- 1Inter-Departmental Division of Critical Care Medicine, University of Toronto, Toronto, ON, Canada
- 2Department of Critical Care Medicine, Hospital for Sick Children, Toronto, ON, Canada
- 3Department of Paediatrics, University of Toronto, Toronto, ON, Canada
- 4Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON, Canada
- 5Child Health and Evaluative Sciences, SickKids Research Institute, Toronto, ON, Canada
- 6Centre for Safety Research, Sick Kids Research Institute, Toronto, ON, Canada
- 7Department of Critical Care Medicine, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB, Canada
- 8Department of Paediatrics, University of Pennsylvania, Philadelphia, PA, United States
- 9Department of Critical Care Medicine and O’Brien Institute for Public Health, University of Calgary & Alberta Health Services, Calgary, AB, Canada
- 10Department of Medicine and Physiology, University of Toronto, Toronto, ON, Canada
- 11Department of Medicine and Clinical Epidemiology & Biostatistics, McMaster University, Hamilton, ON, Canada
- 12Division of Critical Care Medicine, McMaster University, Hamilton, ON, Canada
- 13Division of Neonatology, Children’s Hospital of Eastern Ontario, Ottawa, ON, Canada
- 14Division of Newborn Care, The Ottawa Hospital, Ottawa, ON, Canada
- 15Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 16Clinical Research Unit, Research Institute, Children’s Hospital of Eastern Ontario, Ottawa, ON, Canada
Aim: Infants and children who require specialized medical attention are admitted to neonatal and pediatric intensive care units (ICUs) for continuous and closely supervised care. Overnight in-house physician coverage is frequently considered the ideal staffing model. It remains unclear how often this is achieved in both pediatric and neonatal ICUs in Canada. The aim of this study is to describe overnight in-house physician staffing in Canadian pediatric and level-3 neonatal ICUs (NICUs) in the pre-COVID-19 era.
Methods: A national cross-sectional survey was conducted in 34 NICUs and 19 pediatric ICUs (PICUs). ICU directors or their delegates completed a 29-question survey describing overnight staffing by resident physicians, fellow physicians, nurse practitioners, and attending physicians. A comparative analysis was conducted between ICUs with and without in-house physicians.
Results: We obtained responses from all 34 NICUs and 19 PICUs included in this study. A total of 44 ICUs (83%) with in-house overnight physician coverage provided advanced technologies, such as extracorporeal life support, and included all ICUs that catered to patients with cardiac, transplant, or trauma conditions. Residents provided the majority of overnight coverage, followed by the Critical Care Medicine fellows. An attending physician was in-house overnight in eight (15%) out of the 53 ICUs, seven of which were NICUs. Residents participating in rotations in the ICU would often have rotation durations of less than 6 weeks and were often responsible for providing care during shifts lasting 20–24 h.
Conclusion: Most PICUs and level-3 NICUs in Canada have a dedicated in-house physician overnight. These physicians are mainly residents or fellows, but a notable variation exists in this arrangement. The potential effects on patient outcomes, resident learning, and physician satisfaction remain unclear and warrant further investigation.
Introduction
Intensive care units (ICUs) provide continuous care to critically ill children and newborns. The quality of care significantly affects the survival rates and the neurocognitive outcomes of approximately 95% of children who survive an ICU admission in Canada each year (1–4). While multi-disciplinary ICU care led by intensivists may improve outcomes (5, 6), it is unclear whether increasing ICU physician engagement by mandating overnight presence of fully certified specialists is beneficial (7–9). Moreover, implementing this strategy is complicated by workforce and funding limitations. The utilization of trainees and other caregivers for staffing purposes ensures the continuous presence of in-house physicians, allowing for the timely addressing of various clinical, educational, and stakeholder-related needs.
