- 1Department of Pediatric Dentistry and Orthodontics, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
- 2College of Dentistry, King Saud University, Riyadh, Saudi Arabia
Background: This study aimed to evaluate and compare the shear bond strength (SBS) of EQUIA Forte HT with that of other restorative materials, including EQUIA Forte, glass ionomer cement (GIC), and resin-modified glass ionomer cement (RMGIC) when bonded to NeoMTA 2.
Materials and methods: A total of 120 holes were created in Teflon molds and filled with NeoMTA 2. The restorative materials were immediately applied using customized silicone molds. The samples were randomly divided into two main groups: one to measure the immediate SBS and the other to measure the delayed SBS. These two main groups were further divided into four subgroups based on the restorative material used: EQUIA Forte HT, EQUIA Forte, GIC, and RMGIC.
Results: The study groups showed statistically significant differences in the mean SBS (p < 0.0001). The immediate SBS of the RMGIC group (mean ± SD: 5.43 ± 1.22) was significantly higher than those of the GIC and EQUIA Forte groups, with no significant difference found compared to the SBS of EQUIA Forte HT. In the delayed SBS, both the RMGIC and EQUIA Forte HT groups (4.98 ± 0.67 and 4.93 ± 0.60, respectively) demonstrated significantly higher bond strengths than the GIC and EQUIA Forte groups (3.81 ± 0.57 and 4.2 ± 0.63, respectively). However, there were no statistically significant differences between the RMGIC and EQUIA Forte HT groups or between the GIC and EQUIA Forte groups.
Conclusion: Based on our findings, EQUIA Forte HT has shown promising outcomes when used as a restorative material following pulpotomies, with results comparable to those of RMGIC.
1. Introduction
Glass ionomer cement (GIC) materials have a wide range of applications in pediatric and restorative dentistry due to their ability to release fluoride over an extended period (1, 2). However, they are vulnerable to fracture due to their poor flexural strength and fatigue properties (3).
To circumvent these disadvantages, resin-modified glass ionomer cement (RMGIC) was developed. However, RMGIC has a mechanical strength that is inferior to that of composite resin materials and is not considered a permanent restorative material. Furthermore, it has the disadvantage of polymerization shrinkage due to its resin content. To overcome these mechanical limitations, EQUIA Forte was introduced as a long-term restorative alternative.
EQUIA Forte is a self-curing, resin-free, highly viscous GIC that releases fluoride (F−) and calcium ions (Ca2+) (4). It is a bulk-fill glass hybrid (GH) reinforced with ultrafine reactive glass particles. To strengthen the cross-linking of the matrix and enhance the material's flexural strength, EQUIA Forte has also been reinforced with secondary silicate particles of smaller size and higher reactivity, along with acrylic acid molecules of elevated molecular weight. The application of a resin coat to these restorations is allegedly meant to enhance both their wear resistance and esthetic appearance (5).
To further enhance the aesthetic properties, EQUIA Forte HT (GC, Tokyo, Japan) was released in 2019, featuring increased translucency (6). This restorative material exhibits a refined smaller particle size distribution in comparison to its precursor, EQUIA Forte. This refinement contributed to the enhancement of both flexural and compressive strength, resulting in improved matrix loading (7).
Several studies have been conducted on EQUIA Forte HT, demonstrating its reliability as a restorative material with good clinical performance in both primary and permanent teeth (5, 8). Kutuk et al. conducted a study on EQUIA Forte HT in stress-bearing Class II restorations in pediatric patients and concluded that it offers more strength and superior aesthetics compared to a microhybrid composite (G-aenial Posterior, GC Corp., Tokyo, Japan) for both primary and permanent teeth (5).
To date, the application of the relatively newly introduced EQUIA Forte HT to the novel bioceramic material NeoMTA 2 (NuSmile, Houston, TX, USA) has not been studied for its use in primary teeth after pulpotomies. Therefore, this study aimed to evaluate and compare the shear bond strength (SBS) of EQUIA Forte HT with that of other restorative materials—namely, EQUIA Forte, GIC, and RMGIC—when applied to NeoMTA 2.
