- Department of Pediatrics, The Second Affiliated Hospital of Nanchang University, Nanchang, China
Background: Short sleep duration has been related to obesity in children and adolescents. However, it remains unknown whether late bedtime is also associated with obesity and whether the association is independent of sleep duration. A meta-analysis was performed to address this issue.
Methods: In order to accomplish the aim of the meta-analysis, a comprehensive search was conducted on databases including PubMed, Embase, and Web of Science to identify observational studies. The cutoff to determine late bedtime in children in this meta-analysis was consistent with the value used among the included original studies. As for obesity, it was typically defined as a body mass index (BMI) > 95th percentile of age and sex specified reference standards or the International Obesity Task Force defined age- and gender-specific cut-off of BMI. The Cochrane Q test was employed to evaluate heterogeneity among the included studies, while the I2 statistic was estimated. Random-effects models were utilized to merge the results, considering the potential impact of heterogeneity.
Results: Tweleve observational studies with 57,728 participants were included. Among them, 6,815 (11.8%) were obese. Pooled results showed that late bedtime reported by the participants or their caregivers was associated with obesity (odds ratio [OR]: 1.27, 95% confidence interval [CI]: 1.16–1.39, p < 0.001; I2 = 0%). Subgroup analysis showed consistent results in studies with (OR: 1.33, 95% CI: 1.04–1.70, p = 0.02) and without adjustment of sleep duration (OR: 1.27, 95% CI: 1.14–1.41, p < 0.001). Further subgroup analysis also showed that the association was not significantly affected by study location, design, age of the participants, or diagnostic methods for obesity (p for subgroup difference all >0.05).
Conclusion: Late bedtime is associated with obesity in children and adolescents, which may be independent of sleep duration.
Introduction
Childhood obesity has emerged as a significant global public health concern, attributable to the evolving lifestyles of individuals in both developed and developing nations (1, 2). The escalating prevalence of childhood obesity is indicative of an ongoing trend (3, 4). The findings of the 2019/2020 English National Child Measurement Program indicate that 9.9% of children aged 4–5 were classified as obese (5). Upon conducting a subsequent assessment of the same cohort at age 10–11, it was observed that the prevalence of obesity had escalated to 21% (5). Similarly, a recent systematic review conducted in China revealed a persistent and heterogeneous prevalence of overweight and obesity among children and adolescents in the country (6). The presence of obesity in children and adolescents has been linked to heightened lifetime susceptibility to metabolic disorders (7, 8), cardiovascular diseases (9, 10), and cancer (7, 11). Consequently, it is imperative to identify the risk factors associated with childhood obesity, particularly those related to unhealthy lifestyles, in order to improve the overall body weight status within this population (12, 13).
Accumulating evidence indicates that children and adolescents with insufficient nighttime sleep are at a heightened risk of childhood obesity, in contrast to those with sufficient sleep duration (14, 15). In recent decades, insufficient nighttime sleep has been closely related to delayed bedtime in both adults and children, which are likely to be caused by various external factors, such as social interactions, food, entertaining activity, and increased screen time etc. Nevertheless, prior investigations examining the correlation between delayed bedtime and obesity in children have yielded inconclusive findings (16). Furthermore, given the close interrelation between bedtime and sleep duration, it remains uncertain whether the potential association between delayed bedtime and obesity is independent of the impact of inadequate sleep duration (17). In light of this dearth of knowledge, a meta-analysis of observational studies was conducted to evaluate the potential association between late bedtime and obesity in children and adolescents.
Materials and methods
The study adhered to the Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guideline (18) and the Cochrane Handbook (19) throughout the stages of planning, conducting, and reporting.
Inclusion and exclusion criteria of studies
The development of inclusion criteria adhered to the Participant, Intervention, Comparison, Outcome, and Study design (PICOS) recommendations and aligned with the objective of the meta-analysis.
P (participants): Children and adolescents from general population or community population.
I (exposure): Late bedtime. To the best of our knowledge, a universal cutoff has not been developed and it is likely to be varied according to the age of the children. Because we are focusing on the comparison between children with early vs. late bedtime, the cutoff to determine late bedtime in children in this meta-analysis was consistent with the value used among the included original studies.
C (control): Early bedtime. The cutoff to define children and adolescents with early bedtime were consistent with that used among the included studies.
O (outcomes): The prevalence or the incidence of obesity compared between children and adolescents with later vs. early bedtime. The diagnostic methods and criteria for obesity were in accordance with that used in the original studies. As for obesity, it was typically defined as BMI > 95th percentile of age and sex specified reference standards or the International Obesity Task Force (IOTF) defined age- and gender-specific cut-off of BMI. For studies reporting multiple categories of participants with different late bedtime, those with the latest bedtime were included for analysis.
S (study design): This study incorporated observational studies, such as case-control study, cross-sectional study, or cohort study. Excluded from the meta-analysis were reviews, editorials, meta-analyses, and studies that included children or adolescents with specific clinical conditions, studies that included adult population, did not evaluate the influence of bedtime, or did not report the outcome of obesity. In cases where there was an overlap in populations, the study with the largest sample size was included in the meta-analysis.
Search of databases
A comprehensive search was conducted in electronic databases, namely PubMed, Embase, and Web of Science, encompassing the period from inception to August 10, 2023. The search strategy employed relevant terms pertaining to the subject matter of our investigation, aiming to identify studies published within this timeframe, which included: (1) “sleep time” OR “bed time” OR “bedtime” OR “late sleep” OR “late-time sleeping” OR “late time sleeping” OR “sleep timing”; (2) “obesity” OR “obese”; and (3) “child” OR “children” OR “adolescents” OR “pediatric” OR “pediatric” OR “preschool” OR “toddler”. Only studies that met the criteria of being published as full-length articles in English or Chinese and appearing in peer-reviewed journals were included in our analysis. Additionally, during our manual screening process, we thoroughly examined the references cited in relevant original and review articles to identify any potentially relevant studies.
