- Department of Pediatric Surgery, Children’s Hospital of Fudan University, Shanghai, China
Objective: To investigate health-related quality of life (HRQOL) in patients after surgical repair for esophageal atresia (EA) and identify its potential influencing factors.
Methods: A total of 102 EA children who had previously visited our hospital participated in this cross-sectional study. Basic data and disease data of the patients were collected. The HRQOL was measured with the Pediatric Quality of Life Inventory™4.0 (PedsQL™4.0) and EA-QOL questionnaire and ranked on a reverse 0–100 scale, with a higher number indicative of a better HRQOL perception. The scores of PedsQL™4.0 in children with EA were collected and compared with that of the demographically matched healthy control group. Meanwhile, the condition-specific HRQOL of EA was analyzed by the EA-QOL questionnaire, and the potential clinical factors that influenced the HRQOL were determined by the generalized linear model.
Results: The group of EA and control reached a similar score in the generic PedsQL™4.0 (EA group: 86.55 ± 9.69; control group: 89.41 ± 6.54; p = 0.670). There was no significant difference between the EA group and the control group in other domains except the school functioning. Condition-specific HRQOL in the 2–7-year-old group had the highest score in social isolation and stress domain and the lowest score in the physical health and treatment domain, with an overall quality of life score of 83.48 ± 10.22. The scores of the 8–17-year-old group were relatively high in social relationships and health and well-being and lowest in the eating domain, with an overall quality of life score of 89.43 ± 8.57. Heart malformation, complicated esophageal surgery history, respiratory symptoms,and digestive symptoms in the past 1 month were the main factors affecting the HRQOL of children aged 2–7 years. Complicated esophageal surgery history, respiratory symptoms, and digestive symptoms in the past 1 month were the main factors affecting the HRQOL of children aged 8–17 years.
Conclusions: The findings suggest that patients with EA generally had a good HRQOL. However, EA children with postoperative complications and associated symptoms have lower scores in the EA-QOL questionnaire.
Introduction
Esophageal atresia (EA) is one of the most serious congenital gastrointestinal developmental malformations, requiring neonatal surgery, with an incidence rate of 2.4:100,000 births (1). With the continuous improvement in surgery and neonatal care, the postoperative survival rate of EA children has exceeded 90% (2). However, postoperative EA patients are at risk of gastrointestinal and respiratory complications, which affects the long-term prognosis of some children (3). The health-related quality of life (HRQOL) after surgical repair has become the focus of follow-up and research.
HRQOL refers to a patient's subjective experience of daily life their physical, mental, and social functioning under the influence of the disease itself, and with medical interventions. These HRQOL instruments are generic or condition-specific (4). The generic instruments have wider applicability, which enable applications to compare differences between patients and healthy people (5). In the past, due to the lack of condition-specific instruments, HRQOL in EA patients after surgical repair was assessed using generic instruments, but these scales may ignore the influence of heterogeneity and the concomitant factors of EA. A few years ago, an EA-specific HRQOL instrument named EA-QOL questionnaire was developed in Sweden and Germany, with confirmed feasibility, reliability, and validity (6). It is reasonable to hypothesize that clinical factors associated with birth characteristics, surgery, and EA-related digestive and respiratory morbidity would affect these HRQOL domains negatively. However, only a few studies in the literature use this instrument to evaluate the postoperative quality of life in children with EA (7, 8). Due to the heterogeneity of EA, larger cohorts need to be investigated to ensure data reliability.
To fill this gap in our knowledge and yield more information for future studies, we aimed to evaluate generic as well as condition-specific HRQOL in Chinese children with EA. Moreover, we explored the risk factors that affect the HRQOL of children with EA to provide more evidence to improve the HRQOL.
Methods
Study design and participants
The cross-sectional survey was conducted during the period from September to December in 2022 and approved by the Ethics Committee of the Children's Hospital of Fudan University. All procedures were in compliance with the principles of the Declaration of Helsinki (as revised in 2013) and followed approved research protocols. The families of children who were accepted for the initial surgery in our hospital were selected as the study group. The medical records of the children were complete and their current ages ranged from 2 to 18. Meanwhile, we recruited children who were enrolled in the outpatient department for postoperative follow-up of oblique inguinal hernia as a healthy control group based on the demographic characteristics of the EA group. These healthy control group members did not have other disease or other abnormalities. All children in our study had been taken care of in the same way as in all other centers in the world. The cross-sectional survey was completed through the outpatient service, telephone, or internet. All the parents or guardians of the participating children read and signed the informed consent prior to participation. All surveys and questionnaires were completed by proxy-report.
