- 1Faculty of Psychology, Tianjin Normal University, Tianjin, China
- 2School of Teacher Education, Shandong University of Aeronautics, Shandong, China
- 3School of Education, Binzhou Polytechnic, Shandong, China
- 4Mental Health Education and Research Center, Nanjing Medical University, Jiangsu, China
Background: Adverse childhood experiences (ACEs) are strongly linked to many mental health problems, and play important role in the intergenerational transmission of psychopathology. Additionally, the developmental timing may also be critical in ACEs' impact on these problems. The Adverse Life Experiences Scale (ALES), as a recently developed measure, has demonstrated good reliability and validity in indexing cumulative risk, developmental timing, and intergenerational transmission. This scale has not been used in China. The purpose of present study was to revise the Chinese version of the ALES and examine its psychometric properties.
Methods: A total of 527 parents (fathers n = 246, mothers n = 281) from families with at least one child (12–18 years) completed this online survey. Internal consistency, test–retest reliability, correlations, regression models were examined for assessing the psychometric properties of the Chinese version of the ALES.
Results: The Chinese version of the ALES showed acceptable internal consistency (children: α = .72, parents: α = .74) and test–retest reliability (children: r = .86, parents: r = .84). In terms of validity, both parents and children's ACEs scores (total score and most age intervals scores) were significantly correlated with their current symptoms; ACEs scores of some age intervals in early childhood and adolescence significantly predicted symptoms in regression models; and parents' ACEs total score significantly correlated with children's ACEs total score and symptoms (all, girls, boys) except boys' Strengths and Difficulties Questionnaire total score.
Conclusion: The Chinese version of the ALES showed good psychometric properties for assessing ACEs cumulative risk, developmental timing, and intergenerational transmission, and can serve as a reliable tool to evaluate ACEs in Chinese samples.
Introduction
Adverse Childhood Experiences (ACEs) include a range of traumatic events that could directly or potentially impede healthy development during the 0–18 years, which primarily consist of child abuse, neglect, domestic violence, severe disruptions of parenting, and other factors related to increased risk for negative health outcomes. These events are highly interrelated, and when considering the cumulative risk, ACEs prove to be a robust predictor of physical and psychosocial problems (1). Although there are some variations in the relationships between ACEs and health problems, the long-term effects are generally consistent across different cultures (2, 3).
Much evidence supports the strong dose-response relationship between ACEs and mental health problems. As a result, the assessment of ACEs in prevalent studies is commonly based on cumulative scoring of ACEs, the validity of which has been well discussed. Other emerging evidence suggests that there may be synergistic effects between different ACEs, and that some specific combinations of ACEs synergistically increase the risk of negative outcomes significantly beyond what is predicted by cumulative scores. However, the dose-response effect is particularly robust for individuals exposed to multiple ACEs, especially four and more (4, 5). In a word, cumulative scoring of ACEs is a concise and practical measurement.
The developmental timing of ACEs may be critical. The impact of ACEs on children is not equal in different developmental stages, and specific sensitive periods may exist. In addition to considering the exposure timing of ACEs, variations in mental health problems may also depend on the chronicity of ACEs (6). Controlling for the number of cumulative ACEs, the chronicity of ACEs can significantly influence the externalizing symptoms (7). Therefore, ACEs measures require competent temporal sensitivity. Some tools used for assessing childhood maltreatment possess the capability to gather temporal information of exposure (8, 9). However, in addition to maltreatment, ACEs also include other important types of childhood adversity, and current measures of ACEs have limited capacity to provide temporal information of exposure. The effects of ACEs in the intergenerational transmission of psychopathology are supported by previous research (10). In general, the measures used to assess caregivers and children ACEs were implemented separately, with the two tools for caregivers and children often being temporarily integrated. Accordingly, recent reviews emphasized the importance of using a unified tool to assess both caregivers and children ACEs (11, 12).
Considering the developmental timing and intergenerational transmission, Hawes and colleagues developed the Adverse Life Experiences Scale (ALES). They also added more qualified ACEs items into this scale based on Felitti and Finkelhor's work (12–14). By employing this scale, researchers can simultaneously assess the level of exposure to ACEs for caregivers and children under the same standard. In Australia, the ALES demonstrated good reliability and validity in measuring both a community sample of families with children aged 2–12 years and a clinical sample of families with children aged 2–9 years. This scale has not been applied to the Chinese sample. With the original author's permission, we revised the Chinese version of the ALES, and replicated the research process of the original scale (community sample part) to examine its cross-cultural psychometric properties.
Materials and methods
Participants
Participants were parents from families with at least one child (12–18 years). All participants are anonymous. A total of 527 parents (fathers n = 246, mothers n = 281) finally completed the survey. Parents were aged between 35 and 58 years (M = 44.43; SD = 4.55), 53.3% were mothers; children were aged between 12 and 18 years (M = 15.05; SD = 1.94), 51.6% were girls. Four weeks later, 60 parents were randomly selected to examine the test-retest reliability. Data was collected between April and May 2023.
Procedure
Participants were recruited from middle schools in Shandong and Yunnan provinces. This survey was conducted via the Wen Juan Xing online survey platform (https://www.wjx.cn). The platform was set up to guarantee that participants input all items and automatically paid each participant 20 Yuan (about $2.8) after they completed the questionnaire. By telephone, we explained to the participants the purpose of the study, the confidentiality of the data, informed them that participation was voluntary and they could quit at any time. The questionnaire link was sent to the participants with their consent. The Tianjin Normal University Ethics Committee approved the procedures (IRB number: 2023033001).
