460
19. Maldonado D, Tu E, Mahmood SN, Wahezi DM, Darapaneni R, Sima N, et al. Association of medication access difficulty and COVID-19-related distress with disease flares in rheumatology patients during the COVID-19 pandemic. Arthritis Care Res (Hoboken). (2021) 73(8):1162–70. doi: 10.1002/acr.24531
20. Prahalad P, Leverenz B, Freeman A, Grover M, Shah S, Conrad B, et al. Closing disparities in pediatric diabetes telehealth care: lessons from telehealth necessity during the COVID-19 pandemic. Clin Diabetes. (2022) 40(2):153–7. doi: 10.2337/cd20-0123
21. Zeineddin S, Macy ML, Bouchard ME, Carroll MS, Linton S, De Boer C, et al. Disparities in telemedicine use among children seen in surgical clinics during the COVID-19 pandemic: experience of one tertiary care freestanding children’s hospital. Telemed J E Health. (2024) 30(3):642–50. doi: 10.1089/tmj.2023.0212
22. Duke EM. The Pediatric Rheumatology workforce: a study of the supply and demand for pediatric rheumatologists. Report to Congress. Bureau of Health Professions. Health Resources & Services Administration. Washington, DC: US Department of Health & Human Services (2007). Available online at: http://bhpr.hrsa.gov/healthworkforce/reports/pedrheumatology.pdf (accessed July 28, 2011)
23. Foster H, Rapley T. Access to pediatric rheumatology care—a major challenge to improving outcome in juvenile idiopathic arthritis. J Rheumatol. (2010) 37(11):2199–202. doi: 10.3899/jrheum.100910
24. Henrickson M. Policy challenges for the pediatric rheumatology workforce: part I. Education and economics. Pediatr Rheumatol Online J. (2011) 9:23. doi: 10.1186/1546-0096-9-24
25. Bateman J, Cleaton N. Managing patients using telerheumatology: lessons from a pandemic. Best Pract Res Clin Rheumatol. (2021) 35(1):101662. doi: 10.1016/j.berh.2021.101662
26. Kessler EA, Sherman AK, Becker ML. Decreasing patient cost and travel time through pediatric rheumatology telemedicine visits. Pediatr Rheumatol Online J. (2016) 14(1):54. doi: 10.1186/s12969-016-0116-2
27. Bullock DR, Vehe RK, Zhang L, Correll CK. Telemedicine and other care models in pediatric rheumatology: an exploratory study of parents’ perceptions of barriers to care and care preferences. Pediatr Rheumatol. (2017) 15(1):55. doi: 10.1186/s12969-017-0184-y
28. Strickler AS, Palma J, Charris R, Candia T, Grez M, González B, et al. Contribution of the use of basic telemedicine tools to the care of children and adolescents with juvenile idiopathic arthritis at the Puerto Montt Hospital, Chile. Rev Chil Pediatr. (2018) 89(1):59–66. doi: 10.4067/S0370-41062018000100059
29. Matsumoto RA, Barton JL. Telerheumatology: before, during, and after a global pandemic. Curr Opin Rheumatol. (2021) 33(3):262–9. doi: 10.1097/BOR.0000000000000790
30. Teixeira V, Cordeiro I, Gonçalves MJ, Fonseca JE, Macieira C. Telerheumatology - breaking barriers to access care in Rheumatology. Acta Reumatol Port. (2018) 43(4):253–5. English.30641532
31. Giray E, Kenis-Coskun O, Karadag-Saygi E, Ozyemisci-Taskiran O. Interrater reliability, acceptability, and practicality of real-time video pediatric gait, arms, legs, and spine for musculoskeletal assessment of children during telemedicine visits. J Clin Rheumatol. (2022) 28(5):235–9. doi: 10.1097/RHU.0000000000001840
32. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
33. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
34. McDonnell Busenbark M, Children’s Hospital Association. COVID19: Pandemic to Permanently Change How Children’s Hospitals Deliver Care. (2020). [cited 2020 Nov 5]. Available online at: https://www.childrenshospitals.org/Newsroom/Childrens-Hospitals-Today/Summer-2020/Articles/COVID19-Pandemic-to-Permanently-Change-How-Childrens-Hospitals-Deliver-Care
35. Mohammad I, Berlie HD, Lipari M, Martirosov AL, Duong AA, Faraj M, et al. Ambulatory care practice in the COVID-19 era: redesigning clinical services and experiential learning. J Am Coll Clin Pharm. (2020) 3(6):1129–37. doi: 10.1002/jac5.1276
36. Keesara S, Jonas A, Schulman K. COVID-19 and health care’s digital revolution. N Engl J Med. (2020) 382(23):e82. doi: 10.1056/NEJMp2005835
37. Rimsza ME, Hotaling AJ, Keown ME, Marcin JP, Moskowitz WB, Sigrest TD, et al. The use of telemedicine to address access and physician workforce shortages. Pediatrics. (2015) 136(1):202–9. doi: 10.1542/peds.2015-1253
38. Haimi M, Brammli-Greenberg S, Baron-Epel O, Waisman Y. Assessing patient safety in a pediatric telemedicine setting: a multi-methods study. BMC Med Inform Decis Mak. (2020) 20(1):1–14. doi: 10.1186/s12911-020-1074-7
39. Cavagna L, Zanframundo G, Codullo V, Pisu MG, Caporali R, Montecucco C. Telemedicine in rheumatology: a reliable approach beyond the pandemic. Rheumatology. (2021) 60(1):366–70. doi: 10.1093/rheumatology/keaa554
40. Shenoy P, Ahmed S, Paul A, Skaria TG, Joby J, Alias B. Switching to teleconsultation for rheumatology in the wake of the COVID-19 pandemic: feasibility and patient response in India. Clin Rheumatol. (2020) 39(9):2757–62. doi: 10.1007/s10067-020-05200-6
41. Makhlouf Y, Nessib DB, Ferjani H, Triki W, Maatallah K, Dhia K, et al. The concept of telemedicine in pediatric rheumatology in Tunisia: parents’ perceptions. J Pediatr Nurs. (2023) 69:6–9. doi: 10.1016/j.pedn.2022.12.005
42. Oh Y, Hennessey A, Young L, Barrett C. Evaluation of patient satisfaction for telehealth (telephone and video) in rheumatology outpatients during COVID-19 pandemic. Intern Med J. (2022) 52(4):559–65. doi: 10.1111/imj.15663
43. Poulsen KA, Millen CM, Lakshman UI, Buttner PG, Roberts LJ. Satisfaction with rural rheumatology telemedicine service. Int J Rheum Dis. (2015) 18(3):304–14. doi: 10.1111/1756-185X.12491
44. Tornero-Molina J, Sánchez-Alonso F, Fernández-Prada M, Bris-Ochaita ML, Sifuentes-Giraldo A, Vidal-Fuentes J. Tele-rheumatology during the COVID-19 pandemic. Reumatol Clin (Engl Ed). (2022) 18(3):157–63. doi: 10.1016/j.reuma.2020.10.004
45. Chock EY, Putman M, Conway R, Danila MI, Hoyer B, Hsieh E, et al. Experience with telemedicine among rheumatology clinicians during the COVID-19 pandemic: an international survey. Rheumatol Adv Pract. (2022) 6(2):rkac039. doi: 10.1093/rap/rkac039
46. Pooni R, Ronis T, Lee T, the CARRA Investigators. Telemedicine use by pediatric rheumatologists during the COVID-19 pandemic. Pediatr Rheumatol. (2021) 19(1):93. doi: 10.1186/s12969-021-00565-7
47. Shenoi S, Hayward K, Curran ML, Kessler E, Mehta JJ, Riebschleger MP, et al. Telemedicine in pediatric rheumatology: this is the time for the community to embrace a new way of clinical practice. Pediatr Rheumatol. (2020) 18(1):85. doi: 10.1186/s12969-020-00476-z