Instruments
General information collection
A parent reported that the general information questionnaire developed by our team was used to obtain information on sociodemographic factors and health-related data of the children and their families. All questions were answered using a 1-month recall period, mainly including a child's gender, age, sleep quality, acute or chronic disease symptoms, as well as the age, gender, address, education level, and health status of the adult caregiver or parent. For children with EA, clinical data including birth weight, gestational week, combined deformity, therapies, postoperative complication, and the child's digestive and respiratory symptoms during the previous 1 month were collected.
PedsQL™ 4.0 generic core scale
The Pediatric Quality of Life Inventory™4.0 (PedsQL™ 4.0) was originally developed in the English language by Varni et al. (9, 10) and has a reliable and validated Chinese version. The PedsQL™ 4.0 generic core scale is adapted to children and adolescents aged 2–18 years and consists of questions related to four functional domains, including physical, emotional, social, and school functioning, with a total of 23 items. Each item is a question on the frequency of something that happend in the previous month, using a five-point Likert scale for responses. All items are linearly transformed to the 0–100 scale, with higher scores indicating better HRQOL. The normal values of PedsQL 4.0 were derived from previously conducted validation studies and a score below 80 could be considered as impaired quality of life (11–13).
EA-QOL questionnaire
The condition-specific EA-QOL questionnaire was originally developed for the Swedish-German study by Dellenmark-Blom et al. (14) and already has a standardized and content-validated Chinese Mandarin version (15). Our team also confirmed that the Chinese version of the scale showed good reliability and validity in the preliminary study. The EA-QOL questionnaire have two versions: (1) one for 2–7-year-old children and (2) another for 8–17-year-old children. The 2–7-year-old version includes three domains: eating, physical health and treatment, and social isolation and stress, for a total of 17 items; and the 8–17 year-old version includes four domains: eating, social relationships, body perception, and health and well-being, for a total of 22 items. Each item is a question on the frequency of something that happened in the previous month, according to a five-point Likert scale. All items are linearly transformed to the 0–100 scale. Higher scores indicate better HRQOL. Based on experience from previous studies, a score below 80 could be considered as impaired quality of life (16).
Statistical analysis
The general characteristics of the patients with EA are presented using descriptive statistics. The missing data are treated by the multiple imputation methods. For quantitative data with a normal distribution, the mean ± standard deviation (SD) is presented. Independent sample t-tests were used for comparisons of differences between groups. For quantitative data with a non-normal distribution, medians with interquartile intervals are presented. Mann–Whitney U tests were used for comparisons of differences between groups. For categorical data, comparisons between groups were performed using chi-square (χ2) tests or Fisher's precision probability test. The generalized linear model was then used to identify independent determinants of the HRQOL. A value of P < 0.05 was considered to be statistically significant. All statistical analyses were performed with the SPSS 28.0 statistical software (SPSS Inc., Chicago, USA).
Results
Children’s characteristics and questionnaire response
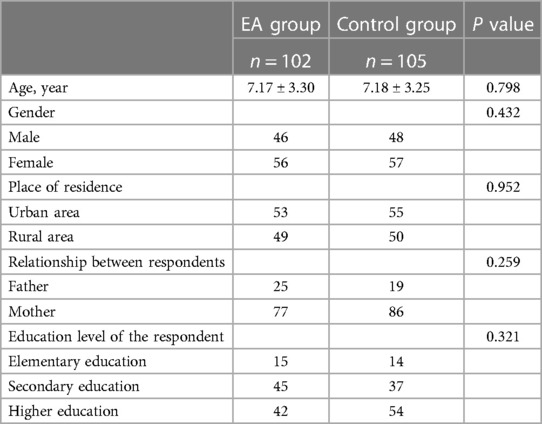
In total, 207 questionnaires were effectively collected including for 102 children with EA (46 male, 56 female) and 105 healthy children (48 male, 57 female). The mean age of the patients was 7.17 ± 3.30 years, median age was 7 years, range from 2 months to 14 years (IQR 4–10). The mean age of the healthy children was 7.18 ± 3.25 months, median age was 7 years, range from 2 months to 14 years (IQR 4–10). Table 1 shows the baseline characteristics of the children with EA and those in the control group. Age, gender, and family factors such as education level of the parents were not significantly different between the EA group and the control group.