We previously described physician staffing in Canadian pediatric ICUs (PICUs) in 2006, where it was observed that only one PICU mandated in-house call for attending intensivists (10). According to the Canadian Neonatal Network, the presence of senior in-house physicians in neonatal ICUs (NICUs) has been associated with a decreased mortality rate among newborns (11). In the intervening decade, several changes have occurred. These include new regulations on resident work hours, expectations of physician engagement, and improved outcomes following NICU and PICU admission (12–14). The objective of this study is to describe overnight staffing practices in Canadian NICUs (level 3) and PICUs.
Materials and methods
We conducted a cross-sectional survey of directors of PICUs and NICUs across Canada. Eligible ICUs were level-3 NICUs or PICUs (15). Level-3 NICUs must provide acute critical care to infants (16). We defined ICU as an area that routinely provided invasive mechanical ventilation for >48 h, and where other advanced life support therapies may be provided.
Survey design
The design of this questionnaire was informed by the results of our 2006 survey on staffing in adult ICU and PICU (10). All respondents were asked 29 items describing the ICU's capacity, technology, staffing, and duty duration; the neonatal questionnaire included one additional item related to delivery room coverage. NICU and PICU directors were also asked to describe their typical staffing, as well as the staffing that was actually observed during the month of February 2017. Institutional review board approval was obtained at the Hospital for Sick Children in Toronto prior to study initiation (approval no. 1000008569).
Survey administration
All PICUs and level-3 NICUs were identified from a report by the Canadian Institutes of Health Information (CIHI) and the Canadian Neonatal Network database. The ICU director was contacted to confirm the eligibility of the ICU and was invited to participate in the study. Surveys were sent by mail or email to be completed by the director or a delegate. Surveys were returned by mail, fax, or email to the study team between March and August 2017. A maximum of four reminders were sent by email and/or telephone.
Outcomes
The primary outcome was overnight physician coverage, defined as the presence or absence of a physician who was physically present in the hospital to provide care in the ICU overnight. Descriptions of in-house physician coverage included seniority, overnight shift duration, clinical responsibilities outside the ICU, and the availability of advance practice nurses or physician assistants. Descriptions of each ICU included the ICU type and size and the available ICU technologies. The assessment of ICU size encompassed the evaluation of the number of ministry-funded beds, the number of ventilated beds, and the annual count of patient admissions.
Data management and analyses
Surveys that lacked complete primary outcome data required ICU directors to provide clarification for missing survey responses. Response rates were calculated as the proportion of ICUs to which questionnaires were sent overall, as well as separately for NICUs and PICUs, respectively. Data were transcribed into a bespoke database (Oracle Corporation, Austin, TX, USA). Descriptive statistics were used to describe ICU characteristics, and by ICUs with and without overnight in-house coverage. The continuous data were described as median with interquartile range (IQR), while proportions were described as the number and percentage using SAS v9.4 statistical software (SAS N.C, USA).
Results
We identified 53 eligible pediatric and neonatal ICUs, and all units opted to participate in the study. The directors of each ICU confirmed their eligibility and agreed to participate. We received responses from all 19 PICUs and 34 NICUs, resulting in an overall response rate of 100%.