Measures
The adverse life experiences scale (ALES)
The ALES is a caregiver-reported scale that assesses the ACEs of caregivers and their children. Authorized by the original author, the Chinese version of the scale was translated using a standard back-translation procedure. The translation involved two bilingual psychologists, who first translated it from English to Chinese and then back from Chinese to English. The translated Chinese version was cross-checked with the original version to ensure the equivalence of items' meanings. This scale consists of two parallel components with identical items for caregivers and children, each containing 23 risk factor items (yes/no). Considering the cultural differences, some items were adjusted or eliminated to align with the Chinese native culture. In the Chinese version (Appendix A), the items about “dangerous neighborhoods” (1 item) and “war” (2 items) are removed from the original scale, and the item about “bullied by siblings at home” (1 item) is added. The reason for adding the item “bullied by siblings at home” is that studies conducted on Chinese adolescent samples have shown that the proportion of those who experienced sibling bullying was 12.9%–20.9%, and that sibling bullying was significantly associated with mental health problems (15–17). Total score is calculated by summing the “yes” responses across all items (ACEs exposed during 0–18 years), resulting in scores ranging from 0 to 21. In this scale, the entire period of 0–18 years is divided into distinct age intervals to assess the developmental timing of ACEs, including 0–1 year, 2–3 years, 4–5 years, 6–8 years, 9–12 years, 13–18 years. The chronicity of ACEs score is calculated by summing the number of age intervals in which any ACEs item is affirmed and then dividing it by the individuals' age (12). In this study, only parents as caregivers reported ACEs for themselves and their children, and parents only reported the oldest child under 18 years in the household.
The strengths and difficulties questionnaire (SDQ)
The SDQ is widely used in the assessment of children's emotional and behavioral problems. The Chinese version of the parent-reported SDQ selected for this study contains 25 items, and consists of five subscales (hyperactivity/inattention, conduct problems, emotional symptoms, peer problems, and prosocial behavior). The SDQ has demonstrated acceptable reliability and validity in Chinese sample studies (18). In this study, the total difficulties score was used and showed good internal consistency (α = .75).
The child stress disorder checklist (CSDC)
The CSDC is used to assess acute and recent psychopathy responses following traumatic events, and is applicable to children aged 2–18 years (19). This checklist contains 36 items, including 1 item for traumatic events, 5 items for acute reactions, and 30 items for recent responses. In this study, the subscale of recent responses was employed to assess the children's stress symptoms in the past month by calculating the total score. The Chinese version of the CSDC was parent-reported and showed good reliability in the current sample (α = .94).
The Kessler psychological distress scale (K10)
The scale is widely used to assess the psychological problems in adulthood. In this study, the scale was used to assess parents' anxiety and stress in the past month. The Chinese version of K10 had acceptable internal consistency in the previous study (α = .80) (20), and showed good internal consistency in this study (α = .94).
Analytic strategy
The ACEs scores and symptoms were analyzed descriptively. The median ACEs scores of parents and children corresponding to the 50th, 75th, 90th, and 95th percentiles in the sample were counted. The median ACEs scores of parents were counted for ACEs accumulated before 18 years. Since the age range of children is 12–18 years in this study, the median ACEs scores of children were counted for ACEs accumulated before 12 years. Correlations between children's ACEs scores and current symptoms (CSDC, SDQ) were examined. Correlations between parents' ACEs scores and current symptoms (K10) were examined. The predictive power of developmental timing on current symptoms in children and parents was examined using regression models. In the first block, the chronicity scores (independent variable) and age (covariate) were included to test whether the chronicity predicted the current symptoms; in the second block, the ACEs scores (independent variable) corresponding to each age interval were included, to explain the variance in current symptoms beyond the chronicity.
Results
Descriptive statistics
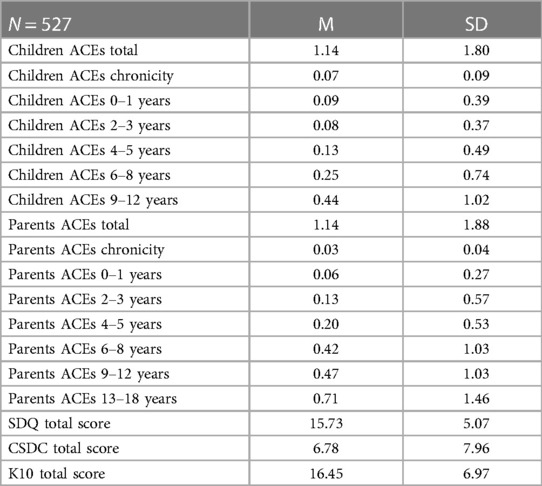
The means and standard deviations of ACEs and symptoms are presented in Table 1. In the children's data, the median ACEs scores at the 50th, 75th, 90th, and 95th percentiles of ACEs scores corresponded to one, two, six, and nine; before 12 years, 38.3% of children were exposed to at least one ACE, 9.7% of children were exposed to at least four ACEs. In the parents' data, the median ACEs scores at the 50th, 75th, 90th, and 95th percentiles of ACEs scores corresponded to two, three, six and six; before 18 years, 54.5% of parents were exposed to at least one ACE, 11.6% of parents were exposed to at least four ACEs.
Reliability
The Chinese version of ALES for both children and parents had shown acceptable internal consistency (children: α = .72, parents: α = .74). Reliabilities for children and parents were both good in four weeks later retest (children: r = .86, parents: r = .84).
