- 1Pediatric Surgery, Faculty of Medicine, South Valley University, Qena, Egypt
- 2Faculty of Medicine, South Valley University, Qena, Egypt
- 3Faculty of Medicine, Tanta University, Tanta, Egypt
- 4Faculty of Medicine, Minia University, Minia, Egypt
Background: Acute abdominal pain in pediatrics is a medical emergency that requires special attention. During COVID-19 pandemic, this disease presented in pediatric age by different presentations including abdominal presentations.The affected children are presented with abdominal pain, which may be caused by surgical causes or by the virus itself that necessitate surgical consultation.
Purpose: This study highlights the impact of the coronavirus pandemic on pediatric patients with acute abdominal pain regarding the presentation, clinical evaluation, and surgical management.
Methods: A retrospective cohort study was done through the collection of data from medical records and authors’ data repositories of pediatric patients presented with acute abdomen from March 2020 to March 2022, in three pediatric surgery tertiary centers.
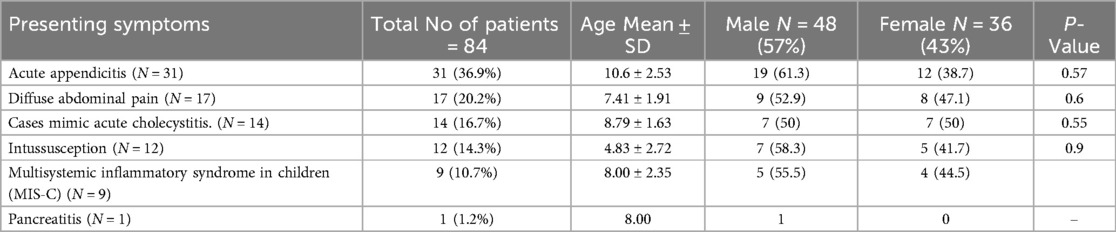
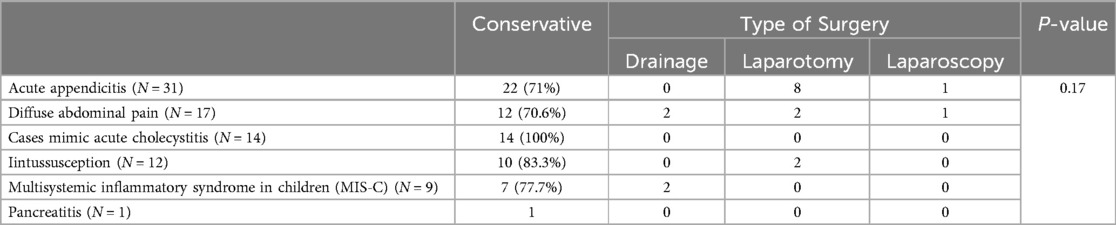
Results: Eighty-four pediatric patients with acute abdominal pain were included in this study. The diagnosis of acute appendicitis was found in 31 patients (36.9%). Generalized abdominal pain was noted in 17 patients (20.2%) and presentation mimicked acute cholecystitis was occured in 14 patients (16.7%). ultrasonography revealed intussusception in 12 cases (14.3%). Multisystem inflammatory syndrome in children (MIS-C) was present in 9 cases (10.7%) and only one case of pancreatitis (1.2%). Conservative management was successful in 66 cases (78.6%), while operative intervention was needed in18 cases (21.4%).
Conclusion: During the COVID-19 pandemic, acute abdominal pain in children was frequently observed. Careful follow up is critically important as most cases do not necessitate surgical intervention. It is crucial to consider COVID-19 as a differential diagnosis in children presenting with acute abdominal pain, particularly in cases of atypical appendicitis and intussusception to prevent unnecessary surgical procedures.
Introduction
Globally, only 1%–3% of documented COVID-19 cases occur in children. Nevertheless, children exhibit a higher propensity for gastrointestinal (GI) symptoms, with approximately 25% displaying at least one GI symptom. In some instances, GI symptoms may be the sole presenting symptoms of COVID-19 in children. The most reported GI symptoms are abdominal pain, diarrhea, and nausea/vomiting (1, 2).
