- Department of Neonatology, Affiliated Hospital, Inner Mongolia Medical University, Hohhot, China
Objective: The study aimed to compare the efficacy and safety of different noninvasive ventilation (NIV) modalities as primary respiratory support following extubation in Neonatal Respiratory Distress Syndrome (NRDS).
Methods: A search was conducted in PubMed, Embase, Cochrane, Web of Science, China National Knowledge Network (CNKI), Wanfang database, VIP, and Chinese Biomedical Literature databases with a search time limit of April 2024 for the year of construction, and included randomized controlled clinical trials of different modes of noninvasive respiratory support after extubation in NRDS. The primary outcome indicators were the need for re-tracheal intubation within 72 h of extubation on noninvasive ventilatory support and carbon dioxide retention (PCO2) 24 h after extubation. Secondary outcome indicators included the incidence of bronchopulmonary dysplasia (BPD), nasal injury, pneumothorax, intraventricular hemorrhage (IVH) or periventricular white matter softening (PVL), retinopathy of prematurity (ROP), necrotizing enterocolitis (NEC), and mortality rate. A systematic review and network meta-analysis of the literature was performed by two investigators who screened, extracted, and evaluated the quality of the data. A systematic review and network meta-analysis were then performed using R software.
Results: A total of 23 studies involving 2,331 neonates were analyzed. These studies examined four noninvasive respiratory modalities: continuous positive airway pressure ventilation (NCPAP), noninvasive intermittent positive pressure ventilation (NIPPV), bi-level positive airway pressure ventilation (N-BiPAP), and noninvasive high-frequency oscillatory ventilation (NHFOV). Results indicated that NHFOV, NIPPV, and N-BiPAP were significantly more effective than NCPAP in reducing the risk of reintubation (all P < 0.05), with NHFOV being the most effective. For carbon dioxide clearance, NHFOV outperformed both NIPPV and NCPAP (P < 0.05). Regarding the reduction of bronchopulmonary dysplasia (BPD) incidence, NHFOV and NIPPV showed a significant advantage over NCPAP.
Conclusions: This network meta-analysis (NMA) suggested that NHFOV is the most effective mode of noninvasive respiratory support post-extubation, while NCPAP is the least effective. However, these findings should be interpreted with caution due to the limited number and quality of the studies included.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/#recordDetails, identifier (CRD42024544886).
1 Introduction
Neonatal Respiratory Distress Syndrome (NRDS) is a prevalent respiratory crisis in neonatology, which is defined as acute respiratory failure with extensive alveolar atrophy damage exudation in both lungs due to pulmonary surfactant (PS) deficiency (1, 2), manifesting as progressive dyspnoea, cyanosis, and respiratory failure within the first few hours after birth, predominantly in preterm infants. The incidence of NRDS increases with decreasing gestational age. Treatment primarily involved postnatal mechanical ventilation using an autonomous ventilator to enhance the respiratory status of the neonate. In recent years, the use of invasive mechanical ventilation (IMV) has significantly enhanced survival rates in NRDS, however, it also heightens the risk of ventilator-associated complications, particularly among infants requiring repeated intubations or prolonged periods of IMV. Consequently, to enhance survival quality, early extubation to noninvasive respiratory support (NRS) has become a critical focus (3). NRS modalities commonly utilized in neonatal care include continuous positive airway pressure ventilation (NCPAP), noninvasive intermittent positive pressure ventilation (NIPPV), bi-level positive airway pressure ventilation (N-BiPAP), and noninvasive high-frequency oscillatory ventilation (NHFOV). NCPAP delivers a constant positive pressure to the airways, primarily through a nasal cannula or mask, to maintain alveolar expansion and prevent collapse. In contrast, NIPPV adds periodic bursts of higher pressure on top of the baseline CPAP, aiding the infant's spontaneous breathing, increasing tidal volume, and enhancing overall ventilation. N-BiPAP (Nasal Bi-level Positive Airway Pressure) offers two distinct pressure levels—a higher pressure during inspiration (IPAP) and a lower pressure during expiration (EPAP). This approach improves ventilation and oxygenation, making it particularly effective for infants who need extra inspiratory support. NHFOV is a newer noninvasive support method that delivers rapid, small breaths through high-frequency oscillations, helping to keep the airways open and improve carbon dioxide clearance (4–6). The physiological mechanisms underlying these NRS modalities vary significantly, and their relative merits remain under debate (7). Although numerous systematic reviews have compared the effects of these modalities on post-extubation ventilatory support, a comprehensive evaluation through a network meta-analysis (NMA) has not yet been conducted. Therefore, this systematic review and NMA aimed to assess the effectiveness and safety of various NRS modalities—NCPAP, NIPPV, N-BiPAP, and NHFOV-through a network meta-analysis. Effectiveness was assessed primarily by successful extubation rates and reduced reintubation rates, while safety focused on the incidence of ventilator-related complications such as bronchopulmonary dysplasia, nasal injury, air leaks, and cerebral hemorrhage. This study aimed to provide an evidence-based basis for selecting the optimal mode of noninvasive ventilation after extubation in preterm infants.
2 Methods
2.1 Register
In this study, we compared the efficacy and safety of various noninvasive ventilation strategies for respiratory support post-extubation in NRDS, utilizing a systematic evaluation protocol registered in the PROSPERO registry (CRD42024544886). This review adhered to the PRISMA guidelines for network meta-analyses (8).
2.2 Search strategy
A comprehensive search was conducted for clinical randomized controlled trials on NRDS in databases including PubMed, Embase, Cochrane, Web of Science, CNKI, Wanfang Database, VIP, and China Biomedical Literature Database from their inception until April 2024. This search focused on trials that adhered to the established diagnostic criteria for NRDS and explored noninvasive ventilation strategies. The search was guided by the PICOS framework: (P) Population: neonates diagnosed with NRDS; (I) Intervention: noninvasive ventilation strategies; (C) Comparison: the effectiveness and safety of NHFOV, NIPPV, NCPAP, and N-BiPAP in respiratory support for neonates post-extubation; (O) Outcome: 1. The primary outcome: re-tracheal intubation within 72 h of extubation on noninvasive ventilatory support; 2. carbon dioxide retention (PCO2) 24 h after extubation. Secondary outcome: the incidence of bronchopulmonary dysplasia (BPD), nasal injury, pneumothorax, intraventricular hemorrhage (IVH) or periventricular white matter softening (PVL), retinopathy of prematurity (ROP), necrotizing enterocolitis (NEC) and mortality rate; (S) Study Type: Randomized controlled trials. Details of the search terms are available in the Additional Materials section (Supplementary Table S1).
2.3 Inclusion criteria and exclusion criteria
Inclusion criteria: (1) Study subjects: neonates aged 0–28 days postnatally; (2) diagnosed with NRDS (9): 1. Clinical manifestations: These include shortness of breath (>60 breaths/min), nasal flaring, expiratory groaning, subpectoral or intercostal depression, and bruising. 2. Chest imaging: chest radiographs show typical “hairy glass-like” changes, accompanied by air bronchial signs. 3. Blood gas analysis: hypoxaemia (PaO2 < 50 mmHg) with or without metabolic or respiratory acidosis. 4. Preterm labour: gestational age < 37 weeks, and the risk of RDS is higher the earlier the birth; (3) initially intubated and provided invasive ventilatory support for NRDS, followed by noninvasive support upon meeting extubation standards. Exclusion criteria: (1) studies lacking clear diagnostic criteria; (2) studies involving congenital anomalies (e.g., congenital diaphragmatic hernia, congenital lung anomalies, congenital heart disease, except for patent foramen ovale and arterial ductus arteriosus) or infectious shock; (3) prophylactic, retrospective studies, and case reports; (4) studies with unclear endpoints or those that failed to provide valid data for analysis; (5) studies published multiple times.
