
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 07 December 2023
Sec. Neonatology
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1278104
 Lulu Mussa Muhe1*
Lulu Mussa Muhe1* Christina R. Paganelli2
Christina R. Paganelli2 Rahell Hailu Ayele1
Rahell Hailu Ayele1 Tigist Desta3
Tigist Desta3 Amha Mekasha1
Amha Mekasha1 Asrat Demtse1
Asrat Demtse1 Tesfamichael Awoke1
Tesfamichael Awoke1 Teferi Elfu4
Teferi Elfu4 Tewodros Yalew Gebremariam1
Tewodros Yalew Gebremariam1 Dagnachew Tamrat1
Dagnachew Tamrat1 Amanuel Damie Jiffar1
Amanuel Damie Jiffar1 Aklilu Mekasha Zenabu1
Aklilu Mekasha Zenabu1 Moti Sori1
Moti Sori1 Lindsay Parlberg2
Lindsay Parlberg2 Alemayehu Worku1
Alemayehu Worku1 Assaye Kassie Nigussie5
Assaye Kassie Nigussie5
Background: With a neonatal mortality rate of 33 per 1,000 live births in 2019, Ethiopia is striving to attain the Sustainable Development Goal target of 12 deaths per 1,000 live births by 2030. A better understanding of the major causes of neonatal mortality is needed to effectively design and implement interventions to achieve this goal. Minimally Invasive Tissue Sampling (MITS), an alternative to conventional autopsy, requires fewer resources and through task-shifting of sample collection from pathologists to nurses, has the potential to support the expansion of pathology-based post-mortem examination and improve mortality data. This paper evaluates the accuracy and adequacy of MITS performed by nurses at a tertiary and general hospital and in the home of the deceased.
Methods: Nurses in a tertiary and general hospital in Ethiopia were trained in MITS sample collection on neonatal deaths and stillbirths using standardized protocols. MITS sample collection was performed by both pathologists and nurses in the tertiary hospital and by nurses in the general hospital and home-setting. Agreement in the performance of MITS between pathologists and nurses was calculated for samples collected at the tertiary hospital. Samples collected by nurses in the general hospital and home-setting were evaluated for technical adequacy using preestablished criteria.
Results: One hundred thirty-nine MITS were done: 125 in hospitals and 14 inside homes. There was a perfect or almost perfect agreement between the pathologists and the nurses in the tertiary hospital using Gwet's agreement interpretation criteria. The adequacy of MITS samples collected by nurses in the general hospital was more than 72% when compared to the preset criteria. The adequacy of the MITS sampling yield ranged from 87% to 91% on liveborn neonatal deaths and 76% for the liver, right and left lungs and 55% for brain tissues in stillbirths.
Conclusions: This study demonstrated that task-shifting MITS sample collection to nurses can be achieved with comparable accuracy and adequacy as pathologists. Our study showed that with standardized training and supportive supervision MITS sample collection can be conducted by nurses in a tertiary, general hospital and, at the home of the deceased. Future studies should validate and expand on this work by evaluating task-shifting of MITS sample collection to nurses within community settings and with larger sample sizes.
Globally countries are striving to meet the Sustainable Development Goal (SDG) target of reducing neonatal mortality to less than 12 per 1,000 livebirths by 2030 (1). The neonatal mortality rate in Ethiopia in 2019 was 33 per 1,000 livebirths (2) and it has not decreased since 2017 (2). To attain the SDG target of reducing neonatal mortality to fewer than 12 neonatal deaths per 1,000 livebirths targeted interventions need to be scaled up.
