
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr. , 09 January 2024
Sec. Pediatric Urology
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1245842
As a benign disease, the incidence of epididymal cyst (EC) is 5%–25%, and it is relatively common in adults but rare in children. Although the pathogenesis of EC is still unclear, the symptoms of most asymptomatic patients can disappear with conservative treatment. EC torsion is even rarer in adults and children. Only ten cases have been reported in the literature, and we add this 3-year-old boy as the eleventh case of EC torsion. He was admitted to the hospital due to scrotum emergency without a history of EC or recent scrotal trauma. The ultrasonic examination revealed signs of an epididymal cyst. However, the pain and swelling of his scrotum were very similar to those of patients with testicular torsion, so we performed surgery on him. Therefore, EC torsion is very necessary to attract our attention as a differential diagnosis of testicular torsion in scrotal emergencies. Furthermore, our case is also the second youngest case of EC torsion.
EC is a cystic accumulation of fluid in the scrotum, which is generally considered to be benign and is usually characterized by painless swelling at the top of the testis. It is reported that the incidence is 5%–25%. ECs are thought to be relatively common in adults and rare in children, but they are more common before puberty than previously thought. At present, there is no consensus on the pathogenesis of EC, but it is generally considered to be acquired rather than congenital (1). EC can be easily diagnosed by scrotal ultrasound. The degree of scrotal swelling and whether it is accompanied by pain are usually the reasons for patients seeking medical attention. In most patients with epididymal cyst, the symptoms will disappear spontaneously after conservative treatment. In rare cases, trauma or torsion of epididymal cyst requires surgical exploration of the scrotum in order to make a clear diagnosis and timely treatment (2). EC torsion is extremely rare, and only 10 cases have been reported in the known literature (Table 1). As the second youngest EC torsion patient, the boy will become the eleventh case of EC torsion added to the literature (9).
A 3-year-old boy came to our hospital because of redness and swelling of the scrotum for one day. His parents denied a history of scrotal trauma and the child had no fever, vomiting, or urinary symptoms. Physical examination showed redness and swelling of the bilateral scrotum (Figure 1), elevated skin temperature, especially on the right side, and positive tenderness. Ultrasonography immediately showed that the echo and perfusion of the right testis were normal and no space occupying was found. The cystic hypoechoic lesion in the right scrotum was 2.5 cm × 2.1 cm without perfusion and septum could be seen in it. The left scrotal was empty, and an 1.8 × 0.8 cm testicular echo was seen in the left inguinal area. Bilateral epididymal echo and perfusion were normal (Figure 2). The white blood cell count was 12.26 × 109/L. As the boy's scrotal pain had not been relieved, and considering the high incidence of testicular torsion in scrotal emergencies and the possible impairment of testicular function, we decided to perform surgery immediately on the second day after the patient was admitted to the hospital. The patient underwent scrotal exploration under general anesthesia. After opening the edematous and thickened right scrotal membrane, we found a 2 × 2 cm dark red soft cystic mass on the upper pole of the right testis (Figure 3). The right testis and testicular appendages were normal and root torsion could be seen after fully dissociating the mass. The cyst was incised and decompressed, and dark red bloody fluid was seen flowing out. Relieve the torsion of the cyst, ligate and remove the cyst at the root, and then fix the right testis. After opening the left scrotum, we found normal left testis and testicular appendages in the left inguinal area, and performed left testicular descending fixation. Pathological examination showed fibrous tissue hyperplasia, extensive hyperemia with bleeding, and chronic inflammatory cell infiltration in the cyst (Figure 4). After operation, we continued to treat the patient with intravenous antibiotics and stopped when the patient was discharged from the hospital on the 4th day after operation. After a year of follow-up, the patient completely returned to normal.
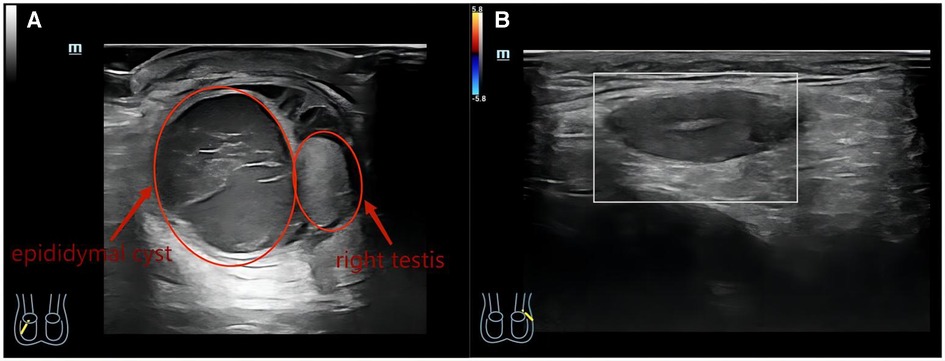
Figure 2. (A) Ultrasound image of right testis with epididymal cyst (on acute presentation). (B) Ultrasound image of the left testis in the left inguinal area.