2.4 Noninvasive ventilation modes categories
Ventilation strategies in the included randomized controlled trials were classified into four models:
1. NHFOV; 2. NIPPV; 3. NCPAP; 4. N-BiPAP
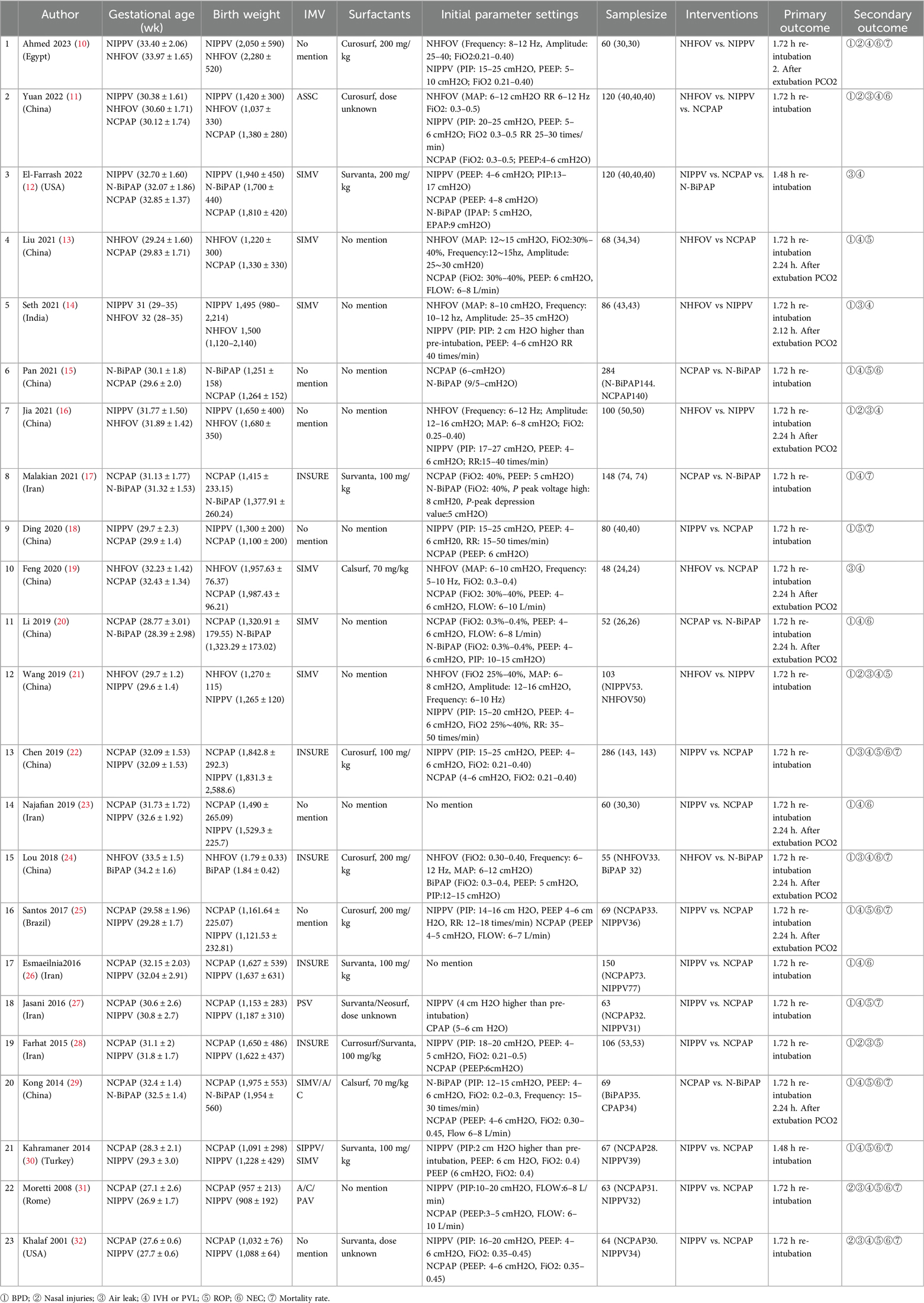
The parameter settings for each mode, including settings used during ventilation and those applied after meeting extubation criteria (Table 1).
2.5 Study selection
In this study, two uniformly trained researchers independently performed the initial screening and selected studies based on the inclusion and exclusion criteria. In the event of a disagreement during the screening process, a third researcher resolved whether to include or exclude the studies.
2.6 Risk of bias of individual studies
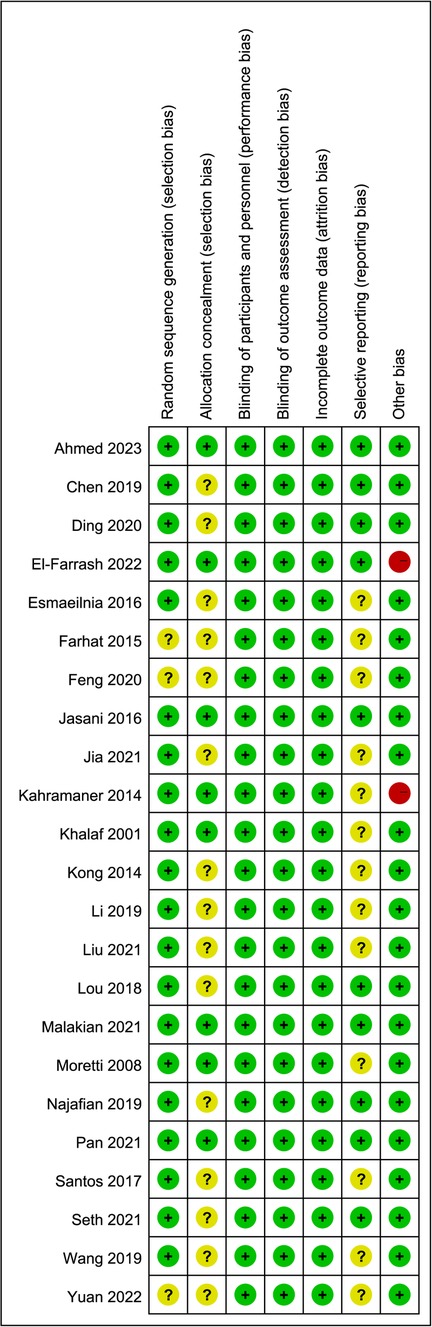
To evaluate the quality of the included studies, this study employed the Cochrane Risk of Bias Tool for bias assessment (33), which assesses several criteria including randomized sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources of bias. Trials were categorized into three levels based on the number of bias-prone components identified: high risk (five or more), some concerns (three or four), and low risk (two or fewer). Due to the impracticality of blinding participants in the ventilation strategy intervention protocol, all studies were deemed at high risk for “subject blinding,” this component was therefore excluded from the overall risk of bias evaluation.
2.7 Data extraction
Baseline data extracted for this study included: the first author, publication date, ventilation strategy, number of cases, gender, birth weight, gestational age, initial mode parameter settings, and data related to outcome indicators. The study incorporated four mechanical ventilation strategies: NCPAP, NIPPV, N-BiPAP, and NHFOV. Primary outcome indicators were the need for re-tracheal intubation within 72 h post-noninvasive respiratory support and PCO2 retention 24 h post-extubation. Secondary outcome indicators included the incidence of bronchopulmonary dysplasia (BPD), nasal injury, air leaks, intraventricular hemorrhage (IVH) or periventricular leukomalacia (PVL), retinopathy of prematurity (ROP), necrotizing enterocolitis (NEC) and mortality rate.
2.8 Statistical analysis
This study assessed the safety of each ventilation treatment strategy using risk ratios (RR) with 95% credible intervals (CrIs) addressing both dichotomous and continuous data to maximize accuracy. Literature that met the inclusion criteria was subjected to Cochrane bias assessment using Revman 5.3 software. Network geometry was evaluated using a network diagram in R software (Version-R 4.3.3) (34), where the size of the nodes reflects the number of subjects in each intervention, and the thickness of the lines between nodes indicates the number of studies in each comparison. Model convergence was assessed with Gelman-Rubin plots, trace, and density plots. Inconsistencies were examined through node splitting. Additionally, a paired meta-analysis of direct evidence across different modes of noninvasive respiratory support was conducted, and heterogeneity was assessed using the I2 statistic and the Cochran Q-test. The results of the NMA were presented as 95% CIs in league matrix tables and forest plots. The league matrix illustrates the RR of the intervention outcomes with rows vs. columns in the lower triangles and vice versa in the upper triangles. All interventions were ranked for outcomes using the Surface Under the Cumulative Ranking curve (SUCRA), an index ranging from 0 (least effective intervention) to 1 (most effective intervention). Interpretation of SUCRA should consider the 95% CrIs and the quality of evidence. The confidence in the final estimates for all the outcomes was assessed using the GRADE approach as recommended by the GRADE working group (8).