An accurate understanding of cause of death is needed to identify and inform interventions to reduce neonatal deaths and stillbirths. This is especially true in resource-constrained settings such as Ethiopia, where the cause of death is rarely medically certified and even when causes are documented, they are often based on sources such as verbal autopsy, which has variable validity and accuracy (3–5). The gold standard for determining cause of death, the Complete Diagnostic Autopsy (CDA), is recognized to be the most accurate post-mortem examination method (6, 7). However, it is resource intensive, requires pathologists, and is time consuming (8). In 2019 it was estimated that Ethiopia had fewer than 100 pathologists nationwide, resulting in a ratio of one pathologist per one million population (9, 10), few of whom work in rural settings where most stillbirths, neonatal and young infant deaths occur. Minimally Invasive Tissue Sampling (MITS), a pathology-based post-mortem examination typically conducted by pathologists, consists of transcutaneous needle sampling of organs and body fluids for histological and microbiological analysis (11–13). MITS has been validated against CDA, including comparing CDA to MITS in neonates in a large tertiary hospital in Addis Ababa (14, 15), Ethiopia. Because MITS requires fewer resources, is less invasive, and is more acceptable to families (16, 17), the utility of MITS in resource-constrained settings is high and more so if MITS can be conducted by health workers with less specialized training than pathologists.
In 2020 the Ethiopia Nurses Association estimated there were more than 43,000 nurses nationwide (one nurse per 2,299 population), most of whom work at the primary care level (9, 10). The process of shifting specific tasks from highly qualified health workers to health workers with shorter training is called task-shifting. Task-shifting has been shown to increase efficiency, cost effectiveness and improve access within health systems (18–21). When implemented with standardized training and quality assurance processes, task-shifting MITS sample collection from pathologists to nurses has the potential to reduce barriers to improving mortality data for stillbirths and neonates in primary and community settings.
To date, the operational feasibility and effectiveness of task-shifting within the context of MITS has not been systematically evaluated. The objective of this study was to assess the accuracy and adequacy of MITS samples collected by nurses compared with pathologists in a tertiary hospital and to assess the operational feasibility of nurses performing MITS at a general hospital and in the home of the deceased.
This was an observational study using standardized procedures and protocols to prospectively collect MITS samples in a tertiary hospital, a general hospital and in the homes of deceased stillbirths and neonates. Prior to the initiation of MITS sample collection formative research, including community engagement involving community leaders, was conducted to inform study design and implementation.
In March 2020 through February 2021 MITS samples were collected by both pathologists and nurses at Ethiopia's largest referral hospital, Tikur Anbessa Specialized Hospital (TASH) Neonatal Intensive Care Unit (NICU) in the capital city of Ethiopia, Addis Ababa. TASH has a well-organized 40-bed capacity NICU.
Beginning March 2021 through August 2022 MITS samples were collected by trained nurses working in Butajira General Hospital (BGH), in the town of Butajira, located 138 km south of Addis Ababa. BGH serves rural communities in Butajira District and is part of the Butajira Health and Demographic Surveillance Site (HDSS), established in 1987 (22). BGH has a delivery room and small 12-bed NICU. MITS samples were collected from neonatal deaths and stillbirths occurring both in the hospital as well as deaths occurring at home. Unlike at TASH, MITS sampling at BGH was not done by the pathologists as it was logistically infeasible. Instead, a team of pathologists reviewed the adequacy of the samples collected by the nurses using preset evaluation criteria.
Nurses were trained to perform MITS using a standardized training curriculum (23). Five nurses from TASH and twelve nurses from BGH, were trained on MITS sample collection. These trainings were conducted by senior pathologists experienced in MITS. Training of the nurses consisted of a one-day mostly didactic session followed by 4 days of practical training collecting lung, liver, and brain tissues. Per the standardized curriculum, training facilitators utilized a step-by-step checklist to ensure that nurses performed MITS sample collection completely and consistently. Throughout the course of the study senior investigators and pathologists provided in-person and virtual supportive supervision to reinforce the nurses' skills and ensure sample quality.
The inclusion criteria for MITS were neonatal deaths occurring in the hospital before the age of 28 days and stillbirths in both TASH and BGH. Inclusion criteria for BGH also included stillbirths born in the NICU or at home within the HDSS catchment area. In both settings the exclusion criteria included deaths where MITS could not be completed within 24 h of death or parents or legal guardians refused consent.
Written consent for MITS was obtained from the parents or legal guardians in Amharic, the local language, within 24 h of death for both hospital and home deaths.
