
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr. , 29 July 2024
Sec. Pediatric Cardiology
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1258725
Background: The associated factors of malnutrition in children with congenital heart disease (CHD) must be evaluated to provide evidence for the treatment and care of such children.
Methods: Two investigators searched the PubMed database until 25 June 2023 for literature about the associated factors of malnutrition in children with CHD. A meta-analysis of associated factors of malnutrition was performed by RevMan 5.3 software.
Results: Thirteen studies involving 8,031 children with CHD were included. Pulmonary hypertension (OR = 3.81, 95% CI: 2.46–4.12), low birth weight (OR = 2.69, 95% CI: 1.25–5.77) and parents’ height (OR = 2.15, 95% CI: 1.89–2.92) were the associated factors of growth retardation (all P < 0.05). Pulmonary hypertension (OR = 3.77, 95% CI: 3.13–4.24), low birth weight (OR = 3.04, 95% CI: 2.61–4.18) and pneumonia (OR = 2.35, 95% CI: 2.08–2.83) were the associated factors of low body weight of children with CHD (all P < 0.05).
Conclusions: Medical staff should fully understand the risk factors, strengthen nutritional support and enhance nursing care for children with CHD to reduce malnutrition.
Congenital heart disease (CHD) is the disorder or abnormal development of the heart and large blood vessels caused by various factors during embryonic development, and it leads to abnormal anatomical structure of the heart and/or large vessels (1). CHD occurs in about 0.8% of newborns (2). Most children with CHD need interventional or surgical treatment, and their nutritional status directly affects perioperative complications and postoperative recovery (3). Children with CHD are likely to be complicated with infection, heart failure and hypoxemia, which can lead to malnutrition and growth retardation. As a result of changes in systemic nutritional supply caused by abnormal haemodynamics, increased energy demand caused by surgical stress and the use of positive inotropic drugs and insufficient energy supply caused by fluid restriction, malnutrition is common in children with CHD (4, 5). Studies (6–8) have shown that the incidence of acute and chronic malnutrition in children with CHD can be as high as 50%, which is higher than the average level of hospitalised children in the same age. Therefore, the treatments and nursing care of malnutrition in children with CHD are critical.
The relevant guidelines (9, 10) define child malnutrition as an imbalance between nutritional needs and intake, resulting in insufficient accumulation of energy, protein or micronutrients, which has a negative impact on the growth and development of children. Malnutrition can increase the risk of postoperative infection in children with CHD, prolong mechanical ventilation and hospital stay, increase mortality and increase the economic burden of children's families (11–13). Therefore, the associated factors of malnutrition in children with CHD must be identified for targeted intervention to be carried out. At present, numerous studies have investigated the associated factors of malnutrition in children with CHD, but the sample size of most studies is small, and the factors included in these studies vary. Related meta-analyses to evaluate the associated factors of malnutrition in children with CHD are few. Therefore, this study analysed the related studies of malnutrition in children with CHD and systematically evaluated the associated factors of malnutrition in children with CHD to provide reference and evidence for the clinical treatment and nursing care of children with CHD.
This meta-analysis was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (14).
The two researchers searched the literature about the associated factors of malnutrition in children with CHD in PubMed, web of science, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Database, Weipu and Chinese Biomedical Literature Database until 25 June 2023. The combination of subject words and free words was adopted. The search strategies were as follows: (“congenital heart disease” OR “congenital heart defects” OR “CHD”) AND (“malnutrition”) OR “nutrition” OR “weight” OR “retardation” OR “development”). We also reviewed and screened the references of included studies and related reviews to retrieve as many relevant studies as possible.
The inclusion criteria of this study were as follows: the type of study was a case–control study, cohort study or cross-sectional study; the study population were children with CHD; the age was less than 18 years old; and the exposure factors were related to malnutrition in children with CHD. The outcome index was malnutrition, the definition of malnutrition was based on the growth standard Z score established by World Health Organization (WHO) (15) and Z score < −2 was defined as malnutrition. The exclusion criteria of this study were as follows: literature with low quality or high bias risk (quality score < 4); literature that could not obtain full text or incomplete data; and repeatedly published studies.