A significant dilemma exists concerning the etiology of acute abdominal pain in children and the complications associated with multisystemic inflammatory syndrome in children (MIS-C). A diverse range of potential causes includes mesenteric adenitis, appendicitis, abdominal fluid collection, pancreatitis, terminal ileitis, cholecystitis, and intussusception (3–5).
Extensive research has been conducted on the gastrointestinal manifestations of COVID-19 in pediatric cases, including acute abdominal pain. However, currently, no study provides a quantitative analysis of abdominal pain cases from a surgical standpoint (4, 6, 7).
COVID-19 can induce abdominal pain resembling that in abdominal emergencies, particularly in MIS-C cases. These patients may exhibit symptoms akin to acute enteritis or an acute abdomen requiring surgery, posing a risk of misdiagnosis (8). According to AL Vecchio et al. (4), only 60% of children with COVID-19 who underwent surgery for acute appendicitis received a histologically confirmed diagnosis of acute appendicitis. Additionally, certain studies have indicated instances where children underwent emergency abdominal surgery for acute conditions only to have negative intraoperative diagnoses (9–12).
This study explored how the COVID-19 pandemic has affected pediatric patients’ presentation, assessment, and surgical management of acute abdominal pain.
Patients and methods
Study cohort
Following institutional review board approval, we conducted a retrospective study at three pediatric surgery tertiary centers in Egypt. All pediatric patients presenting with acute abdomen were included from March 2020 to March 2022. Data were collected from medical records and authors’ data repositories.
Inclusion criteria
- Age <18 years
- Patients with abdominal pain and diagnosis of COVID-19 according to the protocol of diagnosis in our country (13).
- Patients with abdominal pain and diagnostic criteria of MIS-C according to the WHO definition and diagnosis of MIS-C (14, 15).
Exclusion criteria
- Patients with incomplete data
Patients’ presentation and data collection
- Demographic data
- Gastrointestinal symptoms, characteristics of abdominal pain
- Diagnosis of COVID-19 according to the protocol of our medical authority (13).
- Laboratory investigations and imaging studies
- Surgical management
- Hospital stay and follow-up
Statistical analysis
The data were presented as numbers and percentages for qualitative data, while mean and standard deviation were used for quantitative data. Normality testing was performed using the Shapiro-Wilk test. Comparisons were conducted using the Mann-Whitney U test for non-normally distributed continuous variables and the independent T-test for normally distributed variables. Fisher's exact test was applied for categorical variables, with a significance level of P < 0.05.
Results
Clinical characteristics
During the review period, 223 children presented with GI manifestations of COVID-19. Ninety-eight (43.94%) of these children presented with acute abdominal pain. However, 14 cases were excluded due to incomplete data; therefore, 84 patients fulfilled the criteria of this study.
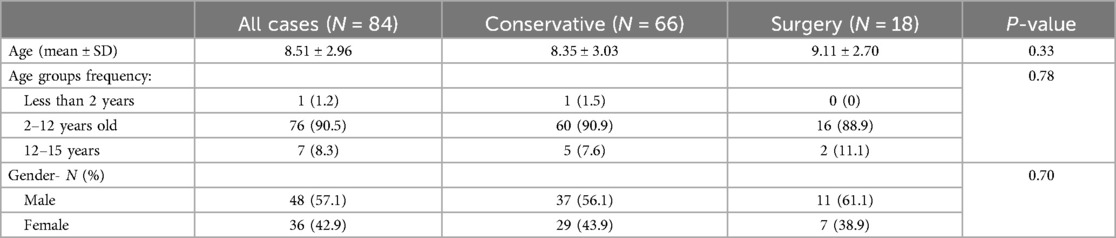
The age of the patients ranged from 6 months to 15 years (mean 8.51 ± 2.96 years). After performing ultrasound examinations (Appendix 1) and necessary laboratory investigations, the predominant presentation was right iliac fossa pain with a provisional diagnosis of acute appendicitis in 31 cases (36.9%). Generalized abdominal pain was noted in 17 cases (20.2%), ultrasonography revealed intussusception in 12 patients (14.3%), and 9 patients (10.7%) presented with MIS-C. The presentation mimicked acute cholecystitis was found in 14 patients (16.7%), and only one case presented with pancreatitis. There was no significant correlation between demographic data of the studied patients, likely due to the small sample size as shown in Table 1.