In both TASH and BGH, tissue samples were obtained from brain, lungs (left and right) and the liver per the MITS Surveillance Alliance standard operating procedures for MITS sample collection (24). Blood and CSF specimens were not collected as part of this study. A sample was considered adequate if a minimum of two cores of target tissues were collected for each organ. Target tissue for the brain was defined as a sample including grey matter, white matter, ependymal, meninges, and at least one intact (unfragmented) large tissue bit identified for brain. Target tissue for the lung was defined as a sample that included tissue from both small airways and large airways with at least one large and intact tissue segment. Liver target tissue was defined as including at least six portal tracts and at least one intact large tissue segment (Supplementary Material S1). In the TASH study, MITS was performed twice for each recruited death, first by a nurse followed by a pathologist, both trained in MITS sample collection; at BGH only nurses collected samples.
A team of four pathologists independently assessed the quality of all samples to determine if adequate target tissue was obtained using preset histopathological criteria (25). A consensus of the histopathological findings is reached by the four pathologists to categorize the results as follows:
(1) Technically adequate if there were 2 or more full cores of target tissue or if there was significant tissue that was diagnostically relevant.
(2) Technically inadequate if there were <2 cores of the target tissue or no significant findings.
(3) No target tissue if the sample lacked target tissue and only contained diagnostically irrelevant tissue (e.g., skin or cartilage).
Structured clinical summary forms and standardized MITS sample collection forms were used to collect relevant clinical information, document the MITS procedure and the histopathological findings (Supplementary Material S2). Tissue specimens were fixed in 10% neutral buffered formalin for 24 h and stained with hematoxylin and eosin as per standard procedures. The samples were then evaluated histologically using light microscopy.
Data was initially collected on pretested case reporting forms and subsequently entered electronically on tablets. Data quality was monitored regularly. For samples from TASH, agreements on the identification of target tissue between pathologists and nurses were assessed using the first-order agreement coefficient, or the AC1 statistic which is proposed by Gwet (26). This was chosen over using Cohen's kappa due to the “kappa Paradox”, explained by Feinstein and Cicchetti (27), where a high value of observed agreement (Po) is substantially lowered due to the imbalance in the contingency table marginal totals either vertically or horizontally. This appears to be the case in our sample where Kappa is negative despite a high level of agreement. Gwet's AC1 statistic provides a chance corrected agreement coefficient which is in line with the observed level of agreement (28, 29). We used Kappa etc. package of Stata 18 (Stata Corp. 2023. Stata Statistical Software: Release 18. College Station, TX: Stata Corp LLC) to estimate Gwet's AC1 agreement coefficient and the 95% CI.
Samples collected at BGH were evaluated calculating the proportions of technically adequate or diagnostically relevant samples compared with the proportion of inadequate samples or samples containing no target tissue. Statistical significance was tested using the Chi-squared test at p < 0.05.
A total 139 MITS were conducted: 48 at TASH, 77 at BGH and 14 inside homes of rural communities within Butajira district.
During March 2020–February 2021, there were 2,527 NICU admissions and 356 NICU deaths eligible for MITS at TASH. A total of 170 families were approached, and consent was obtained for 50 (29.4%) deaths. Two cases were excluded because death occurred after the age of 28 days i.e., outside the neonatal period. Samples from 48 MITS cases were included in the final analysis.
Between March 2021 and August 2022 there were a total of 1,333 admissions and 322 deaths in BGH NICU, 150 of which were eligible, and approached for consent and 77 (51.3%) consented to MITS. Overall, consent rate was 39.7%. Due to local norms around reporting of perinatal deaths, the total number of home deaths in Butajira district during the study period could not be precisely determined; of the 18 deaths reported within the HDSS, 14 were eligible, approached and consented for MITS. Together with the home MITS, a total of 91 MITS was conducted by BGH nurses (Figure 1: Flow Diagram of Enrolment).
As shown in Table 1, a total of 139 MITS (68 males and 71 females) were conducted. There were 44 stillbirths, 36 of which occurred in hospital. Most liveborn deaths (77/94) happened within 7 days of birth. All cases had birthweight taken within 24 h of birth. Gestational age was not possible to estimate for most cases. Most neonatal deaths had a birthweight of 2,000 g or more; nine cases were extremely low birthweight (two in TASH and seven in BGH).