Data extraction and quality evaluation
Two authors independently performed literature searches, data collection, and assessments of study quality. In cases where discrepancies emerged, discussions between the two authors were indicated to come to a consensus. The analysis of studies encompassed the gathering of data related to study information, design characteristics, sample size, demographic factors of the participants, methods and cutoffs for evaluating bedtime, follow-up durations for cohort studies, diagnostic methods for obesity, number of participants with obesity, and potential confounding variables adjusted when the association between late bedtime and obesity were analyzed. The quality of the study was assessed using the Newcastle-Ottawa Scale (NOS) (20). For cohort studies, this scale judges the quality regarding three aspects: selection of the study groups; the comparability of the groups; and the ascertainment of the outcome of interest. For case-control and cross-sectional studies, this scale assess the quality of the studies also via three aspects: selection and definitions of cases and controls, comparability between cases and controls, and ascertainment of expose between cases and controls. The NOS varied between one to nine stars, with a higher star indicating a better study quality.
Statistics
Odds ratios (ORs) and their corresponding 95% confidence intervals (CIs) were utilized as the variables to assess the relationship between late bedtime and obesity in children and adolescent. To stabilize and normalize the variance, a logarithmical transformation was applied to the OR and its corresponding standard error in each study (21). The Cochrane Q test and the I2 statistic (22) were employed to estimate between-study heterogeneity. A value of I2 greater than 50% indicates the presence of significant heterogeneity among the studies. The random-effects model was utilized to combine the findings, as it has been recognized to account for potential heterogeneity (19). Sensitivity analysis excluding one dataset at a time was performed to evaluate the robustness of the finding. Additionally, predefined subgroup analysis was conducted to explore whether the results were significantly affected by characteristics such as study country, design, age of the participants, definition of obesity, or adjustment of sleep duration. Publication bias was estimated using a funnel plot, which involved visual assessments of symmetry, as well as Egger's regression asymmetry test (23). A p value < 0.05 was considered as statistically significant. This applies to the statistical in meta-analysis and the result of the Egger's regression test The statistical analyses were conducted using RevMan (Version 5.1; Cochrane Collaboration, Oxford, UK) and Stata software (version 12.0; Stata Corporation, College Station, TX).
Results
Database search and study retrieval
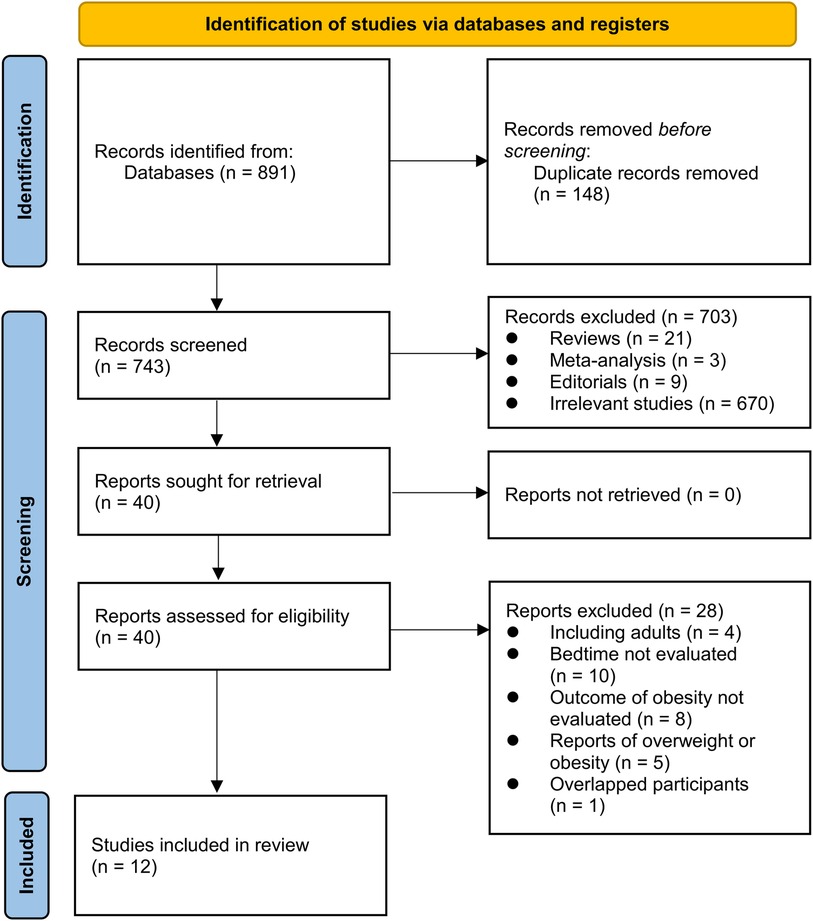
Figure 1 illustrates the procedure employed for conducting the literature search and study retrieval. Initially, a total of 891 records were acquired from the designated database, and subsequently, 148 duplicate entries were eliminated. Upon scrutinizing the titles and abstracts, an additional 703 studies were excluded due to their incompatibility with the objectives of the meta-analysis. Following comprehensive evaluations of the full texts of 40 studies, 28 were excluded based on the rationales outlined in Figure 1. Consequently, twelve studies were deemed suitable for the subsequent meta-analysis (24–35).