2. Materials and methods
2.1. Ethical clearance
Ethical clearance for this study was obtained from the institutional review board (No. E-22-7160), and the College of Dentistry Research Center (CDRC No. IR 043).
2.2. Sample size calculation
The sample size was calculated from the previously available literature with a 95% confidence interval and 80% power of the study. For an α value of 0.05, an effect size of 0.45, and a power of 0.95, the total sample size should be at least 120.
2.3. Study design
A total of 120 holes were created in Teflon molds, each measuring 4 mm in diameter and 2 mm in depth, filled with NeoMTA 2. Next, the surface was smoothened using a plastic filling instrument (PF13) to prepare the samples for bonding. A universal adhesive (Single Bond Universal 3M, ESPE, St. Paul, MN, USA) was applied to the surface of the bioceramic material using a rubbing motion for 20 s. The adhesive was subsequently subjected to air drying for 5 s and a light-curing process for 10 s.
To apply the restorative material, a customized silicone mold with a diameter of 3 mm and a thickness of 2 mm was fabricated for use in the bonding procedure. The mold was placed at the center of the NeoMTA 2 layer. The restorative materials were applied immediately after the placement of NeoMTA 2 according to the manufacturer's instructions (Table 1).
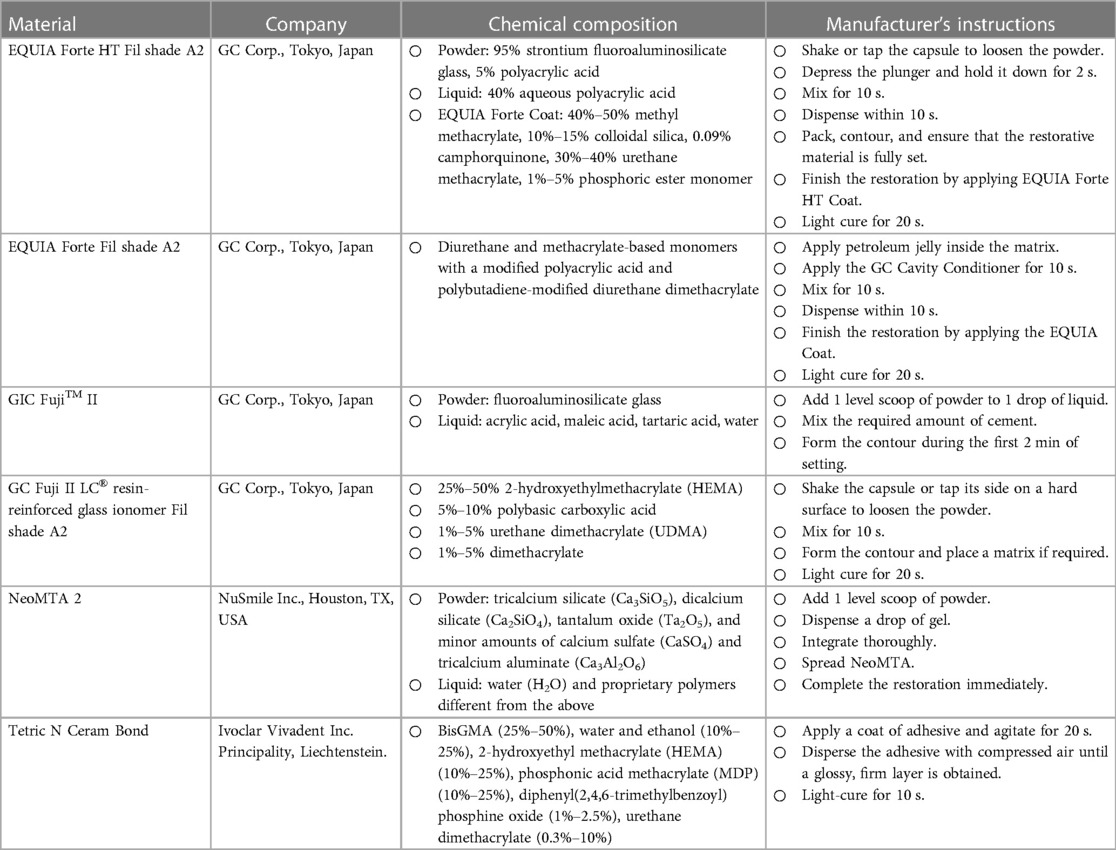
Table 1. Materials used in the study (name, company, chemical composition, and manufacturer's instructions).
