
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 09 May 2024
Sec. Pediatric Endocrinology
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1362076
Background: A potential association between the onset of diabetes and normal birth weight (NBW) has been discovered. Diverse conclusions and study methodologies exist regarding the connection between low birth weight (LBW) and impaired glucose tolerance in children, underscoring the need for further robust research. Our institution is embarking on this study to thoroughly examine the association between LBW and impaired glucose tolerance in children.
Methods: We conducted searches on Cochrane Library, ScienceDirect, EMBASE, PubMed, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature data (CBM) online database, VIP full-text Database, and Wanfang Database to identify correlation analyses or case-control studies investigating the relationship between LBW and abnormal glucose tolerance in children. The search spanned from January 2010 to September 2023. The quality of observational studies was evaluated using the Newcastle–Ottawa Scale (NOS) tool. Data synthesis was performed using the statistical software RevMan 5.3 for meta-analysis.
Results: Based on the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines, we finally included 10 clinical control studies consisting of a total of 2971 cases. There wasn’t considerably change in blood sugar levels among LBW, NBW and high birth weight (HBW) infants (P > 0.05). There was no significant difference in insulin levels between LBW infants and NBW infants (P > 0.05). The HOMA-IR of LBW infants was considerably higher than that of NBW infants (P < 0.05). The risk of abnormal glucose tolerance in LBW infants was 0.42 times higher than that in NBW and HBW infants [Fisher's Z = 0.42, 95% CI = (0.09, 0.75), P = 0.01].
Conclusion: LBW is associated with an increased risk of abnormal glucose tolerance, as indicated by elevated HOMA-IR level in LBW infants compared to NBW and HBW pediatric population. Further research is needed to confirm and expand upon these findings to better understand the complex relationship between LBW and impaired glucose tolerance in children.
In China, the prevalence of diabetes has surged, with over 30 million individuals affected, marking a substantial rise from 0.8% in 1980 to 3.5% in 2000 (1, 2). A study conducted from 2015 to 2017 revealed that in China, the overall prevalence of diabetes among adults is 12.8%, including a newly diagnosed diabetes prevalence of 6.8% and a self-reported diabetes prevalence of 6.0% (3–6). The rising incidence of diabetes has led to an increased prevalence of the condition among young adults, and reports indicate that diabetes can manifest in individuals as young as 13 years old (7, 8). The presence of concurrent complications such as hyperlipidemia, hypertension, and other conditions alongside diabetes has garnered increasing attention in terms of the onset, progression, outcomes, and management of diabetes. Diabetic complications are more common in macrovascular and microvascular diseases, and abnormal blood lipid metabolism is involved in the whole process of this disease. A randomized controlled trial study has demonstrated the intricate interplay between blood glucose and blood lipids in individuals with diabetes (9–11).
Given the rising incidence and prevalence of type 2 diabetes among children and adolescents, this issue may emerge as a significant public health concern impacting both developed and developing nations. Consequently, from a population standpoint, it is imperative to identify potential risk factors and identify susceptible groups that could benefit from screening and preventive measures (12–14). So far, scholars have explored the etiology of diabetes from various perspectives and directions, including pathology, genetics, genomics, social factors, and other fields. The formation of diabetes corresponds to abnormal birth weight (15, 16). The occurrence of high birth weight infants, often stemming from fetal overnutrition, maternal diabetes, and other maternal health conditions, can significantly predispose individuals to obesity and diabetes in adulthood, typically around the age of 18. This association may be attributed to genetic polymorphisms and the onset of insulin resistance (17). Additionally, abnormal insulin secretion during the fetal period, impacting fetal growth and development, may contribute to the prevalence of infants with low birth weight (LBW) and heighten the risk of diabetes in adulthood (18, 19).
At present, numerous investigations have explored the link between LBW and impaired glucose tolerance in children. However, these studies yield varying conclusions and employ designs, leading to poor applicability. The findings of a single study regarding the correlation between LBW and impaired glucose tolerance in children may lack conviction without robust scientific support. Therefore, additional research is warranted, necessitating reputable scientific studies to comprehensively evaluate this relationship. Consequently, a thorough, quantitative, and systematic meta-analysis of independent studies with similar objectives was conducted to investigate the association between LBW and impaired glucose tolerance in children. This analysis aims to provide valuable insights to inform further exploration of the underlying causes of type 2 diabetes and to enhance eugenic strategies.