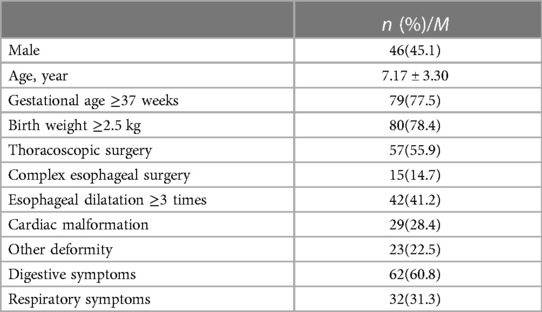
The demographic details and clinical data of the EA group are provided in Table 2. Among them, 79(77.5%) patients were full-term at birth and 80(78.4%) patients had normal birth weight. Furthermore, 29(28.4%) patients had accompanied heart malformation and 15(14.7%) children had other associated abnormalities. In addition, 57(55.9%) patients had thoracoscopic surgery, and 15(14.7%) patients had a history of complex esophageal surgery, including eight cases of long gap EA (seven patients received delayed primary anastomosis and one received colon replacement), two cases of esophageal re-anastomosis due to refractory stricture, and five cases of recurrent tracheoesophageal fistulas. A total of 62(60.8%) children had gastrointestinal symptoms at ordinary times, primarily mild dysphagia, which manifested as slow eating (eating speed lagging behind the healthy children in the same age and with each meal lasting for more than half an hour). A total of 36 (35.2%) cases had symptoms of reflux or heartburn after eating. Most of them only had slight symptoms, which could be controlled by pillow padding. Two patients had severe reflux symptoms and had to further undergo fundus folding surgery after being confirmed by esophagography as having gastroesophageal reflux. Their reflux symptoms are much improved currently. In addition, 32(31.3%) children had respiratory symptoms, including coughing, chest distress, or polypnea when resting or active, or frequent respiratory infections.
Comparison of PedsQL™4.0 scores between children with EA and control group
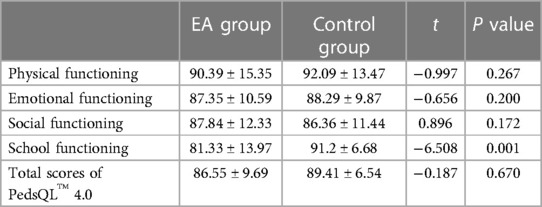
The results showed that children with EA had the highest score in the physical functioning domain and the lowest score in the school functioning domain, as shown in Table 3. They had a good quality of life in the areas of physiological, emotional, and social functioning, and there was no significant statistical difference compared with the control group. However, the scores in the areas of school functioning were still significantly lower than that of the control group, although the average score exceeded 80 points (P < 0.05). Compared with the control group, there was no significant difference in the overall score of EA children (P > 0.05).
Scores of the EA-QOL questionnaire in children with EA
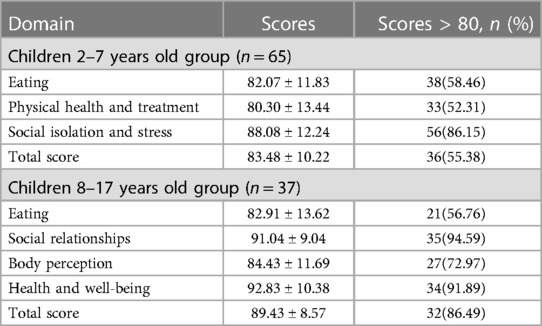
A total of 65 questionnaires were collected from the 2–7-year-old group. The results showed that the HRQOL scores were the lowest in the area of physical health and treatment, with a score of 80.30 ± 13.44, and 33 (52.31%) children had a score more than 80 points. The children had the highest average scores of 88.08 ± 12.24 in the areas of social isolation and stress domain, and 56 (86.15%) children had a score more than 80 points. The score in the area of eating was 82.07 ± 11.83, and 38 (58.46%) children had a score more than 80 points. The overall HRQOL score was 83.48 ± 10.22, and 36 (55.38%) cases scored above 80 points.