Validity
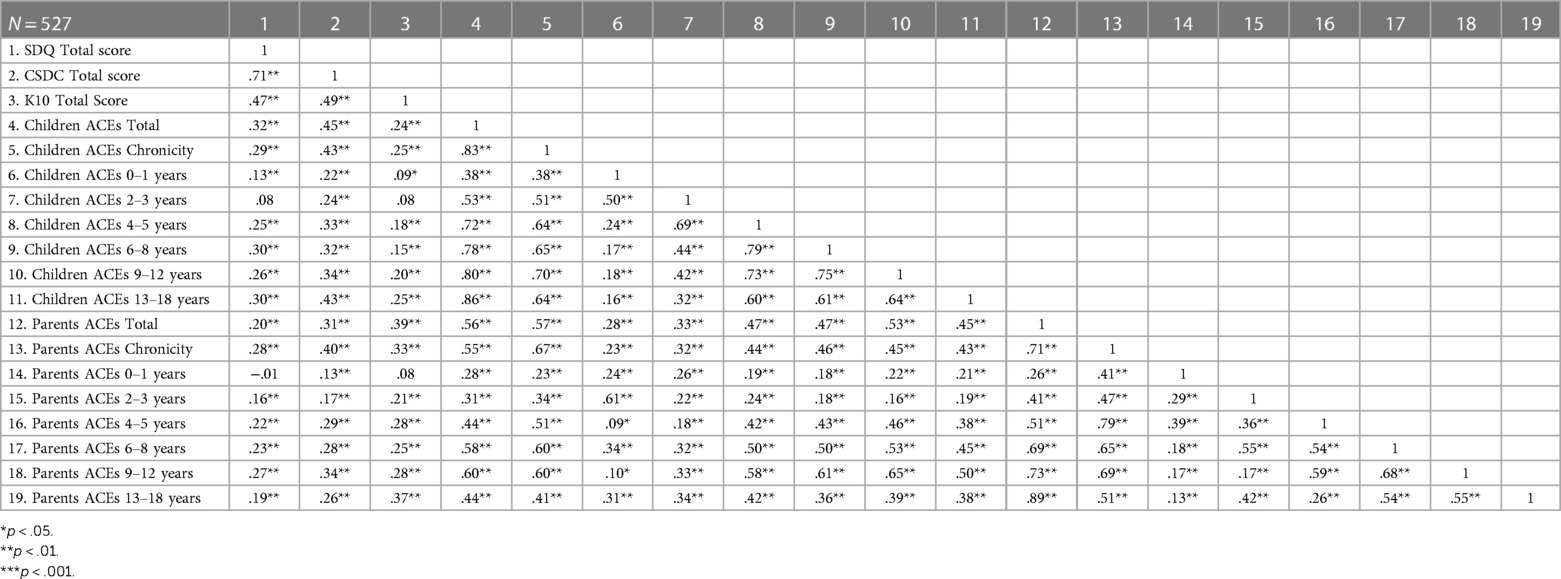
The bivariate correlations between ACEs Scores and Symptoms are shown in Table 2. In children, the ACEs total score were significantly correlated with SDQ total score (r = .32, p < .01) and significantly correlated with CSDC total score (r = .45, p < .01). For each age interval, the correlation between ACEs and SDQ total score was not significant for 2–3 years, the correlations were significant for 0–1 year (r = .13, p < .01) and the remaining age intervals (r = .25–.30, p < .01); the correlations between ACEs and CSDC total score were significant across all age intervals (r = .22–.43, p < .01). The children's ACEs chronicity was significantly correlated with SDQ total score (r = .29, p < .01) and significantly correlated with CSDC total score (r = .43, p < .01).
In parents, the ACEs total score were significantly correlated with K10 total score(r = .39, p < .01). For each age interval, the correlation between ACEs and K10 total score was not significant for 0–1 year, and the correlations were significant for the remaining age intervals (r = .21–.37, p < .01). The parents' ACEs chronicity was significantly correlated with K10 total score (r = .33, p < .01).
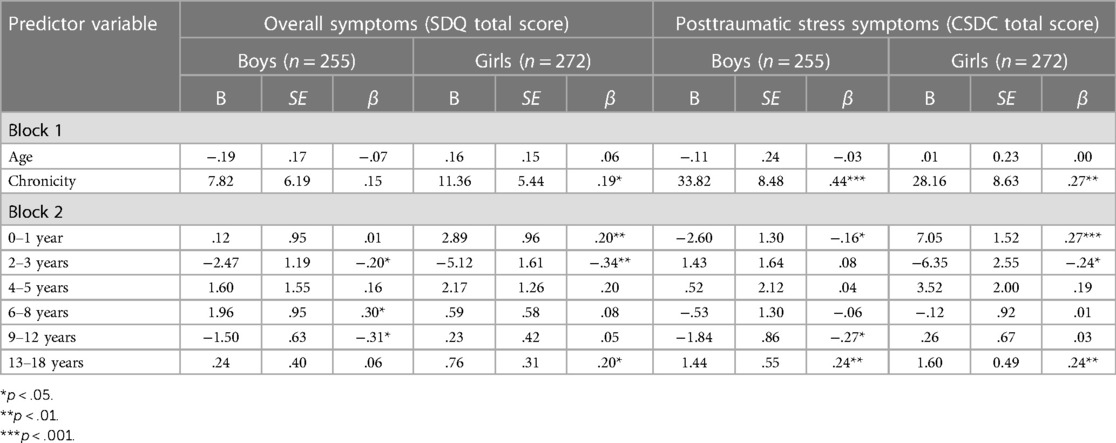
Regression models for the developmental timing of children's ACEs and their current symptoms are presented in Table 3. In boys, the ACEs chronicity and age did not yield significant predictions for overall symptoms, the ACEs scores corresponding to the age intervals of 2–3 years (β = −.20, p < .05), 6–8 years (β = .30, p < .05), 9–12 years (β = −.31, p < .05) were found to be significant predictors of overall symptoms. Posttraumatic stress symptoms in boys were significantly predicted by ACEs chronicity (β = .44, p < .001), and the ACEs scores corresponding to the age intervals of 0–1 year (β = −.16, p < .05), 9–12 years (β = −.27, p < .05), and 13–18 years (β = .24, p < .01) were significant predictors of posttraumatic stress symptoms.
In girls, the ACEs chronicity significantly predicted overall symptoms (β = .19, p < .05), and the ACEs scores corresponding to the age intervals of 0–1 year (β = .20, p < .01), 2–3 years (β = −.34, p < .01), 13–18 years (β = .20, p < .05) were significant predictors of overall symptoms. Posttraumatic stress symptoms in girls were significantly predicted by the ACEs chronicity (β = .27, p < .01), and the ACEs scores corresponding to the age intervals of 0–1 year (β = .27, p < .001), 2–3 years (β = −.24, p < .05), 13–18 years (β = .24, p < .01) significantly predicted posttraumatic stress symptoms. Multicollinearity among all age intervals was controlled for in all regression models.