3 Results
3.1 Screening process for inclusion of studies
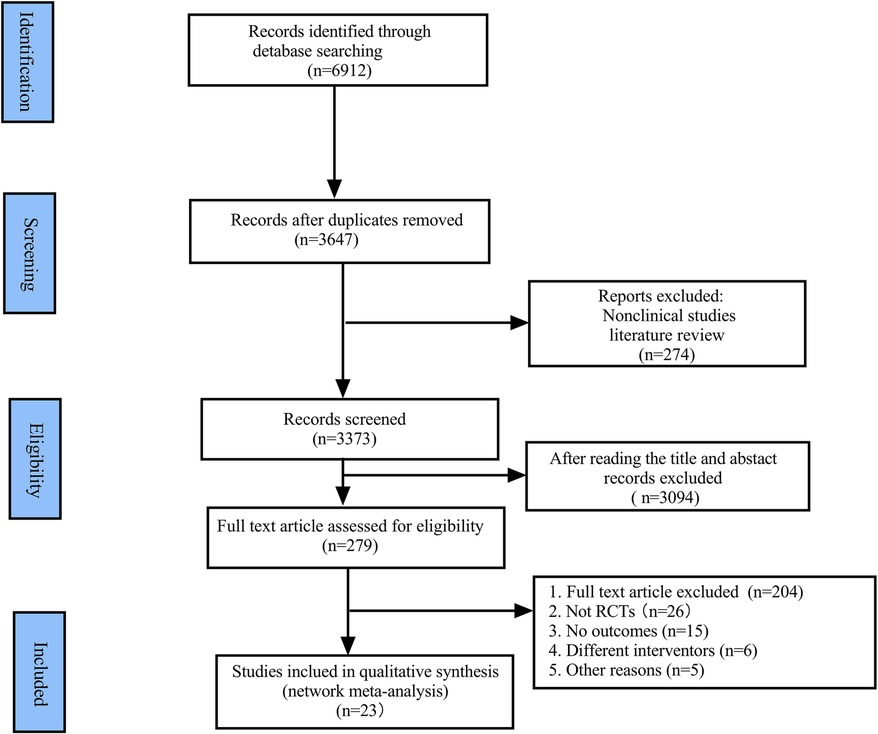
A total of 6,912 studies were initially identified from various databases, with 23 studies ultimately included after excluding those for relevant reasons. The PRISMA flow chart is depicted in Figure 1.
3.2 Characteristics of the included studies
Table 1 outlines the general characteristics of the included studies, comprising 2,331 newborns across 23 studies, which include 21 two-armed trials and 2 three-armed trials. The geographic distribution of these trials included 17 in Asia, 2 in North America, 2 in Europe, 1 in South America, and 1 in Africa. Study durations varied from 1 year to over 3 years. The subjects were predominantly preterm infants diagnosed with NRDS at birth, with gestational ages ranging from 28 to 35 weeks. 14 studies involved neonates who had received surfactant treatment prior to randomization into subgroups. In the majority of these studies, treatment failures and reintubations occurred within 72 h of randomization. The specific NRS setup parameters employed are detailed in Table 1.
3.3 Risk of bias assessment of included studies
Three studies were assessed as having a moderate risk of bias, and 15 were considered to have a low risk of bias, primarily due to issues with randomized sequence generation and allocation concealment. Due to the nature of the interventions, it was impossible to blind personnel and outcome assessors in all trials. The overall risk of bias is illustrated in Figure 2.
3.4 Primary outcomes
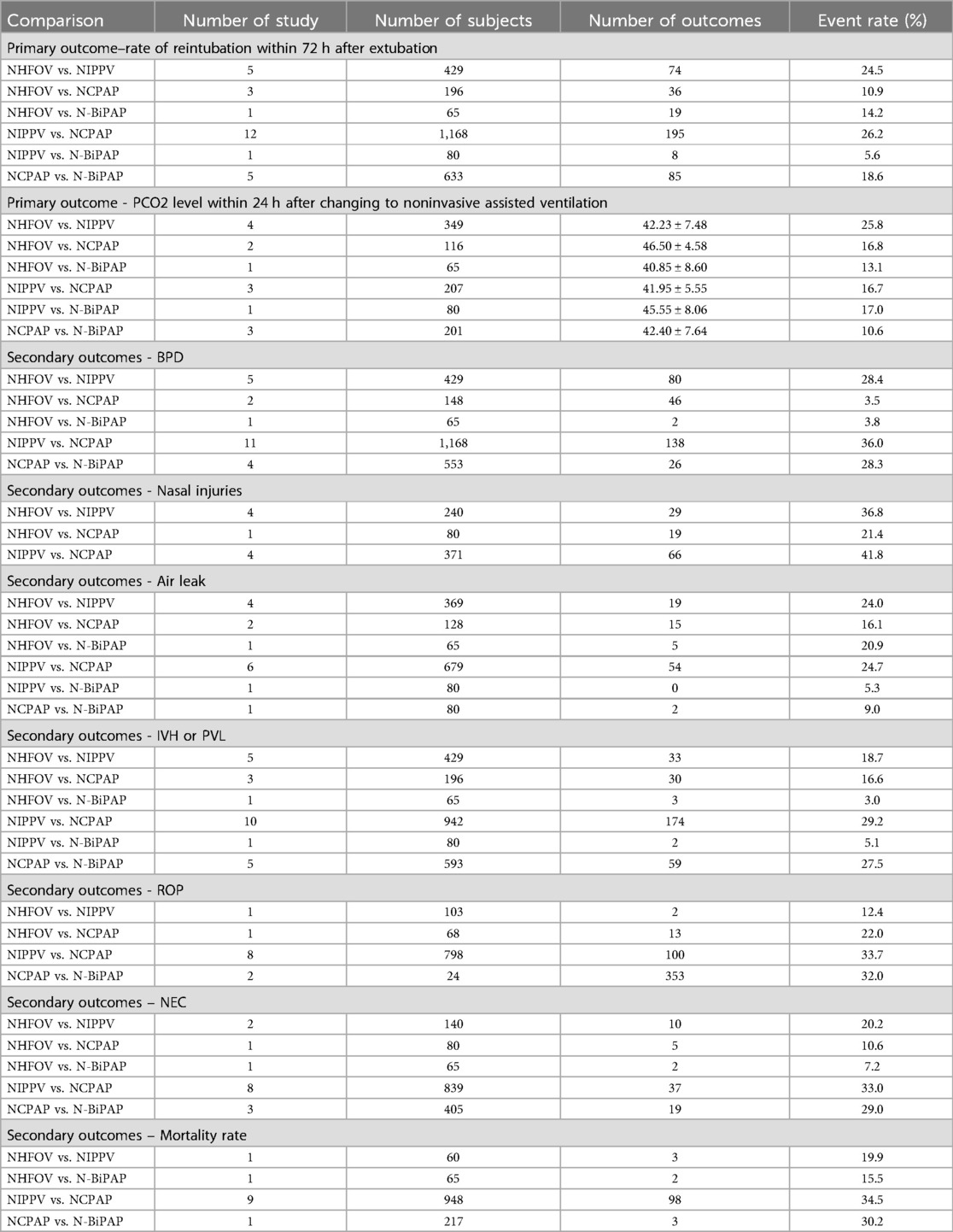
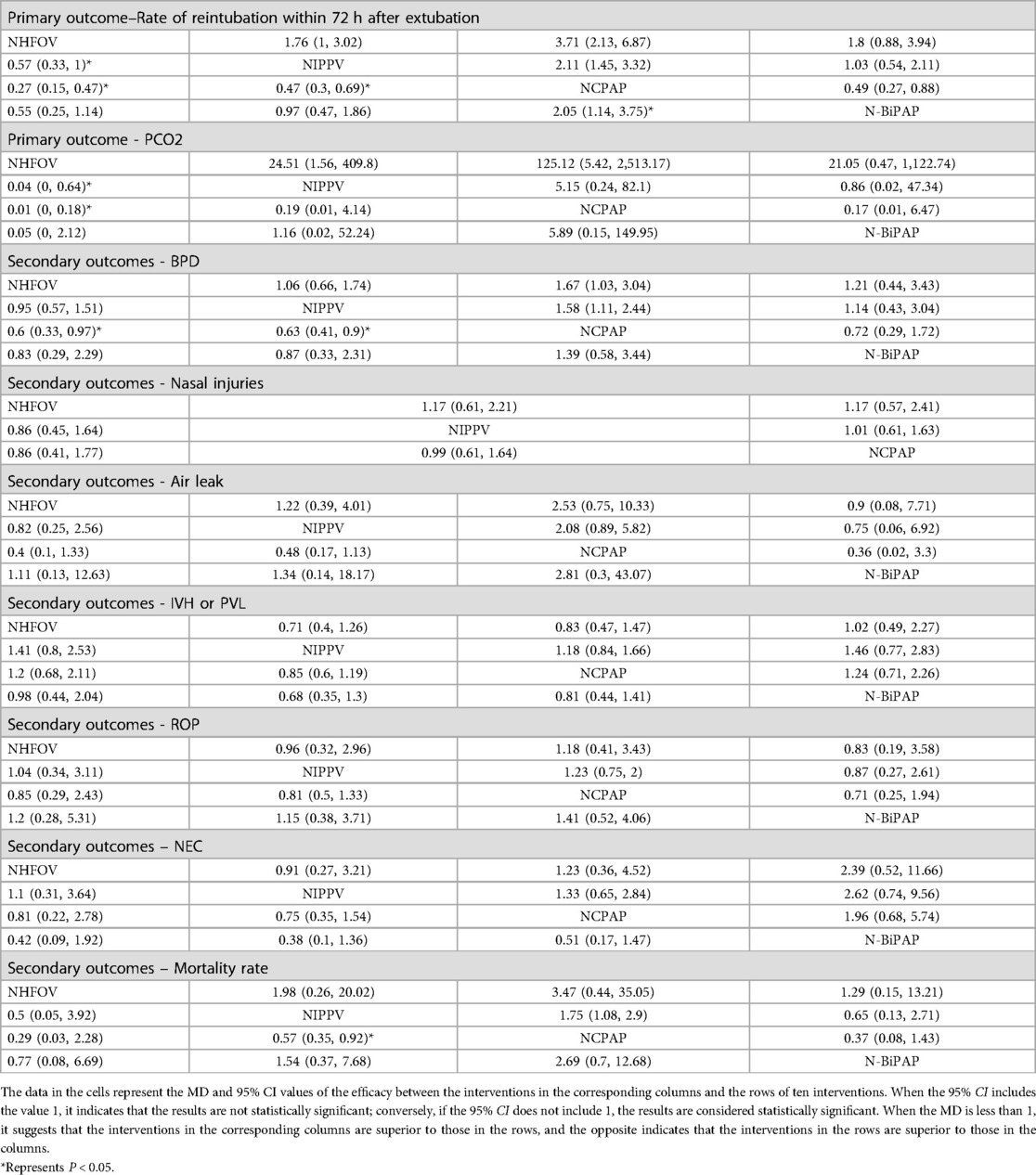
3.4.1 Rate of reintubation within 72 h after extubation
A total of 23 studies (10–32) involving 2,331 newborns were analyzed, documenting 417 events within the network (Table 2). Closed loops among all interventions were depicted in the network relationship diagram (Figure 3), with the majority of data, contributing 26.2%, coming from comparisons between NIPPV and NCPAP (Table 2; Supplementary Material). A local inconsistency test using node splitting indicated P > 0.05, and data were analyzed using a consistency model. Potential Scale Reduction Factor (PSRF) is a metric in Bayesian statistics used to assess the convergence of the Markov Chain Monte Carlo (MCMC) algorithm. The PSRF for all three outcome indicators converged to 1, suggesting robust convergence (Supplementary Material). Separate heterogeneity tests on the original studies with two or more contributions showed significant heterogeneity between NCPAP and N-BiPAP (I2 = 54.8), though still within acceptable limits; no significant heterogeneity was noted among the remaining studies. Network meta-analysis revealed that NHFOV [0.27 (0.15,0.47)], NIPPV [0.47 (0.30,0.69)], and N-BiPAP [0.49 (0.27,0.88)] significantly reduced the risk of reintubation compared to NCPAP (Figure 4; Table 3). The SUCRA values for the four ventilation modes were 0.97, 0.52, 0.00, and 0.50, respectively, ranking the effectiveness in reducing reintubation post-extubation from highest to lowest as NHFOV > NIPPV > N-BiPAP > NCPAP. This suggests that NHFOV was the most effective mode for post-extubation respiratory support, offering the greatest likelihood of reducing reintubation (Figure 5).