A total of 37 questionnaires were collected from the 8–17-year-old group. The results showed that the scores of the 8–17-year-old children with EA in the domain of eating were relatively low, 82.91 ± 13.62, and 24 (64.8%) children were above 80 points. The scores were relatively high in the domain of social relationships and health and well-being. The scores of the two domains were 91.04 ± 9.04 and 92.83 ± 10.38, 35 (94.59%) and 34 (91.89%) cases were above 80 points. In the domain of body perception, the score was 84.43 ± 11.69, with 34 (91.89%) cases higher than 80 points. The overall HRQOL score was 89.43 ± 8.57, and 32 (86.49%) cases were above 80 points. The scores of each domain are shown in Table 4.
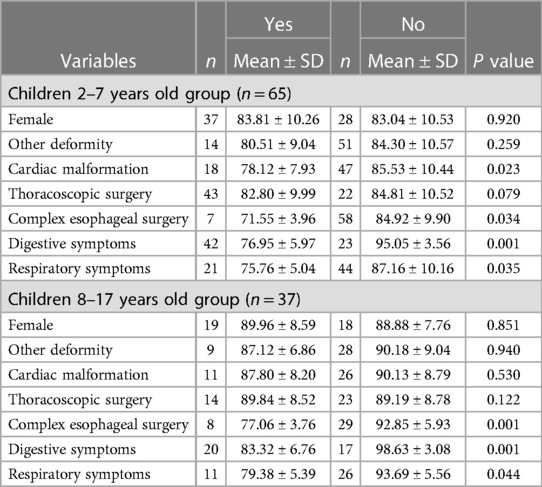
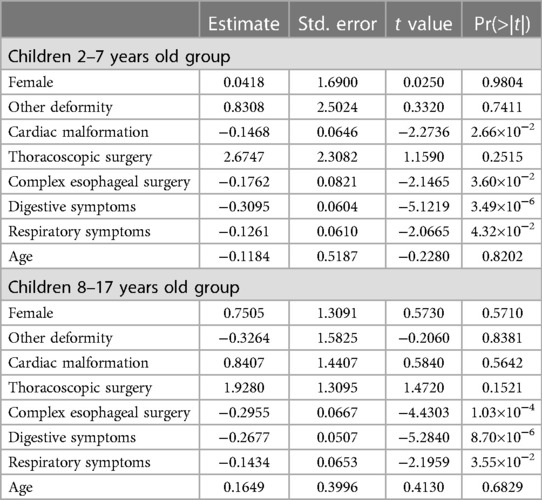
Factors influencing the quality of life of patients with EA
The generalized linear model was used to further explore influencing factors of the 2–7 and 8–17-year-old groups of children, respectively. As shown in Tables 5, 6, heart malformation, complicated esophageal surgery history, respiratory symptoms, and digestive symptoms in the past 1 month were the main factors affecting the quality of life of children aged 2–7 years. Complicated esophageal surgery history, respiratory symptoms, and digestive symptoms in the past 1 month were the main factors affecting the quality of life of children aged 8–17 years. Besides, the relationship between thoracoscopic surgery and body perception is presented in Supplementary Table S1.
Discussion
Despite advances in the prognosis of EA, knowledge on patients’ HRQOL is relatively sparse in the literature. This study reported postoperative quality of life in children with EA in the Chinese population, which fills several knowledge gaps of the medium and long-term prognosis in China. First, these data indicated children with EA had a good quality of life, generally no different from normal children. Second, the study showed the the HRQOL of children with EA aged 2–7 years was mainly impaired in the Physical health and Treatment domain, while those aged 8–17 years were in the eating domain. Finally, a history of complex esophageal surgery, and postoperative digestive and respiratory symptoms, were identified as major factors affecting the condition-specific HRQOL of EA patients throughout childhood, while cardiac malformation primarily affected children aged 2–7 years. Our study used a combination of generic and specific instruments to evaluate the HRQOL of children with EA, providing more comprehensive information for such studies.