A computer-based search was carried out across multiple databases, including CochraneLibrary, ScienceDirect, EMBASE, Wanfang Database, the Chinese Biomedical Literature Data (CBM), VIP Full-text Database, China National Knowledge Infrastructure (CNKI). This extensive search strategy encompassed a wide range of sources, including both degree papers, conference papers, Chinese and foreign periodicals, news articles, and manual searches, among others.
The main aim was to collect pertinent data regarding the association between LBW and impaired glucose tolerance in children. The literature retrieval process utilized a combination of free-text and subject-specific keywords. Key search terms such as “newborn,” “low birth weight,” and “impaired glucose tolerance” were employed, with the search period spanning from January 2010 onwards. This comprehensive strategy aimed to encompass the latest and most relevant research findings in the field.
(1) Observational studies that were published in full-text format.
(2) Inclusion of newborns with birth weight of less than 1,500 g.
(3) Assessment of the correlation between LBW and impaired glucose tolerance in children.
(4) Adjustment or control for the potential confounding factors, with the reporting of relative risk factors or the comparison of blood glucose, insulin, and Model Assessment for Insulin Resistance (HOMA-IR) indices with those of normal newborns and high-birth-weight newborns. Based on a previous literature (20), children were classified into LBW (<2,500 g), normal birth weight (NBW; 2,500–3,999 g), and high birth weight (HBW; ≥4,000 g). Impaired glucose tolerance was defined as having 2-h plasma glucose concentration (2hPG) 140–199 mg/dl (21).
(1) Studies with incomplete and unusable data.
(2) Duplicate research content, with preference given to the most recent study.
(3) Reviews, editorials, preclinical studies, and literature that did not directly relate to the special purpose of the current meta-analysis.
(4) Clinical cases, which were not considered in this particular meta-analysis.
The process of extracting data and screening books followed a rigorous and systematic approach.
Two researchers conducted separate reviews of the selected literature and extracted relevant information.
These researchers also assessed the quality of the included studies.
To ensure accuracy and consistency, the results of the independent screenings and data extractions were cross-checked. Any discrepancies were addressed through discussion and consensus. In instances of unresolved discrepancies, a third researcher was consulted to provide adjudication.
NoteExpress document management software and Excel office software were employed for data management and extraction, facilitating efficient organization and analysis of the research data.
In cases where the literature lacked necessary information, the authors of the respective articles were contacted to request Supplementary Data.
The information retrieved from the data comprised: (1) the authors’ names, the publishing year and the country of the institute; (2) the characteristics of the study design; (3) the characteristics of participants, including health status, sample size and average age; (4) the number of normal weight, overweight and LBW newborns; and (5) confounding factors adjusted or controlled when reporting correlations.
For assessing the quality of observational studies in this meta-analysis, the Newcastle-Ottawa Scale (NOS) tool was utilized. Studies with a NOS score of ≥6 were categorized as medium to high quality, whereas those with an NOS score <6 were classified as low quality.
RevMan 5.3 software, derived from the Cochrane Collaboration, was used for conducting meta-analyses. The mean values, and standard deviations for Blood glucose levels, insulin levels, HOMA-IR in each group were input into RevMan 5.3 for analysis. The weighted mean difference (WMD) was used as the effect size, and 95% confidence intervals (CI) were calculated. Heterogeneity was evaluated using the χ2 test and the I2 statistic, which quantifies the total variation across studies attributed to heterogeneity. P-value below 0.05 was deemed statistically significant (22, 23).
In adherence to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines, the study initiated with a computer-based database search, resulting in the retrieval of 742 studies. After eliminating duplicate studies, 561 unique studies remained. These papers were then subject to preliminary screening, during which 308 studies were reviewed.
After the initial screening, 142 studies met the inclusion criteria for further assessment, while irrelevant studies, reviews, case reports, and uncontrolled documents were excluded. Subsequently, the full texts of the selected literature underwent thorough examination, with papers containing incomplete data or lacking key outcome indicators being excluded. Ultimately, the study integrated data from 10 clinical control studies, comprising a total of 2,971 samples. This meticulous selection process ensured that the included studies were pertinent, met the required criteria, and enhanced the robustness of the meta-analysis. Figure 1 illustrates the flow chart detailing the literature screening process, while Table 1 presents the fundamental characteristics identified in the literature.
All the literatures described the detailed intervention methods and observation indicators, and all the literatures did not describe the quantity and causes of blind procedures, as well as missed follow-up or withdrawal, in detail. The NOS scale study indicated that low-quality literature had a score of <6, while high-quality literature had a score of ≥6 (Table 2).