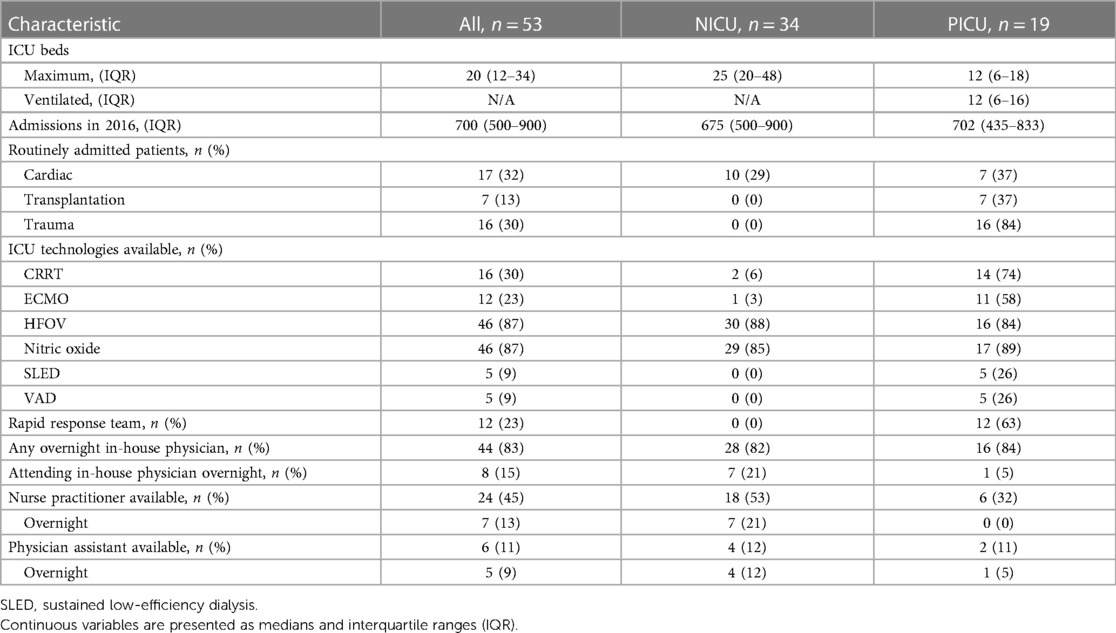
The 53 ICUs provided care for 35,457 patient admissions in 2016, ranging from 200 to 1,500 admissions annually. High frequency oscillatory ventilation (HFOV) and inhaled nitric oxide (iNO) were available in 46 (87%) ICUs. Continuous renal replacement therapy (CRRT) was available in 16 (30%) ICUs, and extracorporeal membrane oxygenation (ECMO) was available in 12 (23%) ICUs (Table 1). An ICU-based Rapid Response Team was present in association with 23% of ICUs.
The 34 (100%) NICUs had 1,141 beds with a median (IQR) of 25 (20–48) ventilated beds per ICU. In 2016, there was a total of 22,039 admissions, with a median (IQR) of 675 (500–900) admissions per ICU. HFOV was available in 30 (88%) NICUs, and iNO was available in 29 (85%) NICUs. CRRT was used in two (6%) NICUs, and one (3%) had ECMO. Nurse practitioners were employed in 18 (53%) NICUs, of which seven (21%) employed nurse practitioners overnight.
The 19 (100%) PICUs had 246 beds, including 232 beds that were allocated for mechanical ventilation. Each ICU had a median (IQR) of 12 (6–18) beds. In 2016, PICUs had 13,418 admissions, with a median (IQR) of 702 (435–833) admissions per ICU. Seven PICUs routinely admitted cardiac patients, and two were specialized Pediatric Cardiac Critical Care Units. HFOV was available in 16 (84%) PICUs, CRRT was available in 14 (74%) PICUs, ECMO was used in 11 (58%) PICUs, and five (26%) PICUs had ventricular assist devices (VAD). Six (32%) PICUs had nurse practitioners, none of which had nurse practitioners overnight. Twelve (63%) PICUs had a Rapid Response Team.