Our study adopted the most commonly used generic scale for children, the PedsQL™ 4.0, to evaluate the HRQOL of EA survivors. Previously, some centers have conducted studies on generic HRQOL, with conflicting results. Legrand et al. (17) described that overall HRQOL in children with EA was reduced as compared with healthy children, with impairments in all the four domains of PedsQL™ 4.0. Children with dyspnea and dysphagia had impaired emotional functioning, and children with combined malformations, especially heart disease, had lower school performance scores. Another cohort was consistent and proposed that children with EA had significantly impaired emotional and social functioning. The average score of emotional functioning in all age groups was 52.73–60.05, which was the lowest in all domains (18). In addition, some researchers have reported different degrees of impaired HRQOL in different areas (19, 20). However, a study reported that overall HRQOL among children with EA was similar to that of a healthy reference group (21). Our research showed that children with EA had a good quality of life in the physiological, emotional, and social functioning domains, and there were no significant statistical differences compared with the control group, except for significantly lower scores in the school functioning domain. The overall quality of life score of children with EA was not significantly different from that of the control group. The HRQOL condition in our study appeared to be better than in some of the aforementioned literature reports (16, 17). In this study, the cases of EA combined with severe malformations, chromosome abnormalities, and severe disease status were more likely to be abandoned or lost to follow-up, while cases with fewer malformations, no chromosome abnormalities, and mild disease status were more likely to adhere to treatment and obtain long-term follow-up, which may lead to better prognosis of follow-up and evaluation in this study.
Our study also provides a preliminary reference for EA-specific HRQOL in the Chinese population. In previous reports from other countries, four of six articles stated that the 2–7-year-old group had the lowest scores in the physical health and treatment domain (6, 22–24), one article described lowest scores in the social isolation and stress domain (25), and one article did not report the specific HRQOL of the 2–7-year-old group (26). All six articles reported that the 8–17-year-old group had the lowest scores in the eating domain (6, 22–26). Our results were similar to these studies. In the 2–7-year-old group, young EA postoperative patients still need to be hospitalized repeatedly owing to esophageal anastomotic stenosis, combined with heart defects, tracheomalacia, and recurrent respiratory symptoms, which could lead to an impaired physical health and treatment domain. In the 8–17-year-old group, EA postoperative patients in this age group have received treatment and shown improvement for problems such as anastomotic stenosis, combined deformity, tracheomalacia, and recurrent respiratory symptoms that they faced at a younger age, and have entered a stable stage, while the problem of postoperative esophageal motor dysfunction has become increasingly prominent.
Our study also identified several potential factors associated with lower condition-specific HRQOL, including a history of complex esophageal surgery, digestive and respiratory symptoms in both groups, and cardiac malformation in the 2–7-year-old group. Although prior studies have identified several acknowledged factors associated with lower generic HRQOL, including prematurity, respiratory and digestive symptoms, gastrostomy procedure, and severe EA (17, 20, 21, 27), only a few studies in the literature have described potential factors affecting condition-specific HRQOL (16, 28). One report suggested that the condition-specific HRQOL domain of pediatric patients after EA repair was negatively affected by digestive symptoms throughout childhood, while respiratory symptoms primarily affected children aged 2–7 years (16). In addition, no primary anastomosis, esophageal dilatation, as well as gastrostomy insertion secondary to long-gap EA or severe gastroesophageal reflux predicted worse scores related to eating domain in all ages; associated anomalies were related to worse body perceptions (16). Another research stated that days of discharge after EA repair and concomitant abnormalities were significantly negatively correlated with HRQOL scores in the 2–7 age group, while relevant respiratory and digestive tract symptoms such as airway infection, swallowing difficulties, and heartburn were associated with lower HRQOL scores in the 8–17 years group (28). Our results support the relevant opinions of the previous literature. Besides, we found thoracoscopic surgery was related to better scores in the body perception domain, which has rarely been discussed in the previous HRQOL studies. Only one study mentioned that there are no significant differences in the HRQOL of children after school age between the traditional and thoracoscopic surgery groups (29). Our findings support that thoracoscopic repair has the advantages of less trauma and superior cosmetic results compared with the thoracotomy (30), which could improve body perception.