The blood glucose levels of each group were examined using meta, and the heterogeneity test results revealed that LBW vs. NBW: Chi2 = 25.86, I2 = 85%, P < 0.0001, df = 4; LBW vs. HBW: Chi2 = 0.31, I2 = 0%, P = 0.58, df = 1. From the analysis shown as Figures 2, 3, there was no statistical difference in blood sugar levels between LBW infants and normal weight and overweight infants (P > 0.05).
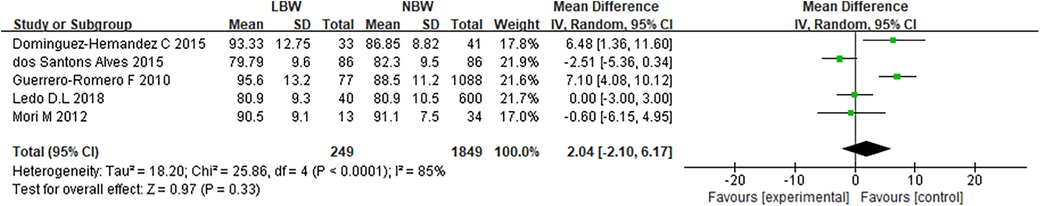
Figure 2. Comparison of blood glucose levels between normal weight and low birth weight children forest analysis chart F.
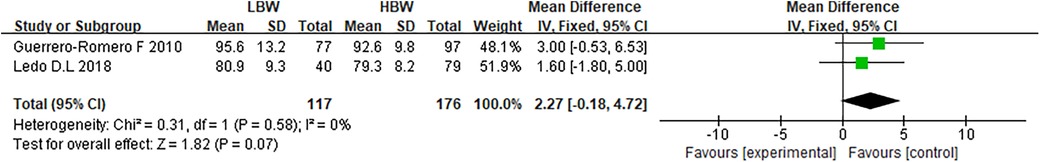
Figure 3. Comparison of blood glucose levels between overweight and low birth weight children forest analysis map.
A meta-analysis of the comparative results of insulin levels was performed in each group. In the comparison between LBW and NBW, with four degrees of freedom, the Chi2 statistic yielded a value of 6.85, resulting in a p-value of 0.14 and an I2 of 42%. These findings indicate moderate heterogeneity among the studies for this comparison. In the comparison between LBW and HBW, the Chi-squared value was 11.78 with one degree of freedom, resulting in a p-value of 0.0006, and I2 was determined to be 92%. These results indicate a high level of heterogeneity among the studies for this comparison. According to the analysis of the random-effect model (Figure 4), there wasn't considerably difference in insulin level between LBW infants and normal weight children (P > 0.05).
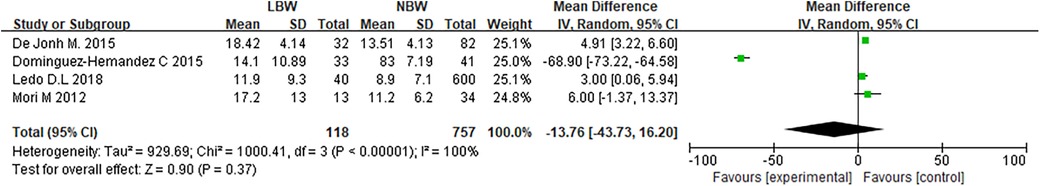
Figure 4. Comparison of insulin levels between normal weight and low birth weight children forest analysis map.
In the comparison between LBW and normal birth weight (NBW) children (Figure 5), with four degrees of freedom, the Chi-squared statistic was 6.85, yielding a p-value of 0.14 and an I2 of 42%, indicating a moderate level of heterogeneity among the studies.
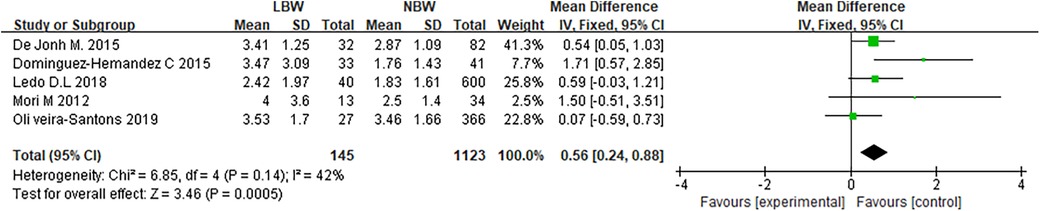
Figure 5. Forest analysis map of HOMA-IR comparison between normal weight and low birth weight children.