Surgical management
Acute appendicitis
Of the 31 patients presenting with acute appendicitis, surgical intervention was performed in 9 cases (8 laparotomies and 1 laparoscopy). Surgical findings in the first two cases revealed a non-inflamed appendix with congested serosa, enlarged mesenteric lymph nodes, and a considerable amount of peritoneal fluid. The remaining 7 cases were positive for purulent appendicitis.
Generalized abdominal pain
In patients presenting with generalized abdominal pain (n = 17), 5 cases (29.4%) required surgical intervention. Surgical findings in one of these cases included multiple perforations of the rectosigmoid and descending colon, diffuse wall thickening of the remaining colon, and an adherent pyogenic membrane, necessitating an ileostomy.
Intussusception
Out of 12 patients, 9 cases showed transient radiological intussusception with mild abdominal pain (7 cases presented with small bowel intussusception and 2 cases with ileocolic intussusception), all of which showed spontaneous resolution during follow-up after conservative treatment.
Hydrostatic reduction was performed in 2 cases with ileocolic intussusception, but it failed in one case, necessitating laparotomy. This revealed colo-colic intussusception and multiple enlarged mesenteric lymph nodes. One case with peritonitis and intestinal gangrene required bowel resection and anastomosis (Table 2).
Operative vs. non-operative outcomes
Our findings revealed a notable shift in managing acute abdomen during COVID-19, with successful conservative treatment in 66 (78.6%) patients, while 18 (21.4%) underwent surgical management, including laparotomy, laparoscopy, or drainage. There was no statistically significant difference between the groups (p = 0.17), likely due to the small sample size. Hospital stays ranged from 8 to 29 days (mean: 16.92 ± 3.55 days). Age variation was insignificant between the groups with different presentations, as detailed in Tables 2, 3.
Discussion
The coronavirus pandemic represents a medical paradigm shift, influencing our comprehension and treatment strategies for various illnesses. The decision to undergo surgical treatment can be problematic for children with COVID-19 due to the increased risk of postoperative complications. Therefore, it is generally advisable to avoid surgery unless deemed necessary (16, 17).
The current investigation identified 31 patients with appendicitis. The first case revealed intraoperative findings of a congested appendix with mesenteric adenitis and ileitis accompanied by peritoneal fluid. Unfortunately, this case experienced a challenging postoperative period, which caused the development of MIS-C. In the second case, diagnostic laparoscopy exhibited findings similar to the first but was managed conservatively. Subsequently, four complicated cases underwent appendectomy initially, while the remaining 25 cases received conservative treatment, with only three requiring subsequent surgery.
Overall, surgery was conducted in 29% of cases presenting with appendicitis. COVID-19 can lead to acute abdomen that mimics appendicitis, as supported by existing literature indicating cases where appendectomy was performed with histologically proven negative results (4, 6, 16). Conversely, during COVID-19, severe gastrointestinal involvement, including ileitis and mesenteric adenitis, can occasionally mimic appendicitis (3, 18, 19). Similar to our findings, there is a noticeable shift toward conservative treatment of appendicitis during the COVID-19 pandemic (20–24).
Another significant finding involves 17 cases presenting with generalized abdominal pain. The initial laparotomy in the first case revealed peritoneal fluid in the pelvis, right and left iliac fossa, hepatorenal pouch, mesenteric adenitis, and edematous intestine, necessitating drainage. The second case underwent laparoscopy, displaying diffuse edematous terminal ileum and colon with intra-abdominal fluid and mesenteric adenitis. Subsequently, two cases received drainage in the right iliac fossa, while the remaining 14 cases were treated conservatively with spontaneous resolution, except in one case where laparotomy revealed sigmoid colon perforation. In four cases, conservative treatment was employed, and anticoagulant therapy was administered due to suspicion of mesenteric thrombosis based on duplex study findings of mesenteric vessels.