An LED light-curing device (Bluephase G2, Ivoclar Vivadent, Schaan, Liechtenstein) was used to cure all the samples. After that, the samples were divided equally into two main groups: one to measure the immediate SBS and the other to measure the delayed SBS.
Before performing the SBS tests, all the samples were preserved in artificial saliva and stored in an incubator (GI2 So-Low Cincinnati, OH, USA) at 37 °C and 100% humidity for 24 h. Next, only the samples in the delayed restorative group were loaded in a thermocycling machine (Huber, SD-Mechatronik-Thermocyclerr, Germany) at 5 °C for 2,000 cycles of thermocycling and 55 °C for 5,000 cycles of thermocycling to mimic 6 months of physiological use.
2.4. SBS test
The SBS of each sample was determined using a universal testing machine (Instron 5965, Instron, England) with a knife-edged rod moving at a crosshead speed of 0.5 mm/min (Supplementary Material Figure S1). The SBS was calculated in MPa using the following formula: stress (MPa) = force2 (N)/bonding area (mm2).
In the case of the immediate SBS group, after 24 h, the samples were mounted in the universal testing machine with the crosshead perpendicular and flush to the interface of the restoration and the bioceramic material (Supplementary Material Figure S2). For the delayed SBS group, the SBS test was performed after 7 days in the same manner as for the immediate SBS group.
2.5. Mode of failure
To discover the fracture pattern after the SBS test, the samples' surfaces were examined using a digital microscope (HIROX, KH-7700, Digital microscope system, Tokyo, Japan).
The failure modes were categorized as follows: (1) adhesive failure: failure between the NeoMTA 2 layer and the restorative material; (2) cohesive failure type 1: cohesive failure within the NeoMTA 2 layer; (3) cohesive failure type 2: cohesive failure within the restorative material; and (4) mixed failure: both adhesive and cohesive failures.
2.6. Statistical analysis
The immediate SBS and SBS after the aging process of NeoMTA 2 combined with the four types of restorative materials were reported as the mean ± standard deviation (SD). The mean SBS of each group was determined using a one-way analysis of variance (ANOVA) followed by Tukey's multiple comparison test to assess the differences between the groups. The significance of the difference between the immediate and delayed SBS for each material was calculated using the Student's t-test. The data were analyzed using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA). A p-value of <0.05 was considered statistically significant.
3. Results
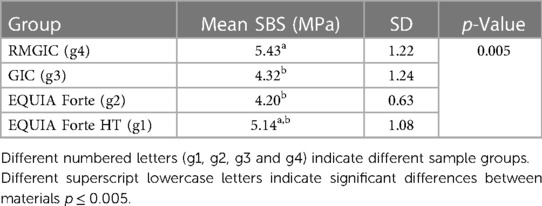
Table 2 shows the mean immediate SBSs of the self-adhering glass ionomer materials on NeoMTA 2. There were statistically significant differences between the mean SBSs of some of the study groups (p = 0.005). The SBS of the RMGIC group (5.43 ± 1.22) was significantly higher than that of the GIC and EQUIA Forte groups (4.32 ± 1.24 and 4.2 ± 0.63, respectively). However, there was no statistically significant difference between the RMGIC group and the EQUIA Forte HT group.