In the comparison of LBW with HBW children (Figure 6), with one degree of freedom, the Chi-squared statistic was 11.78, yielding a p-value of 0.0006, and I2 was determined to be 92%, suggesting a high level of heterogeneity among the studies for this comparison. The meta-analysis findings reveal that LBW infants have significantly higher HOMA-IR values when compared to NBW children (P < 0.05). Nonetheless, in comparing LBW to HBW children, the observed high level of heterogeneity underscores the need for caution in interpreting the results. This heterogeneity indicates significant variability among the included studies in this comparison, potentially influencing the overall findings.
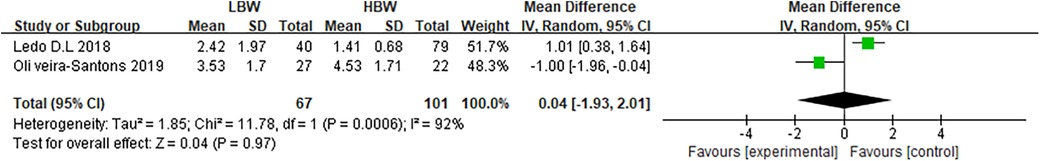
Figure 6. Forest analysis map of HOMA-IR comparison between overweight and low birth weight children.
This study encompassed data from 10 clinical controlled studies, comprising a total of 2,971 samples, and conducted a meta-analysis on the association between LBW and HOMA-IR. The heterogeneity test results indicated significant heterogeneity, with Chi2 = 912.67, df = 7, P < 0.00001, and I2 = 99%. These findings suggest a substantial level of variation among the included studies’ meta-analyses, assessed using a random effects model (Figure 7), the risk of abnormal glucose tolerance in LBW newborns was 0.42 times higher than that in normal and overweight children [Fisher's Z = 0.42,95% CI:0.09–0.75, P = 0.01].
The funnel diagram was created using the blood glucose, insulin level, HOMA-IR value and correlation analysis results of each group, and an examination of publication bias was conducted (Supplementary Figures S1–S4). The results revealed that while a small proportion of the included studies exhibited asymmetry, the majority of funnel plots appeared symmetrical, suggesting potential publication bias in the included literature. This bias could be linked to the heterogeneity observed in the study.
Previous research has shown a link between diabetes and LBW (33). The “Fetal Origin hypothesis,” proposed in the 1990s, suggests that the conditions experienced during fetal intrauterine development significantly influence the risk of developing diseases in adulthood. According to this hypothesis, individuals born with LBW are at a considerably higher risk of developing type 2 diabetes later in life (34). Preterm delivery or intrauterine growth restriction is the most common cause of LBW (35). 63% of LBW infants are born prematurely, while the remaining cases are attributed to intrauterine dysplasia. It is noteworthy that nearly all very low birth weight infants are born prematurely, with some being extremely premature, with gestational ages of less than 25 weeks. In utero stunting of development in LBW infants impairs the development and function of the pancreas, leading to problems with lipid and glucose metabolism and hypertension in adulthood (36, 37). Genetic research indicates that variations in susceptibility genes associated with type 2 diabetes may also be linked to LBW. This suggests a potential genetic predisposition for both lower birth weight and an increased risk of type 2 diabetes later in life. These findings underscore the intricate interplay between genetic factors and health outcomes across the lifespan (38). If an individual has a low birth weight or childhood weight, there is a tendency for rapid weight gain in adulthood (after 18 years of age) due to dietary changes, which significantly increases the risk of developing diabetes and other related metabolic disorders. Reduced birth weight has been associated with the upregulation of certain genes, commonly known as “thrift genes.” These genes might be involved in metabolic adaptations to prenatal undernutrition. Furthermore, there is evidence connecting LBW to a higher risk of developing several disorders, including diabetes, in adulthood, suggesting that early life factors, including birth weight, can influence gene expression and can aid in the later-life development of chronic illnesses.