Our study also had some limitations. First, in accordance with the wishes of the majority of the respondents, we adopted parent-proxy questionnaire in this investigation. This could create potential bias, although some studies have shown a good parent–child agreement (26). Second, as a single-center pilot study conducted on Chinese patients, the generalizability of the result and value in practical applications needs to be further verified. Third, the type of EA and the surgical options (early vs. delayed primary anastomosis) may also impact the HRQOL. Because of the limited sample size, these factors have not been fully explored in this study. In the future, we hope to continue this study by enlarging the sample size and seeking the cooperation of other centers to further verify the accuracy of these results.
In conclusion, patients with EA generally have a good quality of life after surgery, although children with postoperative complications and associated symptoms have lower scores in the EA-QOL questionnaire. Early repeated hospitalizations and surgeries may have long-term effects on the physical health. Children with EA with symptoms and scars have more negative perceptions of their bodies. At the same time, complex esophageal surgeries such as fundoplication worsen esophageal outlet obstruction and esophageal functional disorders, negatively affecting the eating domain of patients’ quality of life. Therefore, postoperative follow-up of patients with EA is necessary, early attention should be paid, and their quality of life should be improved through psychological counseling, health education, and by alleviating complications.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Children’s Hospital of Fudan University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
ZF: Conceptualization, Methodology, Supervision, Writing – original draft. HZ: Conceptualization, Writing – review & editing. WH: Investigation, Methodology, Writing – review & editing. XP: Investigation, Writing – review & editing. RG: Investigation, Writing – review & editing. YT: Writing – review & editing. XC: Writing – review & editing. GC: Writing – review & editing. KD: Writing – review & editing. SZ: Writing – review & editing. CS: Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
The work was supported by Shanghai Municipal Key Clinical Specialty (No. shslczdzk05703), National Natural Science Foundation of China (81873849), and Shanghai Medical Innovation Research Special Project (21Y1907300).
Acknowledgments
We acknowledge the support of the patients and their parents. We are also grateful to development team of Chinese-Mandarin EA-QOL-questionnaire for their help and support during the research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1332979/full#supplementary-material
References
1. van Lennep M, Singendonk M, Dall'Oglio L, Gottrand F, Krishnan U, Terheggen-Lagro S, et al. Oesophageal atresia. Nat Rev Dis Primers. (2019) 5:26. doi: 10.1038/s41572-019-0077-0
2. Sulkowski JP, Cooper JN, Lopez JJ, Jadcherla Y, Cuenot A, Mattei P, et al. Morbidity and mortality in patients with esophageal atresia. Surgery. (2014) 156:483–91. doi: 10.1016/j.surg.2014.03.016
3. Acher C, Ostlie D, Leys C, Struckmeyer S, Parker M, Nichol P. Long-term outcomes of patients with tracheoesophageal fistula/esophageal atresia: survey results from tracheoesophageal fistula/esophageal atresia online communities. Eur J Pediatr Surg. (2016) 26:476–80. doi: 10.1055/s-0035-1570103
4. Koivusalo A, Pakarinen MP, Turunen P, Saarikoski H, Lindahl H, Rintala RJ. Health-related quality of life in adult patients with esophageal atresia—a questionnaire study. J Pediatr Surg. (2005) 40:307–12. doi: 10.1016/j.jpedsurg.2004.10.014