There was minimal or no autolysis of the samples. Both nurses and pathologists were able to perform MITS on 48 neonatal deaths and no stillbirths at TASH. Table 2 shows the number of adequate samples collected by nurses compared to pathologists. There was perfect agreement or almost perfect agreement (91.8%–100%) in terms of adequacy between samples collected by nurses and pathologists for all tissue types.
MITS samples collected by BGH nurses were evaluated using preset criteria by an independent team of pathologists. As shown in Table 3, the adequacy of MITS samples in both liveborn deaths and stillbirths combined was 72%, 78%, 82% and 79% for the brain, liver, right lung and left lung tissue samples respectively. Sample adequacy was higher in liveborn deaths at 91%, 87%, 91% and 87% for brain, liver, right lung and left lung samples respectively; compared to stillbirths with 55% sample adequacy for brain and 76% sample adequacy each for liver, right lung, and left lung samples. The difference in sample adequacy of brain tissue between neonates and stillbirths (91% vs. 55%) was significant (p < 0.05).
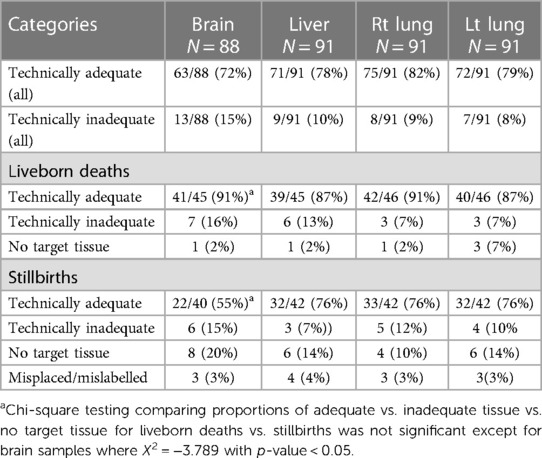
Table 3. Proportions of adequate samples of tissue collected by BGH nurses in hospital and home (N = 91).
Overall, the proportions of samples evaluated as either technically inadequate or missing target tissue was higher in stillbirths compared to neonates, 25% vs. 13.7%, respectively. The proportion of neonatal samples evaluated as technically inadequate or missing target tissue were highest in brain tissue (17.7%), followed by liver (15.5%), left lung (13%) and right lung (8.6%). Similarly, the proportion of stillbirth samples that were inadequate or lacking target tissue were highest in brain tissue (35%), followed by left lung (24.8%) and liver and right lung (21.4% each).
Table 4 shows the proportions of adequate samples of tissue collected by nurses at home only. Of the 14 MITS conducted in the home, technically adequate tissue was obtained in 79%, 86% and 93% of the liver, the left lung, and the right lung tissue samples respectively. Only 57% of brain samples were evaluated at technically adequate. The sample size was too small to calculate statistical significance. There was no target tissue in three samples for the brain.
On average, it took nurses 30.3 min to complete each MITS case including sample collection and preparation of samples for storage and transport. In contrast, on average, it took pathologists 25.2 min to complete each MITS. In addition to MITS sample collection, the nurses participated in community engagement activities for MITS, counselling families for consent, and notifying families of MITS results. Anecdotally nurses felt that families were more inclined to consent to MITS if their neonates were cared for in the NICU prior to death. Barriers to conducting MITS identified by the nurses included families' lack of awareness of MITS, family members' discomfort with the sound made by the sample collection instrument and technical challenges with electronic data entry. Overall nurses found the experience to be positive and all nurses stated that they would be supportive of broader implementation of MITS.
This is the first time a study has evaluated the feasibility and results of task-shifting MITS sample collection from pathologists to nurses. Our study showed that with standardized training and supportive supervision MITS sample collection can be conducted by nurses in a tertiary care setting, a general hospital and in the community, at the home of the deceased.