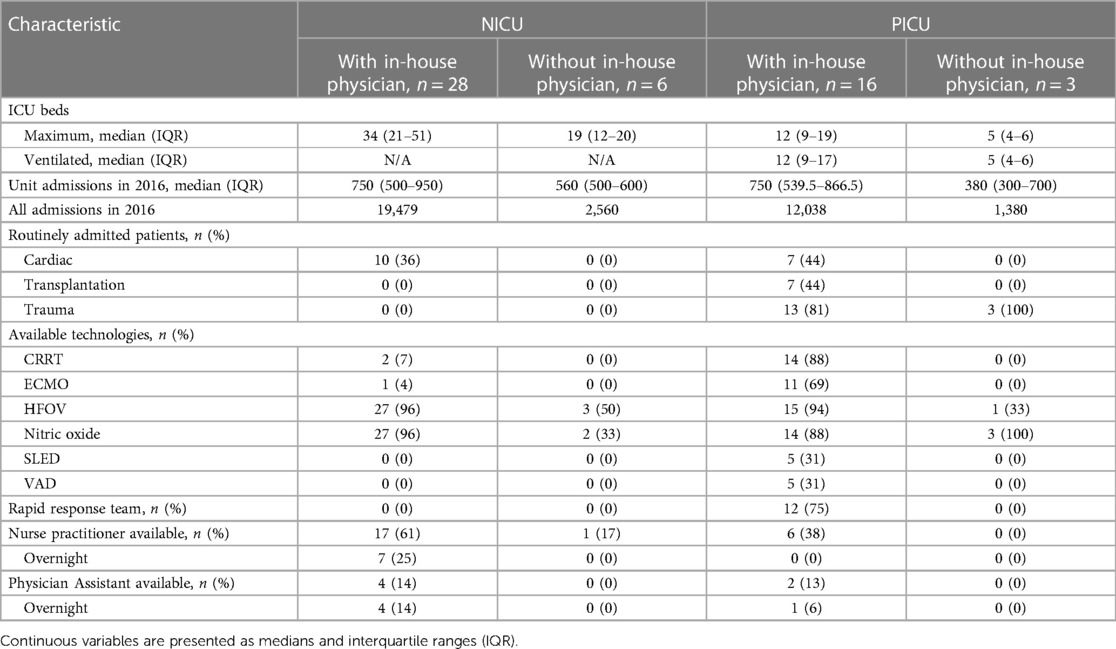
One or more overnight in-house physicians were present in 44 (83%) ICUs: 28 (82%) NICUs and 16 (84%) PICUs had overnight in-house physician coverage. ICUs with in-house physicians overnight had more ventilated beds and more admissions and offered more advanced therapeutic technologies. All ICUs providing specialized care in cardiothoracic surgery, transplant, or trauma had in-house overnight physicians (Table 2). Eight (15%) of the sites evaluated, which comprised one (5%) PICU and seven (21%) NICUs, had an attending in-house physician present overnight.
Most of the NICUs and PICUs were staffed with year 1 (R1) residents (29/53, 55%) and year 2–5 (R2–R5) residents (41/53, 77%) in February 2017 (Table 3). Half of the ICUs had dedicated Critical Care Medicine (CCM) fellows (27/53, 51%). Overnight, NICUs and PICUs were predominantly staffed by a mix of R1s, R2–R5s and CCM fellows. In the NICUs, the most senior in-house physician was often one of the following: an R2–R5 (18%), a CCM fellow (29%), a clinical associate (15%), or an attending physician (21%).
