
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Pediatr. , 30 October 2024
Sec. Pediatric Urology
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1445205
This article is part of the Research Topic Reviews in Pediatric Urology 2024 View all 14 articles
 Vinaya P. Bhatia1*
Vinaya P. Bhatia1* Kristin Ebert1
Kristin Ebert1 Shannon Cannon1
Shannon Cannon1 Walid A. Farhat1
Walid A. Farhat1 Heidi W. Brown2
Heidi W. Brown2 Jane Mahoney3
Jane Mahoney3 Marisa E. Hilliard4
Marisa E. Hilliard4 Kristina L. Penniston1
Kristina L. Penniston1
Long-term follow-up for individuals with hypospadias remains a critical area of need, yet evidence-based guidelines for such follow-up are lacking, and the role of involvement of relevant experts is not yet established. Using our hypospadias-specific health-related quality of life conceptual framework and a subsequent qualitative study of prepubertal males and parents of males with hypospadias, we identified potential priorities for long-term follow-up of youth with hypospadias. Using thematic codes from our patient and parent interviews, we searched PubMed for relevant articles and identified the specialties represented by all the authors of these articles. Our search strategy revealed consistent expertise across HRQOL themes and subthemes, including pediatric and adult urology, health psychology, psychiatry, endocrinology, genetics, and social work. Communication experts, as well as patients and families, were also represented in our literature search. Using these findings, we compiled a comprehensive list of potential stakeholders to inform the development of holistic care guidelines for individuals with hypospadias. By engaging these stakeholders, we aim to develop consensus-based, long-term follow-up guidelines and tools to address the evolving physical and psychosocial needs of people with hypospadias over a lifetime. The use of qualitatively derived thematic codes to search for relevant literature is an accessible approach to identifying relevant stakeholders. These findings underscore the importance of involving diverse, multidisciplinary expertise to ensure comprehensive, patient-centered care in complex genitourinary conditions.
Current longitudinal research suggests that long-term follow-up for youth and adults with hypospadias is required for close monitoring of physical and psychological complications after repair (1–3). However, no formal guidelines for long-term follow-up exist, and there is a paucity of literature on which specialties or experts should be involved in the long-term follow-up of this population. Research on improving the quality of care in chronic pediatric urologic diseases suggests that identifying experts who need to be involved in long-term care is a critical step to facilitate appropriate long-term follow-up (4).
Frameworks to identify appropriate experts in other urological conditions refer to the understanding of condition-specific health-related quality of life (HRQOL) (5) and use extensive patient input to identify and prioritize concerns (6). To apply these approaches to hypospadias, we previously published a novel conceptual framework for health-related quality of life (HRQOL) for youth with hypospadias based on a scoping literature review (7). This framework included themes of penile appearance, voiding function, social function, psychological and behavioral function, and sexual function. Our subsequent qualitative study of 8–12-year-old males and their parents supported the hypospadias-specific HRQOL Framework for prepubertal males (Figure 1, manuscript in review). Together, our previous work has synthesized youth and parent experiences after hypospadias repair, which are important to consider in identifying clinical priorities.
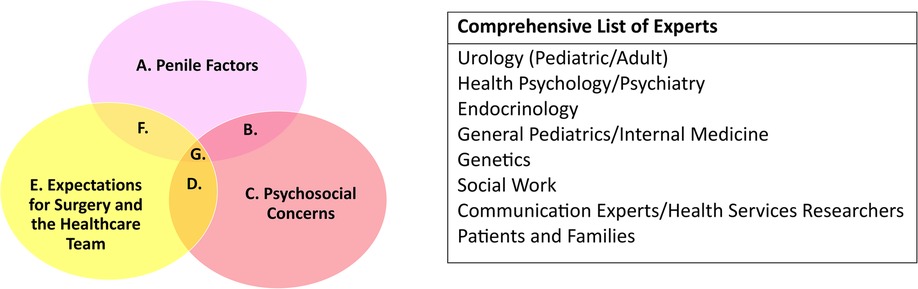
Figure 1. Themes and experts. Below, we include themes identified from the literature review and parent/youth interviews, as well as identified stakeholders for expert consensus.
