
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr., 04 January 2024
Sec. Pediatric Urology
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1269879
This article is part of the Research TopicInsights in Pediatric UrologyView all 7 articles
Purpose: This case report aims to enhance the understanding of clinical physicians regarding splenogonadal fusion (SGF) and to help them consider SGF as a differential diagnosis when testicular tumors are suspected, thus avoiding unnecessary orchiectomies.
Methods: We report three cases of SGF admitted to our hospital, one of which presented as a suspected testicular tumor. We also searched the literature on scrotal masses from the last 25 years and summarize the characteristics of cases of SGF manifesting as scrotal swelling combined with our cases.
Results: After conducting a thorough search, we found a total of 24 publications relevant to this case study, which included 25 testes. All lesions were located on the left side, and the average age of those affected was 20.22 years. Seven cases were of the continuous type. Three cases presented with pain, all of which were intratesticular masses. Thirty cases had a definite onset duration, ranging from 3 weeks to 10 years. Nine patients (36%) underwent orchiectomy, and one underwent partial orchiectomy.
Conclusion: It is crucial to identify SGF in the clinic. When a patient presents with scrotal swelling, diagnosing SGF preoperatively is challenging, and it should be considered when there is a long history of a stable testicular mass. An intraoperative frozen section should be performed if a testicular tumor is suspected to avoid unnecessary orchiectomy.
Splenogonadal fusion (SGF) is a congenital malformation in which the spleen and gonads fuse during embryogenesis (1). SGF has two types, a continuous type and a discontinuous type, distinguished according to whether there is a connection between the two organs. Clinical physicians usually discover SGF accidentally through laparoscopic testicular exploration and preoperative ultrasonography, which reveals a laparoscopic testis attached to the spleen (2). Although there have been several reports using laparoscopic staged Fowler-Stephen (FS) surgery for SGF combined with impalpable testis, to our knowledge, we are the first to successfully detach the spleen and correct the testis using single-stage FS. When SGF presents as scrotal swelling, especially the discontinuous type, preoperative diagnosis of SGF is difficult, and some patients have undergone unnecessary orchiectomy due to misdiagnosis of SGF as a malignant tumor (3). Combining our cases with the relevant literature retrieved, we summarize the characteristics of SGF. Hopefully, this case report can enhance the understanding of this condition among doctors in urology, ultrasound, radiology, pathology, and other related departments, so they can make more accurate diagnoses and avoid overtreatment.
Case 1: A 20-month-old boy was admitted to the hospital for bilateral cryptorchidism. He had previously undergone atrial septal defect repair at the age of 8 months. Physical examination revealed bilateral impalpable testes and coronal hypospadias (Figure 1A). Preoperative ultrasound suggested bilateral intra-abdominal cryptorchidism, with the left testis positioned adjacent to the lower pole of the spleen (Figure 1B). Laparoscopic exploration revealed that both internal rings were closed, the left testis was fused with the spleen, and the diagnosis was continuous SGF (Figure 1C). The right testis was located in a flat umbilical position (Figure 1D), the gubernacular cord and vas deferens were thinly vascularized, and there was a possibility of bilateral testicular atrophy; furthermore, the urethra needed an additional operation for repair. Considering all these circumstances, the patient was considered to need three to four operations. However, the parents refused further surgery and withdrew from care, despite being informed in detail of the risk of testicular tumors.