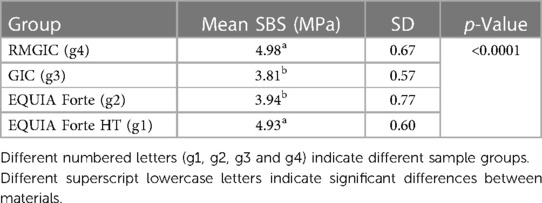
The mean SBSs of the self-adhering glass ionomer materials to NeoMTA 2 after the aging process are presented in Table 3. There was a statistically significant difference between the mean SBSs of some of the study groups (p < 0.0001). The SBSs of the RMGIC and EQUIA Forte groups (4.98 ± 0.67 and 4.93 ± 0.60, respectively) were significantly higher than those of the GIC and EQUIA Forte groups (3.81 ± 0.57 and 4.2 ± 0.63, respectively). However, there was no statistically significant difference between the RMGIC and EQUIA Forte HT groups or between the GIC and EQUIA Forte groups.
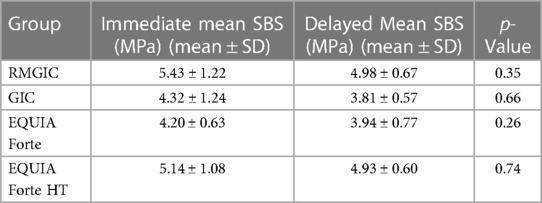
Table 4 presents the mean SBSs of the different study materials at different times. Overall, the immediate SBS was higher than the SBS after the aging process among all groups, although the differences were not statistically significant.
The types of failure modes in the immediate and delayed SBS groups are represented in Supplementary Material Figure S4, S5, respectively. In the immediate SBS groups, EQUIA Forte HT showed a combination (cohesive–adhesive) failure rate of 53.3%, while Equia Forte and GIC had adhesive failure rates of 93.3% and 86.6%, respectively. Finally, RMGIC showed a cohesive failure rate within the NeoMTA 2 layer of 93.3%.
In the delayed SBS groups, cohesive failure within the NeoMTA 2 layer was the most common form of failure found in the EQUIA Forte HT (66.6%), EQUIA Forte (53.3%), and RMGIC (73.3%) groups. However, adhesive failure was predominant in the GIC group (80%).
4. Discussion
Within the limitations of the current study, the null hypothesis that there was no significant difference between the SBS of EQUIA Forte HT and that of other restorative materials—namely, EQUIA Forte, GIC, and RMGIC—when combined with NeoMTA 2 was rejected. The results of the present study regarding both the immediate and delayed SBS revealed a significantly higher mean SBS for EQUIA Forte HT compared to GIC and EQUIA Forte. However, RMGIC showed the highest mean SBS, which is consistent with a previous study, which found that the immediate placement of RMGIC on ProRoot MTA showed the highest SBS (7.18 MPa), followed by NeoMTA 2 (4.15 MPa) (9). Al-homaidhi et al. reported that the SBS of RMGI immediately placed over NeoMTA 2 was statistically high (10), which is consistent with the results of this study.
In another recent study conducted by El-Refai et al. in 2023 (11), the delayed SBSs of four different restorative materials (Fuji II LC, EQUIA Forte Fil, Cention N, and Venus Bulk Fil) applied to a pre-mixed bioceramic material (NeoPutty) were calculated. The findings indicated that the mean SBS for the RMGIC (Fuji II LC) was high (18.33 ± 2.29 MPa), which is consistent with the results of our study. However, it was demonstrated that EQUIA Forte exhibited the lowest mean SBS (7.07 ± 1.06 MPa) of all materials. When comparing the findings of prior research, it can be observed that NeoPutty exhibits similarities to NeoMTA 2 in terms of its primary compositional elements. Similarly, EQUIA Forte can be regarded as comparable to EQUIA Forte HT (7, 12). However, it is crucial to consider a significant aspect of the methodology employed in the previous literature: the delayed application time of the restorative material.
Previous studies (13–15) have provided evidence in favor of delayed restoration following the placement of mineral trioxide aggregate (MTA). It has been claimed that the water sorption from freshly mixed MTA could be attributed to the presence of GIC, resulting in inadequate hydration of MTA and the presence of significant porosity, the interface junction between the glass ionomer and MTA exhibited a notable presence of microcracking, leading to the separation of the two materials and the subsequent degradation of the adhesive junction (11). However, additional research (16–18) has provided support for the immediate application of the restorative material directly over the MTA, taking the advantage of short initial setting time of 14 min at 37 °C, thereby aligning with the real clinical scenario.