We hypothesized that we could identify a consistent and comprehensive list of potential experts and stakeholders by using our previously generated codes from qualitative interviews of people with hypospadias as our search terms. Our goal would then be to contact these potential expert stakeholders and attempt to establish consensus between healthcare providers and patients on priority concerns and an optimal timeframe for follow-up for different concerns.
We previously conducted an IRB-approved, semi-structured interview study of English-speaking 8–12-year-old males with a history of repaired hypospadias (8). Potential participants with medical or neurocognitive conditions that would prevent the ability to autonomously answer interview questions were excluded. We completed interviews for 20 families (18 individuals, 10 adults parents, 8 youth). Interviews were conducted over the telephone, audiorecorded, transcribed, and de-identified. We employed hybrid thematic analysis to generate a first-round codebook to describe patient experiences, parent–proxy experiences, and parent experiences. Interviews were continued until thematic saturation was achieved (i.e., no new concepts or codes were generated). The second round of value-based coding was then performed with two investigators. The final thematic analysis was completed using the second-round coding with expertise from the listed authors in qualitative research, pediatric urology, and psychology. All coding was completed in NVivo 12 software (QSR International, 2020). Highest-order themes and subthemes were confirmed by the study investigators (VPB, SC, ME, HWB, WAF).
To identify expertise related to hypospadias-specific HRQOL, we used the domains of our published HRQOL framework (7) and the themes and subthemes of our qualitative research as search terms in PubMed. Specifically, the three overarching themes were penile factors, psychosocial concerns, and expectations of surgery and the healthcare team (Figure 1), each of which had subthemes that are listed in Table 1 (8). The duration of inclusion of our search was 15 years (December 2008–December 2023). PubMed was selected as the search engine of choice for article identification and selection due to the precision of search results, reliability of the search algorithms for future reproducibility of our methods, and higher utility of clinically oriented searches based on existing studies (9, 10). The word “hypospadias” was added to each search term to improve the specificity of our search. Articles were reviewed for relevancy to hypospadias in each search by the first author. Engagement of physicians, parents, or youth and adults with hypospadias was also collected for the included studies and authors (Table 1). Article titles and author affiliations and expertise were then disseminated to the author list for approval prior to the final analysis and compilation of the potential expert list.
For this exploratory study, a “potential expert” was defined as someone beyond the training phase of education (i.e., completed residency and/or fellowship) who had published at least one article as a first, middle, or senior author on the topic of hypospadias. We performed confirmation searches of the specialties of all listed authors in Google Scholar and ORCID (when available) to determine the correct specialty based on the author's most recent institution affiliation on publications within the last 5 years. At least two sources were required to confirm the author's expertise and affiliation at the time of publication, either two articles or one article and an ORCID (when available) that was linked to up-to-date references (within the past 5 years). For authors who were non-specialized trainees (i.e., undergraduate, medical students, residents, or fellows) at the time of publication, as confirmed by Google searches, the specialty of record was excluded. We generated an initial list of potential expert stakeholders for the holistic care of people with hypospadias from the list of represented specialties (Figure 1).
We identified at least one relevant article for each hypospadias-specific HRQOL theme and subtheme, as detailed in Table 1. The table also includes information on patient or parental participation and general authorship expertise for each relevant article.
Penile functions refer to erections and voiding. Our search of “penile functions hypospadias” revealed articles authored mainly by pediatric urologists (11). The search of “urinary spraying hypospadias” elicited articles by pediatric and adult urologists (12). Searches regarding “discomfort with penile appearance hypospadias” (13, 14) included psychiatrists, endocrinologists, health psychologists, and pediatric urologists. A search regarding “hypospadias penile length” included authors from genetics and endocrinology (15, 16). Searches with the terms embarrassment and penile size comparison did not identify any articles. We did find that authors engaged the input of patients (pediatric and adult) in an attempt to understand the impacts of urinary spraying and control and penile appearance on quality of life.