The two researchers independently assessed the quality of the included studies, cross-checked after the evaluation and negotiated with a third researcher to resolve differences. The case–control study and cohort study were evaluated with the Newcastle–Ottawa scale (16), which consists of eight items. The literature was evaluated by the semi-quantitative principle of star system, with a total score of 9 points and a high-quality study ≥6. The cross-sectional study was evaluated using the bias risk assessment criteria recommended by the American Institute for Health Care quality and Research (17). A total of 11 items were answered with “yes”, “no” and “unclear”. The total score was 11; ≤3 indicates low quality, 4–7 indicates medium quality and ≥8 indicates high quality.
In this study, RevMan 5.3 software was used for statistical analysis of the data. The effect was evaluated by odds ratio (OR) and its 95% confidence interval (CI). The included studies were analysed for clinical heterogeneity. Chi-square test combined with I2 was used to quantitatively assess the heterogeneity. If P ≥ 0.1, I2 < 50%, then there was no heterogeneity among studies, and the fixed-effect model was used. If P < 0.1, I2 ≥ 50%, then there was heterogeneity among studies, and the random-effect model was used. If clinical heterogeneity was too large, descriptive analysis was used. Sensitivity analysis was performed to test the stability of the results. In this study, the difference was statistically significant when P < 0.05.
We initially identified 198 related reports, and we screened the remaining 185 articles after duplicate removal. After reading the titles and abstracts and removing the articles that obviously did not meet the inclusion criteria, we then read the full text and finally included 13 reports (18–30). The 13 studies (18–30) involved a total of 8,031 children with CHD. The literature screening process is shown in Figure 1, and the basic characteristics of the literature are shown in Table 1.
Eight cross-sectional studies were included in this study. The score of bias risk assessment was 510, of which five studies carried out quality control on the measurement of outcome indicators, and four studies explained the reasons for excluding analysis to be included in the study. Only two studies summarised the response rate of patients and the integrity of data collection. Three cohort studies were included, and the score of bias risk assessment was 7–8. Three case–control studies were included, in which one study did not explain the method of determining the case group and whether the response rate of the case group and the control group was the same, and the two other studies did not explain whether the response rate of the case group and the control group was the same.
As shown in Table 2, several studies reported the associated factors of growth retardation of children with CHD. This meta-analysis indicated that pulmonary hypertension (OR = 3.81, 95% CI: 2.46–4.12), low birth weight (OR = 2.69, 95% CI: 1.25–5.77) and parents' height (OR = 2.15, 95% CI: 1.89–2.92) were the associated factors of growth retardation of children with CHD (all P < 0.05).
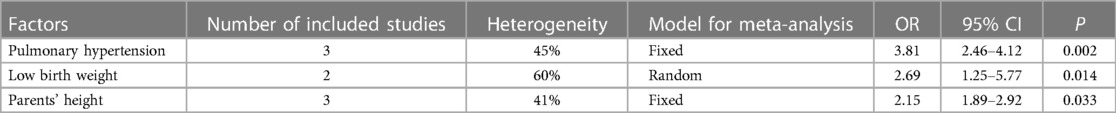
Table 2 Meta-analysis on the associated factors of growth retardation of children with congenital heart disease.
As shown in Table 3, several studies reported the associated factors of low body weight of children with CHD. This meta-analysis indicated that pulmonary hypertension (OR = 3.77, 95% CI: 3.13–4.24), low birth weight (OR = 3.04, 95% CI: 2.61–4.18) and pneumonia (OR = 2.35, 95% CI: 2.08–2.83) were the associated factors of low body weight of children with CHD (all P < 0.05).
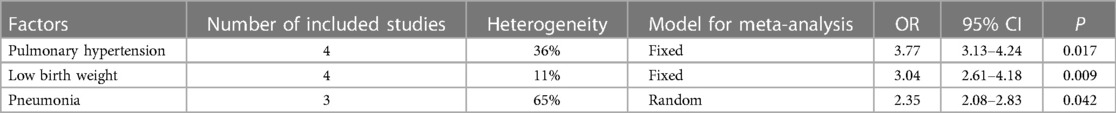
Table 3 Meta-analysis on the associated factors of low body weight of children with congenital heart disease.