One case showed multiple perforations in the rectosigmoid region and descending colon. The involvement of the sigmoid colon may be attributed to evidence suggesting that the vascular effects of COVID-19, such as ischemic colitis, tend to impact the left colonic flexure and sigmoid colon more than the distal rectum, concerning their dual blood supply (25, 26).
Conservative methods proved effective in treating diffuse abdominal pain. This aligns with other studies recommending conservative treatment with regular reassessment, as most cases naturally resolve without intervention. Moreover, multiple lines of evidence indicate that intraperitoneal fluid results from increased intestinal permeability, and bacteriological examinations yield negative results (4, 5, 27).
Among patients in our study, 14 cases presented with symptoms resembling acute cholecystitis, particularly abdominal pain in the right hypochondrium. Ultrasound examinations revealed mild hepatomegaly with gallbladder wall thickening and mesenteric adenitis in three cases, mild hepatomegaly with a small amount of free fluid in six cases, and gallbladder wall thickening and edema with mesenteric adenitis in five cases. All these cases responded to conservative treatment.
The pathogenesis of hepatobiliary involvement is attributed to mild sinusoidal lymphocytic infiltration and sinusoidal dilatation. These factors result in mild pain and manifest on ultrasound as mild hepatomegaly with various gall bladder-related changes (28, 29).
Previous literature has documented intussusception as a cause of abdominal pain during COVID-19. However, no documented evidence of transient intussusception associated with COVID-19 exists in the literature (4). Transient intussusception is a distinct phenomenon that may impact children (30–32). The pathogenesis of transient intussusception associated with COVID-19 is not clearly defined, but it may be attributed to pathological features such as mesenteric adenitis, bowel wall thickness, and edema associated with COVID-19. This pathogenic mechanism could contribute to the occurrence of intussusception, as observed in cases involving other intestinal viruses (4, 33).
MIS-C is a systemic hyperinflammatory syndrome secondary to COVID-19 infection; its diagnostic criteria include abdominal pain, diarrhea, vomiting, colitis, ileitis, abnormal liver function tests, and ascites (14, 15, 34). It impacts multiple organs and can lead to shock with heart dysfunction, with predominant involvement of the gastrointestinal tract observed in 70%–90% of cases. The gastrointestinal symptoms associated with MIS-C may mimic those of an acute abdomen (33, 35). In this study, 9 cases with MIS-C presented with diffuse abdominal pain and ultrasound findings of mesenteric adenitis and ileitis with fluid collection. Drainage was performed in 2 cases, while the remaining 7 cases responded well to conservative treatment. Similarly, Lo Vecchio et al. performed drainage in 5 out of 21 children (23.8%), with most fluid collections resolving over time and the fluid being bacteriologically sterile (4).
Abdominal pain in MIS-C can manifest in different presentations, such as pseudo-appendicitis pain and diffuse abdominal pain. The associated pathological changes in the abdomen are diverse and may include mesenteric adenitis, ileitis, and thickening of the bowel loop, with a predominant presence of fluid collection (36, 37). Appendicitis in MIS-C is typically associated with a patent lumen, serositis, and perivasculitis. Conservative treatment approaches are recommended for these cases (4, 38).
Acute abdominal pain in children has traditionally been evaluated surgically to exclude common causes such as appendicitis or perforated intestine. However, the COVID-19 pandemic has necessitated a shift in approach due to similarities between COVID-19 and other coronaviruses affecting gastrointestinal enterocytes and causing abdominal pain (39). The primary challenge now is distinguishing between surgical causes of acute abdominal pain and those related to COVID-19, emphasizing the need for precise diagnostic methods to prevent medical errors and unnecessary surgeries.