Study characteristics
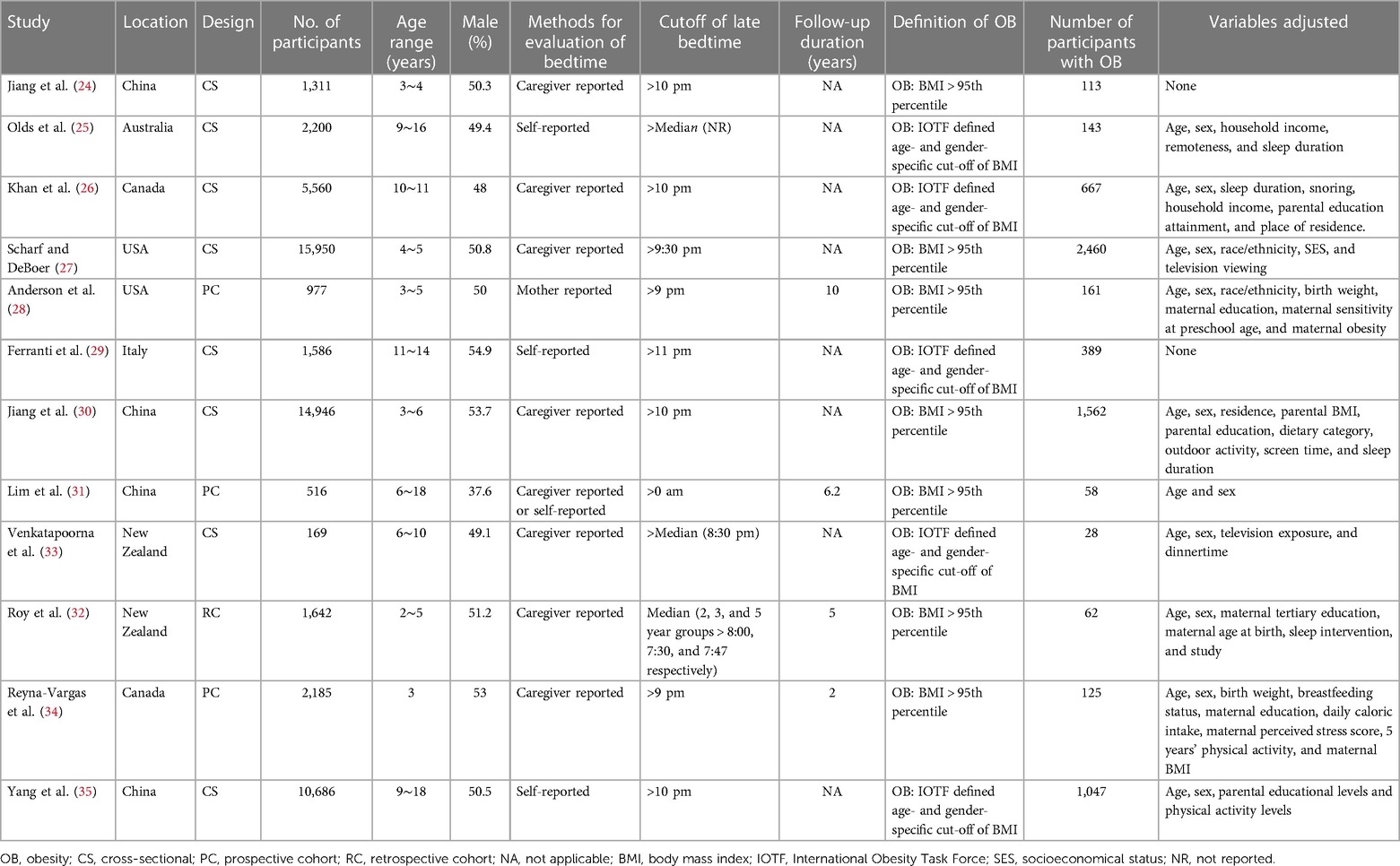
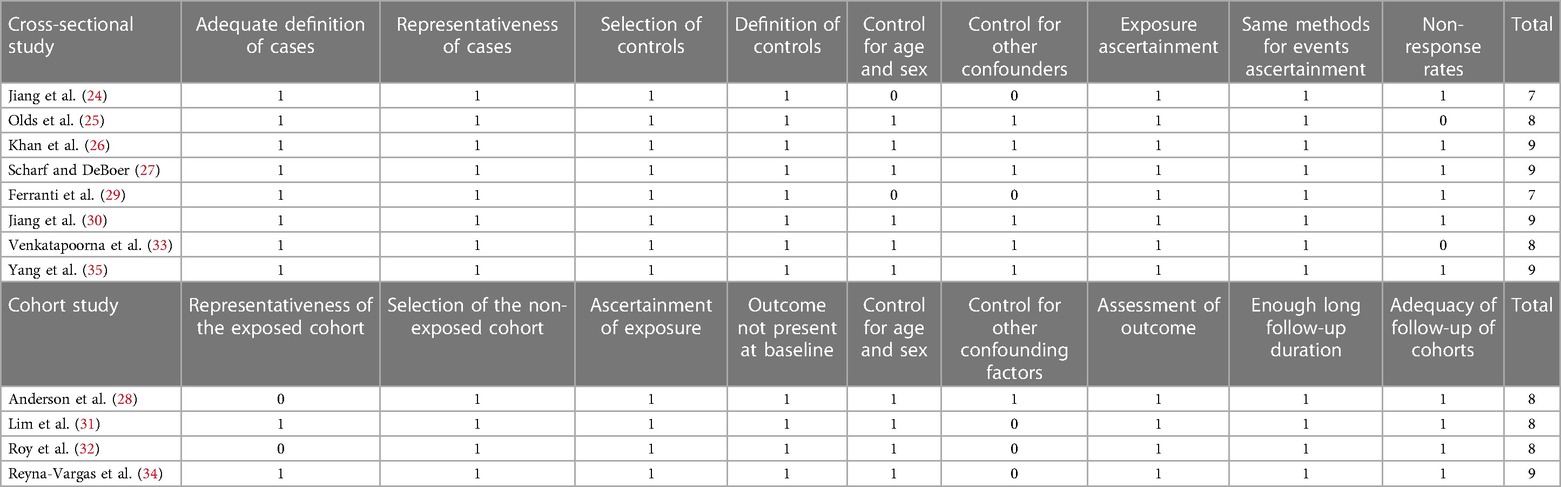
The characteristic of the studies are summarized in Table 1. Overall, 12 observational studies, including eight cross-sectionals studies (24–27, 29, 30, 33, 35) and four cohort studies (28, 31, 32, 34) were included. These studies were published between 2009 and 2023, and performed in China, Australia, Canada, the United States, Italy, and New Zealand. A total of 57,728 children and adolescents were included. The bedtime of the participants were self-reported or reported by their caregivers. As for the cutoffs for refining late bedtime, medians of sleep time of the included participants were used in three studies (25, 32, 33), while in the other eight studies, cutoffs of later than 9:00 pm (28, 34), 9:30 pm (27), 10:00 pm (24, 26, 30, 35), 11:00 pm (29), or midnight (31) were selected. The diagnosis of obesity in children and adolescents was made if the body mass index (BMI) > 95th percentile according to age and gender using the local children growth charts or using the IOTF defined age- and gender-specific cut-off of BMI. Accordingly, 6,815 (11.8%) of the participants were obese. Univariate analyses were performed in two studies (24, 29), while for the other ten studies, age, sex and other confounding factors were incorporated in the multivariate analysis (25–28, 30–35). The NOS of the included studies were seven to nine, indicating that they were of good quality (Table 2).