A study conducted by Nandini et al. (16) showed that conventional GIC may be applied over a partially set MTA in a single visit. The authors also observed that the setting process of MTA remained unaffected beneath the GIC layer. Another study conducted by Palma et al. (19) yielded results comparable to those of our study: the researchers concluded that the use of Biodentine and the immediate placement of the final restoration yielded the highest average SBS (4.44 MPa). Furthermore, Alqahtani et al. (9) stated that the immediate application of the Fuji II LC resin-modified glass ionomer on ProRoot MTA exhibited significantly higher SBS compared to delayed application.
Regarding the modification of the MTA surface before the application of restorative materials, previous studies (14, 20, 21) have demonstrated that the process of acid etching when performed as a separate step, can lead to the degradation of the MTA surface. This degradation is characterized by a reduction in cohesive strength, a decrease in microhardness, a decline in compressive strength, and the formation of an amorphous gel-like surface structure.
Furthermore, it is imperative to prioritize the simplification of dental procedures and the reduction of working time when addressing pediatric patients. Based on this fact, it can be inferred that employing a universal bonding agent without performing a distinct pre-etching procedure would be the more favorable approach. Furthermore, the selection of the 3M Single Bond Universal Adhesive for the present study was predicated upon its pH value of 2.7. Based on this characteristic, it can be categorized as an ultra-mild etching system, thereby enabling the generation of appropriate surface micro-irregularities on the NeoMTA 2 surface while maintaining the integrity of the surface crystals, which is essential for establishing a strong adhesive junction (22).
In the present study, EQUIA Forte HT exhibited the second highest SBS among all the materials. When a conventional GIC is applied on top of MTA, two potential reactions may occur at the interface. First, the carboxylate groups (COO–) of the polyacrylic acid within the GIC may interact with the calcium ions present in the MTA, resulting in the formation of calcium salts. Second, the silicate hydrate gel of the MTA can undergo condensation with the silicate hydrate gel of the GIC, leading to the generation of by-products (16). Rodríguez-Lozano et al. (23) demonstrated that NeoMTA 2 exhibits a greater release of calcium ions compared to alternative bioceramic materials, such as NeoMTA Plus and Bio-C Repair, suggesting the theoretical existence of a strong bond between EQUIA Forte HT and NeoMTA 2. However, the lack of calcium, which is substituted by strontium in EQUIA Forte HT, could be a cause of the weak bonding to NeoMTA 2, which resulted in a lower mean SBS than in conventional RMGIC. Nicholson et al. (24) also stated that strontium functions as a cement-forming ion. However, the addition of strontium oxide powder to GIC did not significantly enhance its properties (24).
EQUIA Forte HT is a high-viscosity GIC that does not contain any resinous constituents. As a result, the formation of strong chemical bonds with the resinous component of the universal adhesive is not feasible, suggesting potential limitations in the capacity for chemical bonding with 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) molecules. The main mechanism of bonding in EQUIA Forte HT is likely the micromechanical interlocking facilitated by etching the surface of NeoMTA 2 using the ultra-mild universal adhesive. Nevertheless, the resulting micromechanical interlocking may not have had major effects. This is primarily due to the high viscosity of EQUIA Forte, which may have impeded its flow and penetration into the micro-irregularities of the NeoMTA 2 surface (11).
This suggests that the primary chemical interaction occurs between the silicate hydrate gel of the MTA and the silicate hydrate gel of the GIC. It should be noted that there is a lack of literature on the chemical interactions at the interface between EQUIA Forte HT and NeoMTA 2. Tsuzuki et al. found that the early stages of the GIC-setting reaction comprised both endothermic and exothermic reactions, confirming the occurrence of reactions other than carboxylate formation (25).
In 2021, Duman et al. compared the SBSs of Medcem Pure Portland Cement, Medcem MTA, and NeoMTA to those of compomer, RMGIC, EQUIA Forte HT, and Cention N (26). They found that EQUIA Forte HT showed the highest SBS along with Medcem Pure Portland Cement, while the lowest SBSs of all groups were yielded by EQUIA Forte HT and NeoMTA.