In the realm of psychosocial concerns, searches regarding “stigma hypospadias” yielded expertise from health psychologists (17), pediatric urologists (18), and pediatricians (19). A search of “future worries hypospadias” identified articles by health psychologists, psychiatrists, and pediatric urologists (20). A subsequent search of “interpersonal actions hypospadias” and “teasing hypospadias” referred to articles by pediatric urologists (21) and endocrinologists, psychologists, and geneticists (22). Searches related to “public restroom/public toilet hypospadias” referred to articles authored by psychologists and urologists (7), while searches surrounding “growth and development hypospadias” were authored by geneticists and pediatricians (23). The authors engaged adult patients, parents, and social media to perform their analysis
When searching “knowledge of hypospadias surgery” and “provider experience hypospadias,” we identified two articles written by urologists, endocrinologists, and patient–provider communication experts (24, 25). When searching “setting expectations hypospadias surgery,” we found articles authored by pediatric urologists and social workers (26). A search for “education and advocacy hypospadias” did not yield any results. Researchers obtained these perspectives from adult and pediatric patients, parents, and physicians.
When examining “trauma from hypospadias surgery” in the overlap of psychosocial functions and expectations of surgery, one article authored by urologists, psychologists, and psychiatrists was identified (27). A search focused on the overlap of expectations of surgery and penile factors was authored by psychologists and pediatric urologists (28).
Searches regarding “uncertainty hypospadias” led to an article previously identified from “knowledge of hypospadias surgery,” which was authored by pediatric urologists and patient-provider communication experts. A search regarding “social determinants of health hypospadias” was authored by pediatric urologists (29). Finally, searches regarding sources of “worry associated with hypospadias” drew articles with experts from pediatric urology (30, 31) and andrology (32).
This analysis illustrates a research-driven approach to the identification of appropriate experts for a complex and multifaceted disease. We used a conceptual framework for HRQOL and qualitative feedback from patient and parent stakeholders to identify clinical priorities and a wide range of clinical, research, and lived-experience expertise, which can be used to guide clinical care guidelines in this area. In addition, the ethnically, racially, and socioeconomically diverse demographics of our initial interview study should contribute to the broad applicability of our findings to English-speaking youth in the postoperative, prepubertal setting (8). Our search strategy successfully identified consistent expertise based on the search terms, as most of the article authors and experts were evident across multiple themes. This stepwise approach to identifying an array of potential stakeholders can prepare the field to develop comprehensive consensus-based holistic care guidelines, screening tools, and a referral network for youth and adults with hypospadias. Furthermore, this system for identifying stakeholders may be a useful approach for clinicians and researchers undertaking similar efforts in other complex, chronic genitourinary pediatric conditions, such as spina bifida, variations of sexual characteristics, or cloacal anomalies.
Engaging stakeholders in research requires identifying the appropriate domains of expertise (including not only clinical and research experts from various domains but also people with lived experience) in advance and adequately involving them in the development of research questions (4). Stakeholders may also help conduct studies and interpret results (4–6). Identifying all of the potential stakeholders is critical to ensure that the conducted research is of high quality, rigorous, and holistic (4), as well as relevant to the people impacted by the condition. Prominent examples of stakeholder identification in pediatric urology have included the use of a national patient advocacy network for care of spina bifida (6) and the creation of a partnership between physician and patient stakeholder core to iteratively revise and improve clinical trial design and surgical selection in pediatric kidney stone disease (33).
The current study extends this methodology to advance stakeholder engagement in research related to supporting HRQOL among people with hypospadias. Building on the results of this study that identified key stakeholders and important domains of expertise (Figure 1), our next goal will be to engage stakeholders in the design of screening tools and treatment strategies for hypospadias over the long term. Including our patient and parent experts will be critical to ensure that our study design is thorough and pragmatically addresses the lived experiences of youth and adults with hypospadias (5, 34).
Some stakeholders may bring expertise that is more relevant to specific stages of care for hypospadias than others. For example, an andrologist or adult reconstructive urologist may be particularly pertinent as the patient reaches sexual maturity (e.g., after puberty). Similarly, child psychology may need to be involved in care at the time point in development when body image, self-esteem, and interpersonal interactions are becoming a larger concern. Further qualitative study of patients in multiple different stages of development will be needed to ascertain these types of important details.