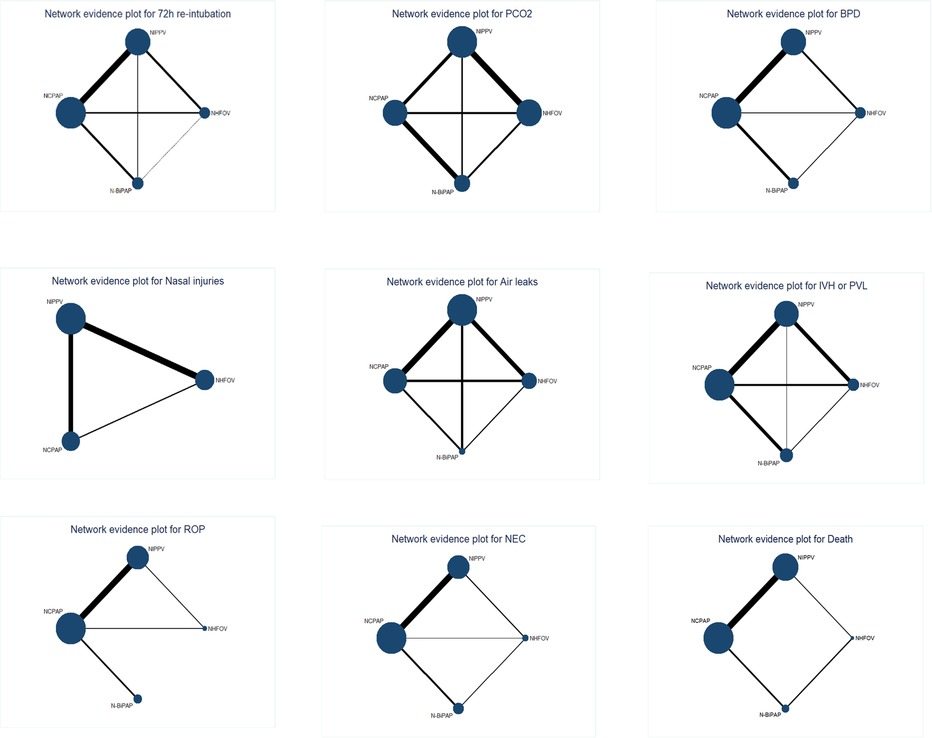
Figure 3. Geometry of the network for the outcomes. The size of the nodes reflects the number of studies and total number of patients involved in each intervention. The thickness of the edges indicates the number of trials directly compared.
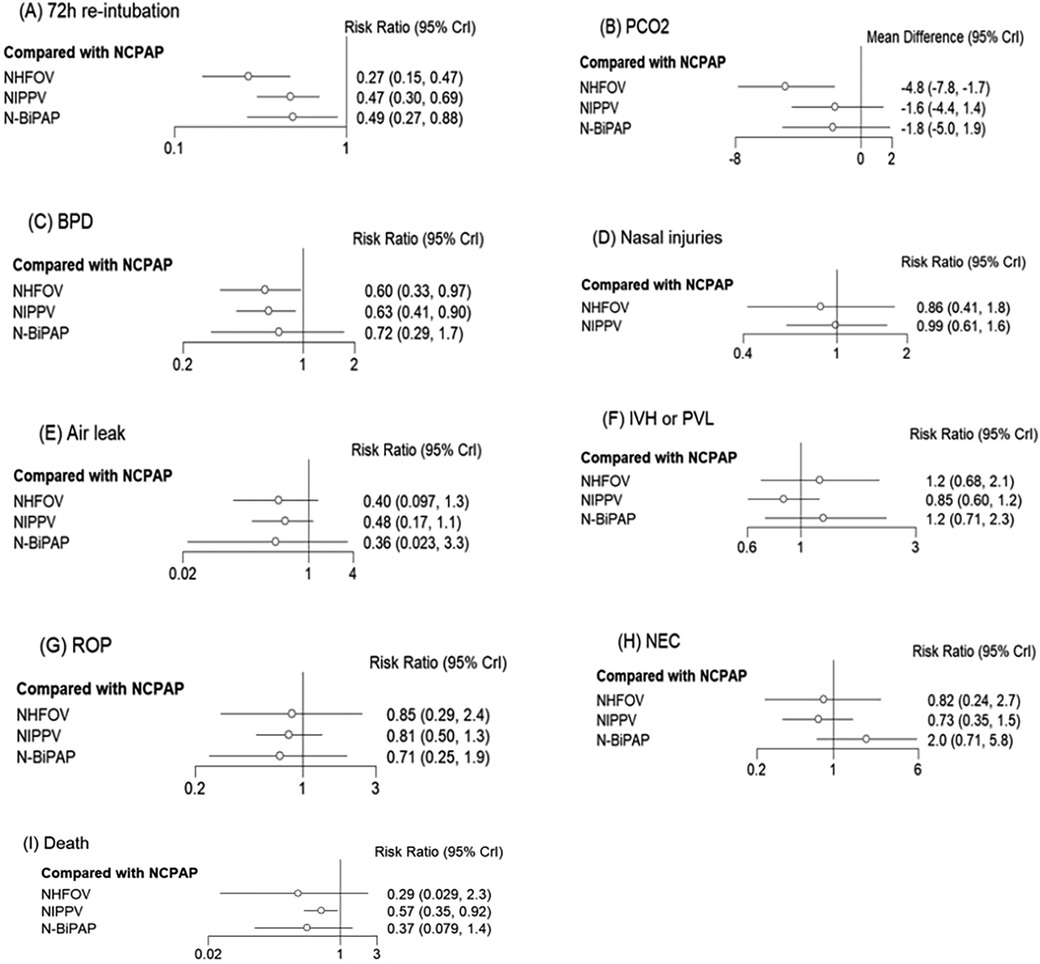
Figure 4. Forest plots depicting the RR (95% CrI) for different NRS modalities: (A) 72 h re-intubation, (B) PCO2, (C) BPD, (D) Nasal injuries, (E) Air leak, (F) IVH or PVL, (G) ROP, (H) NEC, (I) Death.