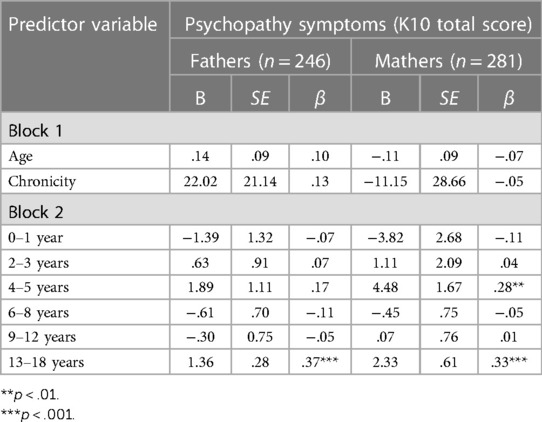
Two regression models for the developmental timing of parents' ACEs and current symptoms are presented in Table 4. In fathers, the ACEs chronicity and age did not yield significant predictions for psychopathy symptoms, the ACEs scores corresponding to the age interval of 13–18 years (β = .37, p < .001) significantly predicted current symptoms. In mothers, the ACEs chronicity and age failed to predict their psychopathy symptoms, the ACEs scores corresponding to the age intervals of 4–5 years (β = .28, p < .01) and 13–18 years (β = .33, p < .001) were significant predictors of current symptoms. Multicollinearity among all age intervals was controlled for in all regression models.
Intergenerational transmission of psychopathology was examined. Parents' ACEs total scores were significantly correlated with children's ACEs total score (r = .56, p < .01, n = 527), girls' ACEs total score (r = .63, p < .0, n = 272), and boys' ACEs total score (r = .51, p < .01, n = 255). Using Fisher's z transformation for testing, the correlation between parents' ACEs total score and girls' ACEs total score was significantly higher than that of boys (z = 2.04, p < .05) (21). Parents' ACEs total score demonstrated significant correlations with children's SDQ total score (r = .20, p < .01, n = 527) and girls' SDQ total score (r = .46, p < .01, n = 272), while no significant association was found with boys’ SDQ total score (n = 255). Significant correlations were observed between the parents' ACEs total score and children's CSDC total score (r = .31, p < .01, n = 527), girls' CSDC total score (r = .56, p < .01, n = 272), and boys' CSDC total score (r = .14, p < .05, n = 255). Using Fisher's z transformation for testing, the correlation between parents' ACEs total score and girls' CSDC total score was significantly higher than that of boys (z = 5.61, p < .001) (21).
Discussion
The results of this study indicate that the Chinese version of the ALES has acceptable reliability and validity, within a sample of Chinese families raising at least one child (12–18 years). Both parent and children ACEs total score, as measured by this scale, were associated with current symptoms, consistent with findings from previous studies. ACEs chronicity and ACEs scores corresponding to the specific age intervals further explained variance in these outcomes. Several ACEs age intervals in early childhood and adolescence significantly predicted symptoms (refer to Tables 3, 4). In intergenerational transmission of psychopathology, parents' ACEs total score significantly correlated with children's ACEs total score and symptoms (all, girls, boys) except boys' SDQ total score, and the correlations were all significantly higher in girls than in boys.
Based on the regression models of children and parents, the results indicate that the impact of ACEs on subsequent psychopathy symptoms is significant in early childhood and adolescence. In other words, these findings suggest that both early childhood and adolescence are sensitive periods for individual responses to adversity. The effects of exposure to stress and adversity during early childhood on long-term bio-behavioral functioning in life-course health development, which surpass the effects observed in other developmental stages, have been extensively discussed (22, 23). Previous findings support that early childhood exposure to ACEs leads to greater variations in amygdala development and DNA methylation patterns, thereby increasing sensitivity in responding to subsequent stress and adversity (24–26). Some studies suggested that adolescence may provide children another opportunity to shape their stress response system (27–29). Adolescence emerges as a sensitive period for stress response due to the synchronous maturation of the endocrine system, neural system, psychosocial functioning, and increased plasticity across multiple systems (30).
In children models, significant negative associations were found between ACEs in some age intervals (under 12 years) and current symptoms. The results may be explained by the stress acceleration theory and cultural contexts. The Stress Acceleration Hypothesis posits that early-life adversity can result in an accelerated maturation of the emotional circuits in the children's brain, thereby facilitating rapid adaptation to stressful environmental stimuli (31). Individuals exposed to adversity during early childhood may exhibit better cognitive performance in stressful or risky tasks, compared to their peers living in supportive environment (32). Accelerated development can ensure conditional adaptation in resource-disadvantaged and uncertain environments, thereby increasing survivability (33, 34). The potential cost associated with the benefits of accelerated development is the alteration in neurodevelopmental plasticity, consequently increasing the risk of developing psychopathy symptoms in adulthood (31, 35, 36). Overall, emerging studies suggest that children exposed to early adversity may exhibit a holistic pattern of accelerated neurodevelopment (37). Due to the influence of multiple factors, the mechanisms by which accelerated neurodevelopment in response to early adversity yields benefits and costs throughout the lifespan are complex (34, 38). From the cultural context perspective, Chinese traditional culture, rooted in Confucianism, emphasizes a positive appraisal of adversity, and believes that successfully coping with adversity is an essential way to promote resilience and enhance self-worth. Studies among Chinese participants (including Hong Kong) have found that children who have experienced poverty show greater resilience, more positive beliefs and behaviors in the face of adversity (39, 40). Furthermore, in Chinese family, virtues of harmony and endurance are underscored, which would help children cope with family conflict (41, 42). Research suggests that balanced sibling relationships, including both conflict and support, are associated with the better social-emotional skills. Therefore, although sibling bullying is significantly associated with mental health problems overall, moderate exposure to sibling bullying in such a family context may potentially have positive effects on children's development (43).