Limitations include the use of qualitative themes derived from interviews of patients at a specific time point in development (i.e., peri-pubertal), and the use of PubMed without other search engines to review available literature on our search terms. Additional research using interviews over multiple stages of development may identify additional themes and other experts not reflected in this study (e.g., adolescent medicine or sexual function/health). We acknowledge the importance of conducting such interviews in the near future to elucidate the needs of patients across a lifespan and ensure that appropriate experts are available to deliver optimal, long-term care. Our reliance on English language articles may exclude culturally relevant issues or expertise found in studies conducted in other regions of the world. Finally, this work is limited by the current state of the field—as research on medical, psychosocial, and healthcare delivery aspects of hypospadias care grows and innovates over time, this search should be repeated.
Hypospadias-specific HRQOL is complex and may change over time as children become adolescents and then adults. Finding the experts to facilitate care and support patients over a lifetime requires a thoughtful approach to ensuring comprehensive multidisciplinary care. In this study, we identified potential stakeholders to be involved in the development of multidisciplinary care guidelines for long-term follow-up care of people with hypospadias, including urology (pediatric/adult), health psychology, psychiatry, endocrinology, general pediatrics, internal medicine, genetics, social work, communication experts/health services researchers, and patients and families. Our next goal will be to interview and survey these proposed specialists and patients across multiple stages of development (youth and adults) to obtain qualitative feedback on whether these proposed experts are needed for multidisciplinary care for youth and adults with hypospadias. Once we have obtained this additional feedback, we intend to use the revised list of experts to develop consensus-based guidelines for long-term follow-up after hypospadias repair. Future efforts will also involve the development of implementable care tools that will refer patients and families to appropriate experts as their physical and psychological concerns evolve over time, to support disease-specific HRQOL.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Internal Review Board of the University Wisconsin-Madison School of Medicine and Public Health. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
VB: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. KE: Writing – review & editing. SC: Investigation, Writing – review & editing. WF: Writing – review & editing. HB: Supervision, Visualization, Writing – review & editing. JM: Formal Analysis, Visualization, Writing – review & editing. MH: Formal Analysis, Methodology, Visualization, Writing – review & editing. KP: Supervision, Visualization, Writing – review & editing.
The authors declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the NIH K12 Wisconsin Multidisciplinary Urologic Research Career Development Program 2K12DK100022-06 and the Texas Pediatric Society Foundation Grant from 2020–2021.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Tack LJW, Springer A, Riedl S, Tonnhofer U, Hiess M, Weninger J, et al. Adolescent and young adult urogenital outcome following childhood hypospadias repair: perfection revisited. J Urol. (2021) 206:734–44. doi: 10.1097/JU.0000000000001869
2. Long CJ, Chu DI, Tenney RW, Morris AR, Weiss DA, Shukla AR, et al. Intermediate-term followup of proximal hypospadias repair reveals high complication rate. J Urol. (2017) 197:852–8. doi: 10.1016/j.juro.2016.11.054