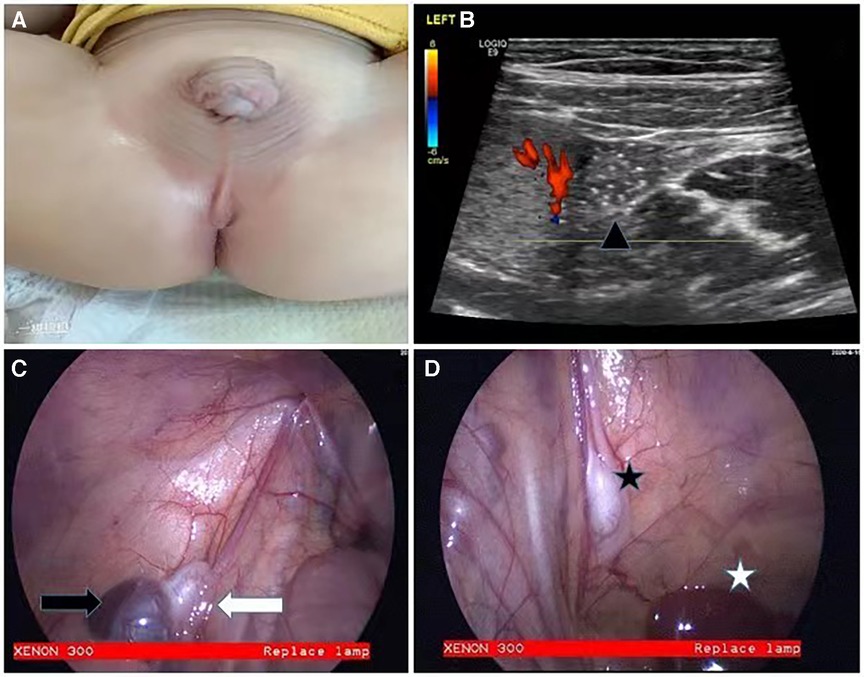
Figure 1. Appearance of case 1 and intraoperative findings. Physical examination showed bilateral impalpable testes and coronal hypospadias (A). Preoperative ultrasound suggested that the left testis was adjacent to the lower pole of the spleen (B). The left testis was fused to the spleen (C), and the right testis was located in a flat umbilical position at the lower edge of the liver (D) (Black triangle: left testis; black arrow: spleen; white arrow: left testis; black star: right testis; white star: liver.)
Case 2: A 1-year-old boy was admitted to the hospital for bilateral cryptorchidism and hypospadias (penoscrotal type). Preoperative ultrasound suggested that the boy had SGF on the left side (Figure 2A). A single-stage Fowler–Stephens orchiopexy (FSO) was performed. After confirmation of the viability of the left testicle (Figure 2B), the boy underwent another single-stage FSO to bring the right testicle down into the scrotum. This procedure was performed 9 months after initial diagnosis. Four months later, the boy underwent repair of hypospadias. Ultrasound at this time showed that both testicles were in a good position and were viable.
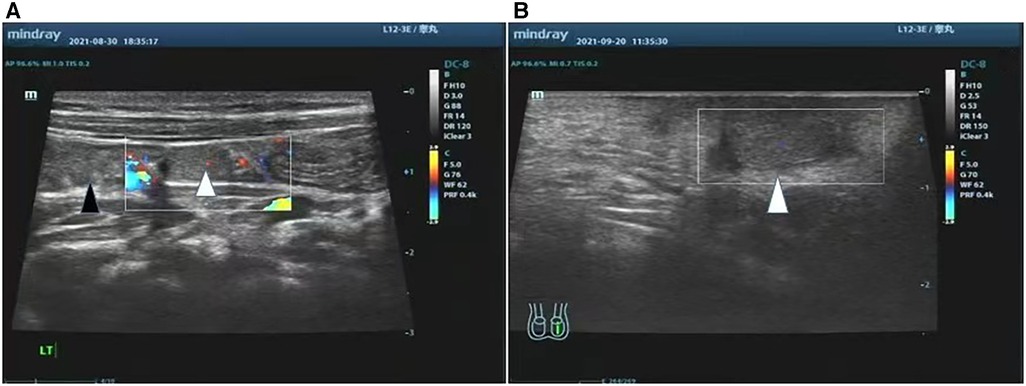
Figure 2. Pre-operative ultrasound and post-operative ultrasound of case 2 US examination of the left testis, it indicated the left testis was adjacent to the lower pole of the spleen (A). 1 month after surgery, the left testis was well positioned and survived (B). (Black triangle: spleen, white triangle: left testis).