While laparoscopic surgery is considered the gold standard for appropriate cases of acute abdominal pain, our study utilized laparoscopy in only 2 cases (11.1%) out of 18 patients. Initially, there was concern about the safety of laparoscopy during the pandemic, with some studies suggesting an increased risk of virus particle aerosolization during CO2 insufflation (40, 41).
Despite the WHO declaring on May 5, 2023, that COVID-19 is no longer an international public health emergency, the disease remains prevalent. Therefore, it is essential to consider COVID-19 as a potential cause of abdominal pain in all cases.
Our study's relatively small number of cases can be attributed to several factors. COVID-19 presentation in pediatric patients is less common than in adults, and respiratory symptoms are more prevalent than abdominal ones. Additionally, some cases were transferred to other centers following local protocols. Despite these limitations, our retrospective study provides valuable data on a globally significant disease. It captures a diverse range of presentations of acute abdomen in pediatrics, highlighting the need for further research to enhance our understanding of this complex issue.
Conclusion
Acute abdominal pain in children during COVID-19 is a common occurrence, often resolving without surgical intervention due to the self-limiting nature of most gastrointestinal manifestations. It is crucial to consider COVID-19 as a differential diagnosis in patients presenting with acute abdominal pain, particularly in cases of atypical appendicitis and intussusception. Meticulous evaluation and accurate diagnosis are essential to avoid unnecessary surgical interventions in children with persistent abdominal pain.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Local Ethics Committee of Faculty of Medicine, South Valley University, Qena, Egypt. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
NA-H: Writing – original draft. MN: Methodology, Writing – original draft. MA: Formal Analysis, Writing – review & editing. MF: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tsabouri S, Makis A, Kosmeri C, Siomou E. Risk factors for severity in children with coronavirus disease 2019: a comprehensive literature review. Pediatric Clinics. (2021) 68(1):321–38. doi: 10.1016/j.pcl.2020.07.014
2. Akobeng AK, Grafton-Clarke C, Abdelgadir I, Twum-Barimah E, Gordon M. Gastrointestinal manifestations of COVID-19 in children: a systematic review and meta-analysis. Frontline Gastroenterol. (2021) 12(4):332–7. doi: 10.1136/flgastro-2020-101529
3. Tullie L, Ford K, Bisharat M, Watson T, Thakkar H, Mullassery D, et al. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. The Lancet Child & Adolescent Health. (2020) 4(7):e19–20. doi: 10.1016/s2352-4642(20)30165-6
4. Vecchio AL, Garazzino S, Smarrazzo A, Venturini E, Poeta M, Berlese P, et al. Factors associated with severe gastrointestinal diagnoses in children with SARS-CoV-2 infection or multisystem inflammatory syndrome. JAMA network Open. (2021) 4(12):e2139974. doi: 10.1001/jamanetworkopen.2021.39974
5. Espiñeira C, Romero HS, Góngora RE, Vega ML, Calderón JL. Acute abdomen in COVID-19 disease: the pediatric surgeon’s standpoint. Cirugía Pediátrica (English Edition). (2021) 34(1):3–8. Available online at: https://secipe.org/coldata/upload/revista/2021_34-1_3.pdf