Recently, LBW infants are prone to developing obesity, insulin resistance, hypertension, and vascular diseases in adulthood. Additionally, the incidence and mortality rates of other conditions such as enterocolitis, late-onset septicemia, and intraventricular hemorrhage are elevated in this population (39). The prevalence of diabetes and hypertension in LBW infants heightened significantly in adulthood. A survey has shown that the incidence of type 2 diabetes and birth weight are correlated in a U-shaped manner, and the quantity of diabetes cases complicated with hypertension in LBW is significantly increased. Diabetes is also associated with high birth weight, while hypertension is notably more prevalent among high birth weight infants. It is hypothesized that hypertension in high birth weight infants and LBW infants may arise from distinct metabolic phenotypes or similar environmental factors. Moreover, LBW infants exhibit a significantly higher prevalence of hyperlipidemia compared to those with normal birth weight (40). Previous study has found that 300 cases of high birth weight infants, and the results show the detection rates of overweight and obesity in the macrosomia group (13.10% vs. 2.86%) are higher than those in the control group (9.69% vs. 1.61%) (41), which suggested that the risk of insulin resistance and abnormal lipid metabolism in abnormal birth weight infants is greater than that in normal birth weight infants. China's Chinese multi-provincial Study on Risk Factors of Cardiovascular Diseases (CMCS) has suggested that the proportion of diabetic patients with abnormal blood lipid metabolism is considerably higher, and the proportion of diabetic patients with atherosclerosis risk factors such as coronary heart disease, cerebral infarction and venous thrombosis is also significantly higher than that of non-diabetic patients.
More and more evidence shows that the LBW of newborns is directly related to the abnormal glucose tolerance of children. The blood sugar and insulin levels of LBW newborns, normal newborns and overweight newborns were analyzed by meta-analysis. The findings indicated that there was not a significant variation between the blood sugar levels of LBW newborns and overweight and normal newborns. Meta-analysis of the comparison results of HOMA-RI values in each group showed that the HOMA-IR values of LBW infants were considerably higher. It is suggested that there is a certain correlation between LBW of newborns and HOMA-IR. Meta-analysis was made on the correlation between LBW and HOMA-IR, and random effect model analysis showed the risk of abnormal glucose tolerance in LBW newborns was 0.42 times higher than that in normal and overweight children [Fisher's SZ = 0.42, P = 0.01, 95%CI = (0.09, 0.75)]. Through an analysis of existing research in this domain, it is evident that there exists a connection between abnormal glucose tolerance and atypical birth weight in LBW infants. This association cannot be solely attributed to factors related to the fetus itself, prenatal malnutrition, or the intrauterine environment; rather, it encompasses various other contributing factors. These factors encompass aspects related to the pregnant woman's health, as well as lifestyle choices and dietary habits during adulthood. Additionally, genetic modifications resulting from certain factors in adulthood may also influence this intricate relationship. Understanding these multifaceted connections is crucial for comprehensively addressing and managing health risks associated with abnormal glucose tolerance and birth weight.
However, the study has certain limitations that warrant consideration:
(1) Stringent Criteria for Inclusion and Exclusion: The study employed rigorous criteria for inclusion and exclusion, leading to a relatively small number of included studies. Furthermore, detailed subgroup analysis was not conducted on studies displaying heterogeneity. This limited the diversity of the included literature and may affect the generalizability of the findings.
(2) Inconsistent Treatment Protocols and Outcome Measures: Variability in the treatment protocols and outcome indicators across the included studies may introduce heterogeneity and impact the reliability of the outcomes.For example, insulin level is influenced by age and gender (42). Therefore, these factors may influence the results in this study. To bolster the robustness of the findings, it is imperative to conduct further research, encompassing high-quality correlation studies and case-control trials. These endeavors will provide a deeper understanding of the relationship between abnormal glucose tolerance and birth weight, thus advancing our knowledge in this critical area of study.
It has been shown that LBW in babies is associated with poor glucose tolerance in pediatric population and a higher chance of type 2 diabetes in adults. This underscores the significance of preventive measures to manage birth weight abnormalities.Highlighting the significance of dietary and exercise management during the perinatal and developmental stages is crucial for mitigating the risk of diabetes. These insights underscore the necessity of early interventions and a comprehensive healthcare approach to mitigate the enduring adverse impacts of low birth weight on health outcomes.
The datasets used and analyzed during the current study available from the corresponding author on reasonable request.
JM: Data curation, Formal Analysis, Writing – original draft. YW: Conceptualization, Writing – review & editing. MM: Data curation, Methodology, Writing – original draft. ZL: Conceptualization, Formal Analysis, Methodology, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1362076/full#supplementary-material
Supplementary Figure S1
Funnel chart based on blood glucose level. Note: (A) Comparison between LBW and DBW; (B) LBW compared with HBW.
Supplementary Figure S2
Funnel chart based on insulin level.
Supplementary Figure S3
Funnel diagram based on HOMA-IR. Note: (C) LBW compared with DBW; (D) LBW compared with HBW.