Results of meta-analysis
Since two studies reported the results according to the age group of the included children and adolescents (27, 35), these datasets were included in the meta-analysis independently. Overall, 15 datasets from 12 observational studies were involved in the meta-analysis. Pooled results showed that late bedtime was significantly associated with obesity in children and adolescents (OR: 1.27, 95% CI: 1.16–1.39, p < 0.001; Figure 2A) with no significant heterogeneity (I2 = 0%). Sensitivity analyses by omitting one dataset at a time showed consistent results (OR: 1.24–1.32, p all < 0.05). In addition, sensitivity analysis limited to studies with multivariate analyses (25–28, 30–35) showed similar results (OR: 1.26, 95% CI: 1.15–1.39, p < 0.001; I2 = 0%). Subgroup analysis showed consistent results in studies of Asian and Western countries (p for subgroup difference = 0.39, Figure 2B), in cross-sectional and cohort studies (p for subgroup difference = 0.59, Figure 3A), in preschool children and school children and adolescents (p for subgroup difference = 0.98, Figure 3B), and in studies of obesity defined as BMI > 95th percentile or according to the IOTF criteria (p for subgroup difference = 0.83, Figure 4A). Specifically, subgroup analysis showed consistent results in studies with (OR: 1.33, 95% CI: 1.04–1.70, p = 0.02) and without the adjustment of sleep duration (OR: 1.27, 95% CI: 1.14–1.41, p < 0.001; p for subgroup difference = 0.72; Figure 4B).
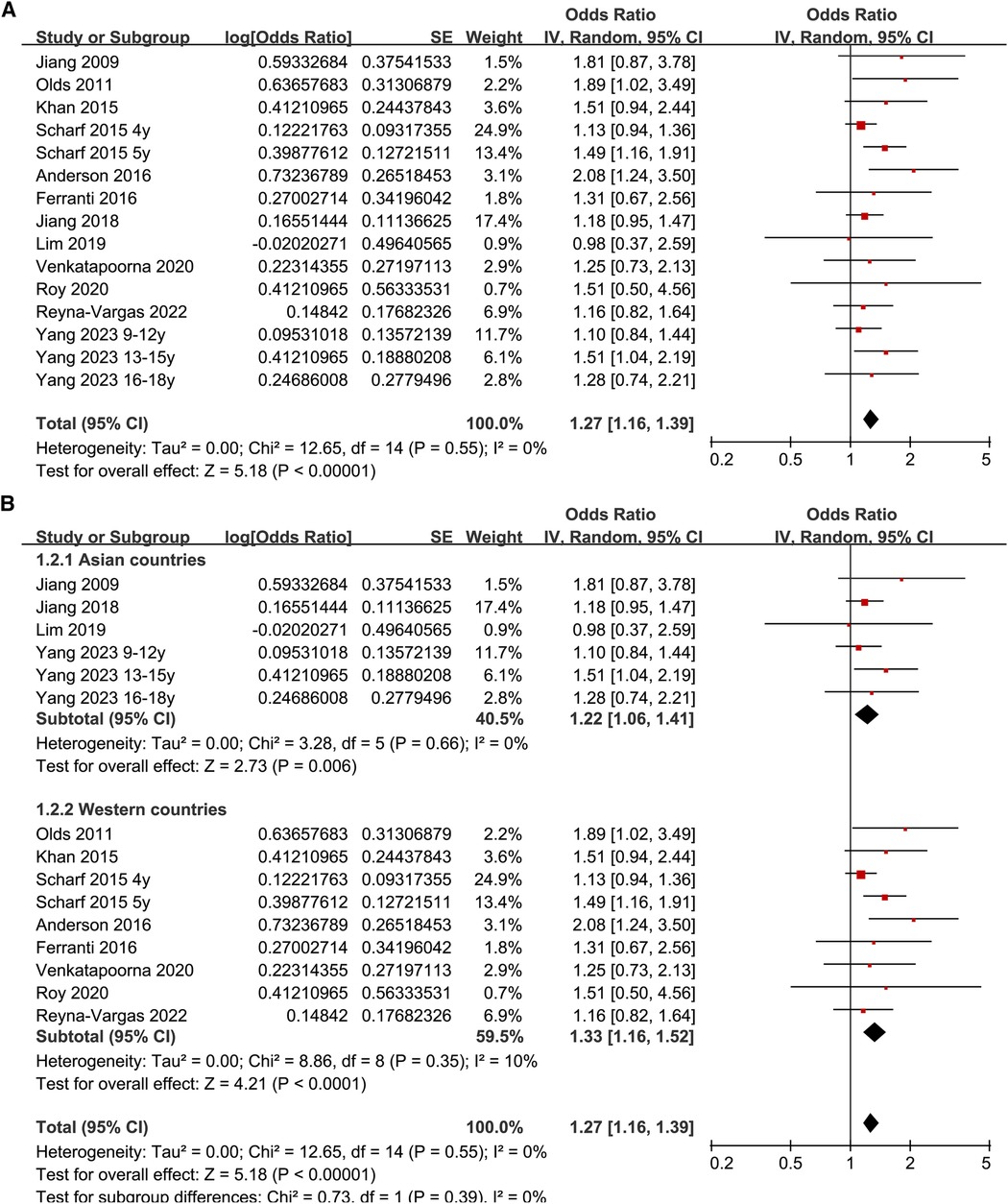
Figure 2. Forest plots for the meta-analyses regarding the association between late bedtime and obesity in children and adolescents; (A) overall meta-analysis; and (B) subgroup analysis according to study country.