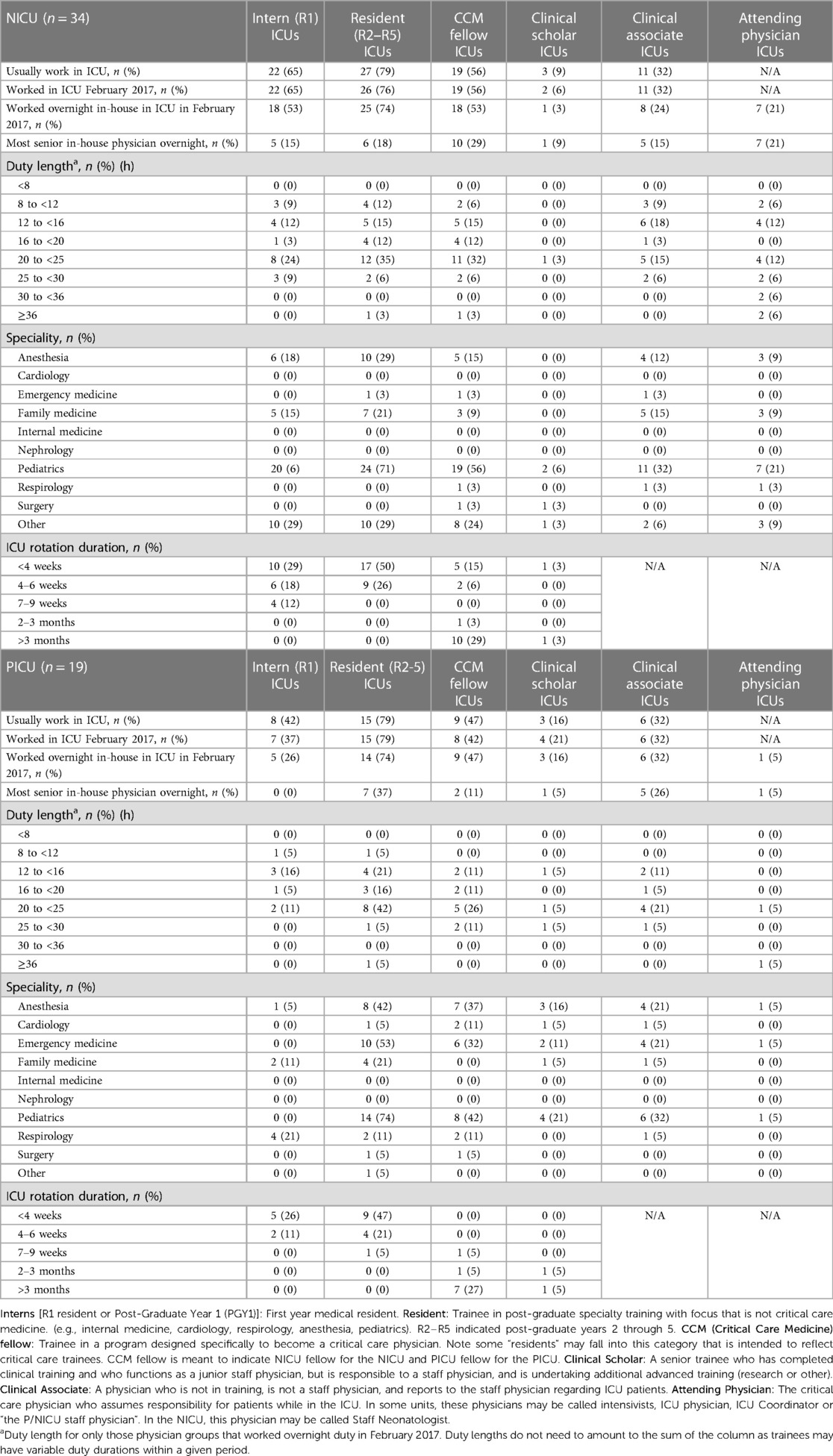
Table 3. Description of daytime and overnight in-house staffing of PICUs and NICUs in February 2017.
The ICUs were predominantly staffed by pediatric trainees or attending physicians. However, trainees from many medical specialties, including Anesthesia, Family Medicine, Emergency Medicine, and Cardiology, also participated in rotations inside both NICUs and PICUs. Most trainees provided care for periods of 6 weeks or less, except for CCM fellows working in the PICU who often worked for periods >3 months. A duty duration of 20–24 h was found to be prevalent among all types of physicians providing care, especially among R1–R5 residents, CCM fellows, and attending physicians (Table 3).
Discussion
This national cross-sectional survey of NICU and PICU staffing describes the ICU capacity and staffing patterns for neonates and children across Canada for the contemporary period prior to the COVID-19 pandemic. Eighty-three percent of all the 53 identified ICUs had a dedicated in-house physician staffing during overnight hours. This is higher than that of adult ICUs in Canada (17). We found that the NICUs and PICUs with physicians (residents, fellows, or attending physicians) in-house overnight were primarily located in either freestanding children's hospitals or in regional academic centers. In addition, these units were equipped with advanced technologies such as ECMO, VAD, and CRRT. Where in-house overnight physician staffing was available, it tended to be in larger ICUs with greater medical complexity or where advanced therapies would be administered.