In intergenerational transmission of psychopathology, the results suggest that girls may be more susceptible than boys, indicating the potential moderating role of gender in this process. In a study of the relationship between mothers' exposure to childhood sexual abuse and their children's externalizing behavioral problems, the relationship was found to be significant for mother-girl dyads but not for mother-boy dyads (44). In another study, contrasting findings were observed, suggesting that boys are more susceptible to the indirect effects generated by mothers' ACEs through perinatal anxiety and depression (45). Additionally, in Chinese preschool children sample, no significant gender differences were found in the influence of mothers' ACEs on children's behavioral problems (46). One possible explanation for the above disagreement is that the transmission pathways of parents' ACEs differ between boys and girls, which is supported by the study of genetic epigenetic biomarkers (47). Another explanation is that the contributions of different ACEs types in the intergenerational transmission may be not equal (48).
This study has several limitations. First, it's recommended that participants from diverse demographic backgrounds, such as socioeconomic statuses, ethnicities, and religious beliefs, be included to ensure a more representative sample, especially clinical-related participants. Second, for some specific ACEs, such as “Adult has repeatedly cursed, insulted, threatened to hurt”, parents may act as the perpetrators and intentionally conceal or underreport their children's ACEs. In future studies, the ACEs scores of children (12–18 years) should consider self-report. Third, to avoid participants impatience caused by excessive response time, the number of all items in this survey was controlled. As a result, the collection of symptoms information was relatively inadequate, especially for parents. Additional symptom measures could be included in the future to provide more evidence to support the Chinese version of the ALES.
Conclusions
In summary, the findings of this study indicate that the Chinese version of ALES has good psychometric properties and can be considered a reliable and valid tool. This scale provides a comprehensive approach to assessing ACEs by considering cumulative score, developmental timing, and intergenerational transmission. Implementation of this scale would contribute to a deeper understanding of the relationship between ACEs and mental health problems, thereby improving current prevention and intervention strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Tianjin Normal University Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LZ: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YL: Data curation, Formal Analysis, Investigation, Methodology, Resources, Validation, Writing – review & editing. ZW: Data curation, Formal Analysis, Investigation, Methodology, Resources, Validation, Writing – review & editing. JW: Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to acknowledge the support provided by Professor David J. Hawes (School of Psychology, The University of Sydney) and Professor Jinsong Zhang (Xinhua Hospital affiliated to Shanghai Jiao Tong University).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ports KA, Ford DC, Merrick MT, Guinn AS. ACEs: definitions, measurement, and prevalence. In: Asmundson GJG, Afifi TO, editors. Adverse Childhood Experiences. London: Academic Press (2020). p. 17–34.
2. Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. (2017) 2(8):e356–66. doi: 10.1016/S2468-2667(17)30118-4
3. Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: a systematic review and meta-analysis. Child Abuse Negl. (2019) 97:104127. doi: 10.1016/j.chiabu.2019.104127
4. Briggs E, Amaya-Jackson L, Putnam K, Putnam F. All adverse childhood experiences are not equal: the contribution of synergy to adverse childhood experience scores. Am Psychol. (2021) 76(2):243–52. doi: 10.1037/amp0000768
5. Hamby SL, Elm JH, Howell KH, Merrick MT. Recognizing the cumulative burden of childhood adversities transforms science and practice for trauma and resilience. Am Psychol. (2021) 76(2):230–42. doi: 10.1037/amp0000763
6. McKelvey LM, Selig JP, Whiteside-Mansell L. Foundations for screening adverse childhood experiences: exploring patterns of exposure through infancy and toddlerhood. Child Abuse Negl. (2017) 70:112–21. doi: 10.1016/j.chiabu.2017.06.002
7. Schroeder A, Slopen N, Mittal M. Accumulation, timing, and duration of early childhood adversity and behavior problems at age 9. J Clin Child Adolesc Psychol. (2020) 49(1):36–49. doi: 10.1080/15374416.2018.1496440
8. Bifulco A, Bernazzani O, Moran P, Jacobs C. The childhood experience of care and abuse questionnaire (CECA. Q): validation in a community series. Br J Clin Psychol. (2005) 44(4):563–81. doi: 10.1348/014466505X35344
9. Teicher MH, Parigger A. The “maltreatment and abuse chronology of exposure” (MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One. (2015) 10(2):e0117423. doi: 10.1371/journal.pone.0117423
10. Narayan AJ, Lieberman AF, Masten AS. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin Psychol Rev. (2021) 85:101997. doi: 10.1016/j.cpr.2021.101997
11. Barnes AJ, Anthony BJ, Karatekin C, Lingras KA, Mercado R, Thompson LA. Identifying adverse childhood experiences in pediatrics to prevent chronic health conditions. Pediatr Res. (2020) 87(2):362–70. doi: 10.1038/s41390-019-0613-3
12. Hawes DJ, Lechowicz M, Roach A, Fisher C, Doyle FL, Noble S, et al. Capturing the developmental timing of adverse childhood experiences: the adverse life experiences scale. Am Psychol. (2021) 76(2):253–67. doi: 10.1037/amp0000760
13. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14(4):245–25. doi: 10.1016/S0749-3797(98)00017-8
14. Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of adverse childhood experiences. Child Abuse Negl. (2015) 48:13–21. doi: 10.1016/j.chiabu.2015.07.011
15. Liu X, Wolloh Ii MG, Lin X, Qiu X, Qing Z, Wang W, et al. The association between sibling bullying and psychotic-like experiences among children age 11–16 years in China. J Affect Disord. (2021) 284:31–7. doi: 10.1016/j.jad.2021.01.073
16. Peng C, Wang Z, Yu Y, Cheng J, Qiu X, Liu X. Co-occurrence of sibling and peer bullying victimization and depression and anxiety among Chinese adolescents: the role of sexual orientation. Child Abuse Negl. (2022) 131:105684. doi: 10.1016/j.chiabu.2022.105684
17. Qing Z, Ma Y, Liu X. Prevalence and associated family factors of sibling bullying among Chinese children and adolescents. Front Psychol. (2022) 13:892598. doi: 10.3389/fpsyg.2022.892598
18. Kou J, Du Y, Xia L. Reliability and validity of “children strengths and difficulties questionnaire” in Shanghai Norm. Shanghai Arch Psychiatry. (2005) 17(1):25–8. doi: 10.3969/j.issn.1002-0829.2005.01.007
19. Kong Y, Zhang J, Shuai L, Xia W, Wang Z. Validity and reliability of the Chinese version of the child stress disorders checklist. Chin Ment Health J. (2014) 28(6):452–7 doi: 10.3969/j.issn.1000-6729.2014.06.010.