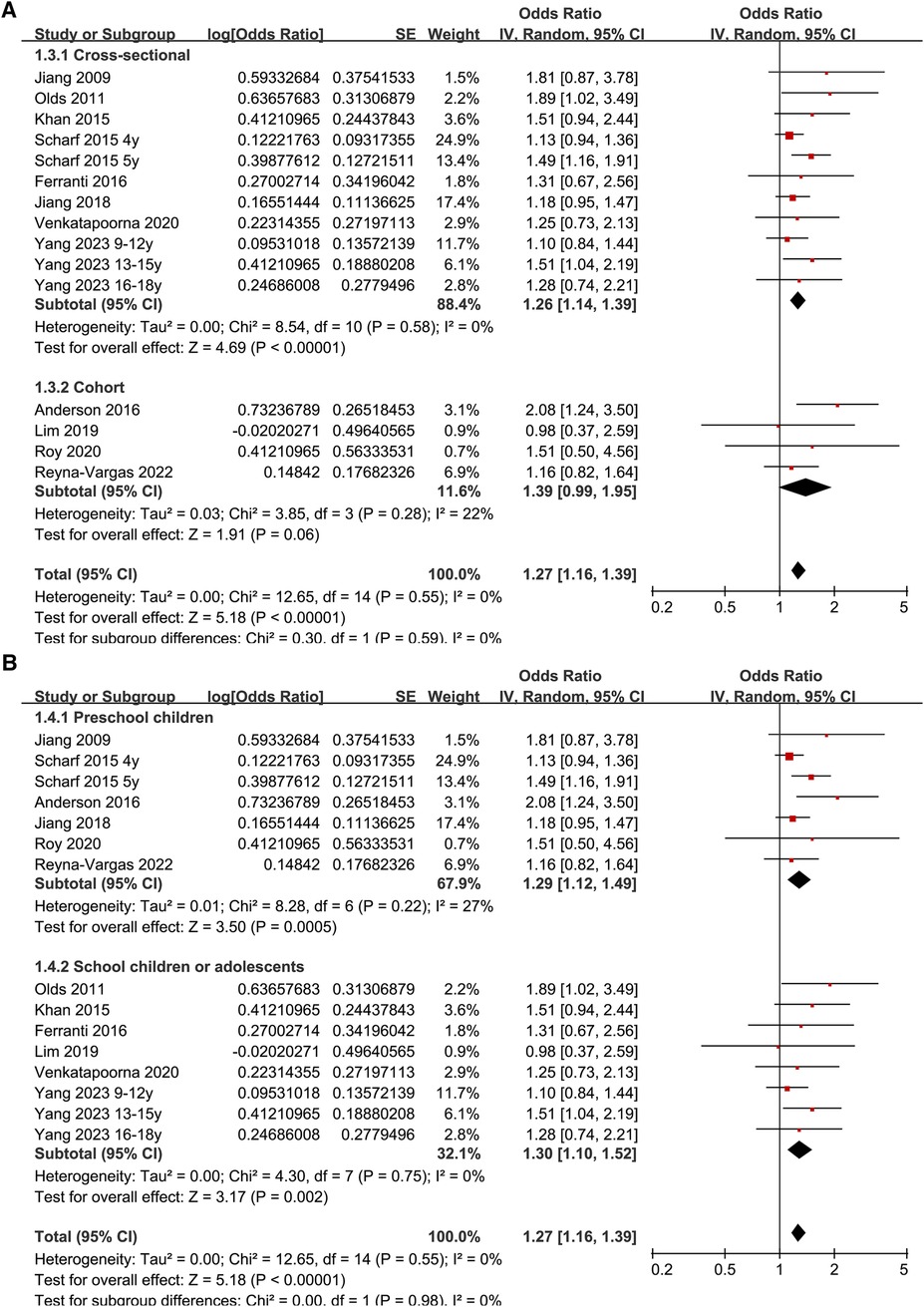
Figure 3. Forest plots for the subgroup-analyses regarding the association between late bedtime and obesity in children and adolescents; (A) subgroup analysis according to study design; and (B) subgroup analysis according to age group.
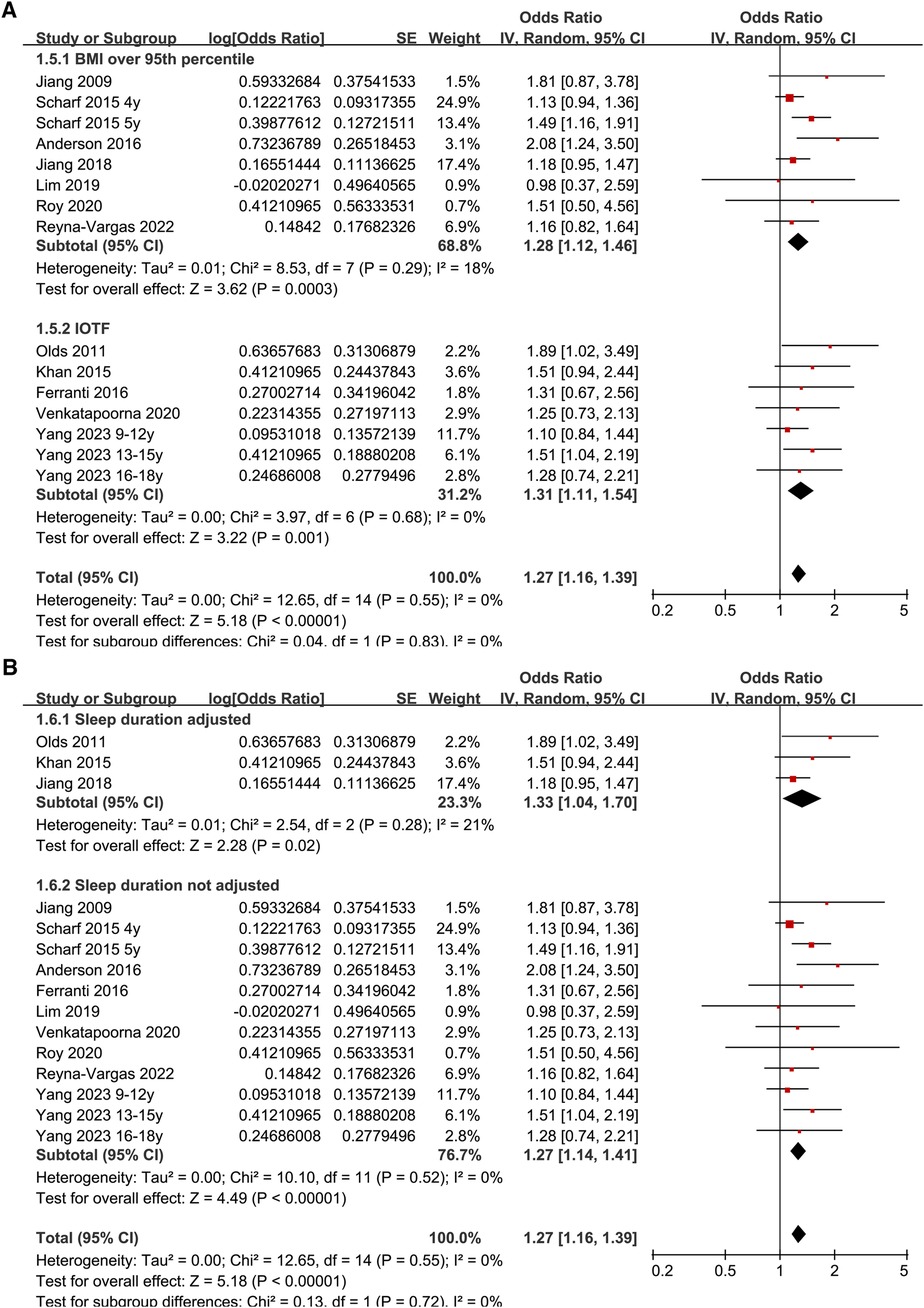
Figure 4. Forest plots for the subgroup-analyses regarding the association between late bedtime and obesity in children and adolescents; (A) subgroup analysis according to diagnostic methods for obesity; and (B) subgroup analysis according to the adjustment of sleep duration.