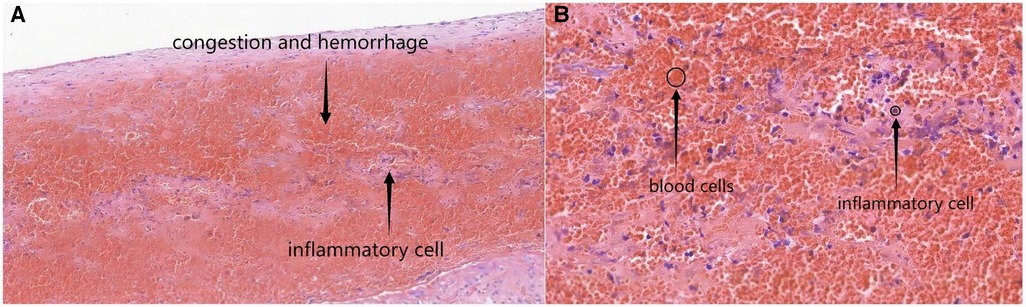
Figure 4. The microscopic views of the epididymal cyst characterized by congestion, hemorrhage and inflammatory cell [(A) HE,×100 and (B) HE,×400].
EC usually occurs in adults around the age of 40. The incidence of EC in children is 5% Mur20%, and the incidence of EC increases with age (1). Currently, EC is widely regarded as an acquired disease, such as scrotal trauma, which is why EC usually occurs in middle-aged men. However, some studies suggest that they may be congenital abnormalities caused by hormone disorders in the process of embryonic growth and development (11). It has been reported that EC is associated with cryptorchidism and VHL. As we reported in this patient,it was complicated by cryptorchidism (1). Pain and scrotal mass are the most common clinical symptoms in patients with EC, and most patients seek medical treatment because of pain or scrotal swelling. But most patients with EC are asymptomatic, so they usually take conservative treatment. In up to 60% of patients, symptoms can disappear spontaneously, particularly when EC is less than 3 mm (1, 8, 9). However, once symptoms such as acute scrotal pain, swelling, and redness occur, it should be immediately identified in testicular torsion, testicular adnexal torsion, epididymitis and other scrotal emergencies. Because it is difficult to tolerate even short-term testicular ischemia, testicular torsion has become the most urgent disease to be identified or excluded in scrotal emergencies (12).
As reported by Schalamon et al., scrotal ultrasonography is capable of distinguishing surgical emergencies from other causes in 84% of children with acute scrotal pain (13). In our case, the patient presented with typical pain and scrotal swelling in a scrotal emergency. Scrotal ultrasonography showed that while the blood perfusion of the right testis was normal, a hypoechoic mass without blood perfusion was found in the right scrotum, and the patient had persistent scrotal pain. This forced us to explore the scrotum immediately.
This is the significance of our reporting on such cases. Because scrotal emergencies often occur in children, and whether the disease is related to the testicles and whether it will have an impact on the fertility in the future is always the most concern of all people. Therefore, if we can make the correct identification as soon as possible and carry out surgical exploration in time when necessary, it will provide a great guarantee for the quality of patients’ life in the future.
Our case is unique in that he is the second youngest case of EC torsion in the literature. Liolios et al. reported the youngest case (6 months old) of EC torsion (4). Moreover, this is also the fourth case of right EC torsion reported after Bleve et al. (2), Ozaal et al. (9) and Vafadar et al. (10).
All cases reported in the literature ultimately underwent surgical exploration. Although the cases reported by Messina et al. (8), Ozaal et al. (9), and Erikçi et al. (6) chose conservative treatment at first, they all underwent surgery to effectively relieve the scrotal emergency eventually.