3. McNamara ER, Schaeffer AJ, Logvinenko T, Seager C, Rosoklija I, Nelson CP, et al. Management of proximal hypospadias with 2-stage repair: 20-year experience. J Urol. (2015) 194:1080–5. doi: 10.1016/j.juro.2015.04.105
4. Williams VW, Finkelstein JB. Speaking and listening: the importance of stakeholder engagement in quality improvement in pediatric urology. J Pediatr Urol. (2023) 19:792–9. doi: 10.1016/j.jpurol.2023.08.017
5. Smith AB, Chisolm S, Deal A, Spangler A, Quale DZ, Bangs R, et al. Patient-centered prioritization of bladder cancer research. Cancer. (2018) 124:3136–44. doi: 10.1002/cncr.31530
6. Struwe S, Thibadeau J, Kelly MS, Widener-Burrows D. Establishing the first community-centered Spina Bifida research agenda. J Pediatr Urol. (2022) 18:800.e1–7. doi: 10.1016/j.jpurol.2022.06.014
7. Bhatia VP, Mittal AG, Austin PF, Hilliard ME. The hypospadias-specific health-related quality of life conceptual framework: a scoping review of the literature. Qual Life Res. (2021) 30:1537–46. doi: 10.1007/s11136-021-02773-w
8. Bhatia V, Cannon S, Patel AN, Brown HW, Farhat WA, Hilliard ME. Understanding health-related quality of life after hypospadias repair: a qualitative study with Pre-adolescent males and parents. J Pediatr Urol. (2024), in press. doi: 10.1016/j.jpurol.2024.08.011
9. Anders ME, Evans DP. Comparison of PubMed and Google Scholar literature searches. Respir Care. (2010) 55:578–83.20420728
10. Giustini D, Boulos MN. Google Scholar is not enough to be used alone for systematic reviews. Online J Public Health Inform. (2013) 5:214. doi: 10.5210/ojphi.v5i2.4623
11. Hadidi AT, Fawzy M, Sennert M, Wirmer J. The natural (non-invasive) erection test: is it a reliable alternative to the artificial erection test? J Pediatr Urol. (2023) 19:702–7. doi: 10.1016/j.jpurol.2023.08.009
12. Rourke K, Braga LH. Transitioning patients with hypospadias and other penile abnormalities to adulthood: what to expect? Can Urol Assoc J. (2018) 12:S27–33. doi: 10.5489/cuaj.5227
13. Gulseth E, Urdal A, Andersen MH, Falk RS, Aksnes G, Emblem R, et al. Sexual well-being and penile appearance in adolescents operated for distal hypospadias in childhood. J Pediatr Urol. (2023) 19:293.e1–8. doi: 10.1016/j.jpurol.2023.03.001
14. Schober JM, Meyer-Bahlburg HF, Dolezal C. Self-ratings of genital anatomy, sexual sensitivity and function in men using the “self-assessment of genital anatomy and sexual function, male” questionnaire. BJU Int. (2009) 103:1096–103. doi: 10.1111/j.1464-410X.2008.08166.x
15. Ryu DS, Cho WY, Chung JM, Kang DI, Lee SD, Park S. Comparison of penile length at 6–24 months between children with unilateral cryptorchidism and a healthy normal cohort. Investig Clin Urol. (2018) 59:55–60. doi: 10.4111/icu.2018.59.1.55
16. Stancampiano MR, Suzuki K, O'Toole S, Russo G, Yamada G, Faisal Ahmed S. Congenital micropenis: etiology and management. J Endocr Soc. (2022) 6:bvab172. doi: 10.1210/jendso/bvab172
17. Media LM, Fauske L, Sigurdardottir S, Feragen KJB, Heggeli C, Waehre A. ‘It was supposed to be a secret’: a study of disclosure and stigma as experienced by adults with differences of sex development. Health Psychol Behav Med. (2022) 10:579–95. doi: 10.1080/21642850.2022.2102018
18. Cheng JW, Fernandez N, Shnorhavorian M, Merguerian PA, Kieran K. Engagement of common pediatric urologic conditions on social media. J Pediatr Urol. (2022) 18:236.e1–7. doi: 10.1016/j.jpurol.2021.12.003
19. Lee P, Schober J, Nordenstrom A, Hoebeke P, Houk C, Looijenga L, et al. Review of recent outcome data of disorders of sex development (DSD): emphasis on surgical and sexual outcomes. J Pediatr Urol. (2012) 8:611–5. doi: 10.1016/j.jpurol.2012.10.017