Supplementary Figure S4
Funnel chart based on the results of correlation analysis.
1. Champion ML, Battarbee AN, Biggio JR, Casey BM, Harper LM. Postpartum glucose intolerance following early gestational diabetes mellitus. Am J Obstet Gynecol MFM. (2022) 4(3):100609. doi: 10.1016/j.ajogmf.2022.100609
2. Ueki K, Sasako T, Okazaki Y, Miyake K, Nangaku M, Ohashi Y, et al. Multifactorial intervention has a significant effect on diabetic kidney disease in patients with type 2 diabetes. Kidney Int. (2021) 99(1):256–66. doi: 10.1016/j.kint.2020.08.012
3. Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American diabetes association: national cross sectional study. BMJ. (2020) 369:m997. doi: 10.1136/bmj.m997
4. Li W, Zhang H, Chen Z, Tao Y, Huang X, Chen W, et al. MiRNA-92a-3p mediated the association between occupational noise exposure and blood pressure among Chinese adults. Sci Total Environ. (2024) 907:168148. doi: 10.1016/j.scitotenv.2023.168148
5. Jinyi W, Zhang Y, Wang K, Peng P. Global, regional, and national mortality of tuberculosis attributable to alcohol and tobacco from 1990 to 2019: a modelling study based on the global burden of disease study 2019. J Glob Health. (2024) 14:04023. doi: 10.7189/jogh.14.04023
6. Zhang Y, Wang K, Zhu J, Wu J. A network suspected infectious disease model for the development of syphilis transmission from 2015 to 2021 in Hubei province, China. J Appl Microbiol. (2023) 134(12):lxad311. doi: 10.1093/jambio/lxad311
7. Yajnik CS, Bandopadhyay S, Bhalerao A, Bhat DS, Phatak SB, Wagh RH, et al. Poor in utero growth, and reduced β-cell compensation and high fasting glucose from childhood, are harbingers of glucose intolerance in young Indians. Diabetes Care. (2021) 44(12):2747–57. doi: 10.2337/dc20-3026
8. Green JB, Mottl AK, Bakris G, Heerspink HJL, Mann JFE, McGill JB, et al. Design of the COmbinatioN effect of FInerenone anD EmpaglifloziN in participants with chronic kidney disease and type 2 diabetes using a UACR endpoint study (CONFIDENCE). Nephrol Dial Transplant. (2023) 38(4):894–903. doi: 10.1093/ndt/gfac198
9. Subramanian SC, Porkodi A, Akila P. Effectiveness of nurse-led intervention on self-management, self-efficacy and blood glucose level among patients with type 2 diabetes mellitus. J Complement Integr Med. (2020) 17(3). doi: 10.1515/jcim-2019-0064
10. Wu J, Wang K, Tao F, Li Q, Luo X, Xia F. The association of blood metals with latent tuberculosis infection among adults and adolescents. Front Nutr. (2023) 10:1259902. doi: 10.3389/fnut.2023.1259902
11. Wang K, Xia F, Li Q, Luo X, Wu J. The associations of weekend warrior activity patterns with the visceral adiposity index in US adults: repeated cross-sectional study. JMIR Public Health Surveill. (2023) 9:e41973. doi: 10.2196/41973
12. Li W, Feng X, Zhang H, Wang YX, Zeng Q, Liu C, et al. Association of shift work with oxidative stress and alteration of fasting plasma glucose level in Chinese adults. Obesity (Silver Spring). (2023) 31(10):2505–14. doi: 10.1002/oby.23845
13. Li W, Chen D, Peng Y, Lu Z, Wang D. Association of polycyclic aromatic hydrocarbons with systemic inflammation and metabolic syndrome and its components. Obesity (Silver Spring). (2023) 31(5):1392–401. doi: 10.1002/oby.23691
14. Li W, Chen D, Tao Y, Lu Z, Wang D. Association between triglyceride-glucose index and carotid atherosclerosis detected by ultrasonography. Cardiovasc Diabetol. (2022) 21(1):137. doi: 10.1186/s12933-022-01570-0
15. Bianco ME, Kuang A, Josefson JL, Catalano PM, Dyer AR, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcome follow-up study: newborn anthropometrics and childhood glucose metabolism. Diabetologia. (2021) 64(3):561–70. doi: 10.1007/s00125-020-05331-0