5. Dellenmark-Blom M, Chaplin JE, Gatzinsky V, Jönsson L, Abrahamson K. Health-related quality of life among children, young people and adults with esophageal atresia: a review of the literature and recommendations for future research. Qual Life Res. (2015) 24:2433–45. doi: 10.1007/s11136-015-0975-x
6. Dellenmark-Blom M, Dingemann J, Witt S, Quitmann JH, Jönsson L, Gatzinsky V, et al. The esophageal-atresia-quality-of-life questionnaires: feasibility, validity and reliability in Sweden and Germany. J Pediatr Gastr Nutr. (2018) 67:469–77. doi: 10.1097/MPG.0000000000002019
7. Dellenmark-Blom M, Quitmann J, Dingemann C. Health-related quality of life in patients after repair of esophageal atresia: a review of current literature. Eur J Pediatr Surg. (2020) 30:239–50. doi: 10.1055/s-0040-1710389
8. International EA-QOL Group. Establishment of a condition-specific quality-of-life questionnaire for children born with esophageal atresia aged 2-7 across 14 countries. Front Pediatr. (2023) 11:1253892. doi: 10.3389/fped.2023.1253892
9. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Med Care. (2001) 39:800–12. doi: 10.1097/00005650-200108000-00006
10. Desai AD, Zhou C, Stanford S, Haaland W, Varni JW, Mangione-Smith RM. Validity and responsiveness of the pediatric quality of life inventory (PedsQL) 4.0 generic core scales in the pediatric inpatient setting. JAMA Pediatr. (2014) 168:1114–21. doi: 10.1001/jamapediatrics.2014.1600
11. Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 generic core scales. Health Qual Life Out. (2007) 5:43. doi: 10.1186/1477-7525-5-43
12. Amedro P, Huguet H, Macioce V, Dorka R, Auer A, Guillaumont S, et al. Psychometric validation of the French self and proxy versions of the PedsQL™ 4.0 generic health-related quality of life questionnaire for 8–12 year-old children. Health Qual Life Out. (2021) 19:75. doi: 10.1186/s12955-021-01714-y
13. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. (2003) 3:329–41. doi: 10.1367/1539-4409(2003)003%3C0329:tpaapp%3E2.0.co;2
14. Dellenmark-Blom M, Chaplin JE, Gatzinsky V, Jönsson L, Wigert H, Apell J, et al. Health-related quality of life experiences among children and adolescents born with esophageal atresia: development of a condition-specific questionnaire for pediatric patients. J Pediatr Surg. (2016) 51:563–9. doi: 10.1016/j.jpedsurg.2015.09.023
15. Li S, Dellenmark-Blom M, Zhao Y, Gu Y, Li S, Yang S, et al. The Chinese Mandarin version of the esophageal-atresia-quality-of-life questionnaires for children and adolescents: evaluation of linguistic and content validity. Int J Environ Res Public Health. (2022) 19:14923. doi: 10.3390/ijerph192214923
16. Dellenmark-Blom M, Quitmann J, Dingemann J, Witt S, Ure BM, Bullinger M, et al. Clinical factors affecting condition-specific quality-of-life domains in pediatric patients after repair of esophageal atresia: the Swedish-German EA-QOL study. Eur J Pediatr Surg. (2020) 30:096–103. doi: 10.1055/s-0039-1693729
17. Legrand C, Michaud L, Salleron J, Neut D, Sfeir R, Thumerelle C, et al. Long-term outcome of children with oesophageal atresia type III. Arch Dis Child. (2012) 97:808–11. doi: 10.1136/archdischild-2012-301730
18. Rozensztrauch A, Śmigiel R, Patkowski D. Congenital esophageal atresia—surgical treatment results in the context of quality of life. Eur J Pediatr Surg. (2019) 29:266–70. doi: 10.1055/s-0038-1641597
19. Peetsold MG, Heij HA, Deurloo JA, Gemke RJ. Health-related quality of life and its determinants in children and adolescents born with oesophageal atresia. Acta Paediatr. (2010) 99:411–7. doi: 10.1111/j.1651-2227.2009.01579.x
20. Leibovitch L, Zohar I, Maayan-Mazger A, Mazkereth R, Strauss T, Bilik R. Infants born with esophageal atresia with or without tracheo-esophageal Fistula: short- and long-term outcomes. Isr Med Assoc J. (2018) 20:161–6.29527854