Publication bias
The funnel plots depicting the meta-analyses of the association between late bedtime and obesity in children and adolescents are presented in Figure 5. Upon visual inspection, the plots exhibit symmetrical patterns, indicating a minimal presence of publication bias. Furthermore, the application of Egger's regression test yielded p-value of 0.75, further supporting the notion of a low probability of publication bias.
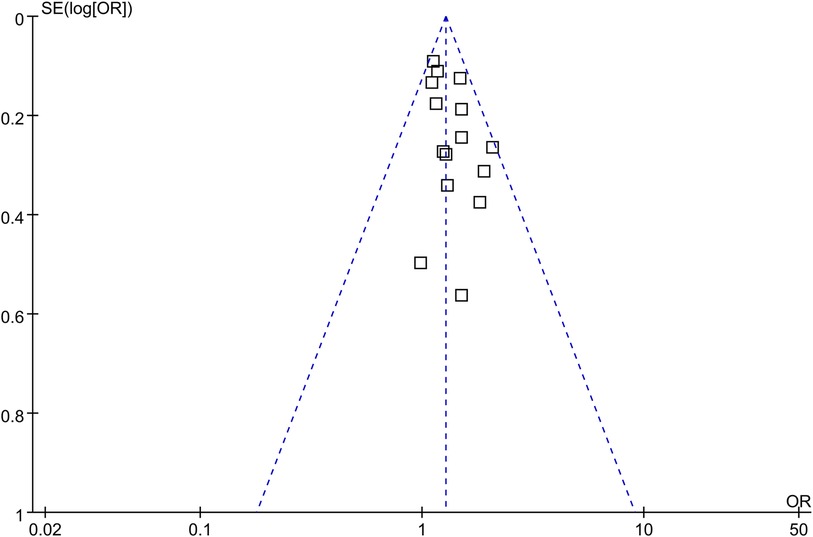
Figure 5. Funnel plots for the publication bias underlying the meta-analysis of the association between late bedtime and obesity in children and adolescents.
Discussion
In this meta-analysis, we combined the results of 15 datasets from 12 eligible observational studies and the results showed that compared to participants with early bedtime, children and adolescents with late bedtime were significantly associated with the prevalence and incidence of obesity. Further sensitivity analyses by excluding one dataset at a time showed consistent results. In addition, subgroup analyses showed that the association between late bedtime and obesity in children and adolescents was not significantly affected by study country, study design, age group of the participants, and diagnostic methods for obesity. Particularly, the association was consistent in studies with and without the adjustment of sleep duration. Taken together, results of the meta-analysis indicate that late bedtime is associated with obesity in children and adolescents, which may be independent of the influence of sleep duration.
As far as we know, this study may be the first meta-analysis regarding the association between bedtime and obesity in children and adolescents. There are some methodological advantages of the meta-analysis. We performed extensive literature search in three commonly used literature databases and retrieved the up-to-date literatures that evaluated the association between bedtime and obesity. Ten of the included studies were based on data of multivariate analyses, and a sensitivity analysis limited to these studies showed similar results, which suggested a potentially independent association between late bedtime and obesity in children and adolescents. Subsequent sensitivity analyses by excluding one dataset at a time suggested that the results were not primarily driven by either of the included studies, reflecting the stability of the results. Finally, subgroup analysis showed that the association between late bedtime and obesity was not likely to be significantly affected by study characteristics such as study country, design, age group, definition of obesity, or adjustment of sleep duration. The latter is particularly important because inadequate sleep duration has been established as a risk factor of obesity in children (36), and late bedtime is closely related to short sleep duration. These findings support that besides short sleep duration, late bedtime may also be a risk factor of obesity in children and adolescents. These findings are important to designate optimal lifestyle modification regarding sleep habit to reduce the risk of obesity in children.
The association between late bedtime and obesity in children and adolescents may be influenced by various mechanisms. One potential factor is the alteration of dietary habits in this population. A study conducted on 93 adolescents in the United States demonstrated that late bedtime and sleep deprivation were linked to increased consumption of carbohydrates, added sugars, foods with higher glycemic load, and sweet beverages. Conversely, there was a decrease in the intake of fruits and vegetables, which could potentially contribute to adverse weight and cardiometabolic outcomes (37). A subsequent randomized cross-over study indicated that children who had a later bedtime consumed an additional 35 calories per day from sugar-sweetened beverages during periods of decreased sleep, compared to controls that had an earlier bedtime (38). These instances of late bedtime were more likely to occur after 8 pm (38). In addition to its impact on dietary patterns, late bedtime has also been linked to prolonged screen time before sleep (39), decreased physical activity (40), and the development of insulin resistance (41). These factors may also contribute to the connection between late bedtime and obesity. Besides, increased screen time and television time before bed has also been associated with late bedtime in children (42, 43). In addition, these two factors, together with room light before beds have all been related to the suppressed melatonin onset and shortened melatonin duration (44). Interestingly, endogenous melatonin has been shown to protect against body weight gain induced by sleep deprivation in a previous study (45), suggesting change in endogenous melatonin may be a key mechanisms underlying the association between late bedtime and obesity in children. However, the specific mechanisms and molecular pathways that underlie this association remain to be clarified in future studies.