16. Cherney DZI, Charbonnel B, Cosentino F, Dagogo-Jack S, McGuire DK, Pratley R, et al. Effects of ertugliflozin on kidney composite outcomes, renal function and albuminuria in patients with type 2 diabetes mellitus: an analysis from the randomised VERTIS CV trial. Diabetologia. (2021) 64(6):1256–67. doi: 10.1007/s00125-021-05407-5
17. Kumbhojkar A, Saraff V, Nightingale P, Högler W. Glycated haemoglobin as a screening test for abnormal glucose homeostasis in childhood obesity. Diabet Med. (2020) 37(2):356–61. doi: 10.1111/dme.14192
18. Soh J F, Beaulieu S, Trepiccione F, Linnaranta O, Torres-Platas G, Platt RW, et al. A double-blind, randomized, placebo-controlled pilot trial of atorvastatin for nephrogenic diabetes insipidus in lithium users. Bipolar Disord. (2021) 23(1):66–75. doi: 10.1111/bdi.12973
19. Pop-Busui R, Braffett BH, Wessells H, Herman WH, Martin CL, Jacobson AM, et al. Diabetic peripheral neuropathy and urological complications in type 1 diabetes: findings from the epidemiology of diabetes interventions and complications study. Diabet Care. (2022) 45(1):119–26. doi: 10.2337/dc21-1276
20. Ledo DL, Suano-Souza FI, Franco M, Strufaldi MWL. Body mass index and cardiovascular risk factors in children and adolescents with high birth weight. Ann Nutr Metab. (2018) 72(4):272–8. doi: 10.1159/000488595
21. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabet Care. (2018) 41(Suppl. 1):S13–s27. doi: 10.2337/dc18-S002
22. Li W, Chen D, Ruan W, Peng Y, Lu Z, Wang D. Association of polycyclic aromatic hydrocarbons exposure, systemic inflammation with hearing loss among adults and adolescents. Environ Pollut. (2022) 296:118772. doi: 10.1016/j.envpol.2021.118772
23. Zheng X, Shi J, Wu J. Analysis of factors and corresponding interactions influencing clinical management assistant ability using competency model in China. Medicine (Baltimore). (2020) 99(51):e23516. doi: 10.1097/MD.0000000000023516
24. Oliveira-Santos J, Santos R, Moreira C, Abreu S, Lopes L, Agostinis-Sobrinho C, et al. Associations between anthropometric indicators in early life and low-grade inflammation, insulin resistance and lipid profile in adolescence. Nutr Metab Cardiovasc Dis. (2019) 29(8):783–92. doi: 10.1016/j.numecd.2019.05.052
25. de Jong M, Cranendonk A, van Weissenbruch MM. Components of the metabolic syndrome in early childhood in very-low-birth-weight infants and term small and appropriate for gestational age infants. Pediatr Res. (2015) 78(4):457–61. doi: 10.1038/pr.2015.118
26. Domínguez Hernández C, Klünder Klünder M, Huang F, Flores Armas EM, Velázquez-López L, Medina-Bravo P. Association between abdominal fat distribution, adipocytokines and metabolic alterations in obese low-birth-weight children. Pediatr Obes. (2016) 11(4):285–91. doi: 10.1111/ijpo.12060
27. dos Santos Alves PJ, PTH AC, Pinto LR, SM RM, MA CH, Alves RS, et al. Endothelial and metabolic disorders in adolescence: low birth weight is not an isolated risk factor. J Pediatr Endocrinol Metab. (2015) 28(3-4):407–13. doi: 10.1515/jpem-2014-0146
28. Mori M, Mori H, Yamori Y, Tsuda K. Low birth weight as cardiometabolic risk in Japanese high school girls. J Am Coll Nutr. (2012) 31(1):39–44. doi: 10.1080/07315724.2012.10720007
29. Guerrero-Romero F, Aradillas-García C, Simental-Mendia LE, Monreal-Escalante E, de la Cruz Mendoza E, Rodríguez-Moran M. Birth weight, family history of diabetes, and metabolic syndrome in children and adolescents. J Pediatr. (2010) 156(5):719–23. 23.e1. doi: 10.1016/j.jpeds.2009.11.043
30. Huang Y, Li Y, Chen Q, Chen H, Ma H, Su Z, et al. Low serum adiponectin levels are associated with reduced insulin sensitivity and lipid disturbances in short children born small for gestational age. Clin Endocrinol (Oxf). (2015) 83(1):78–84. doi: 10.1111/cen.12663
31. Sebastiani G, Díaz M, Bassols J, Aragonés G, López-Bermejo A, de Zegher F, et al. The sequence of prenatal growth restraint and post-natal catch-up growth leads to a thicker intima-media and more pre-peritoneal and hepatic fat by age 3–6 years. Pediatr Obes. (2016) 11(4):251–7. doi: 10.1111/ijpo.12053