20. Zhou C, Chu J, Wang T, Peng Q, He J, Zheng W, et al. Reliability and validity of 10-item Kessler scale (K10) Chinese version in evaluation of mental health status of Chinese population. Chin J Clin Psychol. (2008) 16(6):627–9.
21. Meng XL, Rosenthal R, Rubin DB. Comparing correlated correlation coefficients. Psychol Bull. (1992) 111:172–5. doi: 10.1037/0033-2909.111.1.172
22. Halfon N, Larson K, Lu M, Tullis E, Russ S. Lifecourse health development: past, present and future. Matern Child Health J. (2014) 18:344–65. doi: 10.1007/s10995-013-1346-2
23. Luby JL, Baram TZ, Rogers CE, Barch DM. Neurodevelopmental optimization after early-life adversity: cross-species studies to elucidate sensitive periods and brain mechanisms to inform early intervention. Trends Neurosci. (2020) 43(10):744–51. doi: 10.1016/j.tins.2020.08.001
24. Dunn EC, Soare TW, Zhu Y, Simpkin AJ, Suderman MJ, Klengel T, et al. Sensitive periods for the effect of childhood adversity on DNA methylation: results from a prospective, longitudinal study. Biol Psychiatry. (2019) 85(10):838–49. doi: 10.1016/j.biopsych.2018.12.023
25. Essex MJ, Boyce WT, Hertzman C, Lam LL, Armstrong JM, Neumann SM, et al. Epigenetic vestiges of early developmental adversity: childhood stress exposure and DNA methylation in adolescence. Child Dev. (2013) 84(1):58–75. doi: 10.1111/j.1467-8624.2011.01641.x
26. Luby J, Belden A, Botteron K, Marrus N, Harms MP, Babb C, et al. The effects of poverty on childhood brain development: the mediating effect of caregiving and stressful life events. JAMA Pediatr. (2013) 167(12):1135–42. doi: 10.1001/jamapediatrics.2013.3139
27. DePasquale CE, Donzella B, Gunnar MR. Pubertal recalibration of cortisol reactivity following early life stress: a cross-sectional analysis. J Child Psychol Psychiatry. (2019) 60(5):566–75. doi: 10.1111/jcpp.12992
28. Fuhrmann D, Knoll LJ, Blakemore SJ. Adolescence as a sensitive period of brain development. Trends Cogn Sci (Regul Ed). (2015) 19(10):558–66. doi: 10.1016/j.tics.2015.07.008
29. Gunnar MR, DePasquale CE, Reid BM, Donzella B, Miller BS. Pubertal stress recalibration reverses the effects of early life stress in postinstitutionalized children. Proc Natl Acad Sci U S A. (2019) 116(48):23984–8. doi: 10.1073/pnas.1909699116
30. Sisk LM, Gee DG. Stress and adolescence: vulnerability and opportunity during a sensitive window of development. Curr Opin Psychol. (2022) 44:286–92. doi: 10.1016/j.copsyc.2021.10.005
31. Callaghan BL, Tottenham N. The stress acceleration hypothesis: effects of early-life adversity on emotion circuits and behavior. Curr Opin Behav Sci. (2016) 7:76–81. doi: 10.1016/j.cobeha.2015.11.018