The adequacy of MITS samples collected by nurses was comparable to that of pathologists in the tertiary hospital, with perfect or almost perfect agreement. Overall, the proportion of adequate samples collected by nurses across all tissue types ranged from 91% to 100% in neonates for nurses at TASH and 87%–91% in neonates and 55%–76% in stillbirths for nurses at BGH. Observing the slightly higher proportions of adequate samples at TASH likely reflects a higher volume of MITS cases and increased opportunities for nurses to practice and hone their skills compared to BGH. Our study results showed obtaining adequate samples of brain tissue, particularly in stillbirths, was the most challenging samples for nurses to collect. While brain tissue was included as part of our sampling protocol, recent studies indicate that histological analysis of brain tissue has limited utility in determining cause of death in stillbirths. It is reasonable to reconsider the inclusion of brain tissue as part of MITS sampling in stillborn populations as part of future studies (30).
Human resource shortages in the health services are widely acknowledged as a threat to the attainment of the SDGs (1) and optimization of the existing health workforce is crucial to attain the SDGs. Redistribution of tasks and responsibilities among cadres of health workers is seen as a promising strategy for improving access and cost effectiveness within health systems. Such task-shifting or sharing strategies might be particularly attractive to countries that lack the means to improve access to care in maternal and child health, in management of malaria, tuberculosis, HIV and other conditions within short periods of time (31–33). Task shifting to nurses and midwives has been demonstrated as an effective strategy to increase access to care without compromising outcomes and reduce costs across several health issues including reducing HIV transmission through male medical circumcision (34), supporting early infant diagnosis of HIV and expanding family planning through tubal ligation (35), performing point of care HIV testing (36), and obstetric surgery (37). Key components of effective and sustainable task-shifting programs include conducting high-quality standardized training, providing ongoing supervision, utilizing quality assurance processes, ensuring potential career progression and offering incentive packages for health workers. In addition, programs need to address the distribution of roles among cadres, regulatory issues, stakeholder involvement, systems for referral, and supply chains when shifting tasks from one health worker cadre to another (38). While we were not able to implement the broader questions such as regulatory issues at this stage, our study ensured that training and supervision, supplies and incentives were fully implemented.
Our study demonstrates that task-shifting MITS sample collection to nurses is a feasible strategy to increase the use of pathology-based post-mortem examination, improve mortality data and ultimately, reduce stillbirths and neonatal mortality.
Our study had several limitations. This was a small study comparing two cadres of health professions; a randomized controlled design and a larger sample size might have provided definitive results. The total number of MITS cases performed by nurses was limited making it difficult to determine how additional practice and oversight would have impacted the adequacy of samples. This study included a limited number of histology types (lung, liver and brain). Including microbiology and additional samples such as blood and cerebral spinal likely would have impacted the results.
Our study showed that, except for brain tissue in stillbirths, nurses can conduct MITS sample collection with comparable accuracy and adequacy as pathologists. Task-shifting MITS sample collection was perceived as acceptable by the nurses participating in our study, noting that they felt competent and comfortable collecting MITS samples. We demonstrated the feasibility of conducting MITS both in a tertiary hospital, a general hospital and in the homes of the deceased. Task-shifting MITS sample collection to nurses and collecting MITS samples in community settings is an important step in paving the way for scaling-up of MITS sample collection both within and outside of health facilities. We recommend further validation of the performance of nurses as part of task-shifting of MITS on a larger scale involving both liveborn deaths and stillbirths at community levels.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Addis Ababa University IRB committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
LM: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. CP: Conceptualization, Methodology, Writing – review & editing. RA: Conceptualization, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. TD: Conceptualization, Methodology, Writing – review & editing. AM: Conceptualization, Investigation, Methodology, Writing – review & editing. AD: Investigation, Methodology, Writing – review & editing. TA: Data curation, Methodology, Supervision, Writing – review & editing. TE: Supervision, Writing – review & editing. TG: Methodology, Writing – review & editing. DT: Investigation, Methodology, Writing – review & editing. AJ: Investigation, Methodology, Writing – review & editing. AZ: Investigation, Methodology, Writing – review & editing. MS: Investigation, Writing – review & editing. LP: Investigation, Methodology, Writing – review & editing. AW: Data curation, Methodology, Writing – review & editing. AN: Investigation, Methodology, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was funded by grants from the Bill & Melinda Gates Foundation (INV-004160) and RTI international project number 0216178 (Opp-1180554).