32. Blusková Z, Koštálová L, Celec P, Vitáriušová E, Pribilincová Z, Maršálková M, et al. Evaluation of lipid and glucose metabolism and cortisol and thyroid hormone levels in obese appropriate for gestational age (AGA) born and non-obese small for gestational age (SGA) born prepubertal Slovak children. J Pediatr Endocrinol Metab. (2014) 27(7-8):693–9. doi: 10.1515/jpem-2013-0334
33. Suzuki Y, Kido J, Matsumoto S, Shimizu K, Nakamura K. Associations among amino acid, lipid, and glucose metabolic profiles in childhood obesity. BMC Pediatr. (2019) 19(1):273. doi: 10.1186/s12887-019-1647-8
34. Chuar PF, Ng YT, Phang SCW, Koay YY, Ho JI, Ho LS, et al. Tocotrienol-rich vitamin E (tocovid) improved nerve conduction velocity in type 2 diabetes mellitus patients in a phase II double-blind, randomized controlled clinical trial. Nutrients. (2021) 13(11):3770. doi: 10.3390/nu13113770
35. Zohdi V, Sutherland MR, Lim K, Gubhaju L, Zimanyi MA, Black MJ. Low birth weight due to intrauterine growth restriction and/or preterm birth: effects on nephron number and long-term renal health. Int J Nephrol. (2012) 2012:136942. doi: 10.1155/2012/136942
36. Mehrzadi S, Mirzaei R, Heydari M, Sasani M, Yaqoobvand B, Huseini HF. Efficacy and safety of a traditional herbal combination in patients with type II diabetes mellitus: a randomized controlled trial. J Diet Suppl. (2021) 18(1):31–43. doi: 10.1080/19390211.2020.1727076
37. Schmitt A, Kulzer B, Reimer A, Herder C, Roden M, Haak T, et al. Evaluation of a stepped care approach to manage depression and diabetes distress in patients with type 1 diabetes and type 2 diabetes: results of a randomized controlled trial (ECCE HOMO study). Psychother Psychosom. (2022) 91(2):107–22. doi: 10.1159/000520319
38. Maddaloni E, Coleman RL, Agbaje O, Buzzetti R, Holman RR. Time-varying risk of microvascular complications in latent autoimmune diabetes of adulthood compared with type 2 diabetes in adults: a post-hoc analysis of the UK prospective diabetes study 30-year follow-up data (UKPDS 86). Lancet Diab Endocrinol. (2020) 8(3):206–15. doi: 10.1016/S2213-8587(20)30003-6
39. Hainsworth DP, Gao X, Bebu I, Das A, de Koo L O, Barkmeier AJ, et al. Refractive error and retinopathy outcomes in type 1 diabetes: the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Ophthalmology. (2021) 128(4):554–60. doi: 10.1016/j.ophtha.2020.09.014
40. Kurnikowski A, Nordheim E, Schwaiger E, Krenn S, Harreiter J, Kautzky-Willer A, et al. Criteria for prediabetes and posttransplant diabetes mellitus after kidney transplantation: a 2-year diagnostic accuracy study of participants from a randomized controlled trial. Am J Transplant. (2022) 22(12):2880–91. doi: 10.1111/ajt.17187
41. Koundal H, Dhandapani M, Thakur P, Dutta P, Walia R, Sahoo SK, et al. Effectiveness of dietary diabetes insipidus bundle on the severity of postoperative fluid imbalance in pituitary region tumours: a randomized controlled trial. J Adv Nurs. (2021) 77(9):3911–20. doi: 10.1111/jan.14894
Keywords: newborn, low birth weight, abnormal glucose tolerance, diabetes, meta-analysis
Citation: Ma J, Wang Y, Mo M and Lian Z (2024) Association between low birth weight and impaired glucose tolerance in children: a systematic review and meta-analysis. Front. Pediatr. 12:1362076. doi: 10.3389/fped.2024.1362076
Received: 27 December 2023; Accepted: 23 April 2024;
Published: 9 May 2024.
Edited by:
Feihong Luo, Fudan University, ChinaReviewed by:
Irene Rutigliano, IRCCS Casa Sollievo della Sofferenza Hospital, Italy© 2024 Ma, Wang, Mo and Lian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zerong Lian bHpyMjM1OTI3NTkzMUAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.