Case 3: A 34-month-old boy was admitted to the hospital with painless enlargement of the left scrotum persisting for 2 years, with a recent slight increase in size; outpatient ultrasound revealed a testicular tumor. Physical examination suggested that, in addition to the cord-like mass in the upper pole of the left testis, a small amount of fluid could be found around the gonad (Figure 3A). There was no abnormality in the penis. After admission, the results of blood tests for tumor markers were normal. The outpatient ultrasound revealed only testicular tumors, with no hydrocele or inguinal hernia. Prior to conducting a pelvic enhanced MRI, we consulted with the radiologist to discuss any specific considerations that needed to be taken into account. During the examination, the radiologist found that the upper edge of the lesion entered the pelvic cavity along the left groin and eventually connected with the spleen (Figure 3D). Since the child was unable to cooperate with a lengthy MRI examination, no other sequences or cross-sections were added, but this observation can essentially explain the issue. Afterward, we arranged for a re-examination ultrasound. As we all know, the most common testicular tumor is teratoma, and the typical procedure for addressing it involves an inguinal or scrotal incision. This was also the procedure that we communicated to the patient’s parents prior to surgery. However, after the completion of pelvic MRI, we changed our minds based on the previous case of splenogonadal fusion. Continuous SGF was confirmed by laparoscopic exploration. A high ligation of the cord was performed, followed by a transverse incision in the left scrotum (Figure 3B). The left testis and the attached splenic cord were fully extracted, and the accessory spleen was removed while preserving the testis (Figure 3C). The presence of a fibrous capsule provides a clear demarcation between the splenic tissue and the normal testicular parenchyma, thus facilitating easier separation. Postoperative pathology confirmed the spleen. Ten days after the operation, the volume of the bilateral testes was mostly symmetrical, and the blood supply and the spleen in the abdominal cavity were good. The ultrasound was repeated three months later, and the results were the same as at the previous examination.
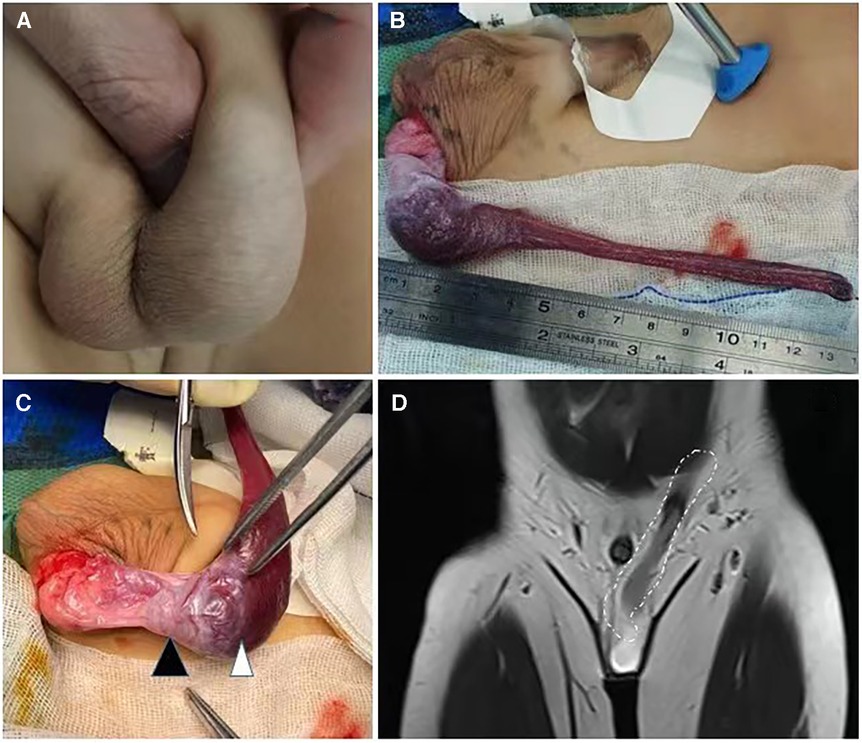
Figure 3. The appearance of case 3 and intraoperative findings On palpation of the scrotum, there was a firm mass located in the upper pole of the left testis (A). MR showed a cordlike structure extending from the upper pole of the mass to the abdominal cavity (D). The cord was ligated at a high position, and a transverse incision was taken in the left scrotum (C). The left testis and the connected splenic cord were pulled out completely (B), and the accessory spleen was removed and the testis was preserved. (White dotted circle: splenic cord, black triangle: left testis, white triangle: spleen)
The mechanism of splenogonadal fusion is not yet fully understood. The prevailing theory is that the genital crest and spleen primordium adhere or fuse during embryonic development. During the downward migration of the gonads, cases are divided into the continuous type and discontinuous type due to the breakage of fiber cords (4). It has also been suggested that splenic progenitor cells fuse with the primitive gonads via the retroperitoneal pathway, which could explain the phenomenon of right-sided non-contiguous splenogonadal fusion. Since the condition was first reported in 1883, approximately 230 cases have been reported; most of these cases were detected intraoperatively or at autopsy, and the rate of SGF detection is expected to increase with the availability of laparoscopic techniques. The male-to-female ratio is approximately 16:1, which may be an overestimate given that the male gonads are more superficial and easily examined. SGF is often combined with cryptorchidism, hypospadias, congenital heart disease, limb hypoplasia, micrognathia, and cranial anomalies. In our patients, the first two cases were combined with hypospadias and cryptorchidism. However, we performed diagnostic laparoscopy for impalpable testes, and SGF was diagnosed intraoperatively. Therefore, endocrine examination was not performed before surgery, even though karyotype analysis revealed a karyotype of 46XY. Fewer than 10 cases of SGF combined with cryptorchidism and hypospadias have been reported. Whether there is a relationship between SGF, cryptorchidism, and hypospadias requires more research.