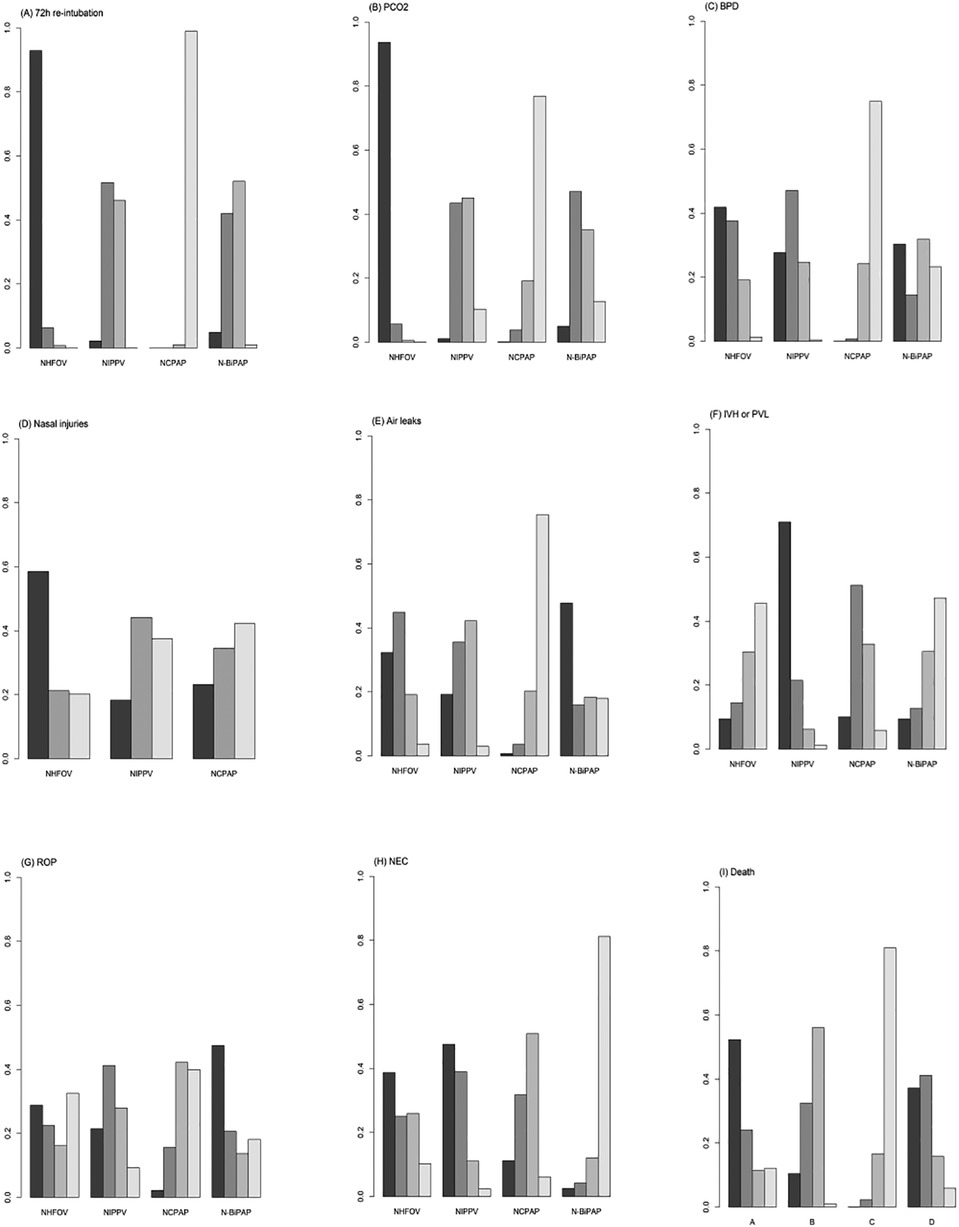
Figure 5. SUCRAs plots for the outcomes: (A) 72 h re-intubation, (B) PCO2, (C) BPD, (D) Nasal injuries, (E) Air leaks, (F) IVH or PVL, (G) ROP, (H) NEC, and (I) Death.
3.4.2 PCO2 level within 24 h after changing to noninvasive assisted ventilation
A total of 12 studies (10, 12–14, 16, 19–21, 24, 29, 31, 32) involving 898 newborns were analyzed, demonstrating closed loops between all interventions as depicted in the network diagram (Figure 3). A significant portion of the data, representing 25.8%, was derived from comparisons between NHFOV and NIPPV (Table 2; Supplementary Material). A local inconsistency test using node splitting indicated P > 0.05, and the data were analyzed using a consistency model. The PSRF for all three outcome indicators converged to 1, suggesting good convergence (Supplementary Material). Heterogeneity was assessed separately for original studies with two or more contributions. Significant heterogeneity was observed, which might relate to variations in the timing of blood gas analysis and the types of diseases among the studies. The results of the network meta-analysis demonstrated that NHFOV was more effective than both NIPPV and NCPAP in facilitating carbon dioxide removal (both P < 0.05). However, no significant difference was observed between NIPPV and NCPAP (P > 0.05). No significant differences were found among the other three modes of respiratory support, excluding NHFOV (all P > 0.05) (Figure 4; Table 3). The SUCRA values for the four ventilation modes were 0.98, 0.45, 0.09, and 0.48, respectively, ranking the effectiveness in removing carbon dioxide post-extubation from highest to lowest as NHFOV>N-BiPAP>NIPPV>NCPAP. This highlights NHFOV's superiority in carbon dioxide removal compared to other ventilation strategies (Figure 5).
3.5 Secondary outcomes
3.5.1 BPD
A total of 21 studies (10, 11, 13–18, 20–30) involving 2,163 children were analyzed. The results of the network meta-analysis indicated that NHFOV and NIPPV significantly reduced the odds of BPD compared to NCPAP, while no statistically significant difference was observed with N-BiPAP (P > 0.05). No significant differences were found among the other modes of respiratory support (all P > 0.05) (Figure 4; Table 3). The SUCRA values for NHFOV, NIPPV, NCPAP, and N-BiPAP were 0.73, 0.67, 0.08, and 0.50, respectively, suggesting a descending efficacy in reducing BPD from NHFOV to N-BiPAP to NIPPV to NCPAP (Figure 5).
3.5.2 Nasal injuries
A review of seven studies (10, 11, 16, 21, 28, 31, 32) involving 621 children showed no statistically significant differences between the interventions (P > 0.05) (Figure 4; Table 3). The SUCRA values for NHFOV, NIPPV, NCPAP, and N-BiPAP were 0.68, 0.41, and 0.41, respectively (Figure 5).
3.5.3 Air leakage
A total of 11 studies (11, 12, 14, 16, 19, 21, 22, 24, 28, 31, 32) involving 1,161 children were analyzed. The results of the network meta-analysis indicated no statistically significant differences between the interventions (P > 0.05) (Figure 4; Table 3). The SUCRA values for NIPPV, NCPAP, and N-BiPAP were 0.68, 0.57, 0.09 and 0.65, respectively (Figure 5).
3.5.4 IVH or PVL
A total of 21 studies (10–17, 19–27, 29–32) including 2,145 children were reviewed. The network meta-analysis revealed no statistically significant differences between the interventions (P > 0.05) (Figure 4; Table 3). The SUCRA values for NHFOV, NIPPV, NCPAP, and N-BiPAP were 0.30, 0.87, 0.56, and 0.27, respectively (Figure 5).
3.5.5 ROP, NEC
Network meta-analysis revealed no significant differences between the interventions (P > 0.05) (Figure 4; Table 3), and the ordination diagram is depicted in Figure 5.
3.5.6 Mortality rate
The results of the network meta-analysis showed that NIPPV significantly reduced mortality compared to NCPAP, with no significant differences found between the other modes of respiratory support (all P > 0.05) (Figure 4; Table 3).