6. Ataollahi M, Hamzavi SS, Dehghani SM, Haghighat M, Imanieh MH, Honar N, et al. Prevalence of COVID-19 in children with gastrointestinal manifestations: a cross-sectional study of 184 cases in 2020–2021. Arch Pediatr Infect Dis. (2022) 10(4):19–27. doi: 10.5812/pedinfect-121640
7. Bolia R, Dhanesh Goel A, Badkur M, Jain V. Gastrointestinal manifestations of pediatric coronavirus disease and their relationship with a severe clinical course: a systematic review and meta-analysis. J Trop Pediatr. (2021) 67(2):fmab051. doi: 10.1093/tropej/fmab051
8. Meyer JS, Robinson G, Moonah S, Levin D, McGahren E, Herring K, et al. Acute appendicitis in four children with SARS-CoV-2 infection. J Pediatr Surg Case Rep. (2021) 64:101734. doi: 10.1016/2Fj.epsc.2020.101734
9. Belhadjer Z, Méot M, Bajolle F, Khraiche D, Legendre A, Abakka S, et al. Acute heart failure in multisystem inflammatory syndrome in children in the context of global SARS-CoV-2 pandemic. Circulation. (2020) 142(5):429–36. doi: 10.1161/circulationaha.120.048360
10. Rouva G, Vergadi E, Galanakis E. Acute abdomen in multisystem inflammatory syndrome in children: a systematic review. Acta Paediatr. (2022) 111(3):467–72. doi: 10.1111/apa.16178
11. Yock-Corrales A, Lenzi J, Ulloa-Gutiérrez R, Gómez-Vargas J, Antúnez-Montes OY, Aida JA, et al. Acute abdomen and appendicitis in 1010 pediatric patients with COVID-19 or MIS-C: a multinational experience from Latin America. Pediatr Infect Dis J. (2021) 40(10):e364–9. doi: 10.1097/inf.0000000000003240
12. Jackson RJ, Chavarria HD, Hacking SM. A case of multisystem inflammatory syndrome in children mimicking acute appendicitis in a COVID-19 pandemic area. Cureus. (2020) 12(9):e10722. doi: 10.7759/cureus.10722
13. Mostafa AS, Abdalbaky A, Fouda EM, Shaaban HH, Elnady HG, Hassab-Allah M, et al. Practical approach to COVID-19: an Egyptian pediatric consensus. Egypt Pediatr Assoc Gaz. (2020) 68:1–8. doi: 10.1186/s43054-020-00037-9
14. Brief S, World Health Organization. Multisystem inflammatory syndrome in children and adolescents with COVID-19. Geneva: WHO (2020). Available online at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19
15. World Health Organization. Living Guidance for Clinical Management of COVID-19: Living Guidance, 23 November 2021. Geneva: World Health Organization (2021). Available online at: https://iris.who.int/bitstream/handle/10665/338882/WHO-2019-nCoV-clinical-2021.1-eng.pdf
16. Haffner MR, Le HV, Saiz AM, Han G, Fine J, Wolinsky P, et al. Postoperative in-hospital morbidity and mortality of patients with COVID-19 infection compared with patients without COVID-19 infection. JAMA network Open. (2021) 4(4):e215697. doi: 10.1001/2Fjamanetworkopen.2021.5697
17. Troisi J, Venutolo G, Tanya MP, Carri MD, Landolfi A, Fasano A. COVID-19 and the gastrointestinal tract: source of infection or merely a target of the inflammatory process following SARS-CoV-2 infection? World J Gastroenterol. (2021) 27(14):1406. doi: 10.3748/wjg.v27.i14.1406
18. Abdalhadi A, Alkhatib M, Mismar AY, Awouda W, Albarqouni L. Can COVID 19 present like appendicitis? IDCases. (2020) 21:e00860. doi: 10.1016/j.idcr.2020.e00860
19. Gerall CD, DeFazio JR, Kahan AM, Fan W, Fallon EM, Middlesworth W, et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. (2021) 56(5):905–10. doi: 10.1016/j.jpedsurg.2020.10.008
20. Kvasnovsky CL, Shi Y, Rich BS, Glick RD, Soffer SZ, Lipskar AM, et al. Limiting hospital resources for acute appendicitis in children: lessons learned from the US epicenter of the COVID-19 pandemic. J Pediatr Surg. (2021) 56(5):900–4. doi: 10.1016/j.jpedsurg.2020.06.024