There have been several cases of successful treatment of splenogonadal fusion combined with intra-abdominal cryptorchidism (5). However, SGF manifesting as scrotal enlargement is still mistaken for malignancy in many cases, ultimately leading to unnecessary orchiectomy. Improving awareness of the disease also makes our preoperative diagnosis more precise and avoids intraoperative changes during surgery, thus serving the best interests of the patient and their family. To this end, we searched the literature and identified 24 relevant publications (Table 1) in the last 25 years, focusing on diagnosis and treatment of SGF where testicular tumor was suspected (3, 6–28). The 24 cases in the literature plus the one case reported herein bring the total number of documented cases to 25, all left-sided, with a mean age of 20.22 years. Three cases presented with pain. We excluded one case from this count of presentations with pain because the lesion was a painless mass that had persisted for a long time before the patient was admitted with sudden pain. The remaining cases presented with painless scrotal swelling. There were 13 cases of clearly recorded duration, ranging from 3 weeks to 10 years, with no obvious change or a slight increase in swelling. Of the 25 cases, 7 (28%) were of the continuous type. In 32% of cases (8/25), the mass was located in the testis, including one case with two masses, one inside and one outside the testis (20). SGF was suspected before operation in only seven cases, of which five were of the continuous type. Finally, nine cases (36%) underwent orchiectomy, and one underwent partial orchiectomy (26). SGF patients usually have a distinct history in cases presenting as testicular tumors. The SGF mass persists for a relatively long time and takes a more variable course than testicular tumors, with fewer comorbidities, and only two of the 25 cases were combined with congenital malformations.
It is relatively challenging to distinguish the discontinuous type of SGF from testicular tumors because it often appears as a painless mass with a negative transillumination test, while the continuous type of SGF may show cord-like mass on physical examination. Laboratory tests are non-specific. Ultrasound is helpful in differentiating the two types of SGF. The continuous type usually emerges as a homogeneous mass entering the scrotum through the groin to the pelvis. In contrast, the non-continuous type usually presents as a low-reflectivity mass and may contain multiple small hypoechoic nodules, which may be associated with peak development of the lymphatic system and splenic white marrow in younger children; as a result, it has a higher diagnostic value in children aged 1–5 years who develop this condition (21). High vascular density in color Doppler flow imaging (CDFI) is helpful in the differential diagnosis of malignant tumors, and contrast-enhanced ultrasonography is also valuable in identifying benign and malignant testicular tumors (19). CT and MRI have high diagnostic value for continuous splenogonadal fusion. Sometimes, they can reveal the fibrotic tissue structure connected to the spleen and the left testis. However, no characteristic features have been observed in discontinuous splenogonadal fusion. 99mTc sulfur colloid SPECT can reveal splenic tissue in the scrotum, but surgical exploration cannot be avoided, and histological examination is still required for final confirmation of the diagnosis (3, 23). As for continuous splenogonadal fusion, we believe that laparoscopic exploration should be performed.