For patients with scrotal emergency, scrotal exploration should be carried out immediately if they have a recent history of scrotal trauma or are suspected of EC torsion. Otherwise, we should improve the ultrasound examination immediately and, if necessary, perform surgical exploration to clearly diagnose and deal with the disease.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The requirement of ethical approval was waived by West China Hospital, Sichuan University for the studies on humans because The consent of the patient's parents has been obtained. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. The human samples used in this study were acquired from a by- product of routine care or industry. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
XM and YW: performed the operation. YW: reviewed the literature. YW, XM, KW and LY: collected the data and drafted the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Erikci V, Hoşgör M, Aksoy N, Okur Ö, Yildiz M, Dursun A, et al. Management of epididymal cysts in childhood. J Pediatr Surg. (2013) 48(10):2153–6. doi: 10.1016/j.jpedsurg.2013.01.058
2. Bleve C, Conighi ML, Bucci V, Costa L, Chiarenza SF. Torsion of huge epididymal cyst in a 16-year-old boy: case report and review of the literature. Pediatr Med Chir. (2018) 40(1):20–2. doi: 10.4081/pmc.2022.279
3. Kaye RI, Cromie WJ. Torsion of a spermatocele: a case report and review of the literature. J Urol. (1990) 143(4):786. doi: 10.1016/s0022-5347(17)40094-2
4. Liolios N, Anagnostopoulos D, Sinopidis X, Vassou N, Kasselas V. Torsion of spermatocele and aplasia of the vas deferens. A case report. Eur J Pediatr Surg. (1997) 7(2):118–9. doi: 10.1055/s-2008-1071069
5. Yilmaz E, Batislam E, Bozdogan O, Basar H, Basar MM. Torsion of an epididymal cyst. Int J Urol. (2004) 11(3):182–3. doi: 10.1111/j.1442-2042.2003.00764.x
6. Erikçi V, Hoşgör M, Yıldız M, Aksoy N, Okur Ö, Örnek Y, et al. Torsion of an epididymal cyst: a case report and review of the literature. Turk J Pediatr. (2013) 55(6):659–61.
7. Ameli M, Boroumand-Noughabi S, Gholami-Mahtaj L. A 14-Year-Old Boy with Torsion of the Epididymal Cyst. Case Rep Urol. (2015) 2015:731987:1–3. doi: 10.1155/2015/731987
8. Messina M, Fusi G, Ferrara F, Bindi E, Pellegrino C, Molinaro F, et al. A rare cause of acute scrotum in a child: torsion of an epididymal cyst. Case report and review of the literature. Pediatr Med Chir. (2019) 41(1):22–3. doi: 10.4081/pmc.2019.210
9. Ozaal AMOM, Pragalathan B, Lavanya S, Sarma ST. Torsion of an epididymal cyst: a rare finding on scrotal exploration for acute scrotum. Case Rep Urol. (2020) 2020:8858606. doi: 10.1155/2020/8858606
10. Vafadar M, Rakhshankhah N, Salek M, Zarei E. Torsion of epididymal Cyst as a cause of acute Scrotum in a child. Urol Case Rep. (2023) 48:102417:1–2. doi: 10.1016/j.eucr.2023.102417
11. Boscarelli A, Bellini T. Epididymal cyst in children. Eur J Pediatr. (2021) 180(9):2723–9. doi: 10.1007/s00431-021-04080-5
12. Günther P, Rübben I. The acute scrotum in childhood and adolescence. Dtsch Arztebl Int. (2012) 109(25):449–57; quiz 458. doi: 10.3238/arztebl.2012.0449
Keywords: epididymal cyst, torsion, scrotum emergency, ultrasonic examination, conservative treatment, scrotal exploration
Citation: Wang Y, Wang K, Yu L and Ma X (2024) A rare case of scrotal emergency: torsion of epididymal cyst—a case report and literature review. Front. Pediatr. 11:1245842. doi: 10.3389/fped.2023.1245842
Received: 23 June 2023; Accepted: 21 December 2023;
Published: 9 January 2024.
Edited by:
Sajid Sultan, Sindh Institute of Urology and Transplantation, PakistanReviewed by:
Xiaokun Lin, Second Affiliated Hospital & Yuying Children’s Hospital of Wenzhou Medical University, China© 2024 Wang, Wang, Yu and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xue Ma aW1hbWF4dWVAMTYzLmNvbQ==
Abbreviation EC, epididymal cyst.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.