20. Ortqvist L, Engberg H, Strandqvist A, Nordenstrom A, Holmdahl G, Nordenskjold A, et al. Psychiatric symptoms in men with hypospadias—preliminary results of a cross-sectional cohort study. Acta Paediatr. (2019) 108:1156–62. doi: 10.1111/apa.14658
21. Blankstein U, McGrath M, Randhawa H, Braga LH. A survey of parental perceptions and attitudes related to disclosure in hypospadias repair. J Pediatr Urol. (2022) 18:178.e1–7. doi: 10.1016/j.jpurol.2022.01.009
22. Rolston AM, Gardner M, Vilain E, Sandberg DE. Parental reports of stigma associated with child’s disorder of sex development. Int J Endocrinol. (2015) 2015:980121. doi: 10.1155/2015/980121
23. Toufaily MH, Roberts DJ, Westgate MN, Hunt AT, Holmes LB. Hypospadias, intrauterine growth restriction, and abnormalities of the placenta. Birth Defects Res. (2018) 110:122–7. doi: 10.1002/bdr2.1087
24. Chan KH, Panoch J, Carroll A, Wiehe S, Cain MP, Frankel R. Knowledge gaps and information seeking by parents about hypospadias. J Pediatr Urol. (2020) 16:166.e1–8. doi: 10.1016/j.jpurol.2020.01.008
25. Chan KH, Misseri R, Cain MP, Whittam B, Szymanski K, Kaefer M, et al. Provider perspectives on shared decision-making regarding hypospadias surgery. J Pediatr Urol. (2020) 16:307–15. doi: 10.1016/j.jpurol.2020.03.015
26. Phillips L, Dennermalm N, Ortqvist L, Engberg H, Holmdahl G, Fossum M, et al. A qualitative content analysis of the experience of hypospadias care: the importance of owning your own narrative. Front Pediatr. (2023) 11:1118586. doi: 10.3389/fped.2023.1118586
27. Duarsa GWK, Pratiwi DA, Tirtayasa PW, Yudiana W, Santosa KB, Oka AAG, et al. Functional and cosmetic urethroplasty outcome, emotional stress after genital examination, post traumatic stress disorder, and ages at the time of urethroplasty as potential risk factor causing psychosocial disorder of hypospadia children. Open Access Maced J Med Sci. (2019) 7:1452–5. doi: 10.3889/oamjms.2019.227
28. Keays MA, Starke N, Lee SC, Bernstein I, Snodgrass WT, Bush NC. Patient reported outcomes in preoperative and postoperative patients with hypospadias. J Urol. (2016) 195:1215–20. doi: 10.1016/j.juro.2015.11.066
29. Chang E, Nicassio L, Whalen J, Cheng J, Merguerian P, Lendvay TS, et al. Understanding why caregivers call after ambulatory pediatric urologic surgery. Can J Urol. (2022) 29:11243–8.35969728
30. Snodgrass P, Snodgrass W, Bush N. Parental concerns of boys with hypospadias. Res Rep Urol. (2021) 13:73–7. doi: 10.2147/RRU.S285626
31. van der Horst HJ, de Wall LL. Hypospadias, all there is to know. Eur J Pediatr. (2017) 176:435–41. doi: 10.1007/s00431-017-2864-5
32. Gul M, Hildorf S, Silay MS. Sexual functions and fertility outcomes after hypospadias repair. Int J Impot Res. (2021) 33:149–63. doi: 10.1038/s41443-020-00377-5
33. Tasian GE, Ellison JS. Measuring patient-centered outcomes: the need to move beyond quality of life. J Pediatr Urol. (2021) 17:444. doi: 10.1016/j.jpurol.2021.03.033
Keywords: hypospadias, stakeholders, engagement, holistic care, adolescent and youth
Citation: Bhatia VP, Ebert K, Cannon S, Farhat WA, Brown HW, Mahoney J, Hilliard ME and Penniston KL (2024) Call the experts: identifying stakeholders in the long-term care of youth with hypospadias. Front. Pediatr. 12:1445205. doi: 10.3389/fped.2024.1445205
Received: 6 June 2024; Accepted: 7 October 2024;
Published: 30 October 2024.
Edited by:
Yuval Bar-Yosef, Dana-Dwek Children's Hospital, IsraelReviewed by:
Earl Cheng, Ann & Robert H. Lurie Children's Hospital of Chicago, United StatesCopyright: © 2024 Bhatia, Ebert, Cannon, Farhat, Brown, Mahoney, Hilliard and Penniston. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vinaya P. Bhatia, YmhhdGlhQHVyb2xvZ3kud2lzYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.