After confirmation of the diagnosis of SGF, the splenic cord should be resected at a high position, and the patent processus vaginalis should be ligated simultaneously to avoid hernia, splenic torsion necrosis, or internal hernia. We chose to pull out the testis and splenic cord through the scrotum, which produces better aesthetic results (avoiding the inguinal incision) and can prevent the occurrence of iatrogenic cryptorchidism. In the case of an exploratory procedure for testicular tumor, an intraoperative frozen section should be performed simultaneously to avoid radical orchiectomy. There is also controversy as to whether the pars splenium should be removed, with a report of partial preservation of the spleen due to concerns about testicular blood supply, resulting in swelling of the accessory spleen during follow-up (29). In a case of SGF presenting as a testicular tumor, it was reported that dynamic observation was continued only after a biopsy of the mass. Subsequently, the diagnosis of discontinuous splenogonadal fusion was made (18). A fibrous capsule can be clearly observed between the testes and the spleen in both the continuous and the discontinuous types. This observation is based on previous publications that have showcased specimens and pathological sections (1, 12). However, most physicians choose to remove the spleen, not only because it is easy to detach the mass from the testis, but also because of the possibility of simultaneous pathological changes in the pars splenic tissue and normal splenic tissue, as reported in two cases of viral infection causing persistent painless swelling of the spleen in the scrotum (6, 8). In some hematologic diseases, such as hemolytic jaundice, where splenectomy is mandatory, all paratenic spleens should be removed together during surgery.
Interestingly, all three patients reviewed in this paper who presented with pain had masses in the testes, presumably due to local compression (10, 22, 27). In addition, long-term compression of spleen tissue may cause infertility, as shown by a 25-year-old patient whose puncture biopsy confirmed the absence of spermatogenesis in the left testis (30). Despite reports of SGF combined with testicular tumors, the patients in all five of these cases had a history of cryptorchidism, which is a known risk factor for testicular cancer, and there is no established relationship between SGF and testicular cancer (31).
Increased awareness of SGF is crucial. SGF presenting as cryptorchidism is often diagnosed by preoperative ultrasound or intraoperatively. Laparoscopic FS staged or single-stage surgery can achieve a satisfactory result. Preoperative diagnosis of SGF manifesting as scrotal swelling is complex, and clinical physicians should consider SGF when the patient has a long history of a stable testicular mass. We recommend laparoscopic high ligation of the splenic cord, ligation of the processus vaginalis, and transscrotal separation of the splenic cord from the testis to deal with the continuous type. Transinguinal incision is better for the discontinuous type, and intraoperative biopsy is needed to avoid unnecessary orchiectomy. Regarding the decision to keep or remove the accessory spleen, performing a transinguinal incision for mass excision is recommended. This is because an extratesticular mass can be easily separated from the testis or spermatic cord, while an intratesticular mass may compress the testis, causing pain or testicular atrophy.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Ethics Board of Shenzhen Children’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardians/next of kin, for the publication of any potentially identifiable images or data included in this article.
NL: Data curation, Formal analysis, Investigation, Supervision, Writing – review & editing. QX: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. HW: Investigation, Methodology, Supervision, Writing – review & editing. JS: Data curation, Methodology, Supervision, Writing – review & editing. SL: Funding acquisition, Methodology, Resources, Supervision, Validation, Writing – review & editing.
The authors declare that financial support was received for the research, authorship, and/or publication of this article.