We would like to acknowledge the support we received from the administrative, clinical, nursing, and pathology staff of TASH as well as BGH. We would like to acknowledge the contribution of the NICU head of BGH, Sister Etaferahu Teklu and all her supporting nursing staff to conduct MITS. We would like to acknowledge the contributions of the Butajira DHSS staff especially the field coordinators: Mr. Mulugetta Tadesse and Mr. Abiot Weldemariam and all health promoters. The following individuals worked as panel of experts to determine COD and we would like to acknowledge their contributions: Dr. Ayalew Moges (pediatrician) from Addis Ababa University, Ethiopia, and Hailu Berta (neonatologist) from Zewditu hospital, Ethiopia.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1278104/full#supplementary-material
1. United Nations: Sustainable Development Goals 3. Available at: https://sustainabledevelopment.un.org/sdg3
2. Ministry of health Ethiopia: health sector transformation plan II: 2020/21-2024/25. 2021. Available at: file:///C:/Users/user/AppData/Local/Temp/HSTP-II.pdf
3. Nichols EK, Byass P, Chandramohan D, Clark JC, Flaxman AD, Jakob R, et al. The WHO 2016 verbal autopsy instrument: an international standard suitable for automated analysis by InterVA, InSilicoVA, and tariff 2.0. PLoS Med. (2018) 15:e1002486. doi: 10.1371/journal.pmed.1002486
4. Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. (2006) 84(3):239–45. doi: 10.2471/blt.05.027003
5. Ganapathy SS, Khoo YY, Azahadi MO, Mohamad Anuar MF, Jeevananthan C, Rao C. Validation of verbal autopsy: determination of cause of deaths in Malaysia. BMC Public Health. (2017) 17:653. doi: 10.1186/s12889-017-4668-y
6. Garg S, Punia RPS, Basu S, Mohan H, Bal A. Comparison of needle autopsy with conventional autopsy in neonates. Fetal Pediatr Pathol. (2009) 28(3):139–50. doi: 10.1080/15513810902772482
7. Blokker BM, Wagensveld IM, Weustink AC, Oosterhuis JW, Mariahann MG. Non-invasive or minimally invasive autopsy compared to conventional autopsy of suspected natural deaths in adults: a systematic review. EurRadiol. (2016) 26:1159–79. doi: 10.1007/s00330-015-3908-8
8. Ekanem VJ, Clement O, Vhriterhire CO. Relevance of clinical autopsy in medical practice in Sub-Saharan Africa. Sahel Med J. (2015) 18:49–56. doi: 10.4103/1118-8561.160795
9. The population of Ethiopia: worldometer. Available at: https://www.worldometers.info/world-population/ethiopia-population/
10. The federal Democratic Republic of Ethiopia Ministry of Health, national human resource for health strategic plan for Ethiopia: health workforce density and distribution, page 16. Available at: https://platform.who.int/docs/default-source/mca-documents/policy-documents/plan-strategy/ETH-RH-18-02-PLAN-STRATEGY-2016-eng-National-Human-Resource-For-Health-2016-2025.pdf
11. McClure EM, Saleem S, Goudar SS, Tikmani SS, Dhaded SM, Hwang K, et al. The causes of stillbirths in south Asia: results from a prospective study in India and Pakistan (PURPOSe). Lancet Glob Health. (2022) 10(7):e970–7. doi: 10.1016/S2214-109X(22)00180-2
12. Njuguna HN, Zaki SR, Roberts DJ, Rogena EA, Walong E, Fligner CL, et al. Post-mortem study of cause of death among children hospitalized with respiratory illness in Kenya. Pediatr Infect Dis J. (2021) 40(8):715–22. doi: 10.1097/INF.0000000000003159
13. Caballero MT, Grigaites SD, De la Iglesia Niveyro PX, Esperante S, Bianchi AM, Nuño A, et al. Uncovering causes of childhood death using the minimally invasive autopsy at the community level in an urban vulnerable setting of Argentina: a population-based study. Clin Infect Dis. (2021) 73(Suppl_5):S435–41. doi: 10.1093/cid/ciab838