Some studies did not explain the type of malnutrition involved, so we could not combine those data for analysis. Among them, the higher the Ross score of heart failure in children with CHD, the higher the risk of malnutrition. Some studies also reported that heart failure is the associated factor of malnutrition in children with CHD. Besides, age, gender, feeding difficulties, social status, postoperative residual shunt and long-term oral diuretics all affect the nutritional status of children with CHD.
We excluded each of the results of the meta-analysis one by one, and the results of the meta-analysis did not change significantly. The results of sensitivity analysis suggested that the results of the meta-analysis had good stability. Limited by the number of included studies, we could not perform the funnel plots. Regression analyses on those synthesised outcomes showed no publication biases (all P > 0.05).
Children with CHD are prone to malnutrition because of increased energy consumption and energy utilisation disorders, and postoperative complications and mortality in children with malnutrition are higher than those in children with normal nutritional status (31). Among 89 hospitalised children with CHD aged 12–45 months, 65.2% children have different degrees of malnutrition, and poor cardiopulmonary function is a common associated factor of malnutrition in children with CHD (32). Cardiac dysfunction and pneumonia lead to increased catecholamine secretion, increased work done by respiratory muscles, increased resting energy consumption and increased demand for nutrition (33). On the one hand, if complicated with pulmonary hypertension or heart failure, CHD will cause venous blood stasis and gastrointestinal dysfunction, affecting digestion and absorption; on the other hand, CHD will cause insufficient tissue perfusion, tissue ischemia and hypoxia and limited nutrition utilisation (34). The liquid intake of children is usually limited to reduce the cardiac volume load, further hindering the intake of nutrition (35). The interaction of the above factors leads to malnutrition in children with CHD. Therefore, timely treatment of the primary disease and active prevention of complications are the basis for improving malnutrition in children with CHD. This study analysed the associated factors of malnutrition in children with CHD. Clinical medical workers should adopt early warning and nursing measures for children with these risk factors to reduce the incidence of malnutrition.
The possible mechanisms of CHD affecting growth, development and nutritional status should be considered. Intestinal dysfunction due to venous congestion caused by heart failure leads to digestive and absorption disorders; at the same time, cardiac output decreases during heart failure, resulting in insufficient blood supply to the systemic circulation, hypoxia and acidosis in the surrounding tissues and nutritional utilisation disorders (36). Children with CHD are often complicated with purple, pulmonary hypertension and congestive heart failure. The more serious the pulmonary hypertension is, the longer the course of disease is, the greater the effect on growth and development will be (33, 37). Pulmonary hypertension can cause increased right ventricular afterload and pulmonary vasoconstriction, resulting in hypoxia and right heart failure, insufficient tissue oxygen supply, disturbance of nutritional utilisation and intestinal venous congestion (38, 39). These factors may increase the risk of poor growth and malnutrition in children. The effects of these factors on growth and development must be evaluated, because improving the state of malnutrition is beneficial to postoperative rehabilitation and reducing the risk of surgical complications and perioperative mortality.
Different from disease factors, congenital or genetic factors will affect the nutritional status of children with CHD for a long time, and preoperative malnutrition has a greater impact on weight than on height. Through surgical treatment, the abnormal anatomical structure of the heart can be corrected, and the timely supply of adequate nutrition after operation can help the children improve malnutrition (40). Studies (41, 42) have shown that low birth weight newborns often require 1 to 2 years to “catch up” to their peers. With the progress of medical technology, the age of children with CHD receiving surgical treatment is becoming increasingly younger. If children are born with a low weight, they may not be able to catch up with their growth in a short time, so they are characterised by growth retardation. In addition, height is a polygenic trait, and a child's height is affected by genetic factors. For tall parents with offspring who may also be taller than their peers, coupled with the causes of disease, their children are highly likely to develop growth retardation (43). Children with CHD with low birth weight and low parental height have low growth potential and are more likely to develop stunting in the long term than their counterparts. In clinical practice, attention should be paid to the identification of such children, and guidance and intervention to their families should be given if necessary.