In the previous study done by Duman et al.2021, the samples were loaded with different biomaterials and held at 37 °C for 4 h in distilled water, as it was believed that a moist environment is necessary to ensure the appropriate setting of MTA. However, this technique proved ineffective due to the lack of moisture control, resulting in heightened porosity and solubility, which ultimately compromised the material's strength (27). Therefore, preserving the samples for 4 h might not be favorable for the experiment, which is why this step was not performed in our study.
Moreover, comparing the findings of different research studies is challenging due to the variability of multiple relevant factors, including the specific characteristics of the restorative materials, adhesive systems, technical application methods, and restoration application time used. Such comparisons are further complicated by variations in experimental methods, such as the rate of load application and the magnitude of the maximum load employed to assess the SBS.
Overall, the immediate SBS was higher than the SBS after the aging process among all groups in our study, although the difference was not statistically significant. Concerning the failure modes, the examination demonstrated that the two most common failure modes for EQUIA Forte HT were cohesive failure within the bioceramic material (Neo MTA 2) or combination (cohesive–adhesive) failure.
Cohesive failure indicates that the materials have reached maximum adhesive strength; therefore, it is a preferred mode of fracture. In the present study, the immediate SBS of EQUIA Forte HT showed a 53.3% combination (cohesive–adhesive) failure rate and a 66.6% cohesive failure rate within NeoMTA 2 in the delayed SBS group. The results are somewhat consistent with previously conducted studies on MTA and premixed bioceramics, which showed more cohesive and mixed cohesive–adhesive failures (9, 10).
Davis et al. explained the intricate nature of mixed-mode failures (28). These failures pose challenges in terms of interpretation, as it is uncertain whether the bond failure was the cause or the consequence of the crash. Quantifying the degree of bond degradation is difficult, as it is inherently subjective and cannot be measured precisely. Consequently, the terminology employed to describe the extent of degradation is limited to subjective terms, such as “moderate” or “predominant.” The sole ascertainable fact is that the bond strength decreased compared to its initial value. Regarding the impact of thermocycling on the SBS, Arıc et al. determined that the mean SBS of RMGIC decreased following this process (29).
In vitro, studies ignore the presence of dentin and thus do not fully reflect real clinical settings in which three interfaces can be identified: the interface between the bioceramic and dentin, the interface between the restorative material and dentin, and the interface between the bioceramic and the restorative material. This study assessed only the third interface. Therefore, further clinical trials are needed, particularly in the presence of saliva contamination. Additionally, only immediate placement was assessed in this study, highlighting the pressing need for future studies to assess the delayed application time of the restorative material.
5. Conclusion
Following conclusions are drawn. First, this study can aid clinicians in selecting the optimal material for clinical applications. Based on our results, EQUIA Forte HT has shown promising outcomes when used as a restorative material following MTA pulpotomies, with results comparable to those of RMGIC. Second, we showed that the immediate SBS was higher than the SBS after the aging process among all the studied groups. However, these differences were not statistically significant.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical clearance for this study was obtained from the institutional review board (No. E-22-7160), and the College of Dentistry Research Center (CDRC No. IR 043).
Author contributions
SB: Data curation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. AS: Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. MA: Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. MA: Supervision, Writing – original draft, Writing – review & editing. NA: Data curation, Visualization, Writing – original draft. LA: Data curation, Visualization, Writing – original draft. NA: Data curation, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank the College of Dentistry Research Center and the Deanship of Scientific Research at King Saud University, Saudi Arabia, for funding this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1303005/full#supplementary-material
References
1. Ge KX, Quock R, Chu CH, Yu OY. The preventive effect of glass ionomer restorations on new caries formation: a systematic review and meta-analysis. J Dent. (2022) 125:1–10. doi: 10.1016/j.jdent.2022.104272
2. Sikka N, Brizuela M. Glass ionomer cement. Treasure Island, FL: StatPearls Publishing (2023). (Updated March 19, 2023).