14. Muhe LM, McClure EM, Nigussie AK, Mekasha A, Worku B, Worku A., et al. Major causes of death in preterm infants in selected hospitals in Ethiopia (SIP): a prospective, cross-sectional, observational study. Lancet Global Health. (2019) 7:e1113–38. doi: 10.1016/S2214-109X(19)30220-7
15. Hailu R, Desta T, Muhe L, Bezabih M, Alemu A, Bekele T, et al. Minimally invasive tissue sampling in preterm deaths: a validation study. Glob Pediatr Health. (2020) 7. doi: 10.1177/2333794X20953263
16. Paganelli CR, Goco NJ, McClure EM, Banke KK, Blau DM, Breiman RF, et al. The evolution of minimally invasive tissue sampling in post-mortem examination: a narrative review. Glob Health Action. (2020) 13(1):1792682. doi: 10.1080/16549716.2020.1792682
17. Castillo P, Ussene E, Ismail MR, Jordao D, Lovane L, Carrilho C, et al. Pathological methods applied to the investigation of causes of death in developing countries: minimally invasive autopsy approach. PLoS One. (2015) 10:e0132057. doi: 10.1371/journal.pone.0132057
18. World Health Organization. Health worker roles in providing safe abortion care and post-abortion contraception. (2012). Available at: http://www.who.int/reproductivehealth/publications/unsafe_abortion/abortion-task-shifting/en/
19. Polus S, Lewin S, Glenton C, Lerberg LM, Rehfuess E, Gülmezoglu AM. Optimizing the delivery of contraceptives in low- and middle-income countries through task shifting: a systematic review of effectiveness and safety. Reprod Health. (2015) 12:27. doi: 10.1186/s12978-015-0002-2
20. Yadav V, Balasubramaniama S, Das S, Srivastava A, Kumar S, Sooda B. Comparison of outcomes at 6 weeks following postpartum intrauterine contraceptive device insertions by doctors and nurses in India: a case–control study. Contraception. (2016) 93:347–55. doi: 10.1016/j.contraception.2015.12.012
21. Lassner KJ, Chen CH, Kropsch LA, Oberle MW, Lopes IM, Morris L. Comparative study of safety and efficacy of IUD insertions by physicians and nursing personnel in Brazil. Bull Pan Am Health Organ. (1995) 29:206–15. Available at: https://pubmed.ncbi.nlm.nih.gov/8520606/8520606
22. Butajira Health and Demographic Surveillance System. Global health data exchange (GHDE). Available at: http://ghdx.healthdata.org/record/ethiopia-butajira-health-and-demographic-surveillance-system
23. MITSAllinace. MITS sample collection the standard operating procedure for MITS sample collection includes handling. MITS_Sample_Collection_SOP.pdf Standard Operating. Available at: https://mitsalliance.org/resource-center/mits-alliance-toolkit
24. Paganelli CR, Parlberg L, Goco NJ, Ritter JM, Martines RB, Zaki SR, et al. Building global capacity to conduct pathology-based postmortem examination: establishing a new training hub for minimally invasive tissue sampling. Clin Infect Dis. (2021) 73(Suppl_5):S390–5. doi: 10.1093/cid/ciab765
25. Rakilova N, Fernandes F, Lovane L, Jamisse L, Castillo P, Sanz A, et al. Standardization of minimally invasive tissue sampling specimen collection and pathology training for the child health and mortality prevention surveillance network. Clin Infect Dis. (2019) 69(4):S302–10. doi: 10.1093/cid/ciz565
26. Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. (2008) 61(1):29–48. doi: 10.1348/000711006X126600
27. Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. (1990) 43(6):543–9. doi: 10.1016/0895-4356(90)90158-L
28. Wongpakaran N, Wongpakaran T, Wedding D, Gwet K. A comparison of Cohen’s kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol. (2013) 13:61. doi: 10.1186/1471-2288-13-61
29. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33(1):159–74. doi: 10.2307/2529310