Family factors are the associated factors of malnutrition in children with CHD. Given the particularity of children's age, parents play an important role in children's disease management. Many studies have shown that family economic status, parents' education level and parents' feeding behaviour are the associated factors of poor nutrition in children with CHD (44). Parents’ correct perception of disease is the protective factor of malnutrition in children with CHD, whereas parents' anxiety and depression will increase the risk of malnutrition (45). The caregivers' incorrect perception of the disease will lead to negative mood, incorrect diet structure and forced eating behaviour (46). Whilst paying attention to the children, the clinical medical staff should also pay close attention to the caregivers and guide the caregivers to adopt scientific and reasonable feeding behaviour.
In conclusion, many factors are associated with malnutrition in children with CHD, amongst which pulmonary hypertension and low birth weight are the most common factors. In addition, the cardiopulmonary function of the children and the disease cognition and emotion of the caregivers are common associated factors. The limitations of this meta-analysis were the wide age range of the studied population, different types of CHDs and no heterogenicity between the studied groups. Clinical health care providers should prioritise the prevention and active intervention of children with CHD, such as provide timely treatment of primary diseases, improve caregivers' awareness of the disease, alleviate their negative emotions and promote them to adopt correct feeding behaviour to reduce the risk of malnutrition in children with CHD.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
ChZ: Investigation, Writing – original draft. BX: Methodology, Writing – original draft, Writing – review & editing. CuZ: Conceptualization, Formal Analysis, Writing – original draft. KP: Formal Analysis, Writing – original draft, Writing – review & editing. LB: Formal Analysis, Funding acquisition, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liu A, Diller GP, Moons P, Daniels CJ, Jenkins KJ, Marelli A. Changing epidemiology of congenital heart disease: effect on outcomes and quality of care in adults. Nat Rev Cardiol. (2023) 20(2):126–37. doi: 10.1038/s41569-022-00749-y
2. van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. (2011) 8(1):50–60. doi: 10.1038/nrcardio.2010.166
3. Palleri D, Bartolacelli Y, Balducci A, Bonetti S, Zanoni R, Ciuca C, et al. Moderate and severe congenital heart diseases adversely affect the growth of children in Italy: a retrospective monocentric study. Nutrients. (2023) 15(3):4–8. doi: 10.3390/nu15030484
4. Frogoudaki AA. Congenital heart disease prevalence: what does the future hold? Eur J Prev Cardiol. (2023) 30(2):167–8. doi: 10.1093/eurjpc/zwac296
5. Nasr VG, Markham LW, Clay M, DiNardo JA, Faraoni D, Gottlieb-Sen D, et al. Perioperative considerations for pediatric patients with congenital heart disease presenting for noncardiac procedures: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. (2023) 16(1):e000113. doi: 10.1161/HCQ.0000000000000113
6. Diao J, Chen L, Wei J, Shu J, Li Y, Li J, et al. Prevalence of malnutrition in children with congenital heart disease: a systematic review and meta-analysis. J Pediatr. (2022) 242:39–47.e34. doi: 10.1016/j.jpeds.2021.10.065
7. Silva-Gburek J, Marroquin A, Flores S, Roddy J, Ghanayem NS, Shekerdemian LS, et al. Perioperative nutritional status and organ dysfunction following surgery for congenital heart disease. Pediatr Cardiol. (2023) 24:1–5. doi: 10.1007/s00246-023-03111-2
8. Tsega T, Tesfaye T, Dessie A, Teshome T. Nutritional assessment and associated factors in children with congenital heart disease-Ethiopia. PLoS One. (2022) 17(9):e0269518. doi: 10.1371/journal.pone.0269518
9. Baldini L, Librandi K, D'Eusebio C, Lezo A. Nutritional management of patients with Fontan circulation: a potential for improved outcomes from birth to adulthood. Nutrients. (2022) 14(19):16–20. doi: 10.3390/nu14194055
10. Mehta NM, Corkins MR, Lyman B, Malone A, Goday PS, Carney LN, et al. Defining pediatric malnutrition: a paradigm shift toward etiology-related definitions. JPEN J Parenter Enteral Nutr. (2013) 37(4):460–81. doi: 10.1177/0148607113479972