Physicians working in-house overnight were predominantly pediatric residents and CCM fellows. Attending physicians were rarely mandated to be in-house overnight in NICUs, and were only required to be in-house overnight in a single PICU. There were differences between practices described in the United States, where approximately half of NICUs and PICUs have attending physicians in-house overnight. However, comparisons are limited due to significant differences in staffing task force expectations and funding (18, 19). Similar severity-adjusted mortality rates in the United States and Canada may indicate support for the staffing model with overnight trainee coverage that we report. While some studies conducted in the United States report a decrease in mortality rates in ICUs with in-house physicians present overnight, this effect is attenuated or absent in ICUs with training programs (18, 20, 21).
From an educational standpoint, staffing decisions also reflect a balance between competency for overnight coverage and progressive autonomy for trainees. The discretionary presence of the attending physician, together with the availability of in-house nurse practitioners and other trainees present overnight, may mitigate potential drawbacks from a trainee's perspective. North American trainees reported that the requirement of having an in-house attending coverage in the PICU overnight may be beneficial for their educational experience. However, there are some trainees who have expressed concerns regarding their ability to move to independent practice once their training period with in-house attending coverage ended (22). The increase in the number of overnight attending neonatologist in-house coverage in the United States has also resulted in concerns regarding the competencies of future neonatologists (23) and may serve to fuel the future “need” for in-house attending ICU physicians in NICUs and PICUs.
We found that current staffing patterns in PICUs resembled those from the results of our survey in 2006 (10, 24). In our previous study, 16 out of 18 PICUs had reported the presence of a physician on duty overnight, and one had an in-house attending physician overnight. Findings of the status quo may reflect financial implications of mandated in-house model for the healthcare system or unresolved workforce limitations. Alternatively, the clinical needs of critically ill neonates and children may simply be unchanged.
In contrast, the current NICU data suggest that overnight attending coverage may have changed over time. In 1996, a survey of 17 Canadian level-3 NICUs reported that one NICU had an in-house attending physician overnight (11) compared with the seven (21%) with an in-house attending physician overnight of the 34 NICUs we found in the current data. This finding may reflect a smaller number of NICUs with CCM fellows compared with PICUs, differences in the sampled NICUs, or other factors, such as increasing ICU care delivered to patients at lower gestational ages.
The strengths of this study include a 100% response rate, national representation, a comprehensive description of ICUs, and a direct comparison afforded by a similar prior survey. There are several limitations to this study. First, the survey did not capture the duration or frequency that attending physicians were in-house during discretionary home-call. It is probable that these attending physicians will be present at the patient’s bedside during the admission and during the management of a deteriorating critically ill neonate or child. It is possible that if actual bedside presence of attending physicians with discretionary in-house presence were assessed, an appreciable difference in patient-level outcomes between mandated and discretionary overnight presence would be unlikely. Second, the questionnaire did not assess patient outcomes such as survival, length of stay, safety events, or long-term functional outcomes. Third, the learning environment for residents and fellows was not assessed nor was their perception of readiness for independent practice. Fourth, these data reflect the practices of Canadian NICUs and PICUs in 2017. While dating a few years back, they do provide insight into the practice and training landscape prior to the COVID-19 pandemic. However, it is important to note that the survey was completed prior to the pandemic, and therefore, there might have been some changes to staffing models and overnight presence. Although significant changes due to the pandemic are unlikely in the pediatric setting, these potential modifications will be assessed in future surveys. Finally, the professional satisfaction and burnout levels of attending physicians, fellows, and residents were not captured in the survey. These issues need to be further explored.