21. Hegde B, Garcia E, Hu A, Raval M, Takirambudde S, Wakeman D, et al. Management of pediatric appendicitis during the COVID-19 pandemic: a nationwide multicenter cohort study. J Pediatr Surg. (2023) 58(7):1375–82. doi: 10.1016/j.jpedsurg.2022.08.005
22. Theodorou CM, Beres AL, Nguyen M, Castle SL, Faltermeier C, Shekherdimian S, et al. Statewide impact of the COVID pandemic on pediatric appendicitis in California: a multicenter study. J Surg Res. (2021) 267:132–42. doi: 10.1016/j.jss.2021.05.023
23. Emile SH, Hamid HK, Khan SM, Davis GN. Rate of application and outcome of non-operative management of acute appendicitis in the setting of COVID-19: systematic review and meta-analysis. J Gastrointest Surg. (2021) 25(7):1905–15. doi: 10.1007/s11605-021-04988-1
24. Chan KH, Lim SL, Damati A, Maruboyina SP, Bondili L, Hanoud AA, et al. Coronavirus disease 2019 (COVID-19) and ischemic colitis: an under-recognized complication. Am J Emerg Med. (2020) 38(12):2758–e1. doi: 10.1016/j.ajem.2020.05.072
25. Giuffrè M, Di Bella S, Sambataro G, Zerbato V, Cavallaro M, Occhipinti AA, et al. COVID-19-induced thrombosis in patients without gastrointestinal symptoms and elevated fecal calprotectin: hypothesis regarding mechanism of intestinal damage associated with COVID-19. Trop Med Infect Dis. (2020) 5(3):147. doi: 10.3390/tropicalmed5030147
26. Calinescu AM, Vidal I, Grazioli S, Lacroix L, Wildhaber BE. Beware of too aggressive approach in children with acute abdomen during COVID-19 outbreak!. Ann Surg. (2020) 272(3):e244–5. doi: 10.1097/SLA.0000000000004100
27. Langroudi AP, Varniab ZS, Amouei M, Pak N, Khosravi B, Mirsharifi A, et al. Findings of abdominal imaging in patients with COVID-19–part 1: hollow organs. Middle East J Dig Dis. (2022) 14(3):278. doi: 10.34172/mejdd.2022.284
28. Blumfield E, Levin TL, Kurian J, Lee EY, Liszewski MC. Imaging findings in multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease (COVID-19). Am J Roentgenol. (2021) 216(2):507–17. doi: 10.2214/ajr.20.24032
29. Li Y, Xiao SY. Hepatic involvement in COVID-19 patients: pathology, pathogenesis, and clinical implications. J Med Virol. (2020) 92(9):1491–4. doi: 10.1002/jmv.25973
30. Munden MM, Bruzzi JF, Coley BD, Munden RF. Sonography of pediatric small-bowel intussusception: differentiating surgical from nonsurgical cases. Am J Roentgenol. (2007) 188(1):275–9. doi: 10.2214/ajr.05.2049
31. Güney LH, Fakıoğlu E, Acer T, Ötgün İ, Arslan EE, Akıllı MS, et al. Is every intussusception treatment an emergency intervention or surgery? Ulus Travma Acil Cerrahi Derg. (2016) 22(2):139–44. doi: 10.5505/tjtes.2015.06013
32. Okimoto S, Hyodo S, Yamamoto M, Nakamura K, Kobayashi M. Association of viral isolates from stool samples with intussusception in children. Int J Infect Dis. (2011) 15(9):e641–5. doi: 10.1016/j.ijid.2011.05.008
33. Zou H, Lu J, Liu J, Wong JH, Cheng S, Li Q, et al. Characteristics of pediatric multi-system inflammatory syndrome (PMIS) associated with COVID-19: a meta-analysis and insights into pathogenesis. Int J Infect Dis. (2021) 102:319–26. doi: 10.1016/j.ijid.2020.11.145
34. Schlapbach LJ, Andre MC, Grazioli S, Schöbi N, Ritz N, Aebi C, et al. Best practice recommendations for the diagnosis and management of children with pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS; multisystem inflammatory syndrome in children, MIS-C) in Switzerland. Front Pediatr. (2021) 9:667507. doi: 10.3389/fped.2021.667507