11. Mignot M, Huguet H, Cambonie G, Guillaumont S, Vincenti M, Blanc J, et al. Risk factors for early occurrence of malnutrition in infants with severe congenital heart disease. Eur J Pediatr. (2023) 30:7–11. doi: 10.1007/s00431-023-04812-9
12. Sethasathien S, Silvilairat S, Sittiwangkul R, Makonkawkeyoon K, Kittisakmontri K, Pongprot Y. Prevalence and predictive factors of malnutrition in Thai children with congenital heart disease and short-term postoperative growth outcomes. Nutr Health. (2022) 18:28–35. doi: 10.1177/02601060221082382
13. Zheng Y, Yang L, Wu Z, Zhu H, Xiao B, Li Z, et al. Assessment of dietary nutrient intake and its relationship to the nutritional status of children with congenital heart disease in Guangdong province of China. Asia Pac J Clin Nutr. (2022) 31(3):520–5. doi: 10.6133/apjcn.202209_31(3).0019
14. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. (2021) 134:178–89. doi: 10.1016/j.jclinepi.2021.03.001
15. Mitting R, Marino L, Macrae D, Shastri N, Meyer R, Pathan N. Nutritional status and clinical outcome in postterm neonates undergoing surgery for congenital heart disease. Pediatr Crit Care Med. (2015) 16(5):448–52. doi: 10.1097/PCC.0000000000000402
16. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25(9):603–5. doi: 10.1007/s10654-010-9491-z
17. Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. (2007) 36(3):666–76. doi: 10.1093/ije/dym018
18. Qin C, Juan J, Ying L. Preoperative nutritional status and influencing factors of children with congenital heart disease. J Cent South Univ. (2017) 42(9):1066–71.
19. Hu L, Wei B, Liao S. Analysis of influencing factors and quality of life of postoperative malnutrition in children with congenital heart disease. Chin J Child Health. (2021) 29(8):5–7.
20. Huang J, Lu F, Zhao Y. Nutritional status and risk factors of children with congenital heart disease. Adv Cardiol. (2020) 41(12):1324–7.
21. Jiao W. Nutritional status and its influencing factors of infants with ventricular septal defect before and after operation. J Peking Union Med Coll. (2012) 13(4):1–45.
22. Li L, Hu C, Shi H. Analysis of preoperative nutritional status of infants with congenital heart disease. Clin Med Eng. (2020) 27(6):2–5.
23. Monteiro FP, de Araujo TL, Lopes MV, Chaves DB, Beltrao BA, Costa AG. Nutritional status of children with congenital heart disease. Rev Lat Am Enfermagem. (2012) 20(6):1024–32. doi: 10.1590/s0104-11692012000600003
24. Okoromah CA, Ekure EN, Lesi FE, Okunowo WO, Tijani BO, Okeiyi JC. Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case-control observational study. Arch Dis Child. (2011) 96(4):354–60. doi: 10.1136/adc.2009.176644
25. Vaidyanathan B, Radhakrishnan R, Sarala DA, Sundaram KR, Kumar RK. What determines nutritional recovery in malnourished children after correction of congenital heart defects? Pediatrics. (2009) 124(2):e294–299. doi: 10.1542/peds.2009-0141
26. Wang X. Growth and intellectual development of infants with congenital heart disease. J Nanjing Univ. (2012) 32(1):12–7.
27. Xie S, Yin X, Zhao Y. Analysis of preoperative nutritional status and influencing factors in children with congenital heart disease. Chin Food Nutr. (2020) 26(3):86–8.
28. Xu M. Analysis of preoperative nutritional status and influencing factors of children with congenital heart disease. Chin J Clin. (2019) 547(9):1092–4.
29. Zhang C, Li X, Chen M. Effect of preoperative malnutrition on postoperative hospital prognosis in children with congenital heart diseas. Chongqing Med. (2022) 51(12):10–4.
30. Zhang M, Wang L, Huang R, Sun C, Bao N, Xu Z. Risk factors of malnutrition in Chinese children with congenital heart defect. BMC Pediatr. (2020) 20(1):213. doi: 10.1186/s12887-020-02124-7
31. Mills KI, Kim JH, Fogg K, Goldshtrom N, Graham EM, Kataria-Hale J, et al. Nutritional considerations for the neonate with congenital heart disease. Pediatrics. (2022) 150(Suppl 2):10–6. doi: 10.1542/peds.2022-056415G
32. Yanghua Z, Jianmei D, Lijuan W. Preoperative nutritional status and influencing factors in children with congenital heart disease. J Commun Med. (2019) 3(4):4–6.