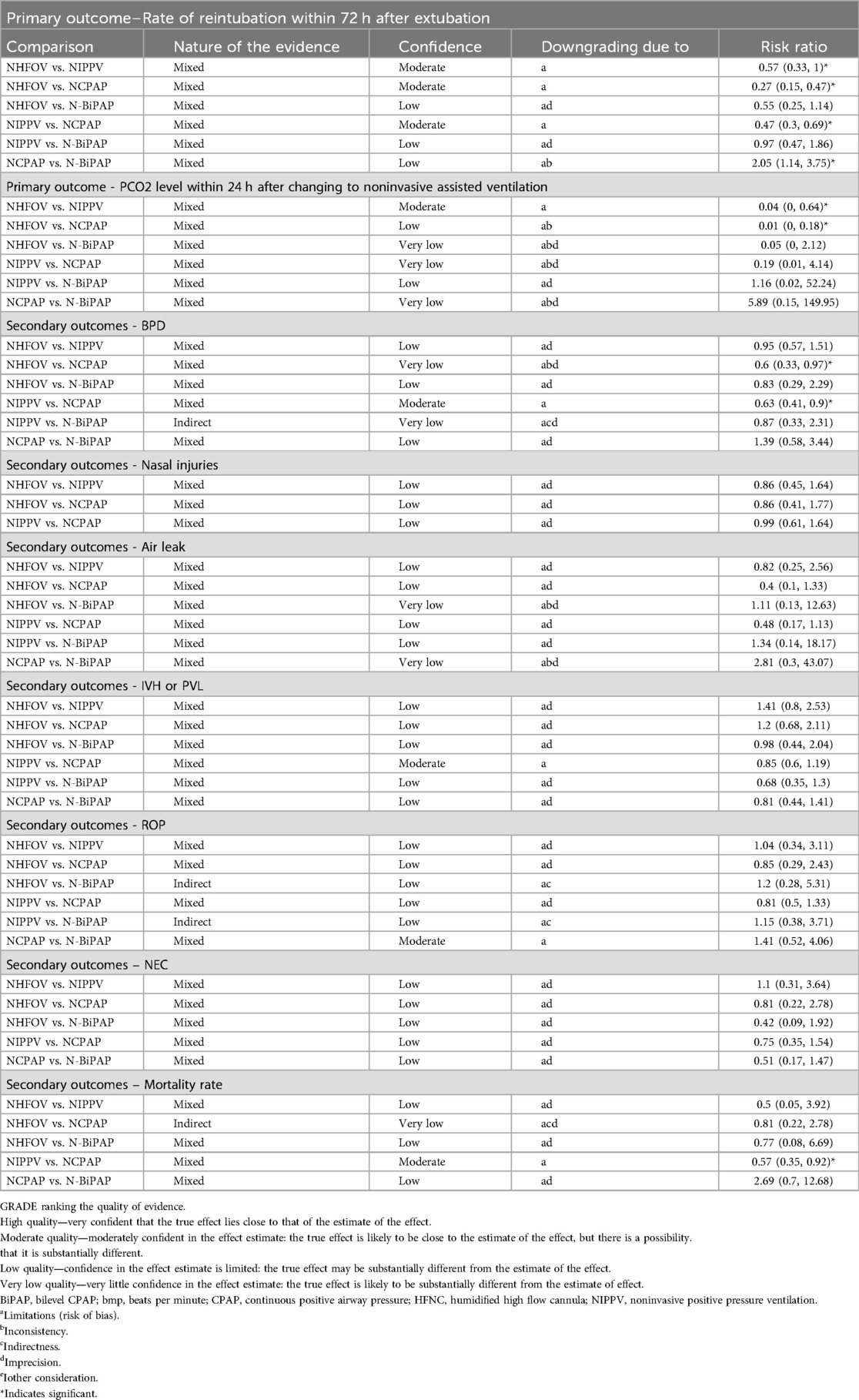
3.5.7 Quality of evidence
The overall confidence level of the network meta-analysis (NMA) effect estimate for reintubation within 72 h was moderate for nasal high-flow oxygen ventilation (NHFOV) compared with noninvasive positive pressure ventilation (NIPPV) and nasal continuous positive airway pressure (NCPAP). The confidence level for CO2 retention within 24 h was rated as moderate for NHFOV vs. NIPPV, and low to very low when directly compared to other interventions. The quality of evidence for all other secondary outcomes ranged from very low to moderate across comparisons. Refer to Table 4 for the quality of evidence for all outcome comparisons.
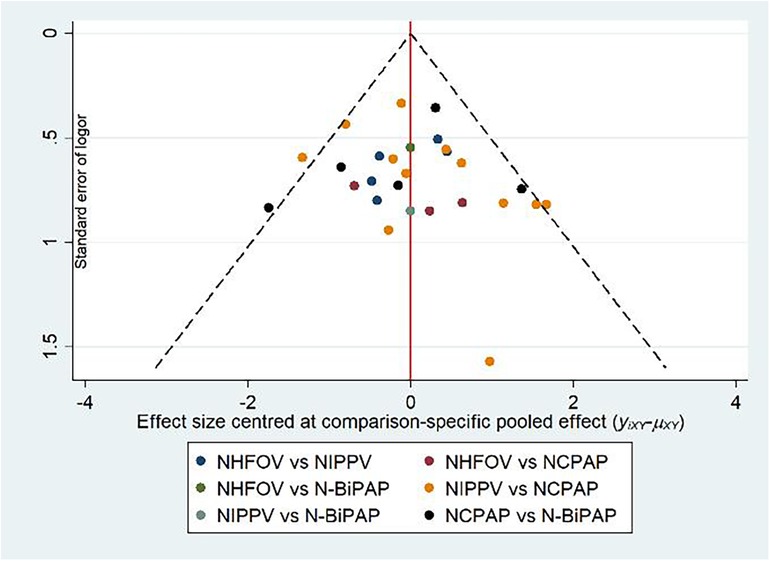
3.5.8 Publication bias test
A corrected one-comparison funnel plot focusing on 72 h reintubation as the primary outcome showed a concentrated scatter in the upper middle with good symmetry, indicating no significant publication bias (Figure 6).
4 Discussion
Currently, mechanical ventilation has a primary treatment modality in NRDS due to its irreplaceable role (35). Critically ill neonates exhibit low resistance, and prolonged mechanical ventilation may increase the risk of ventilator-associated complications such as lung injury and infection (36). Consequently, identifying a safer and more effective noninvasive respiratory support methods post-extubation was crucial. This study evaluated various NRS modalities, focusing on outcomes like reintubation and carbon dioxide retention following extubation in 2,331 neonates across 23 studies.
The results of this NMA study indicated that NHFOV is potentially the most effective NRS mode for post-extubation respiratory support, compared to NIPPV, NCPAP, and N-BiPAP. From biomechanical and physiological perspectives (37), the high-frequency oscillations provided by NHFOV improve lung ventilation homogeneity, minimize ventilation/blood flow mismatch, and may reduce lung injury by stabilizing the ventilation pressure gradient (38). This study supported these findings, showing that NHFOV significantly reduced reintubation risks, enhanced carbon dioxide removal, and lowered the incidence of BPD. Czernik et al. (39) and Seth et al. (14) reported that NHFOV effectively addressed extubation challenges and outperformed NIPPV in reducing CO2 retention. However, Ramaswamy and Wu et al. (40, 41) conclusions are in contrast to this study, where they showed that NIPPV performed best in reducing the need for mechanical ventilation, while high-frequency oscillatory ventilation (nHFOV) was the least effective. This may be due to the fact that the effectiveness of nHFOV has been more widely validated and optimized in recent years with the continuous advancement of nHFOV equipment and techniques, especially in premature infants with respiratory distress syndrome (RDS). Moreover, that study focused on the initial treatment of noninvasive breathing in NRDS, whereas this study focused on the efficacy and safety of noninvasive respiratory support after extubation, and our results added to the existing literature.
The results of this NMA analysis indicated that NIPPV was also employed as a mode of respiratory support post-extubation. Although less effective than NHFOV in preventing reintubation within 72 h, NIPPV significantly reduced the reintubation rates among children with NRDS, demonstrating greater clinical efficacy than NCPAP and N-BiPAP. Ramanathan (42) reported that NIPPV, by incorporating intermittent positive pressure into NCPAP, provides stronger respiratory support and reduces reintubation rates.
In this study, N-BiPAP was shown to significantly decrease the risk of reintubation compared to NCPAP, a finding supported by Victor et al. (43) and consistent with existing literature (32, 44, 45). N-BiPAP may enhance respiratory outcomes by reducing thoracoabdominal asynchrony and airway resistance, dilating the airways with peak inspiratory pressure (PIP), increasing tidal volume and minute ventilation, expanding the collapsed trachea, and enhancing functional residual capacity. Notably, the PaCO2 levels post-extubation were lower with N-BiPAP than with NCPAP, attributed to the effective bi-level airway pressure support of N-BiPAP which stimulates breathing and provides robust respiratory support. However, no significant differences were observed in CO2 clearance compared to other interventions; this could be due to the higher frequency of re-tracheal intubation within 24 h post-extubation in the sickest children in the NCPAP group, which improved respiratory support, making the differences statistically insignificant when compared with the N-BiPAP group.
Although this study indicated that NCPAP may not be as effective as newer noninvasive respiratory support modalities in reducing the risk of reintubation and enhancing carbon dioxide elimination, its significance should not be overlooked. NCPAP, a traditional method in NRDS management, boasts extensive clinical application and research, effectively maintaining alveolar stability by providing continuous positive airflow, which prevents alveolar collapse and enhances lung ventilation (46). Thus, based on current clinical research data, it is recommended that the appropriate NRS mode be selected according to the specific clinical condition of the neonate and the respiratory support required.
Regarding safety, the results of this NMA analysis demonstrated that the NHFOV group significantly lowered the incidence of BPD compared to both the NIPPV and NCPAP groups, aligning with findings by Null (47). However, no significant differences were observed among the intervention groups concerning complications such as air leakage, nasal injury, PVL, IVH, and ROP, suggesting comparable safety across these groups. Consequently, all four noninvasive ventilation strategies were promotable and applicable in clinical settings as effective and safe noninvasive ventilation modes.