32. Frankenhuis WE, de Weerth C. Does early-life exposure to stress shape or impair cognition? Curr Dir Psychol Sci. (2013) 22(5):407–12. doi: 10.1177/0963721413484324
33. Boyce WT, Ellis BJ. Biological sensitivity to context: i. An evolutionary–developmental theory of the origins and functions of stress reactivity. Dev Psychopathol. (2005) 17(2):271–301. doi: 10.1017/S0954579405050145
34. Del Giudice M, Ellis BJ, Shirtcliff EA. The adaptive calibration model of stress responsivity. Neurosci Biobehav Rev. (2011) 35(7):1562–92. doi: 10.1016/j.neubiorev.2010.11.007
35. De France K, Evans GW, Brody GH, Doan SN. Cost of resilience: childhood poverty, mental health, and chronic physiological stress. Psychoneuroendocrinology. (2022) 144:105872. doi: 10.1016/j.psyneuen.2022.105872
36. Fragale JE, Khariv V, Gregor DM, Smith IM, Jiao X, Elkabes S, et al. Dysfunction in amygdala–prefrontal plasticity and extinction-resistant avoidance: a model for anxiety disorder vulnerability. Exp Neurol. (2016) 275:59–68. doi: 10.1016/j.expneurol.2015.11.002
37. McLaughlin KA, Weissman D, Bitrán D. Childhood adversity and neural development: a systematic review. Ann Rev Dev Psychol. (2019) 1:277–312. doi: 10.1146/annurev-devpsych-121318-084950
38. Ellis BJ, Sheridan MA, Belsky J, McLaughlin KA. Why and how does early adversity influence development? Toward an integrated model of dimensions of environmental experience. Dev Psychopathol. (2022) 34(2):447–71. doi: 10.1017/S0954579421001838
39. Ge T, Ngai S-y. Three pathways to promote poverty resilience: the effects of poverty on children’s educational and behavioral performance under multisystems in China. Child Youth Serv Rev. (2020) 113:104962. doi: 10.1016/j.childyouth.2020.104962
40. Shek DT. Chinese cultural beliefs about adversity: its relationship to psychological well-being, school adjustment and problem behaviour in Hong Kong adolescents with and without economic disadvantage. Childhood. (2004) 11(1):63–80. doi: 10.1177/0907568204040185
41. Jiang C, Jiang S. Growing up in adversity: a moderated mediation model of family conflict, cyberbullying perpetration, making sense of adversity and depression. Youth Soc. (2024) 56(4):754–73. doi: 10.1177/0044118X231179245
42. Leung JT, Shek DT. Psychometric properties of the Chinese cultural beliefs about adversity scale. Res Soc Work Pract. (2013) 23(3):326–35. doi: 10.1177/1049731512473782
43. Wolke D, Tippett N, Dantchev S. Bullying in the family: sibling bullying. Lancet Psychiatry. (2015) 2(10):917–29. doi: 10.1016/S2215-0366(15)00262-X
44. Linde-Krieger L, Yates TM. Mothers’ history of child sexual abuse and child behavior problems: the mediating role of mothers’ helpless state of mind. Child Maltreat. (2018) 23(4):376–86. doi: 10.1177/1077559518775536