21. Lepeytre C, De Lagausie P, Merrot T, Baumstarck K, Oudyi M, Dubus J. Medium-term outcome, follow-up, and quality of life in children treated for type III esophageal atresia. Arch Pediatrie. (2013) 20:1096–104. doi: 10.1016/j.arcped.2013.06.035
22. Rozensztrauch A, Śmigiel R, Patkowski D, Gerus S, Kłaniewska M, Quitmann JH, et al. Reliability and validity of the Polish version of the esophageal-atresia-quality-of-life questionnaires to assess condition-specific quality of life in children and adolescents born with esophageal atresia. Int J Environ Res Public Health. (2022) 19:8047. doi: 10.3390/ijerph19138047
23. Ten Kate CA, IJsselstijn H, Dellenmark-Blom M, van Tuyll Van Serooskerken ES, Joosten M, Wijnen RMH, et al. Psychometric performance of a condition-specific quality-of-life instrument for Dutch children born with esophageal atresia. Children (Basel, Switzerland). (2022) 9:1508. doi: 10.3390/children9101508
24. Witt S, Bloemeke J, Bullinger M, Dingemann J, Dellenmark-Blom M, Quitmann J. Agreement between mothers’, fathers’, and children’s’ ratings on health-related quality of life in children born with esophageal atresia—a German cross-sectional study. BMC Pediatr. (2019) 19:330–330. doi: 10.1186/s12887-019-1701-6
25. Soyer T, Arslan UE, Ulukaya Durakbaşa Ç, Aydöner S, Boybeyi-Türer Ö, Quitmann JH, et al. Feasibility, reliability, and validity of the Turkish version of the esophageal-atresia-quality-of-life questionnaires to assess condition-specific quality of life in children and adolescents born with esophageal atresia. Turk J Gastroenterol. (2021) 32:640–50. doi: 10.5152/tjg.2021.201005
26. Witt S, Dellenmark-Blom M, Kuckuck S, Dingemann J, Abrahamsson K, Dingemann C, et al. Parent—child-agreement on health-related quality of life and its determinants in patients born with esophageal atresia: a Swedish—German cross-sectional study. Orphanet J Rare Dis. (2021) 16:120. doi: 10.1186/s13023-021-01748-x
27. Flieder S, Dellenmark-Blom M, Witt S, Dingemann C, Quitmann J, Jönsson L, et al. Generic health-related quality of life after repair of esophageal atresia and its determinants within a German—Swedish cohort. Eur J Pediatr Surg. (2019) 29:075–84. doi: 10.1055/s-0038-1672144
28. Dellenmark-Blom M, Örnö Ax S, Öst E, Svensson JF, Kassa A, Jönsson L, et al. Postoperative morbidity and health-related quality of life in children with delayed reconstruction of esophageal atresia: a nationwide Swedish study. Orphanet J Rare Dis. (2022) 17:239. doi: 10.1186/s13023-022-02381-y
29. Miyano G, Seo S, Nakamura H, Sueyoshi R, Okawada M, Doi T, et al. Changes in quality of life from infancy to school age after esophagus ophagostomy for tracheoesophageal fistula: thoracotomy versus thoracos copy. Pediatr Surg Int. (2017) 33:1087–90. doi: 10.1007/s00383-017-4141-0
Keywords: esophageal atresia, quality of life, questionnaire, PedsQL™ 4.0, EA-QOL questionnaire
Citation: Feng Z, Zhu H, He W, Peng X, Gao R, Tian Y, Cao X, Chen G, Dong K, Zheng S and Shen C (2024) Health-related quality of life in children after surgical repair of esophageal atresia: a cross-sectional study in China. Front. Pediatr. 11:1332979. doi: 10.3389/fped.2023.1332979
Received: 20 November 2023; Accepted: 19 December 2023;
Published: 9 January 2024.
Edited by:
Andrea Conforti, Bambino Gesù Children’s Hospital (IRCCS), ItalyReviewed by:
Tutku Soyer, Hacettepe University, TürkiyeRiccardo Coletta, University of Florence, Italy
© 2024 Feng, Zhu, He, Peng, Gao, Tian, Cao, Chen, Dong, Zheng and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun Shen Y2h1bnNoZW5AZnVkYW4uZWR1LmNu
 Zhong Feng
Zhong Feng Haitao Zhu
Haitao Zhu Weijing He
Weijing He Yuxin Tian
Yuxin Tian Xuqing Cao
Xuqing Cao Gong Chen
Gong Chen Chun Shen
Chun Shen