Conclusion
We conducted a national cross-sectional survey of 34 level-3 NICUs and 19 PICUs in Canada. We documented that 83% of the ICUs have overnight in-house physicians, with these physicians predominantly being pediatric residents and fellows who work in duty periods of 24 h. Notable variation was observed among ICUs. A minority (15%) of ICUs had a constant presence of in-house attending physicians, which is consistent with the findings of our previous national survey of PICU in-house attending coverage. However, it is worth noting that the presence of attending physicians overnight may have increased in NICUs across Canada (11). Further investigation is warranted to examine the effect of the differences in physician staffing on patient care processes and outcomes, as well as trainee education and readiness for independent practice.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study protocol was reviewed and approved by the Research Ethics Board at the Hospital for Sick Children, approval number 1000008569. The study was granted exemption from informed consent from participants.
Author contributions
CM: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review and editing. KH: Writing – review & editing, Conceptualization, Project administration. JN: Writing – review & editing. SB: Conceptualization, Writing – review & editing. JG: Conceptualization, Writing – review & editing. HK: Conceptualization, Writing – review & editing. HS: Conceptualization, Writing – review & editing. NF: Conceptualization, Writing – review & editing. DC: Conceptualization, Writing – review & editing. CP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. GM: Conceptualization, Formal analysis, Investigation, Supervision, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Beltempo M, Yoon EW, Chan P, Balachandran N, Committee MotARR. The Canadian neonatal network 2018 annual report. (2019).
3. Shah PS, Mirea L, Ng E, Solimano A, Lee SK. Association of unit size, resource utilization and occupancy with outcomes of preterm infants. J Perinatol. (2015) 35(7):522–9. doi: 10.1038/jp.2015.4
4. Gaetani M, Frndova H, Seto W, Parshuram C. Pharmacotherapy in critically ill children: a retrospective review of 17,199 admissions. Pediatr Crit Care Med. (2020) 21(4):e170–6. doi: 10.1097/PCC.0000000000002236
5. Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, et al. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. (2013) 41(10):2253–74. doi: 10.1097/CCM.0b013e318292313a
6. Gajic O, Afessa B. Physician staffing models and patient safety in the ICU. Chest. (2009) 135(4):1038–44. doi: 10.1378/chest.08-1544
7. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. (2002) 288(17):2151–62. doi: 10.1001/jama.288.17.2151
8. Kerlin MP, Adhikari NK, Rose L, Wilcox ME, Bellamy CJ, Costa DK, et al. An official American Thoracic Society Systematic Review: the effect of nighttime intensivist staffing on mortality and length of stay among intensive care unit patients. Am J Respir Crit Care Med. (2017) 195(3):383–93. doi: 10.1164/rccm.201611-2250ST
9. Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. (2012) 366(22):2093–101. doi: 10.1056/NEJMsa1201918
10. Parshuram CS, Kirpalani H, Mehta S, Granton J, Cook D. In-house, overnight physician staffing: a cross-sectional survey of Canadian adult and pediatric intensive care units. Crit Care Med. (2006) 34(6):1674–8. doi: 10.1097/01.CCM.0000218808.13189.E7
11. Lee SK, Lee DS, Andrews WL, Baboolal R, Pendray M, Stewart S. Higher mortality rates among inborn infants admitted to neonatal intensive care units at night. J Pediatr. (2003) 143(5):592–7. doi: 10.1067/S0022-3476(03)00367-6
12. Namachivayam P, Shann F, Shekerdemian L, Taylor A, van Sloten I, Delzoppo C, et al. Three decades of pediatric intensive care: who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med. (2010) 11(5):549–55. doi: 10.1097/PCC.0b013e3181ce7427
13. Simpson CDA, Ye XY, Hellmann J, Tomlinson C. Trends in cause-specific mortality at a Canadian outborn NICU. Pediatrics. (2010) 126(6):e1538. doi: 10.1542/peds.2010-1167
14. Sankaran K, Chien LY, Walker R, Seshia M, Ohlsson A. Variations in mortality rates among Canadian neonatal intensive care units. CMAJ. (2002) 166(2):173–8.11826939
15. Levels of care guidance document for the neonatal intensive care unit. Guidance Document - Version 1.0. Critical Care Services Ontario. (2021). Available from: https://criticalcareontario.ca/wp-content/uploads/2021/10/NICU-Levels-of-Care-Update_Guidance-Document_FINAL-2021.pdf.