48. Balmuri N, Onel KB. Glitches in the utilization of telehealth in pediatric rheumatology patients during the COVID-19 pandemic. Pediatr Rheumatol. (2020) 18(1):78. doi: 10.1186/s12969-020-00477-y
49. Jackson LE, Danila MI. Healthcare disparities in telemedicine for rheumatology care. Curr Opin Rheumatol. (2022) 34(3):171–8. doi: 10.1097/BOR.0000000000000869
50. Kavadichanda C, Shah S, Daber A, Bairwa D, Mathew A, Dunga S, et al. Tele-rheumatology for overcoming socioeconomic barriers to healthcare in resource constrained settings: lessons from COVID-19 pandemic. Rheumatology (Oxford). (2021) 60(7):3369–79. doi: 10.1093/rheumatology/keaa791
51. George MD, Danila MI, Watrous D, Reddy S, Alper J, Xie F, et al. Disruptions in rheumatology care and the rise of telehealth in response to the COVID-19 pandemic in a community practice-based network. Arthritis Care Res (Hoboken). (2021) 73(8):1153–61. doi: 10.1002/acr.24626
52. de Thurah A, Stengaard-Pedersen K, Axelsen M, Fredberg U, Schougaard LMV, Hjollund NHI, et al. Tele-health followup strategy for tight control of disease activity in rheumatoid arthritis: results of a randomized controlled trial. Arthritis Care Res (Hoboken). (2018) 70(3):353–60. doi: 10.1002/acr.23280
53. Vora SS, Buitrago-Mogollon TL, Mabus SC. A quality improvement approach to ensuring access to specialty care for pediatric patients. Pediatr Qual Saf. (2022) 7(3):e566. doi: 10.1097/pq9.0000000000000566
54. Pediatric Musculoskeletal Matters. Virtual or Video-pGALS (V-pGALS) [Internet]. (2020). [cited 2021 Jun 6]. Available online at: http://www.pmmonline.org/doctor/approach-to-clinical-assessment/examination/v-pgals (accessed June 6, 2021).
55. Sen BP, Sharma P, Brisendine A, Blackburn J, Morrisey M, Menachemi N, et al. Disparities in telehealth utilization in a population of publicly insured children during the COVID-19 pandemic. Popul Health Manag. (2022) 25(2):178–85. doi: 10.1089/pop.2021.0343
Keywords: pediatric rheumatology, telemedicine, virtual, data documentation, eHealth, telehealth, telerheumatology, quality of care
Citation: Goh YI, Ryan ME, Akoghlanian S, Pooni R, Harris JG, Bullock DR, Vora SS, Lee TC, Tse SML and Barbar-Smiley F (2024) Key data elements for a successful pediatric rheumatology virtual visit: a survey within the PR-COIN network. Front. Pediatr. 12:1457607. doi: 10.3389/fped.2024.1457607
Received: 1 July 2024; Accepted: 12 August 2024;
Published: 22 October 2024.
Edited by:
Lovro Lamot, University of Zagreb, CroatiaReviewed by:
Agneza Marija Pasini, Children's Hospital Srebrnjak, CroatiaSwee Ping Tang, Hospital Selayang, Malaysia
Copyright: © 2024 Goh, Ryan, Akoghlanian, Pooni, Harris, Bullock, Vora, Lee, Tse and Barbar-Smiley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Y. Ingrid Goh, aW5ncmlkLmdvaEB1dG9yb250by5jYQ==
 Y. Ingrid Goh
Y. Ingrid Goh Meghan E. Ryan3
Meghan E. Ryan3 Shoghik Akoghlanian
Shoghik Akoghlanian Rajdeep Pooni
Rajdeep Pooni Julia G. Harris
Julia G. Harris Danielle R. Bullock
Danielle R. Bullock Sheetal S. Vora
Sheetal S. Vora Tzielan C. Lee
Tzielan C. Lee Shirley M.L. Tse
Shirley M.L. Tse Fatima Barbar-Smiley
Fatima Barbar-Smiley