3. Amend S, Boutsiouki C, Bekes K, Kloukos D, Lygidakis NN, Frankenberger R, et al. Clinical effectiveness of restorative materials for the restoration of carious primary teeth without pulp therapy: a systematic review. Eur Arch Paediatr Dent. (2022) 23:727–59. doi: 10.1007/s40368-022-00725-7
4. Lauro D, Di Duca A, Montuori F, Dal P, Di Lauro A, Di Duca F, et al. Citation: fluoride and calcium release from alkasite and glass ionomer restorative dental materials: in vitro study. J Funct Biomater. (2023) 14:109. doi: 10.3390/jfb14020109
5. Kutuk ZB, Ozturk C, Cakir FY, Gurgan S. Mechanical performance of a newly developed glass hybrid restorative in the restoration of large MO class 2 cavities. Niger J Clin Pract. (June 2019) 22(6):833–41. doi: 10.4103/njcp.njcp_628_18
6. Kisby L. Glass-hybrid restorations in pediatric patients. Compend Contin Educ Dent. (2021) 42(Suppl. 1):4–5.34612659
7. EQUIA. ForteTM HT EQUIA ForteTM HT Comprehensive Guide (2018). Available at: http://www.gceurope.comhttp://uk.gceurope.com (Accessed March 2023).
8. Mickenautsch S. High-viscosity glass-ionomer cements for direct posterior tooth restorations in permanent teeth: the evidence in brief. J Dent. (2016) 55:121–3. doi: 10.1016/j.jdent.2016.10.007
9. Alqahtani AS, Sulimany AM, Alayad AS, Alqahtani AS, Bawazir OA. Evaluation of the shear bond strength of four bioceramic materials with different restorative materials and timings. Materials (Basel, Switzerland). (2022) 15(13):4668. doi: 10.3390/ma15134668
10. Al-Homaidhi M. Shear bond strength of an endodontic tricalcium silicate-based putty to different adhesive systems at different time intervals. J Res Med Dent Sci. (2021) 9(9):149–53.
11. El-Refai D. Shear bond strength of NuSmile-neoputty bio-ceramic material to four different restorative materials used in pedodontics. Egypt Dent J. (2023) 69(2):1343–65. doi: 10.21608/edj.2023.186169.2402
12. Primus C. Bioactive ceramics for pediatric dentistry. In: Fuks AB, Moskovitz M, Tickotsky N, editors. Contemporary endodontics for children and adolescents. Cham: Springer (2023). p. 362–63. doi: 10.1007/978-3-031-23980-9_11
13. Atabek D, Sillelioglu H, Ölmez A. Bond strength of adhesive systems to mineral trioxide aggregate with different time intervals. J Endod. (2012) 38(9):1288–92. doi: 10.1016/j.joen.2012.06.004
14. Kayahan MB, Nekoofar MH, Kazandag` M, Canpolat C, Malkondu O, Kaptan F, et al. Effect of acid-etching procedure on selected physical properties of mineral trioxide aggregate. Int Endod J. (2009) 42(11):1004–14. doi: 10.1111/j.1365-2591.2009.01610.x
15. VanderWeele RA, Schwartz SA, Beeson TJ. Effect of blood contamination on retention characteristics of MTA when mixed with different liquids. J Endod. (2006) 32(5):421–4. doi: 10.1016/j.joen.2005.09.007
16. Nandini S, Ballal S, Kandaswamy D. Influence of glass-ionomer cement on the interface and setting reaction of mineral trioxide aggregate when used as a furcal repair material using laser Raman spectroscopic analysis. J Endod. (2007) 33(2):167–72. doi: 10.1016/j.joen.2006.10.010
17. Ballal S, Venkateshbabu N, Nandini S, Kandaswamy D. An in vitro study to assess the setting and surface crazing of conventional glass ionomer cement when layered over partially set mineral trioxide aggregate. J Endod. (2008) 34(4):478–80. doi: 10.1016/j.joen.2008.01.020