This study was supported by grants from the Shenzhen Fund for Guangdong Provincial High-level Clinical Key specialties (No. SZXK035) and the National Natural Science Foundation of China (Grant no. U1904208).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lin CS, Lazarowicz JL, Allan RW, Maclennan GT. Splenogonadal fusion. J Urol. (2010) 184(1):332–3. doi: 10.1016/j.juro.2010.04.013
2. Celik A, Tiryaki S, Darcan S, Ergun O. Splenogonadal fusion-limb deformity syndrome: a rare but important cause of undescended testis. World J Pediatr. (2016) 12(2):246–8. doi: 10.1007/s12519-015-0046-y
3. Guney IB, Temiz A, Oksuzler M, Alkan M. Splenogonadal fusion in children: a rare entity mimicking inguinal tumor. Clin Nucl Med. (2020) 45(6):453–4. doi: 10.1097/RLU.0000000000002989
4. Carragher AM. One hundred years of splenogonadal fusion. Urology. (1990) 35(6):471–5. doi: 10.1016/0090-4295(90)80097-7
5. Aoyagi C, Matsuoka H, Gunge N, Tominaga K, Tsubouchi K, Irie S, et al. Successful Fowler-Stephens orchiopexy for an abdominal testis associated with continuous type of splenogondal fusion: a case report. Urology. (2021) 156:e137–40. doi: 10.1016/j.urology.2021.03.040
6. Ferron SA, Arce JD. Discontinuous splenogonadal fusion: new sonographic findings. Pediatr Radiol. (2013) 43(12):1652–5. doi: 10.1007/s00247-013-2730-1
7. Kocher NJ, Tomaszewski JJ, Parsons RB, Cronson BR, Altman H, Kutikov A, et al. Splenogonadal fusion: a rare etiology of solid testicular mass. Urology. (2014) 83(1):e1–2. doi: 10.1016/j.urology.2013.09.019
8. Jayasundara JA, Vithana VH, Lamahewage AK. A case of continuous-type splenogonadal fusion. Singapore Med J. (2013) 54(6):e123–4. doi: 10.11622/smedj.2013096
9. Liu W, Wu R, Guo Z. The diagnosis and management of continuous splenogonadal fusion in a 6-year-old boy. Int Urol Nephrol. (2013) 45(1):21–4. doi: 10.1007/s11255-012-0349-z
10. Bal K, Ermete M, Balci U, Dincel C. Splenogonadal fusion: a very rare congenital anomaly in the differential diagnosis of a testicular mass. Turk J Urol. (2014) 40(1):62–4. doi: 10.5152/tud.2014.90757
11. Chiaramonte C, Siracusa F, Li Voti G. Splenogonadal fusion: a genetic disorder?—report of a case and review of the literature. Urol Case Rep. (2014) 2(2):67–9. doi: 10.1016/j.eucr.2014.01.003
12. Sountoulides P, Neri F, Bellocci R, Schips L, Cindolo L. Splenogonadal fusion mimicking a testis tumor. J Postgrad Med. (2014) 60(2):202–4. doi: 10.4103/0022-3859.132350
13. Zhou L, Muthucumaru M, Stunden R, Lenghaus D. Splenogonadal fusion: a rare scrotal mass in a 9-year-old boy. ANZ J Surg. (2018) 88(1-2):E81–E2. doi: 10.1111/ans.13250
14. Harris AM. Splenogonadal fusion: a rare benign testicular mass in a 55-year-old male. Urol Case Rep. (2016) 9:41–2. doi: 10.1016/j.eucr.2016.08.013
15. Li X, Ye J, Jiang G. Sonographic diagnosis of splenogonadal fusion in a 2-year-old boy. J Clin Ultrasound. (2017) 45(3):179–82. doi: 10.1002/jcu.22392
16. Uglialoro AD, Goltzman ME, Niazi M, Lehman D, Silletti J, Bjurlin MA. Splenogonadal fusion presenting as an asymptomatic testicular mass. Urology. (2016) 97:1–4. doi: 10.1016/j.urology.2016.07.019