In recent years, the INSURE technique has gained increased use in clinical practice, aimed at minimizing the potential harm caused by mechanical ventilation (MV) in neonates. This method markedly reduces the duration of intubation by utilizing a therapeutic approach that involves endotracheal intubation, surfactant administration, and subsequent non-invasive ventilation (NIV) post-extubation. Frequently utilized NIV modes include nasal continuous positive airway pressure (NCPAP), and more recently, nasal intermittent positive pressure ventilation (NIPPV) has also gained widespread adoption in clinical settings. It is also noteworthy that the Laryngeal Mask Airway (LMA) can serve as an effective alternative when mechanical ventilation is not feasible. Studies have demonstrated that LMA not only provides airway support but also facilitates the administration of surfactant, thereby enhancing neonatal lung function without requiring endotracheal intubation. De Bernardo et al. highlighted that delivering surfactant via LMA, while simultaneously monitoring oxygen saturation, is a minimally invasive and effective intervention that facilitates a smoother transition from invasive to noninvasive mechanical ventilation. This approach helps to mitigate the complications associated with invasive mechanical ventilation and enables early initiation of noninvasive support. As a result, LMA may be considered a valuable bridging technique in subsequent treatment strategies, particularly for preterm infants who are not suitable candidates for tracheal intubation (48, 49).
4.1 Shortcomings and limitations of this meta-analysis
Limitations of this NMA included: (1) Variability in the number of studies analyzed for different noninvasive ventilation strategies, with some having fewer interventions and smaller sample sizes. (2) A limited number of NRS modalities were included in this analysis; notably, modalities such as humidified high-flow nasal catheter ventilation (HFNC) were excluded. (3) Inconsistencies were observed in one secondary outcome (air leak). (4) Most of the data in this study were derived from Asian populations and thus may have some limitations in terms of generalisability across ethnicities and regions. Future research should expand the geographic and ethnic diversity of the study sample to more fully validate the generalisability and applicability of the findings. (5) The literature included in this study was not clearly harmonised in terms of diagnostic criteria for RDS.
5 Conclusions
Current evidence indicates that NHFOV significantly reduced the need for mechanical ventilation in NRDS compared to other ventilation modes, enhanced the success rate of extubation, and decreased the incidence of BPD. However, it had not been conclusively demonstrated that each intervention significantly lowered the incidence of complications such as nasal injury, air leakage, IVH, ROP, and NEC. Furthermore, the efficacy of each noninvasive ventilation strategy post-extubation in NRDS requires further investigation through large-scale clinical multicenter RCTs.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author contributions
JY: Formal Analysis, Methodology, Software, Visualization, Writing – original draft. HM: Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing. XW: Data curation, Resources, Writing – original draft. JZ: Formal Analysis, Writing – review & editing. MH: Investigation, Visualization, Writing – review & editing. CX: Software, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Inner Mongolia Natural Science Foundation (Grant NO. 2020MS08034) and the Inner Mongolia Autonomous Region Science and Technology Programme (Grant NO. 2022YFSH0088).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1435518/full#supplementary-material
References
1. Li J, Chen L, Shi Y. Nasal high-frequency oscillatory ventilation versus nasal continuous positive airway pressure as primary respiratory support strategies for respiratory distress syndrome in preterm infants: a systematic review and meta-analysis. Eur J Pediatr. (2022) 181(1):215–23. doi: 10.1007/s00431-021-04190-0
2. Sweet DG, Carnielli VP, Greisen G, Hallman M, Klebermass-Schrehof K, Ozek E, et al. European consensus guidelines on the management of respiratory distress syndrome: 2022 update. Neonatology. (2023) 120(1):3–23. doi: 10.1159/000528914
3. Gaertner VD, Rüegger CM. Optimising success of neonatal extubation: respiratory support. Semin Fetal Neonatal Med. (2023) 28(5):101491. doi: 10.1016/j.siny.2023.101491
4. Kakkilaya V, Jubran I, Mashruwala V, Ramon E, Simcik VN, Marshall M, et al. Quality improvement project to decrease delivery room intubations in preterm infants. Pediatrics. (2019) 143(2):e20180201. doi: 10.1542/peds.2018-0201
5. De Luca D, Dell'Orto V. Non-invasive high-frequency oscillatory ventilation in neonates: review of physiology, biology and clinical data. Arch Dis Child Fetal Neonatal Ed. (2016) 101(6):F565–70. doi: 10.1136/archdischild-2016-310664
6. Victor S, Roberts SA, Mitchell S, Aziz H, Lavender T, Extubate trial group. Biphasic positive airway pressure or continuous positive airway pressure: a randomized trial. Pediatrics. (2016) 138(2):e20154095. doi: 10.1542/peds.2015-4095
7. Zhu X, Li F, Shi Y, Feng Z, De Luca D. Effectiveness of nasal continuous positive airway pressure vs nasal intermittent positive pressure ventilation vs noninvasive high- frequency oscillatory ventilation as support after extubation of neonates born extremely preterm or with more severe respiratory failure: a secondary analysis of a randomized clinical trial. JAMA Netw Open. (2023) 6(7):e2321644. doi: 10.1001/jamanetworkopen.2023.21644
8. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. Br Med J. (2021) 372:n160. doi: 10.1136/bmj.n160
9. Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European consensus guidelines on the management of respiratory distress syndrome - 2016 update. Neonatology. (2017) 111(2):107–25. doi: 10.1159/000448985
10. Ahmed WO, AbuSaif ISH, Salaheldin SA, Hashem HE, Obaid OA, Obaid AA, et al. Noninvasive high frequency oscillatory ventilation versus noninvasive positive pressure ventilation in preterm neonates after extubation: a randomized controlled trial. J Neonatal Perinatal Med. (2023) 16(3):393–402. doi: 10.3233/NPM-221199
11. Yuan G, Liu H, Wu Z, Chen X. Evaluation of three non-invasive ventilation modes after extubation in the treatment of preterm infants with severe respiratory distress syndrome. J Perinatol. (2022) 42(9):1238–43. doi: 10.1038/s41372-022-01461-y
12. El-Farrash RA, DiBlasi RM, AbdEL-Aziz EA, El-Tahry AM, Eladawy MS, Tadros MA, et al. Postextubation noninvasive ventilation in respiratory distress syndrome: a randomized controlled trial. Am J Perinatol. (2022) 29(14):1577–85. doi: 10.1055/s-0041-1723999
13. Liu WN, Ge J, Qiao YX, Ma J, Cui SF. Clinical research of noninvasive high frequency oscillatory ventilation after machine withdrawing in premature infants (≤32 weeks)with respriatory distress syndrome. Hebei Med. (2021) 43(2):235–8. doi: 10.3969/j.issn.1002-7386.2021.02.016
14. Seth S, Saha B, Saha AK, Mukherjee S, Hazra A. Nasal HFOV versus nasal IPPV as a post-extubation respiratory support in preterm infants-a randomised controlled trial. Eur J Pediatr. (2021) 180(10):3151–60. doi: 10.1007/s00431-021-04084-1
15. Pan R, Chen GY, Wang J, Zhou ZX, Zhang PY, Chang LW, et al. Bi-level nasal positive airway pressure (BiPAP) versus nasal continuous positive airway pressure (CPAP) for preterm infants with birth weight less than 1500 g and respiratory distress syndrome following INSURE treatment: a two-center randomized controlled trial. Curr Med Sci. (2021) 41(3):542–7. doi: 10.1007/s11596-021-2372-8
16. Jia YL, Zhao H, Zhang MZ. Effect of different ventilation modes on low birth weight premature infants with respiratory distress syndrome after extubation and weaning. Chin J Pract Med. (2021) 48(12):49–52. doi: 10.3760/vema.j.cnl15689-20210216-00757
17. Malakian A, Aramesh MR, Agahin M, Dehdashtian M. Non-invasive duo positive airway pressure ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: a randomized controlled trial. BMC Pediatr. (2021) 21(1):301. doi: 10.1186/s12887-021-02741-w