18. Tsujimoto M, Tsujimoto Y, Ookubo A, Shiraishi T, Watanabe I, Yamada S, et al. Timing for composite resin placement on mineral trioxide aggregate. J Endod. (2013) 39(9):1167–70. doi: 10.1016/j.joen.2013.06.009
19. Palma PJ, Marques JA, Falacho RI, Vinagre A, Santos JM, Ramos JC. Does delayed restoration improve shear bond strength of different restorative protocols to calcium silicate-based cements? Materials (Basel). (2018) 11(11):2216. doi: 10.3390/ma11112216
20. Lee YL, Lee BS, Lin FH, Yun Lin A, Lan WH, Lin CP. Effects of physiological environments on the hydration behavior of mineral trioxide aggregate. Biomaterials. (2004) 25(5):787–93. doi: 10.1016/S0142-9612(03)00591-X
21. Namazikhah MS, Nekoofar MH, Sheykhrezae MS, Salariyeh S, Hayes SJ, Bryant ST, et al. The effect of pH on surface hardness and microstructure of mineral trioxide aggregate. Int Endod J. (2008) 41(2):108–16. doi: 10.1111/j.1365-2591.2007.01325.x
22. Giannini M, Makishi P, Ayres APA, Vermelho PM, Fronza BM, Nikaido T, et al. Self-etch adhesive systems: a literature review. Braz Dent J. (2015) 26:3–10. doi: 10.1590/0103-6440201302442
23. Rodríguez-Lozano FJ, Lozano A, López-García S, García-Bernal D, Sanz JL, Guerrero-Gironés J, et al. Biomineralization potential and biological properties of a new tantalum oxide (Ta2O5)–containing calcium silicate cement. Clin Oral Invest. (2022) 26:1427–41. doi: 10.1007/s00784-021-04117-x
24. Deb S, Nicholson JW. The effect of strontium oxide in glass–ionomer cements. J Mater Sci Mater Med. (1999) 10:471–4. doi: 10.1023/A:1008944924726
25. Tsuzuki FM, Pascotto RC, Malacarne LC, Bento AC, Neto AM, de Castro-Hoshino LV, et al. Studies of the early stages of the dynamic setting process of chemically activated restorative glass-ionomer cements. Biomater Investig Dent. (2021) 8(1):39–47. doi: 10.1080/26415275.2021.1898964
26. Çalışkan A, Çalışkan S, Duman S. Comparison of medcem MTA, medcem pure Portland cement and NeoMTA to pediatric restorative materials to shear bond strength. Necmettin Erbakan Universitesi Dis Hekimligi Dergisi (NEU Dent J). Necmettin Erbakan. (2021) 3(3):115–21.
27. Savitri D, Suprastiwi E, Margono A. Applying glass ionomer cement to MTA flowTM and biodentineTM and its effects on the interface layer. J Phys Conf Ser. (2017) 884:1–5. doi: 10.1088/1742-6596/884/1/012109
28. Davis MJ, McGregor A. Assessing adhesive bond failures: mixed-mode bond failures explained. Proceedings of the ISASI Australian safety seminar; 4–6 June 2010; Canberra, Australia (2010).
Keywords: EQUIA Forte HT, NeoMTA 2, resin-modified glass ionomer, shear bond strength, pulpotomy
Citation: BinSaleh S, Sulimany AM, Aldowsari MK, Al-Homaidhi M, Alkuait N, Almashham L and Alghamdi N (2023) Evaluation of the shear bond strength of a tricalcium silicate-based material to four self-adhering glass ionomer materials: an in vitro study. Front. Pediatr. 11:1303005. doi: 10.3389/fped.2023.1303005
Received: 27 September 2023; Accepted: 23 November 2023;
Published: 4 December 2023.
Edited by:
Sreekanth Kumar Mallineni, Tohoku University, JapanReviewed by:
Jaya Chandra Bhumireddy, RIMS Medical College Ongole, IndiaAnshad Mohamed Abdulla, King Khalid University, Saudi Arabia
© 2023 BinSaleh, Sulimany, Aldowsari, Al-Homaidhi, Alkuait, Almashham and Alghamdi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mannaa Aldowsari bWFsZG93c2FyaUBrc3UuZWR1LnNh
 Saad BinSaleh1
Saad BinSaleh1 Mannaa K. Aldowsari
Mannaa K. Aldowsari