35. Nakra NA, Blumberg DA, Herrera-Guerra A, Lakshminrusimha S. Multi-system inflammatory syndrome in children (MIS-C) following SARS-CoV-2 infection: review of clinical presentation, hypothetical pathogenesis, and proposed management. Children. (2020) 7(7):69. doi: 10.3390/children7070069
36. Lazova S, Tomov L, Miteva D, Tzotcheva I, Priftis S, Velikova T. Clinical and laboratory manifestation of gastrointestinal involvement in MIS-C: a single-center observational study. Gastroenterol Insights. (2023) 14(2):236–48. doi: 10.3390/gastroent14020017
37. Lishman J, Kohler C, de Vos C, Van der Zalm MM, Itana J, Redfern A, et al. Acute appendicitis in multisystem inflammatory syndrome in children with COVID-19. Pediatr Infect Dis J. (2020) 39(12):e472–3. doi: 10.1097/inf.0000000000002900
38. Malhotra A, Sturgill M, Whitley-Williams P, Lee YH, Esochaghi C, Rajasekhar H, et al. Pediatric COVID-19 and appendicitis: a gut reaction to SARS-CoV-2? Pediatr Infect Dis J. (2021) 40(2):e49–55. doi: 10.1097/inf.0000000000002998
39. Saviano A, Brigida M, Petruzziello C, Zanza C, Candelli M, Morabito Loprete MR, et al. Intestinal damage, inflammation and microbiota alteration during COVID-19 infection. Biomedicines. (2023) 11(4):1014. doi: 10.3390/biomedicines11041014
40. Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. (2020) 272(1):e5–6. doi: 10.1097/sla.0000000000003924
41. Prato A P, Conforti A, Almstrom M, Van Gemert W, Scuderi MG, Khen-Dunlop N, et al. Management of COVID-19-positive pediatric patients undergoing minimally invasive surgical procedures: systematic review and recommendations of the board of European society of pediatric endoscopic surgeons. Front Pediatr. (2020) 8:259. doi: 10.3389/fped.2020.00259
Appendix 1
Ultrasound findings
In all cases especially MIS-C
• Mesenteric fat inflammation
• Intestinal wall thickening
• Mesenteric adenopathy
• Peritoneal fluid collection
US finding in cases mimic acute appendicitis
Appendix diameter 6–7 mm
• Hypoechoic wall not echogenic.
• Mildly inflamed ilium.
• Not encysted or turbid.
• Few mesenteric LNs.
US finding in cases mimic cholecystitis
Thickening of gall bladder wall, hepatomegaly, decreased echogenicity of the liver.
US finding in cases of intussusception
• 3 cases with ileo-colic intussusception in epigastrium and mesenteric adenitis with thickened ileum and free fluid
• 7 cases with ileo-ileal intussusception and mesenteric adenitis with thickened ileum and free fluid
2 cases with ileo-colic intussusception in Rt lumbar and mesenteric adenitis with thickened ileum and free fluid.
Keywords: acute abdominal pain, pediatric, COVID-19, appendicitis, multisystemic inflammatory syndrome in children (MIS-C)
Citation: Abo-Halawa N, Negm MA, Arafa M and Fathy M (2024) Surgical aspects of pediatric abdominal pain in the era of COVID-19: clinical consideration and outcomes. Front. Pediatr. 12:1400638. doi: 10.3389/fped.2024.1400638
Received: 13 March 2024; Accepted: 29 August 2024;
Published: 30 September 2024.
Edited by:
Nikolaos Zavras, University General Hospital Attikon, GreeceReviewed by:
Dolores Freire, University of Guayaquil, EcuadorSanja Miodrag Sindjic Antunovic, University of Belgrade, Serbia
Wojciech Górecki, Jagiellonian University, Poland
Copyright: © 2024 Abo-Halawa, Negm, Arafa and Fathy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nezar Abo-Halawa, ZHJuZXphcjFAZ21haWwuY29t
 Nezar Abo-Halawa
Nezar Abo-Halawa Mohamed A. Negm
Mohamed A. Negm Mohamed Arafa
Mohamed Arafa Mohamed Fathy
Mohamed Fathy