45. Letourneau N, Dewey D, Kaplan BJ, Ntanda H, Novick J, Thomas JC, et al. Intergenerational transmission of adverse childhood experiences via maternal depression and anxiety and moderation by child sex. J Dev Orig Health Dis. (2019) 10(1):88–99. doi: 10.1017/S2040174418000648
46. Wang X, Yin G, Guo F, Hu H, Jiang Z, Li S, et al. Associations of maternal adverse childhood experiences with behavioral problems in preschool children. J Interpers Violence. (2022) 37(21–22):NP20311–330. doi: 10.1177/08862605211050093
47. Christensen J, Beveridge JK, Wang M, Orr SL, Noel M, Mychasiuk R. A pilot study investigating the role of gender in the intergenerational relationships between gene expression, chronic pain, and adverse childhood experiences in a clinical sample of youth with chronic pain. Epigenomes. (2021) 5(2):9. doi: 10.3390/epigenomes5020009
48. Stargel LE, Easterbrooks MA. Diversity of adverse childhood experiences among adolescent mothers and the intergenerational transmission of risk to children’s behavior problems. Soc Sci Med. (2020) 250:112828. doi: 10.1016/j.socscimed.2020.112828
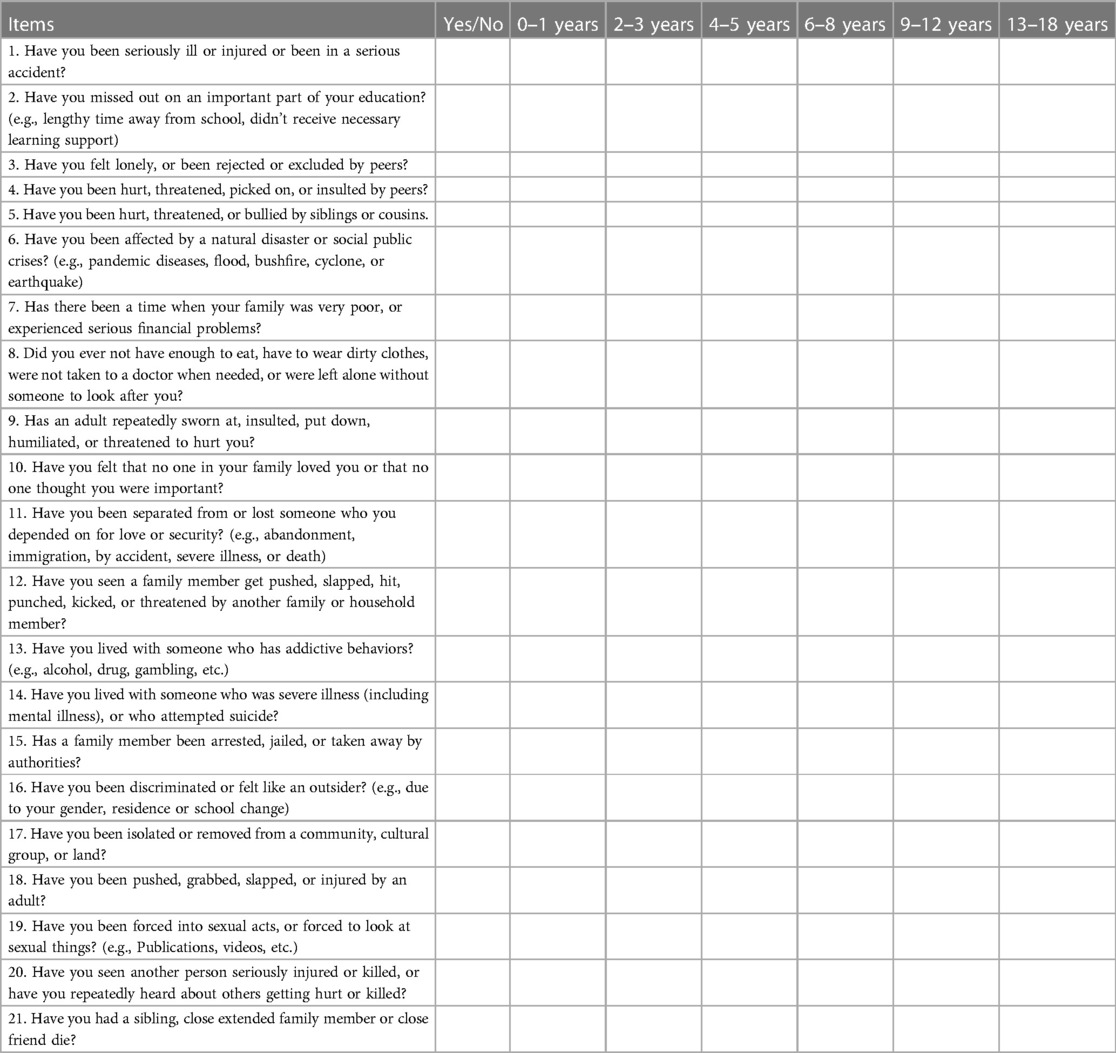
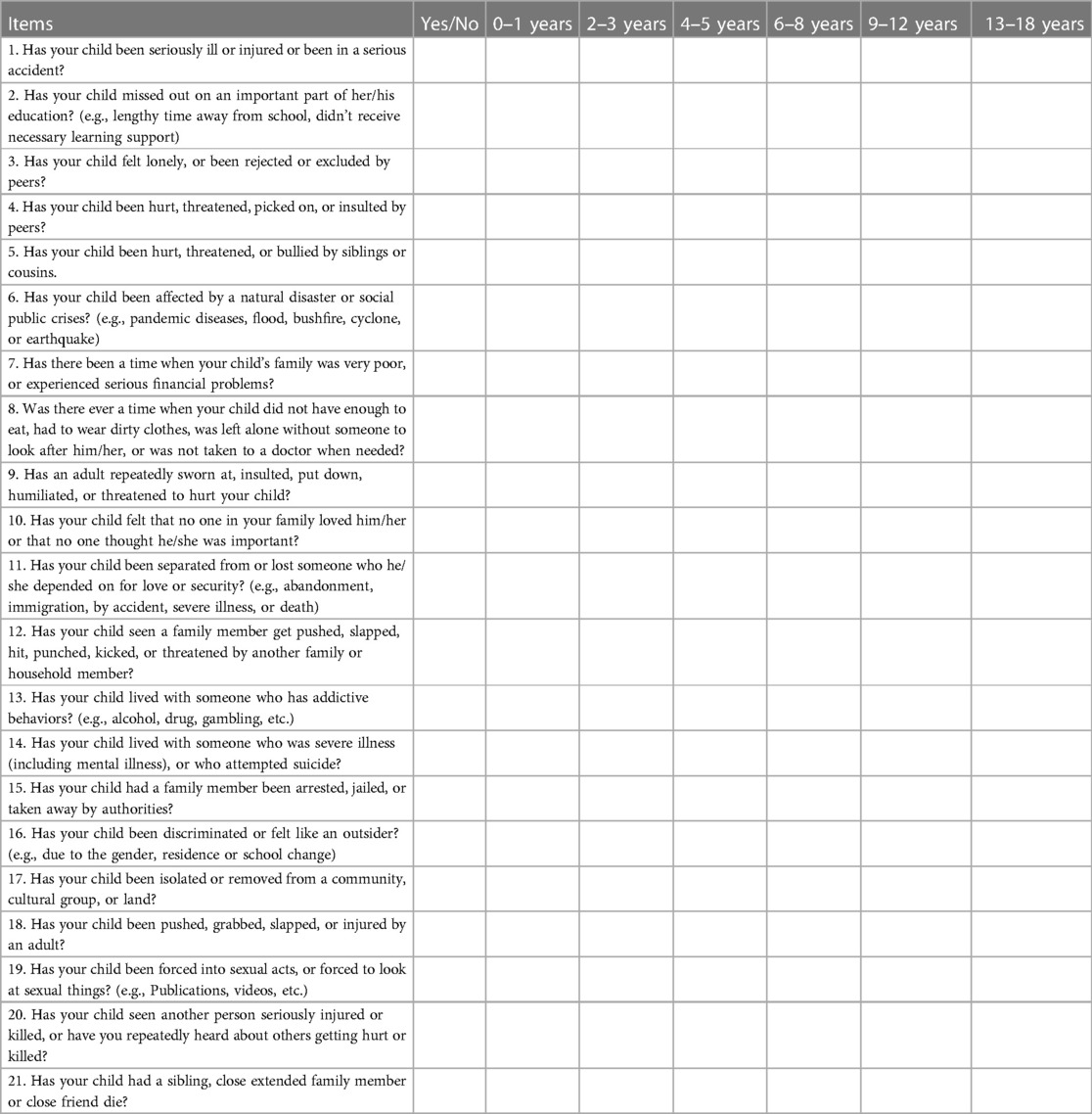
Appendix A. The Chinese version of adverse life experiences scale
1 Parents: self-report
The following part is about challenging things sometimes happen in your lives before 18 years. Please select “No” if you have not experienced, “yes” if you have experienced and continued select the age intervals.
2 Children: parent-report
The following part is about challenging things sometimes happen in your child lives. Please select “No” if your child have not experienced, “yes” if your child have experienced and continued select the age intervals. If you have more than one child under the age of 18, please report the oldest.
Keywords: adverse childhood experiences, mental health problem, assessment, developmental timing, intergenerational transmission
Citation: Zhao L, Li Y, Wang Z and Wu J (2024) Validation of the Chinese version of the adverse life experiences scale. Front. Pediatr. 12:1403183. doi: 10.3389/fped.2024.1403183
Received: 22 March 2024; Accepted: 26 June 2024;
Published: 10 July 2024.
Edited by:
Yuko Ishizaki, Kansai Medical University, JapanReviewed by:
Kenta Ito, Aichi Child Health And Medical General Center, JapanAndrómeda Ivette Valencia-Ortiz, Autonomous University of the State of Hidalgo, Mexico
© 2024 Zhao, Li, Wang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Wu, YmFiYWx1b3NoYUAxNjMuY29t
 Luowei Zhao
Luowei Zhao Yuling Li3
Yuling Li3