This study has several limitations that should be acknowledged. Firstly, the protocol of the meta-analysis was not prospectively registered. Secondly, the majority of the studies included in this analysis were cross-sectional and retrospective, which introduces the possibility of selection and recall biases. To validate the findings, it is necessary to conduct large-scale prospective studies. Thirdly, the optimal cutoff of early bedtime regarding the influence of bedtime on obesity should be investigated in future studies. Moreover, in view of the close relationship between bedtime and sleep duration, these factors should be both considered in future studies. Furthermore, although most of the included studies employed multivariate regression analyses to determine the association, it is important to acknowledge that the influence of residual factors on the correlation between late bedtime and obesity in this population. Besides, the differences in cutoff of late bedtime and adjusted variables among the included studies may affect the results of the meta-analysis and lead to potential heterogeneity. Ultimately, due to the nature of this meta-analysis being based on observational studies, it is not possible to establish a causal relationship between late bedtime and obesity in children and adolescents.
Conclusions
The findings of the meta-analysis indicate that there is a significant correlation between late bedtime and obesity in children and adolescents, potentially unaffected by the duration of sleep. These results propose late bedtime as a plausible risk factor for obesity within this specific demographic. Consequently, future research should consider both bedtime and sleep duration as crucial factors when determining the most effective lifestyle modifications for reducing the risk of obesity in children and adolescents.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
NH: Conceptualization, Data curation, Formal Analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. YW: Data curation, Formal Analysis, Methodology, Validation, Writing – review & editing. QY: Data curation, Formal Analysis, Methodology, Validation, Writing – review & editing. SH: Investigation, Methodology, Validation, Writing – review & editing. WL: Investigation, Methodology, Validation, Writing – review & editing. ZY: Investigation, Supervision, Validation, Writing – review & editing. CY: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lister NB, Baur LA, Felix JF, Hill AJ, Marcus C, Reinehr T, et al. Child and adolescent obesity. Nat Rev Dis Primers. (2023) 9(1):24. doi: 10.1038/s41572-023-00435-4
2. Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. (2021) 9(6):373–92. doi: 10.1016/S2213-8587(21)00045-0
3. Di Cesare M, Soric M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. (2019) 17(1):212. doi: 10.1186/s12916-019-1449-8
4. Jebeile H, Kelly AS, O'Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. (2022) 10(5):351–65. doi: 10.1016/S2213-8587(22)00047-X
5. Szczyrska J. Pediatric obesity—time to act as early as possible. Pediatr Endocrinol Diabetes Metab. (2023) 29(4):267–73. doi: 10.5114/pedm.2023.133122
6. Hong Y, Ullah R, Wang JB, Fu JF. Trends of obesity and overweight among children and adolescents in China. World J Pediatr. (2023) 19(12):1115–26. doi: 10.1007/s12519-023-00709-7
7. Weihrauch-Bluher S, Schwarz P, Klusmann JH. Childhood obesity: increased risk for cardiometabolic disease and cancer in adulthood. Metab Clin Exp. (2019) 92:147–52. doi: 10.1016/j.metabol.2018.12.001
8. Rendell MS. Obesity and diabetes: the final frontier. Expert Rev Endocrinol Metab. (2023) 18(1):81–94. doi: 10.1080/17446651.2023.2168643
9. Salama M, Balagopal B, Fennoy I, Kumar S. Childhood obesity, diabetes and cardiovascular disease risk. J Clin Endocrinol Metab. (2023) 108(12):3051–66. doi: 10.1210/clinem/dgad361
10. Chung ST, Krenek A, Magge SN. Childhood obesity and cardiovascular disease risk. Curr Atheroscler Rep. (2023) 25(7):405–15. doi: 10.1007/s11883-023-01111-4
11. Fang X, Wang X, Song Z, Han D, Yin X, Liu B, et al. Causal association of childhood obesity with cancer risk in adulthood: a Mendelian randomization study. Int J Cancer. (2021) 149(7):1421–5. doi: 10.1002/ijc.33691
12. Kansra AR, Lakkunarajah S, Jay MS. Childhood and adolescent obesity: a review. Front Pediatr. (2020) 8:581461. doi: 10.3389/fped.2020.581461
13. Ruiz LD, Zuelch ML, Dimitratos SM, Scherr RE. Adolescent obesity: diet quality, psychosocial health, and cardiometabolic risk factors. Nutrients. (2019) 12(1):43. doi: 10.3390/nu12010043
14. Deng X, He M, He D, Zhu Y, Zhang Z, Niu W. Sleep duration and obesity in children and adolescents: evidence from an updated and dose-response meta-analysis. Sleep Med. (2021) 78:169–81. doi: 10.1016/j.sleep.2020.12.027
15. Li L, Zhang S, Huang Y, Chen K. Sleep duration and obesity in children: a systematic review and meta-analysis of prospective cohort studies. J Paediatr Child Health. (2017) 53(4):378–85. doi: 10.1111/jpc.13434
16. Bathory E, Tomopoulos S. Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children. Curr Probl Pediatr Adolesc Health Care. (2017) 47(2):29–42. doi: 10.1016/j.cppeds.2016.12.001
17. Chaput JP. Is sleep deprivation a contributor to obesity in children? Eat Weight Disord. (2016) 21(1):5–11. doi: 10.1007/s40519-015-0233-9
18. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283(15):2008–12. doi: 10.1001/jama.283.15.2008
19. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. The Cochrane Collaboration (2021). Available online at: www.training.cochrane.org/handbook
20. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses (2010). Available online at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
21. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration (2011). Available online at: www.cochranehandbook.org
22. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21(11):1539–58. doi: 10.1002/sim.1186
23. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
24. Jiang F, Zhu S, Yan C, Jin X, Bandla H, Shen X. Sleep and obesity in preschool children. J Pediatr. (2009) 154(6):814–8. doi: 10.1016/j.jpeds.2008.12.043
25. Olds TS, Maher CA, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. (2011) 34(10):1299–307. doi: 10.5665/SLEEP.1266
26. Khan MK, Chu YL, Kirk SF, Veugelers PJ. Are sleep duration and sleep quality associated with diet quality, physical activity, and body weight status? A population-based study of Canadian children. Can J Public Health. (2015) 106(5):e277–82. doi: 10.17269/cjph.106.4892
27. Scharf RJ, DeBoer MD. Sleep timing and longitudinal weight gain in 4- and 5-year-old children. Pediatr Obes. (2015) 10(2):141–8. doi: 10.1111/ijpo.229
28. Anderson SE, Andridge R, Whitaker RC. Bedtime in preschool-aged children and risk for adolescent obesity. J Pediatr. (2016) 176:17–22. doi: 10.1016/j.jpeds.2016.06.005
29. Ferranti R, Marventano S, Castellano S, Giogianni G, Nolfo F, Rametta S, et al. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, southern Italy. Sleep Sci. (2016) 9(2):117–22. doi: 10.1016/j.slsci.2016.04.003
30. Jiang L, Yan SQ, Geng ML, Gu CL, Huang K, Cao H, et al. The associations between nighttime sleep duration, bedtime and preschool children’s obesity. Zhonghua Yu Fang Yi Xue Za Zhi. (2018) 52(11):1146–51. doi: 10.3760/cma.j.issn.0253-9624.2018.11.010
31. Lim LL, Tse G, Choi KC, Zhang J, Luk AOY, Chow E, et al. Temporal changes in obesity and sleep habits in Hong Kong Chinese school children: a prospective study. Sci Rep. (2019) 9(1):5881. doi: 10.1038/s41598-019-42346-z
32. Roy M, Haszard JJ, Savage JS, Yolton K, Beebe DW, Xu Y, et al. Bedtime, body mass index and obesity risk in preschool-aged children. Pediatr Obes. (2020) 15(9):e12650. doi: 10.1111/ijpo.12650
33. Venkatapoorna CMK, Ayine P, Selvaraju V, Parra EP, Koenigs T, Babu JR, et al. The relationship between obesity and sleep timing behavior, television exposure, and dinnertime among elementary school-age children. J Clin Sleep Med. (2020) 16(1):129–36. doi: 10.5664/jcsm.8080
34. Reyna-Vargas ME, Parmar A, Lefebvre DL, Azad MB, Becker AB, Turvey SE, et al. Longitudinal associations between sleep habits, screen time and overweight, obesity in preschool children. Nat Sci Sleep. (2022) 14:1237–47. doi: 10.2147/NSS.S363211
35. Yang L, Han S, Miao C, Lou H, Gao G, Lou X, et al. Associations of multiple sleep dimensions with overall and abdominal obesity among children and adolescents: a population-based cross-sectional study. Int J Obes (Lond). (2023) 47(9):817–24. doi: 10.1038/s41366-023-01324-2
36. Sluggett L, Wagner SL, Harris RL. Sleep duration and obesity in children and adolescents. Can J Diabetes. (2019) 43(2):146–52. doi: 10.1016/j.jcjd.2018.06.006
37. Duraccio KM, Whitacre C, Krietsch KN, Zhang N, Summer S, Price M, et al. Losing sleep by staying up late leads adolescents to consume more carbohydrates and a higher glycemic load. Sleep. (2022) 45(3):zsab269. doi: 10.1093/sleep/zsab269
38. Hart CN, Spaeth AM, Egleston BL, Carskadon MA, Raynor HA, Jelalian E, et al. Effect of changes in children’s bedtime and sleep period on targeted eating behaviors and timing of caloric intake. Eat Behav. (2022) 45:101629. doi: 10.1016/j.eatbeh.2022.101629
39. Ogunleye AA, Voss C, Sandercock GR. Delayed bedtime due to screen time in schoolchildren: importance of area deprivation. Pediatr Int. (2015) 57(1):137–42. doi: 10.1111/ped.12447
40. Ekstedt M, Nyberg G, Ingre M, Ekblom O, Sleep MC. Physical activity and BMI in six to ten-year-old children measured by accelerometry: a cross-sectional study. Int J Behav Nutr Phys Act. (2013) 10:82. doi: 10.1186/1479-5868-10-82
41. Jansen EC, Burgess HJ, Chervin RD, Dolinoy DC, Tellez-Rojo MM, Cantoral A, et al. Sleep duration and timing are prospectively linked with insulin resistance during late adolescence. Obesity (Silver Spring). (2023) 31(4):912–22. doi: 10.1002/oby.23680
42. Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. (2015) 135(2):e367–75. doi: 10.1542/peds.2014-2306
43. Alqarni TA, Alshamrani MA, Alzahrani AS, AlRefaie AM, Balkhair OH, Alsaegh SZ. Prevalence of screen time use and its relationship with obesity, sleep quality, and parental knowledge of related guidelines: a study on children and adolescents attending primary healthcare centers in the Makkah region. J Family Community Med. (2022) 29(1):24–33. doi: 10.4103/jfcm.jfcm_335_21
44. Gooley JJ, Chamberlain K, Smith KA, Khalsa SB, Rajaratnam SM, Van Reen E, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. (2011) 96(3):E463–72. doi: 10.1210/jc.2010-2098
Keywords: sleep, bedtime, obesity, children, adolescents, meta-analysis
Citation: Hu N, Wu Y, Yao Q, Huang S, Li W, Yao Z and Ye C (2024) Association between late bedtime and obesity in children and adolescents: a meta-analysis. Front. Pediatr. 12:1342514. doi: 10.3389/fped.2024.1342514
Received: 22 November 2023; Accepted: 13 February 2024;
Published: 15 March 2024.
Edited by:
Anna Di Sessa, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Shijian Liu, Shanghai Children’s Medical Center, ChinaLenycia De Cassya Lopes Neri, University of Pavia, Italy
© 2024 Hu, Wu, Yao, Huang, Li, Yao and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunfeng Ye eWVjZl9uY0Bob3RtYWlsLmNvbQ==
 Na Hu
Na Hu Chunfeng Ye
Chunfeng Ye