16. Neonatal Intensive Care. Critical Care Services Ontario. (2023). Available from: https://criticalcareontario.ca/about/neonatal-intensive-care/. (Accessed October 23, 2023).
17. Maratta C, Hutchison K, Moore GP, Bagshaw SM, Granton J, Kirpalani H, et al. In-house, overnight physician staffing: a cross-sectional survey of Canadian adult ICUs. Crit Care Med. (2020) 48(12):e1203–10. doi: 10.1097/CCM.0000000000004598
18. Gupta P, Rettiganti M, Rice TB, Wetzel RC. Impact of 24/7 in-hospital intensivist coverage on outcomes in pediatric intensive care. A multicenter study. Am J Respir Crit Care Med. (2016) 194(12):1506–13. doi: 10.1164/rccm.201512-2456OC
19. Sahni M, Mowes A. Effect of 24/7 attending coverage in the neonatal intensive care unit on fellow education. BMC Med Educ. (2020) 20(1):444. doi: 10.1186/s12909-020-02372-2
20. Iannucci GJ, Oster ME, Chanani NK, Gillespie SE, McCracken CE, Kanter KR, et al. The relationship between in-house attending coverage and nighttime extubation following congenital heart surgery. Pediatr Crit Care Med. (2014) 15(3):258–63. doi: 10.1097/PCC.0000000000000068
21. Gupta P, Tang X, Rettiganti M, Lauer C, Kacmarek RM, Rice TB, et al. Association of house staff training with mortality in children with critical illness. Acta Paediatr. (2016) 105(2):e60–6. doi: 10.1111/apa.13223
22. Rehder KJ, Cheifetz IM, Willson DF, Turner DA. Perceptions of 24/7 in-hospital intensivist coverage on pediatric housestaff education. Pediatrics. (2014) 133(1):88–95. doi: 10.1542/peds.2013-1990
23. Jobe AH, Martin RJ. 24/7 neonatal intensive care unit attending physician coverage: a clash of missions. Am J Respir Crit Care Med. (2010) 182(6):729–31. doi: 10.1164/rccm.201006-0884ED
Keywords: PICU (pediatric intensive care unit), NICU (neonatal intensive care unit), overnight, staffing, pediatric critical care, neonatal critical care
Citation: Maratta C, Hutchison K, Nicoll J, Bagshaw SM, Granton J, Kirpalani H, Stelfox HT, Ferguson N, Cook D, Parshuram CS and Moore GP (2023) Overnight staffing in Canadian neonatal and pediatric intensive care units. Front. Pediatr. 11:1271730. doi: 10.3389/fped.2023.1271730
Received: 2 August 2023; Accepted: 3 October 2023;
Published: 1 November 2023.
Edited by:
Heather Viamonte, Children’s Healthcare of Atlanta at Egleston, United StatesReviewed by:
Jason Custer, University of Maryland, United StatesTheresa Ann Mikhailov, Medical College of Wisconsin, United States
© 2023 Maratta, Hutchison, Nicoll, Bagshaw, Granton, Kirpalani, Stelfox, Ferguson, Cook, Parshuram and Moore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christopher S. Parshuram Y2hyaXNAc2lja2tpZHMuY2E=
 Christina Maratta
Christina Maratta Kristen Hutchison6
Kristen Hutchison6 Sean M. Bagshaw
Sean M. Bagshaw