33. Shi H, Yang D, Tang K, Hu C, Li L, Zhang L, et al. Explainable machine learning model for predicting the occurrence of postoperative malnutrition in children with congenital heart disease. Clin Nutr. (2022) 41(1):202–10. doi: 10.1016/j.clnu.2021.11.006
34. Luca AC, Miron IC, Mindru DE, Curpan AS, Stan RC, Tarca E, et al. Optimal nutrition parameters for neonates and infants with congenital heart disease. Nutrients. (2022) 14(8):22–6. doi: 10.3390/nu14081671
35. Horsley M, Pathak S, Morales D, Lorts A, Mouzaki M. Nutritional outcomes of patients with pediatric and congenital heart disease requiring ventricular assist devices. JPEN J Parenter Enteral Nutr. (2022) 46(7):1553–8. doi: 10.1002/jpen.2351
36. Alakeel YS, Ismail WW, Alrubayan NI, Almajed MA. Parenteral versus enteral nutrition in children with post-surgical congenital heart disease. Int J Health Sci (Qassim). (2021) 15(3):34–40.34234634
37. El-Ganzoury MM, El-Farrash RA, Ahmed GF, Hassan SI, Barakat NM. Perioperative nutritional rehabilitation in malnourished children with congenital heart disease: a randomized controlled trial. Nutrition. (2021) 84:111027. doi: 10.1016/j.nut.2020.111027
38. Hassan BA, Albanna EA, Morsy SM, Siam AG, Al Shafie MM, Elsaadany HF, et al. Nutritional Status in children with un-operated congenital heart disease: an Egyptian center experience. Front Pediatr. (2015) 3:53. doi: 10.3389/fped.2015.00053
39. Silvera Ruiz S, Grosso CL, Tablada M, Cabrera M, Dodelson de Kremer R, Juaneda E, et al. Efficacy of citrulline supplementation to decrease the risk of pulmonary hypertension after congenital heart disease surgery. A local experience. Rev Fac Cien Med Univ Nac Cordoba. (2020) 77(4):249–53. doi: 10.31053/1853.0605.v77.n4.27936
40. Woldesenbet R, Murugan R, Mulugeta F, Moges T. Nutritional status and associated factors among children with congenital heart disease in selected governmental hospitals and cardiac center, Addis Ababa Ethiopia. BMC Pediatr. (2021) 21(1):538. doi: 10.1186/s12887-021-03023-1
41. Huiwen Z. Investigation on nutrition and feeding status of children with congenital heart disease. Chin J Nurs. (2016) 51(6):5–7.
42. Yu H, Wenhe G, Lijie W. Effects of different energy feeding on nutrition and clinical outcome of children with congenital heart disease. China Pediatr Emerg Med. (2018) 25(3):5–8.
43. Lijuan L, Chunmei H, Linfang Z. Nutritional assessment and nutritional support analysis of children undergoing congenital heart disease surgery. Jilin Med. (2020) 41(5):3–6.
44. Lin Z, Xu W, Tuo P. Evaluation of nutritional status of infants with congenital heart disease and its relationship with postoperative prognosis. Chin J Mol Cardiol. (2016) 16(6):5–7.
45. Qianhong L. Effect of nutritional nursing intervention on nutritional status of children with ICU congenital heart disease. Chin J Pract Nurs. (2012) 28(18):2–6.
Keywords: malnutrition, children, congenital heart disease, care, paediatric, management
Citation: Zhang C, Xu B, Zhu C, Pu K and Bian L (2024) Risk factors of malnutrition in children with congenital heart disease: a meta-analysis. Front. Pediatr. 12: 1258725. doi: 10.3389/fped.2024.1258725
Received: 26 July 2023; Accepted: 8 July 2024;
Published: 29 July 2024.
Edited by:
Sajid Bashir Soofi, Aga Khan University, PakistanReviewed by:
Mona El Ganzoury, Ain Shams University, Egypt© 2024 Zhang, Xu, Zhu, Pu and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai Pu, cXRwODk1OTQ0QDE2My5jb20=; Lanzheng Bian, cm9uZzQ0MTU0MDc4QDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.