30. Goldenberg RL, Saleem S, Goudar SS, Moore J, Guruprasad G, Kulkarni V, et al. The PURPOSe cause of death study in stillbirths and neonatal deaths in India and Pakistan: a review. BJOG. (2023) 130(S3):26–35. doi: 10.1111/1471-0528.17635
31. Menendez C, Castillo P, Martinez MJ, Jordao D, Lovane L, Ismailet MR, et al. Validity of a minimally invasive autopsy for cause of death determination in stillborn babies and neonates in Mozambique: an observational study. PLoS Med. (2017) 14:e1002318. doi: 10.1371/journal.pmed.1002318
32. Bassat Q, Castillo P, Martinez MJ, Jordao D, Lovane L, Hurtadoet JC, et al. Validity of a minimally invasive autopsy tool for cause of death determination in pediatric deaths in Mozambique: an observational study. PLoS Med. (2017) 14:e1002317. doi: 10.1371/journal.pmed.1002317
33. Bascaran C, Mwangi N, D’Esposito F, Gordon I, Lopez Ulloa JA, Mdala S, et al. Effectiveness of task-shifting for the detection of diabetic retinopathy in low- and middle-income countries: a rapid review protocol. Syst Rev. (2021) 10(1):4. doi: 10.1186/s13643-020-01553-w
34. Ford N, Chu K, Mills EJ. Safety of task-shifting for male medical circumcision: a systematic review and meta-analysis. AIDS. (2012) 26(5):559–66. doi: 10.1097/QAD.0b013e32834f3264
35. Gordon-Maclean C, Nantayi LK, Quinn H, Ngo TD. Safety and acceptability of tubal ligation procedures performed by trained clinical officers in rural Uganda. Int J Gynaecol Obstet. (2013) 124(1):34–7. doi: 10.1016/j.ijgo.2013.07.016
36. Simmonds FM, Cohn JE, Mafaune HW, Nyamundaya TH, Mahomva A, Chadambuka A. Task shifting for point-of-care early infant diagnosis: a comparison of the quality of testing between nurses and laboratory personnel in Zimbabwe. Hum Resour Health. (2020) 18(1):4. doi: 10.1186/s12960-020-0449-2
37. Dawson AJ, Buchan J, Duffield C, Homer CSE, Wijewardena K. Task shifting and sharing in maternal and reproductive health in low-income countries: a narrative synthesis of current evidence. Health Policy Plan. (2014) 29(3):396–408. doi: 10.1093/heapol/czt026
38. World Health Organization. WHO recommendations: Optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. Geneva: World Health Organization (2012). Available at: http://www.who.int/iris/handle/10665/77764
Keywords: task-shifting, neonatal mortality, MITS, stillbirths, community
Citation: Muhe LM, Paganelli CR, Ayele RH, Desta T, Mekasha A, Demtse A, Awoke T, Elfu T, Gebremariam TY, Tamrat D, Jiffar AD, Zenabu AM, Sori M, Parlberg L, Worku A and Nigussie AK (2023) A prospective observational study of nurses performing minimally invasive tissue sampling of brain, liver, and lung tissues among deceased neonates and stillbirths in Ethiopia. Front. Pediatr. 11:1278104. doi: 10.3389/fped.2023.1278104
Received: 7 September 2023; Accepted: 23 November 2023;
Published: 7 December 2023.
Edited by:
Suksham Jain, Government Medical College and Hospital, IndiaReviewed by:
Shiyam Sunder Tikmani, Aga Khan University, Pakistan© 2023 Muhe, Paganelli, Ayele, Desta, Mekasha, Demtse, Awoke, Elfu, Gebremariam, Tamrat, Jiffar, Zenabu, Sori, Parlberg, Worku and Nigussie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lulu Mussa Muhe bXVoZTE5NTJAZ21haWwuY29t
Abbreviations TASH, tikur anbessa specialized hospital; BGH, butajira general hospital; MITS, minimally invasive tissue sampling; HDSS, health and demographic surveillance system; NICU, neonatal intensive care unit; SDG, sustainable development goals; CDA, complete body autopsy; Task-shifting, the process of redistributing tasks and responsibilities among cadres of health workers, referred as task shifting; Rt lung, right lung; Lt lung, left lung.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.