17. Karray O, Oueslati A, Chakroun M, Ayed H, Bouzouita A, Cherif M, et al. Splenogonadal fusion—a rare cause of scrotal swelling: a case report. J Med Case Rep. (2018) 12(1):172. doi: 10.1186/s13256-018-1712-1
18. Shakeri A, Shakeri A, Rasolmali R, Shakeri S. A case of splenogonadal fusion accompanied by accessory spleen in a 4-year-old boy. Urol Ann. (2018) 10(4):406–8. doi: 10.4103/UA.UA_194_17
19. Grosu S, Rubenthaler J, Knosel T, Trottmann M, Marcon J, Clevert DA. Splenogonadal fusion evaluation using contrast enhanced ultrasound and elastography. A case report. Med Ultrason. (2019) 21(3):356–8. doi: 10.11152/mu-1897
20. Mann JA, Ritchie E. Splenogonadal fusion: a case of two lesions. Urol Case Rep. (2019) 24:100878. doi: 10.1016/j.eucr.2019.100878
21. Seager MJ, Alexander S, Muneer A, Walkden M. Splenogonadal fusion: a rare paratesticular lesion and how to recognise it on ultrasound. Ultrasound. (2020) 28(1):54–7. doi: 10.1177/1742271X19876085
22. Kadouri Y, Carnicelli D, Sayegh HE, Benslimane L, Nouini Y. Pathogenesis, diagnosis, and management of splenogonadal fusion: a literature review. Case Rep Urol. (2020) 2020:8876219. doi: 10.1155/2020/8876219
23. Patil SV, Patil PS, Sharma VD, Jadhav SS. Splenogonadal fusion—a rare anomaly. J Indian Assoc Pediatr Surg. (2020) 25(2):115–7. doi: 10.4103/jiaps.JIAPS_6_19
24. Daghas FA, Asiri JA, Hassine H, Ibrahim Aamry A. (99 m)Tc-sulfur colloid SPECT/CT in diagnosis of splenogonadal fusion. J Nucl Med Technol. (2022) 50(1):75–7. doi: 10.2967/jnmt.121.262233
25. Fadel MG, Walters U, Smith A, Bedi N, Davies C, Brock C, et al. Splenogonadal fusion: aiding detection and avoiding radical orchidectomy. Ann R Coll Surg Engl. (2022) 104(2):32–4. doi: 10.1308/rcsann.2021.1170
26. Alkukhun L, Ionno A, Stanton M, Serinelli S, Baker R, Hanumaiah R, et al. Splenogonadal fusion presenting as a testicular mass, a case report and literature review. Radiol Case Rep. (2022) 17(6):2191–4. doi: 10.1016/j.radcr.2022.01.065
27. Hartman NC, Trabzonlu L, Barkan GA, Quek ML. Splenogonadal fusion: a rare mimicker of malignancy. Case Rep Surg. (2022) 2022:2791305. doi: 10.1155/2022/2791305
28. Kerkeni Y, Hannachi W, Zouaoui A, Houidi S, Jouini R. Splenogonadal fusion misdiagnosed as spermatic cord cyst: a case report. Tunis Med. (2022) 100(10):730–2.36571759
29. Huang G, Huang Y, Zeng L, Yuan M, Wu Y, Huang L. Continuous-type splenogonadal fusion: a case report. Exp Ther Med. (2017) 13(5):2019–21. doi: 10.3892/etm.2017.4198
30. Al-Marhoon M, Matthew J, Nirmala V, Kehinde EO. Splenogonadal fusion associated with primary male infertility. BJU Int. (2000) 86(4):560–1. doi: 10.1046/j.1464-410x.2000.00818.x
Keywords: splenogonadal fusion, testicular tumor, intra-abdominal cryptorchidism, orchiectomy, scrotal swelling
Citation: Luo N, Xu Q, Wang H, Su J and Li S (2024) Splenogonadal fusion: a case report of three cases and a literature review. Front. Pediatr. 11:1269879. doi: 10.3389/fped.2023.1269879
Received: 31 July 2023; Accepted: 7 December 2023;
Published: 4 January 2024.
Edited by:
Lisandro Ariel Piaggio, Universidad Nacional del Sur, ArgentinaReviewed by:
Lynn Woo, Cleveland Clinic, United States© 2024 Luo, Xu, Wang, Su and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shoulin Li bGlzaG91bGluc3pAMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.