18. Ding F, Zhang J, Zhang W, Zhao Q, Cheng Z, Wang Y, et al. Clinical study of different modes of non-invasive ventilation treatment in preterm infants with respiratory distress syndrome after extubation. Front Pediatr. (2020) 8:63. doi: 10.3389/fped.2020.00063
19. Feng BQ. Effect of noninvasive high frequency oscillatory ventilation in the treatment of neonatal respiratory distress syndrome and its influence on PaO2 and PaCO2. Chin Foreign Med Res. (2020) 18(12):24–6. doi: 10.14033/i.cnki.cfmr.2020.12.010
20. Li L, Chen LP, Yu ML, Yu C, Yang LQ, Wan LL. Comparison of nBiPAP and nCPAP as respiratory support therapy after removing the ventilator in neonatal respiratory distress syndrome. China Modern Phys. (2019) 57(23):66–9. 1673-9701(2019)23-0066-04
21. Wang Z, Gao WW, Lin X, Shen YZ, Zhou WJ, Chen J, et al. Effects of noninvasive high frequency oscillatory ventilation for respiratory distress syndrome in very low birth weight preterm infants after extubation. Guangdong Med. (2019) 40(10):1391–5. doi: 10.13820/j.cnki.gdyx.20186640
22. Chen L, Wang L, Ma J, Feng Z, Li J, Shi Y. Nasal high-frequency oscillatory ventilation in preterm infants with respiratory distress syndrome and ARDS after extubation: a randomized controlled trial. Chest. (2019) 155(4):740–8. doi: 10.1016/j.chest.2019.01.014
23. Najafian B, Ansari I. Comparing the efficacy of ncpap and nippv in infants with rds after extubation; a randomized clinical trial. Razavi Int J Med. (2019) 7(2):1–5. doi: 10.30483/RIJM.2019.118320
24. Lou WB, Zhang WX, Yuan L, Zhang B. Comparative study of noninvasive high-frequency oscillatory ventilation and bilevel positive airway pressure ventilation for preterm infants with respiratory distress syndrome. Chin Gen Med. (2018) 21(16):1983–8. doi: 10.3969/i.issn.1007-9572.2018.16.016
25. Ribeiro SNS, Fontes MJF, Bhandari V, Resende CB, Johnston C. Noninvasive ventilation in newborns ≤ 1,500 g after tracheal extubation: randomized clinical trial. Am J Perinatol. (2017) 34(12):1190–8. doi: 10.1055/s-0037-1602141
26. Esmaeilnia T, Nayeri F, Taheritafti R, Shariat M, Moghimpour-Bijani F. Comparison of complications and efficacy of NIPPV and nasal CPAP in preterm infants with RDS. Iran J Pediatr. (2016) 26(2):e2352. doi: 10.5812/ijp.2352
27. Jasani B, Nanavati R, Kabra N, Rajdeo S, Bhandari V. Comparison of non-synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as post-extubation respiratory support in preterm infants with respiratory distress syndrome: a randomized controlled trial. J Matern Fetal Neonatal Med. (2016) 29(10):1546–51. doi: 10.3109/14767058.2015.1059809
28. Farhat A, Mohammadzadeh A, Saeidi R, Noorizadeh S. A comparison between nasal intermittent positive pressure ventilation and nasal continuous positive airway pressure ventilation in the treatment of neonatal respiratory distress syndrome. Iran J Neonatol. (2015) 6(4):1–6. doi: 10.22038/IJN.2015.6140
29. Kong LK, Kong XY, Li LH, Dong YY, Shang MY, Chi JH, et al. Comparison of bi-level positive pressure ventilation and transnasal continuous positive airway pressure ventilation in preterm infants with respiratory distress syndrome after withdrawal. Chin J Neonatol. (2014) 29(1):14–8. doi: 10.3969/j.issn.1673-6710.2014.01.004
30. Kahramaner Z, Erdemir A, Turkoglu E, Cosar H, Sutcuoglu S, Ozer EA. Unsynchronized nasal intermittent positive pressure versus nasal continuous positive airway pressure in preterm infants after extubation. J Matern Fetal Neonatal Med. (2014) 27(9):926–9. doi: 10.3109/14767058.2013.846316
31. Moretti C, Giannini L, Fassi C, Gizzi C, Papoff P, Colarizi P. Nasal flow-synchronized intermittent positive pressure ventilation to facilitate weaning in very low-birthweight infants. Unmasked randomized controlled trial. Pediatr Int. (2008) 50(1):85–91. doi: 10.1111/j.1442-200X.2007.02525.x
32. Khalaf MN, Brodsky N, Hurley J, Bhandari V. A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics. (2001) 108(1):13–7. doi: 10.1542/peds.108.1.13
33. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. doi: 10.1136/bmj.l4898
34. Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. (2019) 41:e2019013. doi: 10.4178/epih.e2019013
35. Mammel MC. Evolution of mechanical ventilation of the newborn infant. Semin Perinatol. (2024) 48(2):151884. doi: 10.1016/j.semperi.2024.151884
36. Reiterer F, Schwaberger B, Freidl T, Schmölzer G, Pichler G, Urlesberger B. Lung-protective ventilatory strategies in intubated preterm neonates with RDS. Paediatr Respir Rev. (2017) 23:89–96. doi: 10.1016/j.prrv.2016.10.007
37. Mukerji A, Dunn M. High-frequency ventilation as a mode of noninvasive respiratory support. Clin Perinatol. (2016) 43(4):725–40. doi: 10.1016/j.clp.2016.07.008
38. Yuan Y, Sun J, Wang B, Feng P, Yang C. A noninvasive high frequency oscillation ventilator: achieved by utilizing a blower and a valve. Rev Sci Instrum. (2016) 87(2):025113. doi: 10.1063/1.4942048
39. Czernik C, Schmalisch G, Bührer C, Proquitté H. Weaning of neonates from mechanical ventilation by use of nasopharyngeal high-frequency oscillatory ventilation: a preliminary study. J Matern Fetal Neonatal Med. (2012) 25(4):374–8. doi: 10.3109/14767058.2011.580401
40. Ramaswamy VV, More K, Roehr CC, Bandiya P, Nangia S. Efficacy of noninvasive respiratory support modes for primary respiratory support in preterm neonates with respiratory distress syndrome: systematic review and network meta-analysis. Pediatr Pulmonol. (2020) 55(11):2940–63. doi: 10.1002/ppul.25011
41. Wu J, Wen ZH, Liu DD, Wu CF, Zhang Y, Zhang L, et al. Safety evaluation on different ventilation strategies set for neonatal respiratory distress syndrome: a network meta-analysis. Zhong Hua Liu Xing Bing Xue Za Zhi. (2020) 41(2):249–60. doi: 10.3760/cma.j.issn.0254-6450.2020.02.020
42. Ramanathan R. Nasal respiratory support through the nares: its time has come. J Perinatol. (2010) 30:S67–72. doi: 10.1038/jp.2010.99
43. Victor S, Extubate Trial Group. EXTUBATE: a randomised controlled trial of nasal biphasic positive airway pressure vs. Nasal continuous positive airway pressure following extubation in infants less than 30 weeks’ gestation: study protocol for a randomised controlled trial. Trials. (2011) 12:257. doi: 10.1186/1745-6215-12-257
44. Kugelman A, Feferkorn I, Riskin A, Chistyakov I, Kaufman B, Bader D. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure for respiratory distress syndrome: a randomized, controlled, prospective study. J Pediatr. (2007) 150(5):521–6.e1. doi: 10.1016/j.jpeds.2007.01.032
45. Barrington KJ, Bull D, Finer NN. Randomized trial of nasal synchronized intermittent mandatory ventilation compared with continuous positive airway pressure after extubation of very low birth weight infants. Pediatrics. (2001) 107(4):638–41. doi: 10.1542/peds.107.4.638
46. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. (2010) 362(21):1970–9. doi: 10.1056/NEJMoa0911783
47. Null DM, Alvord J, Leavitt W, Wint A, Dahl MJ, Presson AP, et al. High-frequency nasal ventilation for 21 d maintains gas exchange with lower respiratory pressures and promotes alveolarization in preterm lambs. Pediatr Res. (2014) 75(4):507–16. doi: 10.1038/pr.2013.254
48. Barbieri E, Giordano M, Sorgente G, Borgia G, Improta M, Colonna M, et al. Use and efficacy of I-gel in complicated intubations in newborn infants: a review of case reports in the literature. Curr Pediatr Rev. (2024) 21(1):51–5. doi: 10.2174/0115733963295361240426064436
Keywords: noninvasive ventilation, NHFOV, NIPPV, NCPAP, N-BiPAP, NRDS
Citation: Yang J, Mei H, Wang X, Zhang J, Huo M and Xin C (2024) Efficacy and safety of different noninvasive ventilation strategies for postextubation respiratory support in Neonatal Respiratory Distress Syndrome: a systematic review and network meta-analysis. Front. Pediatr. 12:1435518. doi: 10.3389/fped.2024.1435518
Received: 20 May 2024; Accepted: 28 October 2024;
Published: 15 November 2024.
Edited by:
Giuseppe De Bernardo, Ospedale Buon Consiglio Fatebenefratelli, ItalyReviewed by:
Hyun Ho Kim, Jeonbuk National University, Republic of KoreaMaurizio Giordano, University of Naples Federico II, Italy
Copyright: © 2024 Yang, Mei, Wang, Zhang, Huo and Xin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Mei, bWVpaHVheWFuaUBzaW5hLmNvbQ==
 Jiayi Yang
Jiayi Yang Hua Mei*
Hua Mei* Xiaoli Wang
Xiaoli Wang Mengyue Huo
Mengyue Huo